Abstract
Intestinal parasitic infections are endemic worldwide and have been described as constituting the greatest single worldwide cause of illness and disease. The prevalence of Intestinal parasitic infections was estimated to be 5.92 %. Entamoeba coli was the most common parasite followed by Giardia lamblia and Blastocystis hominis. About 5.15 % of samples contained a single parasite and 0.76 % contained multiple parasites. In this study, the prevalence of intestinal parasites especially helminthic infections was low. The study aimed to estimate prevalence of intestinal parasites in Eghbalieh city from Qazvin Province, Iran.
Keywords: Intestinal parasites, Qazvin, Iran
Introduction
Intestinal parasitic infections (IPIs) are among the most common infections worldwide. Poverty, illiteracy, poor hygiene, lack of access to potable water and hot and humid tropical climate are the factors associated with IPIs. About one-third of the world, more than two billion people, are infected with intestinal parasites Approximately 300 million people are severely ill with these worms and of those, at least 50 % are school-age children (Mehraj et al. 2008).
At present, parasitic diseases are among the hygiene problems in Iran. With regard to social, economic, and geographical conditions of Iran and population changes, this country is an appropriate place for growth and reproduction of all kinds of parasites (Hazrati Tappeh et al. 2010).
The reason for the incidence of parasites in some parts of the country is the special climate of the region, local customs, and use of human and animal fertilizers in agriculture (Daryani et al. 2008). Studies on human parasitic infections have demonstrated a common relationship between parasitic infections and lower socioeconomic status of the region (Legesse and Berhanu 2004). Recently, in different parts of Iran, several studies have been conducted to reveal the intestinal parasites prevalence. According to literature review, there is a sharp decline in the prevalence of human helminthes infections (Mohammad et al. 1994; Meamar et al. 2007).
This research was aimed at estimating the prevalence of intestinal parasites in Eghbalieh city from Qazvin Province, Iran.
Materials and methods
This study was carried out at the Mehr clinical Laboratory in Eghbalieh city from Qazvin Province, Iran. Between April 2011 and April 2013 patients with suspected intestinal infections were referred to the Mehr Laboratory.
All specimens were examined for the presence of parasites by direct wet mount, Lugol’s iodine solution and Guide for Diagnosis of Intestinal parasite. All data (age, sex) were obtained from the main registry at the Mehr Clinical Laboratory.
Statistical analysis
The software, SPSS Version 9.0 for Windows (SPSS Inc., Chicago, IL, USA), was used for analysis. Differences were evaluated using the Chi squared test. Differences were considered significant when P < 0.05.
Results
Prevalence of intestinal parasitic infections (IPIs)
A total of 5,743 patients with suspected intestinal parasites were referred to the Mehr Clinical Laboratory including 4,056 males(70.62) and 1,687 females (29.37 %) and majority aged between 31 and 40 years (39.99 %, 2,297/5,743). Referred patients were laboratory diagnosed with one or more intestinal parasites over the study period.
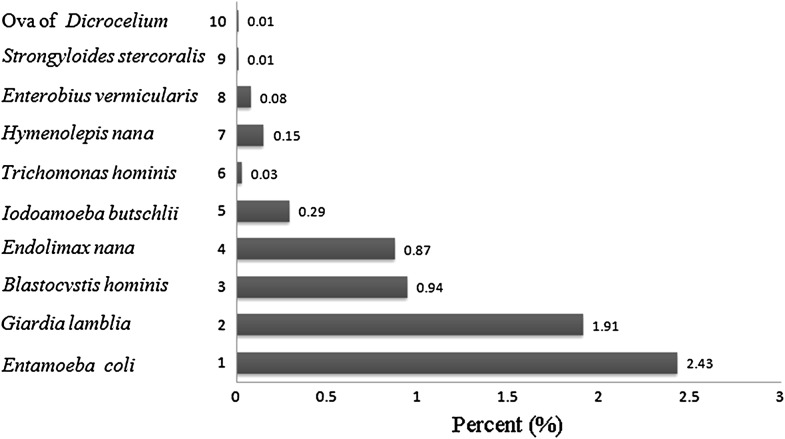
The overall prevalence of the IPIs was estimated at 5.92 %. 340 positive out of 5,743. About 5.15 % of samples contained a single parasite and 0.76 % contained multiple parasites (Table 2). Entamoeba coli, being the most common IP, was present in 140 samples (2.43 %) followed by Giardia lamblia present in 110 samples (1.91 %), Blastocystis hominis in 54 samples (0.94 %), Endolimax nana in 50 samples (0.87 %), Iodoamoeba butschlii in 17 samples (0.29 %), Trichomonas hominis in 2 samples (0.03 %), Hymenolepis nana in 9 samples (0.15 %), Enterobius vermicularis in 5 samples (0.08 %), larva of Strongyloides stercoralis in 1 samples (0.01 %) and ova of Dicrocelium (0.01 %) was identified in 1 stool sample (Tables 1, 2). No statistically significant difference was found between intestinal parasites and sex (P > 0.05). Distribution of intestinal parasites according to age groups is shown in Table 3. Prevalence of B. hominis and G. lamblia were higher in the younger than the older population. The prevalence of other parasites was relatively equal across all age groups.
