Abstract
Objective:
The aim was to obtain normative data for cephalometric measurements of the upper airway in the North Indian population.
Design:
Observational study. Setting: University department and teaching hospital out-patient clinic.
Subjects and Methods:
A total of 180 healthy patients were included out of which 90 were males (age range, 8-16 years), and 90 were females (age range, 8-16 years), with normal skeletal facial profile, no history of snoring, sleep apnea, upper airway disease, tonsillectomy or adenoidectomy, obesity, or pathology in the pharynx. Twenty cephalometric airway measurements, including size of the tongue, soft palate, nasopharynx, oropharynx, hypopharynx, and relative position of the hyoid bone and valleculae were obtained. Landmarks on cephalometric radiographs were digitized and measurements were made using a specially designed computer program. Error analysis of measurements was performed and comparison of measurements according to sex was made.
Results:
Significant sex dimorphism was seen for the majority of measurements, with the exception of minimal depth of the airway, oropharyngeal depth of the airway, and the soft palate angle with the hard palate.
Conclusion:
A minimum sagittal dimension of the upper airway was evident despite differences in measurements between sexes. Findings from this study should be a useful reference for the assessment of sleep apnea in the North Indian population.
Keywords: Cephalometry, North Indian, pharynx
Introduction
Cephalometric radiographs have been used for many years to evaluate facial growth and development.[1,2] Cephalometry enables analysis of dental and skeletal anomalies as well as soft tissue structures and form. Many studies have assessed the anatomic conformation of the upper airway with more sophisticated and expensive techniques, including cine-computed tomography (CT),[3] fluoroscopy,[4] acoustic reflection,[5] fiberoptic pharyngoscopy,[6] and magnetic resonance imaging.[7] Cephalometry is, however, less expensive, more useful, easily achieved with reduced radiation, and correlates with other investigations such as CT or somnofluoroscopy carried out during wakefulness or sleep.[8,9] Cephalometric measurements of the posterior airway space, although a two-dimensional analysis, have proved very reliable in diagnosing pharyngeal volumes.[10,11]
Posterior airway space, as measured by lateral cephalometric radiography, was highly correlated with measurements using three-dimensional CT scan, with a 92% accuracy in predictability.[12]
Many authors have used cephalometry for assessment of the airway in craniofacial syndromes,[13,14,15,16] in patients with obstructive sleep apnea (OSA),[11,16,17,18,19,20,21,22,23] and following orthognathic surgery,[24,25,26,27,28,29] and for evaluation of the airway in various dentofacial deformities.[30,31,32] Understanding of the upper airway in normal subjects can assist management of OSA syndrome and in identifying potential sites of obstruction of the upper airway after surgical correction of dentofacial deformities. Cephalometric measurements of the airway vary according to ethnic group and sex. Therefore, the purpose of this study was to carry out a systematic, cephalometric evaluation of the upper airway in a large group of normal subjects in order to establish cephalometric reference values of the upper airway in North Indian population.
Subjects and Methods
Subjects
Male and female North Indian subjects were selected from a large pool of patients attending the Faculty of Dental Sciences, King George's Medical University, Lucknow for dental treatment. Patients were interviewed and examined for the purpose of selection. The selection criteria included North Indian, normal visual harmony of facial and skeletal profile, and normal dental occlusion (Class I), with 2-4 mm of overbite and intact dental arch. Exclusion criteria included previous orthodontic treatment or corrective jaw (Orthognathic) surgery, active periodontal disease, habitual snoring, habitual mouth breathing, obesity or assessed as clinically overweight, OSA, chronic respiratory disease, previous tonsillectomy and/or adenoidectomy, pathology in the area of study (e.g. nasopharyngeal carcinoma), and irradiation to the head and neck area.
