Abstract
Bacterial IgA1 proteases may sabotage the protective effects of IgA. In vitro, both exogenous and endogenously-produced IgA1 protease inhibited phagocytic killing of Streptococcus pneumoniae by capsule-specific IgA1 human monoclonal antibodies (hMAb's), but not IgA2. These IgA1 proteases cleaved and reduced binding of the the effector Fcα1 heavy chain but not the antigen-binding F(ab)/light chain to pneumococcal surfaces. In vivo, IgA1 protease-resistant IgA2, but not IgA1 protease-sensitive IgA1, supported 60% survival in mice infected with wild-type S. pneumoniae. IgA1 hMAb's protected mice against IgA1 protease-deficient, but not -producing pneumococci. Parallel mouse sera with human IgA2 showed more efficient complement-mediated reductions in pneumococci with neutrophils than did IgA1, particularly with protease-producing organisms. After natural human pneumococcal bacteremia, purified serum IgG inhibited IgA1 protease activity in 7 of 11 patients (64%). These observations provide the first evidence in vivo that IgA1 protease can circumvent killing of S. pneumoniae by human IgA. Acquisition of IgA1 protease-neutralizing IgG after infection directs attention to IgA1 protease both as a determinant of successful colonization and infection and as a potential vaccine candidate.
Keywords: Streptococcus pneumoniae, Immunoglobulin A, IgA1 protease, mucosal immunity
Introduction
Although Streptococcus pneumoniae infections begin as asymptomatic nasopharyngeal colonization, this organism is the most common bacterial cause of community-acquired pneumonia (≈20-30% of cases), purulent otitis media (10-25%) and sinusitis 1-4. As an invasive pathogen, the pneumococcus is the leading cause of bacteremic pneumonia (≈65%) and bacterial meningitis (>30%)5, with ≥ 20,000 deaths/year in the U.S. 6 and up to a million deaths worldwide7. The functional interplay between bacterial virulence factors and host immune responses likely determines whether S. pneumoniae causes asymptomatic colonization, isolated mucosal infection, or invasive disease.
In both blood and the upper respiratory tract, IgA1 comprises ≈90% of total IgA, whereas IgA2 accounts for only ≈10% 8,9. Human IgA1 is cleaved by highly host species-specific proteases produced by S. pneumoniae and several other invasive mucosal pathogens (e.g., Neisseria species and Haemophilus influenzae). Cleavage results in dissociation of the effector function of the Fc fragment of bound IgA1 from its antigen-binding Fab fragments 10-14, a process shown to promote adherence of S. pneumoniae to respiratory epithelial cells in vitro 15. IgA1 protease had been proposed 16-19, and, more recently, shown in vitro to abrogate the protective effects of human IgA1 20, effects that include complement-dependent killing of the organism by phagocytes. However, because of the species- and subclass-specificity of the protease and the prior unavailability of purified IgA1 and IgA2 of comparable antigen-specificities and functional activity from humans 21-23, the contribution of IgA1 proteases to bacterial survival in vivo has not been demonstrated. Thus, we investigated the ability of IgA1 protease to modify killing of S. pneumoniae by using novel IgA1 and IgA2 human monoclonal antibodies (hMAb) specific for the pneumococcal capsule, isogenic wild-type and IgA1 protease-deficient organisms, and both in vitro and in vivo assay systems.
Results
IgA1-protease inhibits IgA-dependent killing of S. pneumoniae in vitro
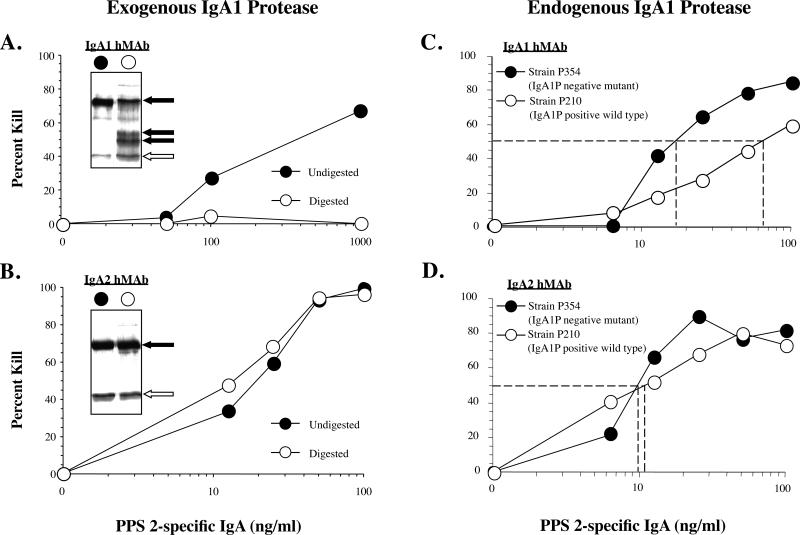
Pneumococcal capsule-specific hMAbs of the IgA1 and IgA2 subclasses can kill wild-type S. pneumoniae in vitro (reduce the number of bacterial colony forming units (CFU)) in the presence of complement and phagocytic cells20. We determined the ability of IgA1 protease, which cleaves the capsule-binding variable region of IgA1 from the phagocyte-binding constant region, to disrupt killing by these antibodies. Indeed, intact capsule-specific IgA1 hMAb supported dose-dependent killing of S. pneumoniae (Fig. 1A). However, pretreatment of the IgA1 hMAB with IgA1 protease (available in recombinant form from H. influenzae Rd) eliminated this IgA-mediated killing of S. pneumoniae (67 ±6% vs. 10 ±4% kill with and without IgA1 protease preincubation, respectively; p<.01). In contrast, the protease had no effect on killing supported by the capsule-specific IgA2 hMAb (Fig. 1B). IgA1 protease cleaved the heavy chain of IgA1, but not of IgA2, into lower molecular weight fragments (inserts; Fig. 1A and B, respectively), although a fraction of the heavy chain remained intact. The protease had comparable inhibitory effects on killing of type 8 organisms with a type 8-specific IgA1 hMAb (not shown). The killing resulted primarily from the opsonophagocytic activity of capsule-specific IgA and complement with neutrophils. However, a small proportion of the decrease in CFU's in the “killing” results (3-5% at 75 ng/mL IgA1, 11-15% at 225 ng/mL) can be ascribed to agglutination of the organisms by polymeric IgA alone rather than phagocytosis (20 and Supplemental Figure 1)
Figure 1. IgA1 protease inhibits killing of S. pneumoniae type 2 by human monoclonal antibodies (hMAb).
