Abstract
Objective:
To examine the impact of a healthy lifestyle on stroke risk in men at higher risk of stroke because of other cardiovascular diseases or conditions.
Methods:
Our study population comprised 11,450 men in the Cohort of Swedish Men who had a history of hypertension, high cholesterol levels, diabetes, heart failure, or atrial fibrillation. Participants had completed a questionnaire about diet and lifestyle and were free from stroke and ischemic heart disease at baseline (January 1, 1998). We defined a healthy lifestyle as a low-risk diet (≥5 servings/d of fruits and vegetables and <30 g/d of processed meat), not smoking, ≥150 min/wk of physical activity, body mass index of 18.5 to 25 kg/m2, and low to moderate alcohol consumption (>0 to ≤30 g/d). Ascertainment of stroke cases was accomplished through linkage with the National Inpatient Register and the Swedish Cause of Death Register.
Results:
During a mean follow-up of 9.8 years, we ascertained 1,062 incident stroke cases. The risk of total stroke and stroke types decreased with increasing number of healthy lifestyle factors. The multivariable relative risk of total stroke for men who achieved all 5 healthy lifestyle factors compared with men who achieved 0 or 1 factor was 0.28 (95% confidence interval 0.14–0.55). The corresponding relative risks (95% confidence interval) were 0.31 (0.15–0.66) for ischemic stroke and 0.32 (0.04–2.51) for hemorrhagic stroke.
Conclusions:
A healthy lifestyle is associated with a substantially reduced risk of stroke in men at higher risk of stroke.
Primary prevention of stroke is of outmost importance because the consequences of the disease are often devastating and irreversible, and stroke is the second leading cause of death in individuals older than 60 years.1 Smoking, being overweight, physical inactivity, alcohol consumption, and poor diet are well-established lifestyle-related risk factors for stroke.2,3 The combined effect of multiple modifiable lifestyle factors on stroke risk have shown impressive 44% to 79% reduced risk.4–9 However, little is known about the impact of a healthy lifestyle on stroke risk in individuals at higher risk of stroke due to other cardiovascular diseases or conditions.
We investigated the joint effect of 5 indicators of a healthy lifestyle (no smoking, healthy body mass index [BMI], physical activity, moderate alcohol consumption, and diet) on total and type-specific stroke incidence in men at higher risk of stroke due to a history of hypertension, high cholesterol levels, diabetes, heart failure, or atrial fibrillation.
METHODS
Study population.
We used data from the Cohort of Swedish Men, which was established in the autumn of 1997 when all men who were born between 1918 and 1952 and resided in Västmanland and Örebro counties in central Sweden received a 350-item questionnaire. A total of 48,850 men (49% response rate) returned a completed questionnaire. Participants are representative of the Swedish male population in age distribution, educational level, and prevalence of overweight.10
Standard protocol approvals, registrations, and patient consents.
The Regional Ethical Review Board at Karolinska Institutet in Stockholm, Sweden, approved this study. Return of the completed questionnaire was considered to imply informed consent.
Assessment of lifestyle and other factors.
At baseline in 1997, all participants completed a self-administered questionnaire that sought information on education, civil status, smoking, physical activity, body weight, height at age 20 years, aspirin use, history of diabetes, family history of myocardial infarction before 60 years of age, alcohol consumption, and diet. History of diabetes was defined as a diagnosis of diabetes in the Swedish National Diabetes Register or the Swedish National Inpatient Register and complemented with self-reported diabetes. The National Inpatient Register also provided data on heart failure. Information on history of hypertension and high cholesterol levels was obtained by self-report. Participants were asked to report their time spent on walking/bicycling (almost never, <20 min/d, 20–40 min/d, 40–60 min/d, 1–1.5 h/d, or ≥1.5 h/d) and exercise (<1, 1, 2–3, 4–5, or ≥5 h/wk). We calculated total leisure-time physical activity by combining minutes per day spent on walking/bicycling and exercise in the last year. BMI was calculated as weight (kg) at baseline divided by height (m) squared. Average consumption of alcohol (ethanol), in the last year, was computed by multiplying the frequency of consumption of beer, wine, and liquor by the amount consumed at each occasion.
