Abstract
Background: Studies have shown the positive effects of multidisciplinary rehabilitation on disability and health-related quality of life in multiple sclerosis (MS). However, many patients do not seek such treatment, even if it is available free of charge. The aim of this study was to identify facilitators and barriers related to use of such treatment options.
Methods: Five focus group interviews with 27 MS patients were conducted. Three groups included patients who had been admitted to a multidisciplinary MS rehabilitation institution, and two groups included outpatients of a university hospital who had not applied for specialized rehabilitation. Interviews were audiotaped and transcribed, and were analyzed qualitatively by means of a modified form of systematic text condensation.
Results: Important factors influencing the use of an MS rehabilitation service were 1) the availability and suitability of initial information about the disease and the service, 2) assumptions and expectations about such a service, and 3) practical barriers in the patient's life. The prospect of having a retreat from work and family was described as a motivational factor. Lack of reorientation after diagnosis, fears and perceptions of being labeled as an MS patient, or having information overload and being confronted with disabled individuals were identified as barriers.
Conclusions: Communication skills, including information-giving skills, of neurologists in relation to newly diagnosed MS patients need improvement. Rehabilitation programs for MS patients should include stays of different durations and purposes to fit patients' needs. Health-care authorities should take measures to secure equal access to information about rehabilitation options across institutions and practicing physicians.
In spite of improvements in immune-modulating therapy,1 multiple sclerosis (MS) remains a leading cause of neurologic disability among young and middle-aged adults.2,3 Motor and cognitive impairment, fatigue, depression, pain, incontinence, sexual dysfunction, and the unpredictability of the disease reduce health-related quality of life4–11 and participation in work and life.2,12,13 Although it has been difficult to show the effect of multidisciplinary rehabilitation stays in clinical trials,14,15 several studies have suggested a positive effect of multidisciplinary rehabilitation on disability15–21 and aspects of health-related quality of life.15,17,18,20,21 A review by Khan et al.15 concluded that there was strong evidence that inpatient or outpatient rehabilitation can increase activity and participation in society, despite a lack of reduction in actual impairment. Multidisciplinary rehabilitation has been shown to have a positive effect on measures of functional independence including locomotion, sphincter control, and self-care.16 In studies of health-related quality of life, improvement has been shown in fatigue,17,18 pain,17 general health,17 physical health,17,20,21 social function,17,21 social support,17 cognitive ability,17 and emotional well-being.20,21
Norwegian residents have the right to rehabilitation if deemed medically indicated by the municipal health authorities, who have the overall responsibility for providing general health services, care, and rehabilitation, including physiotherapy and occupational therapy.22,23 If needed, the specialized health-care system has to provide specialized rehabilitation services, including rehabilitation stays. In practice, people with MS will be offered either outpatient physiotherapy or a stay in a multidisciplinary rehabilitation institution upon admission by a neurologist or their general practitioner. The patient's resident municipality that covers costs will sometimes require limited patient payment, but most rehabilitation stays for people with MS are free of charge in Norway. Nevertheless, many people with MS do not seek such treatment, whereas others seek rehabilitation stays repeatedly. Little is known about why this is so. The aim of this study was to identify the motivational factors and barriers involved in applying for a stay in a specialized rehabilitation institution for MS.
Methods
Sites
All study participants who had applied for a rehabilitation stay were recruited at the MS Centre Hakadal (MS Centre). Participants who had not applied for a stay were recruited from the outpatient clinic at the Department of Neurology at Akershus University Hospital (Ahus).
The MS Centre is the only multidisciplinary rehabilitation institution dedicated to MS in Norway. The rehabilitation staff includes a neurologist, a physiotherapist, an occupational therapist, a social worker, a specialized nurse, and a psychologist. The program comprises both individual and group activities, and is individualized for each patient. The center is also offering 2-week introductory courses for newly diagnosed patients. Several participants had attended the center previously. A recent study showed that patients having just completed a rehabilitation stay at the MS Centre were generally satisfied and expected a major influence on physical and mental health, mastery, social participation, and general quality of life.24
The Department of Neurology at Ahus is situated 25 km from the MS Centre, and offers neurologic services to a population of approximately 500,000, including approximately 750 people with MS who are followed regularly as outpatients. In addition to consultations with a neurologist, patients may contact one of four dedicated MS nurses at the outpatient clinic. The department also offers a 1-day information program to all newly diagnosed patients. It does not, however, have a rehabilitation unit for people with MS, but rather refers to the MS Centre if a rehabilitation stay is needed. The MS Centre hires neurologists from Ahus as liaison neurologists.
