Abstract
Childhood obesity rates have risen dramatically over the past few decades. Although obesity has been linked to poorer neurocognitive functioning in adults, much less is known about this relationship in children and adolescents. Therefore, we conducted a systematic review to examine the relationship between obesity and obesity-related behaviors with neurocognitive functioning in youth. We reviewed articles from 1976 to 2013 using PsycInfo, PubMed, Medline and Google Scholar. Search terms included cognitive function, neurocognitive function/performance, executive function, impulsivity, self-regulation, effortful control, cognitive control, inhibition, delayed gratification, memory, attention, language, motor, visuo-spatial, academic achievement, obesity, overweight, body mass index, waist-hip ratio, adiposity and body fat. Articles were excluded if participants had health problems known to affect cognitive functioning, the study used imaging as the only outcome measure, they were non-peer-reviewed dissertations, theses, review papers, commentaries, or they were non-English articles. Sixty-seven studies met inclusion criteria for this review. Overall, we found data that support a negative relationship between obesity and various aspects of neurocognitive functioning, such as executive functioning, attention, visuo-spatial performance, and motor skill. The existing literature is mixed on the effects among obesity, general cognitive functioning, language, learning, memory, and academic achievement. Executive dysfunction is associated with obesity-related behaviors, such as increased intake, disinhibited eating, and less physical activity. Physical activity is positively linked with motor skill. More longitudinal research is needed to determine the directionality of such relationships, to point towards crucial intervention time periods in the development of children, and to inform effective treatment programs.
Keywords: neurocognition, cognitive functioning, pediatric obesity, treatment implications, obesity-related behaviors, children
INTRODUCTION
Obesity is an epidemic that affects individuals worldwide and is associated with negative health sequelae such as hypertension, diabetes, and certain cancers,1–3 and increasing health care costs.4 The prevalence of overweight and obesity in children in the United States is currently 31%.5 Specifically, the prevalence of obesity has increased from 13.7% of children and 11.5% of adolescents in the 1988–1994 period6 to 17.1% of children and adolescents by the year 2010.5 Moreover, research shows that children who are overweight are more likely to remain overweight as adults.7 These alarming statistics support the necessity for effective interventions to target obesity in children, and to look beyond basic nutrition and physical activity recommendations.
Family-based behavioral treatment (FBT) for childhood obesity typically results in weight loss in the participating child;8 however, data on the long-term outcomes and maintenance of these programs show that only one-third of participating children are a healthy weight in adulthood.9 Thus, two-thirds of children who participate in FBT do not respond as favorably. More research is needed to understand why certain children are successful in these programs and others are not, with the goal of helping to reduce the burden of obesity.
Neurocognitive functioning, which influences cognitions, emotions, and behaviors linked to obesity, may be an important, yet under-emphasized factor, in informing existing and future weight-loss interventions. While limited research has emerged examining differences in neurocognitive functioning between obese versus non-obese youth, only a few studies have explored how neurocognitive factors relate to behaviors that promote weight gain.10–12 It is possible that obesity-related behaviors, such as food intake and physical activity, may play a role in the relationship between neurocognitive functioning and weight (see Figure 1); however, no prior research has systematically examined this. Increasing our knowledge base of whether neurocognitive functioning is associated with obesity and obesity-related behaviors in children and adolescents could better inform treatment development, render more effective and tailored interventions, improve success in treatment, and reduce dropout rate in weight-loss interventions.13 In addition, intervening earlier in a child’s development may lead to greater success in reducing weight gain and preventing obesity later in adulthood.
Figure 1.
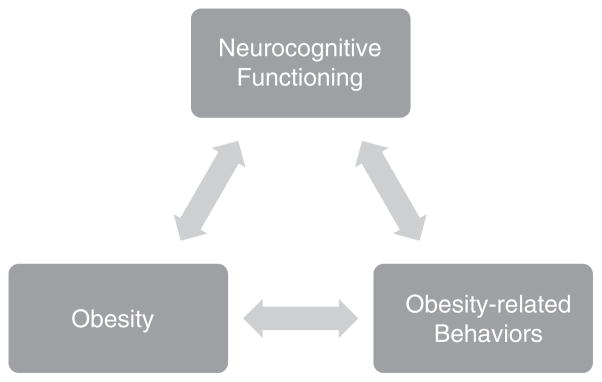
Neurocognitive model of obesity and obesity-related behaviors.
This review seeks to evaluate the state of the current evidence, to identify gaps in the literature, and to provide recommendations for future research and treatment development for overweight and obese youth. The specific goal of the current paper is to address the following question: Is there a relationship between various aspects of neurocognitive functioning, obesity, and obesity-related behaviors in youth (e.g., overeating, reduced physical activity, greater consumption of calorically dense foods)? We hypothesize that neurocognitive functioning will be negatively correlated with obesity and obesity-related behaviors in children and adolescents.
MATERIALS AND METHODS
Articles from 1976 to 2013 were reviewed (no studies meeting inclusion criteria prior to 1976 were found). Inclusion criteria were empirical research that examined the relationship between a) at least one measure of neurocognitive functioning and b) at least one measure of obesity or weight, or at least one measure of an obesity-related behavior. Measures of cognitive functioning were based on neuropsychological tests, self-report measures, or performance-based tasks.
Searches were performed on the following databases: PsycInfo, PubMed, Medline, EBSCO, and GoogleScholar. Studies with participants of all body mass index (BMI) levels and that included participants ages 18 and under were included. Search terms included cognitive function, neurocognitive function/performance, executive function, impulsivity, self-regulation, effortful control, cognitive control, inhibition, delayed gratification, memory, attention, language, motor, visuo-spatial, academic, obesity, overweight, BMI, waist-hip ratio, waist circumference (WC) adiposity, body fat, physical activity, sedentary activity, overeating, and fruit/vegetable intake. Articles that did not meet criteria were excluded for the following reasons: (1) The study had participants with health conditions that could influence their neurocognitive performance, for example, diabetes, hypertension, intellectual or developmental disability (mental retardation, Down’s syndrome), eating disorder. If a study included participants with and without these conditions, only results from participants without the conditions were reported. (2) The study used imaging as the only measure of neurocognitive functioning. If studies include both imaging results and neurocognitive tests, only results from neurocognitive tests were reported. Imaging studies were excluded because the significant difference in methodology between imaging studies and those using neuropsychological testing or self-report measures would make it difficult to compare and contrast the findings; it would be challenging to determine whether or not to attribute discrepancies in findings to differences in methodology. Furthermore, two recently published papers have already reviewed studies using brain imaging to assess brain functioning in relation to obesity in children and adults (see Bruce et al.14; Carnell et al.15). (3) Non-English articles, dissertations and theses, commentaries and review papers. The authors are English-speaking only, and due to the language barrier, we could only include articles in English. Out of the 158 identified articles, 67 met criteria for inclusion.
The presentation of the following literature is organized into two main parts: part I—neurocognitive functioning and obesity and Part II—neurocognitive functioning and obesity-related behaviors. In part I, we present the literature on obesity and different areas of neurocognitive functioning: general intellectual/cognitive functioning, executive functioning, memory, attention, language, visuo-spatial ability, motor skills and academic achievement. Although these areas of neurocognitive functioning have widely-varied definitions, we have operationalized the terms in Table 1. In part II, we present the literature on obesity-related behaviors and the areas of neurocognitive functioning where research is available, using the same definitions as stated in Table 1. A summary of the studies reviewed is presented in Table 2 (studies examining the relationship between obesity and neurocognitive functioning) and Table 3 (studies examining the relationship between obesity-related behaviors and neurocognitive functioning).
Table 1.
Operational definitions for subconstructs of neurocognitive functioning
| Area of neurocognitive functioning | Operationalized definition |
|---|---|
| General intellectual/cognitive functioning | General mental or intellectual ability and measured by tests that encompass a variety of different content areas, such as verbal, quantitative, spatial ability, processing speed and memory. |
| Executive functioning | A set of processes that involve mental control and self-regulation and controls and manages other cognitive processes. It encompasses functions such as planning, decision-making, problem-solving, regulation of one’s behaviors and emotions (for example, inhibition), abstraction, mental flexibility, set-shifting (the ability to switch between different tasks or mental sets) and delayed gratification. |
| Learning and memory | The acquisition, encoding, storage and retrieval of information (includes skills and knowledge). |
| Attention | Selection and concentration on certain aspects of the environment, in the context of competing stimuli. This cognitive process includes the ability to sustain concentration and inhibit attention to other stimuli. |
| Language | Verbal skills and abilities that include reading, spelling, pronunciation, grammar, rhythm of speech and fluency. |
| Visuo-spatial ability | Understanding visual information and their spatial relationships. This includes mental imagery (for example, mental rotation), visual perception and processing, navigation, depth perception and visual construction of objects in space. |
| Motor skill | A set of skills that involve coordination and sequencing of movements to achieve a particular goal. This area of functioning also includes balance, fine and gross motor movements, speed, strength, agility and manual dexterity. |
| Academic achievement | Performance based on standardized tests on reading, math or other subjects within a school or school-like setting. |
Table 2.