Cephalometric analysis
Lateral cephalometric radiographs were taken using a standardized technique, with the jaw in centric relation and the teeth in occlusion, the lips relaxed, and the head in the natural head position. The subject stood with the sagittal plane parallel to the film and with bilateral ear rods gently inserted into the external auditory meatus to stabilize the head position during exposure. Two types of X-ray machines were used. The older was a General Electric GE 100 (General Electric Dental Systems, Milwaukee, US) and the films used were Kodak Ortho-G 24 × 30 (Eastman Kodak Company, Rochester, US). Distance from the anode to the mid-sagittal plane of the patient was 150 cm, while distance from the mid-sagittal plane to the film was 13 cm. The newer machine was a Philips Orthoralix SD (Philips Medical Systems, Monza, Italy) and the film used Kodak Ortho-G 15 × 30 (Eastman Kodak Company, Rochester, US). The mid-sagittal plane to film distance was 15 cm with this machine.
All films were processed under standardized conditions. The magnification factors of the lateral cephalometric radiographs taken with the older and newer X-ray machines were measured separately and corrected for the later cephalometric measurements on the processed films. The magnification factor was measured by the following formula:
M = (X ’ - X)/X.
Where X is the radiopaque ruler used when the radiograph was taken, and X ’ is the figure measured from the magnified ruler on the radiograph.
Landmarks and measurements
The reference points and lines used in the analysis are shown in the Figure 1a and b and Table 1 provides a description of the landmarks used, while Tables 2 and 3 give descriptions of the measurements undertaken and the relevant abbreviations. The methods of measurement used were a modification of those used by Lyberg et al.,[20,21] and have been widely used in other studies.[22,23] Seventeen variables - including 12 linear distances, one angle, four-area measurements, and three ratios of area values were identified and calculated for each cephalometric radiograph on the basis of their clinical relevance in determining the patency of the nasopharyngeal, oropharyngeal, and hypopharyngeal airway space. The tongue was measured in the sagittal length (VT), height (H⊥VT), and a defined sagittal area (tongue area [TA]). The soft palate was also measured in length (pterygo-maxillare uvula [PM-U]), thickness (soft palate thickness), and a defined sagittal area (soft palate area [SPA]). The width of the upper-airway space was measured in the sagittal plane at four levels: The nasopharynx (PM-upper pharyngeal wall [UPW]), oropharynx (U-middle pharyngeal wall [MPW]), hypopharynx (vallecula-lower pharyngeal wall [V-LPW]), and the region of minimal airway space (PASmin). The position of the soft palate was represented by the angle (nasal line [NL]/PM-U) between its long axis (PM-U) and the NL. In addition, the oral area (OA), nasopharyngeal area (NOPA), and three ratios of area values were calculated for further analysis.
Figure 1.
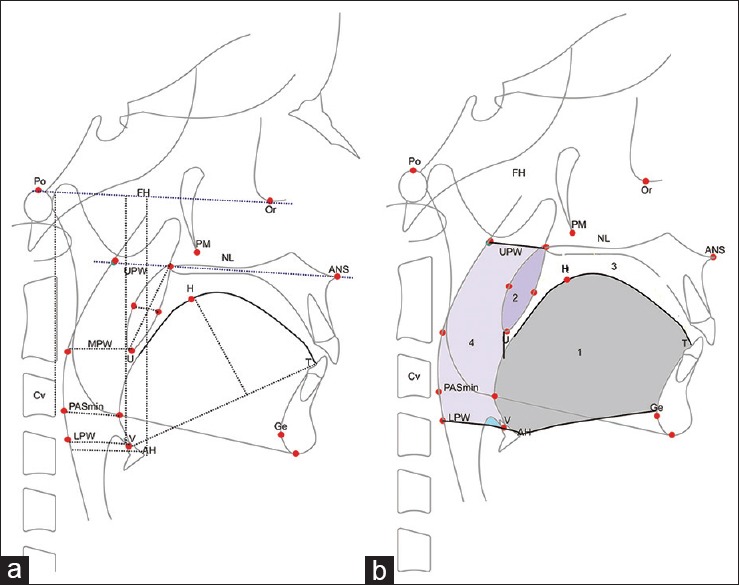
(a) Diagrammatic representation of the oronasopharynx (sagittal view) 1a Landmarks and reference lines used in the analysis of lateral cephalometric radiographs. (b) Area measurements used in the study
Table 1.