Diet was assessed by using a 96-item food-frequency questionnaire (FFQ), designed to assess the Swedish diet, on which participants reported how often, on average, they had consumed various foods/food items during the last year. There were 8 predefined frequency categories, ranging from never to ≥3 times/d. The FFQ had 4 items about consumption of fruits and berries (apples/pears, bananas, citrus fruits, and berries), 11 items on vegetables (lettuce/green salad, spinach, cabbage, cauliflower, broccoli/Brussels sprouts, carrots, beetroots, tomatoes/tomato juice, sweet pepper, green peas, and mixed vegetables), and 4 items on processed meat (sausage/hot dogs, ham/salami/processed meat cuts, liver paté, and blood sausage). The FFQ has been validated for nutrient intake in 248 Swedish men, aged 40 to 74 years, from the study area. The mean Spearman correlation coefficients between estimates from the FFQ and the mean of fourteen 24-hour recall interviews were 0.65 for macronutrients and 0.62 for micronutrients.11
Population for analysis.
Among the 48,850 men in the Cohort of Swedish Men, we excluded those with an erroneous or a missing National Registration Number (n = 297), those with a prior diagnosis of cancer (n = 2,592), stroke (n = 1,373), or ischemic heart disease (n = 4,123), and those who died (n = 55) before start of follow-up (January 1, 1998). After further exclusion of 4,955 men (12%) with missing information on any of the indicators of a healthy lifestyle or who were underweight (i.e., BMI <18.5 kg/m2), 35,455 men (45–79 years of age) remained. Among those, 11,450 men had a history of hypertension, high cholesterol levels, diabetes, heart failure, or atrial fibrillation at baseline. This high-risk group constituted our study population for the present analysis.
Definition of healthy lifestyle.
We considered 5 lifestyle factors, including diet, smoking, physical activity, BMI, and alcohol consumption. We created a healthy lifestyle score by dichotomizing each lifestyle factor into a predefined healthy lifestyle alternative vs a less healthy/unhealthy alternative: low-risk diet (≥5 servings/d of fruits and vegetables12 and <30 g/d [about 0.5–1 serving] of processed meat13 vs <5 servings/d of fruits and vegetables and/or ≥30 g/d of processed meat), smoking5 (not smoking [never and past] vs current smoking), physical activity14 (≥150 min/wk of walking/bicycling or exercise vs <150 min/wk of walking/bicycling and exercise), BMI15 (18.5–25 kg/m2 [normal weight] vs ≥25 kg/m2 [overweight]), and alcohol consumption16 (low to moderate [>0 to ≤30 g/d] vs abstainers or heavy drinkers [>30 g/d]). The total allocated points of lifestyle factors were used to calculate the healthy lifestyle score, which ranged from 0 to 5. Because of small number of stroke cases (n = 11) in the group without any healthy lifestyle factors, we combined men with 0 and 1 lifestyle factor (reference group).
Ascertainment of stroke cases.
Dates of stroke diagnoses were obtained from the Swedish National Inpatient Register and the Swedish Cause of Death Register. A validation study of stroke diagnoses in these registries found that 92% of the stroke patients were correctly classified.17 We classified stroke types according to the ICD-10: ischemic stroke (code I63) and hemorrhagic stroke (I60 and I61). Unspecified strokes (I64) were included in the analyses of total stroke only.
Statistical analysis.
