INTRODUCTION
In 1964 Green and Solnit described a phenomenon, the Vulnerable Child Syndrome (VCS), whereby children who were at one point in their lives expected to die subsequently recovered, but their health continued to be perceived as being more vulnerable than it in actuality was, resulting in heightened anxiety in parents that causes disturbance in parent-child interactions and adverse, long lasting outcomes in the child including separation difficulties, sleep problems, disruptive behavior, school underachievement, physically abusive behavior directed towards the mother and hyperactivity.1 They described five situations that put children at risk for being perceived as vulnerable including three that could occur during pregnancy and delivery. The subsequent development of an instrument to measure VCS has allowed for the examination of this important syndrome.2 A modification of the scale for infants, the Vulnerable Baby Scale (VBS), has made the study of this syndrome among very young children possible.3
That children born prematurely may continue to be perceived as vulnerable is unsurprising and the percentage of parents who fear that their premature infant might die is high. A number of maternal sociodemographic, psychosocial, and family characteristics have been associated with parental heightened perceptions of vulnerability, including age,1 marital status,4-7 socioeconomic status,4-8 education,4-6, 9 reproductive history,1, 6-10 mental health pre-delivery, poor physical health post-delivery, anxiety, well-being, self-efficacy, parenting stress and depression.1, 2-5, 7, 9-14 Similarly, maternal psychosocial response to the preterm birth (anxiety, overall well-being, self-efficacy, parenting stress, post-partum depression, cognitive appraisal of the infant, and mother-child interactions1, 6, 13-14 have been shown to be associated with VCS. Mothers who develop prematurity/stereotyping may be particularly susceptible to developing VCS and women who see their children vulnerable at 5 months of age have been shown to have less positive interactions with their children at 9 months of age15,16 Finally, infant characteristics, including birth order, longer hospital stays, and the presence of medical conditions at birth2, 4-5, 7, 9-10, 13-14, 17-18 have also been related to maternal perception of vulnerability (Table 1). However, much of this previous research has been retrospective, comprised of small, non-representative samples, without identification of mechanisms, and examined a limited number of characteristics.
Table 1.
Research Examining Parental Perceptions of Vulnerability in Premature Infants
| Citation | Study Design | Study Sample | Principle Research Questions/Findings |
|---|---|---|---|
| 1. Culley, BS, Perrin, EC, & Chaberski, MJ. (1989). Parental perceptions of vulnerability of formerly premature infants. Journal of Pediatric Health Care, 3(5), 237-245. | Cross sectional Survey | 80 healthy 3 year-olds who had been admitted to a NICU either because of birth weight <1500 grams or hyaline membrane requiring ventilation attenders at follow-up clinic. Comparison = 41 children born at same hospital during same time period but with no problems – randomly sampled from nursing records. |
• Is there a persistent sense of vulnerability in mothers of children admitted to a NICU but who at 3 are healthy. • Factors related to vulnerability • Is vulnerability related to behavior problems |
| 2. Perrin, EC, West, PD, & Culley, BS. (1989). Is my child normal yet? Correlates of vulnerability. Pediatrics, 83(3), 355-363. | Cross sectional Survey | 80 healthy 3 year-olds who had been admitted to a NICU either because of bw <1500 grams or hyaline membrane requiring ventilation attenders at follow-up clinic. Comparison = 41 children born at same hospital during same time period but with no problems – randomly sampled from nursing records. All children born in NICU between 4/82 and 3/83: 186 total. 105 were contacted, 103 agreed to participate. |
• Is there a persistent sense of vulnerability in mothers of children admitted to a NICU but who at 3 are healthy. • Factors related to vulnerability • Is vulnerability related to behavior problems • 49 = premature, 39 healthy, 10 problems • 54 = full term, 4 healthy, 4 previous problems with neonatal morbidity, 9 are neonatal morbidity but healthy |
| 3. Burger, JA, Horwitz, SM, Forsyth, BWC, Leventhal, JM, & Leaf, PJ. (1993). Psychological Sequelae of Medical Complications During Pregnancy. Pediatrics, 91(3), 566-571. | Longitudinal Cohort | 1095 4-8 year old children recruit from a stratified random sample of pediatric practices | • Whether women with severe medical complications during pregnancy are at increased risk of postpartum depression and/or viewing their child as vulnerable • Depression associated with pregnancy complications |
| 4. Miles, MS, & Holditch-Davis, D. (1995). Compensatory parenting: how mothers describe parenting their 3-year-old, prematurely born children. Journal of pediatric nursing, 10(4), 243. | Longitudinal Cohort | Convenience subsample of premature children born ≤ 1500 grams or needed mechanical ventilation Included 27 caretakers of 30 3 year olds |
• Do mothers’ memories of birth and NICU hospitalizations affect perceptions and parenting of their 3 year olds • 50% seen as vulnerable at age 3 – no correlates of vulnerability |