Participants
Five focus group interviews with a total of 27 people with MS were performed. We aimed to include a variety of participants in terms of gender, age, and disability (Table 1). Overt cognitive impairment or severe speech difficulties were exclusion criteria.
Table 1.
Demographic characteristics of the participants
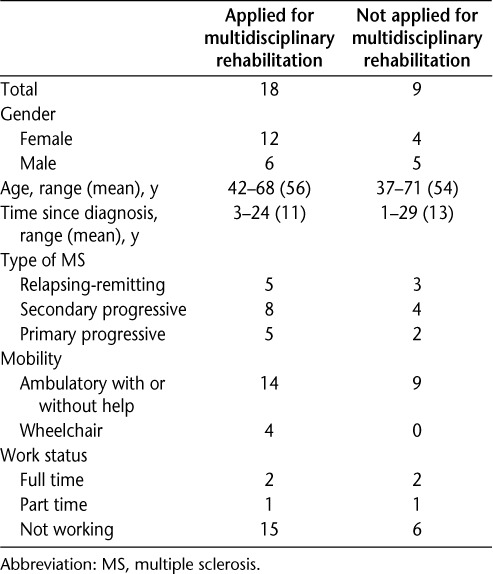
At the MS Centre, all 28 patients during one rehabilitation stay were asked to participate by a coordinating nurse, and the 18 (64%) consenting were included and allocated to three focus groups. At Ahus, potential participants spanning different MS subtypes (relapsing-remitting, secondary progressive, and primary progressive) and disease duration were identified from the hospital files by one of the authors (CBH). The inclusion criterion was never to have applied for a rehabilitation stay. Twenty-two patients were approached via a telephone call made by CBH, and nine (41%) consented. All these patients lived in the same county in which the MS Centre was located. For both groups, all who met at the interviews were included in the study.
Roles of Authors
TH is a consultant neurologist at Ahus. CBH, a resident at Ahus, was serving as a liaison neurologist at the MS Centre, and had performed a clinical interview and examination of the participants there prior to the focus group interviews. PG is an expert on clinical communication and a professor of health-services research, with no relationship to the interviewees. None of the authors were involved in the treatment of any of the participants prior to the interviews.
The study was approved by the Regional Committee for Research Ethics in South-Eastern Norway, and all participants provided written informed consent.
Data Collection
The focus group interviews lasted about 90 minutes. PG facilitated the groups, while CBH took notes. The interviews were audiotaped and transcribed verbatim by CBH, who added observed nonverbal communication to the transcripts. An interview guide was developed in advance, based on a literature review and the authors' clinical experience, including key topic areas for open discussions within the groups. We started the interviews by exploring how MS influenced the participants' family, work, and social life, as well as their identity and limitations. Then we elicited attitudes and perceptions regarding rehabilitation and the information received about the rehabilitation center and the disease. We encouraged free narratives to illuminate the research topic, while limiting interruptions from the two observers to a minimum.25 The facilitator was careful to use silence as a tool, which efficiently brought new contributions from participants, in particular the shyer ones. Questions could be formulated as open-ended statements, like “So, this MS Centre, when you heard about it, . . .” followed by a pause and subsequent specification if no one spoke, “. . . any immediate thoughts or impressions?”
Data Analysis
We used a modification of systematic text condensation as described by Malterud,25,26 which has been shown to be useful when analyzing transcripts and is also used for focus group studies with patients.27,28 First all authors formed an overall impression by reading the transcripts, finding characteristics while paying attention to their own presuppositions and assumptions. Dominating and/or common themes relating to the research topic were identified. Meaningful units in the transcripts were then distributed under the different theme categories, followed by iterative adjustment of theme names. The authors reached consensus on which final themes to emphasize in the results, with only minor disagreements that were easily resolved. The participants' statements were predominantly unequivocal, and if participants expressed ambiguity or ambivalence, they made clear that they were aware of that. Only rarely, clarity was achieved following intervention from the facilitator.
We then abstracted the content under each theme and identified quotes that illustrated the findings. In this process, we took care to check whether some participants were cited too frequently. Finally we summarized the meanings of the findings and tested their validity by going back to the material to ensure representativeness and completeness. We systematically searched for material that challenged our findings and generalizations. Respondent validation was not done. In the final manuscript, we used quantifying words (“some,” “several,” “most”) systematically.