Type 2 capsule-specific human IgA1 (hMAb 2A02) (Fig. 1A) and IgA2 hMAb (MAb 2A01) (Fig. 1B) were incubated overnight with exogenous purified recombinant IgA1 protease from H. influenzae Rd (digested) or PBS (undigested). After protease was removed by binding the IgA1 protease 6x His tag on a nickel column, killing of S. pneumoniae type 2 (strain 6302; ATCC) with IgA1 or IgA2 hMAb was performed in the presence of 10% complement and human neutrophils (PMN: bacteria ratio 500:1), as described in Methods. Inserts. Cleavage of human IgA1 hMAb (Fig. 1A), but not IgA2 hMAb (Fig. 1B) by recombinant IgA1 protease (3 μg). Products resolved on the 12% reducing SDS-PAGE gel include intact heavy chain and cleavage fragments (black arrows) and light chain (light arrows). In Fig. 1C and D, pneumococcal killing experiments were performed to determine the effects of untreated IgA1 and IgA2 MAbs against IgA1-protease positive wild type S. pneumoniae (P210) and the isogenic IgA1 protease-negative mutant (P354). In these experiments, the bacteria themselves were the only source of IgA1 protease. Dotted lines in Figs. 1c and 1d represent the concentration of hMAbs required for 50% kill with complement and PMN's. Open circles (open circle; μ) represent IgA1 protease exposure (exogenous A and B, or endogenous C and D) and closed circles (closed circle; λ) represent no IgA1 protease exposure.
Consistent with the effects of preincubation of IgA1 with exogenous IgA1 protease, endogenous IgA1 protease produced directly by S. pneumoniae also inhibited such killing. Killing of protease-producing organisms required ≈5-fold more IgA1 hMAb than did killing of isogenic IgA1 protease-deficient mutants (for 50% kill, 70 ng/mL vs. 15 ng/mL, respectively) (Fig. 1C). In contrast, the IgA2 hMAb supported killing of both organisms with equal efficiency (Fig. 1D). After overnight incubation, supernatant fluid from the wild-type but not the protease-deficient S. pneumoniae cleaved the heavy chain of IgA1, but not IgA2 (not shown). Thus, IgA1 protease from H. influenzae, as applied exogenously, and from S. pneumoniae, produced endogenously, diminished the ability of human IgA1 to support killing of S. pneumoniae by phagocytes with complement.
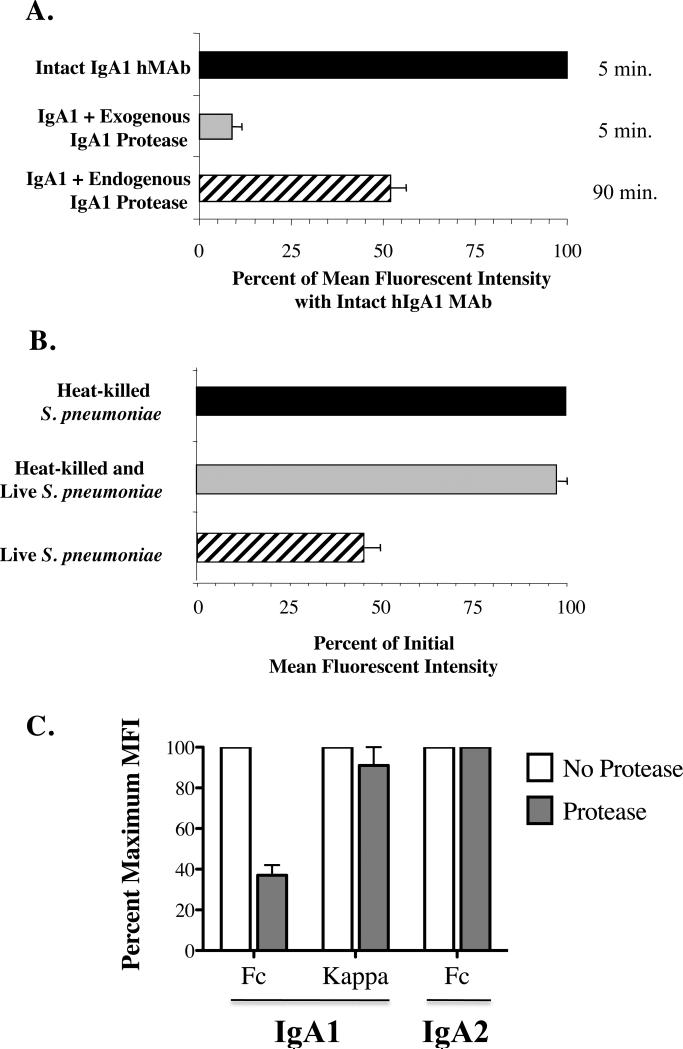
Binding of IgA to S. pneumoniae in vitro
We considered whether IgA1 protease inhibited binding of the heavy chain alone or the whole IgA1 antibody to the organism. Preincubation of capsule-specific IgA1 hMAb with exogenous recombinant IgA1 protease significantly reduced the amount of IgA1 heavy chain bound to S. pneumoniae to 9% of that with intact IgA1 as detected by IgA1-specific detector antibody (Fig. 2A). Similarly, exposure of the IgA1 hMAb to pneumococcal IgA1 protease produced endogenously over 90 minutes by the organism during incubation also decreased detectable bound IgA1 by 43%. However, cleavage of IgA1 by the protease did not affect binding of the light chain, and likely the F(ab) fragment to the organism (Figure 2C).
Figure 2. IgA1 protease reduces IgA1 Fcα bound to S. pneumoniae.
Detection of serotype-specific human IgA1 hMAb bound to serotype 2 organisms (P210). In Fig. 2A, organisms were exposed on ice for 30 minutes to intact hMAb (black and striped bars) or hMAb predigested with exogenous purified IgA1protease from H. influenzae Rd (gray bar), and washed. After 5 minutes at 37°C (black and gray bars) or 90 minute exposure of intact hMAb to endogenous protease produced by the S. pneumoniae organisms (striped bar), residual bound IgA1 was measured on washed bacteria stained with phycoerythrin-labeled mouse anti-human IgA1 by flow cytometry. Values for mean fluorescence intensity (MFI) ± standard deviation (SD) with intact MAb in 6 experiments are considered as 100%. P<.001 for exogenous and p<.02 for endogenous pneumococcal IgA1 protease compard with intact MAb. In Fig. 2B, 90 minute incubation of living wild-type S. pneumoniae (P210) resulted in loss of IgA1 (striped bar), but we observed no such loss of bound IgA1 from FITC-tagged dead organisms alone (black bar), or dead organisms which were washed, followed by addition of an equal number of unopsonized untagged wild-type live organisms (gray bar). The percent binding of IgA1 (Fcα), as determined by the MFI at 90 minutes, was determined by flow cytometry, as in 2A. Data are shown as the mean ±SD for 4 experiments. In Figure 2C, protease-deficient S. pneumoniae (strain P354) are incubated with intact or protease-treated IgA1 or IgA2 are incubated for 90 minutes, washed and surface Fca heavy chains and κ light chains are detectedy by flow cytometry. IgA1 protease decreases the amount of binding of IgA1 Fcα to S. pneumoniae (p=.007) but not the κ light chain binding, nor the Fcα which is resistant to the enzyme. Results are shown as mean of maximum binding (MFI) ±SD for 2 experiments.
