Abstract
Human dirofilariasis is an uncommon zoonotic infection having a widespread geographical distribution. World over 800 cases of Dirofilaria are on record with highest numbers from Italy, Sri Lanka and republics of the ex-Soviet Union. Dirofilaria repens belongs to the subgenus Nochtiella and is the most common species identified in India. Topographically, the orbital/periorbital regions are the most common regions involved by Dirofilaria. We present a brief review of cases from India including two received in our own institute. This review focuses on the epidemiology of the disease including its geographical distribution and the probable causation of the recent increase in its incidence in Indian subcontinent.
Keywords: Dirofilaria, Dirofilaria repens, Subcutaneous dirofilariasis, India, Epidemiology, Zoonosis
Introduction
Dirofilaiasis is an uncommon zoonotic disease where man is the dead end host. Among nearly forty species of Dirofilaria identified, only a few give rise to human infection. There are two forms of the disease—(a) pulmonary dirofilariasis caused primarily by Dirofilaria immitis (the dog heartworm), and (b) subcutaneous dirofilariasis caused primarily by Dirofilaria tenuis and Dirofilaria repens, parasites of the raccoon and of dogs and cats respectively. In rare instances the parasite has also been recovered from deeper locations of peritoneal cavity, omentum, ligaments, breast and liver (Padmaja et al. 2005; Orihel and Eberhard 1998; Mrad et al. 1999; Kim et al. 2002).
Dirofilaria repens is the commonest species identified in India. It belongs to the subgenus Nochtiella. Transmission to humans is via the bite of zoo-anthropophilic vector—the mosquito of the Anopheles, Aedes and Culex species. Clinically infection is apparent as a solitary subcutaneous nodule commonly in the head and neck region with or without pain. Identifying its characteristic longitudinal cuticular ridges by wet mount study or histopathological examination in conjunction with the typical clinical features is usually sufficient for diagnosis in most of the cases (Orihel and Eberhard 1998; Khurana et al. 2010).
Case reports
Case 1
A 37 year old female a resident of Karnataka presented with a slowly enlarging mass over the left side of the neck for 2 months. The mass was preceeded by symptoms of itching, pain and fever. The mass measured 1.5 cm × 1 cm, was irregular, freely mobile and firm in consistency. The lesion was nontender and there was no local rise of temperature. Ultrasonography showed an oval hypoechoic lesion, 8 mm × 5 mm with tubular hyperechoic structure in the subcutaneous plane suggestive of inflammatory swelling due to parasitic infestation. The nodule was excised and the worm was delivered out of the cystic lesion. The worm measured 11.5 cm in length and was identified as D. repens (Fig. 1).
Fig. 1.

Wet mount of the worm showing characteristic longitudinal cuticular ridges
Case 2
A 40 year old male, resident of Dakshina Kannada district of coastal Karnataka presented with swelling of the right upper eyelid for 2 weeks. On examination the swelling was associated with periorbital edema and tenderness. Computed tomographic scan suggested an inflammatory/malignant mass. The excised mass consisted of an irregular grey pink nodule measuring about 1 cm × 0.8 mm. Cut section showed a whitish centre. Microscopy revealed several cross-sections of a slightly degenerated worm showing the cuticular and internal structures (Fig 2).
Fig. 2.
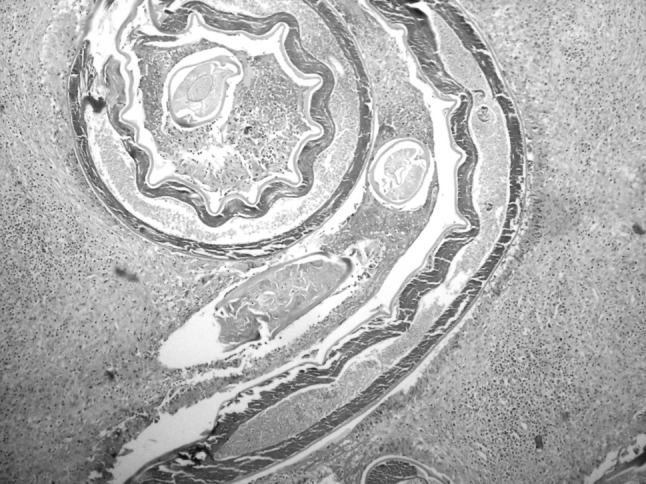
Photomicrograph of the slightly degenerated worm showing the multilayered cuticle, longitudinal ridges and the genital tube. H&E original magnification 40×
Discussion
Dirofilaria has widespread geographical distribution with cases recorded from over 30 countries. It has endemic foci in Southern and Eastern Europe, Asia Minor, Central Asia and Sri Lanka. World over around 800 cases of Dirofilaria are on record (Pampiglione et al. 1995, 1982; Pampiglione and Rivasi 2000).