Participants accumulated follow-up time from January 1, 1998, until the date of diagnosis of stroke, date of death (data from the Swedish Cause of Death Register), or the end of follow-up (December 31, 2008), whichever came first. Relative risks and 95% confidence intervals (CIs) were estimated by using Cox proportional hazards regression models. All analyses were adjusted for age (in months) through stratification in the Cox model. In addition, all models were controlled for education (less than high school, high school, or university), civil status (single, married/cohabiting, divorced, widowed), aspirin use (never, 1–6 tablets/wk, or ≥7 tablets/wk), and family history of myocardial infarction before 60 years of age (yes or no). The proportional hazards assumption was tested using Schoenfeld residuals and was found to be satisfied. All statistical analyses were performed using SAS (version 9.3; SAS Institute, Cary, NC) or Stata (version 12; StataCorp, College Station, TX). Two-sided p values <0.05 were considered statistically significant.
RESULTS
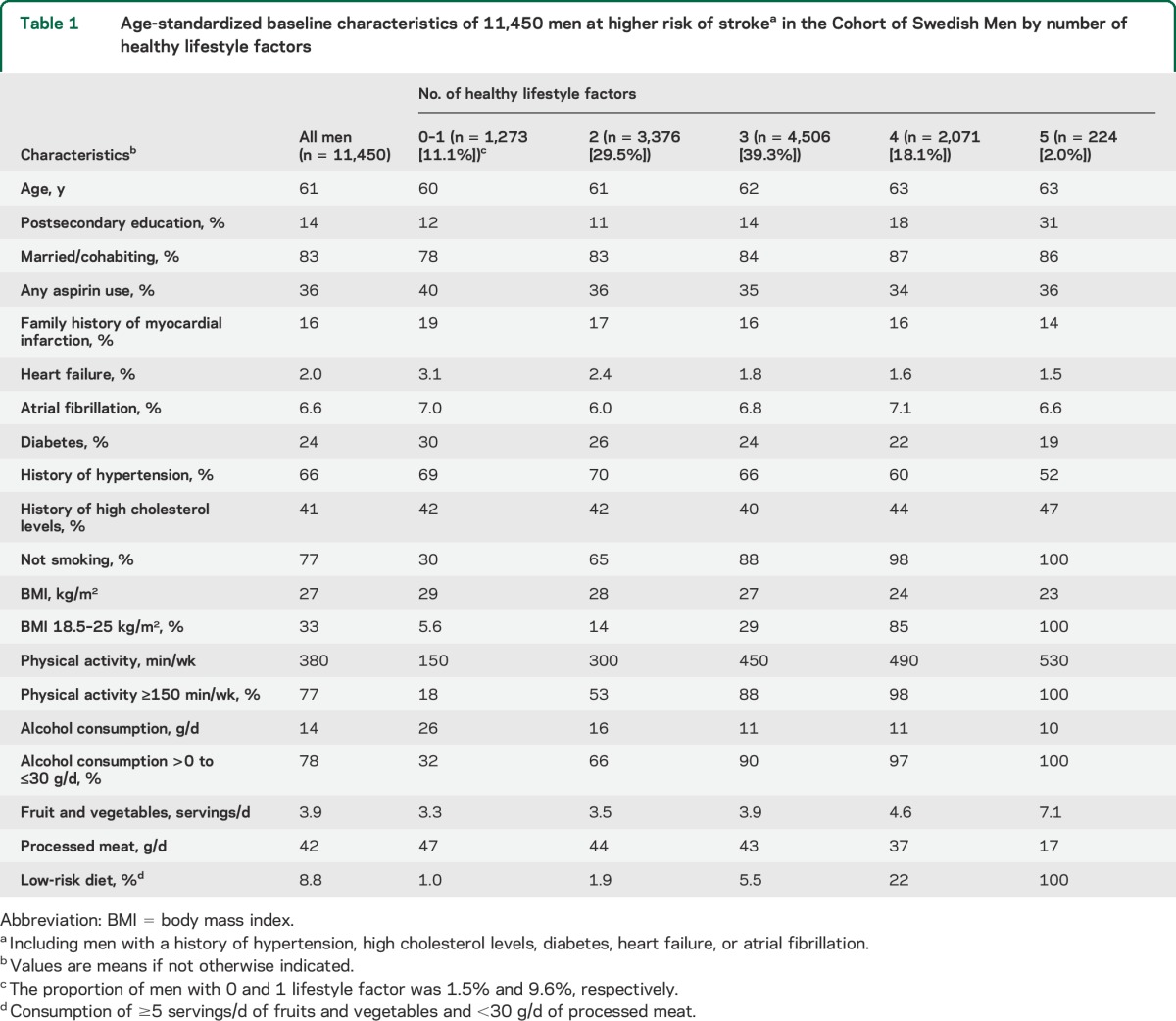
Among the 11,450 men with a history of hypertension, high cholesterol levels, diabetes, heart failure, or atrial fibrillation, we ascertained 1,062 stroke cases, including 800 ischemic strokes, 141 hemorrhagic strokes (119 intracerebral hemorrhages and 22 subarachnoid hemorrhages), and 121 unspecified strokes during a mean follow-up of 9.8 years (111,719 person-years). Baseline characteristics of participants according to number of healthy lifestyle factors are shown in table 