Abstract
The formulation and delivery of biopharmaceutical drugs, such as monoclonal antibodies and recombinant proteins, poses substantial challenges owing to their large size and susceptibility to degradation. In this Review we highlight recent advances in formulation and delivery strategies — such as the use of microsphere-based controlled-release technologies, protein modification methods that make use of polyethylene glycol and other polymers, and genetic manipulation of biopharmaceutical drugs — and discuss their advantages and limitations. We also highlight current and emerging delivery routes that provide an alternative to injection, including transdermal, oral and pulmonary delivery routes. In addition, the potential of targeted and intracellular protein delivery is discussed.
In the past three decades since the launch of recombinant human insulin, biopharmaceutical drugs — including peptides, recombinant therapeutic proteins, enzymes, monoclonal antibodies and antibody–drug conjugates — have transformed the pharmaceutical industry. From 1989 to 2012 the number of marketed biotechnology products grew from 13 to 210, while worldwide product sales increased to US$163 billion1. Biotech products accounted for 71% of the worldwide revenue generated by the ten top-selling pharmaceuticals in 2012, up from 7% in 2001 (REF. 1). This transformation has similarly affected development pipelines. Over 900 biopharmaceutical products are currently in development, targeting diseases across a wide range of therapeutic areas and representing nearly 20% of the total number of drugs in the pipeline2. About 40% of these products are being developed by large pharmaceutical companies1.
As a class, biopharmaceutical drugs offer the advantages of high specificity and potency compared to small molecules. These features arise from their macromolecular nature, which provides the structural complexity that is often required for specificity. However, this structural complexity also makes them some of the most challenging molecules to formulate and deliver. Indeed, the formulation and delivery issues of biopharmaceuticals were recognized as major potential liabilities from the earliest days of biotechnology, which partly made them less appealing drug candidates. Loss of activity in response to environmental triggers such as moisture or temperature, which can occur during storage or in the body, puts a substantial burden on formulation technologies. The high molecular mass of biopharmaceutical drugs also creates delivery challenges, namely a substantial reduction in permeability across biological barriers such as skin, mucosal membranes and cell membranes, which means that injection is currently the primary mode of administration. Delivery of biopharmaceutical drugs to specific sites — for example, intracellular targets — is also challenging owing to their poor membrane permeation3.
In spite of these challenges, novel parenteral formulations and delivery strategies have enabled the launch onto the market of numerous successful products, including products based on luteinizing hormone-releasing hormone (LHRH; also known as GnRH) analogues, such as leuprolide depot (Lupron Depot; AbbVie). This suggests that the advantages of biopharmaceuticals far exceed their limitations. This Review highlights the recent progress and unmet needs in the formulation and delivery of biopharmaceutical drugs. The advances reviewed here suggest that biopharmaceutical drugs will have an even greater impact in the future if the remaining unmet needs are addressed.
Advanced formulations and chemistry
Intravenous, intramuscular and subcutaneous injections are currently the most commonly used ways of delivering biopharmaceuticals. Subcutaneous injections are the most convenient as they require minimal skills and are the least invasive, whereas intramuscular injections are commonly used for vaccines. Intravenous injections are generally used for biopharmaceutical drugs such as monoclonal antibodies. Regardless of the type of injection, many biopharmaceutical drugs (with a few exceptions, such as monoclonal antibodies) are rapidly cleared from the body, meaning that frequent injections are required. Several strategies have been developed to address this challenge and are summarized below (BOX 1).
Box 1 | Challenges in the design of injectable formulations.
The formulation and handling of biopharmaceutical drugs poses unique challenges that are not often experienced with small molecules. One of the key challenges is overcoming the instability of the biologic, which is caused by aggregation, deamidation, isomerization, hydrolysis, oxidation and denaturation181. The tendency of a biologic to exhibit these structural modifications depends on the properties of the protein as well as environmental factors, including temperature, pH and the ionic strength of the surrounding environment. Several agents have been developed to increase the stability of biologics182. These include the use of small sugars such as trehalose183,184 and polysaccharides such as dextrans185. Pluronics are also used to reduce the tendency to aggregate. Finally, non-ionic surfactants such as polysorbates186 are also used in low concentrations to decrease aggregation. Although many of these agents are effective stabilizers, their use requires careful consideration in terms of local toxicity and potential immunogenicity. Understanding the mechanism of inactivation of biopharmaceutical drugs is crucial and can enable a rational approach to determine what excipients should be used in the formulation to provide stabilization187.
Another issue related to biopharmaceutical drug formulation is high and variable viscosity188. The clinical use of monoclonal antibodies is becoming increasingly common. However, the need for very concentrated formulations is often crucial because the required protein doses are often on the order of hundreds of milligrams. The US Food and Drug Administration (FDA) does not permit the subcutaneous injection of large volumes of drug formulations in patients. This requirement makes formulation difficult as solutions that contain multi-hundred-milligram per millilitre protein solutions are very viscous, making them hard to administer. The creation of formulations with lower viscosities will thus be extremely useful. Approaches to achieve this includes the addition of hydrophobic salts or inorganic salts189,190, or the addition of lysine or arginine191. The high viscosity of protein solutions also affects the force necessary to deliver the solution using acceptable needles as well as the time required to complete the injection — an issue referred to as ‘syringeability’. Both parameters have a strong impact on patient acceptance and compliance.
Collaborations among a wide range of experts, including physical chemists, biochemists and engineers, are required to address the issues posed by formulation challenges. Some of the important unmet needs are predictions of the viscosities of biologics solutions192 and the development of novel means to reduce this viscosity. The development of novel tools to characterize, predict and minimize the aggregation of nascent proteins is crucial. An increased understanding of the dynamics and behaviour of protein injections in the subcutaneous space is also important. Towards this goal, recombinant human hyaluronidase could be co-injected with the drug of interest to degrade hyaluronic acid — a key structural component of tissues193 — and facilitate protein delivery. This degradation increases the diffusion rate of biopharmaceutical drugs at the injection site, thus increasing bioavailability and/or increasing injection volume.
Microparticles
Microparticles are generally used for the long-term delivery (1 week or longer) of proteins, peptides and some small molecules, and are generally administered by intramuscular or subcutaneous injection (TABLE 1). They control both the level of the drug and its lifetime in the body4, and can affect drug pharmacokinetics by enabling sustained release of the drug. Poly(lactic-co-glycolic acid) (PLGA) polymers are the most common material used for the encapsulation of peptides or proteins, as they are mechanically strong, hydrophobic, biocompatible and degrade into toxicologically acceptable products that are eliminated from the body5. Other potentially useful materials include polyanhydrides6 and cyclodextrins7,8. PLGA polymers have been widely used in marketed products — for example, for delivering risperidone (Risperdal; Johnson & Johnson) to treat schizophrenia9 and naltrexone for treating alcoholism and narcotic addiction10. They have also been used to deliver peptides such as LHRH analogues for treating advanced prostate cancer and endometriosis11, glucagon-like peptides (GLPs) for treating type 2 diabetes12 and proteins such as human growth hormone for treating pituitary dwarfism13 (Supplementary information S1 (table)).
Table 1.
Comparison of different delivery technologies for biopharmaceutical drugs*
| Method | Advantages | Limitations |
|---|---|---|
| Microparticles |
|
|
| Depot injections |
|
|
| Nanoparticles |
|
|
| Jet injections |
|
|
| Pumps |
|
|
| Transdermal delivery |
|
|
| Pulmonary delivery |
|
|
| Oral delivery |
|
|
| Other mucosal routes (vaginal, nasal and buccal) |
|
|
The summary presented in this table offers a generalized description of several delivery methodologies. Exceptions to generalized descriptions exist in certain cases and ongoing research is actively addressing the limitations discussed throughout the main text.
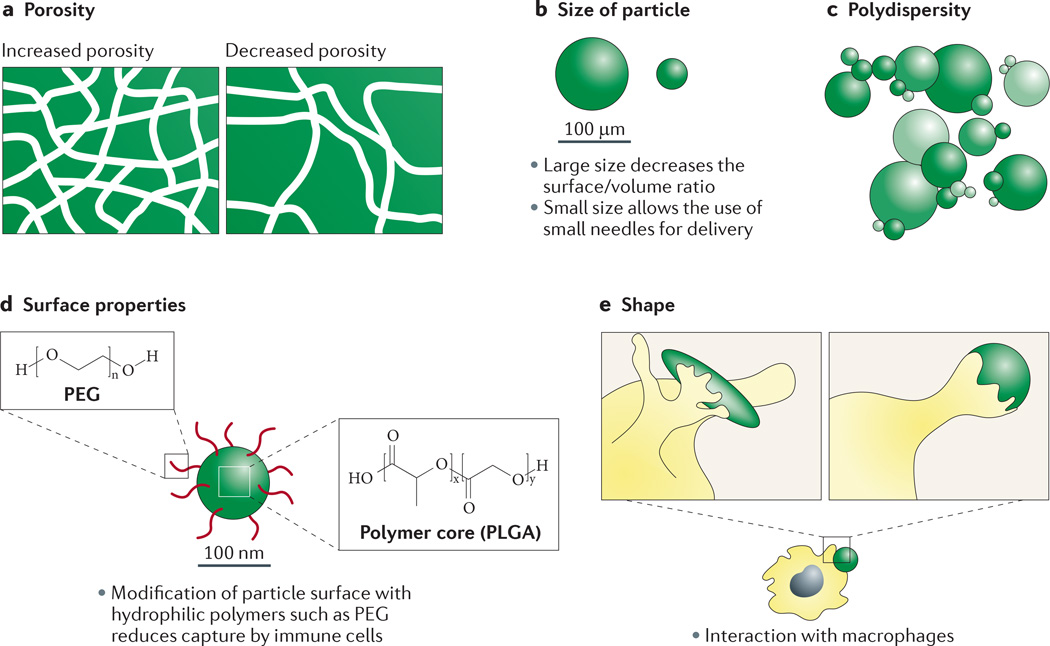
Encapsulation, biocompatibility and protein release from microspheres are closely related to their structural properties. For example, the release rates of proteins depend on the degradation of the polymer and/or diffusion of the protein from the microsphere, which in turn depends on the molecular mass of the polymer and the protein, the lactic/glycolic molar ratio, particle size and the loading of proteins within microspheres, as well as microsphere size and porosity (FIG. 1). The shape of a particle also influences its behaviour, in particular its interactions with macrophages14. Because the diffusional transport of proteins through PLGA is limited, the rate of polymer degradation has an important role in the mechanism and rate of release of the drug from microspheres. In addition, diffusion of the protein through the biological fluid surrounding the microsphere is dependent on the size of the protein, and this will affect the rate of absorption after release15.
Figure 1. Key parameters of polymer microparticle design.
The chemical functionalities of the polymer affect essentially all aspects of microparticle performance, including the efficiency of drug encapsulation, the rate of polymer degradation and drug release, and toxicity at the injection site. a | The porous structure of the polymer alllows penetration of water and facilitates its degradation and subsequent drug release. The porosity of the polymer also affects the diffusion of the drug. b | The size of the microsphere particles affects the duration of drug release (in general, larger particles lead to more prolonged release) and the size of the needle required for administration (smaller needles are required for smaller particles). c | Polydispersity of particle size may introduce variability in the release rates. d | Particle surface properties affect their interactions with the surroundings at the injection site, especially immune cells. Modification of the surface with polymers such as polyethylene glycol (PEG) is used to modulate the interactions of the microsphere with immune cells. e | The shape of the polymer affects the interactions of particles with macrophages; elongated particles exhibit orientation-dependent internalization by macrophages.
The most common method of microencapsulating peptides is through the use of solvent evaporation, but many other approaches such as atomization methods are also used16. The encapsulation of proteins is substantially more challenging, and additional properties of proteins must be considered. Proteins can lose their structure and biological activity upon prolonged incubation with biological fluids under physiological conditions17. For example, aggregation and incomplete release from the microsphere have been observed with growth hormones18 and a covalent dimer formed in a microsphere formulation of darbepoetin alfa (Aranesp; Amgen)19. In addition, the local degradation of polymers at the injection site can lower the pH inside the microsphere, which can further add to the potential for protein inactivation20. The addition of magnesium hydroxide and other antacids within the microsphere has been shown to negate the adverse effects of low pH21.
Although clear advances have been made in the use of microparticles for delivering biopharmaceutical drugs, challenges remain. Specifically, further advances in controlling the burst release can increase the duration of drug release. In addition, methods that provide active control of the rate of drug release, including on-demand termination of release, could open up new opportunities. A reduction in the size of the microsphere (but still within the micron scale) could lead to a subsequent reduction in the required needle size for administration while maintaining the rate of sustained release. Additional unmet needs include the requirement for a robust manufacturing process that can be achieved at a reasonable cost, the need for stabilization and sterilization strategies to be broadly applicable to many biopharma-ceutical drugs, and a need for preclinical tools and/or models for addressing the risk of immunogenicity. In addition, it is important to consider issues such as ease of injection — that is, addressing the reconstitution of the lyophilized product and the clogging of needles with drugs. Many of these issues are not unique to protein- and peptide-based drugs, however, but are in fact common to all microsphere-based drugs.
Nanoparticles
Nanoparticles — which are composed of materials such as polymers, lipids and dendrimers — have been actively studied as carriers, especially for targeted delivery of small-molecule drugs22,23. Indeed, several nanoparticles are currently on the market, including doxorubicin liposomes (Doxil; Janssen) for the treatment of ovarian cancer and AIDS-associated Kaposi’s sarcoma24,25, and paclitaxel-containing albumin nanoparticles (Abraxane; Celgene) for second-line treatment of patients with breast cancer26,27.
There are fewer examples of the use of nanoparticles for delivering proteins and peptides, and these agents are in the early stages of development. There are several examples of nanoparticle-mediated delivery of small-molecule chemotherapeutic agents at clinical and preclinical stages (reviewed in REF. 28). An example of nanoparticle-mediated protein delivery that shows promise for clinical application is the delivery of cytokines for tumour immunotherapy. Specifically, immunosuppressive factors associated with the tumour microenvironment were targeted using a combination of a small-molecule transforming growth factor-β (TGFβ) inhibitor and the immunostimulant interleukin-2 (IL-2)29. Core-shell nanoparticles were developed to encapsulate both the water-soluble protein (IL-2) and the hydrophobic small-molecule cargo (the TGFβ inhibitor) into a single nanoparticle that was designed to enable simultaneous release of both drugs. This method led to sustained local delivery, thereby reducing the toxicity of IL-2, and the combination therapy delayed tumour growth and increased survival in a mouse model of melanoma29.
In another example, which aimed to increase the viability and efficacy of a cell-based therapy, sustained pseudoautocrine stimulation was provided to donor cells in a mouse model of adaptive T cell cancer therapy by conjugating adjuvant nanoparticles to the T cell surface30. The approach mitigates the dose-limiting toxicities that are associated with conventional approaches to adjuvant administration. Multilamellar lipid nanoparticles were directly conjugated to free thiol groups on the surface of various cell types, including CD8+ T cells. Nanoparticle-tethered T cells trafficked to antigen-expressing tumours as effectively as their untethered counterparts. When the particles were bound to melanoma-specific T cells and injected into mice with established lung and bone marrow metastases, complete clearance of the tumour was achieved.
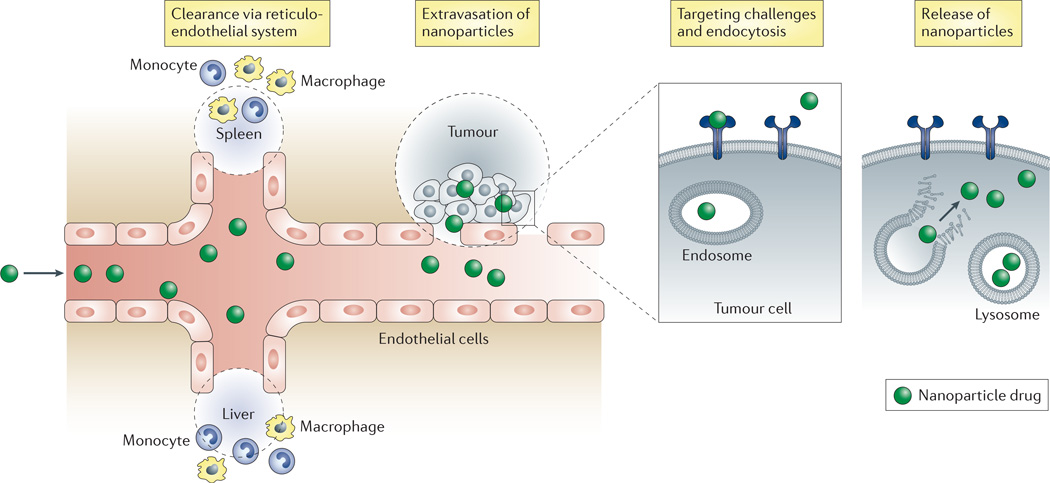
In general, systemically delivered nanoparticles face several physiological barriers before reaching their target (FIG. 2). Technological advances for overcoming these hurdles are important to enable future success in this field; these include pegylation for prolonging the circulation of nanoparticles31 and enhancing tissue penetration32, optimization of particle size33 and the use of substances to enhance deep tumour penetration of nanoparticles34.