Table 2.
The parasites distribution of the study population (multiple)
| Male | Female | Overall prevalence | |
|---|---|---|---|
| No. (%) | No. (%) | No. (%) | |
| Protozoans | |||
| Entamoeba coli + Endolimax nana | 9 (0.22) | 6 (0.35) | 15 (0.26) |
| Entamoeba coli + Giardia lamblia | 11 (0.27) | 0 (0.00) | 11 (0.19) |
| Entamoeba coli + Blastocystis hominis | 6 (0.14) | 2 (0.11) | 8 (0.13) |
| Entamoeba coli + Giardia lamblia + Endolimax nana | 5 (0.12) | 0 (0.00) | 5 (0.08) |
| Blastocystis hominis + Iodoamoeba butschlii | 3 (0.07) | 2 (0.11) | 5 (0.08) |
| Total | 44 (0.76) | ||
Table 1.
The parasites distribution of the study population (single)
| Male | Female | Overall prevalence | |||
|---|---|---|---|---|---|
| No | % | No | % | No (%) | |
| Protozoans | |||||
| Entamoeba coli | 71 | 1.75 | 30 | 1.77 | 101 (1.75) |
| Giardia lamblia | 73 | 1.79 | 21 | 1.24 | 94 (1.63) |
| Blastocystis hominis | 26 | 0.61 | 15 | 0.88 | 41 (0.71) |
| Endolimax nana | 19 | 0.46 | 11 | 0.65 | 30 (0.52) |
| Iodoamoeba butschlii | 7 | 0.17 | 5 | 0.29 | 12 (0.20) |
| Trichomonas hominis | 1 | 0.02 | 1 | 0.05 | 2 (0.03) |
| Helminth | |||||
| Hymenolepis nana | 8 | 0.19 | 1 | 0.15 | 9 (0.15) |
| Enterobius vermicularis | 3 | 0.07 | 2 | 0.11 | 5 (0.08) |
| Larva of Strongyloides stercoralis | 1 | 0.02 | 0 | 0.00 | 1 (0.01) |
| Ova of Dicrocelium | 1 | 0.02 | 0 | 0.00 | 1 (0.01) |
| Total | 296 (5.15) | ||||
Table 3.
The parasites distribution of the study population by age
| Age | No. | Entamoeba coli | Giardia lamblia | Blastocystis hominis | Endolimax nana | Iodoamoeba butschlii | Trichomonas hominis | Hymenolepis nan | Enterobius vermicularis | Larva of Strongyloides stercoralis | Ova of Dicrocelium |
|---|---|---|---|---|---|---|---|---|---|---|---|
| <11 | 229 | 8 (3.49) | 14 (6.11) | 11 (4.80) | 5 (2.18) | 3 (1.31) | 0 (0.00) | 1 (0.43) | 5 (2.18) | 0 (0.00) | 0 (0.00) |
| 11–20 | 516 | 7 (1.35) | 10 (1.93) | 5 (0.96) | 7 (1.35) | 2 (0.38) | 0 (0.00) | 1 (0.19) | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| 21–30 | 1,435 | 34 (2.36) | 16 (1.11) | 11 (0.76) | 14 (0.97) | 3 (0.20) | 2 (0.13) | 2 (0.13) | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| 31–40 | 2,297 | 66 (2.87) | 44 (1.91) | 20 (0.87) | 20 (0.87) | 8 (0.34) | 0 (0.00) | 2 (0.08) | 0 (0.00) | 1 (0.04) | 1 (0.04) |
| 41–50 | 861 | 13 (1.50) | 16 (1.85) | 4 (0.46) | 2 (0.23) | 0 (0.00) | 0 (0.00) | 2 (0.23) | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| >50 | 405 | 12 (2.96) | 10 (2.46) | 3 (0.74) | 2 (0.49) | 1 (0.24) | 0 (0.00) | 1 (0.24) | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| Total | 5,743 | 140 (2.43) | 110 (1.91 %) | 54 (0.94 %) | 50 (0.87 %) | 17 (0.29 %) | 2 (0.03 %) | 9 (0.15 %) | 5 (0.08 %) | 1 (0.01 %) | 1 (0.01 %) |
In addition, a statistically significant difference was found in age group among patients infected with G. lamblia (P < 0.05). In contrary, no statistically significant difference was found between age among patients infected with other parasite (P > 0.05).