Dirofilaria species isolated from humans are divided into two subgenera: Dirofilaria, with D. immitis as the type species, and Nochtiella, with D. repens as its type species. Nematodes in the former, have a smooth cuticle and are typically found in pulmonary arteries, whereas those in the latter (D. repens, D. ursi, D. tenuis and D. striata) exhibit longitudinal cuticular ridges and are usually found in subcutaneous tissues. Epidemiologically, the species recovered, depend upon the geographical location (Orihel and Eberhard 1998).
Dirofilaria is relatively rare in India with approximately 73 on record since 1977. Dirofilaria repens is the commonest species identified followed by D. immitis and D. tenius (Joseph et al. 1976; Bhat et al. 2003, 2012; Teerthanath and Hariprasad 2011; Badhe and Sane 1989; Senthivel and Pillai 1999). Two cases of D. repens were identified in our institute (Table 1).
Table 1.
Case reports of Dirofilaria in India with epidemiological details
| Case No. | Author | Area | Location | Age | Sex | Worm sex | Number of worms | Length of the worm in cm | Species |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Joseph et al. (1976) | Kera | Conjb | 60 | F | F | 1 | NMc | D. repens |
| 2 | (Badhe and Sane 1989) | Mahad | Pulmonary | Child | NM | NM | NM | NM | D. immitis |
| 3 | (Senthivel and Pillai 1999) | Ker | SCe | NM | NM | NM | NM | NM | NM |
| 4 | Sekhar et al. (2000) | Ker | Eyelid | 26 | F | NM | 2 | 10.5 and 5 | NM |
| 5 | Nadgir et al. (2001) | Karf | Conj | 42 | M | M | 1 | 3.5 | D. repens |
| 6 | Gautam et al. (2002) | Haryana | Sub conj | 23 | M | M | 1 | 8.3 | D. repens |
| 7 | Ittyerah and Mallik (2004) | Ker | Eyelid | 14 | F | F | 1 | 10 | D. repens |
| 8 | Bhat et al. (2003) | NM | Eyelid | 70 | F | NM | 1 | 12 | D. tenius |
| 9 | Padmaja et al. (2005) | TN | Lip | 35 | M | F | 1 | 12.5 | D. repens |
| 10 | Mahesh et al. (2005) | Asian | Eyelid | 78 | F | F | 1 | 10 | D. repens |
| 11 | Sathyan et al. (2006) | Ker | Subtenon | 63 | F | F | 1 | 9.5 | D. repens |
| 12–20 | Sabu et al. (2005) | Ker | 9 Eye | NM | NM | 11 F | Single | 9–13.5 | D. repens |
| 21–23 | Sabu et al. (2005) | Ker | 3 SC | NM | NM | 1 M | 1 | 6 | D. repens |
| 24 | Smitha et al. (2008) | Ker | Eyelid | 40 | F | NM | 1 | 13.5 | D. repens |
| 25 | Raju et al. (2008) | Ker | Eyelid | 33 | F | NM | 1 | 9 | D. repens |
| 26 | Raju et al. (2008) | Ker | Eyelid | 46 | F | NM | 1 | 8 | NM |
| 27 | (Dhar and Nambiar 2008) | Ker | Limbus | 24 | F | F | 1 | 10.5 | NM |
| 28 | (Chakrabarti et al. 2009) | Ker | Sub Conj | 60 | F | NM | 1 | D tenius | |
| 29 | Singh et al. (2010) | Orissa | Scrotum | 40 | M | F | 1 | 10.5 | D. repens |
| 30 | Nath et al. (2010) | Assam | Eyelid | 23 | F | F | 1 | 12 | D. repens |
| 31 | Nath et al. (2010) | NM | Eyelid | 30 | M | F | 1 | 13 | D. repens |
| 32 | Nath et al. (2010) | NM | Conj | 70 | M | F | 1 | 12 | D. repens |
| 33 | Khurana et al. (2010) | Kar | AB Wallg | 16 | M | F | 1 | 9 | D. repens |