| 5. Thomasgard, M, & Metz, WP. (1997). Parental overprotection and its relation to perceived child vulnerability. American Journal of Orthopsychiatry, 67(2), 330-335. | Cross sectional Survey | Parents of 5-year olds recruited from 2 pediatric practices serving Worcester, MA 4/92 – 6/92 Of 300 parents, 7% refused |
• Child vulnerability related to antecedent medical factors • Child vulnerability and parental overprotection are not related • Vulnerability and overprotection not the same |
| 6. Estroff, Debra Bendell, Yando, Regina, Burke, Kathleen, & Synder, David. (1994). Perceptions of preschoolers’ vulnerability by mothers who had delivered preterm. Journal of pediatric psychology, 19(6), 709-721. | Cross sectional Survey | 50 preschool children 36-37.5 months enrolled in a follow up clinic since discharged from NICU | • Characteristics related to perceived vulnerability • Do vulnerable versus non vulnerable children differ developmentally and behaviorally |
| 7. Thomasgard, M. (1998). Parental perceptions of child vulnerability, overprotection, and parental psychological characteristics. Child psychiatry and human development, 28(4), 223-240. | Cross sectional Survey | 871 parents of 22 72-month old children recruited from 5 primary care pediatric practices in Columbus, OH 3/94 – 8/94, which represents 84% of those approached | • Are vulnerability and overprotectiveness related • Outcomes of vulnerability • Maternal psychological factors related to vulnerability |
| 8. Green, M, & Solnit, AJ. (1964). Reactions to the Threatened Loss of a Child: A Vulnerable Child Syndrome Pediatric Management of the Dying Child, Part III. Pediatrics, 34(1), 58-66. | Case study | 25 parents of children who were expected to die prematurely | • Description of the vulnerable child syndrome • Predisposing factors |
| 9. Forsyth, BWC, Horwitz, SM, Leventhal, JM, & Burger, J. (1996). The Child Vulnerability Scale: an instrument to measure parental perceptions of child vulnerability. Journal of pediatric psychology, 21(1), 89-101. | Longitudinal Cohort | 1095 children and families recruited from stratified random sample of pediatric practices in the greater New Hampshire area | • Understand the diagnosis and management of psychosocial problems by primary care pediatricians • Develop the Child Vulnerability Scale • Look at correlates of vulnerability |
| 10. Miceli, PJ, Goeke-Morey, MC, Whitman, TL, Kolberg, KS, Miller-Loncar, C, & White, RD. (2000). Brief report: birth status, medical complications, and social environment: individual differences in development of preterm, very low birth weight infants. Journal of pediatric psychology, 25(5), 353-358. | Longitudinal Cohort | 30 infants and families in a longitudinal study of preterm infant development | • Importance of birth status, medical complications and social outcomes for development outcomes in a sample of preterm very low birth weight infants across 3 years |
| 11. De Ocampo, AC, Macias, MM, Saylor, CF, & Katikaneni, LD. (2003). Caretaker perception of child vulnerability predicts behavior problems in NICU graduates. Child psychiatry and human development, 34(2), 83-96. | Cross sectional Survey | 90 low income parents consecutively enrolled at a high risk neonatal developmental follow-up clinic | • Constructs of parental perceptions of child vulnerability and child medical severity |
| 12. Teti, DM, Hess, CR, & O'Connell, M. (2005). Parental Perceptions of Infant Vulnerability in a Preterm Sample: Prediction from Maternal Adaptation to Parenthood during the Neonatal Period. Journal of Developmental & Behavioral Pediatrics, 26, 283-292. | Randomized Controlled Trial | 97 low income AA mothers of preterm infants recruited from 4 NICUs near DC, in a parent-child interaction intervention, 54-58 weeks post birth follow-up | • Mother's assessment that child is unresponsive, inattentive will presage CVS later • Parental self-efficacy will be related to CVS and can be moderated by infant health, depression and social support |
| 13. Allen, EC, Manuel, JC, Legault, C, Naughton, MJ, Pivor, C, & O'Shea, TM. (2004). Perception of child vulnerability among mothers of former premature infants. Pediatrics, 113(2), 267-273. | Longitudinal Cohort | 116 mothers of preterm (≤32 weeks) infants | • Is higher PPCV associated with worse developmental outcomes • Assessed at discharge and at 1 year adjusted age |
| 14. Chambers, PL, Mahabee-Gittens, EM, & Leonard, AC. (2011). Vulnerable Child Syndrome, Parental Perception of Child Vulnerability, and Emergency Department Usage. Pediatric Emergency Care, 27(11), 1009-1013. | Cross sectional Survey | 351 parents/legal guardians of children 1-15 years with no emergent problems | Relationship between high Emergency Department use and perceptions of vulnerability |
| 15. Stern, M, Karraker, K, McIntosh, B, Moritzen, S, & Olexa, M. (2006). Stereotyping and Mothers’ Interactions with their Premature and Full-term Infants during the First Year. Journal of pediatric psychology, 31(6), 597-607. | Longitudinal Cohort | Premature and full-term infants identified through newspaper birth listings were sent a letter. 25% contacted researchers, 22% participated. 115 mothers, 59 of full-term, 56 of premature infants assessed at 5.9 months | • Are premature stereotypes and perceptions of vulnerability stable across time • Are these related • Are these related to later infant outcomes |