1. Men who achieved all 5 indicators of a healthy lifestyle tended to be older and were more likely to have a postsecondary education and to be married/cohabiting but were less likely to have a family history of myocardial infarction and any cardiovascular diseases and conditions compared with men with 0 or 1 lifestyle factor. We compared men with complete information on the lifestyle factors with those with missing values to evaluate the qualitative differences between groups. Those who were excluded because of missing values on any of the lifestyle factors were slightly older (mean age 63 years) and were more likely to have diabetes (35%) but less likely to have a postsecondary education (10%) compared with men with complete data.
Table 1.
Age-standardized baseline characteristics of 11,450 men at higher risk of strokea in the Cohort of Swedish Men by number of healthy lifestyle factors
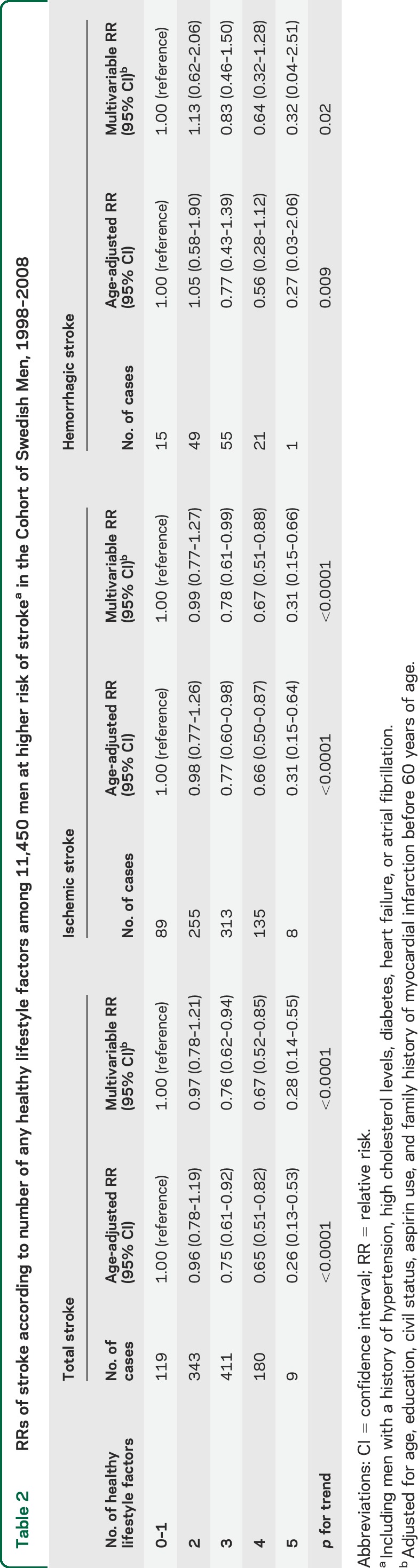
The associations between number of healthy lifestyle factors and risk of stroke are shown in table 2. Men who adhered to all 5 lifestyle factors had a statistically significant 72% lower risk of total stroke compared with men with 0 or 1 factor, after adjustment for other risk factors. Further adjustment for a history of hypertension, high cholesterol levels, diabetes, heart failure, and atrial fibrillation did not alter the results materially (relative risk for all 5 factors vs 0–1 factor = 0.30; 95% CI, 0.15–0.61). The association between a healthy lifestyle and stroke risk was similar for ischemic stroke and hemorrhagic stroke (table 2).