Figure 2. Hurdles associated with nanoparticle-mediated delivery.
The figure depicts various hurdles involved in the delivery of therapeutic nanoparticles to targeted tissues. Nanoparticles injected into the bloodstream are cleared by the reticuloendothelial system, including the liver and spleen, especially by the resident macrophages in these organs. Circulating nanoparticles need to cross the vascular endothelium of the diseased tissue and penetrate into the diseased tissue, both of which pose a considerable hurdle. The vascular endothelium possesses low permeability to nanoparticles, except in some cases — such as tumours — where the endothelium is poorly formed and allows the passage of nanoparticles (known as the enhanced permeation-retention effect). Nanoparticles that escape the blood vessel still need to diffuse through the dense extracellular matrix to reach relevant target cells embedded deep within the tissue. Upon arriving at the surface of the target cells, nanoparticles need to enter the cells via endocytosis. Nanoparticles that are internalized by the cells are trafficked within endosomes and sometimes need to escape the endosome to release the active drug cargo.
Although a limited number of studies can be found on the use of nanoparticles for the delivery of therapeutic proteins, nanoparticles have been actively used for delivering vaccines or as vaccine adjuvants35. The primary advantage of nanoparticulate vaccines is effective antigen presentation to dendritic cells, which yields a stronger immune response than soluble antigens36.
Depot injections
Injectable implants of drugs are an alternative to particulate formulations for sustained drug release, and have been used for both small and large molecules. Surgically implantable depots — that is, formulations that are too large to be injected by needles — have also been developed for small molecules (reviewed in REF. 37), such as the chemotherapeutic drug bis-chloro-ethylnitrosourea (BCNU). Among biopharmaceutical drugs, an injectable formulation of the LHRH agonist goserelin acetate contained in a PLGA rod (Zoladex; AstraZeneca) is the most commercially successful example (Supplementary information S1 (table)). Other polymers such as hyaluronic acid are also being explored for their use in depot injections38.
Injectable monoliths can circumvent some of the manufacturing complexities and challenges associated with particulate systems, such as the suspension and reconstitution of particulate drug formulations. In addition, the lower specific surface area of monoliths can often result in a reduced burst release of drugs. The use of additional ingredients such as PEG 400 in the formulation has been shown to reduce the initial burst39. Blends of block copolymers and PLGA are also effective in offering prolonged release of protein drug. Injectable in situ-forming depot systems, including those based on injectable solutions of PLGA in sucrose acetate isobutyrate40,41 or N-methyl pyrollidone42,43, offer similar potential benefits44.
Reverse thermal gelling systems45 are based on polymers that form solutions at room temperature but become gels at body temperature following injection. The in situ-forming system PB1023, which is based on a fusion of the drug cargo GLP1 with elastin-like polypeptide (ELP), recently completed a Phase II clinical trial for the treatment of diabetes46 (ClinicalTrials.gov identifier: NCT01658501). ELPs undergo a phase transition at body temperature to form a depot that leads to sustained release. A single injection of the GLP1–ELP fusion protein reduced glucose levels for 5 days, which is 120 times longer than with GLP1 alone.
Another example of a protein depot injection consists of a conjugate of poly-l-glutamic acid and α-tocopherol, which forms non-covalent complexes with proteins and peptides through electrostatic and hydrophobic interactions. This results in the formation of an in vivo drug depot after injection, with sustained drug release over 1–14 days47. Proof of concept of this proprietary system was shown for a formulation of IL-2 in patients with renal cell carcinoma48, and a formulation of interferon-alpha-2b is currently in clinical trials for the treatment of hepatitis C virus (HCV) infection (Supplementary information S1 (table); ClinicalTrials.gov identifier: NCT01010646). Another example of an injectable depot technology consists of a solution of naturally occurring polar lipids that self-assemble into reversed liquid crystal phases when injected into the body (known as FluidCrystal® injection depots)49. This system has been used for sustained delivery of proteins and peptides, such as leuprolide acetate (CAM2032) and octreotide (CAM2029; orphan designation EU/3/09/645), which are under clinical evaluation for prostate cancer and acromegaly, respectively (Supplementary information S1 (table); see the Camurus website for further information).
The emergence of biosimilars and the availability of analytical technologies with increased sensitivity for the detection of degradation products have resulted in increasingly high standards for the analytical purity of conventional protein formulations, and recognition from the scientific community that these higher standards also need to be applied to sustained-release protein formulations50.
Although the stresses imposed on protein drugs through the fabrication, storage and administration of sustained-release formulations have been long appreciated, a better understanding of the molecular basis of protein degradation and aggregation pathways could potentially lead to new stabilization approaches or the design of new delivery systems that are more suited to labile macromolecules. Recent examples include a dendritic polyglycerol nanogel system that was used to encapsulate asparaginase under surfactant-free conditions using hydrophilic components51. A pH-sensitive benzacetal crosslinking agent enabled the triggered release of payload under acidic conditions with almost 100% recovery of enzymatic activity compared to a control. Asparaginase that was recovered at the end of matrix degradation after 7 days had the same activity as a control, and its secondary structure was unchanged.
In another example, an alginate depot formulation of a fully humanized immunoglobulin G1 (IgG1) monoclonal antibody was developed to exploit the electrostatic interactions that occur between the protein and the polyanionic gel matrix to enable local sustained delivery52,53. The system was designed to provide a stable pH environment and to avoid protein aggregation at a high payload concentration. In vitro analysis showed 90–100% recovery of intact IgG1, with monomer content >94%. Preliminary evaluation of IgG1 release over 28 days in rats showed that bioavailability was comparable to that observed with a conventional solution formulation.
Most depot formulation technologies, as well as the particle technologies discussed above, rely on non-covalent association between the drug and the matrix. Thus, their implementation does not require the creation of a new molecular entity. This could potentially simplify their development owing to the applicability of analytical methods that were developed for conventional formulations of the same drug, as well as preclinical pharmacology and safety data generated with those formulations.
Injectable modified peptides and proteins
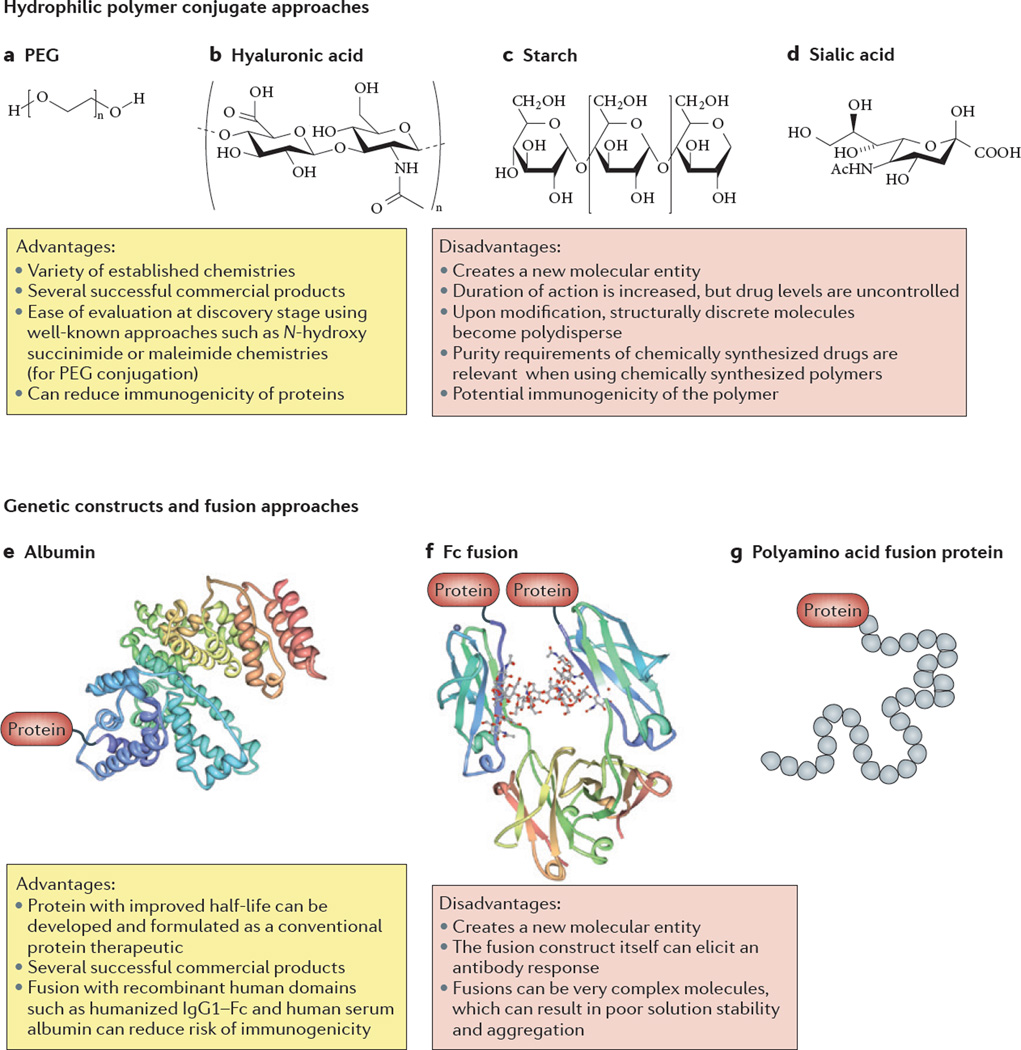
Most macromolecules that are smaller than ~ 60 kDa are cleared from the body via renal filtration54. Attempts have been made to reduce renal clearance by increasing the size of macromolecules or by making modifications to the macromolecule based on known biological phenomena in order to reduce renal clearance and, consequently, injection frequency (FIG. 3).
Figure 3. Modes of biopharmaceutical modification.
Two general types of protein modification are used to extend half-life; conjugation with hydrophilic polymers (parts a–d) and genetic constructs or fusion approaches (parts e–g). Conjugation approaches include protein modification with polymers such as polyethylene glycol (PEG) and hyaluronic acid. The advantages of the conjugation approach include: the availability of a variety of established chemistries; ease of evaluation at a discovery stage using well-known approaches such as N-hydroxy succinimide or maleimide chemistries; reduction of protein immunogenicity; and a proven history with multiple products. Their limitations include the creation of a new molecular entity, polydispersity and potential immunogenicity of polymers. Fusions offer the advantage of being developed and formulated as conventional protein therapeutics, avoiding additional downstream processing such as encapsulation and associated costs. In addition, there is a proven history of several products based on this approach. Their limitations include the creation of a new molecular entity and the associated safety issues and testing, the possibility of generating an immune response to the modified protein and potential formulation challenges owing to the increased molecular complexity.
Types of protein modifications
Chemical modification with hydrophilic polymers can increase the hydrodynamic radius such that glomerular filtration is reduced or eliminated, thus extending the circulating half-life to a commercially attractive range55. There are many examples of pegylated drugs on the market, and alternatives to polyethylene glycol (PEG) — such as sialic acid56, as well as the naturally occurring polysaccharides hyaluronic acid57 and hydroxyl ethyl starch54 — are currently under preclinical and clinical investigation (Supplementary information S1 (table)).
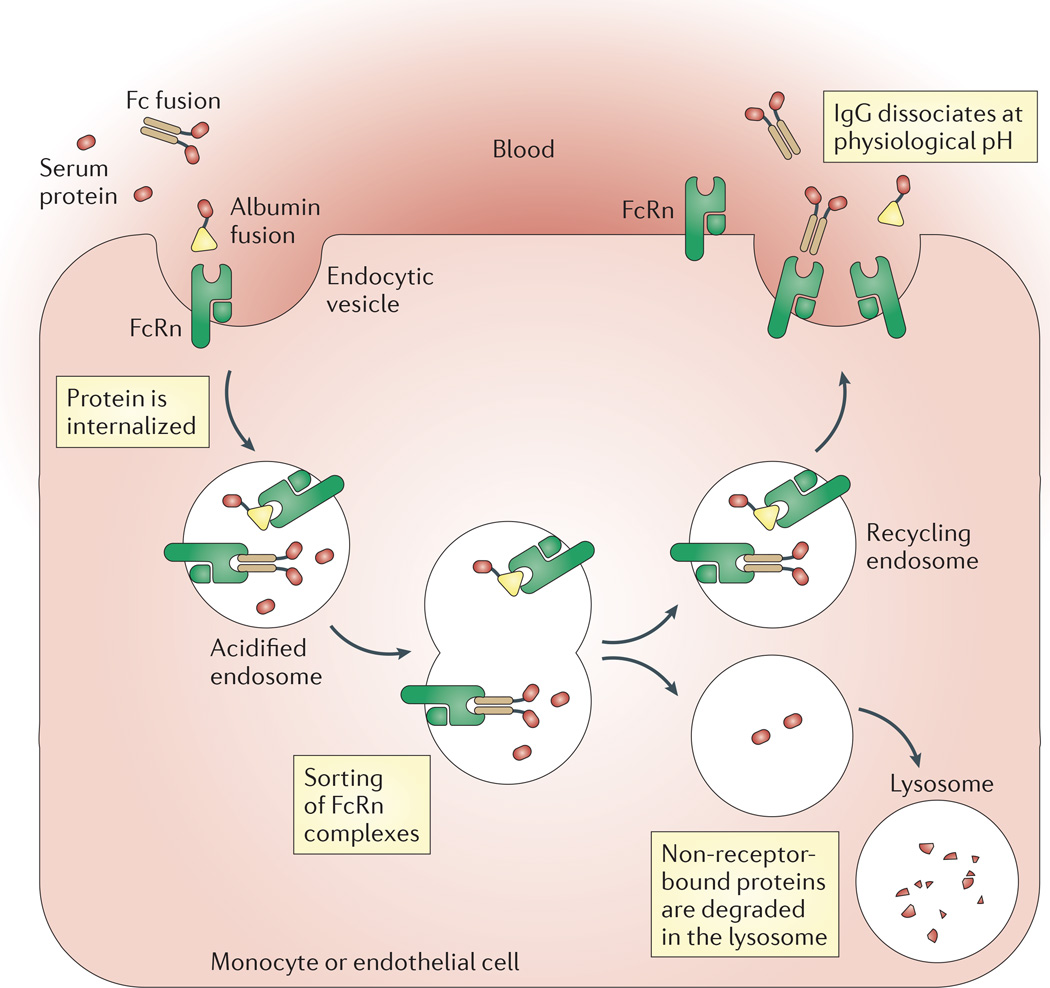
Approaches that exploit the neonatal Fc receptor recycling (FcRn recycling) pathway have also been developed to increase the half-life of macromolecules (FIG. 4). This approach, which involves the creation of genetic fusions between the macromolecule and the Fc region of IgG, has resulted in many approved products, including the blockbuster etanercept (Enbrel; Amgen) and several candidates that are currently in advanced stages of clinical development (Supplementary information S1 (table)).
Figure 4. FcRn recycling mechanism.
Neonatal Fc receptor (FcRn) recycling has a crucial role in the biological activity of Fc- and albumin-fusion proteins. Fc-fusion protein drugs or albumin-fusion protein drugs bind to FcRn on the endothelium. Receptor-bound proteins are internalized into endocytic vesicles. End osomes are acidified and undergo sorting of FcRn. Non-receptor-bound proteins are degraded in the lysosomal compartment and receptor-bound proteins are recycled back to the cell membrane. The protein therapeutic is subsequently released back into the blood. FcRn-mediated recycling leads to prolonged circulation of Fc-fusion and albumin-fusion protein therapeutics. IgG, immunoglobulin G.