| 34 | Khurana et al. (2010) | Maha | Cheek | 45 | M | F | 1 | 8 | D. repens |
| 35 | Khurana et al. (2010) | Maha | Eyelid | 15 | F | F | 1 | 11.5 | D. repens |
| 36 | (Joseph et al. 2011a, b) | Ker | Face | 53 | F | NM | 1 | NM | D. repens in 17 cases |
| 37 | (Joseph et al. 2011a, b) | Ker | Chest | 60 | F | NM | 1 | NM | D. repens in 17 cases |
| 38 | (Joseph et al. 2011a, b) | Ker | Cheek R | 45 | F | NM | 1 | NM | D. repens in 17 cases |
| 39 | (Joseph et al. 2011a, b) | Ker | Arm | 19 | F | NM | 1 | NM | D. repens in 17 cases |
| 40 | (Joseph et al. 2011a, b) | Ker | AB wall | 1 | M | NM | 1 | NM | D. repens in 17 cases |
| 41 | (Joseph et al. 2011a, b) | Ker | Canthus | 27 | M | NM | 1 | NM | D. repens in 17 cases |
| 42 | (Joseph et al. 2011a, b) | Ker | Flank | 65 | M | NM | 1 | NM | D. repens in 17 cases |
| 43 | (Joseph et al. 2011a, b) | Ker | Thigh | 28 | F | NM | 1 | NM | D. repens in 17 cases |
| 44 | (Joseph et al. 2011a, b) | Ker | Neck | 48 | M | NM | 1 | NM | D. repens in 17 cases |
| 45 | (Joseph et al. 2011a, b) | Ker | AB wall | 34 | F | NM | 1 | NM | D. repens in 17 cases |
| 46 | (Joseph et al. 2011a, b) | Ker | Arm | 35 | F | NM | 1 | NM | D. repens in 17 cases |
| 47 | (Joseph et al. 2011a, b) | Ker | Inguinal | 38 | F | NM | 1 | NM | D. repens in 17 cases |
| 48 | (Joseph et al. 2011a, b) | Ker | Arm | 22 | F | NM | 1 | NM | D. repens in 17 cases |
| 49 | (Joseph et al. 2011a, b) | Ker | Axilla | 14 | M | NM | 1 | NM | D. repens in 17 cases |
| 50 | (Joseph et al. 2011a, b) | Ker | Chest | 25 | M | NM | 1 | NM | D. repens in 17 cases |
| 51 | (Joseph et al. 2011a, b) | Ker | Neck | 56 | F | NM | 1 | NM | D. repens in 17 cases |
| 52 | (Joseph et al. 2011a, b) | Ker | Chest wall | 50 | M | NM | 1 | NM | D. repens in 17 cases |
| 53 | (Joseph et al. 2011a, b) | Ker | Nasolabial | 10 | F | NM | 1 | NM | D. repens in 17 cases |
| 54 | (Joseph et al. 2011a, b) | Ker | Parotid | 39 | F | NM | 1 | NM | D. repens in 17 cases |
| 55 | (Joseph et al. 2011a, b) | Ker | Epididymis | 1 | M | NM | 1 | NM | D. repens in 17 cases |
| 56 | (Joseph et al. 2011a, b) | Ker | Infraorbit | 24 | F | NM | 1 | NM | D. repens in 17 cases |
| 57 | (Teerthanath and Hariprasad 2011) | Ker | Muscle | 27 | M | M | 1 | 16 | D. immitis |
| 58 | Kotian et al. (2011) | Supra orbit | 52 | F | F | 1 | D. repens | ||
| 59 | Kotian et al. (2011) | Below eyelid | 34 | F | 1 | D immitis | |||
| 60 | Permi et al. (2011) | Ker | Cheek | 40 | M | F | 1 | NM | D. repens |
| 61 | Permi et al. (2011) | Ker | Neck | 45 | M | NM | 1 | NM | D. repens |
| 62 | (Joseph et al. 2011a, b) | Ker | Orbit | 50 | F | F | 1 | 12.5 | D. repens |
| 63 | Sanjeev et al. (2011) | Ker | Neck | 18 | F | F | 1 | 9 | NM |
| 64 | Kotigadde et al. (2012) | Kar | Eyelid | 47 | F | F | 1 | 10 | D. repens |
| 65 | Chopra et al. (2012) | Bihar | Ant.h Chamber | 25 | M | F | 1 | 10 | NM |
| 66 | Bhat et al. (2012) | NM | Conjun | 75 | M | NM | 1 | NM | D. tenius |