Having a model that provides a framework for investigating the development of perceptions of vulnerability in mothers of preterm infants would facilitate the systematic study of this important problem and the development of interventions to prevent its occurrence. However, there is no theoretical explanation for why VCS develops in some mother-child dyads and not others. Miles and Holditch-Davis (1997) outlined a pathway for influences in parents of prematurely born children but failed to specify specific constructs or how elements in the pathway interrelate.19 Thomasgard and Metz (1995) outlined a conceptual model of parental perceptions of child vulnerability (PPCV) but not specifically for preterm infants.8
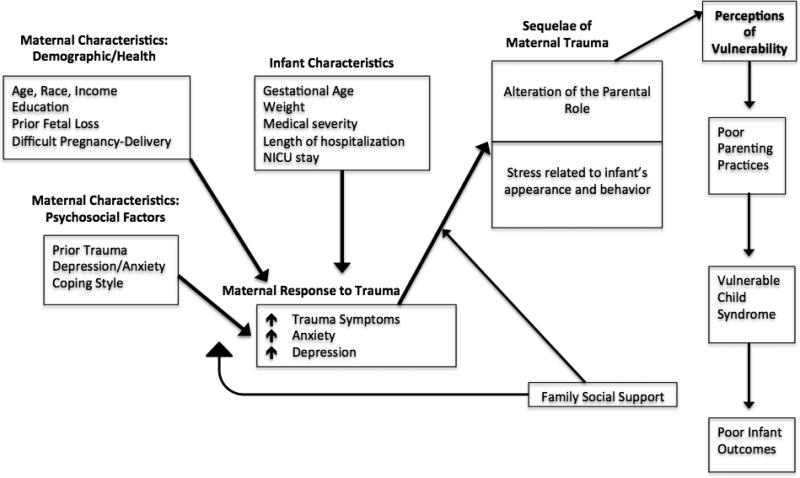
Based on the literature and clinical experience with mothers of preterm infants, we constructed a model that represents how increased perceptions of vulnerability are likely to develop (Figure 1). It is predicated on the fact that a preterm birth, for most women, is a traumatic event associated with symptoms of depression, anxiety and posttraumatic stress disorder.20 These reactions are tempered by several maternal demographic, health and psychosocial characteristics including prior trauma, depression, anxiety, coping style and social support. These maternal features, coupled with infant factors and possibly moderated by mothers’ social support, influence the mothers’ responses (anxiety, depression, trauma symptoms) to the trauma of a premature birth. These maternal responses, again possibly moderated by the mother's social support, in turn are related to the sequelae of the trauma including stress related to the infant's appearance and behavior and alterations in the parental role. We hypothesize that these sequelae result in the development of parental perceptions of child vulnerability8 and PPCV promotes poor parenting practices leading to the development of VCS. The purpose of this manuscript is to test the hypothesized theoretical model of the development of PPCV (Figure 1).
Figure 1.
Theoretical Model of the Development of Increased Maternal Preceptions of Child Vulnerability
METHODS
Participants and Procedure
Participants were mothers of premature infants hospitalized within the first week of delivery in one of the four participating NICUs affiliated with Lucile Packard Children's Hospital. As previously described,20 English and Spanish-speaking mothers >18 years of infants 25-34 weeks, >600 grams, without developmental abnormalities or awaiting cardiac surgery and were likely to survive, were potentially eligible to participate (N = 135). After receiving written informed consent, mothers were screened for clinically significant symptoms of anxiety and Acute Stress Disorder. 20 Mothers meeting the cutoff on ≥1 measure and did not have psychotic symptoms or clinically significant suicidal or infanticidal ideation were invited to participate in this study (105/135, 78%). All 105 eligible women agreed to participate. As described elsewhere,12 mothers were randomly assigned to either a 3-4 week cognitive-behavioral therapy-based trauma-focused intervention plus infant redefinition group or an active comparison group consisting of 45 minutes of education about the NICU environment, symptoms of distress, development of their premature infant and a referral to the hospital parent-mentoring program. Fidelity to the six intervention sessions was extremely high, ranging from 88-.97.21 All participants were assessed at baseline (1-2 weeks after the birth of the infant), one week after the completion of the intervention or 4-5 weeks post birth for the comparison group, and 6 months post birth. The 95 women available at 6 months post birth comprise this sample (95/105 or 90.5% of these initially enrolled). The Stanford University institutional review board approved the protocol.
Measures
Maternal Sociodemographic/health characteristics included age, ethnicity, education, income, marital status, country of birth, language (English or Spanish), number of children, prior premature infants, and bed rest prior to the premature birth.
Infant Characteristics: Gestational age, birth weight, and length of the infant's hospitalization were ascertained from the medical record. As previously described, 20 an infant severity score (probability of death index) was calculated using a multivariable risk adjustment model designed to capture important patient factors risk based upon Vermont Oxford network model 22 modifications tailored to the California Perinatal Quality Care Collaborative data.
Maternal Psychosocial Factors
Prior Trauma: Traumatic Events Questionnaire (TEQ)23
This 11-item questionnaire assesses specific trauma experiences capable of eliciting post-traumatic stress symptoms. The 2-week test-retest reliability for number of events is .91 and for specific events is .72-1.0. For these analyses the TEQ was scored as any (1) versus none (0).
Mini International Neuropsychiatric Interview (MINI) Diagnostic Interview24
This structured diagnostic interview established DSM-IV-TR diagnoses of any major depressive episode, any anxiety disorder and post traumatic stress disorder (PTSD). A multicenter study reported agreement ranging from κ=.41-.68, sensitivity from .41 -.86, and specificity from .84-.97.