Efforts have also been made to extend circulation times by exploiting the favourable circulating half-life of albumin58, thus enabling weekly dosing. For example, an albumin fusion of GLP1(7–36) (albiglutide; ClinicalTrials.gov identifier: NCT01098539)59 was approved by the US Food and Drug Administration (FDA) in April 2014 for the improvement of glycaemic control in adults with type 2 diabetes, and an albumin fusion of factor IX60 is in Phase III clinical evaluation for the prevention of bleeding episodes in children and adults with severe haemophilia B (ClinicalTrials.gov identifier: NCT02053792). In addition, an albumin fusion of granulocyte colony-stimulating factor (G-CSF), neugranin, is under development for the treatment of chemotherapy-induced neutropenia (ClinicalTrials.gov identifier: NCT00837265). A fusion of albumin with two different single-chain variable fragments (scFv fragments), which bind to HER2 and HER3, has been created to form a single-polypeptide-chain bispecific antibody61 that is in Phase II clinical trials for the treatment of certain types of oesophageal cancer (MM-111; ClinicalTrials.gov identifier: NCT01774851). A related approach, which uses chemical conjugation of albumin with a synthetic peptide, has been applied to exendin-4; the conjugate (known as CJC-1134-PC) is under clinical evaluation for the treatment of type 2 diabetes (Supplementary information S1 (table); ClinicalTrials.gov identifier: NCT01514149).
Advantages and disadvantages of protein modification
Although pegylation can decrease protein immunogenicity and increase solubility, the principal benefit of this modification is the ability to reduce the frequency of dosing owing to the longer circulating half-life of the drug. The approach provides sustained — but not controlled — exposure; clearance from the body is still exponential, and so a longer duration of exposure can only be attained by increasing the dose. For compounds with large therapeutic indices (which is typical for many biopharmaceutical drugs), the cost of goods and/or dosing volumes needed for a longer duration of action can become limiting. Alternative approaches may be required for molecules with toxicities that are related to peak exposure. Moreover, pegylation can negatively influence the binding of a molecule to its cognate receptor owing to steric hindrance; however, optimal design of molecules can minimize this effect, and pharmacokinetic benefits can render it inconsequential.
Reactions of the immune system to non-native conjugates or fusion structures pose a potential safety issue. In the case of fusions with native human proteins, cross-reactivity with endogenous homologues could pose a long-term safety threat in addition to potentially altering the clearance of subsequent doses. However, for many Fc-or albumin-fusion products this risk has not proven to be detrimental (Supplementary information S1 (table)). Fusions of recombinant factor VIII62 and factor IX63, which are currently in advanced development for the treatment of haemophilia (ClinicalTrials.gov identifiers: NCT02093897 and NCT02053792, respectively; Supplementary information S1 (table)), are intended for chronic lifelong use, and as such their approval could be an important new milestone in establishing the safety of fusion approaches. The immunogenicity of fusion proteins, however, is an ongoing concern. Many of the approved Fc-fusion drugs (Supplementary information S1 (table)), such as etanercept, which is approved for the treatment of rheumatoid arthritis and psoriasis, are themselves immunosuppressive therapies, whereas others, such as aflibercept (Zaltrap; Regeneron), which is approved for the treatment of metastatic colorectal cancer, have been used for indications where patients’ immune systems are not functioning normally. As a result, effects related to immunogenicity are possibly obscured. The bar for the safety for clotting factors is likely to be higher. Importantly, the Phase III study for a factor IX–Fc fusion protein reported no evidence of immunogenicity63, and the FDA approved this product in March 2014.
New developments in protein modification
Early approaches to conjugation (reviewed in REF. 55) illustrated the potential to affect properties such as potency and pharmacokinetics55. More recent advances in long-circulating biopharmaceutical polymer conjugates have increased the precision with which conjugates are defined at a molecular level, either through polymer chemistry or through site-specific conjugation. At its most advanced stage, conjugate research applies the tools of medicinal chemistry by incorporating insights from structure–function studies into the design of the molecule. A study64 of the site-specific pegylated WW domain of the human protein peptidyl-prolyl cis-trans isomerase NIMA-interacting 1 (PIN1)65 showed that conformational stability depends on the molecular mass of PEG; longer oligomers increased the folding rate and reduced the rate of protein unfolding.
Pegylated proteins are generally considered to have reduced immunogenicity compared to their unmodified equivalents, and one of the earliest pegylated products, pegademase bovine, exploited the ability of PEG to mitigate the immunogenicity of a bovine enzyme for use as a biopharmaceutical. Nevertheless, the formation of antibodies against PEG itself has recently gained attention; PEG end-group chemistry (that is, the substituent at the end of the PEG molecule) is reported to have a substantial role in determining immunogenicity. The use of hydroxyl-PEG, as opposed to the widely used methoxy-PEG, may offer a safety advantage under some circumstances66,67. These types of insights could lead to the future development of biopharmaceutical conjugates with superior properties. Reversible pegylation has been explored as a way of mitigating the reduction in potency induced by conjugation and achieving greater control of drug concentration over time68. The creation of PEG prodrugs that are minimally or partially active could potentially make it possible to administer higher doses — and thus achieve a longer duration of action — of compounds that have toxicities related to Cmax in their fully active form.
Alternatives to PEG that could offer improvements in chemical definition, biocompatibility or manufacturability have been explored. Among the most advanced are polymers that are based on poly(2-oxazoline). These are synthesized by a technique known as living polymerization, which allows for good control of the molecular definition; hydrophobicity can be tuned according to the composition of the side chains. Amphiphilic block copolymers of poly(2-oxazoline) have been shown to increase the uptake of conjugated macromolecules into cells69.
Alternative approaches to protein modification based on genetic engineering
Lessons learned from the success of pegylation and Fc-fusion-based products have helped guide the application of genetic engineering tools to improve the delivery of biopharmaceuticals. The most commercially successful example, darbepoetin alfa, is a variant of erythropoietin that is genetically engineered to include two additional sialic acid chains70. Introducing non-structured polyamino acid tails on the amino and/or carboxy termini of several therapeutic proteins achieved a PEG-like effect on the hydrodynamic radius and on renal clearance by glomerular filtration71. The approach has been used in several development programmes (Supplementary information S1 (table)), including in clinical studies of VRS-859, a GLP1 analogue72, and of VRS-371 (ClinicalTrials.gov identifier: NCT01359488), a long-acting human growth hormone. Native human growth hormone is cleared by glomerular filtration as well as receptor-mediated clearance in the kidney. VRS-371 was designed to have reduced receptor binding, and so it undergoes less receptor-mediated clearance in the kidney73. Based on a Phase I clinical trial in adults with growth hormone deficiency, it is anticipated that VRS-371 can be dosed monthly74, which will be a milestone for a technology that does not involve FcRn recycling. However, the immunogenicity of VRS-371 has yet to be fully assessed.
Site-directed mutagenesis has been used to try to control the half-lives of Fc- and albumin-fusion products by optimizing the binding affinity of the molecule to FcRn. Half-lives for ten marketed antibodies and Fc-fusion proteins were reported to range from 4 to 23 days, depending on the Kd value for FcRn binding75,76. Mutants of an anti-human B cell surface receptor antibody with improved FcRn binding affinity had an impact on pharmacokinetics in primates (although the relationship between FcRn affinity and the level of improvement in pharmacokinetic properties was not directly proportional)77. The relationship between FcRn binding affinity and half-life has informed recent efforts to map the albumin FcRn binding domain78, with a view towards the design of albumin fusions that have a wider range of half-lives than can be achieved with native human albumin domains79.
Devices
In spite of their widespread use in biopharmaceutical drug delivery, injectable biopharmaceutical drugs have several limitations, including the creation of needle phobia in patients, accidental injuries and improper use80. Needle-based autoinjectors are in clinical use; although they are simple to use and avoid visual appearance of the needle, the insertion of a needle is still associated with pain. Accordingly, although needles have undergone substantial improvements over the years, the development of better alternatives to needle-based injections has been a high priority for research and development.
Implantable, patch and microfluidic pumps
Implantable pumps are commercially available to deliver biopharmaceutical drugs, especially insulin81,82. Compared to multiple daily injections, the use of implantable insulin pumps improves glycaemic control83. Insulin patch pumps address the limitations of implantable pumps as they are lightweight and can be worn discreetly on the skin84. Newer, microtechnology-based implantable pumps have also been developed to achieve more precise control over delivery and have been used to deliver human parathyroid hormone fragments in clinical studies85,86. Although currently available pumps have enabled the delivery of insulin, challenges remain. Specifically, the implantation of pumps is invasive and they require frequent refilling with the drug. Moreover, patch pumps have limited longevity owing to the limited duration of the sterility of the skin. The ultimate goal of an insulin pump is to develop a closed-loop device that offers automated control of blood glucose levels. Robust algorithms that utilize the output of an implanted glucose sensor to determine requisite doses have been developed87 and are in clinical trials (ClinicalTrials.gov identifiers: NCT01271023, NCT01472406).
Needle-free injectors
Liquid jet injections offer several advantages, including the ability to use currently approved injectable formulations — which will greatly facilitate clinical adoption — as well as the ability to work without electronics and the provision of small portable devices. Liquid jet injectors have been used for mass immunization programmes against infectious diseases, as well as for the delivery of insulin and growth hormones88,89. However, the acceptance of liquid jet injectors has been low owing to occasional pain and bleeding at the site of injection90. Therefore, efforts are underway to improve the jet injection process, such as the use of pulsed microjets91, variable velocity injectors92 and feedback-controlled injectors93. Although needle-free liquid injectors are the only currently available, broadly applicable, needle-free approach for protein delivery, they have not had a strong impact on the field. Future research must focus on addressing the variability in the amount of drug that is delivered via injection, which originates in part from the variation in skin properties among patients, as well as within different regions of the body. In addition, the devices must be designed so they are inexpensive and sufficiently simple to use.
Alternative routes of drug delivery
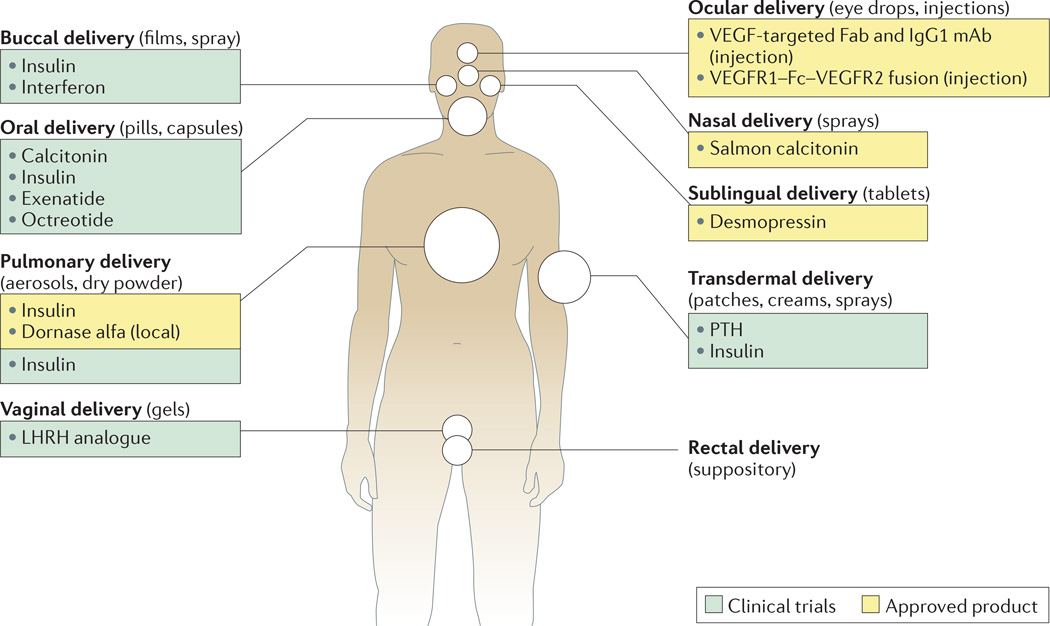
Owing to the limitations of injections, alternative delivery routes — including pulmonary94, nasal95, oral96, transdermal97,98, vaginal and ocular delivery of biopharmaceutical drugs — have been explored to increase patient compliance (FIG. 5). Each route offers its own unique advantages and limitations (TABLE 1). However, the delivery of bio-pharmaceutical drugs through these alternative routes is limited by the associated biological barriers, the biophysical properties of which are reviewed in REFS 99, 100. Nevertheless, device- or formulation-based approaches have been developed to overcome these barriers.
Figure 5. Alternative routes of biopharmaceutical delivery.
Various alternative routes to needle-based injections have been proposed for the delivery of biopharmaceutical drugs. These include oral, transdermal, pulmonary, nasal, vaginal, sublingual, rectal and ocular delivery routes. The figure summarizes some of the approved products that are administered via these routes and those that are in clinical trials. Examples listed in the figure indicate the high level of activity in alternative routes of drug administration. IgG1, immunoglobulin G1; LHRH, luteinizing hormone-releasing hormone; mAb, monoclonal antibody; PTH, parathyroid hormone; VEGF, vascular endothelial growth factor; VEGFR, VEGF receptor.
Pulmonary delivery
To date, most research on the delivery of aerosol formulations has focused on the delivery of small molecules to the lung itself, and has addressed issues such as aggregation of drug particles and decreasing the clearance of drugs by macrophages94. Nevertheless, the delivery of protein drugs though the pulmonary route has been achieved. Inhaled insulin101 received FDA approval in 2006; however, it was discontinued in 2007 owing in part to high costs as well as poor patient uptake of the bulky device. Recent studies have shown that a more compact device can effectively deliver insulin by inhalation in patients with type 2 diabetes102, and the product has recently received regulatory approval (see the 27 Jun 2014 press release on the MannKind Corporation website). Although advances have been made in the field of pulmonary delivery, unmet needs remain; these include potential safety issues, the limited delivery efficiency associated with inhaled proteins and the ease of use of the product, as well as potentially the relatively short duration of action, as the same physiological factors that enable the drug to have a quick onset of action also make sustained delivery challenging.
Transdermal administration
Transdermal patches offer a painless alternative to injections; however, their applications are generally limited to low-molecular-mass hydrophobic drugs. An in-depth review of transdermal drug delivery can be found in REF. 103. Several methods have been developed to temporarily disrupt the skin structure to deliver macromolecular drugs, including the use of peptides such as TD-1 (REF. 104), SPACE (skin-permeating and cell-entering) peptides105 and cell-penetrating peptides such as polyarginine106. TD-1 and SPACE peptides were discovered specifically to penetrate skin using in vivo phage display and effectively delivered large molecules such as insulin104 and hyaluronic acid107 into mice. Several chemical-based formulation strategies108 have also been developed to enhance transdermal drug delivery; however, their clinical applications are generally limited to small molecules.
Devices that are based on the use of ultrasound, electric fields or microneedles have been particularly effective in increasing the permeability of the skin109. Ultrasound and electric-field-based methods such as iontophoresis and electroporation have been used to deliver biopharmaceutical drugs — including insulin110,111 and parathyroid hormone112 — in animal models. Neither method is currently used in the clinic for large molecules, but ultrasound and iontophoresis have been approved by the FDA for the delivery of small molecules in a clinical setting113. Microneedles can penetrate into skin as far as the epidermis and thereby enhance drug penetration without causing pain. Microneedles have successfully delivered insulin, vaccines and parathyroid hormone in clinical studies98, and are proving to be particularly appealing for the delivery of vaccines as they have been shown to induce immune responses that are comparable to or better than intramuscular injections in mouse models114,115. Microneedles are also being developed for the systemic delivery of parathyroid hormone and are in clinical studies of parathyroid hormone-related protein (ClinicalTrials.gov identifier: NCT01674621) and insulin (ClinicalTrials.gov identifier: NCT01684956), as well as vaccines of inactivated polio virus (ClinicalTrials.gov identifier: NCT01686503) and influenza (ClinicalTrials.gov identifier: NCT01368796).
Collectively, the technologies described above have enabled progress in the transdermal delivery of proteins over the past two decades. There are several future challenges in this field; the complexity of the devices, including the size and required expertise, can make their adoption challenging, and so the device-based methods must be simple to use. At the same time, the bioavailability of the drug must be sufficiently high to make the technology economically feasible. Finally, the variability of drug delivery must be sufficiently reduced to allow the administration of drugs that have a narrow therapeutic window.