Table 2.
RRs of stroke according to number of any healthy lifestyle factors among 11,450 men at higher risk of strokea in the Cohort of Swedish Men, 1998–2008
Results for the whole Cohort of Swedish Men (n = 35,455) are presented in supplemental data (tables e-1 and e-2, and figure e-1 on the Neurology® Web site at Neurology.org).
DISCUSSION
In this prospective study of middle-aged and elderly men at higher risk of stroke because of other cardiovascular conditions, a healthy lifestyle pattern was associated with a substantially reduced risk of stroke. Men who achieved all 5 healthy lifestyle factors had a 72% lower risk of stroke compared with those who achieved 0 or 1 factor.
In previous studies in the general population,4–9 the relative risk (95% CI) of total stroke for those with the most healthy lifestyle factors, compared with those with the least, has ranged from 0.21 (0.12–0.36) in the Nurses' Health Study5 to 0.56 (0.30–1.05) in the Women's Health Study.4 One of those prior studies investigated whether the relation between a healthy lifestyle and stroke was modified by cardiovascular risk factors, including history of diabetes, hypertension, and total cholesterol levels.7 For total stroke, the inverse associations between number of healthy lifestyle factors and risk of stroke were present both in those with and without a history of diabetes, hypertension, and high cholesterol levels.7 That finding is consistent with our results showing that a reduction in stroke risk by a healthy lifestyle pattern can be achieved also in men with prior cardiovascular conditions. Another study examined the effect of a healthy lifestyle on mortality after stroke and observed that combinations of 5 indicators of healthy lifestyle were associated with lower all-cause and cardiovascular disease mortality in a dose-response manner.18
Major strengths of this study are the large number of incident stroke cases and the almost complete follow-up of participants through linkage to population-based Swedish registries. Because of the observational nature of this study, we cannot rule out the possibility that our results were affected by residual confounding due to unmeasured or imprecise measurement of other risk factors. Our study is also limited by the reliance on self-reported information of diet and lifestyle, which will inevitably lead to some degree of measurement error and misclassification of participants into wrong exposure category. However, because of the prospective design, any misclassification would most likely be nondifferential and lead to attenuation of the risk estimates. Because the lifestyle factors were assessed only at one time (baseline), we do not know whether the individuals adhered to the healthy lifestyle practices during the whole follow-up. Another limitation is that there may be some misclassification of the stroke patients. Finally, because our study population mainly consisted of Caucasians, our results may not be applicable to other more heterogeneous populations.
Findings from this prospective study showed that men at higher risk of stroke may lower their stroke risk by adopting a healthy lifestyle. Even though the criteria used to define the healthy lifestyle behaviors were relatively lenient and potentially achievable, the combined healthy lifestyle pattern had a profound impact on stroke risk.
Supplementary Material
GLOSSARY
- BMI
body mass index
- CI
confidence interval
- FFQ
food-frequency questionnaire
- ICD-10
International Classification of Diseases, Tenth Revision
Footnotes
Supplemental data at Neurology.org
AUTHOR CONTRIBUTIONS
The contributions of the authors to the manuscript were as follows: study concept and design (S.C.L., A.Å., A.W.), data collection (A.W.), statistical analyses (S.C.L.), manuscript writing (S.C.L.), interpretation of results (S.C.L., A.Å., A.W.), and critical revision of manuscript (S.C.L., A.Å., A.W.). S.C.L. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
STUDY FUNDING
Supported by a research grant from the Strategic Research Area in Epidemiology (SfoEpi) at Karolinska Institutet. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the article.