Studies examining the neurocognitive correlates of obesity in children and adolescents
| Authors | Population | N | Age range (mean, s.d.) | Areas of cognitive functioning assessed (measures) | Findings (abbreviated) |
|---|---|---|---|---|---|
| Barrigas and Fragoso67 | Children | 792 | 6–12 years | Assessment Tests; academic achievement on Portuguese, Math and Science; reasoning ability (Raven’s Colored Progressive Matrices Test) | ø: Academic achievement |
| Baxter et al.68 | Children | 1504 | 10 years | Academic achievement (standardized Tests in English, math, social studies and science) | ø: Academic achievement |
| Best et al.70 | Children, overweight | 241 | 7–12 years | Relative reinforcing value of food; impulsivity; delay discounting | (−): Relative reinforcing value of food, delay discounting of food |
| Bonato and Boland33 | Children, obese, and healthy weight | 40 | 8–11 years | Inhibition | ø: inhibition |
| Bonato and Boland40 | Children, obese, and healthy weight | 40 | 8–11 years | Delay of gratification | (−): Delay of gratification (edible incentives only) |
| Bonvin et al.62 | Children | 529 | 2–4 years (3.4, 0.6) | Motor skills (Zurich Neuromotor Assessment Test) | ø: Motor skills |
| Bourget and White31 | Children, overweight and healthy weight girls | 36 | 5–9 years (overweight 7.13; healthy weight 7.19) | Delay of gratification, inhibition | ø: Delay of gratification; (+): less effective inhibition strategies |
| Braet and Crombez47 | Children and adolescents | 74 | 9–16 years (obese 13.3, 2; controls 13.9, 2) | Interference (Stroop task, emotional Stroop); language (vocabulary subtest WISC-R) | (−): Lower reading skills; (−): interference (color of food words in Stroop); ø: language level |
| Bruce et al.102 | Children, obese, overweight, and healthy weight | 59 | 8–12 years (10.29, 1.39) | Delay of gratification | (−): Delay of gratification |
| Castelli et al.65 | Children, 3–5 grade public school students | 259 | (9.5, 0.74) | Academic achievement (ISAT) | (−): BMI and academic, mathematics, and reading achievement; (+): aerobic fitness and academic achievement |
| Cliff et al.52 | Children, overweight and healthy weight | 132 | 6–10 years (8.4, 1.0) | Motor skills (fundamental movement skill mastery) | (−): Motor skills |
| Cliff et al.53 | Children, overweight/obese and healthy weight | 153 | 6–10 years (8.3, 1.1) | Locomotor skills, object-control skills (Test of Gross Motor Development) | (−): Locomotor, object-control, gross motor development skills |
| Cserjesi et al.39 | Children, obese and healthy weight boys | 24 | obese (12.1, 0.9), healthy weight (12.44, 0.51) | Working memory (digit span on WAIS-III); Logical reasoning (Raven’s progressive matrix); Verbal flexibility and inhibition (semantic verbal fluency Test); Attention and visual scanning (D2 attention endurance Test); and Cognitive flexibility and set-shifting (WCST) | ø: Memory, logic reasoning, verbal fluency; (−): cognitive flexibility and shifting, attention endurance |
| Datar and Sturm66 | Children, kindergarten at T1, third grade at T2 | ~7000 | At T2 (3rd grade: 9.24, 0.34) | Math and reading assessment; teacher-reported behaviors (approaches to learning, self-control, attentiveness, task persistence, flexibility, organization, eagerness to learn, learning independence) | (−): Weight gain and reading/ mathematics (girls only); (−): weight gain over time and reading/ mathematics scores at baseline |
| Davis and Cooper18 | Children, overweight and obese | 170 | 7–11 years (9.3, 1.0) | Cognitive Assessment System, mathematics and reading (Woodcock-Johnson Tests of Achievement II, Broad Reading and Broad Mathematics clusters), parent-reported behaviors (Conner’s Parent Rating Scales-Revised), teacher-reported behaviors (Conner’s Teacher Ratings Scales-Revised) | (−): cognitive performance, attention, math/reading scores; (+): parent-reported cognitive problems/inattention, teacher-reported cognitive problems/ inattention |
| Delgado-Rico et al.35 | Adolescents, overweight | 42 | 12–17 (14.19, 1.38) | Impulsivity (UPPS-P); mental flexibility (letter-number sequencing); inhibition (Stroop); decision-making (Iowa Gambling Task) | (−): weight loss and impulsivity; (+): weight loss and inhibition |
| Delgado-Rico et al.36 | Adolescents, obese, overweight and healthy weight | 63 | 12–17 years | Impulsivity (UPPS-P); mental flexibility (Delis-Kaplan Executive Function System—Color Work Interference Test) | (+): Impulsivity; (−): mental flexibility |
| D’Hondt et al.60 | Children, obese, overweight, and healthy weight | 540 | 5–12.8 years (9.3, 1.6) | Fine motor skills (Movement Assessment Battery for Children) | (−): Fine motor skills |
| D’Hondt et al.58 | Children, overweight, obese, healthy weight | 117 | 5–10 years | Motor skills (Movement Assessment Battery for Children) | (−): Motor skills, balance, ball skills |
| D’Hondt et al.64 | Children, obese, overweight, and healthy weight | 72 | 7–13 years (10.5, 1.4) | Motor coordination (Körperkoordinations Test für Kinder; walking backwards, moving sideways, one-leg hopping, two-leg hopping) | (−): Motor coordination; (+): participation in treatment program and improvement in motor coordination |
| D’Hondt et al.63 | Children, overweight and healthy weight | 100 | 6–10 years | Motor coordination (Körperkoordinations Test für Kinder) | (−): Motor coordination (baseline and 2 years later); (−): motor coordination progress over time |
| Francis and Susman43 | Children | 1061 | 3, 5, 7, 9, 11, and 12 years | Delay of gratification and self-control | (−): Delay of gratification and self-control |
| Gale et al.19 | Children at T1, adults at T2 | 6147 (1958 cohort); 6445 (1970 cohort) | 11 years (1958 cohort time 1); 33 years (1958 cohort time 2); 10 years (1970 cohort time 1); 30 years (1970 cohort time 2) | 1958 Cohort had 40 verbal and 40 nonverbal items from National Foundation for Educational Research; 1970 cohort had a modifed version of the British Ability Scales, including word definitions, word similarities, recall digits and recall matrices | (−): Childhood cognitive ability and adult obesity; ø: childhood cognitive ability and childhood BMI; (−): childhood motor coordination and prevelance of obesity in adulthood |
| Gelleret al.46 | Children, obese and healthy weight | 48 | 3rd, 4th, and 5th graders | Delay of gratification paradigm | ø: Delay of gratification |
| Graziano et al.32 | Children, overweight and healthy weight | 57 | Assessments administered at age 2 and 5.5 | Self-regulation (laboratory tasks) | (−): Self-regulation (poorer self-regulation skills at age 2 related to increased risk of obesity at age 5.5) |
| Guerrieri et al.26 | Children, overweight and healthy weight | 78 | 8–10 years (9, 0.60) | Response inhibition (Stop-signal task); Reward sensitivity (Door opening task) | (−): Response inhibition; ø: reward sensitivity |
| Gunstad et al.21 | Children and adolescents, underweight, healthy weight, at risk of overweight and overweight | 478 | 6–19 years (12.45, 3.26) | Estimated intellectual functioning (Spot-the-Word task); Attention (Digit Span Backward); Executive functioning (switching of attention—letter/number); Memory (Verbal Recall), Language (Animal Fluency); and Motor (Finger Tapping) | ø: Cognitive Test performance |
| Holcke et al.24 | Children and adolescents, obese and one overweight | 30 | 8–15 years (12.0) | Motor skills, executive functions, perception, memory, language, learning, social skills and emotional/ behavioral problems (5–15 questionnaire) | (−): Executive function, motor skills, memory, learning, language |
| Jansen et al.51 | Children, overweight and healthy controls | 32 | 9–10 years (overweight–10, 0.89; controls–9.94, 0.68) | Perceptual reasoning (Colored Progressive Matrices Test); Motor skills (DKT; jumping, strength, endruance, flexibility), chronometric mental rotation Test | (−): Motor coordination, mental rotation performance |
| Kamijo et al.28 | Children | 126 | 7 and 9 years | Inhibitory control (Go NoGo Task); Achievement (WRAT-3) | (−): Inhibitory control, achievement |
| Kantomaa et al.59 | Children | 8061 | 8 and 16 years | Parent and child self-report of motor function | (−): Motor function |
| Krombholz22 | Children, overweight and healthy weight | 350 | Overweight (4.43, 0.8), healthy weight (4.43, 0.6) | Motor skills (Motor Test Battery); verbal ability (Peabody Picture Vocabulary Test); concentration (Frankfurter Test für Fünfjährige—Konzentration); and intelligence (Culture Fair Test) | (−): Motor skills; ø: manual dexterity, verbal ability, concentration, intelligence |
| Li et al.16 | Children and adolescents, healthy weight, at risk overweight, overweight | 2519 | 8–16 years (12.03) | Nonverbal reasoning and visuo- spatial construction (WISC-R) block design Test:); Attention and working memory (digit span); Reading and arithmetic (WRAT-R) | (−): Nonverbal reasoning/visuouspatial construction; (−): academic achievement and cognitive functioning |
| Lokken et al.29 | Adolescents, obese | 25 | 15–19 years (15.88, 1.69) | Academic achievement (WRAT-4); general intellectual functioning (WISC-IV); executive functioning (Computerized Cognitive Test Battery—digit span, continuous performance task, verbal interference, switching of attention, maze task, Go NoGo Task); | Obese adolescents had decreased performance, compared to normative data, on attention, mental flexibility, and disinhibition |
| London and Castrechini69 | Children and adolescents | 2735 | 4th to 7th grade, 6th to 9th grade | Academic achievement (California standardized Test in math and English language arts) | ø: Academic achievement Tests at baseline and over four year period |
| Lopes et al.61 | Children | 7175 | 6–14 years | Motor coordination (Kiphard-Schilling body coordination Test, Körperkoordination-Test-für-Kinder; balance, lateral jumping, hopping one leg, shifting platforms) | (−): Motor coordination (stronger in childhood than early adolescence) |
| Maayan et al.17 | Adolescents, obese and lean | 91 | 14–21 years (obese—17.5, 1.6; lean—17.3, 1.6) | Attention (Trail Making Test Part A); Cognitive Flexibility (Trail Making Test Part B); verbal fluency (COWAT), response inhibition (Stroop Task), Attention/Concentration Index (WRAML) and Working Memory Index (WRAML) | (−): Estimated full-scale IQ; (−): inhibition, cognitive flexibility, verbal fluency, attention and concentration, working memory |
| Mond et al.20 | Children | 9415 | 4–8 years (6.0, 0.37) | Memory and concentration, perserverance, abstraction, visual perception, arithmetic (Bavarian Model for school entry examination) | (−): Perseverance in females; (−): motor skills in males; ø: abstraction, visual perception, arithmetic, memory and concentration, speech |
| Morano et al.54 | Children | 80 | 4.5, 0.5 | Locomotor skills, object-control skills (Test of Gross Motor Development) | (−): Locomotor, object-control, gross motor development skills |
| Nederkoorn et al.13 | Children, healthy weight, obese | 63 | 12–15 years | Response perseveration (Door opening task); Inhibitory control (Stop-signal task); Impulsivity (BIS/ BAS scales). | (−): Response perseveration, inhibitory control, impulsivity; (+): weight loss in treatment and inhibitory control |
| Nederkoorn et al.34 | Children, obese | 26 | 8–12 years (9.3, 1.2) | Impulsivity and inhibition (Stop signal task) | (+): Impulsivity (even 12 months post-tx) |