| 67 | (Vaidya and Srikar 2012) | NM | AB wl | 30 | F | F | 1 | NM | D. repens |
| 68 | (Sangit and Haldipurkar 2012) | NM | Conjuc | 48 | M | F | 2 | 3.5 cm | D. repens |
| 69 | Mukherjee et al. (2012) | Asian | Eyelid | 61 | M | NM | 1 | NM | NM |
| 70 | (Srinivasamurthy et al. 2012) | Indian | Neck | 40 | F | F | 1 | NM | NM |
| 71 | Sahdev et al. (2012) | Maha | Eye lid | 3 | M | NM | 1 | NM | D. repens |
| 72 | Case 1* | Kar | Neck | 35 | F | F | 1 | D. repens | |
| 73 | Case 2* | Kar | Eyelid | 45 | M | NM | 1 | D. repens |
M Male, F Female
* Cases received in our institute (unpublished)
aKerala
bConjunctiva
cNot mentioned
dMaharashtra
eSubcutaneous
fKarnataka
gabdominal
hAnterior chamber
Dirofilaria repens is the most prevalent agent of zoonotic dirofilariasis in many parts of the world including Africa, Canada, Japan Kuwait France, Italy, Turkey, Africa, Thailand, USA and Southeast Asia (Athari 2003; Sekhar et al. 2000).
Dirofilaria repens was first reported in India by Joseph et al. who described a case of ocular Dirofilaria in a patient from southern coastal state of Kerala. Following this, isolated case reports of Dirofilaria were published throughout the nineties. It is probable that the sudden spurt in the cases seen over the last decade is not only indicative of greater awareness of this entity but also an actual increase in its incidence (Fig. 3).
Fig. 3.
Year-wise distribution of cases in India since 1977
The state of Kerala has so far been the main reservoir of infection. Its close geographical proximity to Srilanka, one of the most affected countries may be the cause. Out of the 70 odd case reports, more than half of the patients either were residents of or provided history of travels to Kerala. Recent trends however indicate a northward migration of the disease with cases being reported from Karnataka and Maharashtra and occasionally from Northern and Eastern states of Assam, Bihar Orissa and Haryana (Gautam et al. 2002; Singh et al. 2010; Nath et al. 2010; Chopra et al. 2012).
The prevalence of microfilaremia in dogs in Kerala and Karnataka is around 7 and 21 % respectively. This high prevalence in dogs—both domestic and stray explains the high incidence of disease in these regions. Moreover, India is endemic for malaria and lymphatic filariasis. The humid climate and recent industrialization have given rise to a conductive atmosphere for the breeding mosquitoes. Hence, it is not surprising that the incidence of Dirofilaria, which shares its arthropod vectors with these, should also rise (Pampiglione and Rivasi 2000; Sahdev et al. 2012; Rani et al. 2010).
Dirofilaria in India is more common in females with the age range from 1 to 75 years. The details of socio-economic status/living conditions and loco—regional details including local vector control measures if any, residence in rural/urban regions and contact history with animals were not available (Bhat et al. 2012; Nath et al. 2010).