Results
Availability and Suitability of Information
The participants had received information about the MS Centre from the neurologist, the MS nurse, local health-care workers, the general practitioner, the Internet, television, friends, family, or the patient association. Several participants knew that the MS Centre existed but had not obtained information about what a rehabilitation stay means and includes, or had not directly received the offer.
Some participants described that they felt lost in the health-care system, and that it was up to them to search for further information about rehabilitation and how to apply. Two participants, who had not applied, also lacked knowledge about regular outpatient services by a neurologist, the availability of MS nurses, and whom to contact for aid and social support. Statements like “you have to be fit to be ill” or “being a package in the system” were made by several participants: “I am a bit interested in this rehabilitation thing, especially with the MS Centre. . . . Eh, what do you emphasize there? Of course that is because I am thinking about if I should apply, and how. If it is through a neurologist in hospital or my GP or—where do you start this. And that's hard for me, because I have almost never been to a doctor before. And I find the system a bit hard, that I almost don't know what it is like to visit a doctor. Before this started” (male, aged 62 years, not applied).
An important factor reported to influence acceptance and reorientation was how the diagnosis was conveyed and whether adequate follow-up was offered. The participants underscored the importance of feeling taken care of by the doctor and the hospital for their ability to accept the diagnosis and to consider a rehabilitation stay as newly diagnosed patients. Most patients treated by a neurologic department with an organized program for disclosure of the diagnosis involving a neurologist, a specialized MS nurse, a social worker, an occupational therapist, and a physiotherapist were satisfied. The hospital's recommendation to attend a course for newly diagnosed patients was also valued. Several participants underscored the importance of involving their partner or another close relative in these settings.
Some participants had experienced an insensitive, overwhelming, or even brutal disclosure of the diagnosis, without individually adjusted explanation and follow-up. Several participants expressed the wish for a follow-up consultation shortly after receiving the diagnosis, and having questions, worries, and the feeling of being left to themselves. One participant, who had not applied for specialized rehabilitation, became very upset when he described how he experienced the communication about the diagnosis and how he had not been ready for the information about the MS Centre: “I got the message that now, death is next. I was told there is no cure. Everything was wrong. . . . And I got so much dead man talk that when I was first offered to go to the MS Centre, I said damn if I will. No way. I wasn't able to deal with that message, I don't believe it. Finished. . . . So I feel that it is off target as far as I am concerned. Because I got the impression that, ‘he hasn't understood what he has.’ That's it, I have understood, but then I haven't. It was hammered in so hard, and then I broke down [on the verge of tears]” (male, aged 45 years, not applied).
The interviews illustrated varying experiences related to communication with health-care workers regarding referral to the MS Centre. Some participants reported that they had to either argue to get an appointment for referral or convince their doctor that they were ill enough to be referred. Others reported that the doctor offered referrals both at the time of diagnosis and at follow-up visits, regardless of progression of the disease: “Yes, yes, he meant, no, yes, very mild, good type of MS. And that it couldn't be necessary. Yes, I said, but you cannot come and tell me what I feel in my legs. It's—I feel a lot, I always get—you can note that I have impaired sensitivity. Yes, it was pretty rough. Before he wrote that referral. And I think that's unnecessary” (female, aged 62 years, applied).
Even though the participants mainly appreciated being offered referrals to the rehabilitation center, some of the newly diagnosed people underscored the importance of not feeling pressure from the doctor. They were satisfied knowing about the possibility. However, others had experienced unexpected benefits of rehabilitation and retrospectively valued the encouragement to attend. Two of the participants, one who had applied and one who had not, particularly clearly described their ambivalence to rehabilitation stays when they were newly diagnosed. They were both encouraged to postpone applying until they had let the diagnosis sink in. Even though they somewhat agreed initially, in hindsight they would have appreciated more persuasive arguments and a direct offer soon after the initial information was given. The one who later applied realized that she initially had an inaccurate perception of the rehabilitation: “Yes, that they, a bit better promotion, maybe, by the neurologist and this MS nurse, I think. That it could . . . because that could in a way, have made it a bit less frightening. Because it, I thought it was somewhat scary” (female, aged 52 years, applied). “The neurologist said actually what I was thinking myself, that it was too early for you. Get to know yourself before you start taking any steps in the direction others tell you about what the disease is. But if I had got the offer, I think I would have gone there immediately” (male, aged 37 years, not applied). The reasons for not applying reported by participants with long disease duration involved concrete matters such as lack of need or the home situation, rather than inadequate communication with health-care workers.