| Nederkoorn et al.30 | Children | 89 | 7–9 years | Inhibition (Stop signal task) | (−) Inhibition (with food cues) |
| Okely et al.55 | Children and adolescents | 4363 | Grades 4, 6, 8, 10 | Motor skills (fundamental movement skills) | (−): Motor skills, advanced locomotor skills, object-control skills |
| Pauli-Pott et al.38 | Children and adolescents, overweight and obese | 111 | 7–15 years (11.1, 2.0) | Inhibitory control and attention (Go-NoGo, attention assessment battery Testbatterie zur Aufmerksamkeitsprufung) | (+): Weight loss and impulsivity (adolescents only) |
| Poulsen et al.57 | Children, overweight and healthy weight | 116 | overweight (8.75, 1.4), healthy weight (8.25, 1.5) | Motor performance (Bruninks-Oseretsky Test of Motor Performance-2 subtests: bilateral coordination, upper limb coordination, strength, balance, running speed, agility) | (−): Motor skills |
| Seeyave et al.44 | Children | 805 | 4 years T1, 11 years T2 | Delay of gratification (Mischel and Ebbesen’s delay of gratification waiting task) | (−): Delay of gratification |
| Sigal and Adler41 | Children (boys only, obese and healthy weight) | 64 | 8–13 years | Delay of gratification (laboratory paradigm) | (−): Delay of gratification |
| Soetens and Braet48 | Adolescents, overweight and healthy weight | 87 | 12–18 years; overweight (14.98, 1.51); healthy weight (14.74, 1.81) | Attention processing (Imbedded word task); free-recall (mazes from WISC-R) | (+): Recall of food words; ø: recall of control words: ø: attention interference effects for food |
| Staiano et al.25 | Adolescents, overweight and obese | 54 | 15–19 years (16.46) | Spatial skills, response inhibition, motor planning, viusal scanning, speed, and flexibility (design fluency and trail making subscales of Delis-Kaplan Executive Function System) | (+): Weight loss and executive function |
| van Egmond-Froehlich et al.49 | Children and adolescents, overweight and obese | 394 | 8–16 years (11.7, 2.0) | Inattention and hyperactivity/ impulsivity (parent report on the Strengths and Difficulties Questionnaire) | (−): Weight loss and inattention, impulsivity |
| Verbeken et al.23 | Children, healthy weight, overweight | 81 | 10–14 years | Verbal inhibition (Opposite worlds Test); Inhibition (Circle drawing task, Stop Task); Motivation inhibition (Door opening task); Delay aversion (Maudsley index of childhood delay aversion) | ø: Verbal inhibition, delay aversion; (+): inhibition circle drawing; (−): inhibition stop task, motivation inhibition |
| Verdejo-Garcia et al.27 | Adolescents, healthy weight, excessive weight | 61 | 13–16 years | Self-report questionnaires of impulsivity and sensitivity; Neuropsychological battery (intelligence, working memory, planning, reasoning, inhibition, set-shifting, self-regulation, decision-making)—see actual article for full list of tests. | ø: Impulsivity, sensitivity to reward/ punishment, working memory, planning; (−): inhibition, flexibility, decision-making, set-shifting |
| Zhu et al.56 | Children | 2029 | 9–10 years (healthy weight 9.42, 0.49; overweight 9.41, 0.49; obese 9.47, 0.50) | Motor coordination (MABC; manual dexterity, ball skills, balance) | (−): Balance; (−): total motor impairment (for girls, effect found only among obese subgroup) |
Abbreviations: BMI, Body mass index; BIS/BAS scales, Behavioral Inhibition System/Behavioral Activation System scales; COWAT, Controlled Oral Word Association Test; ISAT, Illinois Standards Achievement Test; MABC, Movement Assessment Battery for Children Test; WISC-R, Wechsler Intelligence Scale for Children—Revised; WAIS-III, Wechsler Abbreviated Intelligence Scale-III; WCST, Wisconsin Card Sort Test; WRAML, Wide Range Assessment of Learning and Memory; WRAT, Wide Range Achievement Test (R, Revised, 3, 3rd edition, 4, 4th edition). ø indicates null findings. (−) indicates inverse correlation between weight and area of cognitive functioning. (+) indicates positive correlation between weight and area of cognitive functioning.
Table 3.
Studies examining the neurocognitive correlates of obesity-related behaviors in children and adolescents
| Authors | Population | N | Age range (mean, s.d.) | Areas of cognitive functioning assessed (measures) | Findings (abbreviated) |
|---|---|---|---|---|---|
| Adsiz et al.74 | Children | 60 | 11–12 years | Attention (Bourdon Attention Test) | (+): Physical activity and attention |
| Best70 | Children | 33 | 6–10 years (8.1, 1.3) | Executive function (modified flanker task) | (+): Physical activity and executive function |
| Burgi et al.77 | Children | 217 | 4–6 years (5.2, 0.6) | Motor skills (agility obstacle course, balance beam) | ø: Physical activity and agility/ balance, accounting for body fat |
| Castelli et al.71 | Children | 59 | (8.79, .54) | Verbal and nonverbal intelligence (Kaufman Brief Intelligence Test); reading, spelling, arithmetic (Wide Range Achievement Test); interference (Stroop), Trail Making Tests | (+): Heart rate and high demand cognitive tasks |
| Davis et al.72 | Children | 171 | 7–11 years (9.3, 1.0) | Cognitive functioning (Cognitive Assessment System), academic achievement (Woodcock-Johnson Tests of Achievement III) | (+): Physical activity and planning; (+): high-level physical activity and math scores; ø: physical activity and attention, simultaneous processes, successive processes, math/reading achievement |
| Edwards et al.79 | Children | 800 | 11–13 years (11.76) | Measures of Academic Progress (MAP) standardized tests | (−): Television watching and math/ reading test scores; (+): physical activity and math/reading test scores; (+): physical performance and math test scores |
| Hartmann et al.37 | Children and adolescents | 90 | 10–14 years (LOC: 12.01, 1.28; Control: 12.11, 1.52) | Impulsivity (Barratt Impulsiveness Scale for Adolescents, German version) | ø: LOC eating and impulsivity |
| Hume et al.78 | Children | 248 | 9–12 years | Object-control skills, locomotor skills, fundamental movement skills | ø: Physical activity, weight, motor skills |
| Kantomaa et al.59 | Children | 8061 | 8 and 16 years | Parent and child self-report of motor function and physical activity | (+): Motor function and physical activity |
| Maayan et al.17 | Adolescents, obese and lean | 91 | 14–21 years (obese—17.5, 1.6; lean—17.3, 1.6) | Three Factor Eating Questionnaire; Attention (Trail Making Test Part A); Cognitive Flexibility (Trail Making Test Part B); verbal fluency (COWAT), response inhibition (Stroop Task), Attention/Concentration Index (WRAML) and Working Memory Index (WRAML) | (−): Disordered eating and inhibition |
| Morrison et al.75 | Children | 498 | 6–8 years | Motor performance (Koordinations Test für Kinder, throwing accuracy Test) | (+): Physical activity and motor skills; (−): greater body fat/lower physical activity and motor skills |
| Reilly et al.76 | Children | 545 | (4.2, 0.2) | Movement skills | (+): Physical activity and motor skills |
| Riggs et al.10 | Children (4th graders) | 184 | (9.38, 0.61) | Emotional control, inhibitory control, working memory, and organization of materials (Behavioral Rating Inventory of Executive Function, Self-Report) | (+): Current and future fruit/ vegetable intake and executive functioning; ø: current physical activity and executive functioning; (+): future physical activity and executive functioning; (−): snack intake and executive functioning; ø: future snack intake and executive functioning |
| Riggs et al.11 | Children (4th graders) | 997 | (9.26, 0.48) | Emotional control, inhibitory control, working memory, and organization of materials (Behavioral Rating Inventory of Executive Function, Self-Report) | (−): Sedentary behavior and executive functioning; (−): high-fat/high-sugar snack intake and executive functioning |
| Riggs et al.12 | Children (4th graders) | 1587 | 9.3 | Emotional control, inhibitory control, working memory, and organization of materials (Behavioral Rating Inventory of Executive Function, Self-Report) | (−): High-calorie snack food intake and executive functioning; (−): sedentary behavior and executive functioning; (+): fruit/vegetable intake and executive functioning; (+): physical activity and executive functioning |
| Tomporowski et al.73 | Children, overweight | 69 | 7–11 years (9.2, 1.2) | Switch Task | ø: Physical activity and task-switching performance |
Abbreviations: COWAT, Controlled Oral Word Association Test; LOC, loss of control; WRAML, Wide Range Assessment of Learning and Memory. ø indicates null findings. (−) indicates inverse correlation between obesity-related behavior and area of cognitive functioning. (+) indicates positive correlation between obesity-related behavior and area of cognitive functioning.
RESULTS
Part I: neurocognitive functioning and obesity
General intellectual/cognitive functioning
Four studies demonstrated a negative relationship between general cognitive functioning and weight. In cross-sectional studies comparing overweight or obese children and adolescents with healthy weight participants, global functioning, performance on tests of cognitive ability, and estimated full scale IQ were lower in overweight or obese youth than healthy weight youth.16,17 Within a sample of overweight, sedentary youth, BMI z-score, WC, percent body fat, visceral fat and abdominal fat were all negatively correlated with cognitive ability.18 In a longitudinal study, general cognitive ability (measuring verbal and nonverbal abilities) during childhood predicted a lower likelihood of obesity during adulthood.19
On the other hand, a few studies found no relationship between general cognitive ability and weight. Obese preschool children performed similarly to non-obese children on a test battery measuring cognitive development.20 Other studies have shown no relationship between BMI, intelligence and cognitive performance in children and adolescents.21,22
Executive functioning
General executive function
Overweight children have been found to have poorer executive control than healthy weight children,23 and obese children have twice the rate of executive dysfunction as the normative population.24 In an intervention for overweight and obese adolescents, improvements in executive function skill were related to weight loss,25 suggesting that executive function can improve and have positive implications for reducing weight.
Inhibition
Numerous studies supported a negative correlation between weight and inhibition, from preschool age to adolescence.17,23,26–28 Children who were the least effective in inhibiting responses on the Stop Task lost less weight in the treatment program.13 Obese adolescents (BMI >99%) had decreased performance on tests of attention compared with normative data.29 Overweight children had more difficulty with inhibition and displayed less effective inhibition strategies (for example, looking at and touching the reward) than healthy weight children, more so for food than non-food cues.30,31 Poor self-regulation skills (both behavioral and emotional) in toddlers at age two were predictive of increased risk for being overweight or obese at age five.32 Only one study failed to show a difference between obese and overweight children on response inhibition.33 It is possible that this 1983 study used a laboratory paradigm (a free-access to food task) to measure inhibition that was remarkably different from the more recent studies that used cognitive tasks (such as the Stop Task and Stroop Test) as measures of inhibition.