Coping Styles: The Brief COPE25
a 28-item questionnaire, was used to assess maternal coping styles. Two adaptive coping scales (emotion-focused and problem-focused) and one maladaptive coping scale (dysfunctional) were created. Internal consistency in the current study ranged from 0.68 to 0.76.
Maternal Response to Trauma
Depression: Beck Depression Inventory-II (BDI-II)26
This 21-item questionnaire assesses depressive symptoms. The one-week test-retest reliability was .92. Internal consistency in this sample was .88. 26
Anxiety: Beck Anxiety Inventory (BAI)27
This 21-item self-report measure, which assesses symptoms of anxiety, has good internal consistency (in this sample, .90) and one week test-retest reliability of .75.24
Depression: Davidson Trauma Scale28
This 17-item scale, which assesses DSMIV-TR symptoms of Post Traumatic Stress Disorder (PTSD), has solid test-retest reliability (r=.86), internal consistency (α =.99; .91 this sample), and 83% diagnostic accuracy with the Structured Clinical Interview for DSM Disorders (SCID) at a score of 4.28
Sequelae of Maternal Trauma
Parental Stressor Scale: Neonatal Care Unit (PSS: NICU)29
This 35-item scale evaluates parents’ perceptions of stressors due to the infants’ NICU stay in three areas: physical environment of the NICU, infant's behavior/appearance, and alterations of the parental role. Internal consistency was α >.70 for all scales; in this sample, .94. These analyses examined the latter two subscales.
Family Social Support
One question with 5-point ordinal response (1=not at all to 5=very supportive) measured family social support at 4-5 weeks post birth. Due to the skewed and sparse distribution of this measure, it was dichotomized as high (5) vs. not high (1-4).
Parental Perception of Child Vulnerability at 6 months past birth
The Vulnerable Baby Scale (VBS)3
A 10-item scale measuring a parent's perception of their child's vulnerability, has adequate internal consistency (α=.70).3 The VBS was derived from the Child Vulnerability Scale, which has acceptable construct validity and internal consistency of 0.74 (in this sample, .59).2 The six-month post birth VBS is the outcome measure.
ANALYSIS
Unadjusted bivariate associations were examined using Pearson and Spearman correlations, the two-sample t-test, and Analysis of Variance. The MacArthur Mediator-Moderator approach, 30, 31 a structured exploratory approach to examining potential risk factors and their role as mediators and/or moderators of outcomes of longitudinal studies, was used to assess the theoretical model (Figure 1). Following the four step approach used by Essex et al., (2006) to examine risk factors for mental health problems in pediatric populations,30 measures were first grouped by time and domain, as indicated by the rectangles in Figure 1. Second, bivariate associations of each potential risk factor with 6-month VBS scores were examined; given the relatively small sample size, associations p<.15 were included in subsequent analyses. Third, measures ascertained contemporaneously within the same theoretical domain were grouped together. Within each group, overlapping risk factors (correlated measures, with main effects and/or their interaction influencing the outcome) were identified. The results showed that trauma, depression, and anxiety from the maternal response to trauma domain were overlapping, as were the two PSS: NICU measures (alteration of parent role and stress related to the infant's appearance and behavior) from the sequelae of maternal trauma domain. Before conducting the path analyses, overlapping variables were combined to create a single measure using the first principal component as the common construct. The final step included chronologically ordering the risk factors and specifying mediators and moderators. Mediation models were estimated using the PROCESS macro for SAS v2.11 (Andrew F Hayes, copyright 2014). For direct effects, ordinary least squares estimates were used to construct 95% confidence intervals; for indirect effects, 95% bias-corrected confidence intervals were constructed from 10,000 bootstrapped samples. Estimates are reported in the path diagram figures, and statistically significant pathways (p<.05) are bold and highlighted.
RESULTS
Mothers were, on average, 32.6 years of age, most often White non-Hispanic (34%) or Hispanic (31%) and 63% were at least college graduates (Table 2). Forty-three percent reported ≥1 traumatic event prior to the infant's birth. On the MINI, 37% met criteria for depression, and nearly 10% for anxiety. Nearly 7 out of 10 reported high family social support. Infants were, on average, born at 31.4 weeks gestation and weighed 1581g.
Table 2.