Assumptions and Expectations
The participants revealed a range of assumptions and expectations about rehabilitation stays, which had influenced their decision-making regarding application. Some participants, both applicants and nonapplicants, stated that the fear of being labeled as an MS patient was a barrier to applying for rehabilitation. They related that they did not want to feel sicker than they were and wished to live as normally as possible, as if the disease were never there: “I think it is very much a threshold to go to such a, such a place. Or, I have heard others say about other places, if it isn't MS, and, that you make it happen, like ‘now you're like ill’” (female, aged 53 years, applied). Also, the assumption that rehabilitation focuses on needs and limitations rather than mastery and improvement was described as a barrier: “I do not want to hear any more that if I cannot brush my teeth, I will get help. Because that is the most common thing in the world. I do not need to hear that one more time” (male, aged 45 years, not applied).
The thought of listening to talks about disease was reported by some participants as a reason for not attending specialized rehabilitation. They described fear of being “bombarded” with MS facts and negativity for a week or longer, and that information overload could break them down or dominate their life: “Yes, it can appear so frightening, to be bombarded with MS, for many days in a week at a stretch” (male, aged 44 years, not applied). Most participants who had attended the rehabilitation center did not share this view. They even thought that all newly diagnosed patients should be offered a stay, and that it was an advantage that the center was only for people with MS. They underscored the value of getting important knowledge early—for example, to realize that they would not necessarily become totally dependent or die from MS—getting advice about career choices, and so on. However, as can be seen from the dialogue below, the possibility of with-drawing from some of the courses if the information was “too much” came up during the interviews, an option some participants would have appreciated knowing in advance: “But, I do not want to have too much to hear. . . . when maybe that disease dominates your whole day . . . that you're going to go around thinking about it all the time . . . you would have to filter” (male, aged 50 years, applied). “That's completely possible” (female, aged 56 years, applied). “Yes, yes. But when we get here so, so, you'd better be part of everything. Right, because you don't know if it is mandatory or not” (male, 50 years, applied). Some participants described fear of being confronted with disabled people when applying for the first time. In this context the word “wheelchair” came up several times during the interviews: “Yes, no, certainly when you hear about MS, the first thing is, you know, wheelchair. You know, I didn't know much. I didn't know anything about that disease before I started reading” (female, aged 62 years, applied).
Following acceptance and reorientation after diagnosis, positive expectations about rehabilitation dominated. Several participants with long disease duration were attracted by having a 4-week retreat from work, home, and family, being surrounded by a multidisciplinary MS team. They favored being able to focus on their own physical and psychological health, and gaining knowledge about MS and how to live with the disease. The prospect of breaking passivity and connecting to other people with MS was also regarded as attractive. Such expectations also motivated them to re-apply for further stays, and several participants had attended the center several times. For these people the quality of the physiotherapy, getting help with social matters, and sharing experiences, understanding, and acceptance with other people with MS were emphasized: “So I had to pull myself together and say that, if you're going to function at all in life ahead, you'll just have to make an effort yourself. I thought I'd get a kick in the ass here at this house. And that's what I've got” (male, aged 54 years, applied). “We are allowed to and need to take a break from everyday chores, to come here and meet others, plus we get very good training and continuation of previous training from last time here. Which we would not have received in another hospital, because I don't think they could manage, to follow up and have the competence to provide” (female, aged 53 years, applied).
Life Situation
Whereas some people with MS welcome a rehabilitation stay as a retreat from everyday life, others feel that this is not compatible with their work or family life. Several participants reported that caring for small children, elderly parents, or other family members, including a child with Down syndrome and a husband with diabetes, prohibited a rehabilitation stay. They also expressed wishes and suggested possible solutions to overcome these obstacles: “Eh, I'd like to have a bit more . . . flexible options for rehabilitation. Like what would you say, weekend allowances and, and maybe I could have stayed a little back home. . . . Could have delivered children in the morning and, so that my husband could have left for his job and he could have fetched them. Impossible for us with small children now” (female, aged 37 years, not applied).