Oral delivery
Oral delivery offers increased patient acceptance, but the oral delivery of macromolecules is limited by enzymatic degradation in the gastrointestinal tract and limited permeation across the intestinal epithelium116. In addition, the mucus layer on the epithelium provides a barrier for the diffusion of macromolecules. These limitations lead to poor drug absorption into systemic circulation and insignificant bioavailability of macromolecules.
Several absorption enhancers, including fatty acids, surfactants and bile salts, have been tested for their ability to improve the oral delivery of macromolecules117 in animal models. Sodium caprate enhances the delivery of macromolecules such as oligonucleotides and low-molecular-weight heparin118 in animal models and humans. Another absorption enhancer is tetradecylmaltoside, which also enhances the uptake of low-molecular-weight heparin119. The screening of a large library of chemicals and chemical mixtures to identify compositions that enhance the uptake of peptides and proteins120 led to the identification of the zwitterionic surfactant dimethyl palmitoyl ammonio propanesulphonate (PPS), which enhanced the intestinal permeation of calcitonin in mice121. Other methods of increasing absorption include pH-sensitive hydrogels to protect the drug from low pH in the stomach122, chitosans123 and chitosan derivatives124 to induce mucoadhesion of the drug carrier and increase intestinal permeation, and acrylate-based polymers to increase mucoadhesion125.
Device-based approaches are also being actively pursued for oral drug delivery. Mucoadhesive devices that mimic the structure of skin patches have been tested for the oral delivery of insulin and calcitonin in rodent models96,126. These devices continue to be researched and developed127, but have yet to be tested in humans. The current design of these mucoadhesive devices is based on layered structures that comprise a mucoadhesive layer that attaches and retains the device on the mucus, a drug layer, and a backing layer that prevents diffusion of the drug back into the lumen and entry of gastrointestinal enzymes into the patch. This design creates a depot of high-concentration drug on the surface of the intestine, which enhances the concentration gradient across the intestine and increases oral drug bioavailability.
The use of nanoparticles, which are absorbed across the intestinal epithelium, has also been explored for the oral delivery of biopharmaceuticals. The uptake, which can be mediated by Peyer’s patches, M cells and enterocytes, depends on several parameters, including the size and surface chemistry of nanoparticles. Although unmodified particles are known to permeate the epithelium, targeted nanoparticles further enhance uptake. In this regard, several targeting ligands — including lectin, the M cell-targeted monoclonal antibody and the Fc region of antibodies128 — have been explored for the oral uptake of nanoparticles in mice. Further testing of such novel technologies in larger animal models is necessary to understand their clinical potential.
The ability of penetration enhancers, nanoparticles and mucoadhesive devices to deliver insulin, calcitonin and other biopharmaceutical drugs has been established in small animals118,129,130. Oral delivery of proteins and peptides, however, has had limited clinical success. Clinical studies have shown oral delivery of salmon calcitonin using the permeation enhancer 5-CNAC131 but the clinical programme was terminated owing to lack of efficacy in Phase III clinical trials (see the 14 Dec 2011 press release on the Emisphere website). Permeation enhancers from the same family have also been shown to enhance the oral uptake of heparin in humans132. Another enhancer, sodium caprate, has been shown to increase the delivery of oligonucleotides in humans133 and of low-molecular-weight heparin in rats118. Advances have also been made using other medium-chain fatty acids as enhancers to enable the oral delivery of peptides, especially octreotide134.
Another technology that is based on the use of protease inhibitors and an absorption enhancer has been tested in humans for the delivery of insulin135. Orally delivered insulin reduced the frequency of high glucose readings (>200 mg per dl) when compared to control. The same technology has also been tested in humans for delivery of the GLP1 analogue exenatide136. Orally delivered exenatide increased peak plasma insulin levels by 28% in healthy individuals. A technology based on the use of citric acid (which has proteolysis-inhibiting properties)137 has also been tested for the oral delivery of salmon calcitonin for the treatment of postmenopausal osteoporosis in women; oral calcitonin improved lumbar spine bone mineral density by about threefold compared to placebo138.
In spite of substantial research over the past two decades, the goal of oral protein delivery remains difficult. Limited bioavailability and variability in absorption remain general challenges in the field. The appeal of oral protein delivery, however, has not diminished. Future research must focus on enhancing bioavailability to economically feasible levels, which will be different for each drug. In addition, issues related to the variability in absorption and interference from food must be addressed. Other delivery routes that are not discussed in this Review include the buccal, nasal, vaginal and ocular routes139–144.
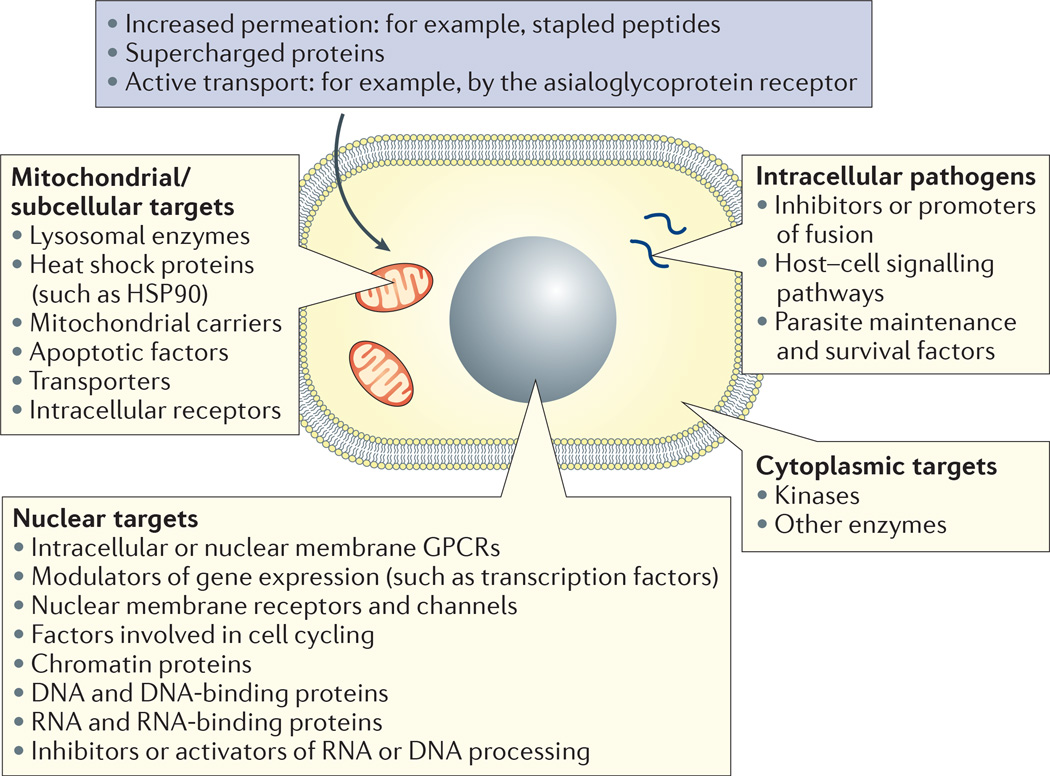
Targeted and intracellular delivery
Although the focus of biopharmaceutical delivery has largely been on systemic delivery, targeted and intracellular delivery are important goals (FIG. 6). The local delivery of conventional formulations is the simplest option for targeting specific tissues — for example, the intravitreally administered vascular endothelial growth factor (VEGF) inhibitors bevacizumab (Avastin; Roche/Genentech), ranibizumab (Lucentis; Genentech/Novartis) and aflibercept (Eylea; Regeneron) for the treatment of neovascular age-related macular degeneration. Controlled-release depot formulations provide more consistent local exposure, which is important for the delivery of growth factors for tissue engineering (BOX 2).
Figure 6. A summary of intracellular targets for biopharmaceutical drugs.
The cell interior is the site of numerous potential drug targets where biopharmaceuticals may be attractive candidates provided they can be delivered successfully. Approaches to the intracellular delivery of biopharmaceuticals include increasing their membrane permeability (particularly in the case of peptides) and active transport via internalizing receptors on the cell surface, such as the asialoglycoprotein receptor on hepatocytes. Potential intracellular targets include those associated with mitochondria, the nucleus and the cytoplasm. Intracellular pathogens are another potential application. These include the liver stages of Plasmodium spp. mycobacteria in alveolar macrophages and associated granuloma, and amastigotes of Leishmania spp. in infected macrophages and various tissues including the liver and bone marrow. GPCR, G protein-coupled receptor; HSP90, heat shock protein 90.
Box 2 | Biopharmaceutical drug delivery and its relationship with tissue engineering.
Engineered tissues and artificial organs have an important role in maintaining and improving the quality of life of patients suffering from illnesses and injuries; for example, skin substitutes and cartilage replacements have already helped thousands of patients, and several other tissues such as the liver194, cornea195 and spinal cord196 are being studied in animals or in clinical trials. Engineered tissues may have a role in the assessment of drug toxicity in the form of organs on a chip197. There are several forms of engineered tissues, including cell aggregates, three-dimensional polymer cell constructs, decellularized tissue constraints and entire functioning organs198.
The delivery of proteins has a major role in tissue engineering by providing controlled and localized release of cytokines, growth factors and nucleic acids to improve cell survival or otherwise contribute to tissue growth199,200. The spatiotemporal control of the release of growth factors and cytokines can be crucial for tissue growth201. These factors also stimulate delivered cells to proliferate or perform specific functions, such as recruiting immune cells to the site of implantation of the engineered tissue. In addition, the delivery of growth factors that promote vascular neogenesis is essential for tissue growth202. Various approaches have been developed to encapsulate and release proteins, peptides and nucleic acids from matrices that are used for tissue engineering. These delivery approaches include matrix embedding203, encapsulation of drug-loaded microparticles and the immobilization and covalent attachment of drugs to the scaffolds204.
The active targeting of biopharmaceuticals to specific tissues following systemic administration using ligands of, or antibodies against, cell surface receptors is an attractive concept. Recent advances with antibody–drug conjugates145 and a small-molecule nanoparticle formulation of docetaxel22 enabled preferential delivery of cytotoxic agents to cancerous tissue; this could potentially increase the therapeutic index and enhance the efficacy of such cytotoxic drugs. The extension of this approach to the delivery of macromolecular cargo is, however, in the early stages of development.
Interest in the intracellular delivery of biopharmaceutical drugs in part originates from recent advances in RNA interference (RNAi), where small interfering RNA (siRNA) must overcome the cellular barrier to access the RNAi machinery; these advances have focused attention on the potential opportunity for developing protein and peptide drugs against intracellular targets. Several technologies have been developed to deliver siRNA to the skin105,146, liver147, brain148 and tumours149, as well as other tissues. siRNA delivery technologies are not discussed here; see REF. 150 for an overview of the field.
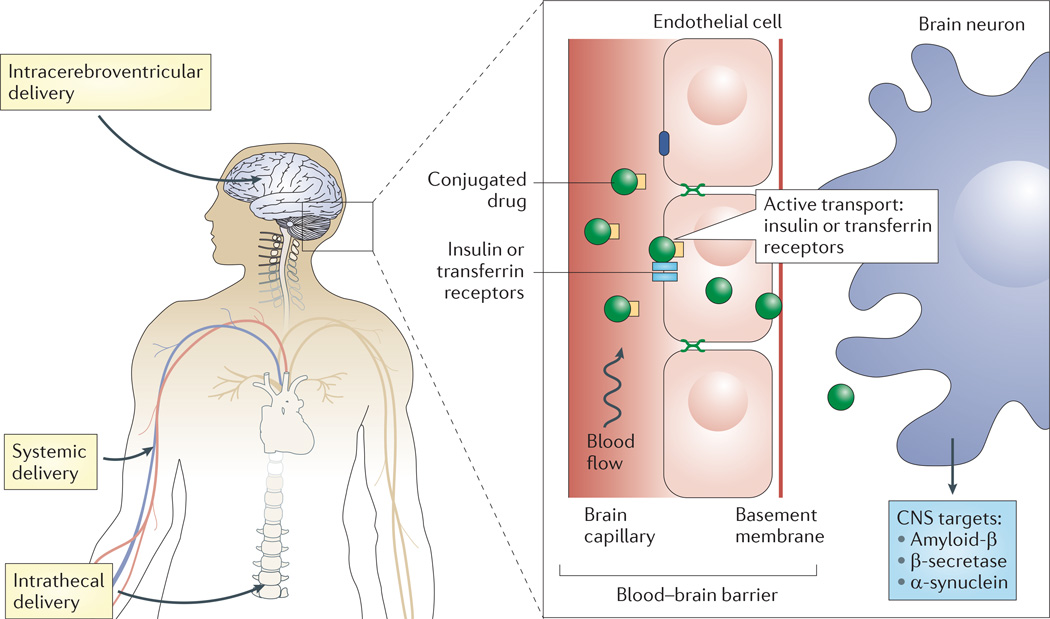
Targeted delivery to the brain
The blood–brain barrier poses a unique challenge for the targeted delivery of biopharmaceuticals to the brain (FIG. 7). Nevertheless, there has been growing interest in this area, which has been fuelled in part by the therapeutic promise seen in the peripheral administration of antibodies for the treatment of neurodegenerative disease. Antibodies are attractive owing to their high specificity and reduced off-target effects, and peripherally administered monoclonal antibodies result in measurable, albeit low, central nervous system (CNS) exposure151 that probably results from a nonspecific mechanism of uptake across the blood– brain barrier. For example, systemically circulating IgG levels in the CNS are 0.1% of their levels in plasma152. Neurodegenerative disease is an area of particular focus, in part owing to the difficulty of developing CNS-penetrant, specific, small-molecule therapeutics. An antibody inhibitor of β-secretase, the enzyme that processes amyloid precursor protein (APP), reduced peripheral and CNS amyloid-β concentrations in mice and in non-human primates153 following systemic administration. An antibody against α-synuclein, which accumulates abnormally in certain forms of dementia, alleviated behavioural deficits in an α-synuclein transgenic mouse model when dosed systemically154; trafficking and histology studies showed that the antibody crossed into the CNS and resulted in reduced levels of α-synuclein aggregates in the cortex and hippocampus.
Figure 7. Various means to access the central nervous system for therapeutic delivery.
Delivery of biopharmaceutical drugs into the central nervous system (CNS) is highly challenging. Intracerebroventricular injections offer a direct mode of drug delivery into the brain; however, this approach is limited by its invasive nature. Systemic delivery in the vascular compartment is another option. Although this approach is easy, its use is limited by the low permeability of the blood-brain barrier. Specifically, endothelial cells in the brain possess highly regulated tight junctions that limit passive diffusion of drugs. Biopharmaceutical drugs must exhibit active uptake in order to cross the endothelium. Intrathecal administration provides an optimal blend of ease of use and access to the cerebrospinal compartment, although diffusion within the brain can be a limiting factor.
Antibodies targeted to tau reduced tau pathology and delayed the onset of motor function decline in transgenic mouse models when delivered peripherally155 and reduced cognitive impairment when delivered by intracerebroventricular infusion156. Several antibodies against amyloid-β have been evaluated in the clinic for the treatment of Alzheimer’s disease, most notably bapineuzumab (ClinicalTrials.gov identifier: NCT01254773) and solane-zumab (ClinicalTrials.gov identifier: NCT01900665). Although both recently failed to meet their primary end points in several Phase III trials — calling into question the amyloid-targeted approach to treating Alzheimer’s disease157 — passive immunotherapy for the treatment of neurodegenerative disease remains an active area of investigation. A humanized IgG4 antibody binding to semaphorin 4D (SEMA4D) attenuated disease severity in rodent models of multiple sclerosis (when dosed intravenously), including chronic experimental autoimmune encephalomyelitis (EAE)158. The antibody is being evaluated in a Phase I trial for safety and tolerability in patients with multiple sclerosis (ClinicalTrials.gov identifier: NCT01764737).