A single case of pulmonary Dirofilaria has been reported from India in a child manifesting as portal cavernoma with pulmonary dirofilariasis detected at autopsy (Badhe and Sane 1989).
Orbital/periorbital Dirofilaria accounted for more than half the number of cases with worms located in the eyelid, subconjunctival region, canthus, limbus, subtenon space and anterior chamber. Preferred location for subcutaneous Dirofilaria was the head and neck, followed by face, arm and chest. The torso, thigh and scrotum were favoured locations in the lower half of the body. The distribution is similar to that observed by Orihel and Eberhard (1998). An isolated case of intramuscular Dirofilaria by D. immitus is reported (Teerthanath and Hariprasad 2011).
Where the sex of the worm was identified female worms were found with greater frequency than male worms (24 out of 27) which is in concurrence with the world literature. The male worms of D. repens ranged from 3.5 cm to 6 cm and female worms ranged from 10 cm to 13.5 cm. D. tenius was 12 cm to 16 cm.
Diagnosis of D repens is mainly by morphological examination of the worm. An adult male worm is 5–6 cm long with anal spicules. The female are 10–17 cm long and 460–650 μm wide with a vulva 1.15–1.62 cm from the anterior end. More important are the morphologic features seen in transverse- sections of the worms. The cuticle is multilayered and has transverse striations with prominent longitudinal ridges. On the inner surface of the cuticle in the lateral fields, a conspicuous cuticular ridge protrudes into the inner surface of the lateral chords. The muscle coat is characteristically well developed. The number of reproductive tubes and their contents (eggs, microfilariae, and sperm) help identify the sex of the worm (Orihel and Eberhard 1998).
Dirofilaria repens reproduces sexually, its lifecycle consisting of five developmental stages requiring a vertebrate main host (usually a dog or cat) and an arthropod intermediate host/vector. The immature filaria migrate subcutaneously, undergoes development into an adult worm and then dies inciting an inflammatory reaction of the Th2 type dominated by eosinophils. Blood counts including the white cell differentials are usually within normal limits (Orihel and Eberhard 1998).
Conclusion
We support the opinion that Dirofilaria is emerging zoonoses in Indian subcontinent. With its increasing incidence it becomes imperative for the regional pathologists and microbiologists to be well versed with its morphology and the surgeons and ophthalmologists be aware of this parasite. A DNA study may help in further epidemiological characterization of the Dirofilaria species.
Contributor Information
Reshma G. Kini, Phone: +91-9986287395, Email: drreshmakini@gmail.com
J. B. Leena, Email: drleenapriye@gmail.com
References
- Athari A. Zoonotic subcutaneous dirofilariases in Iran. Arch Iran Med. 2003;6:63–65. [Google Scholar]
- Badhe BP, Sane SY. Human pulmonary dirofilariasis in India: a case report. J Trop Med Hyg. 1989;92:425–426. [PubMed] [Google Scholar]
- Bhat KG, Wilson G, Mallya S. Human dirofilariasis. Indian J Med Microbiol. 2003;21:65. [PubMed] [Google Scholar]
- Bhat S, Sofia O, Raman M, Biswas J. A case of subconjunctival dirofilariasis in South India. J Ophthal Inflamm Infect. 2012;2:205–206. doi: 10.1007/s12348-012-0078-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakrabarti A, John SR, Chakrabarti M. Worm wobble: subconjunctival Dirofilaria. Kerala J Ophthalmol. 2009;XXI:202–204. [Google Scholar]