Although the rehabilitation stay is free of charge for the participants, private economy may be an obstacle, especially for those who are self-employed: “I have to take a week off, that'll cost me 40,000 crowns. There aren't any wages, that I can receive money while I am on a stay” (male, aged 45 years, not applied). For several participants the same factors, especially having small children or being self-employed at the time of diagnosis, seemed to make reorientation complicated and made them keep distance from the disease: “I did not want to have anything to do with the disease the first 8 years. My daughter was only 4 when I got the diagnosis. So the first 8 years, each time the MS Journal arrived, it went directly into the garbage” (female, aged 42 years, applied).
Discussion
The aim of this study was to identify motivational factors and barriers related to applying for a stay in a specialized rehabilitation institution for MS, in order to facilitate the inclusion of patients with need and a potential benefit from rehabilitation. We found important factors influencing application to the MS Centre to be 1) the availability and suitability of initial information about the disease and the service, 2) the participants' assumptions and expectations about such a service, and 3) practical barriers in the patient's life. Health-care providers may influence some of these factors.
To our knowledge, this is the first study on this topic in MS. Clark et al.29 performed a qualitative systematic review of attendance at cardiac rehabilitation programs after referral. Barriers to attendance, consistent with our findings, were the lack of personal knowledge of services, beliefs about disease, patient identity, and financial, family, and work constraints. They concluded that decisions to attend were influenced more by social factors than by health professional advice or clinical information. In our study, direct communication between the person with MS and health-care professionals played a prominent role.
How the participants got the information about the MS Centre and what the information included seemed random. We suggest better organization of information about such a service in order to reach more patients. This would require neurologists, specialized MS nurses, physiotherapists, and general practitioners to be aware of and updated about the service and to make sure that patients receive direct offers repeatedly, adjusting the information to the patient's situation and receptiveness. This is in line with studies of participation in physical activities among people with MS and other chronic diseases.30–34 Also, the need for improvement in information throughout the whole patient's disease course is highlighted in several surveys on patient satisfaction,35–38 especially involving cancer patients.35,37,38
Our study demonstrates that lack of individually adjusted explanation and immediate follow-up when the patient receives the diagnosis of MS can lead to major fears and aversions to everything concerning the disease, including rehabilitation. Also, communication with health-care workers regarding referral to MS rehabilitation played an important role in participants' consideration of an application. These findings illustrate the importance of patient-centered communication, taking into account the individuals' different needs, level of reorientation, and feelings and perceptions, both when receiving and when giving information.39 This is consistent with the qualitative study of Kayes et al.40 on facilitators and barriers related to engagement in physical activity for people with MS. We suggest that an immediate follow-up visit could facilitate reorientation after diagnosis and make the patient more receptive to information about rehabilitation. The decision to apply for a rehabilitation stay is well suited for shared decision making between physician and patient.41 One prominent observation in this study was that the perceived barriers to application were reported among applicants as well as nonapplicants, showing that individuals emphasize motivational factors and barriers differentially. There was no uniform characteristic of patients that could predict how they acted, which emphasizes the importance of the health-care provider's ability to uncover the patients' perspectives. Unfortunately, most specialist physicians are still not well trained in modern principles of communication with patients.42
For several participants a 4-week stay was not compatible with work and family life. There is a concern that offering mainly 4-week inpatient stays might lead some people with MS to more easily accept a “sick role” and reduce normal activities on a permanent basis. Notably, none of the participants mentioned increased ability to work as a motivating factor, whereas several participants were attracted by the prospect of repeated 4-week retreats from normal social life. Hence more flexible solutions should be sought.
Because of the adjacency of the MS Centre to Ahus and to the residency of the nonapplicants, we assume that they were probably more likely to have received information about the center than MS patients in other parts of Norway. All participants received some regular health care, which could have implications for the representativeness of the nonapplicants. Some bias may have been introduced, as the MS Centre participants had been examined by the first author at arrival; however, she was not otherwise involved in their treatment. Moreover, the participants had no relationship to the group moderator, who observed that the participants talked freely and expressed critical and divergent views, demonstrating trust in the first author and each other. This indicates that there was not a severe lack of information. The total number of participants in the study was relatively low but included applicants and nonapplicants with varied social, disease-related, and demographic backgrounds. It was difficult to recruit nonapplicants with long disease duration, possibly suggesting that this project was of less interest to such patients.