We next considered whether the effects of the endogenously-produced protease on IgA1 were due to enzymatic activity expressed on the bacterial cell surface or released into solution. When specific monoclonal IgA1 was incubated with live wild-type S. pneumoniae for 90 minutes, less than half the IgA1 heavy chain was detected on the bacterial surface with the anti-IgA1 detector antibody compared with that bound to heat-killed organisms (Fig. 2B). However, incubation of IgA1 hMAb with heat-killed organisms caused no such decrement in bound antibody, suggesting that the protease is heat-labile or the activity required active production. Moreover, co-incubation of IgA1-opsonized heat-killed FITC-tagged organisms with an equal number of untagged and unopsonized live IgA1 protease-producing organisms over the same period also resulted in no decrement in IgA1 detection on the heat-killed bacterial surface. Thus, the proteolytic effects of IgA1 protease on capsule-specific IgA1 bound to bacteria appears to occur primarily on IgA1 bound to the cell surface of living bacteria and are not due to effects of release of the enzyme into the fluid-phase of the culture medium{Weiser, 2003 #7580}. Consistent with this observation, IgA1 protease is anchored to the cell surface and not actively secreted24.
However, IgA1 bound to S. pneumoniae can be cleaved by soluble IgA1 protease added to the media so bound antibody is not protected from cleavage by exogenous enzyme (data not shown). Whether live organisms can produce enough (and release) sufficient IgA1 protease to cleave the antibody on neighboring organisms in vivo has not been proven to date.
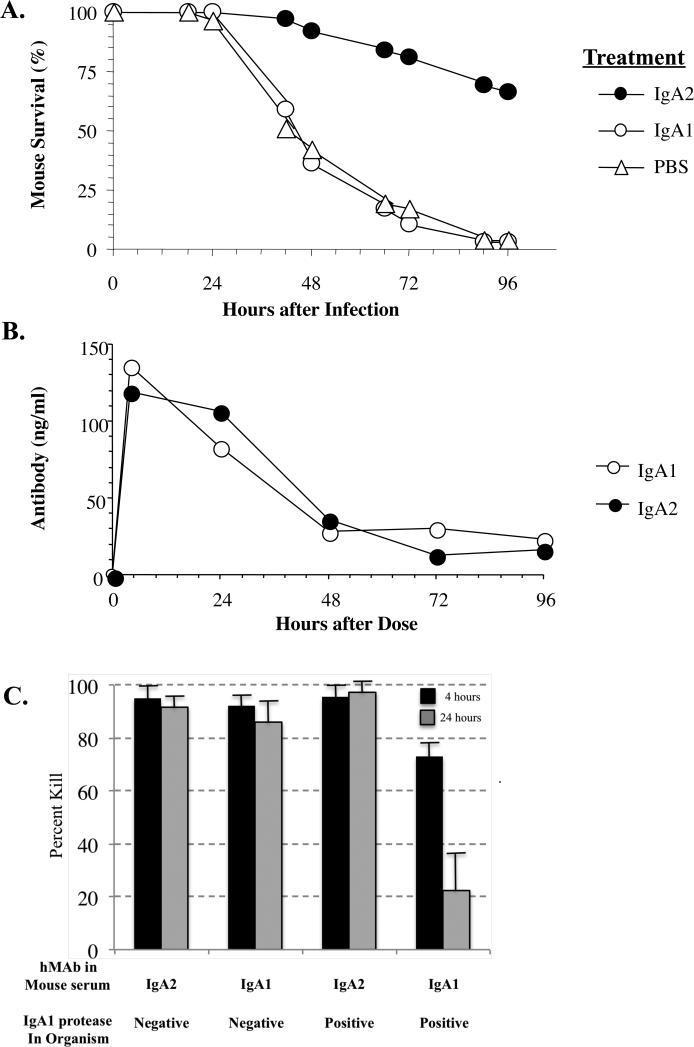
IgA1 protease eliminates IgA1-mediated protection against S. pneumoniae in vivo
We compared the ability of the two capsule-specific hMAbs, each of which supported killing of S. pneumoniae in vitro, to provide passive protection against fatal infection in vivo. After intraperitoneal administration of the protease-resistant IgA2 hMAb, 81% of mice given intranasal challenge of wild type S. pneumoniae survived at 72 hours compared with 10% of those pretreated with IgA1 hMAb or 17% of those given PBS control (P<.0001; Fig. 3A). However, levels of the two hMAbs achieved in mouse sera after passive immunization were comparable over time (Fig. 3B). No human IgA was detected in the nares. These IgA subclass-related differences in survival were associated with differences in the ability of sera from mice passively immunized with IgA1 and IgA2 hMAbs to support complement-dependent killing by phagocytes in vitro (Fig. 3C). The IgA1 hMAb in mouse sera from the earliest time point (4 hours), which contained the highest hMAb level, killed the IgA1 protease-producing wild type organism effectively (right column pair; black bar). However, this activity declined over time as antibody levels declined (right column pair; grey bar). In contrast, these same sera consistently supported killing of an isogenic IgA1 protease-deficient mutant at both time points examined (second column pair). With the protease-resistant IgA2 hMAb, killing of both organisms was comparable at each time and antibody concentration (first and third column pairs). In addition, a serotype-specific IgG1 MAb also showed similar killing of both wild type and mutant organisms (not shown). The heat-inactivated mouse serum had no activity against the organisms. Thus, the pneumococcal protease appears to specifically target human IgA1 and not other aspects of phagocyte-dependent killing.
Figure 3. Protection of mice against fatal infection with serotype 2 wild-type S. pneumoniae by human IgA monoclonal antibodies.
In Fig. 3A, survival of mice pre-treated intraperitoneally with 2 μg human IgA1 (open circle; μ) (n=36 mice), IgA2 (closed circle; λ)(n=37) hMAb or buffer (Δ) (n=53) 4 hours prior to intranasal challenge with wild type S. pneumoniae (P210) (P<.00001 for IgA2 vs. both other groups). In Fig. 3B, we measured changes in the concentrations of specific IgA1 and IgA2 hMAb in pooled mouse serum by ELISA in control mice (4 per group) over time after passive immunization. In Fig. 3C, we tested the ability of sera containing IgA1 or IgA2 hMAb from these animals obtained over time at 4 and 24 hours to support killing by human neutrophils of IgA1-producing wild-type S. pneumoniae (positive; strain P210) or its isogenic IgA1 protease-deficient mutant (negative; strain P354) in the presence of 10% baby rabbit complement (Fig. 3C). Data are shown as mean ±SD for 2 experiments using pooled sera from 4 mice at each time point with each condition.
