Abstract
What kills people around the world and how it varies from place to place and over time is critical in mapping the global burden of disease and therefore, a relevant public health question, especially in developing countries. While more than two thirds of deaths worldwide are in developing countries, little is known about the causes of death in these nations. In many instances, vital registration systems are nonexistent or at best rudimentary, and even when deaths are registered, data on the cause of death in particular local contexts, which is an important step toward improving context-specific public health, are lacking. In this paper, we examine the trends in the causes of death among the urban poor in two informal settlements in Nairobi by applying the InterVA-4 software to verbal autopsy data. We examine cause of death data from 2646 verbal autopsies of deaths that occurred in the Nairobi Urban Health and Demographic Surveillance System (NUHDSS) between 1 January 2003 and 31 December 2012 among residents aged 15 years and above. The data is entered into the InterVA-4 computer program, which assigns cause of death using probabilistic modeling. The results are presented as annualized trends from 2003 to 2012 and disaggregated by gender and age. Over the 10-year period, the three major causes of death are tuberculosis (TB), injuries, and HIV/AIDS, accounting for 26.9, 20.9, and 17.3 % of all deaths, respectively. In 2003, HIV/AIDS was the highest cause of death followed by TB and then injuries. However, by 2012, TB and injuries had overtaken HIV/AIDS as the major causes of death. When this is examined by gender, HIV/AIDS was consistently higher for women than men across all the years generally by a ratio of 2 to 1. In terms of TB, it was more evenly distributed across the years for both males and females. We find that there is significant gender variation in deaths linked to injuries, with male deaths being higher than female deaths by a ratio of about 4 to 1. We also find a fifteen percentage point increase in the incidences of male deaths due to injuries between 2003 and 2012. For women, the corresponding deaths due to injuries remain fairly stable throughout the period. We find cardiovascular diseases as a significant cause of death over the period, with overall mortality increasing steadily from 1.6 % in 2003 to 8.1 % in 2012, and peaking at 13.7 % in 2005 and at 12.0 % in 2009. These deaths were consistently higher among women. We identified substantial variations in causes of death by age, with TB, HIV/AIDS, and CVD deaths lowest among younger residents and increasing with age, while injury-related deaths are highest among the youngest adults 15–19 and steadily declined with age. Also, deaths related to neoplasms and respiratory tract infections (RTIs) were prominent among older adults 50 years and above, especially since 2005. Emerging at this stage is evidence that HIV/AIDS, TB, injuries, and cardiovascular disease are linked to approximately 73 % of all adult deaths among the urban poor in Nairobi slums of Korogocho and Viwandani in the last 10 years. While mortality related to HIV/AIDS is generally declining, we see an increasing proportion of deaths due to TB, injuries, and cardiovascular diseases. In sum, substantial epidemiological transition is ongoing in this local context, with deaths linked to communicable diseases declining from 66 % in 2003 to 53 % in 2012, while deaths due to noncommunicable causes experienced a four-fold increase from 5 % in 2003 to 21.3 % in 2012, together with another two-fold increase in deaths due to external causes (injuries) from 11 % in 2003 to 22 % in 2012. It is important to also underscore the gender dimensions of the epidemiological transition clearly visible in the mix. Finally, the elevated levels of disadvantage of slum dwellers in our analysis relative to other population subgroups in Kenya continue to demonstrate appreciable deterioration of key urban health and social indicators, highlighting the need for a deliberate strategic focus on the health needs of the urban poor in policy and program efforts toward achieving international goals and national health and development targets.
Keywords: Adult mortality, Cause-specific mortality, Urban poor, Verbal autopsy, Informal settlements, Nairobi, Kenya
Introduction
The importance of cause-specific mortality rates for mapping the geographical burden of disease, policy, and program interventions has been well documented. Consistent estimates of cause-specific mortality are essential for understanding the overall epidemiological profile of disease in a population.1,2 Consequently, any planning process for health development ought to be based on a thorough understanding of the health needs of the population that is sufficiently comprehensive to include the causes of premature death and of disability, as well as the major risk factors that underlie disease and injury within geographical boundaries.3
Developing countries experience more than two thirds of deaths in the world, but the causes of these deaths are not well documented, and in many developing countries, vital registration systems are nonexistent or at best rudimentary, and even when deaths are registered, data on the cause of death, which is an important step toward improving public health, are lacking.4 According to WHO, mortality statistics in 87 % of countries suffer from incomplete registration of births and deaths, and incorrect reporting of the cause of death and ages.5 In SSA, only Mauritius is reported to register birth and death events in the last decade according to UN standards6, and millions of poor people are missing from national statistics, particularly those living in informal settlements, because they are simply not counted.7 Consequently, slum areas of fast-growing cities in developing countries are failing to benefit from the better and cheaper health services that are supposed to be derived from economies of scale, and this is linked to shortage of local data sets, which would reveal issues to prioritize in each slum.8 Moreover, governments cannot design effective public health policies or measure their impact when deaths go uncounted and the causes of death are not documented.5
In response to the general lack of consistent, timely, and reliable information on the levels and cause of death patterns and the accompanying dearth of vital registration systems, many developing countries in the last 10 years have turned to alternative sources of cause of death (COD) information, particularly through the verbal autopsy (VA) based on data from Health and Demographic Surveillance Systems (HDSS).9 The HDSS are platforms for monitoring and tracking demographic and health indicators in a population within a defined geographical area at regular intervals.10 HDSS platforms typically record vital events of births, deaths, and migration, which in turn become crucial inputs in health planning at both local and national levels, and estimating regional and global disease burdens.11–14 The VA process entails interviewing the primary caregivers of recently deceased persons to gather information on the circumstances surrounding the death.15 It is based on the premise that the primary caregiver—usually a family member—can recall, volunteer, and recognize symptoms experienced by the deceased that can be interpreted later to derive a probable cause of death. 16
Out of the many processes of interpreting VA data, the Interpreting Verbal Autopsy-4 (InterVA-4) computer program, which assigns cause of death using Bayes probabilistic theorem, has most recently been successfully explored in a number of settings by a wide range of experts and shown to achieve maximum consistency in VA data interpretation.17–19 While challenges remain concerning the efficacy of InterVA, particularly its lower sensitivity relative to other electronic methods,20 this approach to interpreting VA data remains a useful, easy to use tool, and alternative to the expensive and time-consuming practice of physician coding in countries without vital registration and medical certification of causes of death.21 In this paper, we utilize the InterVA-4 to examine the VA data collected in the Nairobi Urban Health and Demographic Surveillance Sites (NUHDSS) between 2003 and 2012.
Apart from identifying the most current key causes of death among the urban poor, our study examines the changing nature of the causes of death in the last 10 years. Nairobi city typifies the current urban population boom and associated urban health and poverty problems. Its population increased from about 120,000 in 1980 to about 3 million in 2009,22 with over 60 % of the population living in slums, which cover only 5 % of city’s residential land area.23 In the context of growing urban poverty, the urban advantage in health and well-being has been shown to have been eroded with rates of mortality higher in slums and periurban areas than in more privileged urban neighborhoods and rural areas.24–26 Our study provides a unique opportunity to examine causes of death among the urban poor in the last decade, in the context of the global push for the achievement of MDGs and the substantial attention and resources invested in the past decade by the Kenyan Government and its development partners to improve health and economic outcomes in the country, especially among vulnerable groups.
Global and national estimates are more easily available on major causes of death,3 but such macrolevel estimates, blur subgroup differentials, and the extent of health and mortality inequities borne by disadvantaged groups. In Kenya, the recent 2008/2009 Kenya Demographic and Health Survey (KDHS) show that there are positive results at the national level on key demographic and health indicators.27 However, due to the limited coverage of slum residents in the sample, such report is unable to answer a number of questions that are critical to the health and livelihood of the urban poor. Our study contributes to filling such gaps in knowledge by focusing on residents of informal settlements of a major city over a 10-year period.