Discussion
The current study was performed to estimate the frequency of the parasitic infection during 2011–2013 in Eghbalieh city from Qazvin Province, Iran. Knowing this issue is necessary to design a prevention and control program.
The present study showed that about 5.92 % of people in this study were carriers of one or more of intestinal parasites. Prevalence of intestinal parasites vary in different parts of Iran, with 10.7 % reported from Tehran (Capital of Iran) (Shojae Arani et al. 2008), 4.7 % in Karaj (Nasir et al. 2009), 61 % in Yazd (Central of Iran) (Firoozabadi and Azizi 2003), 56.6 % in Qazvin (North of Iran) (Mahyar et al. 2000). Socio-economic, geographic, sanitary/hygienic, cultural, and nutritional factors may contribute to the fact that the prevalence of intestinal parasites in Iran.
The rate of contamination with intestinal worms was 0.27 % and contamination with intestinal protozoa was 5.64 %. The most common intestinal parasite were E. coli 2.43 % and G. lamblia 1.91 %, respectively (Tables 1, 2). This result was similar to other studies carried out in Iran (Badparva et al. 2009; Haghighi et al. 2009). E. coli and G. lamblia and B. hominis infections are related to ingestion of food or water contaminated by faeces, and are confirmed as the most frequent parasites among underprivileged people (Gualdieri et al. 2011). Although we did not investigate the risk factors which may affect their transmission, we believe that factors including, sanitation conditions of soil, food/water and relatively low neighborhood socioeconomic status of the area are highly correlated with prevalence of these parasites in the study area (see Fig. 1).
Fig. 1.
The parasites distribution of the study population
Our results showed that helminth parasites were lower than protozoan parasites. However, it is recommended that clinicians should consider this parasitic infection. Relatively low incidences of intestinal parasites especially helminthic infections achieved in this study is in accordance with the fact that in general the prevalence of intestinal worms appears to be becoming rarer in Iran (Rokni 2008).
Studies have shown that the prevalence of intestinal parasitic infection is higher in younger people, especially children (Hellard et al. 2000). For instance, in a large study of IPIs in Iran found children aged 2–14 years with a high prevalence of 25 % (Sayyari et al. 2005). In this study, the prevalence of intestinal parasites were found to be higher among young people than older people. The prevalence of G. lamblia was found to be higher among younger children than older people. Children infected with G. lamblia are mostly asymptomatic and can spread the infection to other children or even within their homes and may contribute to high epidemic rates in their communities (Hill 2007).
The prevalence of IPIs was slightly higher in males than females, more or less a similar patterns were previously observed in studies from Iran including these from Kerman, Shahre-kord, Tehran (Shojae Arani et al. 2008). The most probable explanation for the high infection rate in male in our study could be large numbers of male than females that were referred to the Mehr Clinical Laboratory.
In conclusion, according to our results the frequency of intestinal parasites was low. It seems that the low infection is due to progress in public health sanitation in Eghbalie from Qazvin Province, Iran.
