Abstract
Toxocariasis remains a problem throughout the world, and the overall prevalence is estimated to be 2.8 % within the United States. The clinical spectrum of toxocariasis in humans varies from asymptomatic infection to severe organ injury, and is determined by parasitic load, sites of larval migration from the gut, and the host’s inflammatory response. We present a case of eosinophilic ascites with diarrhea in a post-partum woman attributed to toxocariasis. To our knowledge, this is the first reported case of toxocara infection presenting in the post-partum period.
Keywords: Toxocara, Eosinophilia, Post-partum
Introduction
Toxocariasis remains a problem throughout the world, and may induce a multisystem disease known as visceral larva migrans in young individuals. Within the United States, the overall prevalence is estimated to be 2.8 %. Higher seroprevalence has been linked to markers of low socioeconomic status, poverty, crowding, and lower educational level (Won et al. 2008). We present a case of eosinophilic ascites with diarrhea in a post-partum woman attributed to toxocariasis. To our knowledge, this is the first reported case of Toxocara infection presenting in the post-partum period.
Case report
A 25-year-old previously healthy African American female was admitted to our academic medical center with generalized abdominal pain, nausea, vomiting and non-bloody diarrhea for 4 weeks. She had given birth to a boy via spontaneous vaginal delivery without complications 7 weeks prior. Upon presentation, she denied fever, chills, rashes or cough and had no sick contacts or pets at home. She also denied any history of drug use.
Past medical history was remarkable for an allergy to milk since the age of 17 with lip swelling and hives. The patient had been taking levothyroxine for hypothyroidism for many years, and had not taken any new medications prior to admission. She was born and raised in New York City, and had been to the Dominican Republic 6 years prior to admission; during that trip, she had walked barefoot on multiple occasions and swam in a freshwater river.
On physical examination, she was afebrile with normal vital signs, she had a distended abdomen with a fluid wave and mild generalized tenderness. There were no stigmata of chronic liver disease. Laboratory testing revealed significant peripheral eosinophilia of 41 % (absolute count, 5,740 cells/μL) with total white blood cell count of 14,000/mL. The patient’s total serum IgE was 849 U/mL. Abdominal CT scan with intravenous and oral contrast showed diffuse bowel wall thickening and distended loops of small bowel with extensive free peritoneal fluid. The patient subsequently had an upper endoscopy, and biopsy revealed chronic gastritis with numerous eosinophils in the duodenum, jejunum, and stomach. Stool ova and parasite testing was negative, and the patient was seronegative for Strongyloides and HIV. She was initially discharged from the hospital after conservative treatment for presumed small bowel obstruction, but her symptoms persisted and she came back to the hospital after 3 days.
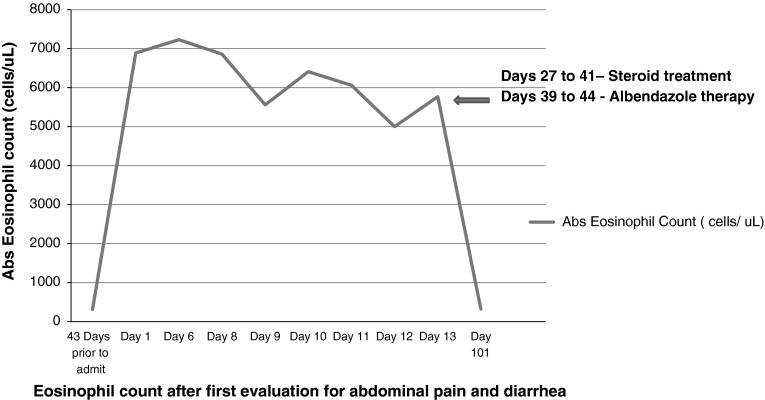
Paracentesis was performed, and the ascitic fluid demonstrated a serum-ascites albumin gradient of 0.7, and 8640 WBCs with 94 % eosinophils. She was started on Prednisone 40 mg per day, and discharged home. Toxocara enzyme-linked immunosorbent assay (ELISA) came back positive at which point she was started on albendazole 400 mg twice daily for 5 days. Ocular exam did not reveal toxocara. With treatment her symptoms improved significantly and the prednisone was tapered over 3 weeks. The total serum IgE decreased to 196 U/mL. Following the administration of steroid therapy, the patient experienced complete resolution of symptoms and peripheral eosinophilia (Fig. 1). She has not relapsed after 16 months of follow-up, and the level of eosinophils remains normal.
Fig. 1.
Eosinophil count after first evaluation for abdominal pain and diarrhea
Discussion
The clinical spectrum of toxocariasis in humans varies from asymptomatic infection to severe organ injury, and is determined by parasitic load, sites of larval migration from the gut, and the host’s inflammatory response. Possible sources of infection include fecal-oral contamination of eggs in cat or dog feces, or fecally-contaminated vegetables (radishes, carrots) or undercooked meat from infected chickens, sheep, lambs or calves (Vázquez Tsuji and Martínez Barbabosa 1997). Gastrointestinal manifestations of toxocariasis correlate with the layer of gastrointestinal tract invaded by the migrating larvae. Mucosal and muscular involvement may be associated with diarrhea, weight loss, abdominal pain, and vomiting. Serosal infiltration results in exudative ascites, which is often eosinophilic as in our patient. There are 5 case reports of eosinophilic ascites related to toxocara but none in a post-partum female.
The variable clinical manifestations of toxocariasis often lead to diagnostic and therapeutic delays. Viable Toxocara larvae may persist in tissues and excrete and/or secrete antigens for several years so infection may have been remote. In dogs, pregnancy is a risk factor for disease activation; a similar phenomenon may have occurred in our patient. The diagnosis of visceral toxocariasis is often based on clinically suggestive disease and exposure history with positive results by serological testing. The recommended test is ELISA with larval stage antigens. Seropositivity can also be present in asymptomatic Toxocara infection, therefore serial serum samples demonstrating a significant rise in antibody levels over time is useful in confirming active infection. Albendazole is the treatment of choice for toxocariasis. In case of severe respiratory, myocardial or liver involvement, concomitant prednisone (0.5–1 mg/kg day) is often utilized (Hotez 2009). Good hygiene practices, timely disposal of pet feces, and routine deworming of pets are important strategies for the prevention of Toxocara infection.
In summary, we present a rare case of eosinophilic ascites in the setting of Toxocara infection in a post-partum patient. The early recognition of toxocariasis may be essential to prevent potential visceral complications. Therefore, a high index of suspicion should be maintained in any patient presenting with eosinophilia.
References
- Hotez PJ. Toxocara canis. In: Burg FD, Wald ER, Ingelfinger JR, Polin PA, editors. Gellis and Kaganís current pediatric therapy. 15. Philadelphia: W. B. Saunders; 2009. pp. 683–684. [Google Scholar]
- Vázquez Tsuji O, Martínez Barbabosa I. Vegetables for human consumption as probable source of Toxocara sp. infection in man. Bol Chil Parasitol. 1997;52(3–4):47–50. [PubMed] [Google Scholar]
- Won KY, Kruszon-Moran D, Schantz PM, Jones JL. National seroprevalence and risk factors for Zoonotic Toxocara spp. infection. Am J Trop Med Hyg. 2008;79:552. [PubMed] [Google Scholar]