Further, our study provides a unique insight into the mortality profile of adults 15 years and above. While unacceptable high maternal and child mortality rates remain a challenge in many developing countries, adult death is an often ignored phenomenon. A majority of the studies (80 %) are focused on causes of maternal and child mortality; yet, early life origins of disparities at older ages in both adult morbidity and mortality have been well documented, particularly how adult mortality outcomes are traced to the long arm of childhood experiences.28,29 It is estimated that risky behaviors initiated in adolescence persist to adulthood, primarily leading to 70 % of all premature deaths among adults.30 In the case of the Nairobi’s urban poor, while research has highlighted poor health outcomes among children and women of reproductive age,31,32 there is limited focus on the health and mortality outcomes of adults aged 15+ and the consequent impact on households as a whole. Adults in this age group constitute about 63 % of the population in the NUHDSS and contribute the largest proportion (48.5 %) of years of life lost (YLL) due to premature mortality.33 This is significantly higher than the 38.7 % of YLLs contributed by this age group in SSA.34 This age group is linked to deaths related to HIV/AIDS and injuries due to interpersonal violence and road traffic accidents, accounting for 55.3 and 18.4 % of YLL, respectively.33 The older region of this age spectrum is more prone to chronic conditions while the younger region is plagued by injuries whose other sequela include disability. As the most economically productive age group, their health status has direct bearing on household economic status; yet, commensurate research and policy focus on adults as a population at-risk of mortality are seldom addressed. Therefore, understanding the main causes of adult mortality over time will be critical not only in addressing major health concerns among this important segment of the population in informal settlements, but also a platform to link the local context to the changing nature of morbidity and mortality burdens in the overarching epidemiological transitions widely reported for developing countries.
Methods
Study Area and Population
We use cause of death data derived from 2646 deaths that occurred among adults aged 15 years and older in the NUHDSS between 1 January 2003 and 31 December 2012. Details of the NUHDSS have been published elsewhere.35 In brief, the NUHDSS is a longitudinal platform being implemented in the informal settlements of Korogocho and Viwandani. They are both located less than 10 km from the Central Business District (CBD) of Nairobi, Kenya’s capital city. The population under surveillance comprises about 28,500 households with about 72,000 residents since 2002. The surveillance involves visits to all households once every 4 months to record all demographic events, including births, deaths, and migrations. Additional data on household amenities and income are collected once a year for all households residing within the surveillance areas.
Cause of Death Data in the NUHDSS
Cause of death in the NUHDSS is generated using verbal autopsy—a process whereby primary caregivers of recently deceased persons are interviewed about the circumstances surrounding death. The process is typically used in areas where vital registration systems are incomplete or lacking. In the two slum areas under surveillance, less than 40 % of deaths occur in a health facility. Most deaths occur at home, and no records of causes of death are usually available. The VA process in the NUHDSS9,33 comprises trained interviewers visiting a household and conducting a VA interview within 3 months, on average, after a death has occurred. The VA interviews are conducted with a credible respondent—usually a spouse, child, or other close family member/neighbor who would have indicated being aware of the circumstances surrounding death. The interviews are conducted using a semistructured questionnaire adapted from the International Network for the Demographic Evaluation of Populations and Their Health (INDEPTH), which inquires about probable symptoms and signs that the deceased may have shown in the duration leading up to death. The questionnaire has an open-ended section for a verbatim narrative of the circumstances surrounding death according to the credible respondent. All other sections of the tool are, however, close-ended and structured. Quality assurance of data is prioritized through the careful training of interviewers on conducting the VA and reinforced through close supervision, which included 5 % spot-checks as well as office editing of all completed questionnaires.
Interpretation of VA Data—the InterVA Model
Once the questionnaires have been completed, their contents are analyzed and interpreted to arrive at possible causes of death. InterVA-4 is a computer program that applies probabilistic modeling based on Bayes’ theorem to interpret VA data and arrive at possible causes of deaths. The InterVA model has been widely tested in several settings, producing cost-effective, quick, and comparable results.17–19,36–40 While challenges remain concerning the efficacy of InterVA, particularly its lower sensitivity relative to other electronic methods,20 this approach to interpreting VA data remains a useful, easy to use tool, and alternative to the expensive and time-consuming practice of physician coding in countries without vital registration and medical certification of causes of death.21 In order to utilize InterVA-4 to interpret our VA data, we first captured the VA questionnaires electronically into an SQL database and then converted the data into a comma separated value (.csv) file. This file was imported into STATA 12, and using a STATA script, the data in the .csv file were then converted into the input indicators required by the InterVA-4 model. These indicators are generated also in .csv format and then run in InterVA-4’s batch mode. InterVA-4 then generates no more than three likely causes of death per case with a likelihood value between 0 and 1 for each of the three causes of death. In some instances, the input indicator data was insufficient for InterVA-4 to generate any likelihood cause of death. Such cases are assigned by the model as “indeterminate” cause of death and typically occur when the credible respondent does not provide sufficient detail during an interview. Again, if the sum of likelihoods for each probable cause of death per cause does not add up to 1, the difference between the sum of the likelihood values for probable causes of death and 1 were allocated to the indeterminate cause. Finally, all identified causes of death were considered proportionate to their likelihood values in the calculation of cause-specific mortality fractions as recommended in the InterVA-4 user guide.41
Statistical Approach
All analysis was performed using STATA 12. Although InterVA generates causes of death that can be mapped to ICD-10, we categorized causes of death into 20 main entities: HIV/AIDS, anemia, asthma, cardiovascular, chronic obstructive pulmonary diseases, diabetes mellitus, diarrheal disease, direct obstetric cause, infectious disease, injury, liver disease, malaria, malnutrition, meningitis, neonatal cause, neoplasm, respiratory tract infection, tuberculosis, and indeterminate cause. All other communicable and noncommunicable diseases were classified as “other.” These were further classified as four main entities: communicable disease, noncommunicable disease, external causes, and unspecified cause as summarized in Table 1. Finally, annualized causes-specific mortality fractions were calculated for each cause of death by gender and age and presented as percentages.
TABLE 1.
Main causes of death
| Communicable diseases | HIV/AIDS, Diarrheal Diseases, Direct Obstetric, Infectious Diseases, Malaria, Malnutrition, Meningitis, Neonatal Causes, Respiratory Tract Infection, TB |
| Non-communicable diseases | Anemia, Asthma, Cardio-vascular, COPD, Diabetes Mellitus, Liver Disease, Malignancies |
| External causes | Injuries |
| Unspecified causes | Indeterminate |
Ethical Considerations
We utilized routine collected data at the NUHDSS. In order to operate the NUHDSS, APHRC applied for and received approval from the Kenya Medical Research Institution’s National Ethics Review Committee (KEMRI/NERC). Informed consent is also obtained from each participant in the interviews.
Results
A total of 2646 VA interviews were completed successfully from January 2003 to December 2012. Overall, there were significantly more male deaths (59 %) than female (41 %). The InterVA model was able to assign cause of death for 91 % of male and 94 % of female VA interviews. The rest of the cases were allocated an indeterminate cause of death by the model.
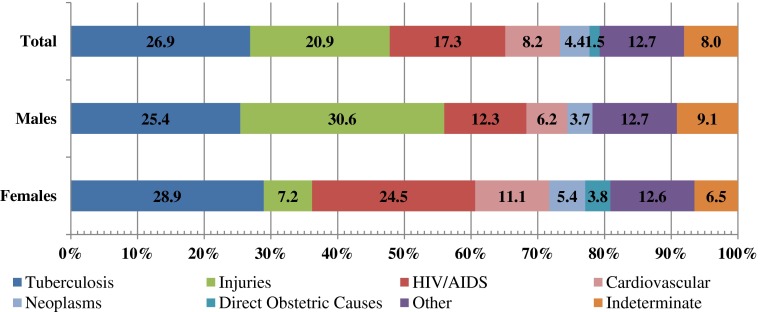
Figure 1 shows the major causes of death over the 10-year period among the whole population and disaggregated by gender. Overall, the three major causes of death over the 10-year period are TB, injuries, and HIV/AIDS accounting for 27, 21, and 17 %, respectively. In this period, one third of male deaths are due to injuries, while TB accounts for 25 % of deaths and 12 % are due to HIV/AIDS. Female deaths are attributable to TB, HIV/AIDS, other causes, and cardiovascular diseases, accounting for 29, 25, 13, and 11 %, respectively. The other main causes of death among females in this period were neoplasms (5 %) and direct obstetric causes (4 %).
FIG. 1.
Causes of death among all NUHDSS residents aged 15+ (N = 2464). 1 January 2003 to 31 December 2012.