Impulsivity
Four studies supported a positive association between impulsivity and weight, whereas the rest of the studies found no relationship or an opposite effect. In treatment programs for weight loss, impulsivity was positively associated with being more overweight13 at baseline and losing less weight after treatment.34–36 Contrarily, no difference was found between overweight and healthy weight children and adolescents on impulsivity scores (based on self-report personality measures).27,37 An unexpected effect was also shown in a study with adolescents, such that higher impulsivity was associated with greater weight loss in a behavioral weight loss program.38 Of note, it is possible that the results from these studies varied by the type of measure used. These inconsistent findings may be related to the design of assessment measures (laboratory paradigms versus self-report personality measures), developmental age (children versus adolescents) or population characteristics (treatment versus non-treatment seeking).
Mental flexibility and set-shifting
Evidence supports an inverse association between overweight or obese status and performance on mental flexibility, set-shifting, and verbal fluency in children and adolescents.17,27,36,39 Obese adolescents had lower performance compared with normative data on tests of mental flexibility.29 However, one study found that BMI did not relate to set-shifting performance in children and adolescents,21 and no differences were found between obese and healthy weight boys on tests of verbal fluency.39
Planning, decision-making, delayed gratification, sensitivity to reward and reasoning
Obese children had more difficulty than healthy weight children with delay of gratification, both for food rewards,40 general rewards (both edible and non-edible),41 and non-food rewards.42 Upon examining the ability to delay gratification longitudinally, children who demonstrated low delay of gratification and low self-control at age 3 had significantly more rapid gains in BMI from age 3–12 compared with children who had high delay of gratification and self-control.43 Similarly, children who failed the ability to delay gratification task at age 4 were 1.3 times more likely to be overweight at age 11, although the strength of the relationship was diminished upon accounting for maternal weight.44 In the context of weight loss treatment, overweight children who showed a higher level of food reinforcement and greater delay discounting of food rewards lost less weight compared with children who did not.45 In comparison, two studies found that weight was unrelated to choices made during delay of gratification tasks for both food and non-food rewards.31,46 In addition, two studies showed no differences between healthy and overweight youth on tests of planning, reasoning, self-regulation and personality measures that assessed sensitivity to reward.27,39 Evidence from these studies suggests a weak association between obesity and planning, decision-making and reasoning. It is possible that these higher level executive functions are less well developed in children and adolescents in general (regardless of weight status), thus clarifying the lack of an association. However, further replication of these studies is needed.
Across this broad area of executive functioning, more consistent evidence regarding an inverse relationship between executive functioning and weight was found in the areas of general executive functioning, inhibition, delayed gratification, mental flexibility, and set-shifting. Mixed results were found with impulsivity and sensitivity to reward, whereas little evidence was found with planning, decision-making, and reasoning.
Attention
All but three studies demonstrated an inverse relationship between attention and obesity. Obese boys and adolescents performed lower on tests of attention and concentration than their healthy weight counterparts.17,39 Another study of obese adolescents demonstrated deficits in attention compared with normative data.29 One study found that among overweight children, there was attentional interference in regards to food words;47 however, a similar subsequent study found no differences between overweight and healthy weight children on attentional interference of food words.48 Children with greater percent body fat scored worse on a test of attention.18 Higher parent ratings of cognitive problems and inattention were reported among children with greater BMI z-scores, WC, and abdominal fat.18 Teacher-reported cognitive problems and inattention were positively correlated with WC.18 Greater inattention predicted less short- and long-term weight loss for children and adolescents in weight-loss treatment.49,50 On the contrary, Gunstad et al.21 found no relationship between BMI and digit span backward performance in children and adolescents, whereas Krombholz22 also found no relationship among weight and concentration ability in a sample of kindergarteners.
Learning and memory
Half of the studies on learning and memory in children found a significant relationship with obesity, whereas the other half did not. One study found that overweight children had selective processing of high caloric food cues, such that they recalled more food words than control words in a free-recall memory task, but recalled an equal number of control words compared with their healthy weight counterparts.48 Parents of obese Swedish children reported the presence of learning and memory problems at approximately three times the expected rate according to norms adjusted for both age and gender.24 Working memory was found to be worse in obese adolescents than healthy weight adolescents.17 However, various studies have reported no relationship between BMI, working memory, and verbal recall performance in children and adolescents.21,27,39
Language
Results from existing studies on language and obesity are mixed. Language problems were present in obese children in Sweden at approximately three times the rate of the normative population, based on parent report.24 Obese children were found to have lower reading skills compared with non-obese age and sex-matched controls.47 However, in some studies with young children and adolescents, there was no relationship among BMI, verbal fluency, and verbal ability.21,22 Also, Mond et al.20 found no differences between obese and non-obese 4-to-8 year-old children in different domains of speech (for example, pronunciation, grammar and rhythm of speech). Perhaps differences were not detected in these latter two studies owing to the younger age range of the samples, who may still be undergoing early stages of language development.
Visuo-spatial ability
The two studies available on obesity and visuo-spatial ability suggest an inverse correlation. In a group of children and adolescents with BMI greater than the fifth percentile, overweight or at-risk-of-overweight children performed worse than healthy weight children on a measure of nonverbal reasoning and visuo-spatial construction.16 Overweight children in Germany had impaired performances on mental rotation tasks compared with healthy weight children.51
Motor skill
Studies examining motor skill overwhelming support a connection with obesity. In cross-sectional studies, children and adolescents who were overweight or obese performed much lower on a fundamental movement skill mastery test, as well as in tasks involving coordination, balance, strength, running speed, agility, fine and gross motor skills, ball skills, locomotor skills, and object-control than non-overweight peers.20,22,51–60 Overweight and obese children performed significantly worse on motor coordination tasks than healthy weight children, with an increasing strength of association between 6 and 11 years of age, and a decreasing strength of relationship through 14 years of age.61 Parent-reported motor skill problems in obese children and adolescents in Sweden were five times the expected rate based on age and gender adjusted population norms.24 Contrary to the above findings, a few studies found no association between weight/BMI on performance tests of manual dexterity and finger tapping.21,22,62
A few studies provide longitudinal data describing the association between obesity and motor skill. In a 2-year longitudinal study, overweight and obese children had lower motor coordination at baseline and follow-up; strikingly, non-overweight children showed even greater increases in scores over time compared with overweight and obese children, indicating the impact of weight on motor coordination progression.63 A significant improvement in gross motor coordination was demonstrated in overweight and obese children after participating in a 4-month residential weight-loss treatment program, even though the overweight and obese children had poorer performance than healthy weight children at baseline.64 Better psychomotor coordination during childhood predicted a lower likelihood of obesity during adulthood.19 These studies suggest that although overweight and obese children have poorer motor skills at baseline, these skills can improve over time, with intervention, and subsequently lead to decreased likelihood of obesity later in life.
Academic achievement
Research that examined academic achievement in the context of weight generally substantiates an inverse relationship between obesity and academic achievement. In public school children, there was a negative correlation between BMI and total academic achievement, mathematics achievement, and reading achievement.65 BMI and fat mass were negatively correlated with WRAT-3 test scores.28 BMI z-score, WC, and body-fat measures were negatively correlated with math and reading scores among a sample that only included overweight children.18 Both boys and girls classified as ‘overweight’ or ‘always overweight’ had lower baseline reading and math test scores in kindergarten compared with their peers that were ‘never overweight’.66 Longitudinally, an increase from non-overweight to overweight status from kindergarten to third grade was associated with a decline in standardized reading and math test scores for girls only.66 However, there was no relationship between obesity and academic achievement in a group of 6–12 year-old Portuguese students, after accounting for socioeconomic status.67 One study with fourth grade, predominantly African American children found no relationship between BMI and scores on academic achievement tests.68 In addition, a large longitudinal study of fourth to ninth graders found that BMI was unrelated to academic achievement scores on math and language arts standardized state-wide tests over a 4-year period.69
Part II: neurocognitive functioning and obesity-related behaviors
Executive functioning
Several studies have found an association between poorer executive functioning and behaviors that promote weight gain. Lower self-reported executive cognitive function in fourth grade children was associated with high-calorie snack food consumption, consumption of high-fat and high-sugar snack foods and sedentary behavior.11,12 Executive cognitive function was positively correlated with fruit and vegetable intake and physical activity, and positively correlated with high-calorie snack food intake and sedentary behavior.10,12,70 Poorer inhibition was associated with greater disinhibited eating.17 Increases in intensive aerobic physical activity predicted improvements in inhibition, visual attention and processing speed, set-shifting and planning.71,72 Only one study did not observe a relationship between moderately intense physical activity and task-switching performance.73 It is conceivable that children and adolescents with deficits in executive functioning may be more likely to engage in obesity-related behaviors, although some aspects of executive functioning may have a weaker relationship with weight status.
Attention
Only one study has examined the link between attention and obesity-related behaviors. At the end of a 12-week volleyball and gymnastics intervention program, participating children had 83% higher attention levels than children who did not follow a physical activity program.74 The data from this single study suggest a positive relationship between attention and physical activity.
Motor skill
A variety of studies have described the link between obesity-related behaviors, specifically physical activity and motor skill. A study among Danish children found that physical activity was positively correlated with motor performance but not percent body fat.75 This study also found that children with higher percent body fat and low physical activity scored worse on motor performance than children with lower percent body fat and higher physical activity.75 Preschoolers randomized to a physical activity intervention program performed significantly better on movement skills tests than a control sample of kids not in the program at 6-month follow-up.76 Children who had poorer motor function at age 8 were more likely to have lower levels of physical activity at age 16.59 In examining only the subgroup of children designating as having a high percent body fat, motor performance was improved in children who reported greater physical activity compared with those that did not.75 However, after accounting for percent body fat, the relationship between physical activity and motor coordination diminished at baseline and 9 months later.77 Another study found no interaction among weight status, physical activity and fundamental movement skills.78 In general, the majority of these studies indicate a positive association between physical activity and motor skill.
Academic achievement
Higher math and reading test scores have also been associated with more vigorous physical activity and better physical activity performance.79 Children participating in a high physical activity exercise program scored higher on math achievement tests compared with children in a low physical activity program; however, this study did not find a difference in math scores among children engaged in physical activity and those who were not.72 Greater television viewing time (sedentary activity) was also related to lower math and reading test scores.79
To date, no studies have investigated the association between obesity-related behaviors and general cognitive functioning, learning and memory, language, and visuo-spatial ability.