Maternal and Infant Characteristics for the Analytic Sample and Bivariate Associations with Maternal Response to Trauma and VBS Scores at 6-Month Follow-Up (N=95)
| Analytic Sample | VBS Scores at 6-Month Follow-up | ||
|---|---|---|---|
| Characteristics | Mean ± SD or N (%) | Corr or Mean ± SD | p-val |
| Maternal Characteristics: | |||
| Demographic / Health | |||
| Age (y; M ± SD) | 32.6 ± 6.2 | −.02 | .83 |
| Race/Ethnicity | |||
| White, Non-Hispanic | 32 (33.7%) | 28.4 ± 5.5 | .83 |
| Hispanic | 29 (30.5%) | 28.1 ± 4.5 | |
| Other | 34 (35.8%) | 28.9 ± 5.6 | |
| Household income | |||
| <$50k | 24 (25.3%) | 28.5 ± 4.0 | .99 |
| $50-$99k | 14 (14.7%) | 28.4 ± 5.4 | |
| ≥$100k or no answer | 57 (60.0%) | 28.5 ± 5.7 | |
| Education | |||
| Less than college | 35 (36.8%) | 29.4 ± 5.6 | .41 |
| College degree | 28 (29.5%) | 27.6 ± 5.3 | |
| Post-graduate degree | 32 (33.7%) | 28.3 ± 4.7 | |
| Prior reproductive health trauma still stressful | |||
| No | 80 (84.2%) | 28.5 ± 4.9 | .98 |
| Yes | 15 (15.8%) | 28.5 ± 6.9 | |
| Bed rest during pregnancy | |||
| No | 66 (69.5%) | 29.0 ± 5.1 | .19 |
| Yes | 20 (21.0%) | 27.9 ± 5.0 | |
| Unknown | 9 (9.5%) | 25.9 ± 5.8 | |
| Psychosocial Factors | |||
| Any traumas during lifetime (TEQ) | 54 (56.8%) | 27.3 ± 4.4 | .009 |
| No | 41 (43.2%) | 30.1 ± 5.7 | |
| Yes | |||
| MINI | |||
| PTSD | |||
| No symptoms | 91 (95.8%) | 28.5 ± 5.1 | .85 |
| Symptoms of PTSD | 4 (4.2%) | 28.0 ± 7.3 | |
| Diagnosis of PTSD | 0 (0%) | n/a | |
| Depression† | |||
| No symptoms | 45 (47.4%) | 26.7 ± 4.3 | .002 |
| Symptoms of depression | 15 (l5.8%) | 28.4 ± 4.7 | |
| Diagnosis of depression | 35 (36.8%) | 30.8 ± 5.7 | |
| Anxiety | |||
| No symptoms | 63 (66.3%) | 28.0 ± 5.0 | .10 |
| Symptoms of anxiety | 23 (24.2%) | 28.5 ± 5.2 | |
| Diagnosis of anxiety | 9 (9.5%) | 32.0 ± 5.8 | |
| Coping Styles | |||
| Emotion-focused | 26.1 ± 5.0 | −.20 | .05 |
| Problem-focused | 18.2 ± 3.8 | −.01 | .96 |
| Dysfunctional | 20.9 ± 4.9 | .42 | <.001 |
| High family social support | |||
| No | 29 (30.5%) | 30.2 ± 5.8 | .03 |
| Yes | 66 (69.5%) | 27.7 ± 4.8 | |
| Maternal Response to Trauma | |||
| Trauma | 45.8 ± 25.4 | .44 | <.001 |
| Depression | 19.3 ± 10.1 | .52 | <.001 |
| Anxiety | 21.3 ± 12.1 | .39 | <.001 |
| Sequelae of Maternal Trauma | |||
| Alteration of parent role | 3.69 ± 0.98 | .27 | .008 |
| Stress related to the infant's appearance and behavior | 2.89 ± 1.01 | .27 | .008 |
| Infant characteristics | |||
| Gestational age (wks) | 31.4 ± 2.9 | −.19 | .06 |
| Birthweight (g) | 1581± 551 | −.19 | .06 |
| Infant severity score* | 2.52 (1.59, 5.50) | .21 | .04 |
| Length of hospitalization* (days) | 39 (22, 71) | .18 | .08 |
Median (25th, 75th percentile)
Mothers with a diagnosis of depression had significantly higher VBS scores than mothers with no symptoms of depression.
No maternal demographic or health characteristic was related to VBS at 6 months (Table 2) and, thus, not included in the path analysis. Prior trauma and depression were strongly related to increased VBS. Additionally, greater endorsement of a dysfunctional coping style, maternal responses to the trauma of a preterm birth (clinically significant trauma, depression and anxiety), and sequelae of the trauma - alteration of the parental role and perceived stress related to the appearance and behavior of the infant - were all related to higher VBS scores. High family social support was related to lower VBS. Most infant characteristics tended to be associated with increased VBS, including lower gestational age, birth weight, higher infant severity scores and longer hospital stay.
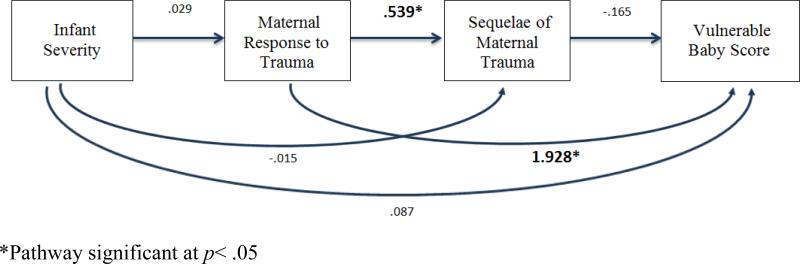
The first path model was a multiple mediator model: maternal response to trauma and sequelae of maternal trauma were hypothesized to mediate the relation between infant severity and VBS (Figure 2a). The results showed that neither were mediators, and infant severity did not have a direct effect on VBS. As both the direct and indirect effect of infant severity on VBS were not significant, infant severity was excluded from subsequent path models. Further, sequelae of maternal trauma did not mediate the relation between maternal response to trauma and VBS, nor did it have a direct effect on VBS. Thus, sequelae of maternal trauma were excluded from further analyses. Finally, the results suggested that maternal response to trauma has a significant direct effect on VBS, and, therefore, was included in further path models.
Figure 2a.