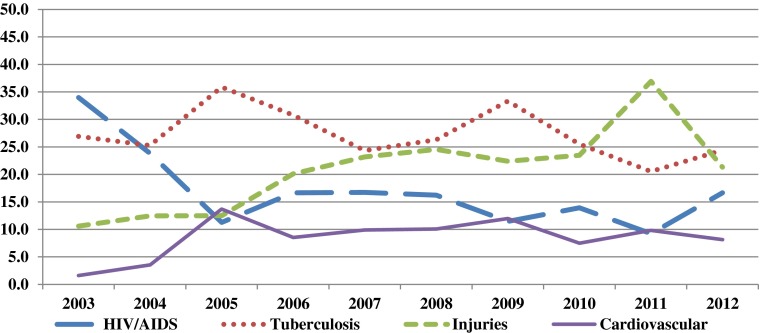
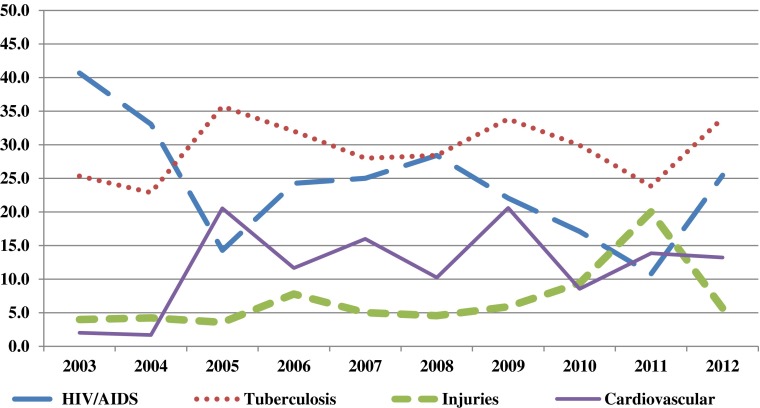
The main cause of death in 2003 was HIV/AIDS (accounting for over 30 % of deaths), followed by TB and then injuries (Fig. 2). However, by 2012, the proportion of deaths in the NUHDSS due to TB was higher than the proportion of deaths due to HIV/AIDS. Deaths due to injuries are on the rise in the study area, increasing steadily from 11 % in 2003 to 21 % in 2012. There is a significant peak in 2011, when 37 % of deaths overall are due to injuries. Cardiovascular disease is emerging as an important cause of death, increasing overall from 2 % in 2003 to 8 % in 2012, peaking at 14 % in 2005 and again at 12 % in 2009.
FIG. 2.
Main causes of death among all NUHDSS residents aged 15+ (N = 2464). 1 January 2003 to 31 December 2012.
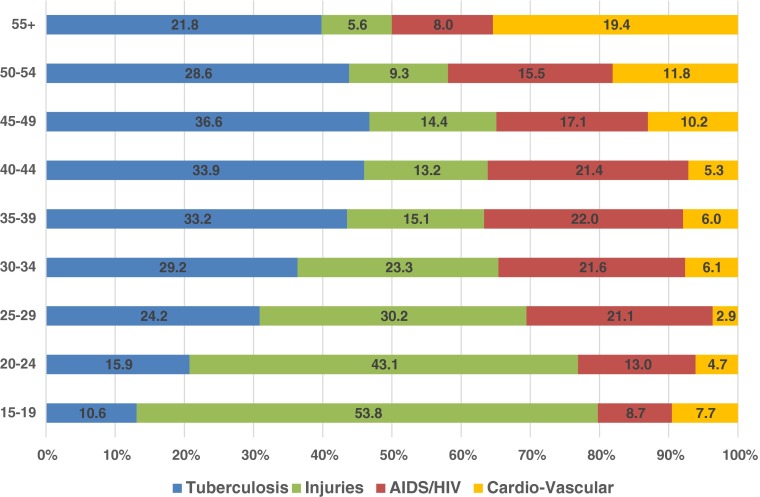
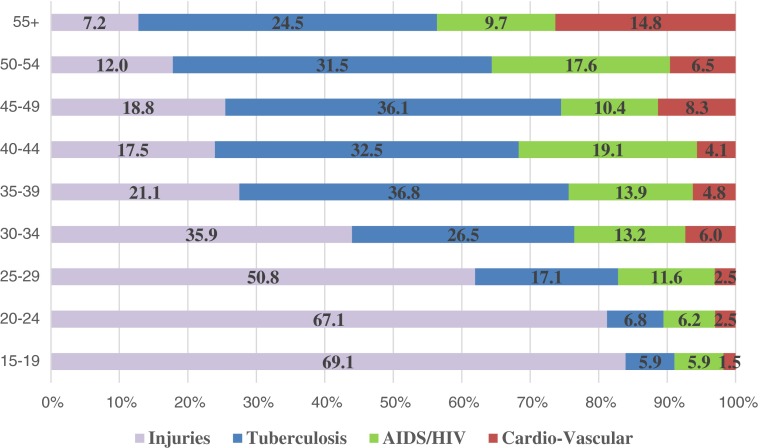
In Fig. 3, we see substantial variations in causes of death by age among the urban poor. TB, HIV/AIDS, and CVD deaths were lowest among younger residents and increased with age. TB deaths were highest among adults 35 to 49 years old, while HIV/AIDS deaths peaked among those aged 30–44 years, and deaths linked to CVD were highest among adults aged 50 years and above. On the contrary, injury-related deaths are highest among the youngest adults, causing 54 % of deaths among adolescents 15–19 and steadily declined with age.
FIG. 3.
Main causes of death among all NUHDSS residents by age.
Tables 2 and 3 summarize all causes of death in the NUHDSS by year and age, respectively, and what further came out more clearly was deaths related to neoplasms and respiratory tract infections (RTIs), which were linked to 4.4 and 3.3 % of all deaths, respectively. It is notable that both neoplasms and RTIs became more pronounced since 2005 and has remained so to date and both are highest among adults 50 years and above. Also important for methodological consideration is evidence that most deaths whose causes are indeterminate were among the same oldest adult cohorts aged 50 years or older. We also see the highest percentages of indeterminate cases between 2003 and 2004, with levels reduced significantly over time, pointing to improvements in the instruments and more efficiency in collecting VA data.
TABLE 2.
Causes of death among all adolescents and adults (> = 15 years), 2003–2012
| Generalized causes of death | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Tuberculosis | 26.9 | 25.3 | 35.9 | 30.8 | 24.3 | 26.3 | 33.3 | 25.5 | 20.5 | 24.4 | 26.9 |
| Injuries | 10.6 | 12.5 | 12.5 | 20.1 | 23.2 | 24.6 | 22.4 | 23.5 | 36.9 | 21.3 | 20.9 |
| AIDS/HIV | 34.0 | 23.8 | 11.3 | 16.7 | 16.7 | 16.2 | 11.5 | 13.9 | 9.2 | 16.7 | 17.3 |
| Cardio-vascular | 1.6 | 3.6 | 13.7 | 8.5 | 9.9 | 10.1 | 12.0 | 7.5 | 9.8 | 8.1 | 8.2 |
| Neoplasms | 0.6 | 0.7 | 8.1 | 5.1 | 6.5 | 6.1 | 3.6 | 7.1 | 2.7 | 5.0 | 4.4 |
| Other | 1.9 | 1.4 | 5.6 | 4.7 | 2.7 | 3.1 | 4.7 | 5.1 | 4.8 | 6.6 | 4.0 |
| Respiratory tract infection | 0.6 | 1.1 | 2.8 | 6.0 | 3.0 | 2.6 | 3.1 | 4.4 | 3.6 | 5.8 | 3.3 |
| Meningitis | 0.3 | 1.1 | 3.2 | 3.4 | 3.0 | 3.9 | 0.5 | 3.1 | 2.7 | 2.7 | 2.4 |
| Direct obstetric causes | 2.9 | 2.8 | 1.2 | 0.0 | 1.1 | 0.4 | 0.0 | 2.7 | 2.4 | 0.4 | 1.5 |
| Asthma | 0.3 | 0.7 | 0.8 | 0.4 | 2.3 | 0.0 | 1.6 | 0.7 | 0.0 | 1.6 | 0.8 |
| Chronic obstructive pulmonary disease | 1.3 | 1.4 | 0.0 | 1.3 | 0.0 | 1.3 | 0.5 | 0.7 | 0.3 | 0.8 | 0.8 |
| Malaria | 0.0 | 0.4 | 0.8 | 0.4 | 0.4 | 0.4 | 0.0 | 0.3 | 0.6 | 1.2 | 0.5 |
| Diarrhoeal disease | 0.0 | 0.4 | 0.4 | 0.0 | 0.0 | 0.4 | 0.5 | 0.3 | 0.6 | 0.8 | 0.3 |
| Liver disease | 0.0 | 0.4 | 0.4 | 0.0 | 0.4 | 0.0 | 0.0 | 0.3 | 0.3 | 0.8 | 0.3 |
| Diabetes mellitus | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.5 | 0.0 | 0.9 | 0.4 | 0.2 |
| Malnutrition | 0.0 | 0.4 | 0.0 | 0.0 | 0.4 | 0.4 | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 |
| Anaemia | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.4 | 0.5 | 0.0 | 0.0 | 0.0 | 0.1 |
| Infectious diseases | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.5 | 0.0 | 0.0 | 0.0 | 0.0 |
| Neonatal causes | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Indeterminate | 18.9 | 24.2 | 3.2 | 2.6 | 6.1 | 3.5 | 4.7 | 4.8 | 4.8 | 3.5 | 8.0 |
| Total number of deaths | 312 | 281 | 248 | 234 | 263 | 228 | 192 | 294 | 336 | 258 | 2,646 |
TABLE 3.