- Chopra R, Bhatti SM, Mohan S, Taneja N. Dirofilaria in the anterior chamber: a rare occurrence middle east. Afr J Ophthalmol. 2012;19:349–351. doi: 10.4103/0974-9233.97965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhar M, Nambiar R. Dirofilaria masquerading as a cyst in the muscle. Kerala J Ophthalmol. 2008;XX:88–90. [Google Scholar]
- Gautam V, Rustagi IM, Singh S, Arora DR. Subconjunctival infection with Dirofilariarepens. Jpn J Infect Dis. 2002;55:47–48. [PubMed] [Google Scholar]
- Ittyerah TP, Mallik D. A case of subcutaneous dirofilariasis of the eyelid in the South Indian state of Kerala. Indian J Ophthalmol. 2004;52:235. [PubMed] [Google Scholar]
- Joseph A, Thomas PG, Subramaniam KS. Conjunctivitis by Dirofilaria conjunctivae. Indian J Ophthal. 1976;24:20–22. [PubMed] [Google Scholar]
- Joseph E, Matthai AA, Latha K, Thomas SA. Subcutaneous human dirofilariasis. J Parasit Dis. 2011;35:140–143. doi: 10.1007/s12639-011-0039-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph K, Vinayakumar AR, Criton S, Vishnu MS, Pariyaram SE. Periorbital mass with cellulitis caused by Dirofilaria. Indian J Med Microbiol. 2011;29:431–433. doi: 10.4103/0255-0857.90190. [DOI] [PubMed] [Google Scholar]
- Khurana S, Singh G, Bhatti HS, Malla N. Human subcutaneous dirofilariasis in India: a report of three cases with brief review of literature. Ind J Med Microbiol. 2010;28:394–396. doi: 10.4103/0255-0857.71836. [DOI] [PubMed] [Google Scholar]
- Kim MK, Kim CH, Yeom BW, Park SH, Choi SY, Choi JS. The first human case of hepatic dirofilariasis. J Korean Med Sci. 2002;17:686–690. doi: 10.3346/jkms.2002.17.5.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotian VB, Amin H, Teerthanath, Devika P. Periorbital subcutaneous dirofilariasis a report from coastal Karnataka. Int J Biomed Adv Res. 2011;02:398–401. doi: 10.7439/ijbar.v2i10.170. [DOI] [Google Scholar]
- Kotigadde S, Ramesh SA, Medappa KT. Human dirofilariasis due to dirofilariasis in Southern India. Trop Parasitol. 2012;2:67–68. doi: 10.4103/2229-5070.97247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahesh G, Giridhar A, Biswas J, Saikumar SJ, Saikumar SJ, Bhat A. A case of Dirofilariasis, masquerading as lid tumor. Indian J Ophtahlmol. 2005;53:63–64. doi: 10.4103/0301-4738.15290. [DOI] [PubMed] [Google Scholar]
- Mrad K, Romani-Ramah S, Driss M, Bougrine F, Hechiche M, Maalej M. Mammary Dirofilariasis: a case report. Int J Surg Pathol. 1999;7:175–178. doi: 10.1177/106689699900700308. [DOI] [Google Scholar]
- Mukherjee B, Biswas J, Varde MA, Noronha V. Orbital dirofilariasis. Ann Trop Med Public Health. 2012;5:42–43. doi: 10.4103/1755-6783.92880. [DOI] [Google Scholar]
- Nadgir S, Tallur SS, Mangoli V, Halesh LH, Krishna BV. Subconjunctival dirofilariasis in India. Southeast Asian J Trop Med Public Health. 2001;32:244–246. [PubMed] [Google Scholar]
- Nath R, Gogoi R, Bordoloi n, Gogoi T. Ocular dirofilariasis. Indian J Pathol Microbiol. 2010;53:157–159. doi: 10.4103/0377-4929.59213. [DOI] [PubMed] [Google Scholar]
- Orihel TC, Eberhard ML. Zoonotic Filariasis. Clin Microbiol Rev. 1998;11(2):366–381. doi: 10.1128/cmr.11.2.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padmaja P, Kanagalakshmi SamuelR, Kuruvilla PJ, Mathai E. Subcutaneous dirofilariasis in southern India: a case report. Ann Trop Med Parasitol. 2005;99:437–440. doi: 10.1179/36485905X36253. [DOI] [PubMed] [Google Scholar]
- Pampiglione S, Rivasi F. Human dirofilariasis due to Dirofilaria (Nochtiella) repens: an update of world literature from 1995 to 2000. Parassitologia. 2000;42:231–254. [PubMed] [Google Scholar]