Finally, we considered the possibility that differences in the activity of IgA1 and IgA2 hMAbs accounted for the differential protection afforded by the two hMAbs, rather than their susceptibility to cleavage by IgA1 protease or in the virulence of the organisms. Indeed, the IgA2 hMAb supported killing more efficiently than did the IgA1 hMAb in vitro (Fig. 1A and C). However, passive immunization of mice with the IgA1 hMAb was associated with 50% survival at 72 hours when the mice were infected with the protease-deficient mutant, but only 10% when infected with the isogenic protease-producing parent (P<.005; Fig. 4). Moreover, in the absence of antibody, the virulence of these isogenic organisms was not significantly different for the protease-deficient vs. wild-type strains, as reflected by the lethal dose50 (LD50: 3×106 CFU and 1×107 CFU, respectively) by Reed-Muench analysis25 with intranasal infection. Moreover, the in vitro growth curves of the two organisms were similar (not shown). Therefore, production of IgA1 protease by the organisms, and the susceptibility of the hMAbs to protease cleavage, was closely associated with the ability of the capsule-specific IgA antibodies to protect against this encapsulated pathogen in vitro and in vivo.
Figure 4. Effect of IgA1 protease on protection by hMAb IgA1.
Mice were passively immunized as described in the legend for Fig. 3, and challenged intranasally with IgA1 protease-producing wild type S. pneumoniae type 2 (Strain P210; n=15 mice) or its IgA1 protease-deficient mutant (Strain P354; n=15 mice).
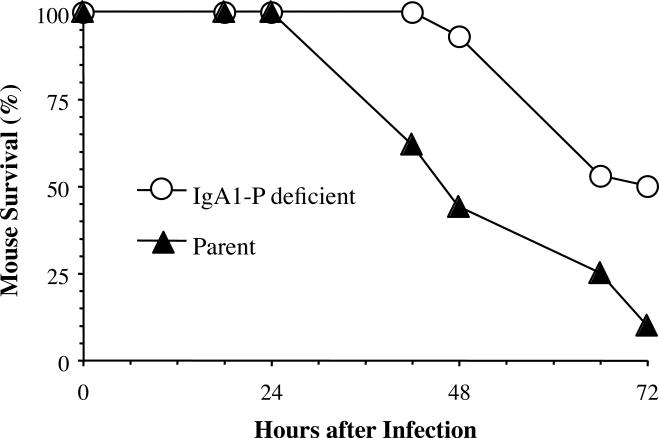
Human immune IgG inhibits IgA1 protease
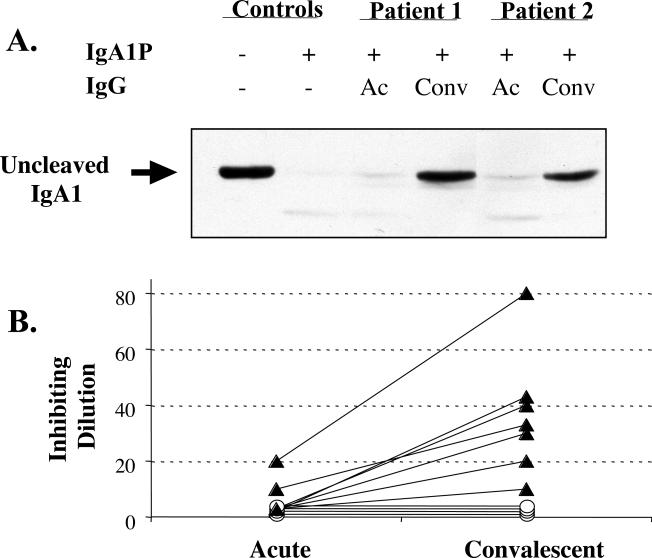
Preincubation of IgA1 with pneumococcal IgA1 protease substantially reduced detection of the hinge region with a hinge-specific murine monoclonal antibody by immunoblot (Fig. 5A; controls). Using this detection system for protease activity, purified IgG from convalescent sera from 2 representative patients obtained one month after resolution of pneumococcal bacteremia inhibited the protease activity, allowing detection of the hinge region. Acute sera from these patients showed no inhibition of protease activity so the hinge region was not detected.
Figure 5. Inhibition of IgA1 protease activity by human serum IgG.
In Fig. 5A, protection of the IgA1 heavy chain hinge region (arrow) from cleavage by IgA1 protease, was determined by immunoblotting with murine anti-human IgA1 MAb. Purified serum IgA was incubated without (−) or with (+) IgA1 protease (partially purified from lysed S. pneumoniae type 14) alone or in the presence of purified IgG from acute (Ac) and convalescent (Conv) sera from 2 patients with pneumococcal bacteremia drawn within 2 days of and 28 days after initial presentation to the hospital, respectively. In Fig. 5B, the reciprocal protease inhibitory titers of purified serum IgG from 11 adult patients with pneumococcal bacteremia include those from 7 patients whose titers rose (closed triangle; σ) in convalescent sera and 4 whose titers did not (open circle; μ).
Among 11 patients surviving bacteremic pneumococcal pneumonia and tested within 2-7 days of the onset of symptoms, two (18%) (both capsular serotype 14) had detectable IgA1 protease inhibiting activity in acute sera drawn within 3 days of admission (Figure 5B). In convalescent sera drawn 3-4 weeks after infection, 7 of 11 (64%) patients, including the 2 with detectable activity in acute sera, generated significantly increased titers of IgA1 protease-inhibiting IgG. Median titers of IgA1 protease-neutralizing activity rose from 1:3 to 1:20 in acute and convalescent sera, respectively. The serum IgG concentrations required for inhibition of IgA1 protease activity ranged from 1.2 - 10 μg/mL (total serum IgG levels were 8-12 mg/mL). Among these samples, neutralizing activity was largely independent of the serotype of the infecting organisms. Four of these patients were infected with serotype 14 S. pneumoniae isolated from blood during their acute bacteremia, and one each had types 1, 4 and 8. These data suggest neutralizing antibodies elicited during natural infection may inhibit the proteolytic activity of bacterial IgA1 proteases. The inability to generate neutralizing activity in 4 patients may have been related to antigenic differences between the proteases 26 or an inability of these patients to respond.