We did not use member check (respondent validation), which could have led to correction of misinterpretations. However, participants have individual perspectives, while our research process aimed to identify typical patterns across individuals. A member check could also lead to biased conclusions.43,44
The referring physicians' perspectives were not explored in this study. It is likely that the physicians' perceptions of rehabilitation would, like those of the patients, depend on their awareness and knowledge of the rehabilitation services. In a study from general practice, low knowledge was a barrier to referring people with chronic obstructive pulmonary disease to pulmonary rehabilitation.45
Conclusion
The findings of this study indicate the need for improvements of the organization and provision of information about rehabilitation of people with MS. There also seems to be potential for better physician communication skills, particularly in the initial phase of the disease. Moreover, there is a need for a broader repertoire of rehabilitation stays. This study could provide a basis for a survey of motivational factors and barriers related to rehabilitation treatment in MS patients.
PracticePoints.
Physicians should be sure to explore the patient's reactions to, understanding of, and expectations about MS and its treatment before presenting treatment options.
Rehabilitation of MS patients should include stays of different duration and purposes to fit patients' needs.
Health-care authorities should take measures to secure equal access to information about rehabilitation options across institutions and practicing physicians.
Acknowledgments
The authors wish to thank the participants, as well as Anne Kristin Posti (for recruitment and facilitation of the study at the MS Centre Hakadal), Antonie G. Beiske (leader of the MS Centre Hakadal), and Jan C. Frich (for valuable advice on the qualitative analysis).
Footnotes
Financial Disclosures: The authors have no conflicts of interest to disclose.
References
- 1.Curtin F, Hartung HP. Novel therapeutic options for multiple sclerosis. Expert Rev Clin Pharmacol. 2014;7:91–104. doi: 10.1586/17512433.2014.865517. [DOI] [PubMed] [Google Scholar]
- 2.DeLuca J, Nocentini U. Neuropsychological, medical and rehabilitative management of persons with multiple sclerosis: 20th anniversary article. Neuro Rehabil. 2011;29:197–219. doi: 10.3233/NRE-2011-0695. [DOI] [PubMed] [Google Scholar]
- 3.Ramagopalan SV, Sadovnick AD. Epidemiology of multiple sclerosis. Neurol Clin. 2011;292:207–217. doi: 10.1016/j.ncl.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 4.Pfennings L, Cohen L, Adèr H et al. Exploring differences between subgroups of multiple sclerosis patients in health-related quality of life. J Neurol. 1999;246:587–591. doi: 10.1007/s004150050408. [DOI] [PubMed] [Google Scholar]
- 5.Shawaryn MA, Schiaffino KM, LaRocca NG, Johnston MV. Determinants of health-related quality of life in multiple sclerosis: the role of illness intrusiveness. Mult Scler. 2002;8:310–318. doi: 10.1191/1352458502ms808oa. [DOI] [PubMed] [Google Scholar]
- 6.Zivadinov R, Zorzon M, Tommasi MA et al. A longitudinal study of quality of life and side effects in patients with multiple sclerosis treated with interferon beta-1a. J Neurol Sci. 2003;216:113–118. doi: 10.1016/s0022-510x(03)00225-9. [DOI] [PubMed] [Google Scholar]
- 7.Benedict RHB, Wahlig E, Bakshi R et al. Predicting quality of life in multiple sclerosis: accounting for physical disability, fatigue, cognition, mood disorder, personality, and behavior change. J Neurol Sci. 2005;231:29–34. doi: 10.1016/j.jns.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 8.Rudick RA, Miller D, Clough JD et al. Quality of life in multiple sclerosis: comparison with inflammatory bowel disease and rheumatoid arthritis. Arch Neurol. 1992;49:1237–1242. doi: 10.1001/archneur.1992.00530360035014. [DOI] [PubMed] [Google Scholar]