- Pampiglione S, Canestri Trotti G, Squadrini F. Human subcutaneous dirofilariasis: a report of 5 new cases of Dirofilariarepens in central and northern Italy and of a sixth case with uncertain parasitological diagnosis. Parassitologia. 1982;24:167–176. [PubMed] [Google Scholar]
- Pampiglione S, Canestri Trotti G, Rivasi F. Human dirofilariasis due to Dirofilaria (Nochtiella) repens: a review of world literature. Parassitologia. 1995;37:149–193. [PubMed] [Google Scholar]
- Permi HS, Veena S, Kishan Prasad HL, Kumar YS, Mohan R, Shetty KJ. Subcutaneous human dirofilariasis due to Dirofilaria repens: report of two cases. J Glob Infect Dis. 2011;3:199–201. doi: 10.4103/0974-777X.81702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raju KV, Anju A, Anju A, Vijayalakshmi Subcutaneous Dirofilariarepens: a report of two cases. Kerala J Ophthalmol. 2008;XX:294–296. [Google Scholar]
- Rani PAMA, Irwin PJ, Gatne M, Coleman GT, Traub RJ. Canine vector-borne diseases in India: a review of the literature and identification of existing knowledge gaps. Parasites & Vectors. 2010;3:28. doi: 10.1186/1756-3305-3-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabu L, Devada K, Subramanian H. Dirofilariosis in dogs and humans in Kerala. Indian J Med Res. 2005;121:691–693. [PubMed] [Google Scholar]
- Sahdev SI, Sureka SP, Sathe PA, Agashe R. Ocular dirofilariasis: still in the dark in western India? J Postgrad Med. 2012;58:227–228. doi: 10.4103/0022-3859.101650. [DOI] [PubMed] [Google Scholar]
- Sangit VA, Haldipurkar SS. Subconjunctival dirofilariasis mimicking scleritis: first report from Western India. Indian J Ophthalmol. 2012;60:76–77. doi: 10.4103/0301-4738.91343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanjeev H, Rajini M, Prasad SR. Human dirofilariasis: an uncommon case of subcutaneous infection with Dirofilariarepens with a brief review of literature. Nitte Univ J Health Sci. 2011;I:60–62. [Google Scholar]
- Sathyan P, Manikandan P, Bhaskar M, Padma S, Singh G, Appalaraju B. Subtenons infection by Dirofilaria repens. Indian J Med Microbiol. 2006;24:61–62. doi: 10.4103/0255-0857.19899. [DOI] [PubMed] [Google Scholar]
- Sekhar HS, Srinivasa H, Batru BR, Mathai E, Shariff S, Macaden RS. Human ocular dirofilariasis in Kerala, Southern India. Indian J Pathol Microbiol. 2000;43:77–79. [PubMed] [Google Scholar]
- Senthivel K, Pillai KM. A case of subcutaneous dirofilariasis in a woman in Kerala. Indian Vet J. 1999;76:263–264. [Google Scholar]
- Singh R, Shwetha JV, Samantaray JC, Bando G. Dirofilariasis: a rare case report. Indian J Med Microbiol. 2010;28:75–77. doi: 10.4103/0255-0857.58739. [DOI] [PubMed] [Google Scholar]
- Smitha M, Rajendran VR, Devarajan E, Anitha PM. Case report: orbital dirofilariasis. Indian J Radiol Imaging. 2008;18:60–62. doi: 10.4103/0971-3026.37050. [DOI] [Google Scholar]
- Srinivasamurthy V, Rao MS, Thejaswini MU, Yoganand Human subcutaneous dirofilariasis. Ann Trop Med Public Health. 2012;5:349–351. doi: 10.4103/1755-6783.102052. [DOI] [Google Scholar]
- Teerthanath S, Hariprasad S. A case of Dirofilariaimmitus presenting as an intramuscular soft tissue mass. Indian J Pathol Microbiol. 2011;54:428–429. doi: 10.4103/0377-4929.81620. [DOI] [PubMed] [Google Scholar]
- Vaidya KA, Srikar SV. Subcutaneous dirofilariasis: a case report. Case Study and Case Report. 2012;2:10–15. [Google Scholar]
- Internet reference. WHO status on malaria in India.URL http://www.who.int/malaria/publications/country-profiles/profile_ind_en.pdf. Accessed 6 Dec 2012