Maternal response to trauma and sequelae of maternal trauma are mediators of the relation between infant severity and VBS
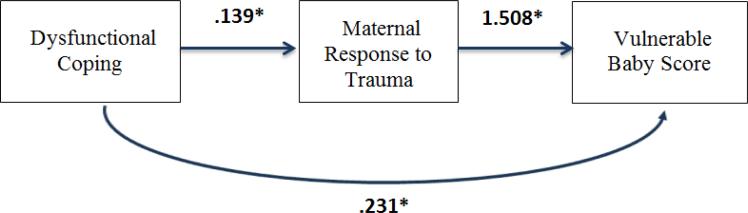
The second path model tested the hypothesis that maternal response to trauma mediates the association between dysfunctional coping and VBS (Figure 2b). The findings suggest that maternal response to trauma is a partial mediator; dysfunctional coping has a direct and indirect effect on VBS, such that mothers with higher dysfunctional coping scores have a greater response to trauma, and in turn, have higher VBS.
Figure 2b.
Maternal response to trauma as a mediator of the relation between dysfunctional coping and VBS
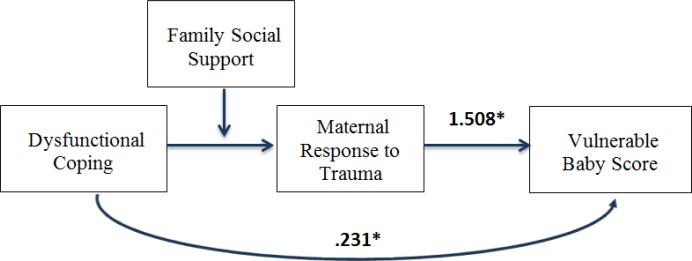
The third path model extends the second model by examining moderated mediation, whereby the effect of maternal response to trauma as a mediator of the association between dysfunctional coping and VBS varies by level of family social support. The results show that maternal response to trauma is a stronger mediator of the relation between dysfunctional coping and VBS among mothers with vs. without high family social support (Beta (SE): 0.358 (0.124) vs. 0.123 (0.060)). These indirect effects are significantly different (index of moderated mediation: 0.235 (0.119), p<.05). Analyses stratified by family social support show that the relation between dysfunctional coping and VBS is stronger among mothers without vs. with high family social support (total effect (SE): 0.787 (0.169) vs. 0.256 (0.117)). Among mothers without high family social support, dysfunctional coping has significant direct and indirect effects on VBS. In contrast, among mothers with high social support, maternal response to trauma mediates the relation between dysfunctional coping and VBS, and dysfunctional coping does not have a direct effect on VBS (Figure 2c).
Figure 2c.
Moderated mediation: the effect of maternal response to trauma as a mediator of the association between dysfunctional coping and VBS varies by level of family social support.
In exploratory path analyses, we examined prior trauma from the maternal characteristics/psychosocial factors domain as a risk factor (results not shown). The findings showed that maternal response to trauma mediates the association between prior trauma and VBS (indirect effect: 1.186 (0.609), p<.05), indicating that prior trauma increases maternal response to trauma, which in turn increases VBS. The direct effect of prior trauma on VBS did not reach statistical significance (1.591 (0.934), p=09). Prior trauma did not moderate the relation between maternal response to trauma and VBS (interaction p-value = .21). Finally, there was no effect of the intervention on VBS.
DISCUSSION
We found overall support for a model that explains the development of maternal perceptions of child vulnerability for women who delivered prematurely. The model illustrates the importance of maternal psychosocial characteristics, social support and maternal responses to the trauma of a preterm birth when examining maternal perceptions of children's vulnerability. The first multiple mediator model (Figure 2a) showed that infant severity was not directly related to maternal response to trauma, sequelae of trauma or the VBS. Further, neither maternal response to trauma nor what we considered sequelae of the maternal trauma caused by a preterm birth were mediators of a relationship between infant severity and VBS. Given that infant health was infrequently related to perceived vulnerability in prior studies, that this study excluded the sickest premature infants and that the medical severity data was derived from chart information not maternal estimation of the infant's health, this finding is not surprising. However, what this first model also shows is that maternal response to trauma in the form of elevated depression, anxiety and trauma symptoms is related to VBS, as suggested by prior research,13, 14 but that this relationship is not mediated by what we have termed sequelae of maternal trauma although maternal response to trauma and sequelae of trauma are closely related. This finding is important since it suggests that women who are likely to perceive their infants as vulnerable can be identified by their responses to the trauma of a preterm birth and targeted for intervention to prevent the development of maternal perceptions of vulnerability.
Importantly, the model displayed in Figure 2b suggests that an important precursor of maternal response to trauma is a dysfunctional coping style, and that a dysfunctional coping style has both direct and indirect (through maternal response to trauma) effects on maternal perceptions of vulnerability. Mothers who endorse a dysfunctional coping style (which includes behavioral disengagement, denial, self-blame, self-distraction, substance use, and venting) would generally be expected to be less likely to process the emotional impact of their infant's premature birth, be less likely to accurately appraise the medical issues affecting their infant and as a result be more prone to distorted perceptions of vulnerability. This suggests that mothers with a dysfunctional coping style, particularly those with lower family social support, should be targeted for early intervention given that they have both a more severe response to the trauma of a premature birth and are more likely to perceive their premature children as vulnerable.