DISCUSSION
Summary
Overall, obesity in youth is associated with poorer cognitive functioning as measured by neurocognitive tasks and self-report measures. This review showed that there is stronger and more consistent evidence supporting a relationship between obesity and deficits in the areas of executive functioning (22 out of 30 studies), attention (7 out of 10 studies), visuo-spatial skills (2 out of 2 studies), and motor skills (17 out of 20 studies). Findings were mixed in the areas of general cognitive functioning (4 out of 7 studies), learning and memory (3 out of 6 studies), language (2 out of 5 studies), and academic achievement (4 out of 7 studies). Obesity-related behaviors such as increased intake, disinhibited eating, sedentary activity, and lower physical activity are generally related to greater executive dysfunction, poorer motor skill, and lower academic achievement.
Although the pattern of findings overall indicates an inverse relationship between BMI and neurocognitive performance, several studies reported data that showed a lack of association. For example, across multiple areas of neurocognitive functioning Gunstad et al.21 found no relationship between cognitive performance and BMI in healthy children and adolescents. As suggested by the authors, this lack of association may be due to differences in study methodology, pathophysiological processes such as altered insulin regulation influencing cognitive functioning and the possibility that developmentally, aspects of cognitive functioning, such as self-regulation, may be more relevant to adults than children. Variations in results may also be related to the type of test administered (for example, self-report measures vs parent-report measures, questionnaires vs neuropsychology tests vs laboratory tasks), differences between studies on which possible confounding factors were controlled for (for example, physical activity, age, gender, ethnicity, health behaviors and comorbidity) and differences in the cut-off points for categorizing healthy weight, overweight or variations in the measures for obesity (for example, BMI vs adiposity vs waist-hip ratio). In addition, studies may not have used standard definitions or measures of impairment,20 limiting the validity and generalizability of the findings. Furthermore, only certain areas of executive functioning (for example, inhibition and delayed gratification) have stronger support for a relationship with overweight. Other areas (for example, decision-making and planning) were less consistently associated with overweight,27 suggesting that not all areas of executive functioning are related to weight through the same mechanisms. From a developmental perspective, differences in neurocognitive functioning may interact with the stages of brain development. For example, differences in some areas of executive functioning may not be detectable at a young age (for example, preschool or kindergarten age children) because the prefrontal cortex (PFC) is less well developed. Another possibility is that the relationship between weight/BMI and neurocognitive functioning is non-linear, or that a threshold exists at which a certain BMI percentile puts an individual at significantly higher risk of poorer neurocognitive functioning. These factors were not directly examined in the studies reviewed but could potentially explain the null findings.
The overall conclusion obtained from the review of the existing research is that although a general sense of the association between obesity and neurocognitive functioning has emerged, this field of research is still in its infancy. The current review provides a more in depth exploration of the role of neurobiology and neurocognitive functioning on childhood obesity and obesity-related behaviors; we expanded upon a previously published review paper on cognitive functioning and obesity across the lifespan (see Smith et al.80) and incorporated obesity-related behaviors. One limitation of this review is that we did not analyze the effect sizes of the associations. However, the large degree of variability between the different neuropsychological assessments for various areas of neurocognitive functioning would likely make it difficult to conduct a thorough meta-analysis. Another limitation is that only articles published in English were included, thus our findings did not include studies written in other languages. This review would have also been strengthened by the inclusion of imaging studies with children.
In some ways, this review revealed more questions than answers to the obesity-cognitive function relationship as there are still many gaps in the literature that need to be addressed. Although the majority of articles in this review fall under the executive functioning and motor skills category, literature is scarce in areas of general cognitive functioning, language, learning and memory, and visuo-spatial skills. Moreover, most of the studies involving obesity-related behaviors only examined the link with areas of executive functioning. It is important to look beyond BMI or weight as a correlate of neurocognitive functioning. For example, it was physical fitness, not BMI, which differentiated a large sample of students on academic achievement scores.69 More research is needed to examine whether there is a link between other aspects of neurocognitive abilities and behaviors that promote weight gain.
Below are suggested questions for future studies
Is there a causal relationship between neurocognitive functioning and obesity?
The majority of the studies were cross-sectional and only a few longitudinal studies with child and adolescent samples were available. Some show improvements in academic achievement, motor skills, and general cognitive functioning over time with weight loss.19,64 Participations in weight loss and physical activity programs have shown neurocognitive improvements in kids over time.13,38,64,65,72 Overweight children were found to improve less over time than non-overweight peers on motor skills.63 Other studies suggest that neurocognitive performance might have some predictive validity in future weight status. Children with lower delay of gratification ability at 4 years old were more likely to become overweight at 11 years.44 Higher childhood verbal and nonverbal IQ and psychomotor coordination were correlated with a decreased likelihood of obesity in adulthood, ~20 years later.19 Early onset obesity was associated with smaller cerebellar volumes compared with healthy sibling controls.81 Therefore, it is possible that early childhood obesity may affect and/or alter brain development. Although there is some evidence that supports both directions of the relationship, more prospective longitudinal studies and studies controlling for confounding variables (for example, age and medical conditions impacting cognitive functioning) are needed to describe the directionality of the relationship.
Does the relationship between neurocognitive functioning and obesity change depend on the age of the child, given that many executive functioning abilities are not fully developed pre adulthood?
It is important to examine this relationship in the context of development, given brain plasticity during childhood. For example, the strength of association between overweight/obesity and motor coordination skills was greater in children than adolescents, possibly emphasizing the role of development and neuroplasticity.61 Neurocognitive interventions may potentially be more effective during some developmental stages than others. For instance, interventions targeting improvement of motor and visuo-spatial skills may be best introduced during early childhood, given that motor and sensory areas of the brain tend to develop first.82,83 On the other hand, executive functioning training may be most effective during adolescence, when gray matter volume peaks, the PFC begins to develop and synaptic pruning begins.84,85 Even within certain developmental age groups, there could be great variation owing to children developing at different rates. More longitudinal research is needed to further examine whether the relationship between obesity and neurocognitive functioning changes across the lifespan.
How ‘food-specific’ should instruments be to best describe the relationship between obesity and neurocognitive functioning?
Compared with healthy weight children, obese children showed greater difficulty with delay of gratification and inhibition for food incentives or cues only.30,40 Overweight and obese children had less preference for non-food items, nutritious foods and non-food-related activities,40 and had more memory recall of food words than non-food words48 than healthy weight children. Yet, some research suggests that delay of gratification was not dependent on whether or not the reward was food-related.41,46 Few other studies have systematically compared performance on food-related tasks to non-food-related tasks. Thus, it would help for future studies to clarify whether obese individuals have general neurocognitive difficulties or whether the deficits are present specifically in the context of food.
What are the mediators and moderators of the relationship between neurocognitive functioning and obesity?
Some of the studies presented in this review have suggested age, gender, socioeconomic status and ethnicity as moderators. Findings from two studies suggested that socioeconomic status, not BMI, is associated with academic achievement.67,68 Among overweight children, those with a lower socioeconomic status had lower motor skill functioning than children with a higher socioeconomic status.22 Depression was a mediating factor between obesity and verbal mental flexibility and inhibition capacity.86 Impulsivity may be associated with attention deficit hyperactivity disorder, which may ultimately contribute to overeating or higher food intake and subsequently, obesity.26,87 Binge eating may also be another mediator between neurocognitive functioning and obesity in children.88
Obesity and neurocognitive functioning are also associated with many direct and indirect biological comorbidities. For example, metabolic syndrome and cardiovascular condition attenuated some correlations between neurocognitive functioning and obesity in adults.89 In obese subjects, serum-free fatty acid concentration had a positive relationship with white matter volume in the left temporal and occipital lobes. This suggests that fatty acid excess could have a negative influence on the metabolism of lipids in the brain that may then affect white matter volume.90 Obesity is often comorbid with cardiovascular disease, which has shown to impact cognitive functioning; waist-hip ratio and WC interacts with hypertension in their association with executive function, motor speed and manual dexterity later in life.91 Obesity has also been found to be associated with leptin resistance,92 metabolic syndrome,93 sleep apnea94 and inflammation related to insulin resistance.95 There is evidence that insulin exerts effects on neural networks,96 and that insulin-resistance may lead to alterations in cerebrovascular reactivity, potentially mediated by impaired vascular reactivity, inflammation, oxidative stress and/or other factors.97
Underlying brain mechanisms, such as poor executive control in regulating response to reward, can also influence weight gain and obesity.98,99 Imaging studies reflect differences between obese and non-obese children and adolescents in brain functioning. Compared with lean adolescents, obese adolescents are likely to have greater anticipation of food reward (in the gustatory cortex and somatosensory brain regions) but experience less actual reward, possibly owing to the decreased neural activation in the dorsal striatum (reward processing brain region), thus increasing the likelihood of overeating and weight gain.14,100 Studies have demonstrated that obese children display higher activation of dorsolateral PFC and occipital front cortex than healthy weight children in response to food images during both hunger and satiety, which is hypothesized to be associated with increased inhibitory activation in the obese group.14,101 Thus, obese children may require more effort or control to produce behavioral restraint when confronted with food cues.101 Obese children also failed to show significant post meal reduction of activation in the prefrontal, limbic and ventral striatum (reward processing) region.102 These studies may support an aberrant neurocircuitry across development among youth at risk for obesity as well as those who are currently obese.
Understanding the connection between neurobiology and obesity may be particularly important for children. It is possible that immature brain processes contribute to an increased risk for developing childhood obesity. During normal brain development, regions that serve primary functions, such as motor and sensory systems, mature earliest; higher-order association areas, which integrate these primary functions, mature later.83 The last area to develop is the PFC, which is vital to the inhibition of impulsive responses and to decision making based on environmental stimuli.85 The PFC receives input from a variety of sources in order to determine the value of a potential reward and to either mobilize the necessary behavioral action or inhibitory response.103 Decision making in children is affected by PFC and corresponding inhibitory control processes that are not yet fully developed.104 A growing body of literature suggests a changing balance between the earlier-developing limbic system and the later-developing frontal/cognitive systems.105 Without the necessary inhibitory processes to aid in decision-making, children and adolescents may be particularly susceptible to making poor health behavior choices, which may be particularly pronounced when evaluating food cues in an obesiogenic environment.106 The research on the link between neurobiological factors and obesity underscore the possibility that obese children may have more abnormalities in neurocognitive functioning. Such factors could potentially impact food intake and weight and may explain why neurocognitive deficits may be more common in children who are obese.
Thus, the type of food intake, physical activity, socio-demographics, health comorbidities and underlying brain mechanisms may mediate or moderate the relationship between neurocognitive functioning and obesity.