Discussion
By exploiting the functional activity of novel serotype-matched human IgA1 and IgA2 hMAbs, we show that IgA1 protease compromises the ability of the capsule-specific IgA1 to provide protection against S. pneumoniae both in vitro and in vivo. For decades, IgA1 proteases have been proposed to enhance the pathogenicity of invasive mucosal bacteria 16,17,27. Different bacterial species express functionally similar proteases that cleave the human IgA1 hinge region after a sequence of specific proline residues, but the proteases have completely different catalytic mechanisms 17. This apparent “convergent evolution” of the enzyme activity among the many different mucosal bacterial pathogens 17 suggests that the activity promotes bacterial survival. However, there has been no direct demonstration of the importance of bacterial IgA1 proteases in vivo because the native IgA of animals used for these experiments is not a substrate for the IgA proteases. Experimental human urethral infection was successful with an IgA1 protease mutant of Neisseria gonorrhoeae, but IgA1 is not the predominant IgA subclass at this site 28. In addition, the mechanism(s) by which the protease accomplishes a benefit to the bacteria in vivo had not been demonstrated.
The majority of bacteria producing IgA-cleaving proteases colonize the oral and upper respiratory mucosa where IgA1 predominates 29,30. Thus, IgA1 protease from S. pneumoniae may contribute to the bacteria's ability to colonize and invade by impairing the function of IgA1. Consistent with this hypothesis we have shown that pneumococcal capsule-specific IgA1 enhances, rather than inhibits, adherence of encapsulated S. pneumoniae to human respiratory epithelium in the presence of IgA1 protease 15.
Although such processes may contribute to colonization, the protease also may facilitate the development of clinical disease by other mechanisms. For example, levels of IgA1 protease activity from H. influenzae are increased in strains causing tissue injury and disease compared with those causing colonization alone 31. The assays we employed in this study, killing by neutrophils and animal protection by systemic antibody following mucosal challenge, may be more directly related to the ability of IgA to protect against disease rather than colonization. We showed that capsule-specific human MAbs of the protease-resistant IgA2 subclass are equal in supporting killing of wild type and protease-deficient mutant organisms, a result that suggests that pneumococcal IgA protease does not appear to impair the phagocytic function of the neutrophils themselves in these settings. In related studies, we also have not identified significant differences in the virulence for mice of isogenic wild-type or protease-deficient mutants of S. pneumoniae serotype 2 32. However, that IgA1 protease did influence survival of infected mice in other reports33-35 suggests that such differences may depend on the inoculum (less effect at higher inoculum), the bacterial serotype (types 4 and 19F vs. type 2), and the strain of mice (out bred MF1 and inbred BALB/c vs. out bred specific-pathogen free Swiss mice), the clinical model (pneumonia vs. bacteremia) and perhaps the specific molecular deletion, each of which differed from our studies. That mice do not produce IgA that is susceptible to IgA1 protease suggests that other functions for the protein in bacterial pathogenesis.
The reduction in killing activity by IgA1 following the cleavage of its heavy polypeptide chain by IgA protease is likely due to the known dissociation of the effector domains of the antibody, unlinking the Fcα CH2/3 fragments that are essential for binding to Fcα receptors (CD89) on neutrophils and alveolar macrophages from the bacterial-binding Fab domains 36-38. These Fcα CH2/3 domains have been associated with complement activity in both the polymeric and secretory forms of IgA 39,40. In addition, protease cleavage yields Fab domains that appear to continue to bind to antigens on the bacterial surface. However, the monomeric Fab binding would not foster the formation of aggregates that would support bacterial clearance that depends on the Fc region of the antibody 41. Although we have focused on killing and invasive infection, the protease may well also limit agglutination, enhance adherence15 and potentially killing at mucosal sites, activities currently under investigation.
Unlike the IgA1 proteases of Gram negative pathogenic microorganisms that are secreted into the medium, the protease produced by S. pneumoniae does not appear to be actively secreted but apparently reaches the medium only when cell lysis has taken place. The IgA1 protease of S. pneumoniae is predominantly bacterial cell surface-associated through an unusual sortase A- dependent, non-covalent mechanism of attachment 24 Our data confirm recent studies that the activity of the protease that is retained at the bacterial surface may have substantial impact on specific pneumococcal capsule-specific antibodies that are directly bound to the pathogen. In contrast, a protease secreted in free form into the medium may be expected to have a more generalized effect on IgA in the mucosal environment, thus facilitating IgA1 evasion by other microbes that are competing for the same niche 9,15,32.
We demonstrate that the activity of IgA1 protease can be inhibited by serum IgG antibodies arising during convalescence from invasive pneumococcal disease. This neutralization of proteolytic activity aligns with earlier observations that antibodies that bind 42 and block activity of the proteases of Neisseriae, H. influenzae, and other species 43-45 can be found in serum and secretions such as breast milk and nasal fluids. Romanello, et. al. showed that sera from patients with invasive pneumococcal disease recognized recombinant pneumococcal IgA protease proteins but these investigators did not report that these antibodies inhibited the enzyme activity 46. The impact of our results may be limited by the antigenic diversity of IgA1 proteases that has been found among clinical pneumococcal isolates, both between and within serotypes 26. Ongoing functional and sequencing data with these strains will determine whether the proteolytic regions and neutralizing domains are most well conserved 47. The immunologic consequences of protease heterogeneity can be determined with greater numbers of patients and a more thorough understanding of proteolytic motifs and inhibitory epitopes. Nevertheless, our results highlight the potential of IgA1 protease as a vaccine candidate that may limit colonization on mucosal surfaces served by secretory IgA1 antibodies and that may reduce the incidence of invasive disease and local mucosal infections caused by this important bacterial pathogen.
In summary, IgA1 proteases produced by S. pneumoniae, and other invasive mucosal pathogens, may enable the bacteria to evade killing by capsule-specific IgA by sabotaging the effector function of the specific humoral immune response. This proteolytic activity of the pneumococcal enzyme appears to be primarily cell-associated and directed to pathogen-specific IgA antibodies bound to the organism. However, this activity is only one element of the host-pathogen interaction in which the pathogen attempts to establish a niche in the context of robust host defense. Following colonization, S. pneumoniae can elicit a local and/or systemic IgA1 response to the bacterial surface 30,48. As demonstrated here, the pathogen produces IgA1 protease that limits the protective effects of this antibody. In turn, the host then generates a specific antibody response in blood (or mucosa) that neutralizes the proteolytic activity of the enzyme. The interplay between bacterial virulence factors and the host's successive ability to circumvent them likely determines the outcome of these common and often serious infections.
Methods
S. pneumoniae strains
Strains included wild type S. pneumoniae isolates of serotypes 2 (ATCC 6302) and 8 (ATCC 6308) (American Tissue Culture Collection; Mannassas, Virginia), and paired isogenic serotype 2 wild type and insertion-deletion IgA1 protease mutant organisms, which yielded a nonfunctional truncated IgA1 protease gene product (strains P210 and P354, respectively) 32.