Causes of death among all adolescents and adults (> = 15 years) by age group, 2003–2012
| Generalized causes of death | 15–19 | 20–24 | 25–29 | 30–34 | 35–39 | 40–44 | 45–49 | 50–54 | 55+ | Total |
|---|---|---|---|---|---|---|---|---|---|---|
| Tuberculosis | 10.6 | 15.9 | 24.2 | 29.2 | 33.2 | 33.9 | 36.6 | 28.6 | 21.8 | 26.9 |
| Injuries | 53.8 | 43.1 | 30.2 | 23.3 | 15.1 | 13.2 | 14.4 | 9.3 | 5.6 | 20.9 |
| AIDS/HIV | 8.7 | 13.0 | 21.1 | 21.6 | 22.0 | 21.4 | 17.1 | 15.5 | 8.0 | 17.3 |
| Cardio-vascular | 7.7 | 4.7 | 2.9 | 6.1 | 6.0 | 5.3 | 10.2 | 11.8 | 19.4 | 8.2 |
| Neoplasms | 2.9 | 1.4 | 1.6 | 1.9 | 4.1 | 3.6 | 3.2 | 7.5 | 12.4 | 4.4 |
| Other | 0.0 | 5.4 | 2.9 | 2.8 | 4.4 | 4.9 | 5.1 | 1.9 | 5.6 | 4.0 |
| Respiratory tract infection | 1.9 | 2.2 | 3.1 | 2.8 | 2.5 | 4.9 | 1.4 | 5.0 | 4.6 | 3.3 |
| Meningitis | 3.8 | 1.4 | 2.3 | 0.9 | 3.6 | 4.3 | 2.8 | 3.1 | 1.2 | 2.4 |
| Direct obstetric causes | 2.9 | 2.9 | 2.9 | 2.6 | 1.6 | 0.7 | 0.0 | 0.0 | 0.0 | 1.5 |
| Asthma | 0.0 | 0.4 | 0.5 | 0.7 | 0.8 | 1.0 | 0.0 | 1.9 | 1.5 | 0.8 |
| Chronic obstructive pulmonary disease | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.7 | 0.0 | 1.2 | 3.9 | 0.8 |
| Malaria | 0.0 | 1.1 | 0.3 | 0.2 | 0.3 | 0.0 | 0.5 | 1.2 | 0.7 | 0.5 |
| Diarrhoeal disease | 0.0 | 0.4 | 0.8 | 0.2 | 0.3 | 0.3 | 0.0 | 0.0 | 0.5 | 0.3 |
| Liver disease | 0.0 | 0.0 | 0.5 | 0.5 | 0.0 | 0.0 | 0.5 | 0.6 | 0.2 | 0.3 |
| Diabetes mellitus | 0.0 | 0.0 | 0.3 | 0.0 | 0.0 | 0.3 | 0.5 | 0.6 | 0.2 | 0.2 |
| Malnutrition | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.7 | 0.1 |
| Anemia | 0.0 | 0.0 | 0.0 | 0.2 | 0.0 | 0.0 | 0.0 | 0.0 | 0.2 | 0.1 |
| Indeterminate | 7.7 | 7.6 | 6.5 | 6.8 | 6.0 | 5.6 | 7.9 | 11.8 | 13.3 | 8.0 |
| Total number of deaths | 104 | 276 | 384 | 425 | 364 | 304 | 216 | 161 | 412 | 2,646 |
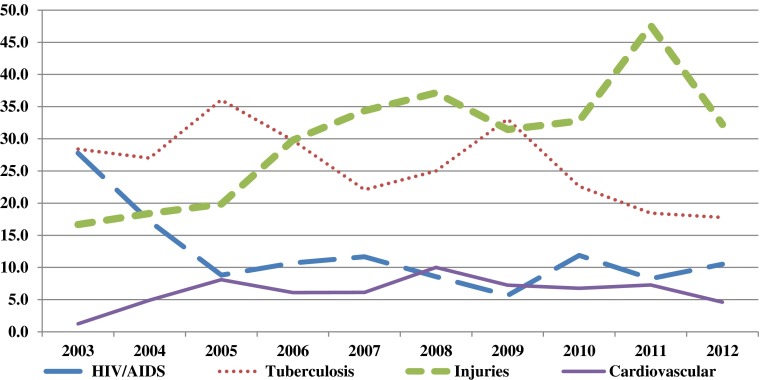
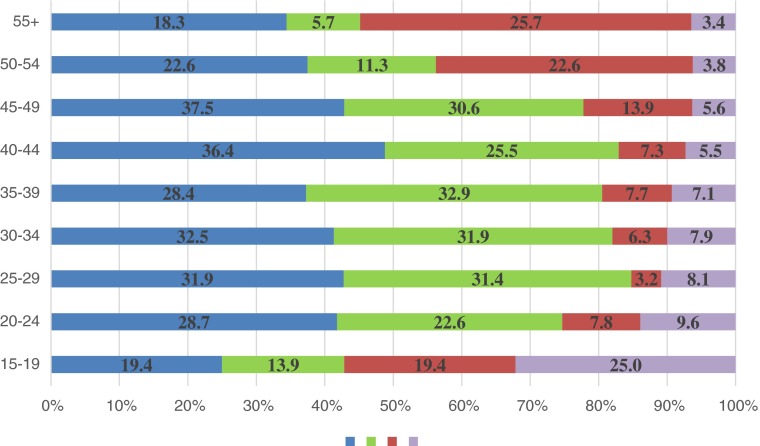
In Figs. 4 and 5, there are clear differences in cause of death between males and females over time. There is particular gender variation in deaths due to HIV/AIDS, injuries, and cardiovascular causes. Throughout the study period, there are generally twice as many deaths due to HIV/AIDS among females than males. Deaths due to injuries are about four times more likely among males than females. Additionally, the prevalence of male deaths due to injuries increases from 17 % in 2003 to 32 % in 2012, with a peak in 2011, when the proportion of male deaths due to injuries was 48 %. Among women, there is no significant variation in the prevalence of injury deaths, until 2011 when the proportion doubled to 20 % compared to the previous year. Cardiovascular deaths were consistently higher among women than men across all years, except in 2008 and 2010 when both sexes were equally likely to die from CVDs. Death due to TB had followed the same trajectory for male and female adults, rising and falling simultaneously over time, except between 2011 and 2012, where TB death shut up for women but remained unchanged for men.
FIG. 4.
Main causes of death among male NUHDSS residents age 15+ by year.
FIG. 5.
Main causes of death among female NUHDSS residents age 15+ by year.
Examined by age (Figs. 6 and 7), we find profound gender differences by age in the main causes of death. Injury accounted for an overwhelming 69 % of deaths among young men 15–19 and remained a leading cause of death among men until ages 30–34. By age 35, TB overtook injuries as a leading cause of death among men and remained so beyond age 55. While most deaths among young women aged 15–19 were linked to injury, it only accounted for 25 % of deaths among them and reduced substantially over time. For women, TB and HIV/AIDS deaths remained major causes of death across most age cohorts even at younger years. For HIV/AIDS, while we do not see its huge devastating mortality effect for males until between 30 and 34, we see evidence of high percentages of deaths among women as early as ages 20–24, and this effect continues to enlarge until ages 44–49, when we begin to see higher male than female deaths due to HIV/AIDS.
FIG. 6.
Main causes of death among males by age.
FIG. 7.
Main causes of death among females by age.
We regrouped our data into communicable, noncommunicable, and external causes of death, and the results summarized in Table 4 showed a 13 percentage point decline in deaths linked to communicable diseases over the 10-year period (declining from 66 % in 2003 to 53 % in 2012). However, we see a four-fold increase in deaths due to noncommunicable causes (from 5 % in 2003 to 21.3 % in 2012) and another two-fold increase in deaths due to external causes (injuries), increasing from 11 % in 2003 to 22 % in 2012. Tables 5 and 6 highlight a decline in deaths due to communicable causes among adolescent and adult males over the observation period and the persistence of higher prevalence among females, with an average difference of about 20 % across the period. For noncommunicable causes of death, we also see higher increases among women than men over the same period. For men, NCD deaths rose from 4 % in 2003 to 19 % in 2012, while for women, it increased from 6 % in 2003 to 25 % in 2012. However, deaths due to external causes (injuries) increased two-fold for men from 17 % in 2003 to 34 % in 2012, while it marginally increased for women from 4 % in 2003 to 5.7 % in 2012 except for the year 2011, when death due to injuries for women suddenly rose to 20 %, but declined again to 5.7 % the following year.