In conclusion, data generally show that obesity is negatively linked to various aspects of neurocognitive functioning, such as executive functioning, attention, visuo-spatial skills and motor skills. The existing literature is mixed on the effects among obesity and general cognitive functioning, learning and memory, language and academic achievement. Most of the literature suggests that greater executive dysfunction is associated with obesity-related behaviors, such as increased food intake, disinhibited eating and less physical activity.
The findings from the research presented could be beneficial in the design and implementation of treatments that target neurocognitive deficits that impact obesity and obesity-related behaviors. Progress in this area has been demonstrated in other areas of disorders. For example, in a study with children with attention deficit hyperactivity disorder, working memory training was shown to improve working memory and inhibition and reduce inattentiveness symptoms.107 A web-based smoking cessation program training contingency management for adolescents showed an increase in abstinence.108 Some evidence suggests that executive functioning training for obese children can improve working memory and inhibition and can help with weight-loss maintenance.109 In addition, programs and interventions focusing on increasing physical activity or decreasing weight may have an essential role. For example, evidence suggesting that participation in exercise programs may improve neurocognitive functioning is encouraging.71,72 Perhaps targeting physical fitness abilities in youth, alone or in combination with weight-loss, may have a beneficial impact on neurocognitive functioning. This research suggests that childhood and adolescence may represent an opportune time during development to influence neurocognitive abilities to augment the success of current weight-loss treatments.
It is likely that neurocognitive functioning may have multiple and indirect pathways that lead to obesity in youth. Although a general pattern has emerged between neurocognitive functioning and obesity from existing evidence, less is known about exactly how and why they are connected. Researchers have proposed conceptual frameworks that could more thoroughly describe the link between obesity and neurocognitive function, such as obesity having an acute effect on neurocognitive function; obesity influencing other chronic conditions which then limit neurocognitive function over time; a vulnerability of poor neurocognitive function that leads to greater risk of obesity; or that higher order neurophysiological processes impact both the development of obesity and neurocognitive dysfunction.21 It is not yet clear which of these frameworks, if any, best describes how neurocognitive function and obesity and obesity-related behaviors are associated in children and adolescents. Continuing research to further expand our understanding of these relationships may be an integral component to the development of more effective interventions to target pediatric obesity. Particularly for those children who have not been successful in losing weight or maintaining weight loss after current standard treatments, targeting neurocognitive impairments in future inventions may improve their chances of having current and long-term weight-loss success.
Acknowledgments
This work was supported by grants from the National Institute of Health (NIH DK094475 and NIH DK075861) to Kerri Boutelle (PI). We would like to acknowledge Amanda Bischoff-Grethe, PhD, (Assistant Adjunct Professor, Department of Psychiatry, University of California, San Diego) for her contributions to the literature review on neurobiology and obesity in children. We also thank the UCSD CHEAR (Center for Healthy Eating and Activity Research) lab for their support and feedback in the writing of this manuscript.
Footnotes
CONFLICT OF INTEREST
The authors declare no conflict of interest.
References
- 1.Vucenik I, Stains JP. Obesity and cancer risk: evidence, mechanisms, and recommendations. Ann N Y Acad Sci. 2012;1271:37–43. doi: 10.1111/j.1749-6632.2012.06750.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA. 1999;282:1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 3.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults. JAMA. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 4.Finkelstein EA, Linnan LA, Tate DF, Leese PJ. A longitudinal study on the relationship between weight loss, medical expenditures, and absenteeism among overweight employees in the WAY to Health study. J Occup Environ Med. 2009;51:1367–1373. doi: 10.1097/JOM.0b013e3181c2bb56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307:483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Troiano RP, Flegal KM. Overweight children and adolescents: description, epidemiology, and demographics. Pediatrics. 1998;101(3 Pt 2):497–504. [PubMed] [Google Scholar]
- 7.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 8.Epstein LH. Family-based behavioural intervention for obese children. Int J Obes Relat Metab Disord. 1996;20(Suppl 1):S14–S21. [PubMed] [Google Scholar]
- 9.Epstein LH, Valoski A, Wing RR, McCurley J. Ten-year outcomes of behavioral family-based treatment for childhood obesity. Health Psychol. 1994;13:373–383. doi: 10.1037//0278-6133.13.5.373. [DOI] [PubMed] [Google Scholar]
- 10.Riggs N, Chou CP, Spruijt-Metz D, Pentz MA. Executive cognitive function as a correlate and predictor of child food intake and physical activity. Child Neuropsychol. 2010;16:279–292. doi: 10.1080/09297041003601488. [DOI] [PubMed] [Google Scholar]
- 11.Riggs NR, Huh J, Chou CP, Spruijt-Metz D, Pentz MA. Executive function and latent classes of childhood obesity risk. J Behav Med. 2012;35:642–650. doi: 10.1007/s10865-011-9395-8. [DOI] [PubMed] [Google Scholar]
- 12.Riggs NR, Spruijt-Metz D, Chou CP, Pentz MA. Relationships between executive cognitive function and lifetime substance use and obesity-related behaviors in fourth grade youth. Child Neuropsychol. 2012;18:1–11. doi: 10.1080/09297049.2011.555759. [DOI] [PubMed] [Google Scholar]
- 13.Nederkoorn C, Braet C, Van Eijs Y, Tanghe A, Jansen A. Why obese children cannot resist food: the role of impulsivity. Eat Behav. 2006;7:315–322. doi: 10.1016/j.eatbeh.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 14.Bruce AS, Martin LE, Savage CR. Neural correlates of pediatric obesity. Prev Med. 2011;52(Suppl 1):S29–S35. doi: 10.1016/j.ypmed.2011.01.018. [DOI] [PubMed] [Google Scholar]
- 15.Carnell S, Gibson C, Benson L, Ochner CN, Geliebter A. Neuroimaging and obesity: current knowledge and future directions. Obes Rev. 2012;13:43–56. doi: 10.1111/j.1467-789X.2011.00927.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li YF, Dai Q, Jackson JC, Zhang J. Overweight is associated with decreased cognitive functioning among school-age children and adolescents. Obesity. 2008;16:1809–1815. doi: 10.1038/oby.2008.296. [DOI] [PubMed] [Google Scholar]
- 17.Maayan L, Hoogendoorn C, Sweat V, Convit A. Disinhibited eating in obese adolescents is associated with orbitofrontal volume reductions and executive dysfunction. Obesity (Silver Spring) 2011;19:1382–1387. doi: 10.1038/oby.2011.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davis CL, Cooper S. Fitness, fatness, cognition, behavior, and academic achievement among overweight children: Do cross-sectional associations correspond to exercise trial outcomes? Prev Med. 2011;52:S65–S69. doi: 10.1016/j.ypmed.2011.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gale CR, Batty GD, Cooper C, Deary IJ. Psychomotor coordination and intelligence in childhood and health in adulthood-testing the system integrity hypothesis. Psychosom Med. 2009;71:675–681. doi: 10.1097/PSY.0b013e3181a63b2e. [DOI] [PubMed] [Google Scholar]
- 20.Mond JM, Stich H, Hay PJ, Kraemer A, Baune BT. Associations between obesity and developmental functioning in pre-school children: a population-based study. Int J Obes (Lond) 2007;31:1068–1073. doi: 10.1038/sj.ijo.0803644. [DOI] [PubMed] [Google Scholar]
- 21.Gunstad J, Spitznagel MB, Paul RH, Cohen RA, Kohn M, Luyster FS, et al. Body mass index and neuropsychological function in healthy children and adolescents. Appetite. 2008;50:246–251. doi: 10.1016/j.appet.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 22.Krombholz H. The motor and cognitive development of overweight preschool children. Early Years. 2012;32:61–70. [Google Scholar]
- 23.Verbeken S, Braet C, Claus L, Nederkoorn C, Oosterlaan J. Childhood obesity and impulsivity: an investigation with performance-based measures. Behav Change. 2009;26:153–167. [Google Scholar]
- 24.Holcke M, Marcus C, Gillberg C, Fernell E. Paediatric obesity: a neurodevelopmental perspective. Acta Paediatr. 2008;97:819–821. doi: 10.1111/j.1651-2227.2008.00816.x. [DOI] [PubMed] [Google Scholar]
- 25.Staiano AE, Abraham AA, Calvert SL. Competitive versus cooperative exergame play for African American adolescents’ executive function skills: short-term effects in a long-term training intervention. Dev Psychol. 2012;48:337–342. doi: 10.1037/a0026938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guerrieri R, Nederkoorn C, Jansen A. The interaction between impulsivity and a varied food environment: its influence on food intake and overweight. Int J Obes (Lond) 2008;32:708–714. doi: 10.1038/sj.ijo.0803770. [DOI] [PubMed] [Google Scholar]
- 27.Verdejo-Garcia A, Perez-Exposito M, Schmidt-Rio-Valle J, Fernandez-Serrano MJ, Cruz F, Perez-Garcia M, et al. Selective alterations within executive functions in adolescents with excess weight. Obesity (Silver Spring) 2010;18:1572–1578. doi: 10.1038/oby.2009.475. [DOI] [PubMed] [Google Scholar]