Landmarks used in cephalometric analysis
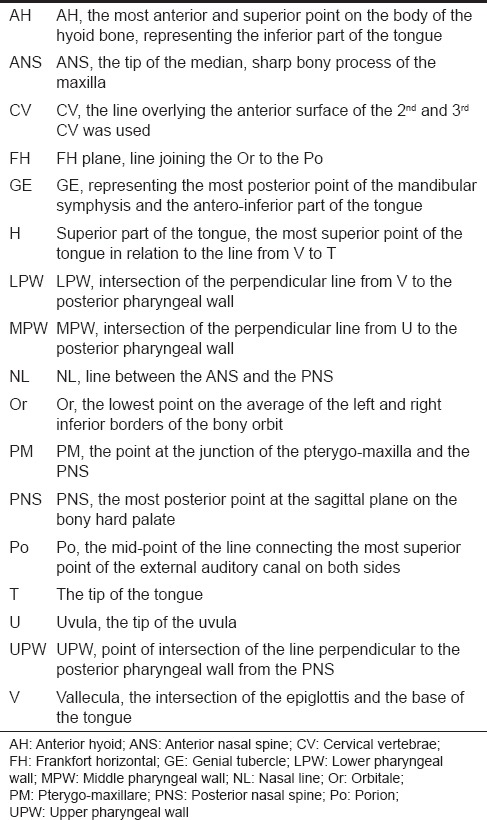
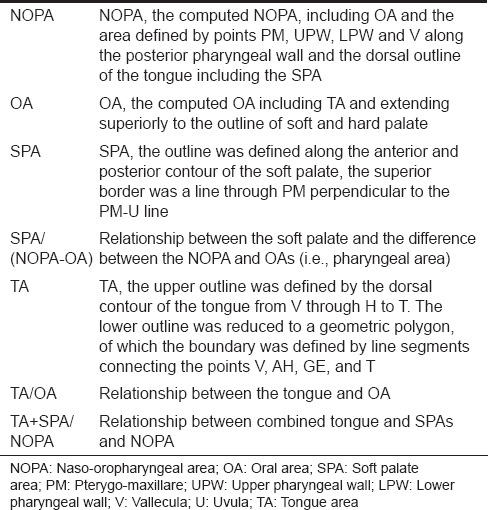
Table 2.
Description of linear measurements (mm) and angle measurement (degree) used
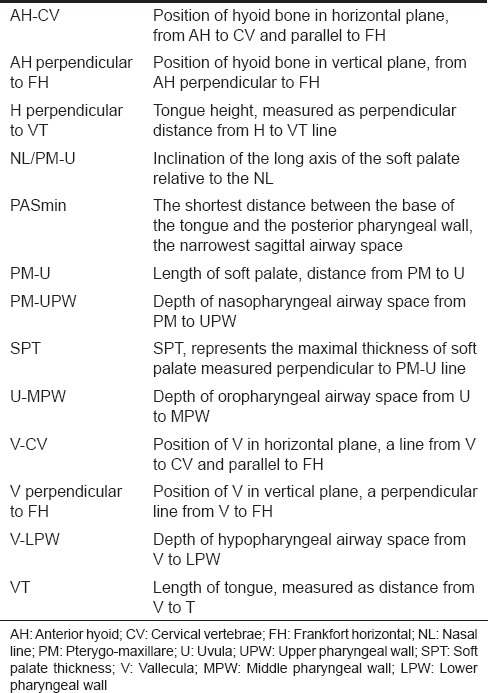
Table 3.
Description of area measurements (mm2) and ratios used
All lateral cephalometric radiographs were scanned by an HP ScanJet 4C scanner (HP, Guangzhou, China). The image was visualized on a 1280 × 1024 noninterlaced monitor. The landmarks were digitized, and the Frankfort plane was used as the horizontal plane during the measurements. Linear, angular, area, and ratio variables were measured and analyzed by computer software designed for that purpose.[33] The digitization and measurements were performed by the same investigator.
The magnification factor was taken into account for each cephalometric radiograph. The computer used in this study was an IBM compatible 486/66 D2 CPU-based personal computer with 16 MB RAM.