Finally, our hypothesis that the relation of trauma experienced prior to the preterm birth to perceptions of child vulnerability would be mediated by maternal response to trauma was supported. Women with prior trauma are more likely to have heightened responses to subsequent trauma like a premature birth and prior trauma may also cause women to misinterpret their infants’ physical appearance or benign physiological changes as indicating potential serious physical illness thus producing perceptions of vulnerability.
These data have certain limitations. The study population was reasonably small, limiting the power to test models with multiple risk factors. The study population came from one geographical area, had few African-American women (only 6%) and was comprised mostly of mothers of higher socioeconomic status. It is unclear if this model will generalize across racial, ethnic and socioeconomic groups. In particular, given the multiple stressors resource challenged mothers face, the model may not apply to these women. Other than medical severity, all other variables were self-reported and may be subject to response bias. Only mothers were included in the study; we have no information on fathers’ perceptions of vulnerability. Additionally, we collected no information on the contribution of medical staff comments to the development of perceptions of vulnerability.
Having a theoretical model to guide research on the development of maternal perceptions of child vulnerability will increase our understanding of important content for interventions to prevent mothers from developing exaggerated perceptions of vulnerability and the subsequent suboptimal parenting behaviors associated with perceiving a child as vulnerable. This initial examination of a theoretical model suggests that maternal responses to trauma are critical in the formation of perceptions of child vulnerability. Further, given that simply reducing these responses has not been associated with reduction in perceptions of vulnerability,32 specific attention should be paid to preventing the development of increased perceptions of vulnerability through the addition of evidence-based cognitive behavioral techniques in any interventions developed to treat symptoms of distress in women of preterm infants. These results also suggest that women with dysfunctional coping styles and low social support are particularly susceptible to perceiving their preterm children as vulnerable and need to be targeted to prevent the development of such perceptions. Given the challenges faced by children who are born prematurely, and the positive impact good parenting behaviors have on their development,33 it is important to intervene early to prevent the possible development of exaggerated perceptions of vulnerability that subsequently result in poor parenting practices and suboptimal child development.
Acknowledgments
Funding Source: Funding Source: R01-MH086579A to Drs. Shaw and Horwitz, Trial Registration: Clinical Trials. 900 Identifier: NCT 01307293
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest: The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Green M, Solnit AJ. Reactions to the threatened loss of a child: A vulnerable child syndrome pediatric management of the dying child, part III. Pediatrics. 1964;34(1):58–66. [PubMed] [Google Scholar]
- 2.Forsyth B, Horwitz S, Leventhal J, et al. The Child Vulnerability Scale: an instrument to measure parental perceptions of child vulnerability. J Pediatr Psychol. 1996;21(1):89–101. doi: 10.1093/jpepsy/21.1.89. [DOI] [PubMed] [Google Scholar]
- 3.Kerruish N, Settle K, Campbell-Stokes P, et al. Vulnerable Baby Scale: development and piloting of a questionnaire to measure maternal perceptions of their baby's vulnerability. J of Pediatr Ch. 2005;41(8):419–423. doi: 10.1111/j.1440-1754.2005.00658.x. [DOI] [PubMed] [Google Scholar]
- 4.Culley BS, Perrin EC, Jordan Chaberski M. Parental perceptions of vulnerability of formerly premature infants. Journal of Pediatric Health Care. 1989;3(5):237–245. doi: 10.1016/0891-5245(89)90003-5. [DOI] [PubMed] [Google Scholar]
- 5.Perrin EC, West PD, Culley BS. Is my child normal yet? Correlates of vulnerability. Pediatrics. 1989;83(3):355–363. [PubMed] [Google Scholar]
- 6.Burger J, Horwitz SM, Forsyth BW, et al. Psychological sequelae of medical complications during pregnancy. Pediatrics. 1993;91(3):566–571. [PubMed] [Google Scholar]
- 7.Miles MS, Holditch-Davis D. Compensatory parenting: how mothers describe parenting their 3-year-old, prematurely born children. J Pediatr N. 1995;10(4):243–253. doi: 10.1016/s0882-5963(05)80021-1. [DOI] [PubMed] [Google Scholar]
- 8.Thomasgard M, Metz WP. The vulnerable child syndrome revisited. J Dev Behav Pediatr. 1995;16(1):47–53. [PubMed] [Google Scholar]
- 9.Thomasgard M, Metz WP. Parental overprotection and its relation to perceived child vulnerability. Am J Orthopsychiatry. 1997;67(2):330. doi: 10.1037/h0080237. [DOI] [PubMed] [Google Scholar]
- 10.Thomasgard M. Parental perceptions of child vulnerability, overprotection, and parental psychological characteristics. Child Psychiatry Hum Dev. 1998;28(4):223–240. doi: 10.1023/a:1022631914576. [DOI] [PubMed] [Google Scholar]