- 9.Vitkova M, Rosenberger J, Krokavcova M et al. Health-related quality of life in multiple sclerosis patients with bladder, bowel and sexual dysfunction. Disabil Rehabil. 2013;20:1–6. doi: 10.3109/09638288.2013.825332. [DOI] [PubMed] [Google Scholar]
- 10.Mitchell AJ, Benito-Leon J, Gonzalez JMM, Rivera-Navarro J. Quality of life and its assessment in multiple sclerosis: integrating physical and psychological components of wellbeing. Lancet Neurol. 2005;4:556–566. doi: 10.1016/S1474-4422(05)70166-6. [DOI] [PubMed] [Google Scholar]
- 11.Beiske AG, Naess H, Aarseth JH et al. Health-related quality of life in secondary progressive multiple sclerosis. Mult Scler. 2007;13:386–392. doi: 10.1177/13524585070130030101. [DOI] [PubMed] [Google Scholar]
- 12.Strober LB, Christodoulou C, Benedict RHB et al. Unemployment in multiple sclerosis: the contribution of personality and disease. Mult Scler. 2012;18:647–653. doi: 10.1177/1352458511426735. [DOI] [PubMed] [Google Scholar]
- 13.Hornarmand K, Akbar N, Kou N, Feinstein A. Predicting employment status in multiple sclerosis patients: the utility of the MS functional composite. J Neurol. 2011;258:244–249. doi: 10.1007/s00415-010-5736-8. [DOI] [PubMed] [Google Scholar]
- 14.Storr LK, Sørensen PS, Ravnborg M. The efficacy of multidisciplinary rehabilitation in stable multiple sclerosis patients. Mult Scler. 2006;12:235–242. doi: 10.1191/135248506ms1250oa. [DOI] [PubMed] [Google Scholar]
- 15.Khan F, Turner-Stokes L, Ng L et al. Multidisciplinary rehabilitation for adults with multiple sclerosis. Cochrane Database Syst Rev. 2007;2:CD006036. doi: 10.1002/14651858.CD006036.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khan F, Pallant JF, Brand C, Kilpatrick TJ. Effectiveness of rehabilitation intervention in persons with multiple sclerosis: a randomised controlled trial. J Neurol Neurosurg Psychiatr. 2008;79:1230–1235. doi: 10.1136/jnnp.2007.133777. [DOI] [PubMed] [Google Scholar]
- 17.Di Fabio RP, Choi T, Soderberg J, Hansen CR. Health-related quality of life for persons with progressive multiple sclerosis: influence of rehabilitation. Phys Ther. 1997;77:1704–1716. doi: 10.1093/ptj/77.12.1704. [DOI] [PubMed] [Google Scholar]
- 18.Di Fabio RP, Soderberg J, Choi T et al. Extended outpatient rehabilitation: its influence on symptom frequency, fatigue, and functional status for persons with progressive multiple sclerosis. Arch Phys Med Rehabil. 1998;79:141–146. doi: 10.1016/s0003-9993(98)90290-8. [DOI] [PubMed] [Google Scholar]
- 19.Freeman JA, Langdon DW, Hobart JC, Thompson AJ. The impact of inpatient rehabilitation on progressive multiple sclerosis. Ann Neurol. 1997;42:236–244. doi: 10.1002/ana.410420216. [DOI] [PubMed] [Google Scholar]
- 20.Craig J, Young CA, Ennis M et al. A randomised controlled trial comparing rehabilitation against standard therapy in multiple sclerosis patients receiving intravenous steroid treatment. J Neurol Neurosurg Psychiatr. 2003;74:1225–1230. doi: 10.1136/jnnp.74.9.1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Freeman JA, Langdon DW, Hobart JC, Thompson AJ. Inpatient rehabilitation in MS; do the benefits carry over into the community? Neurology. 1999;52:50–56. doi: 10.1212/wnl.52.1.50. [DOI] [PubMed] [Google Scholar]
- 22.Norwegian Directorate of Health. Habilitering og rehabilitering [Guidelines in Norwegian] www.helsenorge.no. Accessed January 30, 2014.
- 23.Law on Municipality Healthcare 2011, Chapter 6 on collaboration with specialist healthcare, and Law on Specialist Healthcare 1999, Chapter 2 on division of responsibility, and derived joint regulations on habilitation and rehabilitation and division of costs. www.lovdata.no [Website in Norwegian]. Accessed January 30, 2014.