IgA1 protease (IgAP)
We used recombinant IgA1 protease from an unencapsulated Haemophilus influenzae strain Rd mutant with a nickel-binding 6x His epitope replacement 44 (recombinant pneumococcal IgA1 protease not available), and partially purified pneumococcal IgA1 protease, derived by differential precipitation (30% and 60% ammonium sulfate) of supernatants of log-phase S. pneumoniae type 14 (ATCC 6314) in Todd-Hewitt broth 49. Enzymatic activity was confirmed using silver-stained denaturing polyacrylamide gel electrophoresis (12%) of IgA1 and IgA2 hMAb fragments before and after overnight incubation with IgA1 protease.
Human monoclonal antibodies (hMAb) to pneumococcal capsular polysaccharides (PPS)
hMAbs specific for S. pneumoniae serotypes 2 (IgA1 [2A02], IgA2 [2A01], IgG1 [2G01]) and serotype 8 (IgA1 [8A01]) were purified to >98.5% purity from B cells of recently immunized healthy adults that had been fused with the K6H6/B5 mouse-human heteromyeloma and cloned x3 by limiting dilution, as described 15,18,50,51. Consistent with results with capsule-specific IgA in serum, the majority of the Mab IgA is in the polymeric molecular form18,20,52.
In vitro killing assay
Log phase S. pneumoniae serotypes 2 (ATCC 6302, P210, P354) or 8 (ATCC 6308) were incubated with hMAbs for 30 or 120 minutes, then 1 hour with baby rabbit complement (10%) and human neutrophils (500:1, neutrophil:bacteria) with shaking 18. Colony-forming units (CFU) were determined from serial dilutions on blood agar plates. Percent kill was determined by: (1-[CFU in wells with MAb / CFU in wells without MAb]) x 100.
Murine protection model
In protocols approved by the animal research committee, after inhaled isoflurane anaesthesia, specific pathogen-free Swiss out bred mice in a pathogen-free barrier facility were inoculated intranasally with 2 × 107 log-phase CFU bacterial suspension (≈2x LD50) 4 hours after an intraperitoneal (i.p.) dose of human capsule-specific hMAbs (2 μg) or saline placebo. Survival was recorded every 8 hours until sacrifice at 72 hours 53.
IgA-bacterial binding assays
S. pneumoniae serotype 2 strains (ATCC 6302 and P210) were incubated 30 minutes with capsule-specific IgA1 hMAb that had or had not been digested overnight by recombinant IgA1 protease. Alternatively, an IgA1 protease-producing wild type strain (P210) was incubated with intact capsule-specific IgA1 hMAb for 30 minutes, washed and incubated for 90 minutes. Bacteria were stained with mouse anti-human IgA1-biotin (Southern Biotech Associates), followed by streptavidin (SA)-allophycocyanin (BD PharMingen, San Diego, California). The mean fluorescent intensities (MFI) of the bacteria, identified by forward and side scatter, were compared (FACSVantage cytometer; BectonDickenson; Mansfield, Massachusetts) using control antibodies matched for species, source, isotype, and fluorescent label, and compensation control beads. The mouse anti-IgA1 did not recognize bound IgG or any VH regions that might be shared by IgA and IgG antibodies nor it's associated κ or λ light chains (not shown).
To consider whether the cleavage of the IgA1 occurred on the bacterial surface or in the fluid phase, live unlabeled or dead fluorescein isothyocyanate (FITC)-tagged wild type S. pneumoniae type 2 were opsonized with specific IgA1 hMAb for 30 minutes at 37°C and washed. Three populations of bacteria (opsonized live, opsonized dead, or opsonized FITC-tagged dead+unopsonized live) were incubated for an additional 90 minutes and stained. Dead bacteria were segregated by gating on FITC+ events. MFI's for bound IgA1 were compared between groups.
Inhibition of IgA1 protease cleavage by human IgG
Sera were obtained with protocols approved by the relevant institutional review boards at admission to the Minneapolis Veterans Affairs Medical Center and from convalescent sera 3-4 weeks later from 11 adult patients with bacteremic pneumococcal pneumonia (blood stream infection) and symptoms for 2-7 days but without HIV-1 infection or obvious humoral immune defects. We purified IgG (purity >98%) from IgA-depleted acute sera exactly as described from our laboratory 18. Pneumococcal protease was preincubated with purified IgG dilutions (initial 20 μg IgG/mL) for 15 minutes at 37°C, then incubated with 2.5 μg of purified control serum IgA (>98% pure) for 2 hours. Inhibition of cleavage was determined by the percent loss of heavy chain by densitometry on reducing 10% SDS PAGE and by detection or loss of the IgA1 hinge with mouse anti-human IgA1-biotin by immunoblot.
Statistics
Survival of animals in treatment groups was compared using Cox regression analysis, and if statistically significant differences were found, survival curves were compared by log-rank test. Statistical comparisons were calculated using SPSS for Windows 6.1 (Chicago, Illinois).
Supplementary Material
Acknowledgements
All human and mouse studies were approved by the Human and Animal Subjects Subcommittees, and written informed consent was obtained from patients. The authors thank Ann Emery for secretarial support. This work was supported by the National Institutes of Health Grants AI-092468, AI-48796, AI-42240, HD-41361, AI092468 (ENJ), AI-38446 (JNW), DE15844, the Tufts Digestive Disease Research Center P30 DK34928 (AGP), the Mucosal and Vaccine Research Center at the University of Colorado School of Medicine, and the Department of Veterans Affairs Research Service.
Footnotes
The authors do not have a commercial or other association that might pose a conflict of interest.