- 28.Kamijo K, Khan NA, Pontifex MB, Scudder MR, Drollette ES, Raine LB, et al. The relation of adiposity to cognitive control and scholastic achievement in preadolescent children. Obesity (Silver Spring) 2012;20:2406–2411. doi: 10.1038/oby.2012.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lokken KL, Boeka AG, Austin HM, Gunstad J, Harmon CM. Evidence of executive dysfunction in extremely obese adolescents: a pilot study. Surg Obes Relat Dis. 2009;5:547–552. doi: 10.1016/j.soard.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 30.Nederkoorn C, Coelho JS, Guerrieri R, Houben K, Jansen A. Specificity of the failure to inhibit responses in overweight children. Appetite. 2012;59:409–413. doi: 10.1016/j.appet.2012.05.028. [DOI] [PubMed] [Google Scholar]
- 31.Bourget V, White DR. Performance of overweight and normal-weight girls on delay of gratification tasks. Int J Eating Disord. 1984;3:63–71. [Google Scholar]
- 32.Graziano PA, Calkins SD, Keane SP. Toddler self-regulation skills predict risk for pediatric obesity. Int J Obes (Lond) 2010;34:633–641. doi: 10.1038/ijo.2009.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bonato DP, Boland FJ. Response-inhibition deficits and obesity in children—a disconfirmation. Int J Eat Disorder. 1983;2:61–74. [Google Scholar]
- 34.Nederkoorn C, Jansen E, Mulkens S, Jansen A. Impulsivity predicts treatment outcome in obese children. Behav Res Ther. 2007;45:1071–1075. doi: 10.1016/j.brat.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 35.Delgado-Rico E, Rio-Valle JS, Albein-Urios N, Caracuel A, Gonzalez-Jimenez E, Piqueras MJ, et al. Effects of a multicomponent behavioral intervention on impulsivity and cognitive deficits in adolescents with excess weight. Behav Pharmacol. 2012;23:609–615. doi: 10.1097/FBP.0b013e328356c3ac. [DOI] [PubMed] [Google Scholar]
- 36.Delgado-Rico E, Rio-Valle JS, Gonzalez-Jimenez E, Campoy C, Verdejo-Garcia A. BMI predicts emotion-driven impulsivity and cognitive inflexibility in adolescents with excess weight. Obesity (Silver Spring) 2012;20:1604–1610. doi: 10.1038/oby.2012.47. [DOI] [PubMed] [Google Scholar]
- 37.Hartmann AS, Rief W, Hilbert A. Laboratory snack food intake, negative mood, and impulsivity in youth with ADHD symptoms and episodes of loss of control eating. Where is the missing link? Appetite. 2012;58:672–678. doi: 10.1016/j.appet.2012.01.006. [DOI] [PubMed] [Google Scholar]
- 38.Pauli-Pott U, Albayrak O, Hebebrand J, Pott W. Does inhibitory control capacity in overweight and obese children and adolescents predict success in a weight-reduction program? Eur Child Adolesc Psychiatry. 2010;19:135–141. doi: 10.1007/s00787-009-0049-0. [DOI] [PubMed] [Google Scholar]
- 39.Cserjesi R, Molnar D, Luminet O, Lenard L. Is there any relationship between obesity and mental flexibility in children? Appetite. 2007;49:675–678. doi: 10.1016/j.appet.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 40.Bonato DP, Boland FJ. Delay of gratification in obese children. Addict Behav. 1983;8:71–74. doi: 10.1016/0306-4603(83)90059-x. [DOI] [PubMed] [Google Scholar]
- 41.Sigal JJ, Adler L. Motivational effects of hunger on time estimation and delay of gratification in obese and nonobese boys. J Genetic Psychol. 1976;128:7–16. doi: 10.1080/00221325.1976.10533966. [DOI] [PubMed] [Google Scholar]
- 42.Bruce AS, Black WR, Bruce JM, Daldalian M, Martin LE, Davis AM. Ability to delay gratification and BMI in preadolescence. Obesity (Silver Spring) 2011;19:1101–1102. doi: 10.1038/oby.2010.297. [DOI] [PubMed] [Google Scholar]
- 43.Francis LA, Susman EJ. Self-regulation and rapid weight gain in children from age 3 to 12 years. Arch Pediatr Adolesc Med. 2009;163:297–302. doi: 10.1001/archpediatrics.2008.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Seeyave DM, Coleman S, Appugliese D, Corwyn RF, Bradley RH, Davidson NS, et al. Ability to delay gratification at age 4 years and risk of overweight at age 11 years. Arch Pediatr Adolesc Med. 2009;163:303–308. doi: 10.1001/archpediatrics.2009.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Best JR, Theim KR, Gredysa DM, Stein RI, Welch RR, Saelens BE, et al. Behavioral economic predictors of overweight children’s weight loss. J Consult Clin Psychol. 2012;80:1086–1096. doi: 10.1037/a0029827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Geller SE, Keane TM, Scheirer CJ. Delay of gratification, locus of control, and eating patterns in obese and nonobese children. Addict Behav. 1981;6:9–14. doi: 10.1016/s0306-4603(81)80002-0. [DOI] [PubMed] [Google Scholar]
- 47.Braet C, Crombez G. Cognitive interference due to food cues in childhood obesity. J Clin Child Adolesc. 2003;32:32–39. doi: 10.1207/S15374424JCCP3201_04. [DOI] [PubMed] [Google Scholar]
- 48.Soetens B, Braet C. Information processing of food cues in overweight and normal weight adolescents. Br J Health Psychol. 2007;12(Pt 2):285–304. doi: 10.1348/135910706X107604. [DOI] [PubMed] [Google Scholar]
- 49.van Egmond-Froehlich A, Bullinger M, Holl RW, Hoffmeister U, Mann R, Goldapp C, et al. The hyperactivity/inattention subscale of the strengths and difficulties questionnaire predicts short- and long-term weight loss in overweight children and adolescents treated as outpatients. Obesity facts. 2012;5:856–868. doi: 10.1159/000346138. [DOI] [PubMed] [Google Scholar]
- 50.van Egmond-Froehlich A, Claussnitzer G, Dammann D, Eckstein E, Brauer W, de Zwaan M. Parent reported inattention and hyperactivity/impulsivity as predictor of long-term weight loss after inpatient treatment in obese adolescents. Int J Eating Disord. 2013;46:39–46. doi: 10.1002/eat.22043. [DOI] [PubMed] [Google Scholar]
- 51.Jansen P, Schmelter A, Kasten L, Heil M. Impaired mental rotation performance in overweight children. Appetite. 2011;56:766–769. doi: 10.1016/j.appet.2011.02.021. [DOI] [PubMed] [Google Scholar]
- 52.Cliff DP, Okely AD, Magarey AM. Movement skill mastery in a clinical sample of overweight and obese children. Int J Pediatr Obes. 2011;6:473–475. doi: 10.3109/17477166.2011.575154. [DOI] [PubMed] [Google Scholar]
- 53.Cliff DP, Okely AD, Morgan PJ, Jones RA, Steele JR, Baur LA. Proficiency deficiency: mastery of fundamental movement skills and skill components in overweight and obese children. Obesity (Silver Spring) 2012;20:1024–1033. doi: 10.1038/oby.2011.241. [DOI] [PubMed] [Google Scholar]
- 54.Morano M, Colella D, Caroli M. Gross motor skill performance in a sample of overweight and non-overweight preschool children. Int J Pediatr Obes. 2011;6(Suppl 2):42–46. doi: 10.3109/17477166.2011.613665. [DOI] [PubMed] [Google Scholar]
- 55.Okely AD, Booth ML, Chey T. Relationships between body composition and fundamental movement skills among children and adolescents. Res Q Exerc Sport. 2004;75:238–247. doi: 10.1080/02701367.2004.10609157. [DOI] [PubMed] [Google Scholar]
- 56.Zhu YC, Wu SK, Cairney J. Obesity and motor coordination ability in Taiwanese children with and without developmental coordination disorder. Res Dev Disabil. 2011;32:801–807. doi: 10.1016/j.ridd.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 57.Poulsen AA, Desha L, Ziviani J, Griffiths L, Heaslop A, Khan A, et al. Fundamental movement skills and self-concept of children who are overweight. Int J Pediatr Obes. 2011;6:e464–e471. doi: 10.3109/17477166.2011.575143. [DOI] [PubMed] [Google Scholar]
- 58.D’Hondt E, Deforche B, De Bourdeaudhuij I, Lenoir M. Relationship between motor skill and body mass index in 5- to 10-year-old children. Adapt Phys Activ Q. 2009;26:21–37. doi: 10.1123/apaq.26.1.21. [DOI] [PubMed] [Google Scholar]
- 59.Kantomaa MT, Stamatakis E, Kankaanpaa A, Kaakinen M, Rodriguez A, Taanila A, et al. Physical activity and obesity mediate the association between childhood motor function and adolescents’ academic achievement. Proc Natl Acad Sci USA. 2013;110:1917–1922. doi: 10.1073/pnas.1214574110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.D’Hondt E, Deforche B, De Bourdeaudhuij I, Lenoir M. Childhood obesity affects fine motor skill performance under different postural constraints. Neurosci Lett. 2008;440:72–75. doi: 10.1016/j.neulet.2008.05.056. [DOI] [PubMed] [Google Scholar]
- 61.Lopes VP, Stodden DF, Bianchi MM, Maia JA, Rodrigues LP. Correlation between BMI and motor coordination in children. J Sci Med Sport. 2012;15:38–43. doi: 10.1016/j.jsams.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 62.Bonvin A, Barral J, Kakebeeke TH, Kriemler S, Longchamp A, Marques-Vidal P, et al. Weight status and gender-related differences in motor skills and in child care—based physical activity in young children. BMC Pediatr. 2012;12:23. doi: 10.1186/1471-2431-12-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.D’Hondt E, Deforche B, Gentier I, De Bourdeaudhuij I, Vaeyens R, Philippaerts R, et al. A longitudinal analysis of gross motor coordination in overweight and obese children versus normal-weight peers. Int J Obes (Lond) 2012;37:61–67. doi: 10.1038/ijo.2012.55. [DOI] [PubMed] [Google Scholar]
- 64.D’Hondt E, Gentier I, Deforche B, Tanghe A, De Bourdeaudhuij I, Lenoir M. Weight loss and improved gross motor coordination in children as a result of multidisciplinary residential obesity treatment. Obesity (Silver Spring) 2011;19:1999–2005. doi: 10.1038/oby.2011.150. [DOI] [PubMed] [Google Scholar]
- 65.Castelli DM, Hillman CH, Buck SM, Erwin HE. Physical fitness and academic achievement in third- and fifth-grade students. J Sport Exerc Psychol. 2007;29:239–252. doi: 10.1123/jsep.29.2.239. [DOI] [PubMed] [Google Scholar]
- 66.Datar A, Sturm R. Childhood overweight and elementary school outcomes. Int J Obes (Lond) 2006;30:1449–1460. doi: 10.1038/sj.ijo.0803311. [DOI] [PubMed] [Google Scholar]
- 67.Barrigas C, Fragoso I. Obesity, academic performance and reasoning ability in Portuguese students between 6 and 12 years old. J Biosoc Sci. 2012;44:165–179. doi: 10.1017/S0021932011000538. [DOI] [PubMed] [Google Scholar]
- 68.Baxter SD, Guinn CH, Tebbs JM, Royer JA. There is no relationship between academic achievement and body mass index among fourth-grade, predominantly African-American children. J Acad Nutr Diet. 2013;113:551–557. doi: 10.1016/j.jand.2013.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.London RA, Castrechini S. A longitudinal examination of the link between youth physical fitness and academic achievement. J Sch Health. 2011;81:400–408. doi: 10.1111/j.1746-1561.2011.00608.x. [DOI] [PubMed] [Google Scholar]