DISCLOSURE
The authors report no disclosures relevant to the manuscript. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Mackay J, Mensah G. The Atlas of Heart Disease and Stroke. Geneva: World Health Organization; 2004. [Google Scholar]
- 2.Patra J, Taylor B, Irving H, et al. Alcohol consumption and the risk of morbidity and mortality for different stroke types: a systematic review and meta-analysis. BMC Public Health 2010;10:258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldstein LB, Bushnell CD, Adams RJ, et al. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011;42:517–584. [DOI] [PubMed] [Google Scholar]
- 4.Kurth T, Moore SC, Gaziano JM, et al. Healthy lifestyle and the risk of stroke in women. Arch Intern Med 2006;166:1403–1409. [DOI] [PubMed] [Google Scholar]
- 5.Chiuve SE, Rexrode KM, Spiegelman D, Logroscino G, Manson JE, Rimm EB. Primary prevention of stroke by healthy lifestyle. Circulation 2008;118:947–954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Myint PK, Luben RN, Wareham NJ, Bingham SA, Khaw KT. Combined effect of health behaviours and risk of first ever stroke in 20,040 men and women over 11 years' follow-up in Norfolk cohort of European Prospective Investigation of Cancer (EPIC Norfolk): prospective population study. BMJ 2009;338:b349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang Y, Tuomilehto J, Jousilahti P, Wang Y, Antikainen R, Hu G. Lifestyle factors on the risks of ischemic and hemorrhagic stroke. Arch Intern Med 2011;171:1811–1818. [DOI] [PubMed] [Google Scholar]
- 8.Eguchi E, Iso H, Tanabe N, et al. Healthy lifestyle behaviours and cardiovascular mortality among Japanese men and women: the Japan Collaborative Cohort Study. Eur Heart J 2012;33:467–477. [DOI] [PubMed] [Google Scholar]
- 9.Larsson SC, Åkesson A, Wolk A. Healthy diet and lifestyle and risk of stroke in a prospective cohort of women. Neurology 2014;83:1699–1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Norman A, Bellocco R, Vaida F, Wolk A. Total physical activity in relation to age, body mass, health and other factors in a cohort of Swedish men. Int J Obes Relat Metab Disord 2002;26:670–675. [DOI] [PubMed] [Google Scholar]
- 11.Messerer M, Johansson SE, Wolk A. The validity of questionnaire-based micronutrient intake estimates is increased by including dietary supplement use in Swedish men. J Nutr 2004;134:1800–1805. [DOI] [PubMed] [Google Scholar]
- 12.Larsson SC, Virtamo J, Wolk A. Total and specific fruit and vegetable consumption and risk of stroke: a prospective study. Atherosclerosis 2013;227:147–152. [DOI] [PubMed] [Google Scholar]
- 13.Larsson SC, Virtamo J, Wolk A. Red meat consumption and risk of stroke in Swedish men. Am J Clin Nutr 2011;94:417–421. [DOI] [PubMed] [Google Scholar]
- 14.Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129:S76–S99. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consultation on Obesity. Geneva: World Health Organization; 1998. [PubMed] [Google Scholar]
- 16.Lichtenstein AH, Appel LJ, Brands M, et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation 2006;114:82–96. [DOI] [PubMed] [Google Scholar]
- 17.Appelros P, Terent A. Validation of the Swedish inpatient and cause-of-death registers in the context of stroke. Acta Neurol Scand 2011;123:289–293. [DOI] [PubMed] [Google Scholar]
- 18.Towfighi A, Markovic D, Ovbiagele B. Impact of a healthy lifestyle on all-cause and cardiovascular mortality after stroke in the USA. J Neurol Neurosurg Psychiatry 2012;83:146–151. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