References
- 1.Dagan R, Engelhard D, Piccard E. Epidemiology of invasive childhood pneumococcal infections in Israel: the Israeli Pediatric Bacteremia and Meningitis Group. JAMA. 1992;268:3328–3332. [PubMed] [Google Scholar]
- 2.Bruyn GAW, van der Meer JWM, Hermans J, Knoppert W. Pneumococcal bacteremia in adults over a 10-year period at University Hospital, Leiden. Rev Infect Dis. 1988;10:446–450. doi: 10.1093/clinids/10.2.446. [DOI] [PubMed] [Google Scholar]
- 3.Jetté LP, Lamothe F. Surveillance of invasive Streptococcus pneumoniae infection in Quebec, Canada, from 1984 to 1986: serotype distribution, antimicrobial susceptibility, and clinical characteristics. J Clin Microbiol. 1989;27:1–5. doi: 10.1128/jcm.27.1.1-5.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuikka A, Syrjanen J, Renkonen OV, Valtonen VV. Pneumococcal bacteraemia during a recent decade. J Infect. 1992;24:157–168. doi: 10.1016/0163-4453(92)92850-i. [DOI] [PubMed] [Google Scholar]
- 5.Thigpen MC, et al. Bacterial meningitis in the United States, 1998-2007. The New England journal of medicine. 2011;364:2016–2025. doi: 10.1056/NEJMoa1005384. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention Prevention of pneumococcal disease: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR. 1997;46:1–24. [PubMed] [Google Scholar]
- 7.O'Brien KL, et al. Burden of disease caused by Streptococcus pneumoniae in children younger than 5 years: global estimates. Lancet. 2009;374:893–902. doi: 10.1016/S0140-6736(09)61204-6. [DOI] [PubMed] [Google Scholar]
- 8.Brandtzaeg P. Regionalized immune function of tonsils and adenoids. Immunol Today. 1999;20:383–384. doi: 10.1016/s0167-5699(99)01498-x. [DOI] [PubMed] [Google Scholar]
- 9.Kirkeby L, Rasmussen TT, Reinholdt J, Kilian M. Immunoglobulins in nasal secretions of healthy humans: structural integrity of secretory immunoglobulin A1 (IgA1) and occurrence of neutralizing antibodies to IgA1 proteases of nasal bacteria. Clin Diagn Lab Immunol. 2000;7:31–39. doi: 10.1128/cdli.7.1.31-39.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Male CJ. Immunoglobulin A1 protease production by Haemophilus influenzae and Streptococcus pneumoniae. Infection and immunity. 1979;26:254–261. doi: 10.1128/iai.26.1.254-261.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kilian M, Mestecky J, Schrohenloher RE. Pathogenic species of the genus Haemophilus and Streptococcus pneumoniae produce immunoglobulin A1 protease. Infection and immunity. 1979;26:143–149. doi: 10.1128/iai.26.1.143-149.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kilian M, Mestecky J, Kulhavy R, Tomana M, Butler WT. IgA1 proteases from Haemophilus influenzae, Streptococcus pneumoniae, Neisseria meningitidis, and Streptococcus sanguis: comparative immunochemical studies. J Immunol. 1980;124:2596–2600. [PubMed] [Google Scholar]
- 13.Mulks MH, Plaut AG. IgA protease production as a characteristic distinguishing pathogenic from harmless neisseriaceae. The New England journal of medicine. 1978;299:973–976. doi: 10.1056/NEJM197811022991802. [DOI] [PubMed] [Google Scholar]
- 14.Plaut AG. The IgA1 proteases of pathogenic bacteria. Annu Rev Microbiol. 1983;37:603–622. doi: 10.1146/annurev.mi.37.100183.003131. [DOI] [PubMed] [Google Scholar]
- 15.Weiser JN, et al. Antibody-enhanced pneumococcal adherence requires IgA1 protease. Proc Natl Acad Sci U S A. 2003;100:4215–4220. doi: 10.1073/pnas.0637469100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kilian M, Reinholdt J, Lomholt H, Poulsen K, Frandsen EV. Biological significance of IgA1 proteases in bacterial colonization and pathogenesis: critical evaluation of experimental evidence. Apmis. 1996;104:321–338. doi: 10.1111/j.1699-0463.1996.tb00724.x. [DOI] [PubMed] [Google Scholar]
- 17.Kilian M, Mestecky J, Russell MW. Defense mechanisms involving Fc-dependent functions of immunoglobulin A and their subversion by bacterial immunoglobulin A proteases. Microbiol Rev. 1988;52:296–303. doi: 10.1128/mr.52.2.296-303.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Janoff EN, et al. Killing of Streptococcus pneumoniae by capsular polysaccharide-specific polymeric IgA, complement, and phagocytes. J Clin Invest. 1999;104:1139–1147. doi: 10.1172/JCI6310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Finn A, et al. Induction of functional secretory IgA responses in breast milk by pneumococcal capsular polysaccharides. The Journal of infectious diseases. 2002;186:1422–1429. doi: 10.1086/344356. [DOI] [PubMed] [Google Scholar]
- 20.Fasching CE, et al. Impact of the molecular form of IgA on its functional activity in defense against Streptococus pneumoniae. Infection and immunity. 2007;75:1801–1810. doi: 10.1128/IAI.01758-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Steinitz M, Tamir S, Ferne M, Goldfarb A. A protective human monoclonal IgA antibody produced in vitro: anti-pneumococcal antibody engendered by Epstein-Barr virus-immortalized cell line. Eur J Immunol. 1986;16:187–193. doi: 10.1002/eji.1830160214. [DOI] [PubMed] [Google Scholar]
- 22.Baxendale HE, et al. Immunogenetic analysis of the immune response to pneumococcal polysaccharide. Eur J Immunol. 2000;30:1214–1223. doi: 10.1002/(SICI)1521-4141(200004)30:4<1214::AID-IMMU1214>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 23.Zhong Z, Burns T, Chang Q, Carroll M, Pirofski L. Molecular and functional characteristics of a protective human monoclonal antibody to serotype 8 Streptococcus pneumoniae capsular polysaccharide. Infection and immunity. 1999;67:4119–4127. doi: 10.1128/iai.67.8.4119-4127.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bender MH, Weiser JN. The atypical amino-terminal LPNTG-containing domain of the pneumococcal human IgA1-specific protease is required for proper enzyme localization and function. Molecular microbiology. 2006;61:526–543. doi: 10.1111/j.1365-2958.2006.05256.x. [DOI] [PubMed] [Google Scholar]
- 25.Reed LJM, H. A simple method of estimating fifty percent endpoints. The American Journal of Hygiene. 1938;27:493–497. [Google Scholar]
- 26.Lomholt H. Evidence of recombination and an antigenically diverse immunoglobulin A1 protease among strains of Streptococcus pneumoniae. Infection and immunity. 1995;63:4238–4243. doi: 10.1128/iai.63.11.4238-4243.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Plaut AG, Gilbert JV, Artenstein MS, Capra JD. Neisseria gonorrhoeae and Neisseria meningitidis: extracellular enzyme cleaves human immunoglobulin A. Science. 1975;190:1103–1105. doi: 10.1126/science.810892. [DOI] [PubMed] [Google Scholar]