TABLE 4.
Causes of death among all adolescents and adults (> = 15 years), 2003–2012
| Grouped causes of death | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Communicable diseases | 65.7 | 55.5 | 56.9 | 57.7 | 49.8 | 51.3 | 51.0 | 50.7 | 40.5 | 53.1 | 53.1 |
| Non-communicable diseases | 4.8 | 7.5 | 27.0 | 19.2 | 20.9 | 20.2 | 21.4 | 20.4 | 17.6 | 21.3 | 17.5 |
| External causes | 10.6 | 12.8 | 12.9 | 20.5 | 23.2 | 25.0 | 22.9 | 24.1 | 37.2 | 22.1 | 21.3 |
| Indeterminate | 18.9 | 24.2 | 3.2 | 2.6 | 6.1 | 3.5 | 4.7 | 4.8 | 4.8 | 3.5 | 8.0 |
| Total number of deaths | 312 | 281 | 248 | 234 | 263 | 228 | 192 | 294 | 336 | 258 | 2,646 |
TABLE 5.
Causes of death among male adolescents and adults (> = 15 years), 2003–2012
| Grouped causes of death | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Communicable diseases | 57.4 | 46.6 | 53.7 | 50.4 | 41.1 | 42.1 | 46.0 | 42.9 | 32.5 | 42.1 | 44.9 |
| Non-communicable diseases | 3.7 | 9.2 | 20.6 | 15.3 | 17.2 | 16.4 | 16.9 | 19.2 | 13.1 | 19.1 | 14.9 |
| External causes | 16.7 | 19.0 | 20.6 | 30.5 | 34.4 | 37.9 | 31.5 | 33.3 | 48.1 | 33.6 | 31.1 |
| Indeterminate | 22.2 | 25.2 | 5.1 | 3.8 | 7.4 | 3.6 | 5.6 | 4.5 | 6.3 | 5.3 | 9.1 |
| Total number of deaths | 162 | 163 | 136 | 131 | 163 | 140 | 124 | 177 | 206 | 152 | 1,554 |
TABLE 6.
Causes of death among female adolescents and adults (> = 15 years), 2003–2012
| Grouped causes of death | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Communicable diseases | 74.7 | 67.8 | 60.7 | 67.0 | 64.0 | 65.9 | 60.3 | 62.4 | 53.1 | 68.9 | 64.7 |
| Non-communicable diseases | 6.0 | 5.1 | 34.8 | 24.3 | 27.0 | 26.1 | 29.4 | 22.2 | 24.6 | 24.5 | 21.3 |
| External causes | 4.0 | 4.2 | 3.6 | 7.8 | 5.0 | 4.5 | 7.4 | 10.3 | 20.0 | 5.7 | 7.4 |
| Indeterminate | 15.3 | 22.9 | 0.9 | 1.0 | 4.0 | 3.4 | 2.9 | 5.1 | 2.3 | 0.9 | 6.5 |
| Total number of deaths | 150 | 118 | 112 | 103 | 100 | 88 | 68 | 117 | 130 | 106 | 1,092 |
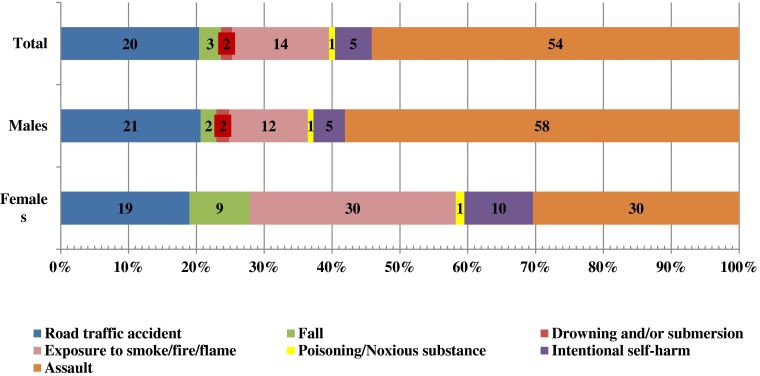
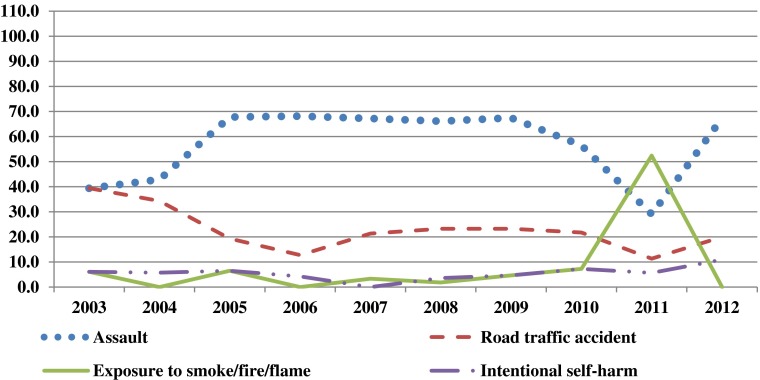
Our analysis of major causes of death due to injuries (see Fig. 8) idenified three main causes: assault (54 %), road traffic accident (20 %), and exposure to smoke/fire/flame (14 %). While we found no gender difference in deaths due to road traffic accidents, we found huge gender differences in deaths due to assault and exposure to smoke/fire/flame. While most injury deaths over the 10-year period for men are linked to assault (58 %), most injury death for women are linked to assault (30 %) and smoke/fire/flame (30 %). An interesting injury-related death more pronounced among women was death due to intentional self-harm, which accouned for 10 % of all injury deaths for women and only 5 % for men over the same period. Examined over time in Fig. 9, assault deaths remained a permanent feature on the top since 2005, except for 2011 when it dipped slightly before jerking back up to previous levels in 2012. While deaths due to road traffic accidents have remained generally stable at 20 % across time, deaths due to other forms of injuries have also remained stable over time except deaths due to exposure to smoke/fire/flame, which showed a sudden significant jump in 2011, accounting for up to 50 % of deaths that year before dropping to almost zero in 2012.
FIG. 8.
Causes of injury death among all NUHDSS residents aged 15+ between January 2003 and December 2012.
FIG. 9.
Main causes of injury death among all NUHDSS residents aged 15+ (1 January 2003 to 31 December 2012).
Examined by age, (Table 7), we find that assault-related deaths ranged from 75 % of deaths among adolescents 15–19 to 40 % among those aged 40–44. Road traffic accidents were mostly spread evenly across all ages, although it peaked among older persons 45–54 of age. Examined by gender and age simultaneously (table not shown), assault-related injury deaths were highest among men from ages 15 to 39 years, accounting for 79 % of injury deaths among young men aged 15–19 years. For women aged 15–19 and 40–44, assault deaths also accounted for 56 and 50 % of all injury deaths, respectively. Deaths linked to exposure to smoke/fire/flame peaked for men at 45–49 years of age, accounting for 19 % of deaths among the group, but linked to 55 % of deaths among women aged 20–24 and 40 % of deaths among women aged 25–29 years over the study period.
TABLE 7.