The above developments have increased interest in approaches to enhance the efficiency of biopharmaceutical drug delivery to the CNS. Local administration, active transport and conjugate approaches are being evaluated. The CNS exposure of systemically administered idursulphase, a lysosomal enzyme that is approved for the treatment of Hunter’s syndrome (a lysosome storage disorder), is insufficient to treat the cognitive impairment associated with the disease. Intrathecal administration via intracerebroventricular and lumbar routes resulted in widespread distribution of the drug in brain parenchyma, including its deposition in neuronal and oligodendrocyte lysosomes in normal non-human primates159. The clinical evaluation of intrathecally dosed idursulphase in conjunction with its systemic administration is underway for the treatment of paediatric patients with Hunter’s syndrome and the associated cognitive impairment (ClinicalTrials.gov identifiers: NCT00920647, NCT02055118).
Several groups have explored approaches to increase penetration within the brain or reduce the frequency of administration relative to what is achievable with local administration of conventional formulations. Following intracranial infusion in a non-human primate, ultrasound increased the distribution in the brain of liposomes and model compounds with a high molecular mass160. Encouraging results were reported when depot formulations of epidermal growth factor were administered epicortically in a mouse model of stroke161, and when brain-derived neurotrophic factor was incorporated in polymeric implants and injected into the rat hippocampus for evaluation in a model of depression162.
Active transport utilizes the internalization of receptors with high expression levels in the brain, such as the transferrin and insulin receptors. The approach has long been considered to be an attractive option for increasing the uptake of drugs into the brain following systemic administration. The fusion of the lysosomal enzyme arylsulphatase A with an insulin receptor-targeted IgG increased uptake to 1–2% of the injected dose in a non-human primate model163. In another study, a bispecific antibody was designed to increase CNS exposure via transcytosis by combining high-affinity binding to the therapeutic target (the enzyme β-secretase) with low-affinity binding against the transferrin receptor. When the binding affinity of the transferrin receptor was reduced, brain uptake was maximized and brain distribution improved164. Although promising, the approach resulted in acute clinical signs (including profound lethargy and spastic movements in some animals) and a reduction in reticulocytes in mice165. These effects were partially mitigated by removing the Fc effector function from the antibody.
In a related approach, a single transferrin receptor-binding Fab was fused to the Fc region of an amyloid-β-targeted monoclonal antibody, which increased target engagement in a mouse model of Alzheimer’s disease by over 55-fold166. Last, receptor-mediated transcytosis via the low-density lipoprotein receptor-related protein 1 (LRP1) is being evaluated for the delivery of antibodies to treat cancer. Preliminary data suggested that ANG4043, a HER2-targeted monoclonal antibody conjugated to a peptide that binds LRP1, increased survival in mice with intracranial BT-474 breast tumour cells167. ANG1005, a related molecule using LRP1 for the delivery of paclitaxel, is being evaluated in patients with breast cancer who have recurring brain metastases (ClinicalTrials.gov identifier: NCT02048059).
Conjugated forms of several biopharmaceutical drugs have improved brain penetration compared to their unmodified counterparts when administered intrathecally or systemically. For example, chemical modification of leptin with poly(ethylene oxide)-poly(propylene oxide) block copolymers improved the delivery of leptin across the blood–brain barrier when injected intravenously in a mouse model. This strategy is potentially attractive for the treatment of leptin resistance (which is attributed to impaired leptin transport) and the consequent obesity168. The approach resulted in a modest (less than twofold) increase in uptake with less than 0.5% of the injected dose detected in the brain, but therapeutic levels were nevertheless achieved. Improved pharmacokinetics of the conjugates may have been responsible for the sustained pharmacological effect observed.
As a second example, intrathecal administration of a PEG conjugate of fibroblast growth factor 2 (FGF2) in a blend of hyaluronan and methylcellulose (HAMC) to rats resulted in enhanced penetration in spinal cord tissue169. Finally, when amphiphilic block copolymers of poly(2-oxazoline) were conjugated to superoxide dismutase 1 (SOD1), there was increased uptake of the conjugate into MDCK cells and Caco-2 cells69. The conjugate also accumulated in mouse parenchyma by a non-saturable mechanism following intravenous administration170. The self-association of the SOD1 conjugates to form aggregates of 8–20 nm (depending on the composition of the side chain) may have affected their uptake into neurons; this effect was reported to occur through a lipid raft- or caveolae-dependent mechanism170.
Intracellular delivery
Owing to their hydrophilicity and poor membrane permeability, biopharmaceuticals have generally been restricted to targets in the vascular compartment or on the surface of cells — often referred to as the ‘accessible target space’. Various approaches have been undertaken to expand this space to include intracellular targets that were traditionally considered to be druggable only by small-molecule therapeutics, or not druggable at all (FIG. 7). A second area of potential opportunity for intracellular delivery involves human gene therapy. Current approaches to targeted genome editing require the intracellular delivery of nucleases or genetic material that encodes them (such as a plasmid DNA or mRNA).
One strategy for accessing intracellular targets focuses on altering the permeability of a biomolecule through the cell membrane. The ability of proteins and peptides to permeate the cell membrane can be enhanced through chemical conjugation or mutagenesis. Stapled peptides, which are a class of helical peptides that are modified by the introduction of aliphatic bridges to enhance cell penetration, are potentially promising as mitochondria-targeted agents for the treatment of cancer. A stapled BCL-2 homology 3 (BH3) peptide was shown to bind to intracellular BAX, a multidomain pro-apoptotic BCL-2 family protein171, and to overcome apoptotic resistance in mouse models of haematological cancers172. Stapled peptides that were designed for the therapeutic modulation of protein–protein interactions involving the intracellular transcription factor Notch had antiproliferative effects in a mouse model of T cell acute lymphoblastic leukaemia173. Moreover, a potent stapled peptide that was a dual inhibitor of MDM2 and MDX restored p53-dependent cell cycle arrest and apoptosis in p53-positive mouse xenografts174.
Zinc finger nucleases are fusions of the nonspecific cleavage domain of the FokI endonuclease and zinc finger proteins that are custom-designed for genome editing applications, and they were recently reported to undergo cellular uptake in culture in an unmodified form; this was attributed to their net positive charge175. In a related approach, macromolecular cargo have been fused to proteins engineered with a high net positive charge (so-called ‘supercharged proteins’) and shown to penetrate mammalian cells; proof of concept was demonstrated by in vivo delivery to mouse retina of Cre recombinase that was fused to a supercharged green fluorescent protein176,177.
Internalizing cell-surface receptors can offer access to intracellular drug targets or an avenue for increasing the efficiency of delivery, in a manner similar to the active transport approaches to CNS delivery discussed above. The conjugation of a zinc finger nuclease with transferrin via a reducible disulphide linkage resulted in rapid and efficient uptake in several cell lines, including primary mouse and human haematopoietic stem cell progenitors178. The approach was reported to match the efficiency of cDNA approaches but with improved temporal control of nuclease activity.
When internalization occurs via a vesicular mechanism, the endosomal membrane presents an additional delivery barrier to accessing the cytosol. Various approaches have addressed this challenge. A polymeric system that incorporates a pH-responsive endosomolytic feature has been developed for the intracellular delivery of several biomolecules. Intracellular delivery of a BH3 peptide with the polymeric system increased apoptotic activity in a HeLa cervical cancer cell line179, providing an alternative to the stapled peptide approach discussed above. The system was also evaluated for use as a prophylactic tumour vaccine by intracellularly delivering a model protein antigen to potentially access the cytosolic major histocompatibility class I (MHC-I) antigen presentation pathway and enhance the CD8+ cytotoxic lymphocyte response180. This resulted in increased tumour-free survival in a mouse xenograft model when the model protein antigen ovalbumin was incorporated in the polymeric carrier.
Concluding thoughts
The impact of biopharmaceutical drugs over the past decade has been facilitated by technological breakthroughs associated with manufacturing, formulation and delivery. Although outstanding progress has been made in the discovery and delivery of biopharmaceutical drugs, challenges and unmet needs remain. Current biopharmaceutical drugs are primarily aimed at extracellular targets owing to the challenges associated with intracellular delivery, and so improving intracellular delivery could result in new classes of biopharmaceutical drugs, including drugs against new intracellular targets.
Another area for future research is the development of new delivery devices for biopharmaceutical drugs that could overcome the hurdles that cannot be addressed by new formulations. Devices that make use of non-parenteral routes are especially appealing owing to their non-invasive nature. Efforts should be focused on making the devices safer and simpler to use. Perhaps one of the most exciting future opportunities lies in the expansion of the therapeutic target space. This will be enabled by new delivery technologies that allow access to sites (intracellular targets and the local tissue environment, such as the nervous system) that are not routinely available to injected molecules and can thus pave the path to unexplored therapeutic opportunities. Future research should focus on the discovery and development of methods that enable intracellular delivery.
Supplementary Material
Acknowledgements
The research of S.M. is supported by the US National Institutes of Health (NIH) grant R01DK097379. The research of R.L. is supported by the NIHR37-EB000244 grant (MIT # 6928649). The authors thank M. Citron for helpful discussions during the preparation of this Review.
Glossary
- Solvent evaporation
A process for microencapsulating drugs or other substances whereby an oil-in-water emulsion is formed, followed by the removal of the organic solvent by its evaporation from the emulsion mixture, resulting in the solidification of the oil phase to form microspheres.
- Atomization
A process for microencapsulating drugs or other substances whereby a polymer solution containing the drugs is broken up into droplets, followed by the removal of the polymer solvent by evaporation or other means, resulting in the formation of solid microspheres.
- Burst release
The quick release of drugs (usually within minutes to 24 hours) that are encapsulated in microspheres; the drug is associated with the microsphere surface and so is not completely protected from release by the microsphere structure.
- Core-shell nanoparticles
Microspheres or precipitates containing a core of one polymer that is surrounded by the shell of another polymer.
- Particulate formulations
Formulations comprising microspheres prepared from a polymer or other materials to encapsulate and release proteins.
- Implantable depots
Formulations that are too large in volume to be injected, and are instead administered by other means (for example, by insertion through a surgical incision)
- Injectable monoliths
A type of depot formulation that is fabricated as a contiguous solid mass, such as a cylinder, and can be administered by positive displacement from a syringe needle without the use of a suspending vehicle.
- Biosimilars
A biopharmaceutical drug that is demonstrated to be similar to, or interchangeable with, a licensed biological product, based on the absence of clinically meaningful differences in safety, purity and potency.
- New molecular entity
A drug product containing an active moiety or moieties that have not been previously approved by a regulatory authority, either as a single ingredient or as part of a combination product.
- Hydrodynamic radius
The effective hydrated radius of a biopharmaceutical drug, which dictates its rate of diffusion in solution and tissues.
- FcRn recycling
A process that is mediated by the neonatal Fc receptor (FcRn), which involves the transcytosis of maternal immunoglobulin G (IgG) across the placental membrane. This process is responsible for the long circulating half-lives of IgG and serum albumin throughout life, through a mechanism of protective vesicular trafficking.
- Cmax
The maximum plasma or serum concentration of a drug following administration.
- Living polymerization
A technique for synthesizing polymers where chain termination and transfer reactions are absent, and the rate of chain initiation substantially exceeds that of chain propagation. The resulting polymer chains have very similar lengths compared to traditional polymerization techniques.
- Kd
The dissociation constant a type of equilibrium constant that characterizes the propensity of a complex to separate reversibly into its constituents.
- Implantable pumps
Small devices that can be placed within the body and used to deliver a drug. The pumps carry a drug reservoir (which, in some cases, can be refilled through a port, thus avoiding the need for surgical intervention), a control mechanism to regulate delivery, and the delivery catheter.
- Insulin patch pumps
A wearable infusion pump that is attached to the skin and delivers insulin into the subcutaneous space.
- Liquid jet injections
A type of injection that enables the delivery of drugs into the skin and subdermal tissues — without using needles — by accelerating a stream of drug solution to high velocities.
- Absorption enhancers
Chemicals that increase the absorption of drugs across biological barriers such as the skin, intestinal epithelium or cell membrane.
- Chitosans
Linear polysaccharides of randomly arranged glucosamine and acetyl glycosamine.
- Therapeutic index
A measure of the safety of a particular drug, typically represented by the ratio of the dose causing overt toxicity to the dose providing a therapeutic effect. A drug with a large therapeutic index can be administered with low risk of eliciting a toxic effect.
- Tau
A highly soluble microtubule-associated protein found in neurons. Misfolded tau is associated with a variety of neurodegenerative disorders, including Alzheimer’s disease, in which interneuronal hyperphosphorylated tau tangles are a common pathological feature.
- Stapled peptides
A class of α-helical peptides incorporating α-methylation and hydrocarbon-based macrocyclic bridging features for increased hydrophobicity and conformational stabilization of the helix, resulting in improved membrane permeation.
Footnotes
Competing interests statement
The authors declare competing interests: see Web version for details.
FURTHER INFORMATION
Emisphere — 14 Dec 2011 press release (“Salmon Calcitonin for Osteoarthritis and Osteoporosis”): http://www.emisphere.com/salmon_calcitonin.html MannKind Corporation — 27 Jun 2014 press release (“MannKind Corporation Announces FDA Approval of AFREZZA®; A Novel, Rapid-Acting Inhaled Insulin for the Treatment of Diabetes”): http://www.news.mannkindcorp.com/phoenix.zhtml?c=147953&p=irol-newsArticle&ID=1943390&highlight=
References
- 1.Biotech products in big pharma clinical pipelines have grown dramatically. Tufts CSDD Impact Report. 2013;15:1–4. [No authors listed.] [Google Scholar]
- 2.Pharmaceutical Research and Manufacturers of America. Medicines in Development — Biologics (2013 report) PhRMA. 2013 [online], http://www.phrma.org/sites/default/files/pdf/biologics2013.pdf.