Reliability and error analysis
A random sample of 30 scanned cephalometric tracings were selected and digitized. The measurements were completed twice on two separate occasions, 4 weeks apart, by the same investigator. The mean value of the variables measured on each of the two occasions was compared using paired t-test to detect any systematic error in measurements made.
Statistics
Cephalometric variables for male and female subjects were compared using the Student's t-test and P value less than 5% was considered as significant. The statistical package used was the Statistical Package for Social Science (Windows version 6.0; SPSS Inc., Chicago, US).
Results
A total of 90 males and 90 females were included in the study. Males ranged in age from 8 to 16 years, and females from 8 to 16 years. The results of the error analysis found no significant difference between any of the paired measurements. The values for cephalometric airway measurements in males and females are compared in Table 4.
Table 4.
Comparison of results of cephalometric analysis of the upper airway in male and female subjects

Fourteen of the 20 measurements demonstrated a significant difference according to sex and overall, larger values was recorded for male subjects. The measurements for which no significant differences were seen between males and females included NL/PM-U, U-MPW depth, PASmin, and the three ratios of the area measurements TA/OA, (TA + SPA)/NOPA, and (SPA/NOPA-OA).
Discussion
This study contained a group of North Indian subjects based on their clinically normal facial profile and dental occlusion, and the absence of any reported abnormality of the upper airway. The cephalometric measurements of the upper airway in this group are thus appropriate to use as normative data for future comparison. In that study, cephalometric measurements of 180 normal subjects were analyzed to determine normative data for the North Indian populations. These researchers used the same measurement method as the current study and reported similar results.
In this study, the variables which did not demonstrate sex dimorphism were: PM-UPW, PASmin depth, and the ratio of TA/OA. This last finding is difficult to explain since one would not expect to see sex dimorphism of angle measurements or ratios. In the current study, all measurements bar six demonstrated sex dimorphism. The exceptions were NL/PM-U, U-MPW depth, PASmin, and all three ratios of area measurement. The two further variables that did not demonstrate sex dimorphism was the U-MPW depth and PAS min. These latter measurements are directly related to the patency of the airway, being the predominant levels at which the pharyngeal airway is reported to narrow in OSA.[10,12] Furthermore, oropharyngeal depth is the most variable measurement in the pharyngeal airway. Several studies in patients with OSA have demonstrated a significant reduction in two-dimensional and three-dimensional measurements at the oropharyngeal level, although this was not a consistent finding across subjects.[16,17,34] Two further measurements of clinical relevance to the patency of the airway are the PM-UPW depth and the V-LPW depth. It is evident from this study that although the majority of airway measurements demonstrate sex dimorphism, those that are most important to the patency of the airway are not dimorphic. This suggests that a minimal sagittal dimension of the upper airway is required for a normal patency.
Bacon et al.[35] used 40 normal subjects aged between 20 and 26 years (mean age, 23.7 years) as a control group in the cephalometric evaluation of pharyngeal obstructive factors in patients with OSA. These researchers reported the mean soft palate length in the male control group to be 38.7 mm (standard deviation [SD], 3.2 mm). Riley et al.[11] reported a normal soft palate length in Caucasian males of 37.0 mm, while our results indicate a soft palate length of 34.3 mm (SD, 3.9 mm). Hochban and Brandenburg,[34] in a cephalometric evaluation of OSA, reported the following measurements from their control group of Caucasian males (mean age, 43 years): Length of the soft palate, 45.1 mm; thickness of the soft palate, 12.2 mm; angle of the soft palate to the palatal plane, 54.5°; hypopharyngeal depth of the airway, 22 mm; and tongue length, 87 mm.
Lyberg et al.[20,21] performed cephalometric analysis of patients with OSA and reported the norms obtained from the control group of Caucasian males (n = 10; mean age, 23.6 years). They reported a magnification factor of approximately 6% but did not correct for this in their measurements.
Neither of the studies conducted by Lyberg et al.[20,21] included females as control subjects. Cephalometric norms for nasopharyngeal measurements were also reported by Poole et al.[36] Norms were calculated for various ages (6 and 16 years) and both sexes, and found to vary according to age and sex.