Causes of injury death among all adolescents and adults (> = 15 years), 2003–2012
| Causes of injury death | 15–19 | 20–24 | 25–29 | 30–34 | 35–39 | 40–44 | 45–49 | 50–54 | 55+ | Total (15+) |
|---|---|---|---|---|---|---|---|---|---|---|
| Assault | 75.0 | 63.9 | 55.2 | 57.6 | 47.3 | 40.0 | 32.3 | 26.7 | 21.7 | 54.2 |
| Road traffic accident | 14.3 | 15.1 | 22.4 | 21.2 | 16.4 | 25.0 | 29.0 | 46.7 | 21.7 | 20.4 |
| Exposure to smoke/fire/flame | 8.9 | 16.0 | 16.4 | 13.1 | 18.2 | 10.0 | 19.4 | 13.3 | 4.3 | 14.3 |
| Intentional self-harm | 1.8 | 2.5 | 5.2 | 4.0 | 10.9 | 17.5 | 6.5 | 0.0 | 4.3 | 5.4 |
| Fall | 0.0 | 0.0 | 0.0 | 0.0 | 5.5 | 0.0 | 9.7 | 6.7 | 47.8 | 3.2 |
| Drowning and/or submersion | 0.0 | 1.7 | 0.0 | 4.0 | 1.8 | 2.5 | 0.0 | 6.7 | 0.0 | 1.6 |
| Poisoning/Noxious substance | 0.0 | 0.8 | 0.9 | 0.0 | 0.0 | 5.0 | 3.2 | 0.0 | 0.0 | 0.9 |
| Venomous plant/animal | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Total number of injury deaths | 56 | 119 | 116 | 99 | 55 | 40 | 31 | 15 | 23 | 554 |
Discussion
We set out to present trends in causes of adult deaths in Nairobi’s informal settlements from 2003 to 2012. Our aim was to understand the main causes of adult mortality over time, which is critical not only in addressing major health concerns in this vulnerable population but also serving as a platform to link the local context to the changing nature of mortality patterns in the overarching epidemiological transitions widely reported for developing countries. Overall, we found that at the start period of our study, communicable diseases—specifically HIV/AIDS and TB—were the dominant causes of death in the study population. Overtime, however, injuries and cardiovascular conditions have become increasingly important contributors to mortality in this adult population.
Specifically, we found gender variation in deaths due to HIV/AIDS, injuries, and cardiovascular causes. Generally, there were twice as many deaths due to HIV/AIDS among females than males over the entire study period. There is conflicting evidence on gender differentials in HIV-related mortality. For example, population-based studies in the USA found significant gender differences in HIV-associated mortality both before and after ART.42–44 These differences were attributed to disparities in access to health care as well as uptake and utilization of ART. Specifically, studies from North America and Europe suggest among those on ART, more women than men die of AIDS whereas the reverse is the case in Sub-Saharan Africa.42,45–48 However, the exact mechanisms for these gender differentials remain uncertain. Some evidence suggests that men usually start ART when they have more advanced disease than women and that they tend to have higher loss to follow-up rates, both of which may lead to increased mortality.48–52 We do not have ART uptake and utilization data from our study population, and therefore, it is difficult to say exactly why more women are dying from HIV in our setting.
Our analysis identified substantial variations in causes of death by age among the urban poor. TB, HIV/AIDS, and CVD deaths were lowest among younger residents and increased with age, while injury-related deaths are highest among the youngest adults 15–19 and steadily declined with age. These findings are suggestive of the aging of people living with HIV/AIDS, following increasing access to HIV testing, care, and treatment, which have been linked to improved survival rates. Further, our analysis identified deaths related to neoplasms and respiratory tract infections (RTIs) as major causes of death, especially since 2005 and among adults 50 years and above.
We identified substantial epidemiological transitions ongoing in this local context over the observation period, with deaths linked to communicable diseases declining from 66 % in 2003 to 53 % in 2012. Conversely, we observed a four-fold increase in deaths due to noncommunicable causes from 5 % in 2003 to 21.3 % in 2012, as well as another two-fold increase in death due to external causes (injuries), increasing from 11 % in 2003 to 22 % in 2012. It is important to note that gender dimensions of the epidemiological transition are clearly visible in our study population over the obervation period. Decline in deaths due to communicable causes was more among males but remained persistent and higher among females. For noncommunicable causes of death, we also see increases among women than men over the same period. However, death due to external causes (injuries) increased two-fold for men from 17 % in 2003 to 34 % in 2012, but increased only marginally for women from 4 % in 2003 to 5.7 % in 2012 except in 2011, when death due to injuries for women suddenly rose to 20 % before it declined again to previous levels the following year.
The major causes of injury-related deaths over the study period were assault (54 %), road traffic accident (20 %), and exposure to smoke/fire/flame (14 %). The particular spike in death due to smoke/fire/flames in 2011 is intuitive, as it reflects the increasing fire hazards in the slums in recent years, particularly the Sinai pipeline fire tragedy of September 12, 2011 that killed about 100 people and left a similar number injured. The fire was linked to an explosion secondary to a fuel spill from the pipeline system operated by the state owned Kenya Pipeline Company (KPC). When the pipeline sprung a leak, people in the adjacent densely populated shanty town of Sinai had started to collect leaking fuel, when a massive explosion occurred at the scene, spreading fire across the area. Further, the high levels of assault-related deaths that stayed stable over time, especially the high incidence among young men and women aged 15–19 years calls for pointed attention.
The overall high levels of deaths from injuries may further be explained by high levels of insecurity and violence, as well as poor social infrastructure and weak legal systems (law enforcement) in the slum settings, which may contribute to significant levels of injuries from homicide and other related causes of violent injury.53 A previous study in the same slums showed that homicides accounted for 91 % of intentional injuries and 47 % of all injury-related deaths. Deaths from firearm discharge (23 %) and road traffic accidents (22 %) were the leading single causes of deaths due to injuries.54 Globally, young men are particularly vulnerable to deaths from injuries than women due to a number of reasons including but not limited to higher risk taking tendencies—overspeeding when driving, alcohol and illicit substance abuse, and higher proneness to commit violent crime.
Cardiovascular deaths were consistently higher in our results among women than men across all years. This is inconsistent with studies from industrialized societies where men have largely been shown to have a higher lifetime risk of dying from CVD than women.55 Results from the internationally acclaimed Framingham study showed that men have about twice the morbidity and mortality incidence from CVD than women and that the approximate 10-year difference between the sexes persists in mortality rates throughout the life span.56,57 For many years, it was believed that the excess mortality among men was mainly explained by unhealthy lifestyle behaviors that were more socially acceptable for men than women.58 These behaviors include tobacco use, heavy alcohol consumption, eating more red meat, among others. However, adjusting for these unhealthy lifestyle behaviors show that they contribute to but do not fully explain the increased risk of CVD in men.59 Overall, cardiovascular disease develops up to 10 years later in women than in men and is still the major cause of death in women in developed societies.57,60 It has been suggested that the risk of CVD in women is usually underestimated due to the misperception by health practitioners that women are “protected” against CVD. Also, women tend to have less typical clinical presentations of CVD. Thus, the underdiagnoses of CVD in women may have led to less aggressive intervention and potentially higher mortality.60
Limitations of the Study
Our study is limited methodologically in certain aspects. First, despite its wide use in settings where vital registration systems are weak or inadequate, the VA process has a few challenges. While showing reasonable sensitivity in identifying deaths due to common infectious diseases such as HIV and TB,61 the jury is still out on how well VA can identify noncommunicable causes, which may have less specific clinical symptoms and signs. Also, there are questions about the validity of the InterVA method of interpreting causes of death, including evidence of its low sensitivity relative to other electronic methods.20 Notwithstanding, InterVA provides a consistent and widely applicable means of interpreting VA data and has been modeled on (though not restricted to) the 2012 WHO Verbal Autopsy instrument, and hence may allow standardized interpretation and comparison of cause of death data from different international and local sources.62 Overall, it provides a cost-effective method for cause of death interpretation in comparison to other established methods such as physician review, particularly because InterVA is a free open-source software that can be used to interpret large numbers of VA deaths over a short period of time, compared to the physician coding, which is often slow and expensive. Further, InterVA is limited by the potential for misclassification of deaths, as some studies have not found strong levels of agreement between causes of death it identified and other widely used methods such as physician reviews.63,64 Additionally, the model does not provide uncertainty bounds around the cause of death estimates it generates.65 Furthermore, despite a high level of determination of causes of death, the inability of InterVA-4 to assign causes of death in about 7 % of deaths in our surveillance area is a limitation. Nevertheless, these limitations did not take away from the important role of verbal autopsy data in filling the gap created by lack of vital registration of key demographic and health events and its significant contribution to public health research, policy, and programs in developing countries. The main strength of our study is the fact that we were able to follow up a large population over a reasonably long period of time and that we captured death and cause of death information that are comparable across wide regions from a setting where vital registration is basically nonexistent. This has to be one of the greatest advantages of operating an HDSS in low-resource settings.