- 3.Albarran B, Hoffman AS, Stayton PS. Efficient intracellular delivery of a pro-apoptotic peptide with a pH-responsive carrier. React. Funct. Polym. 2011;71:261–265. doi: 10.1016/j.reactfunctpolym.2010.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Langer R, Folkman J. Polymers for the sustained release of proteins and other macromolecules. Nature. 1976;263:797–800. doi: 10.1038/263797a0. [DOI] [PubMed] [Google Scholar]
- 5.Cohen S, Yoshioka T, Lucarelli M, Hwang LH, Langer R. Controlled delivery systems for proteins based on poly(lactic/glycolic acid) microspheres. Pharm. Res. 1991;8:713–720. doi: 10.1023/a:1015841715384. [DOI] [PubMed] [Google Scholar]
- 6.Ron E, et al. Controlled release of polypeptides from polyanhydrides. Proc. Natl Acad. Sci. USA. 1993;90:4176–4180. doi: 10.1073/pnas.90.9.4176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gaur S, et al. Preclinical study of the cyclodextrin-polymer conjugate of camptothecin CRLX101 for the treatment of gastric cancer. Nanomedicine. 2012;8:721–730. doi: 10.1016/j.nano.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 8.Davis ME, Brewster ME. Cyclodextrin-based pharmaceutics: past, present and future. Nature Rev. Drug Discov. 2004;3:1023–1035. doi: 10.1038/nrd1576. [DOI] [PubMed] [Google Scholar]
- 9.Muthu MS, Rawat MK, Mishra A, Singh S. PLGA nanoparticle formulations of risperidone: preparation and neuropharmacological evaluation. Nanomedicine. 2009;5:323–333. doi: 10.1016/j.nano.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 10.Dunbar JL, et al. Single- and multiple-dose pharmacokinetics of long-acting injectable naltrexone. Alcohol Clin. Exp. Res. 2006;30:480–490. doi: 10.1111/j.1530-0277.2006.00052.x. [DOI] [PubMed] [Google Scholar]
- 11.Periti P, Mazzei T, Mini E. Clinical pharmacokinetics of depot leuprorelin. Clin. Pharmacokinet. 2002;41:485–504. doi: 10.2165/00003088-200241070-00003. [DOI] [PubMed] [Google Scholar]
- 12.DeYoung MB, MacConell L, Sarin V, Trautmann M, Herbert P. Encapsulation of exenatide in poly-(D,L-lactide-co-glycolide) microspheres produced an investigational long-acting once-weekly formulation for type 2 diabetes. Diabetes Technol. Ther. 2011;13:1145–1154. doi: 10.1089/dia.2011.0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wei Y, et al. A novel sustained-release formulation of recombinant human growth hormone and its pharmacokinetic, pharmacodynamic and safety profiles. Mol. Pharm. 2012;9:2039–2048. doi: 10.1021/mp300126t. [DOI] [PubMed] [Google Scholar]
- 14.Champion JA, Mitragotri S. Role of target geometry in phagocytosis. Proc. Natl Acad. Sci. USA. 2006;103:4930–4934. doi: 10.1073/pnas.0600997103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Radomsky ML, Whaley KJ, Cone RA, Saltzman WM. Macromolecules released from polymers: diffusion into unstirred fluids. Biomaterials. 1990;11:619–624. doi: 10.1016/0142-9612(90)90018-l. [DOI] [PubMed] [Google Scholar]
- 16.Bock N, Dargaville TR, Woodruff MA. Controlling microencapsulation and release of micronized proteins using poly(ethylene glycol) and electrospraying. Eur. J. Pharm. Biopharm. 2014;87:366–377. doi: 10.1016/j.ejpb.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 17.Putney SD, Burke PA. Improving protein therapeutics with sustained-release formulations. Nature Biotech. 1998;16:153–157. doi: 10.1038/nbt0298-153. [DOI] [PubMed] [Google Scholar]
- 18.Kim HK, Park TG. Microencapsulation of human growth hormone within biodegradable polyester microspheres: protein aggregation stability and incomplete release mechanism. Biotechnol. Bioeng. 1999;65:659–667. doi: 10.1002/(sici)1097-0290(19991220)65:6<659::aid-bit6>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 19.Burke PA, et al. Poly(lactide-co-glycolide) microsphere formulations of darbepoetin alfa: spray drying is an alternative to encapsulation by spray-freeze drying. Pharm. Res. 2004;21:500–506. doi: 10.1023/B:PHAM.0000019305.79599.a5. [DOI] [PubMed] [Google Scholar]
- 20.Ding AG, Shenderova A, Schwendeman SP. Prediction of microclimate pH in poly(lactic-co-glycolic acid) films. J. Am. Chem. Soc. 2006;128:5384–5390. doi: 10.1021/ja055287k. [DOI] [PubMed] [Google Scholar]
- 21.Zhu G, Mallery SR, Schwendeman SP. Stabilization of proteins encapsulated in injectable poly (lactide- co-glycolide) Nature Biotech. 2000;18:52–57. doi: 10.1038/71916. [DOI] [PubMed] [Google Scholar]
- 22.Hrkach J, et al. Preclinical development and clinical translation of a PSMA-targeted docetaxel nanoparticle with a differentiated pharmacological profile. Sci. Transl. Med. 2012;4:128ra39. doi: 10.1126/scitranslmed.3003651. [DOI] [PubMed] [Google Scholar]
- 23.Rahman MA, et al. Systemic delivery of siRNA nanoparticles targeting RRM2 suppresses head and neck tumor growth. J. Control Release. 2012;159:384–392. doi: 10.1016/j.jconrel.2012.01.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Simpkins F, et al. Chemoimmunotherapy using pegylated liposomal doxorubicin and interleukin-18 in recurrent ovarian cancer: a phase I dose-escalation study. Cancer Immunol. Res. 2013;1:168–178. doi: 10.1158/2326-6066.CIR-13-0098. [DOI] [PubMed] [Google Scholar]
- 25.Barenholz Y. Doxil® — the first FDA-approved nano-drug: lessons learned. J. Control Release. 2012;160:117–134. doi: 10.1016/j.jconrel.2012.03.020. [DOI] [PubMed] [Google Scholar]
- 26.Miele E, Spinelli GP, Miele E, Tomao F, Tomao S. Albumin-bound formulation of paclitaxel (Abraxane ABI-007) in the treatment of breast cancer. Int. J. Nanomed. 2009;4:99–105. doi: 10.2147/ijn.s3061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Von Hoff DD, et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N. Engl. J. Med. 2013;369:1691–1703. doi: 10.1056/NEJMoa1304369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bertrand N, Wu J, Xu X, Kamaly N, Farokhzad OC. Cancer nanotechnology: the impact of passive and active targeting in the era of modern cancer biology. Adv. Drug Deliv. Rev. 2014;66:2–25. doi: 10.1016/j.addr.2013.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Park J, et al. Combination delivery of TGF-β inhibitor and IL-2 by nanoscale liposomal polymeric gels enhances tumour immunotherapy. Nature Mater. 2012;11:895–905. doi: 10.1038/nmat3355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stephan MT, Moon JJ, Um SH, Bershteyn A, Irvine DJ. Therapeutic cell engineering with surface-conjugated synthetic nanoparticles. Nature Med. 2010;16:1035–1041. doi: 10.1038/nm.2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chaudhari KR, et al. Opsonization, biodistribution, cellular uptake and apoptosis study of PEGylated PBCA nanoparticle as potential drug delivery carrier. Pharm. Res. 2012;29:53–68. doi: 10.1007/s11095-011-0510-x. [DOI] [PubMed] [Google Scholar]
- 32.Nance EA, et al. A dense poly(ethylene glycol) coating improves penetration of large polymeric nanoparticles within brain tissue. Sci. Transl. Med. 2012;4:149ra119. doi: 10.1126/scitranslmed.3003594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sykes EA, Chen J, Zheng G, Chan WC. Investigating the impact of nanoparticle size on active and passive tumor targeting efficiency. ACS Nano. 2014;8:5696–5706. doi: 10.1021/nn500299p. [DOI] [PubMed] [Google Scholar]
- 34.Sugahara KN, et al. Coadministration of a tumor-penetrating peptide enhances the efficacy of cancer drugs. Science. 2010;328:1031–1035. doi: 10.1126/science.1183057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhao L, et al. Nanoparticle vaccines. Vaccine. 2014;32:327–337. doi: 10.1016/j.vaccine.2013.11.069. [DOI] [PubMed] [Google Scholar]
- 36.Leleux J, Roy K. Micro and nanoparticle-based delivery systems for vaccine immunotherapy: an immunological and materials perspective. Adv. Healthc. Mater. 2013;2:72–94. doi: 10.1002/adhm.201200268. [DOI] [PubMed] [Google Scholar]
- 37.Bregy A, et al. The role of Gliadel wafers in the treatment of high-grade gliomas. Expert Rev. Anticancer Ther. 2013;13:1453–1461. doi: 10.1586/14737140.2013.840090. [DOI] [PubMed] [Google Scholar]
- 38.Burdick J, Prestwich G. Hyaluronic acid hydrogels for biomedical applications. Adv. Mater. 2011;23:H41–H56. doi: 10.1002/adma.201003963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ghalanbor Z, Korber M, Bodmeier R. Improved lysozyme stability and release properties of poly(lactide-co-glycolide) implants prepared by hot-melt extrusion. Pharm. Res. 2010;27:371–379. doi: 10.1007/s11095-009-0033-x. [DOI] [PubMed] [Google Scholar]
- 40.Okumu FW, et al. Sustained delivery of human growth hormone from a novel gel system: SABER. Biomaterials. 2002;23:4353–4358. doi: 10.1016/s0142-9612(02)00174-6. [DOI] [PubMed] [Google Scholar]
- 41.Pechenov S, Shenoy B, Yang MX, Basu SK, Margolin AL. Injectable controlled release formulations incorporating protein crystals. J. Control Release. 2004;96:149–158. doi: 10.1016/j.jconrel.2004.01.019. [DOI] [PubMed] [Google Scholar]
- 42.Brodbeck KJ, Pushpala S, McHugh AJ. Sustained release of human growth hormone from PLGA solution depots. Pharm. Res. 1999;16:1825–1829. doi: 10.1023/a:1018943107688. [DOI] [PubMed] [Google Scholar]
- 43.Ravivarapu HB, Moyer KL, Dunn RL. Sustained suppression of pituitary-gonadal axis with an injectable, in situ forming implant of leuprolide acetate. J. Pharm. Sci. 2000;89:732–741. doi: 10.1002/(SICI)1520-6017(200006)89:6<732::AID-JPS4>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 44.Wright JC, Sekar M, Osdol W, Su HC, Miksztal AR. In: Long Acting Injections and Implants. Wright JC, Burgess DJ, editors. Springer; 2012. pp. 153–166. [Google Scholar]
- 45.Zentner GM, et al. Biodegradable block copolymers for delivery of proteins and water-insoluble drugs. J. Control Release. 2001;72:203–215. doi: 10.1016/s0168-3659(01)00276-0. [DOI] [PubMed] [Google Scholar]
- 46.Amiram M, Luginbuhl KM, Li X, Feinglos MN, Chilkoti A. A depot-forming glucagon-like peptide-1 fusion protein reduces blood glucose for five days with a single injection. J. Control Release. 2013;172:144–151. doi: 10.1016/j.jconrel.2013.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chan YP, Meyrueix R, Kravtzoff R, Nicolas F, Lundstrom K. Review on Medusa:a polymer-based sustained release technology for protein and peptide drugs. Expert Opin. Drug Deliv. 2007;4:441–451. doi: 10.1517/17425247.4.4.441. [DOI] [PubMed] [Google Scholar]
- 48.Oudard S, et al. Pharmacokinetics (PK) and immunologic responses in a phase I/II study of a sustained release formulation of IL-2 in renal cell carcinoma (RCC) patients. J. Clin. Oncol. Abstr. 2006;24:S2558. [Google Scholar]
- 49.Roberts J, Linden M, Cervin C, Tiberg F. Octreotide fluid crystal provides sustained octreotide bioavailability and similar IGF1 suppression to that of octreotide LAR (Sandostatin LAR): randomized, open-label, Phase I, repeat-dose study in healthy volunteers. Endocrine Abstracts. 2014;35:P914. [Google Scholar]
- 50.Jiskoot W, et al. Protein instability and immunogenicity: roadblocks to clinical application of injectable protein delivery systems for sustained release. J. Pharm. Sci. 2012;101:946–954. doi: 10.1002/jps.23018. [DOI] [PubMed] [Google Scholar]
- 51.Steinhilber D, et al. Surfactant free preparation of biodegradable dendritic polyglycerol nanogels by inverse nanoprecipitation for encapsulation and release of pharmaceutical biomacromolecules. J. Control Release. 2013;169:289–295. doi: 10.1016/j.jconrel.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 52.Schweizer D, Schonhammer K, Jahn M, Gopferich A. Protein-polyanion interactions for the controlled release of monoclonal antibodies. Biomacromolecules. 2013;14:75–83. doi: 10.1021/bm301352x. [DOI] [PubMed] [Google Scholar]
- 53.Schweizer D, et al. Pharmacokinetics, biocompatibility and bioavailability of a controlled release monoclonal antibody formulation. J. Control Release. 2013;172:975–982. doi: 10.1016/j.jconrel.2013.10.010. [DOI] [PubMed] [Google Scholar]
- 54.Hey T, Knoller H, Vorstheim P. In: Therapeutic Proteins: Strategies to Modulate Their Plasma Half-Lives. Kontermann R, editor. Wiley-VCH Verlag GmbH; 2012. pp. 117–140. [Google Scholar]
- 55.Pasut G, Veronese FM. State of the art in PEGylation: the great versatility achieved after forty years of research. J. Control Release. 2012;161:461–472. doi: 10.1016/j.jconrel.2011.10.037. [DOI] [PubMed] [Google Scholar]
- 56.Constantinou A, et al. Site-specific polysialylation of an antitumor single-chain Fv fragment. Bioconjug. Chem. 2009;20:924–931. doi: 10.1021/bc8005122. [DOI] [PubMed] [Google Scholar]
- 57.Mero A, Pasqualin M, Campisi M, Renier D, Pasut G. Conjugation of hyaluronan to proteins. Carbohydr. Polym. 2013;92:2163–2170. doi: 10.1016/j.carbpol.2012.11.090. [DOI] [PubMed] [Google Scholar]
- 58.Peters J. All About Albumin. Academic Press; 1995. [Google Scholar]
- 59.Bush MA, et al. Safety, tolerability, pharmacodynamics and pharmacokinetics of albiglutide, a long-acting glucagon-like peptide-1 mimetic, in healthy subjects. Diabetes Obes. Metab. 2009;11:498–505. doi: 10.1111/j.1463-1326.2008.00992.x. [DOI] [PubMed] [Google Scholar]
- 60.Santagostino E, et al. Safety and pharmacokinetics of a novel recombinant fusion protein linking coagulation factor IX with albumin (rIX-FP) in hemophilia B patients. Blood. 2012;120:2405–2411. doi: 10.1182/blood-2012-05-429688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.McDonagh CF, et al. Antitumor activity of a novel bispecific antibody that targets the ErbB2/ErbB3 oncogenic unit and inhibits heregulin-induced activation of ErbB3. Mol. Cancer Ther. 2012;11:582–593. doi: 10.1158/1535-7163.MCT-11-0820. [DOI] [PubMed] [Google Scholar]
- 62.Schulte S. Innovative coagulation factors: albumin fusion technology and recombinant single-chain factor VIII. Thromb. Res. 2013;131:S2–S6. doi: 10.1016/S0049-3848(13)70150-6. [DOI] [PubMed] [Google Scholar]
- 63.Powell JS, et al. Phase 3 study of recombinant factor IX Fc fusion protein in hemophilia B. N. Engl. J. Med. 2013;369:2313–2323. doi: 10.1056/NEJMoa1305074. [DOI] [PubMed] [Google Scholar]
- 64.Pandey BK, et al. Impact of site-specific PEGylation on the conformational stability and folding rate of the Pin WW domain depends strongly on PEG oligomer length. Bioconjug. Chem. 2013;24:796–802. doi: 10.1021/bc3006122. [DOI] [PubMed] [Google Scholar]
- 65.Ranganathan R, Lu KP, Hunter T, Noel JP. Structural and functional analysis of the mitotic rotamase Pin1 suggests substrate recognition is phosphorylation dependent. Cell. 1997;89:875–886. doi: 10.1016/s0092-8674(00)80273-1. [DOI] [PubMed] [Google Scholar]
- 66.Sherman MR, Williams LD, Sobczyk MA, Michaels SJ, Saifer MG. Role of the methoxy group in immune responses to mPEG-protein conjugates. Bioconjug. Chem. 2012;23:485–499. doi: 10.1021/bc200551b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Saifer MG, Williams LD, Sobczyk MA, Michaels SJ, Sherman MR. Selectivity of binding of PEGs and PEG-like oligomers to anti-PEG antibodies induced by methoxyPEG-proteins. Mol. Immunol. 2014;57:236–246. doi: 10.1016/j.molimm.2013.07.014. [DOI] [PubMed] [Google Scholar]
- 68.Santi DV, Schneider EL, Reid R, Robinson L, Ashley GW. Predictable and tunable half-life extension of therapeutic agents by controlled chemical release from macromolecular conjugates. Proc. Natl Acad. Sci. USA. 2012;109:6211–6216. doi: 10.1073/pnas.1117147109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tong J, Luxenhofer R, Yi X, Jordan R, Kabanov AV. Protein modification with amphiphilic block copoly(2-oxazoline)s as a new platform for enhanced cellular delivery. Mol. Pharm. 2010;7:984–992. doi: 10.1021/mp100102p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Egrie JC, Dwyer E, Browne JK, Hitz A, Lykos MA. Darbepoetin alfa has a longer circulating half-life and greater in vivo potency than recombinant human erythropoietin. Exp. Hematol. 2003;31:290–299. doi: 10.1016/s0301-472x(03)00006-7. [DOI] [PubMed] [Google Scholar]