- 70.Best JR. Exergaming immediately enhances children’s executive function. Dev Psychol. 2012;48:1501–1510. doi: 10.1037/a0026648. [DOI] [PubMed] [Google Scholar]
- 71.Castelli DM, Hillman CH, Hirsch J, Hirsch A, Drollette E. FIT Kids: time in target heart zone and cognitive performance. Prev Med. 2011;52(Suppl 1):S55–S59. doi: 10.1016/j.ypmed.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 72.Davis CL, Tomporowski PD, McDowell JE, Austin BP, Miller PH, Yanasak NE, et al. Exercise improves executive function and achievement and alters brain activation in overweight children: a randomized, controlled trial. Health Psychol. 2011;30:91–98. doi: 10.1037/a0021766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tomporowski PD, Davis CL, Lambourne K, Gregoski M, Tkacz J. Task switching in overweight children: effects of acute exercise and age. J Sport Exerc Psychol. 2008;30:497–511. doi: 10.1123/jsep.30.5.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Adsiz E, Dorak F, Ozsaker M, Vurgun N. The influence of physical activity on attention in Turkish children. J Soc Dev New Net Environ B & H. 2012;6:1384–1389. [Google Scholar]
- 75.Morrison KM, Bugge A, El-Naaman B, Eisenmann JC, Froberg K, Pfeiffer KA, et al. Inter-relationships among physical activity, body fat, and motor performance in 6- to 8-year-old Danish children. Pediatr Exerc Sci. 2012;24:199–209. doi: 10.1123/pes.24.2.199. [DOI] [PubMed] [Google Scholar]
- 76.Reilly JJ, Kelly L, Montgomery C, Williamson A, Fisher A, McColl JH, et al. Physical activity to prevent obesity in young children: cluster randomised controlled trial. BMJ. 2006;333:1041. doi: 10.1136/bmj.38979.623773.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Burgi F, Meyer U, Granacher U, Schindler C, Marques-Vidal P, Kriemler S, et al. Relationship of physical activity with motor skills, aerobic fitness and body fat in preschool children: a cross-sectional and longitudinal study (Ballabeina) Int J Obes (Lond) 2011;35:937–944. doi: 10.1038/ijo.2011.54. [DOI] [PubMed] [Google Scholar]
- 78.Hume C, Okely A, Bagley S, Telford A, Booth M, Crawford D, et al. Does weight status influence associations between children’s fundamental movement skills and physical activity? Res Q Exerc Sport. 2008;79:158–165. doi: 10.1080/02701367.2008.10599479. [DOI] [PubMed] [Google Scholar]
- 79.Edwards JU, Mauch L, Winkelman MR. Relationship of nutrition and physical activity behaviors and fitness measures to academic performance for sixth graders in a midwest city school district. J School Health. 2011;81:65–73. doi: 10.1111/j.1746-1561.2010.00562.x. [DOI] [PubMed] [Google Scholar]
- 80.Smith E, Hay P, Campbell L, Trollor JN. A review of the association between obesity and cognitive function across the lifespan: implications for novel approaches to prevention and treatment. Obesity rev. 2011;12:740–755. doi: 10.1111/j.1467-789X.2011.00920.x. [DOI] [PubMed] [Google Scholar]
- 81.Miller JL, Couch J, Schwenk K, Long M, Towler S, Theriaque DW, et al. Early childhood obesity is associated with compromised cerebellar development. Dev Neuropsychol. 2009;34:272–283. doi: 10.1080/87565640802530961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sowell ER, Thompson PM, Toga AW. Mapping changes in the human cortex throughout the span of life. Neuroscientist. 2004;10:372–392. doi: 10.1177/1073858404263960. [DOI] [PubMed] [Google Scholar]
- 83.Gogtay N, Giedd JN, Lusk L, Hayashi KM, Greenstein D, Vaituzis AC, et al. Dynamic mapping of human cortical development during childhood through early adulthood. Proc Natl Acad Sci USA. 2004;101:8174–8179. doi: 10.1073/pnas.0402680101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Giedd JN. The teen brain: insights from neuroimaging. J Adolesc Health. 2008;42:335–343. doi: 10.1016/j.jadohealth.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 85.Giedd JN, Rapoport JL. Structural MRI of pediatric brain development: what have we learned and where are we going? Neuron. 2010;67:728–734. doi: 10.1016/j.neuron.2010.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cserjesi R, Luminet O, Poncelet AS, Lenard L. Altered executive function in obesity. Exploration of the role of affective states on cognitive abilities. Appetite. 2009;52:535–539. doi: 10.1016/j.appet.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 87.Dempsey A, Dyehouse J, Schafer J. The relationship between executive function, AD/HD, overeating, and obesity. West J Nurs Res. 2011;33:609–629. doi: 10.1177/0193945910382533. [DOI] [PubMed] [Google Scholar]
- 88.deZwaan M, Mitchell JE, Seim HC, Specker SM, Pyle RL, Raymond NC, et al. Eating related and general psychopathology in obese females with binge eating disorder. Int J Eating Disord. 1994;15:43–52. doi: 10.1002/1098-108x(199401)15:1<43::aid-eat2260150106>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 89.Dore GA, Elias MF, Robbins MA, Budge MM, Elias PK. Relation between central adiposity and cognitive function in the Maine-Syracuse Study: attenuation by physical activity. Annals Behav Med. 2008;35:341–350. doi: 10.1007/s12160-008-9038-7. [DOI] [PubMed] [Google Scholar]
- 90.Haltia LT, Viljanen A, Parkkola R, Kemppainen N, Rinne JO, Nuutila P, et al. Brain white matter expansion in human obesity and the recovering effect of dieting. J Clini Endocrinol Metab. 2007;92:3278–3284. doi: 10.1210/jc.2006-2495. [DOI] [PubMed] [Google Scholar]
- 91.Waldstein SR, Katzel LI. Stress-induced blood pressure reactivity and cognitive function. Neurology. 2005;64:1746–1749. doi: 10.1212/01.WNL.0000161851.01243.62. [DOI] [PubMed] [Google Scholar]
- 92.Munzberg H, Bjornholm M, Bates SH, Myers MG., Jr Leptin receptor action and mechanisms of leptin resistance. Cell Mol Life Sci. 2005;62:642–652. doi: 10.1007/s00018-004-4432-1. [DOI] [PubMed] [Google Scholar]
- 93.Grundy SM. Obesity, metabolic syndrome, and cardiovascular disease. J Clin Endocrinol Metab. 2004;89:2595–2600. doi: 10.1210/jc.2004-0372. [DOI] [PubMed] [Google Scholar]
- 94.Wolk R, Shamsuzzaman AS, Somers VK. Obesity, sleep apnea, and hypertension. Hypertension. 2003;42:1067–1074. doi: 10.1161/01.HYP.0000101686.98973.A3. [DOI] [PubMed] [Google Scholar]
- 95.Bastard JP. Insulin resistance and adipose tissue gene expression in humans. Ann Biol Clin-Paris. 2004;62:25–31. [PubMed] [Google Scholar]
- 96.Hallschmid M, Schultes B. Central nervous insulin resistance: a promising target in the treatment of metabolic and cognitive disorders? Diabetologia. 2009;52:2264–2269. doi: 10.1007/s00125-009-1501-x. [DOI] [PubMed] [Google Scholar]
- 97.Yates KF, Sweat V, Yau PL, Turchiano MM, Convit A. Impact of metabolic syndrome on cognition and brain: a selected review of the literature. Arterioscler Thromb Vasc Biol. 2012;32:2060–2067. doi: 10.1161/ATVBAHA.112.252759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Michaelides M, Thanos PK, Volkow ND, Wang GJ. Dopamine-related frontostriatal abnormalities in obesity and binge-eating disorder: emerging evidence for developmental psychopathology. Int Rev Psychiatry. 2012;24:211–218. doi: 10.3109/09540261.2012.679918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Volkow ND, Wang GJ, Baler RD. Reward, dopamine and the control of food intake: implications for obesity. Trends Cogn Sci. 2011;15:37–46. doi: 10.1016/j.tics.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Stice E, Spoor S, Bohon C, Veldhuizen MG, Small DM. Relation of reward from food intake and anticipated food intake to obesity: a functional magnetic resonance imaging study. J Abnorm Psychol. 2008;117:924–935. doi: 10.1037/a0013600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Davids S, Lauffer H, Thoms K, Jagdhuhn M, Hirschfeld H, Domin M, et al. Increased dorsolateral prefrontal cortex activation in obese children during observation of food stimuli. Int J Obes (Lond) 2010;34:94–104. doi: 10.1038/ijo.2009.193. [DOI] [PubMed] [Google Scholar]
- 102.Bruce AS, Holsen LM, Chambers RJ, Martin LE, Brooks WM, Zarcone JR, et al. Obese children show hyperactivation to food pictures in brain networks linked to motivation, reward and cognitive control. Int J Obes (Lond) 2010;34:1494–1500. doi: 10.1038/ijo.2010.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Tanji J, Hoshi E. Role of the lateral prefrontal cortex in executive behavioral control. Physiol Rev. 2008;88:37–57. doi: 10.1152/physrev.00014.2007. [DOI] [PubMed] [Google Scholar]
- 104.Menon V, Adleman NE, White CD, Glover GH, Reiss AL. Error-related brain activation during a Go/NoGo response inhibition task. Hum Brain Mapp. 2001;12:131–143. doi: 10.1002/1097-0193(200103)12:3<131::AID-HBM1010>3.0.CO;2-C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Casey BJ, Duhoux S, Malter Cohen M. Adolescence: what do transmission, transition, and translation have to do with it? Neuron. 2010;67:749–760. doi: 10.1016/j.neuron.2010.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Somerville LH, Jones RM, Casey BJ. A time of change: behavioral and neural correlates of adolescent sensitivity to appetitive and aversive environmental cues. Brain Cognition. 2010;72:124–133. doi: 10.1016/j.bandc.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Klingberg T, Fernell E, Olesen PJ, Johnson M, Gustafsson P, Dahlstrom K, et al. Computerized training of working memory in children with ADHD--a randomized, controlled trial. J Am Acad Child Adolesc Psychiatry. 2005;44:177–186. doi: 10.1097/00004583-200502000-00010. [DOI] [PubMed] [Google Scholar]
- 108.Reynolds B, Dallery J, Shroff P, Patak M, Leraas K. A web-based contingency management program with adolescent smokers. J Appl Behav Anal. 2008;41:597–601. doi: 10.1901/jaba.2008.41-597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Verbeken S, Braet C, Goossens L, van der Oord S. Executive function training with game elements for obese children: a novel treatment to enhance self-regulatory abilities for weight-control. Behav Res Ther. 2013;51:290–299. doi: 10.1016/j.brat.2013.02.006. [DOI] [PubMed] [Google Scholar]