- 11.Estroff DB, Yando R, Burke K, et al. Perceptions of preschoolers' vulnerability by mothers who had delivered preterm. J Pediatr Psychol. 1994;19(6):709–721. doi: 10.1093/jpepsy/19.6.709. [DOI] [PubMed] [Google Scholar]
- 12.Teti DM, Hess CR, O'Connell M. Parental perceptions of infant vulnerability in a preterm sample: Prediction from maternal adaptation to parenthood during the neonatal period. J Dev Behav Pediatr. 2005;26(4):283–292. doi: 10.1097/00004703-200508000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Allen EC, Manuel JC, Legault C, et al. Perception of child vulnerability among mothers of former premature infants. Pediatrics. 2004;113(2):267–273. doi: 10.1542/peds.113.2.267. [DOI] [PubMed] [Google Scholar]
- 14.Chambers PL, Mahabee-Gittens EM, Leonard AC. Vulnerable child syndrome, parental perception of child vulnerability, and emergency department usage. Pediatr Emerg Care. 2011;27(11):1009–1013. doi: 10.1097/PEC.0b013e318235bb4f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stern M, Karraker K, McIntosh B, Moritzen S, Olexa M. Prematurity stereotyping and mothers’ interactions with their premature and full-term infants during the first year. Journal of pediatric Psychology. 2006;31(6):597–607. doi: 10.1093/jpepsy/jsj051. [DOI] [PubMed] [Google Scholar]
- 16.Porter JS, Stern M, Zak-Place J. Prematurity stereotyping and perceived vulnerability at 5-months: Relations with mothers and their premature and full-term infants at 9-months. Journal of Reproductive and Infant Psychology. 2009;27(2):168–181. [Google Scholar]
- 17.Miceli PJ, Goeke-Morey MC, Whitman TL, Kolberg KS, et al. Brief report: birth status, medical complications, and social environment: individual differences in development of preterm, very low birth weight infants. J Pediatr Psychol. 2000;25(5):353–358. doi: 10.1093/jpepsy/25.5.353. [DOI] [PubMed] [Google Scholar]
- 18.De Ocampo AC, Macias MM, Saylor CF, et al. Caretaker perception of child vulnerability predicts behavior problems in NICU graduates. Child Psychiat Hum D. 2003;34(2):83–96. doi: 10.1023/a:1027384306827. [DOI] [PubMed] [Google Scholar]
- 19.Miles MS, Holditch-Davis D. Parenting the prematurely born child: pathways of influence. Seminars in Perinatology. Elsevier. 1997:254–266. doi: 10.1016/s0146-0005(97)80067-5. [DOI] [PubMed] [Google Scholar]
- 20.Shaw R, St. John N, Lilo E, et al. Prevention of traumatic stress in mothers with preterm infants: A Randomized Controlled Trial. Pediatrics. 2013;132(4):e886–e894. doi: 10.1542/peds.2013-1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shaw R, Sweester C, St. John N, Lilo E, Corcoran J, Jo B, et al. Prevention of postpartum traumatic stress in mothers with preterm infants: manual development and evaluation. Issues in Mental Health Nursing. 2013;34(8):578–586. doi: 10.3109/01612840.2013.789943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zupancic J, Richardson D, Horbar J, et al. Revalidation of the score for neonatal acute physiology in the Vermont Oxford Network. Pediatrics. 2007;119(1):e156–e163. doi: 10.1542/peds.2005-2957. [DOI] [PubMed] [Google Scholar]
- 23.Vrana S, Lauterbach D. Prevalence of traumatic events and post-traumatic psychological symptoms in a nonclinical sample of college students. J Traum Stress. 1994;7(2):289–302. doi: 10.1007/BF02102949. [DOI] [PubMed] [Google Scholar]
- 24.Sheehan D, Lecrubier Y, Sheehan K, et al. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychol. 1998;59(S20):22–33. [PubMed] [Google Scholar]
- 25.Carver CS, Gaines JG. Optimism, pessimism, and postpartum depression. Cognitive Ther Res. 1987;11(4):449–462. [Google Scholar]
- 26.Beck A, Steer R, Brown G. Beck Depression Inventory®-II (BDI® -II) San Antonio, TX: 1996. [Google Scholar]
- 27.Beck A, Epstein N, Brown G, et al. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 28.Davidson J, Book S, Colket J, et al. Assessment of a new self-rating scale for post-traumatic stress disorder. Psychol Med. 1997;27(1):153–160. doi: 10.1017/s0033291796004229. [DOI] [PubMed] [Google Scholar]
- 29.Miles M, Funk S, Carlson J. Parental Stressor Scale: neonatal intensive care unit. Nurs Res. 1993;42(3):148–152. [PubMed] [Google Scholar]
- 30.Essex MJ, Kraemer HC, Armstrong JM, et al. Exploring risk factors for the emergence of children's mental health problems. Arch Gen Psychiatry. 2006;63(11):1246–1256. doi: 10.1001/archpsyc.63.11.1246. [DOI] [PubMed] [Google Scholar]
- 31.Kraemer HC, Stice E, Kazdin A, et al. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. Am J Psychiatry. 2001;158(6):848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- 32.Horwitz S, Storfer-Isser A, Kerker B, et al. Does an intervention to reduce maternal anxiety, depression and trauma also improve mothers' perceptions of their preterm infants' vulnerability? . Inf Mental Hlth J. 2014 doi: 10.1002/imhj.21484. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Forcada-Guex M, Pierrehumbert B, Borghini A, et al. Early dyadic patterns of mother–infant interactions and outcomes of prematurity at 18 months. Pediatrics. 2006;118(1):e107–e114. doi: 10.1542/peds.2005-1145. [DOI] [PubMed] [Google Scholar]