- 24.Holmøy T, Hanssen KT, Beiske AG. Patient satisfaction in rehabilitation of patients with multiple sclerosis. Tidsskr Nor Legeforen. 2012;132:523–526. doi: 10.4045/tidsskr.11.1043. [DOI] [PubMed] [Google Scholar]
- 25.Malterud K. Systematic text condensation: a strategy for qualitative analysis. Scand J Public Health. 2012;40:795–805. doi: 10.1177/1403494812465030. [DOI] [PubMed] [Google Scholar]
- 26.Giorgi A. Sketch of a psychological phenomenological method. In: Giorgi A, editor. Phenomenology and Psychological Research. Pittsburgh, PA: Duquesne University Press; 1985. pp. 8–22. [Google Scholar]
- 27.Aamland A, Werner E, Malterud K. Sickness absence, marginality, and medically unexplained symptoms: a focus-group study of patients' experiences. Scand J Prim Health Care. 2013;31:95–100. doi: 10.3109/02813432.2013.788274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Widarsson M, Kerstis B, Sundquist K, Engström G, Sarkadi A. Support needs of expectant mothers and fathers: a qualitative study. J Perinat Educ. 2012;21:36–44. doi: 10.1891/1058-1243.21.1.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clark AM, King-Shier KM, Thompson DR et al. A qualitative systematic review of influences on attendance at cardiac rehabilitation programs after referral. Am Heart J. 2012;164:835–845. doi: 10.1016/j.ahj.2012.08.020. [DOI] [PubMed] [Google Scholar]
- 30.Brown C, Kitchen K, Nicoll K. Barriers and facilitators related to participation in aquafitness programs for people with multiple sclerosis: a pilot study. Int J MS Care. 2012;14:132–141. doi: 10.7224/1537-2073-14.3.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rimmer JH, Riley B, Wang E et al. Physical activity participation among persons with disabilities: barriers and facilitators. Am J Prev Med. 2004;26:419–425. doi: 10.1016/j.amepre.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 32.Becker H, Stuifbergen AK. What makes it so hard? Barriers to health promotion experienced by people with multiple sclerosis and polio. Fam Community Health. 2004;27:75–85. doi: 10.1097/00003727-200401000-00008. [DOI] [PubMed] [Google Scholar]
- 33.Elsworth C, Dawes H, Sackley C et al. A study of perceived facilitators to physical activity in neurological conditions. Int J Ther Rehabil. 2009;16:17–24. [Google Scholar]
- 34.Stuifbergen A, Rogers S. Health promotion: an essential component of rehabilitation for persons with chronic disabling conditions. Recov Rehabil. 1997;19:1–20. doi: 10.1097/00012272-199706000-00002. [DOI] [PubMed] [Google Scholar]
- 35.Iversen HH, Holmbøe O, Dahle KA. Cancer patients' experiences with somatic hospitals in 2009: national results. Oslo, Norway: Norwegian Knowledge Centre for the Health Services; 2010. [Google Scholar]
- 36.Skudal KE, Holmbøe O, Iversen H Inpatients' experiences with Norwegian hospitals: national results in 2011 and changes from 2006. Oslo, Norway: Norwegian Knowledge Centre for the Health Services; 2012. [Google Scholar]
- 37.Amazian K, Toughrai I, Benmansour N et al. Cancer patient satisfaction survey in a Moroccan University hospital. Sante Publique. 2013;25:627–632. [PubMed] [Google Scholar]
- 38.Naidoo J, Hayes E, Teo MY et al. An Irish breast cancer survivorship study: are we meeting our patients' needs? Ir Med J. 2013;106:262–266. [PubMed] [Google Scholar]
- 39.Fortin AH, VI, Dwamena FC, Frankel RM, Smith RC. Smith's Patient-Centered Interviewing: An Evidence-Based Method. 3rd ed. New York, NY: McGraw Hill Lange; 2012. [Google Scholar]
- 40.Kayes NM, McPherson KM, Schluter P et al. Exploring the facilitators and barriers to engagement in physical activity for people with multiple sclerosis. Disabil Rehabil. 2011;33:1043–1053. doi: 10.3109/09638288.2010.520801. [DOI] [PubMed] [Google Scholar]
- 41.Edwards A, Elwyn G. Shared Decision-Making in Health Care: Achieving Evidence-Based Patient Choice. 2nd ed. Oxford, UK: Oxford University Press; 2009. [Google Scholar]
- 42.Gulbrandsen P, Dalby AML, Ofstad EH, Gerwing JJ. Confusion in and about shared decision-making in hospital encounters. Patient Educ Couns. 2014;96:287–294. doi: 10.1016/j.pec.2014.07.012. [DOI] [PubMed] [Google Scholar]
- 43.Mays N, Pope C. Assessing quality in qualitative research. BMJ. 2000;320:50–52. doi: 10.1136/bmj.320.7226.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Barbour RS. Checklists for improving rigour in qualitative research: a case of the tail wagging the dog? BMJ. 2001;322:1115–1117. doi: 10.1136/bmj.322.7294.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Johnston KN, Young M, Grimmer KA et al. Barriers to, and facilitators for, referral to pulmonary rehabilitation in COPD patients from the perspective of Australian general practitioners: a qualitative study. Prim Care Respir J. 2013;22:319–324. doi: 10.4104/pcrj.2013.00062. [DOI] [PMC free article] [PubMed] [Google Scholar]