In establishing norms, however, these researchers used a random sample of patients for whom the presence or absence of nasopharyngeal obstruction was not known. In addition, all measurements were at the level of the nasopharynx and in the horizontal plane only, limited representation of the upper airway as a whole.
Thus, although a small number of studies have made cephalometric analyses of upper-airway measurements, these had notable limitations and reported results are not directly comparable to the current study for the following reasons:
The majority of investigations did not use a control group and hence lacked reference measurements for the norms. Rather, comparisons between two or more abnormal groups were made (such as OSA with postsurgical groups) in order to identify changes in upper-airway measurements
The magnification factor in many of these investigations was either not considered or not reported
The majority of studies did not include female control subjects, as most studies related to OSA which predominantly occurs in males.[37]
This limits comparison of measurements across studies, the results of which cannot be presumed to be applicable for the diagnosis of abnormalities in the North Indian population
In the current study, detailed cephalometric analysis of the upper airway was conducted, with due consideration of the magnification error for each cephalometric radiograph. The findings showed that there were significant differences between males and females in the size of the tongue, soft palate, nasopharynx, hypopharynx, and oral cavity, and in the relative position of the vallecula and the hyoid bone.
Conclusion
Cephalometric norms for the pharyngeal airway in the North Indian population have been established in this study.
Significant sex dimorphism was evident for measurements other than oropharyngeal depth of the airway, minimal depth of the airway, and the soft palate angle, suggesting that a minimal sagittal dimension is needed for a normal patency of the upper airway. Data derived from this study should thus prove useful as a reference for the assessment of OSA and other conditions in the North Indian population.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Steiner CC. Cephalometrics in clinical practice. Angle Orthod. 1959;29:8. [Google Scholar]
- 2.Khouw FE, Proffit WR, White RP. Cephalometric evaluation of patients with dentofacial disharmonies requiring surgical correction. Oral Surg Oral Med Oral Pathol. 1970;29:789–98. doi: 10.1016/0030-4220(70)90425-1. [DOI] [PubMed] [Google Scholar]
- 3.Haponik EF, Smith PL, Bohlman ME, Allen RP, Goldman SM, Bleecker ER. Computerized tomography in obstructive sleep apnea. Correlation of airway size with physiology during sleep and wakefulness. Am Rev Respir Dis. 1983;127:221–6. doi: 10.1164/arrd.1983.127.2.221. [DOI] [PubMed] [Google Scholar]
- 4.Suratt PM, Dee P, Atkinson RL, Armstrong P, Wilhoit SC. Fluoroscopic and computed tomographic features of the pharyngeal airway in obstructive sleep apnea. Am Rev Respir Dis. 1983;127:487–92. doi: 10.1164/arrd.1983.127.4.487. [DOI] [PubMed] [Google Scholar]
- 5.Bradley TD, Brown IG, Grossman RF, Zamel N, Martinez D, Phillipson EA, et al. Pharyngeal size in snorers, nonsnorers, and patients with obstructive sleep apnea. N Engl J Med. 1986;315:1327–31. doi: 10.1056/NEJM198611203152105. [DOI] [PubMed] [Google Scholar]
- 6.Remmers JE, deGroot WJ, Sauerland EK, Anch AM. Pathogenesis of upper airway occlusion during sleep. J Appl Physiol Respir Environ Exerc Physiol. 1978;44:931–8. doi: 10.1152/jappl.1978.44.6.931. [DOI] [PubMed] [Google Scholar]