Conclusion
In conclusion, we found that HIV/AIDS, TB, injuries, and cardiovascular disease are linked to approximately 73 % of all adult deaths among the urban poor in Nairobi slums of Korogocho and Viwandani over the last 10 years. While the incidence of deaths related to HIV/AIDS is generally declining, we see an increasing proportion of deaths due to TB, injuries, and cardiovascular disease, which may be related to the physical environment in which people live in the slums and increasing significance of noncommunicable diseases among the urban poor. It is important to highlight the elevated levels of disadvantage of slum dwellers in our analysis relative to other population subgroups in Kenya, an outcome which is consistent with previous related studies that have demonstrated appreciable deterioration of key urban health and social indicators and reversals in favor of rural areas.66–69 For instance, HIV/AIDS and TB constitute the highest causes of death in the slums (44.2 %), while death related to HIV/AIDS and TB for all Kenya is 30.7 %.70 Injuries which cause 20.9 % of deaths in the slums are the cause of only 6.5 % of deaths nationwide. All these are legitimate grounds for a deliberate strategic focus on the health needs of the urban poor, a large and rapidly growing segment of the population, if developing country governments will achieve international goals and national health and development targets.71
Acknowledgments
The authors acknowledge funding support from the following:
• The Bill and Melinda Gates Foundation (Global Health Grant: OPP1021893).
• SIDA (Grant No. 2011–001578), and
• The William and Flora Hewlett Foundation (Grant No. 2012–7612).
References
- 1.Rao C, Lopez AD, Hemed Y. Chapter 5: disease and mortality in Sub-Saharan Africa. In: Jamison DT, editor. Causes of death. 2. Washington (DC): World Bank; 2006. [Google Scholar]
- 2.Med PS. Measuring mortality in developing countries. PLoS Med. 2006;3(2):e55–6. doi: 10.1371/journal.pmed.0030055. [DOI] [Google Scholar]
- 3.Lopez AD, Mathers CD. Measuring the global burden of disease and epidemiological transitions: 2002–2030. Ann Trop Med Parasitol. 2006;100(5–6):481–99. doi: 10.1179/136485906X97417. [DOI] [PubMed] [Google Scholar]
- 4.Mathers CD, et al. Counting the dead and what they died from: an assessment of the global status of cause of death data. Bull World Health Organ. 2005;83(3):171–7. [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. World health statistics 2007. Geneva, Switzerland: World Health Organization; 2007
- 6.Attaran A. An immeasurable crisis? A criticism of the millennium development goals and why they cannot be measured. PLoS Med. 2005;2(10):e318. doi: 10.1371/journal.pmed.0020318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.United Nations Development Programme . Beyond scarcity: power, poverty and the global water crisis. New York, NY: United Nations Development Programme; 2006. [Google Scholar]
- 8.Satterthwaite D. Health in urban slums depends on better local data. Manchester, United Kingdom: 11th International Conference on Urban Health; 2014. [Google Scholar]
- 9.Oti SO, Kyobutungi C. Verbal autopsy interpretation: a comparative analysis of the InterVA model versus physician review in determining causes of death in the Nairobi DSS. Popul Health Metrics. 2010;8(21). [DOI] [PMC free article] [PubMed]
- 10.Byass P, et al. The role of demographic surveillance systems (DSS) in assessing the health of communities: an example from rural Ethiopia. Public Health. 2002;116(3):145–50. doi: 10.1038/sj.ph.1900837. [DOI] [PubMed] [Google Scholar]
- 11.de Savigny D, Kasale H, Mbuya C, Reid G. Fixing health systems (In-Focus). Ottawa, Ontario: International Development Research Centre; 2008.
- 12.Korenromp EL, et al. Measurement of trends in childhood malaria mortality in Africa: an assessment of progress toward targets based on verbal autopsy. Lancet Infect Dis. 2003;3(6):349–58. doi: 10.1016/S1473-3099(03)00657-1. [DOI] [PubMed] [Google Scholar]
- 13.Morris SS, Black RE, Tomaskovic L. Predicting the distribution of under-five deaths by cause in countries without adequate vital registration systems. Int J Epidemiol. 2003;32(6):1041–51. doi: 10.1093/ije/dyg241. [DOI] [PubMed] [Google Scholar]
- 14.Murray CJL, Lopez AD. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. In: Murray CJL, Lopez AD, editors. Global Burden of Disease and Injury Series. The Harvard School of Public Health on behalf of the World Health Organization and the World Bank; 1996.
- 15.Baiden F, et al. Setting international standards for verbal autopsy. Bull World Health Organ. 2007;85(8):570–1. doi: 10.2471/BLT.07.043745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Soleman N, Chandramohan D, Shibuya K. Verbal autopsy: current practices and challenges. Bull World Health Organ. 2006;84(3):239–45. doi: 10.2471/BLT.05.027003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dao PB, Huong L, Van Minh H. A probabilistic approach to interpreting verbal autopsies: methodology and preliminary validation in Vietnam. Scand J Public Health. 2003;31(62):32–7. doi: 10.1080/14034950310015086. [DOI] [PubMed] [Google Scholar]
- 18.Byass P, et al. Refining a probabilistic model for interpreting verbal autopsy data. Scand J Public Health. 2006;34(1):26–31. doi: 10.1080/14034940510032202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fantahun M, et al. Assessing a new approach to verbal autopsy interpretation in a rural Ethiopian community: the InterVA model. Bull World Health Organ. 2006;84(3):204–10. doi: 10.2471/BLT.05.028712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Murray CJL, et al. Using verbal autopsy to measure causes of death: the comparative performance of existing methods. BMC Med. 2014; 12: 5. doi:10.1186/1741-7015-12-5. [DOI] [PMC free article] [PubMed]
- 21.Tensou B, et al. Evaluating the InterVA model for determining AIDS mortality from verbal autopsies in the adult population of Addis Ababa. Trop Med Int Health. 2010;15(5):547–53. doi: 10.1111/j.1365-3156.2010.02484.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kenya National Bureau of Statistics & Ministry of Planning National Development and Vision 2030. Kenya population and housing census 2009. Nairobi: Kenya National Bureau of Statistics; 2009.
- 23.United Nations Children’s Fund . The state of the world’s children 2012: children in an urban world. New York, NY: UNICEF; 2012. [Google Scholar]
- 24.African Population and Health Research Center (APHRC). Population and health dynamics in Nairobi’s informal settlements. Nairobi, Kenya: African Population and Health Research Center; 2002.
- 25.Fotso JC. Urban–rural differentials in child malnutrition: trends and socioeconomic correlates in sub-Saharan Africa. Health Place. 2007;13(1):205–23. doi: 10.1016/j.healthplace.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 26.Gould WTS. African mortality and the new ‘urban penalty’. Health Place. 1998;4(2):171–81. doi: 10.1016/S1353-8292(98)00009-4. [DOI] [PubMed] [Google Scholar]
- 27.Kenya National Bureau of Statisitics (KNBS) and ICF Macro . Kenya demographic and health survey 2008–09. Calverton, Maryland: KNBS and ICF Macro; 2010. [Google Scholar]
- 28.Warner DF, Hayward MD. Early-life origins of the race gap in men’s mortality. J Health Soc Behav. 2006;47(3):209–26. doi: 10.1177/002214650604700302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hayward MD, Gorman BK. The long arm of childhood: the influence of early-life social conditions on men’s mortality. Demography. 2004;41(1):87–107. doi: 10.1353/dem.2004.0005. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization. The second decade: improving adolescent health and development. Geneva, Switzerland: World Health Organization; 2001.
- 31.Amuyunzu-Nyamongo M, Taffa N. The triad of poverty, environment and child health in Nairobi informal settlements. J Health Popul Dev Countries. 2004; 1–14.
- 32.Taffa N, Chepngeno G, Amuyunzu-Nyamongo M. Child morbidity and healthcare utilization in the slums of Nairobi, Kenya. J Trop Pediatr. 2005;51(5):279–84. doi: 10.1093/tropej/fmi012. [DOI] [PubMed] [Google Scholar]
- 33.Kyobutungi C, et al. The burden of disease profile of residents of Nairobi’s slums: results from a demographic surveillance system. Popul Health Metrics. 2008; 6(1). [DOI] [PMC free article] [PubMed]
- 34.World Health Organization. The world health report 2004 - changing history. Geneva: World Health Organization; 2004.