- 71.Schellenberger V, et al. A recombinant polypeptide extends the in vivo half-life of peptides and proteins in a tunable manner. Nature Biotech. 2009;27:1186–1190. doi: 10.1038/nbt.1588. [DOI] [PubMed] [Google Scholar]
- 72.Cleland JL, Shore CR, Kipnes MS. A placebo controlled single ascending dose Phase 1 for safety, tolerability, pharmacokinetics and pharmacodynamics of VRS-859 in patients with T2DM (Poster) Diabetologia. 2011;54:S318. [Google Scholar]
- 73.Cleland JL, et al. A novel long-acting human growth hormone fusion protein (VRS-317): enhanced in vivo potency and half-life. J. Pharm. Sci. 2012;101:2744–2754. doi: 10.1002/jps.23229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yuen KC, et al. A long-acting human growth hormone with delayed clearance (VRS-317): results of a double-blind, placebo-controlled, single ascending dose study in growth hormone-deficient adults. J. Clin. Endocrinol. Metab. 2013;98:2595–2603. doi: 10.1210/jc.2013-1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zalevsky J, et al. Enhanced antibody half-life improves in vivo activity. Nature Biotech. 2010;28:157–159. doi: 10.1038/nbt.1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Suzuki T, et al. Importance of neonatal FcR in regulating the serum half-life of therapeutic proteins containing the Fc domain of human IgG1: a comparative study of the affinity of monoclonal antibodies and Fc-fusion proteins to human neonatal FcR. J. Immunol. 2010;184:1968–1976. doi: 10.4049/jimmunol.0903296. [DOI] [PubMed] [Google Scholar]
- 77.Yeung YA, et al. Engineering human IgG1 affinity to human neonatal Fc receptor: impact of affinity improvement on pharmacokinetics in primates. J. Immunol. 2009;182:7663–7671. doi: 10.4049/jimmunol.0804182. [DOI] [PubMed] [Google Scholar]
- 78.Andersen JT, et al. Structure-based mutagenesis reveals the albumin-binding site of the neonatal Fc receptor. Nature Commun. 2012;3:610. doi: 10.1038/ncomms1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sleep D, Cameron J, Evans LR. Albumin as a versatile platform for drug half-life extension. Biochim. Biophys. Acta. 2013;1830:5526–5534. doi: 10.1016/j.bbagen.2013.04.023. [DOI] [PubMed] [Google Scholar]
- 80.Kermode M. Unsafe injections in low-income country health settings: need for injection safety promotion to prevent the spread of blood-borne viruses. Health Promot. Int. 2004;19:95–103. doi: 10.1093/heapro/dah110. [DOI] [PubMed] [Google Scholar]
- 81.Hirose M, Beverly EA, Weinger K. Quality of life and technology: impact on children and families with diabetes. Curr. Diab. Rep. 2012;12:711–720. doi: 10.1007/s11892-012-0313-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ricotti L, Assaf T, Dario P, Menciassi A. Wearable and implantable pancreas substitutes. J. Artif. Organs. 2013;16:9–22. doi: 10.1007/s10047-012-0660-6. [DOI] [PubMed] [Google Scholar]
- 83.Papargyri P, et al. An observational 7-year study of continuous subcutaneous insulin infusion for the treatment of type 1 diabetes mellitus. Endocrinol. Nutr. 2013;61:141–146. doi: 10.1016/j.endonu.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 84.Schaepelynck P, et al. Advances in pump technology: insulin patch pumps, combined pumps and glucose sensors, and implanted pumps. Diabetes Metab. 2011;37:S85–S93. doi: 10.1016/S1262-3636(11)70972-7. [DOI] [PubMed] [Google Scholar]
- 85.Richards Grayson AC, et al. Multi-pulse drug delivery from a resorbable polymeric microchip device. Nature Mater. 2003;2:767–772. doi: 10.1038/nmat998. [DOI] [PubMed] [Google Scholar]
- 86.Farra R, et al. First-in-human testing of a wirelessly controlled drug delivery microchip. Sci. Transl. Med. 2012;4:122ra21. doi: 10.1126/scitranslmed.3003276. [DOI] [PubMed] [Google Scholar]
- 87.Zisser H, et al. Clinical update on optimal prandial insulin dosing using a refined run-to-run control algorithm. J. Diabetes Sci. Technol. 2009;3:487–491. doi: 10.1177/193229680900300312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Engwerda EE, Abbink EJ, Tack CJ, de Galan BE. Improved pharmacokinetic and pharmacodynamic profile of rapid-acting insulin using needle-free jet injection technology. Diabetes Care. 2011;34:1804–1808. doi: 10.2337/dc11-0182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Baxter J, Mitragotri S. Needle-free liquid jet injections: mechanisms and applications. Expert Rev. Med. Devices. 2006;3:565–574. doi: 10.1586/17434440.3.5.565. [DOI] [PubMed] [Google Scholar]
- 90.Jackson LA, et al. Safety and immunogenicity of varying dosages of trivalent inactivated influenza vaccine administered by needle-free jet injectors. Vaccine. 2001;19:4703–4709. doi: 10.1016/s0264-410x(01)00225-0. [DOI] [PubMed] [Google Scholar]
- 91.Arora A, et al. Needle-free delivery of macromolecules across the skin by nanoliter-volume pulsed microjets. Proc. Natl Acad. Sci. USA. 2007;104:4255–4260. doi: 10.1073/pnas.0700182104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Stachowiak JC, Li TH, Arora A, Mitragotri S, Fletcher DA. Dynamic control of needle-free jet injection. J. Control Release. 2009;135:104–112. doi: 10.1016/j.jconrel.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 93.Taberner A, Hogan NC, Hunter IW. Needle-free jet injection using real-time controlled linear Lorentz-force actuators. Med. Eng. Phys. 2012;34:1228–1235. doi: 10.1016/j.medengphy.2011.12.010. [DOI] [PubMed] [Google Scholar]
- 94.Edwards DA, et al. Large porous particles for pulmonary drug delivery. Science. 1997;276:1868–1871. doi: 10.1126/science.276.5320.1868. [DOI] [PubMed] [Google Scholar]
- 95.Peichl P, et al. Salmon calcitonin nasal spray treatment for postmenopausal women after hip fracture with total hip arthroplasty. J. Bone Miner. Metab. 2005;23:243–252. doi: 10.1007/s00774-004-0591-2. [DOI] [PubMed] [Google Scholar]
- 96.Whitehead K, Shen Z, Mitragotri S. Oral delivery of macromolecules using intestinal patches: applications for insulin delivery. J. Control Release. 2004;98:37–45. doi: 10.1016/j.jconrel.2004.04.013. [DOI] [PubMed] [Google Scholar]
- 97.Mitragotri S, Blankschtein D, Langer R. Ultrasound-mediated transdermal protein delivery. Science. 1995;269:850–853. doi: 10.1126/science.7638603. [DOI] [PubMed] [Google Scholar]
- 98.Alba N, Naik A, Guy RH, Kalia YN. Effect of charge and molecular weight on transdermal peptide delivery by iontophoresis. Pharm. Res. 2005;22:2069–2078. doi: 10.1007/s11095-005-8110-2. [DOI] [PubMed] [Google Scholar]
- 99.Lennernas H. Intestinal permeability and its relevance for absorption and elimination. Xenobiotica. 2007;37:1015–1051. doi: 10.1080/00498250701704819. [DOI] [PubMed] [Google Scholar]
- 100.Wertz PW. Current understanding of skin biology pertinent to skin penetration: skin biochemistry. Skin Pharmacol. Physiol. 2013;26:217–226. doi: 10.1159/000351949. [DOI] [PubMed] [Google Scholar]
- 101.Rosenstock J, et al. Safety and efficacy of inhaled human insulin (exubera) during discontinuation and readministration of therapy in adults with type 2 diabetes: a 3-year randomized controlled trial. Diabetes Technol. Ther. 2009;11:697–705. doi: 10.1089/dia.2009.0062. [DOI] [PubMed] [Google Scholar]
- 102.Zisser H, et al. Technosphere insulin effectively controls postprandial glycemia in patients with type 2 diabetes mellitus. Diabetes Technol. Ther. 2012;14:997–1001. doi: 10.1089/dia.2012.0101. [DOI] [PubMed] [Google Scholar]
- 103.Prausnitz MR, Langer R. Transdermal drug delivery. Nature Biotech. 2008;26:1261–1268. doi: 10.1038/nbt.1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Chen Y, et al. Transdermal protein delivery by a coadministered peptide identified via phage display. Nature Biotech. 2006;24:455–460. doi: 10.1038/nbt1193. [DOI] [PubMed] [Google Scholar]
- 105.Hsu T, Mitragotri S. Delivery of siRNA and other macromolecules into skin and cells using a peptide enhancer. Proc. Natl Acad. Sci. USA. 2011;108:15816–15821. doi: 10.1073/pnas.1016152108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Rothbard JB, et al. Conjugation of arginine oligomers to cyclosporin A facilitates topical delivery and inhibition of inflammation. Nature Med. 2000;6:1253–1257. doi: 10.1038/81359. [DOI] [PubMed] [Google Scholar]
- 107.Chen M, Gupta V, Anselmo AC, Muraski JA, Mitragotri S. Topical delivery of hyaluronic acid into skin using SPACE-peptide carriers. J. Control Release. 2014;173:67–74. doi: 10.1016/j.jconrel.2013.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Karande P, et al. Transcutaneous immunization using common chemicals. J. Control Release. 2009;138:134–140. doi: 10.1016/j.jconrel.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 109.Mitragotri S. Engineering approaches to transdermal drug delivery: a tribute to contributions of Prof. Robert Langer. Skin Pharmacol. Physiol. 2013;26:263–276. doi: 10.1159/000351947. [DOI] [PubMed] [Google Scholar]
- 110.Park EJ, Dodds J, Smith NB. Dose comparison of ultrasonic transdermal insulin delivery to subcutaneous insulin injection. Int. J. Nanomed. 2008;3:335–341. doi: 10.2147/ijn.s2761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Rastogi R, Anand S, Dinda AK, Koul V. Investigation on the synergistic effect of a combination of chemical enhancers and modulated iontophoresis for transdermal delivery of insulin. Drug Dev. Ind. Pharm. 2010;36:993–1004. doi: 10.3109/03639041003682012. [DOI] [PubMed] [Google Scholar]
- 112.Medi BM, Singh J. Electronically facilitated transdermal delivery of human parathyroid hormone (1–34) Int. J. Pharm. 2003;263:25–33. doi: 10.1016/s0378-5173(03)00337-5. [DOI] [PubMed] [Google Scholar]
- 113.Kim do K, Choi SW, Kwak YH. The effect of SonoPrep® on EMLA® cream application for pain relief prior to intravenous cannulation. Eur. J. Pediatr. 2012;171:985–988. doi: 10.1007/s00431-012-1696-6. [DOI] [PubMed] [Google Scholar]
- 114.Song JM, et al. Microneedle delivery of H5N1 influenza virus-like particles to the skin induces long-lasting B- and T-cell responses in mice. Clin. Vaccine Immunol. 2010;17:1381–1389. doi: 10.1128/CVI.00100-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Weldon WC, et al. Microneedle vaccination with stabilized recombinant influenza virus hemagglutinin induces improved protective immunity. Clin. Vaccine Immunol. 2011;18:647–654. doi: 10.1128/CVI.00435-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Morishita M, Peppas NA. Is the oral route possible for peptide and protein drug delivery? Drug Discov. Today. 2006;11:905–910. doi: 10.1016/j.drudis.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 117.Niu M, et al. Hypoglycemic activity and oral bioavailability of insulin-loaded liposomes containing bile salts in rats: the effect of cholate type, particle size and administered dose. Eur. J. Pharm. Biopharm. 2012;81:265–272. doi: 10.1016/j.ejpb.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 118.Motlekar NA, Srivenugopal KS, Wachtel MS, Youan BB. Oral delivery of low-molecular-weight heparin using sodium caprate as absorption enhancer reaches therapeutic levels. J. Drug Target. 2005;13:573–583. doi: 10.1080/10611860500471906. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 119.Yang T, Arnold JJ, Ahsan F. Tetradecylmaltoside (TDM) enhances in vitro and in vivo intestinal absorption of enoxaparin, a low molecular weight heparin. J. Drug Target. 2005;13:29–38. doi: 10.1080/10611860400020191. [DOI] [PubMed] [Google Scholar]
- 120.Whitehead K, Karr N, Mitragotri S. Discovery of synergistic permeation enhancers for oral drug delivery. J. Control Release. 2008;128:128–133. doi: 10.1016/j.jconrel.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 121.Gupta V, Hwang BH, Doshi N, Mitragotri S. A permeation enhancer for increasing transport of therapeutic macromolecules across the intestine. J. Control Release. 2013;172:541–549. doi: 10.1016/j.jconrel.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 122.Wood KM, Stone GM, Peppas NA. Wheat germ agglutinin functionalized complexation hydrogels for oral insulin delivery. Biomacromolecules. 2008;9:1293–1298. doi: 10.1021/bm701274p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ahn S, et al. Oral delivery of an anti-diabetic peptide drug via conjugation and complexation with low molecular weight chitosan. J. Control Release. 2013;170:226–232. doi: 10.1016/j.jconrel.2013.05.031. [DOI] [PubMed] [Google Scholar]
- 124.Dunnhaupt S, et al. In vivo evaluation of an oral drug delivery system for peptides based on S-protected thiolated chitosan. J. Control Release. 2012;160:477–485. doi: 10.1016/j.jconrel.2012.04.020. [DOI] [PubMed] [Google Scholar]
- 125.Morishita M, et al. Novel oral insulin delivery systems based on complexation polymer hydrogels: single and multiple administration studies in type 1 and 2 diabetic rats. J. Control Release. 2006;110:587–594. doi: 10.1016/j.jconrel.2005.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Eiamtrakarn S, et al. Gastrointestinal mucoadhesive patch system (GI-MAPS) for oral administration of G-CSF, a model protein. Biomaterials. 2002;23:145–152. doi: 10.1016/s0142-9612(01)00089-8. [DOI] [PubMed] [Google Scholar]
- 127.Gupta V, et al. Mucoadhesive intestinal devices for oral delivery of salmon calcitonin. J. Control Release. 2013;172:753–762. doi: 10.1016/j.jconrel.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 128.Pridgen EM, et al. Transepithelial transport of Fc-targeted nanoparticles by the neonatal Fc receptor for oral delivery. Sci. Transl. Med. 2013;5:213ra167. doi: 10.1126/scitranslmed.3007049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Maher S, Leonard TW, Jacobsen J, Brayden DJ. Safety and efficacy of sodium caprate in promoting oral drug absorption: from in vitro to the clinic. Adv. Drug Deliv. Rev. 2009;61:1427–1449. doi: 10.1016/j.addr.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 130.Raoof AA, et al. Effect of sodium caprate on the intestinal absorption of two modified antisense oligonucleotides in pigs. Eur. J. Pharm. Sci. 2002;17:131–138. doi: 10.1016/s0928-0987(02)00162-8. [DOI] [PubMed] [Google Scholar]
- 131.Karsdal MA, et al. The effect of oral salmon calcitonin delivered with 5-CNAC on bone and cartilage degradation in osteoarthritic patients: a 14-day randomized study. Osteoarthritis Cartilage. 2010;18:150–159. doi: 10.1016/j.joca.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 132.Mousa SA, et al. Pharmacokinetics and pharmacodynamics of oral heparin solid dosage form in healthy human subjects. J. Clin. Pharmacol. 2007;47:1508–1520. doi: 10.1177/0091270007307242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Tillman LG, Geary RS, Hardee GE. Oral delivery of antisense oligonucleotides in man. J. Pharm. Sci. 2008;97:225–236. doi: 10.1002/jps.21084. [DOI] [PubMed] [Google Scholar]
- 134.Harrison C. Deal watch: Chiasma and Roche partner in oral peptide drug delivery. Nature Rev. Drug Discov. 2013;12:255. doi: 10.1038/nrd3989. [DOI] [PubMed] [Google Scholar]
- 135.Eldor R, Arbit E, Corcos A, Kidron M. Glucose-reducing effect of the ORMD-0801 oral insulin preparation in patients with uncontrolled type 1 diabetes: a pilot study. PLoS ONE. 2013;8:e59524. doi: 10.1371/journal.pone.0059524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Kidron M, Shushlav Y, Ovadia O, Arbit E. A novel glucagon-like peptide-1 analog delivered orally reduces postprandial glucose excursion in a porcine model. J. Diabetes Sci. Technol; Ninth Annual Diabetes Technology Meeting; 5–7 November 2009; San Francisco. 2010. Abstract A71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Welling SH, et al. The role of citric acid in oral peptide and protein formulations: relationship between calcium chelation and proteolysis inhibition. Eur. J. Pharm. Biopharm. 2014;86:544–551. doi: 10.1016/j.ejpb.2013.12.017. [DOI] [PubMed] [Google Scholar]