- 7.Rodenstein DO, Dooms G, Thomas Y, Liistro G, Stanescu DC, Culée C, et al. Pharyngeal shape and dimensions in healthy subjects, snorers, and patients with obstructive sleep apnoea. Thorax. 1990;45:722–7. doi: 10.1136/thx.45.10.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maltais F, Carrier G, Cormier Y, Sériès F. Cephalometric measurements in snorers, non-snorers, and patients with sleep apnoea. Thorax. 1991;46:419–23. doi: 10.1136/thx.46.6.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pepin JL, Ferretti G, Veale D, Romand P, Coulomb M, Brambilla C, et al. Somnofluoroscopy, computed tomography, and cephalometry in the assessment of the airway in obstructive sleep apnoea. Thorax. 1992;47:150–6. doi: 10.1136/thx.47.3.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.deBerry-Borowiecki B, Kukwa A, Blanks RH. Cephalometric analysis for diagnosis and treatment of obstructive sleep apnea. Laryngoscope. 1988;98:226–34. doi: 10.1288/00005537-198802000-00021. [DOI] [PubMed] [Google Scholar]
- 11.Riley R, Guilleminault C, Herran J, Powell N. Cephalometric analyses and flow-volume loops in obstructive sleep apnea patients. Sleep. 1983;6:303–11. doi: 10.1093/sleep/6.4.303. [DOI] [PubMed] [Google Scholar]
- 12.Riley RW, Powell NB. Maxillofacial surgery and obstructive sleep apnea syndrome. Otolaryngol Clin North Am. 1990;23:809–26. [PubMed] [Google Scholar]
- 13.Friede H, Lopata M, Fisher E, Rosenthal IM. Cardiorespiratory disease associated with Hallermann-Streiff syndrome: Analysis of craniofacial morphology by cephalometric roentgenograms. J Craniofac Genet Dev Biol Suppl. 1985;1:189–98. [PubMed] [Google Scholar]
- 14.Figueroa AA, Glupker TJ, Fitz MG, BeGole EA. Mandible, tongue, and airway in Pierre Robin sequence: A longitudinal cephalometric study. Cleft Palate Craniofac J. 1991;28:425–34. doi: 10.1597/1545-1569_1991_028_0425_mtaaip_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 15.Gallagher DM, Hyler RL, Epker BN. Hemifacial microsomia: An anesthetic airway problem. Oral Surg Oral Med Oral Pathol. 1980;49:2–4. doi: 10.1016/0030-4220(80)90022-5. [DOI] [PubMed] [Google Scholar]
- 16.Lowe AA, Gionhaku N, Takeuchi K, Fleetham JA. Three-dimensional CT reconstructions of tongue and airway in adult subjects with obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 1986;90:364–74. doi: 10.1016/0889-5406(86)90002-8. [DOI] [PubMed] [Google Scholar]
- 17.Lowe AA, Santamaria JD, Fleetham JA, Price C. Facial morphology and obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 1986;90:484–91. doi: 10.1016/0889-5406(86)90108-3. [DOI] [PubMed] [Google Scholar]
- 18.Jamieson A, Guilleminault C, Partinen M, Quera-Salva MA. Obstructive sleep apneic patients have craniomandibular abnormalities. Sleep. 1986;9:469–77. doi: 10.1093/sleep/9.4.469. [DOI] [PubMed] [Google Scholar]
- 19.Guilleminault C, Riley R, Powell N. Obstructive sleep apnea and abnormal cephalometric measurements. Implications for treatment. Chest. 1984;86:793–4. doi: 10.1378/chest.86.5.793. [DOI] [PubMed] [Google Scholar]
- 20.Lyberg T, Krogstad O, Djupesland G. Cephalometric analysis in patients with obstructive sleep apnoea syndrome. I. Skeletal morphology. J Laryngol Otol. 1989;103:287–92. doi: 10.1017/s0022215100108734. [DOI] [PubMed] [Google Scholar]
- 21.Lyberg T, Krogstad O, Djupesland G. Cephalometric analysis in patients with obstructive sleep apnoea syndrome: II. Soft tissue morphology. J Laryngol Otol. 1989;103:293–7. doi: 10.1017/s0022215100108746. [DOI] [PubMed] [Google Scholar]