- 28.Johannsen DB, Johnston DM, Koymen HO, Cohen MS, Cannon JG. A Neisseria gonorrhoeae immunoglobulin A1 protease mutant is infectious in the human challenge model of urethral infection. Infection and immunity. 1999;67:3009–3013. doi: 10.1128/iai.67.6.3009-3013.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kilian M, Thomsen B, Petersen TE, Bleeg HS. Occurrence and nature of bacterial IgA proteases. Ann N Y Acad Sci. 1983;409:612–624. doi: 10.1111/j.1749-6632.1983.tb26903.x. [DOI] [PubMed] [Google Scholar]
- 30.Opstad NL, et al. Impact of Streptococcus pneumoniae bacteremia and human immunodeficiency virus type 1 on oral mucosal immunity. The Journal of infectious diseases. 1995;172:566–570. doi: 10.1093/infdis/172.2.566. [DOI] [PubMed] [Google Scholar]
- 31.Vitovski S, Dunkin KT, Howard AJ, Sayers JR. Nontypeable Haemophilus influenzae in carriage and disease: a difference in IgA1 protease activity levels. JAMA. 2002;287:1699–1705. doi: 10.1001/jama.287.13.1699. [DOI] [PubMed] [Google Scholar]
- 32.Wani JH, Gilbert JV, Plaut AG, Weiser JN. Identification, cloning, and sequencing of the immunoglobulin A1 protease gene of Streptococcus pneumoniae. Infection and immunity. 1996;64:3967–3974. doi: 10.1128/iai.64.10.3967-3974.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chiavolini D, Memmi G, Maggi T, Ianelli F, Pozzi G, Oggioni MR. The three extra-cellular zinc metalloproteinases of Streptococcus pneumoniae have a different impact on virulence in mice. BMC Microbiol. 2003;3:14. doi: 10.1186/1471-2180-3-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Polissi A, et al. Large-scale identification of virulence genes from Streptococcus pneumoniae. Infection and immunity. 1998;66:5620–5629. doi: 10.1128/iai.66.12.5620-5629.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oggioni MR, et al. Pneumococcal zinc metalloproteinase ZmpC cleaves human matrix metalloproteinase 9 and is a virulence factor in experimental pneumonia. Molecular microbiology. 2003;49:795–805. doi: 10.1046/j.1365-2958.2003.03596.x. [DOI] [PubMed] [Google Scholar]
- 36.Shen L, Lasser R, Fanger MW. My 43, a monoclonal antibody that reacts with human myeloid cells inhibits monocyte IgA binding and triggers function. J Immunol. 1989;143:4117–4122. [PubMed] [Google Scholar]
- 37.Monteiro RC, Kubagawa H, Cooper MD. Cellular distribution, regulation, and biochemical structure of an Fc alpha receptor in humans. J Exp Med. 1999;171:597–613. doi: 10.1084/jem.171.3.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Patry C, Sibille Y, Lehuen A, Monteiro RC. Identification of Fcα receptor (CD89) isoforms generated by alternative splicing that are differently expressed between blood monocytes and alveolar macrophages. J Immunol. 1996;156:4442–4448. [PubMed] [Google Scholar]
- 39.Nikolova EB, Tomana M, Russell MW. The role of the carbohydrate chains in complement (C3) fixation by solid-phase-bound human IgA. Immunology. 1994;82:321–327. [PMC free article] [PubMed] [Google Scholar]
- 40.van Egmond M, et al. IgA and the IgA Fc receptor. Trends Immunol. 2001;22:205–211. doi: 10.1016/s1471-4906(01)01873-7. [DOI] [PubMed] [Google Scholar]
- 41.Dalia AB, Weiser JN. Minimization of bacterial size allows for complement evasion and is overcome by the agglutinating effect of antibody. Cell Host Microbe. 2011;10:486–496. doi: 10.1016/j.chom.2011.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thiesen B, Greenwood B, Brieske N, Achtman M. Persistence of antibodies to meningococcal IgA1 protease versus decay of antibodies to group A polysaccharide and Opc protein. Vaccine. 1997;15:209–219. doi: 10.1016/s0264-410x(96)00138-7. [DOI] [PubMed] [Google Scholar]
- 43.Kobayashi K, Fujiyama Y, Hagiwara K, Kondoh H. Resistance of normal serum IgA and secretory IgA to bacterial IgA proteases: evidence for the presence of enzyme-neutralizing antibodies in both serum and secretory IgA, and also in serum IgG. Microbiol Immunol. 1987;31:1097–1106. doi: 10.1111/j.1348-0421.1987.tb01341.x. [DOI] [PubMed] [Google Scholar]
- 44.Plaut AG, Qiu J, Grundy F, Wright A. Growth of Haemophilus influenzae in human milk: synthesis, distribution, and activity of IgA protease as determined by study of iga+ and mutant iga- cells. The Journal of infectious diseases. 1992;166:43–52. doi: 10.1093/infdis/166.1.43. [DOI] [PubMed] [Google Scholar]
- 45.Devenyi AG, Plaut AG, Grundy FJ, Wright A. Post-infectious human serum antibodies inhibit IgA1 proteinases by interaction with the cleavage site specificity determinant. Mol Immunol. 1993;30:1243–1248. doi: 10.1016/0161-5890(93)90039-e. [DOI] [PubMed] [Google Scholar]
- 46.Romanello V, Marcacci M, Dal Molin F, Moschioni M, Censini S, Covacci A, Baritussio AG, Montecucco C, Tonello F. Cloning, expression, purification, and characterization of Streptococcus pneumoniae IgA1 protease. Protein Expr Purif. 2006;45:142–149. doi: 10.1016/j.pep.2005.07.015. [DOI] [PubMed] [Google Scholar]
- 47.Reinholdt J, Kilian M. Comparative analysis of immunoglobulin A1 protease activity among bacteria representing different genera, species, and strains. Infection and immunity. 1997;65:4452–4459. doi: 10.1128/iai.65.11.4452-4459.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Musher DM, et al. Emergence of antibody to capsular polysaccharides of Streptococcus pneumoniae during outbreaks of pneumonia: association with nasopharyngeal colonization. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 1997;24:441–446. doi: 10.1093/clinids/24.3.441. [DOI] [PubMed] [Google Scholar]
- 49.Blake MS, Swanson J. Studies on gonococcus infection. XVI. Purification of Neisseria gonorrhoeae immunoglobulin A1 protease. Infection and immunity. 1978;22:350–358. doi: 10.1128/iai.22.2.350-358.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Carroll WL, Thielemans K, Dilley J, Levy R. Mouse x human heterohybridomas as fusion partners with human B cell tumors. J Immunol Methods. 1986;89:61–72. doi: 10.1016/0022-1759(86)90032-3. [DOI] [PubMed] [Google Scholar]
- 51.Lefkovits I, Waldmann H. Limiting dilution analysis of the cell of immune system I. The clonal basis of immune response. Immunology Today. 1984;5:265–268. doi: 10.1016/0167-5699(84)90137-3. [DOI] [PubMed] [Google Scholar]
- 52.Johnson S, Opstad NL, Douglas JM, Jr., Janoff EN. Prolonged and preferential production of polymeric immunoglobulin A in response to Streptococcus pneumoniae capsular polysaccharides. Infection and immunity. 1996;64:4339–4344. doi: 10.1128/iai.64.10.4339-4344.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rubins JB, et al. Dual function of pneumolysin in the early pathogenesis of murine pneumococcal pneumonia. J Clin Invest. 1995;95:142–150. doi: 10.1172/JCI117631. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.