- 138.Binkley N, et al. A phase 3 trial of the efficacy and safety of oral recombinant calcitonin: the Oral Calcitonin in Postmenopausal Osteoporosis (ORACAL) trial. J. Bone Miner. Res. 2012;27:1821–1829. doi: 10.1002/jbmr.1602. [DOI] [PubMed] [Google Scholar]
- 139.Pozzilli P, Raskin P, Parkin CG. Review of clinical trials: update on oral insulin spray formulation. Diabetes Obes. Metab. 2010;12:91–96. doi: 10.1111/j.1463-1326.2009.01127.x. [DOI] [PubMed] [Google Scholar]
- 140.Senel S, Rathbone MJ, Cansiz M, Pather I. Recent developments in buccal and sublingual delivery systems. Expert Opin. Drug Deliv. 2012;9:615–628. doi: 10.1517/17425247.2012.676040. [DOI] [PubMed] [Google Scholar]
- 141.Lee YC, Simamora P, Pinsuwan S, Yalkowsky SH. Review on the systemic delivery of insulin via the ocular route. Int. J. Pharm. 2002;233:1–18. doi: 10.1016/s0378-5173(01)00920-6. [DOI] [PubMed] [Google Scholar]
- 142.Davis JL, Gilger BC, Robinson MR. Novel approaches to ocular drug delivery. Curr. Opin. Mol. Ther. 2004;6:195–205. [PubMed] [Google Scholar]
- 143.Illum L. Nasal drug delivery — possibilities, problems and solutions. J. Control Release. 2003;87:187–198. doi: 10.1016/s0168-3659(02)00363-2. [DOI] [PubMed] [Google Scholar]
- 144.Urtti A. In: Proteins and Peptides: Pharmacokinetic, Pharmacodynamic, and Metabolic Outcomes. 1st edn. Mrsny R, Daugherty A, editors. Informa; 2010. pp. 163–172. [Google Scholar]
- 145.Zolot RS, Basu S, Million RP. Antibody-drug conjugates. Nature Rev. Drug Discov. 2013;12:259–260. doi: 10.1038/nrd3980. [DOI] [PubMed] [Google Scholar]
- 146.Zheng D, et al. Topical delivery of siRNA-based spherical nucleic acid nanoparticle conjugates for gene regulation. Proc. Natl Acad. Sci. USA. 2012;109:11975–11980. doi: 10.1073/pnas.1118425109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Akinc A, et al. Development of lipidoid-siRNA formulations for systemic delivery to the liver. Mol. Ther. 2009;17:872–879. doi: 10.1038/mt.2009.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Alvarez-Erviti L, et al. Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nature Biotech. 2011;29:341–345. doi: 10.1038/nbt.1807. [DOI] [PubMed] [Google Scholar]
- 149.Davis ME, et al. Evidence of RNAi in humans from systemically administered siRNA via targeted nanoparticles. Nature. 2010;464:1067–1070. doi: 10.1038/nature08956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Wu SY, Lopez-Berestein G, Calin GA, Sood AK. RNAi therapies: drugging the undruggable. Sci. Transl. Med. 2014;6:240ps247. doi: 10.1126/scitranslmed.3008362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Bard F, et al. Peripherally administered antibodies against amyloid β-peptide enter the central nervous system and reduce pathology in a mouse model of Alzheimer disease. Nature Med. 2000;6:916–919. doi: 10.1038/78682. [DOI] [PubMed] [Google Scholar]
- 152.Thompson EJ, Keir G. Laboratory investigation of cerebrospinal fluid proteins. Ann. Clin. Biochem. 1990;27:425–435. doi: 10.1177/000456329002700503. [DOI] [PubMed] [Google Scholar]
- 153.Atwal JK, et al. A therapeutic antibody targeting BACE1 inhibits amyloid-β production in vivo. Sci. Transl. Med. 2011;3:84ra43. doi: 10.1126/scitranslmed.3002254. [DOI] [PubMed] [Google Scholar]
- 154.Masliah E, et al. Passive immunization reduces behavioral and neuropathological deficits in an alpha-synuclein transgenic model of Lewy body disease. PLoS ONE. 2011;6:e19338. doi: 10.1371/journal.pone.0019338. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 155.Chai X, et al. Passive immunization with anti-Tau antibodies in two transgenic models: reduction of Tau pathology and delay of disease progression. J. Biol. Chem. 2011;286:34457–34467. doi: 10.1074/jbc.M111.229633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Yanamandra K, et al. Anti-tau antibodies that block tau aggregate seeding in vitro markedly decrease pathology and improve cognition in vivo. Neuron. 2013;80:402–414. doi: 10.1016/j.neuron.2013.07.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Karran E, Hardy J. Antiamyloid therapy for Alzheimer’s disease — are we on the right road? N. Engl. J. Med. 2014;370:377–378. doi: 10.1056/NEJMe1313943. [DOI] [PubMed] [Google Scholar]
- 158.Jonason A, et al. P573: Development of anti-SEMA4D monoclonal antibody for the treatment of multiple sclerosis. Mult. Scler. 2013;19:S240–S241. [Google Scholar]
- 159.Calias P, et al. CNS penetration of intrathecal-lumbar idursulfase in the monkey, dog and mouse: implications for neurological outcomes of lysosomal storage disorder. PLoS ONE. 2012;7:e30341. doi: 10.1371/journal.pone.0030341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Liu Y, et al. Ultrasound-enhanced drug transport and distribution in the brain. AAPS PharmSciTech. 2010;11:1005–1017. doi: 10.1208/s12249-010-9458-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Cooke MJ, Wang Y, Morshead CM, Shoichet MS. Controlled epi-cortical delivery of epidermal growth factor for the stimulation of endogenous neural stem cell proliferation in stroke-injured brain. Biomaterials. 2011;32:5688–5697. doi: 10.1016/j.biomaterials.2011.04.032. [DOI] [PubMed] [Google Scholar]
- 162.Sirianni RW, Olausson P, Chiu AS, Taylor JR, Saltzman WM. The behavioral and biochemical effects of BDNF containing polymers implanted in the hippocampus of rats. Brain Res. 2010;1321:40–50. doi: 10.1016/j.brainres.2010.01.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Boado RJ, Lu JZ, Hui EK, Sumbria RK, Pardridge WM. Pharmacokinetics and brain uptake in the rhesus monkey of a fusion protein of arylsulfatase a and a monoclonal antibody against the human insulin receptor. Biotechnol. Bioeng. 2013;110:1456–1465. doi: 10.1002/bit.24795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Yu YJ, et al. Boosting brain uptake of a therapeutic antibody by reducing its affinity for a transcytosis target. Sci. Transl. Med. 2011;3:84ra44. doi: 10.1126/scitranslmed.3002230. [DOI] [PubMed] [Google Scholar]
- 165.Couch JA, et al. Addressing safety liabilities of TfR bispecific antibodies that cross the blood-brain barrier. Sci. Transl. Med. 2013;5:183ra57. doi: 10.1126/scitranslmed.3005338. [DOI] [PubMed] [Google Scholar]
- 166.Niewoehner J, et al. Increased brain penetration and potency of a therapeutic antibody using a monovalent molecular shuttle. Neuron. 2014;81:49–60. doi: 10.1016/j.neuron.2013.10.061. [DOI] [PubMed] [Google Scholar]
- 167.Lachowicz JE, et al. ANG4043, a brain-penetrant anti-HER2 mAb increases survival in mice bearing intracranial BT-474 breast tumor cells. Cancer Res. 2013;73(Suppl. 24) P6-11-05. [Google Scholar]
- 168.Price TO, et al. Transport across the blood-brain barrier of pluronic leptin. J. Pharmacol. Exp. Ther. 2010;333:253–263. doi: 10.1124/jpet.109.158147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Kang CE, Tator CH, Shoichet MS. Poly(ethylene glycol) modification enhances penetration of fibroblast growth factor 2 to injured spinal cord tissue from an intrathecal delivery system. J. Control Release. 2010;144:25–31. doi: 10.1016/j.jconrel.2010.01.029. [DOI] [PubMed] [Google Scholar]
- 170.Tong J, et al. Conjugates of superoxide dismutase 1 with amphiphilic poly(2-oxazoline) block copolymers for enhanced brain delivery: synthesis, characterization and evaluation in vitro and in vivo. Mol. Pharm. 2013;10:360–377. doi: 10.1021/mp300496x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Walensky LD, et al. A stapled BID BH3 helix directly binds and activates BAX. Mol. Cell. 2006;24:199–210. doi: 10.1016/j.molcel.2006.08.020. [DOI] [PubMed] [Google Scholar]
- 172.LaBelle JL, et al. A stapled BIM peptide overcomes apoptotic resistance in hematologic cancers. J. Clin. Invest. 2012;122:2018–2031. doi: 10.1172/JCI46231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Moellering RE, et al. Direct inhibition of the NOTCH transcription factor complex. Nature. 2009;462:182–188. doi: 10.1038/nature08543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Chang YS, et al. Stapled α-helical peptide drug development: a potent dual inhibitor of MDM2 and MDMX for p53-dependent cancer therapy. Proc. Natl Acad. Sci. USA. 2013;110:E3445–E3454. doi: 10.1073/pnas.1303002110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Gaj T, Guo J, Kato Y, Sirk SJ, Barbas CF. Targeted gene knockout by direct delivery of zinc-finger nuclease proteins. Nature Methods. 2012;9:805–807. doi: 10.1038/nmeth.2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Cronican JJ, et al. Potent delivery of functional proteins into mammalian cells in vitro and in vivo using a supercharged protein. ACS Chem. Biol. 2010;5:747–752. doi: 10.1021/cb1001153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Cronican JJ, et al. A class of human proteins that deliver functional proteins into mammalian cells in vitro and in vivo. Chem. Biol. 2011;18:833–838. doi: 10.1016/j.chembiol.2011.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Chen Z, et al. Receptor-mediated delivery of engineered nucleases for genome modification. Nucleic Acids Res. 2013;41:e182. doi: 10.1093/nar/gkt710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Duvall CL, Convertine AJ, Benoit DS, Hoffman AS, Stayton PS. Intracellular delivery of a proapoptotic peptide via conjugation to a RAFT synthesized endosomolytic polymer. Mol. Pharm. 2010;7:468–476. doi: 10.1021/mp9002267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Foster S, Duvall CL, Crownover EF, Hoffman AS, Stayton PS. Intracellular delivery of a protein antigen with an endosomal-releasing polymer enhances CD8 T-cell production and prophylactic vaccine efficacy. Bioconjug Chem. 2010;21:2205–2212. doi: 10.1021/bc100204m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Cleland JL, Powell MF, Shire SJ. The development of stable protein formulations: a close look at protein aggregation, deamidation, and oxidation. Crit. Rev. Ther. Drug Carrier Syst. 1993;10:307–377. [PubMed] [Google Scholar]
- 182.Daugherty AL, Mrsny RJ. Formulation and delivery issues for monoclonal antibody therapeutics. Adv. Drug Deliv. Rev. 2006;58:686–706. doi: 10.1016/j.addr.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 183.Rajagopal K, Wood J, Tran B, Patapoff TW, Nivaggioli T. Trehalose limits BSA aggregation in spray-dried formulations at high temperatures: implications in preparing polymer implants for long-term protein delivery. J. Pharm. Sci. 2013;102:2655–2666. doi: 10.1002/jps.23634. [DOI] [PubMed] [Google Scholar]
- 184.Allison SD, Chang B, Randolph TW, Carpenter JF. Hydrogen bonding between sugar and protein is responsible for inhibition of dehydration-induced protein unfolding. Arch. Biochem. Biophys. 1999;365:289–298. doi: 10.1006/abbi.1999.1175. [DOI] [PubMed] [Google Scholar]
- 185.Sasahara K, McPhie P, Minton AP. Effect of dextran on protein stability and conformation attributed to macromolecular crowding. J. Mol. Biol. 2003;326:1227–1237. doi: 10.1016/s0022-2836(02)01443-2. [DOI] [PubMed] [Google Scholar]
- 186.Kerwin BA. Polysorbates 20 and 80 used in the formulation of protein biotherapeutics: structure and degradation pathways. J. Pharm. Sci. 2008;97:2924–2935. doi: 10.1002/jps.21190. [DOI] [PubMed] [Google Scholar]
- 187.Schwendeman SP, et al. Stabilization of tetanus and diphtheria toxoids against moisture-induced aggregation. Proc. Natl Acad. Sci. USA. 1995;92:11234–11238. doi: 10.1073/pnas.92.24.11234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Yadav S, Shire S, Kalonia D. Factors affecting the viscosity in high concentration solutions of different monoclonal antibodies. J. Pharm. Sci. 2010;99:4812–4829. doi: 10.1002/jps.22190. [DOI] [PubMed] [Google Scholar]
- 189.Du W, Klibanov AM. Hydrophobic salts markedly diminish viscosity of concentrated protein solutions. Biotechnol. Bioeng. 2011;108:632–636. doi: 10.1002/bit.22983. [DOI] [PubMed] [Google Scholar]
- 190.Liu J, Nguyen M, Andya J, Shire S. Reversible self-association increases the viscosity of a concentrated monoclonal antibody in aqueous solution. J. Pharm. Sci. 2005;94:1928–1940. doi: 10.1002/jps.20347. [DOI] [PubMed] [Google Scholar]
- 191.Inoue N, Takai E, Arakawa T, Shiraki K. Arginine and lysine reduce the high viscosity of serum albumin solutions for pharmaceutical injection. J. Biosci. Bioeng. 2014;117:539–543. doi: 10.1016/j.jbiosc.2013.10.016. [DOI] [PubMed] [Google Scholar]
- 192.Yearley EJ, et al. Observation of small cluster formation in concentrated monoclonal antibody solutions and its implications to solution viscosity. Biophys. J. 2014;106:1763–1770. doi: 10.1016/j.bpj.2014.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Jiang P, et al. Effective targeting of the tumor microenvironment for cancer therapy. Anticancer Res. 2012;32:1203–1212. [PubMed] [Google Scholar]
- 194.Domansky K, et al. Perfused multiwell plate for 3D liver tissue engineering. Lab. Chip. 2010;10:51–58. doi: 10.1039/b913221j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Sasaki S, et al. In vivo evaluation of a novel scaffold for artificial corneas prepared by using ultrahigh hydrostatic pressure to decellularize porcine corneas. Mol. Vis. 2009;15:2022–2028. [PMC free article] [PubMed] [Google Scholar]
- 196.Teng YD, et al. Functional recovery following traumatic spinal cord injury mediated by a unique polymer scaffold seeded with neural stem cells. Proc. Natl Acad. Sci. USA. 2002;99:3024–3029. doi: 10.1073/pnas.052678899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Wagner I, et al. A dynamic multi-organ-chip for long-term cultivation and substance testing proven by 3D human liver and skin tissue co-culture. Lab. Chip. 2013;13:3538–3547. doi: 10.1039/c3lc50234a. [DOI] [PubMed] [Google Scholar]
- 198.Orlando G, et al. Production and implantation of renal extracellular matrix scaffolds from porcine kidneys as a platform for renal bioengineering investigations. Ann. Surg. 2012;256:363–370. doi: 10.1097/SLA.0b013e31825a02ab. [DOI] [PubMed] [Google Scholar]
- 199.Mountziaris PM, et al. Effect of temporally patterned TNF-α delivery on in vitro osteogenic differentiation of mesenchymal stem cells cultured on biodegradable polymer scaffolds. J. Biomater. Sci. Polym. Ed. 2013;24:1794–1813. doi: 10.1080/09205063.2013.803455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Huang YC, Simmons C, Kaigler D, Rice KG, Mooney DJ. Bone regeneration in a rat cranial defect with delivery of PEI-condensed plasmid DNA encoding for bone morphogenetic protein-4 (BMP-4) Gene Ther. 2005;12:418–426. doi: 10.1038/sj.gt.3302439. [DOI] [PubMed] [Google Scholar]
- 201.Cao L, Mooney DJ. Spatiotemporal control over growth factor signaling for therapeutic neovascularization. Adv. Drug Deliv. Rev. 2007;59:1340–1350. doi: 10.1016/j.addr.2007.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Silva EA, Mooney DJ. Spatiotemporal control of vascular endothelial growth factor delivery from injectable hydrogels enhances angiogenesis. J. Thromb. Haemost. 2007;5:590–598. doi: 10.1111/j.1538-7836.2007.02386.x. [DOI] [PubMed] [Google Scholar]
- 203.Brunger JM, et al. Scaffold-mediated lentiviral transduction for functional tissue engineering of cartilage. Proc. Natl Acad. Sci. USA. 2014;111:E798–806. doi: 10.1073/pnas.1321744111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Ravichandran R, Sundarrajan S, Venugopal JR, Mukherjee S, Ramakrishna S. Advances in polymeric systems for tissue engineering and biomedical applications. Macromol. Biosci. 2012;12:286–311. doi: 10.1002/mabi.201100325. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.