- 22.Tangugsorn V, Skatvedt O, Krogstad O, Lyberg T. Obstructive sleep apnoea: A cephalometric study. Part I. Cervico-craniofacial skeletal morphology. Eur J Orthod. 1995;17:45–56. doi: 10.1093/ejo/17.1.45. [DOI] [PubMed] [Google Scholar]
- 23.Tangugsorn V, Skatvedt O, Krogstad O, Lyberg T. Obstructive sleep apnoea: A cephalometric study. Part II. Uvulo-glossopharyngeal morphology. Eur J Orthod. 1995;17:57–67. doi: 10.1093/ejo/17.1.57. [DOI] [PubMed] [Google Scholar]
- 24.Yu LF, Pogrel MA, Ajayi M. Pharyngeal airway changes associated with mandibular advancement. J Oral Maxillofac Surg. 1994;52:40–3. doi: 10.1016/0278-2391(94)90011-6. [DOI] [PubMed] [Google Scholar]
- 25.Farole A, Mundenar MJ, Braitman LE. Posterior airway changes associated with mandibular advancement surgery: Implications for patients with obstructive sleep apnea. Int J Adult Orthodon Orthognath Surg. 1990;5:255–8. [PubMed] [Google Scholar]
- 26.Hochban W, Brandenburg U, Peter JH. Surgical treatment of obstructive sleep apnea by maxillomandibular advancement. Sleep. 1994;17:624–9. doi: 10.1093/sleep/17.7.624. [DOI] [PubMed] [Google Scholar]
- 27.Greco JM, Frohberg U, Van Sickels JE. Cephalometric analysis of long-term airway space changes with maxillary osteotomies. Oral Surg Oral Med Oral Pathol. 1990;70:552–4. doi: 10.1016/0030-4220(90)90394-8. [DOI] [PubMed] [Google Scholar]
- 28.Greco JM, Frohberg U, Van Sickels JE. Long-term airway space changes after mandibular setback using bilateral sagittal split osteotomy. Int J Oral Maxillofac Surg. 1990;19:103–5. doi: 10.1016/s0901-5027(05)80204-8. [DOI] [PubMed] [Google Scholar]
- 29.Wenzel A, Williams S, Ritzau M. Relationships of changes in craniofacial morphology, head posture, and nasopharyngeal airway size following mandibular osteotomy. Am J Orthod Dentofacial Orthop. 1989;96:138–43. doi: 10.1016/0889-5406(89)90254-0. [DOI] [PubMed] [Google Scholar]
- 30.Dahl E, Kreiborg S, Jensen BL, Fogh-Andersen P. Comparison of craniofacial morphology in infants with incomplete cleft lip and infants with isolated cleft palate. Cleft Palate J. 1982;19:258–66. [PubMed] [Google Scholar]
- 31.McWilliam J. Hypoplasia of the middle third of the face-a morphological study. Angle Orthod. 1976;46:260–7. doi: 10.1043/0003-3219(1976)046<0260:HOTMTO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 32.Fields HW, Warren DW, Black K, Phillips CL. Relationship between vertical dentofacial morphology and respiration in adolescents. Am J Orthod Dentofacial Orthop. 1991;99:147–54. doi: 10.1016/0889-5406(91)70117-F. [DOI] [PubMed] [Google Scholar]
- 33.Xia J. Quantitative analytic system of velopharyngeal function. Shanghai J Bioeng. 1992;10:16–9. [Google Scholar]
- 34.Hochban W, Brandenburg U. Morphology of the viscerocranium in obstructive sleep apnoea syndrome: Cephalometric evaluation of 400 patients. J Craniomaxillofac Surg. 1994;22:205–13. doi: 10.1016/s1010-5182(05)80559-1. [DOI] [PubMed] [Google Scholar]
- 35.Bacon WH, Turlot JC, Krieger J, Stierle JL. Cephalometric evaluation of pharyngeal obstructive factors in patients with sleep apneas syndrome. Angle Orthod. 1990;60:115–22. doi: 10.1043/0003-3219(1990)060<0115:CEOPOF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 36.Poole MN, Engel GA, Chaconas SJ. Nasopharyngeal cephalometrics. Oral Surg Oral Med Oral Pathol. 1980;49:266–71. doi: 10.1016/0030-4220(80)90059-6. [DOI] [PubMed] [Google Scholar]
- 37.Gislason T, Almqvist M, Eriksson G, Taube A, Boman G. Prevalence of sleep apnea syndrome among Swedish men: An epidemiological study. J Clin Epidemiol. 1988;41:571–6. doi: 10.1016/0895-4356(88)90061-3. [DOI] [PubMed] [Google Scholar]