References
- Badparva E, Fallahi Sh, Birjandi M, Pournia Y, Kayedi MH. Prevalence of intestinal parasites in the rural regions of Kouhdasht, Lorestan Province, Iran 2008. Asian J Biol Sci. 2009;2(4):105–111. doi: 10.3923/ajbs.2009.105.111. [DOI] [Google Scholar]
- Daryani A, Ettehad GH, Sharif M, Ghorbani L, Ziaei H. Prevalence of intestinal parasites in vegetables consumed in Ardebil, Iran. Food Control. 2008;19(8):790–794. doi: 10.1016/j.foodcont.2007.08.004. [DOI] [Google Scholar]
- Firoozabadi AA, Azizi M. Prevalence of intestinal parasitic infections among fast-food restaurant workers in Yazd. J Shahid Sadoghi Univ Med Sci. 2003;1:29–33. [Google Scholar]
- Gualdieri L, Rinaldi L, Petrullo L, Morgoglione ME, Maurelli MP, Musella V, Piemonte M, Caravano L, Coppola MG, Cringoli G. Intestinal parasites in immigrants in the city of Naples (Southern Italy) Acta Trop. 2011;117:196–201. doi: 10.1016/j.actatropica.2010.12.003. [DOI] [PubMed] [Google Scholar]
- Haghighi A, Salimi Khorashad A, Nazemalhosseini Mojarad E, Kazemi B, Rostami Nejad M, Rasti S. Frequency of enteric protozoan parasites among patients with gastrointestinal complains in medical centers of Zahedan, Iran. Trans R Soc Trop Med Hyg. 2009;103(5):452–454. doi: 10.1016/j.trstmh.2008.11.004. [DOI] [PubMed] [Google Scholar]
- Hazrati Tappeh KH, Mohammadzadeh H, Nejad Rahimi R, Barazesh A, Khashaveh SH, Taherkhani H. Prevalence of Intestinal parasitic infections among mentally disabled children and adults of Urmia, Iran. Iran J Parasitol. 2010;5(2):60–64. [PMC free article] [PubMed] [Google Scholar]
- Hellard ME, Sinclair MI, Hogg GG, Fairley CK. Prevalence of enteric pathogens among community based asymptomatic individuals. J Gastroent Hepat. 2000;3:290–293. doi: 10.1046/j.1440-1746.2000.02089.x. [DOI] [PubMed] [Google Scholar]
- Hill . Giardia lamblia. In: Mandell GL, Bennett JE, Dolin R, editors. Principles and practice of infectious diseases. 6. New York: Churchill Livingstone; 2007. pp. 2888–2893. [Google Scholar]
- Legesse M, Berhanu E. Prevalence of intestinal parasites among schoolchildren in a rural area close to the southeast of Lake Langano, Ethiopia engistu. Ethiop J Health Dev. 2004;18:116–121. [Google Scholar]
- Mahyar A, Daneshi kohan MM, Saghafi H, Rezaie M. Intestinal parasitic infections among disabled children in Qazvin. J Qazvin Univ Med Sci. 2000;2:64–67. [Google Scholar]
- Meamar AR, Rezaian M, Mohraz M, Zahabiun F, Hadighi R, Kia EB. A comparative analysis of intestinal parasitic infections between HIV+/AIDS patients and non-HIV infected individuals. Iran J Parasitol. 2007;2:1–6. [Google Scholar]
- Mehraj V, Hatcher J, Akhtar S, Rafique G, Asim Beg M. Prevalence and factors associated with intestinal parasitic infection among children in an Urban slum of Karachi. PLoS ONE. 2008;3(11):e3680. doi: 10.1371/journal.pone.0003680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammad K, Zalie MR, Shadrokh S, Masjedi MR. Intestinal parasites in Iran. Iran J Public Health. 1994;24:9–26. [Google Scholar]
- Nasir M, Esmailnia K, Karim G, Nasiri M, Omid Akhavan. Intestinal parasitic infections among inhabitants of Karaj City, Tehran Province, Iran in 2006–2008. Korean J Parasitol. 2009;47(3):265–268. doi: 10.3347/kjp.2009.47.3.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rokni MB. The present status of human helminthic diseases in Iran. Ann Trop Med Parasitol. 2008;102(4):29–283. doi: 10.1179/136485908X300805. [DOI] [PubMed] [Google Scholar]
- Sayyari AA, Imanzadeh F, Bagheri yazdi SA SA, Karami H, Yaghoobi M. Prevalence of intestinal parasitic infections in the Islamic Republic of Iran. East Mediterr Hlth J. 2005;11:377–383. [PubMed] [Google Scholar]
- Shojae Arani A, Alaghehbandan R, Akhlaghi L, Shahi M, Rastegar Lari A. Prevalence of intestinal parasites in a population in south of Tehran, Iran. Rev Inst Med Trop S Paulo. 2008;50(3):145–149. doi: 10.1590/s0036-46652008000300003. [DOI] [PubMed] [Google Scholar]