- 35.Emina J, et al. Monitoring of health and demographic outcomes in poor urban settlements: evidence from the Nairobi urban health and demographic surveillance system. J U Health: Bulletin N Y Acad Med. 2011; 88(Suppl 2): S200–18. [DOI] [PMC free article] [PubMed]
- 36.Bauni E, et al. Validating physician-certified verbal autopsy and probabilistic modeling (InterVA) approaches to verbal autopsy interpretation using hospital causes of adult deaths. Popul Health Metrics. 2011; 9: 49. doi:10.1186/1478-7954-9-49. [DOI] [PMC free article] [PubMed]
- 37.Fottrell E, et al. Probabilistic methods for verbal autopsy interpretation: InterVA robustness in relation to variations in a priori probabilities. PLoS ONE. 2011;6(11):e27200. doi: 10.1371/journal.pone.0027200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mwanyangala MA, et al. Verbal autopsy completion rate and factors associated with undetermined cause of death in a rural resource-poor setting of Tanzania. Popul Health Metrics. 2011; 9: 41. doi:10.1186/1478-7954-9-41. [DOI] [PMC free article] [PubMed]
- 39.Ramroth H, et al. Cause of death distribution with InterVA and physician coding in a rural area of Burkina Faso. Tropical Med Int Health. 2012;17(7):904–13. doi: 10.1111/j.1365-3156.2012.02998.x. [DOI] [PubMed] [Google Scholar]
- 40.Vergnano S, et al. Adaptation of a probabilistic method (InterVA) of verbal autopsy to improve the interpretation of cause of stillbirth and neonatal death in Malawi, Nepal, and Zimbabwe. Popul Health Metrics. 2011; 9: 48. doi:10.1186/1478-7954-9-48. [DOI] [PMC free article] [PubMed]
- 41.Byass P. InterVA-4 user guide. 2012 [cited November 29 2013]; Available from: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=2&cad=rja&ved=0CDAQFjAB&url=http%3A%2F%2Fwww.globalhealthaction.net%2Findex.php%2Fgha%2Farticle%2FdownloadSuppFile%2F19281%2F6616&ei=yTSYUuuaHeTNygO_9IH4CA&usg=AFQjCNHwhHNsOiv6Qg9WxtQ3K8XaXm5tgg.
- 42.Hariri S, McKenna MT. Epidemiology of human immunodeficiency virus in the United States. Clin Microbiol Rev. 2007;20(3):478–88. doi: 10.1128/CMR.00006-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lemly DC, et al. Race and sex differences in antiretroviral therapy use and mortality among HIV-infected persons in care. J Infect Dis. 2009;199(7):991–8. doi: 10.1086/597124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sackoff JE, et al. Causes of death among persons with AIDS in the era of highly active antiretroviral therapy: New York city. Ann Intern Med. 2006;145(6):397–406. doi: 10.7326/0003-4819-145-6-200609190-00003. [DOI] [PubMed] [Google Scholar]
- 45.Cornell M, et al. Gender differences in survival among adult patients starting antiretroviral therapy in South Africa: a multicentre cohort study. PLoS Med. 2012;9(9):e1001304. doi: 10.1371/journal.pmed.1001304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Klausner JD, et al. Scale-up and continuation of antiretroviral therapy in South African treatment programs, 2005–2009. J Acquir Immune Defic Syndr. 2011;56(3):292–5. doi: 10.1097/QAI.0b013e3182067d99. [DOI] [PubMed] [Google Scholar]
- 47.Stenehjem E, Shlay JC. Sex-specific differences in treatment outcomes for patients with HIV and AIDS. Expert Rev Pharmacoecon Outcomes Res. 2008;8(1):51–63. doi: 10.1586/14737167.8.1.51. [DOI] [PubMed] [Google Scholar]
- 48.Stringer JS, et al. Rapid scale-up of antiretroviral therapy at primary care sites in Zambia: feasibility and early outcomes. JAMA. 2006;296(7):782–93. doi: 10.1001/jama.296.7.782. [DOI] [PubMed] [Google Scholar]
- 49.Braitstein P, et al. Gender and the use of antiretroviral treatment in resource-constrained settings: findings from a multicenter collaboration. J Womens Health (Larchmt) 2008;17(1):47–55. doi: 10.1089/jwh.2007.0353. [DOI] [PubMed] [Google Scholar]
- 50.Cornell M, et al. Temporal changes in programme outcomes among adult patients initiating antiretroviral therapy across South Africa, 2002–2007. AIDS. 2010;24(14):2263–70. doi: 10.1097/QAD.0b013e32833d45c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nglazi MD, et al. Changes in programmatic outcomes during 7 years of scale-up at a community-based antiretroviral treatment service in South Africa. J Acquir Immune Defic Syndr. 2011;56(1):e1–8. doi: 10.1097/QAI.0b013e3181ff0bdc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ochieng-Ooko V, et al. Influence of gender on loss to follow-up in a large HIV treatment programme in western Kenya. Bull World Health Organ. 2010;88(9):681–8. doi: 10.2471/BLT.09.064329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kyobutungi C, et al. The burden of disease profile of residents of Nairobi’s slums: results from a demographic surveillance system. Popul Health Metrics. 2008;6:1. doi: 10.1186/1478-7954-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ziraba AK, Kyobutungi C, Zulu EM. Fatal injuries in the slums of Nairobi and their risk factors: results from a matched case–control study. J Urban Health. 2011;88(Suppl 2):S256–65. doi: 10.1007/s11524-011-9580-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Maas AH, Appelman YE. Gender differences in coronary heart disease. Neth Heart J. 2010;18(12):598–602. doi: 10.1007/s12471-010-0841-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lerner DJ, Kannel WB. Patterns of coronary heart disease morbidity and mortality in the sexes: a 26-year follow-up of the Framingham population. Am Heart J. 1986;111(2):383–90. doi: 10.1016/0002-8703(86)90155-9. [DOI] [PubMed] [Google Scholar]
- 57.Mikkola TS, et al. Sex differences in age-related cardiovascular mortality. PLoS ONE. 2013;8(5):e63347. doi: 10.1371/journal.pone.0063347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Barrett-Connor E. Sex differences in coronary heart disease. Why are women so superior? The 1995 ancel keys lecture. Circulation. 1997;95(1):252–64. doi: 10.1161/01.CIR.95.1.252. [DOI] [PubMed] [Google Scholar]
- 59.Wingard DL, Suarez L, Barrett-Connor E. The sex differential in mortality from all causes and ischemic heart disease. Am J Epidemiol. 1983;117(2):165–72. doi: 10.1093/oxfordjournals.aje.a113527. [DOI] [PubMed] [Google Scholar]
- 60.Maas AH, Appelman YE. Gender differences in coronary heart disease. Neth Heart J. 2010;18(12):598–603. doi: 10.1007/s12471-010-0841-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Byass P, et al. InterVA-4 as a public health tool for measuring HIV/AIDS mortality: a validation study from five African countries. Glob Health Action. 2013;6:22448. doi: 10.3402/gha.v6i0.22448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Byass P, et al. Strengthening standardised interpretation of verbal autopsy data: the new InterVA-4 tool. Glob Health Action. 2012;5:1–8. doi: 10.3402/gha.v5i0.19281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lozano R, et al. Performance of InterVA for assigning causes of death to verbal autopsies: multisite validation study using clinical diagnostic gold standards. Popul Health Metrics. 2011;9:50. doi: 10.1186/1478-7954-9-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Oti SO, Kyobutungi C. Verbal autopsy interpretation: a comparative analysis of the InterVA model versus physician review in determining causes of death in the Nairobi DSS. Popul Health Metrics. 2010;8:21. doi: 10.1186/1478-7954-8-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Oti SO, et al. InterVA versus Spectrum: how comparable are they in estimating AIDS mortality patterns in Nairobi’s informal settlements? Glob Health Action. 2013;6:21638. doi: 10.3402/gha.v6i0.21638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.United Nations Human Settlements Programme (UN-HABITAT) The state of African cities 2010: governance, inequality and urban land markets. Nairobi, Kenya: United Nations Human Settlements Programme (UN-HABITAT); 2010. [Google Scholar]
- 67.United Nations Human Settlements Programme (UN-HABITAT) The state of African cities 2008: a framework for addresing urban challenges in Africa. Nairobi, Kenya: United Nations Human Settlements Programme (UN-HABITAT); 2008. [Google Scholar]
- 68.Garenne M. Migration, urbanisation and child health : an African perspective, in Africa on the move : African migration and urbanisation in comparative perspective. Johannesburg, South Africa: Wits University Press; 2006. [Google Scholar]
- 69.Ziraba A, et al. Maternal mortality in the informal settlements of Nairobi city: what do we know? Reprod Health. 2009;6(1):6. doi: 10.1186/1742-4755-6-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.The Centers for Disease Control and Prevention in Kenya (CDC-Kenya). CDC in Kenya Factsheet. 2013; Available from: http://www.cdc.gov/globalhealth/countries/kenya/pdf/kenya.pdf. Accessed 17 Sept 2014.
- 71.Mberu BU, et al. Bringing sexual and reproductive health in the urban contexts to the forefront of the development agenda: the case for prioritizing the urban poor. Matern Child Health J. 2012;18:1572–7. doi: 10.1007/s10995-013-1414-7. [DOI] [PMC free article] [PubMed] [Google Scholar]