Abstract
Ectodermal dysplasia is a heterogeneous group of inherited disorders, which exhibit a classic triad of hypohydrosis, hypotrichosis, and hypodontia. Hypohidrotic or anhidrotic ectodermal dysplasia or Christ Siemens Touraine syndrome is the most common condition among ectodermal dysplasia patients. This is a case report on two Christ Siemens Touraine syndrome cases and two different approaches to prosthetic management.
Keywords: Congenital anodontia, hypohydrotic ectodermal dysplasia, prosthetic rehabilitation
Introduction
Ectodermal dysplasia is defined by National foundation for ectodermal dysplasia as a genetic disorder in which there are congenital birth defects of two or more ectodermal structures.[1] The term ectodermal dysplasia was coined by Weech in 1929.[2] Ectodermal dysplasia is rare with their incidence at 1 in 10,000–1 in 100,000 births.[3] The most common ectodermal dysplasia is X-linked recessive hypohidrotic ectodermal dysplasia (Christ Siemens Touraine syndrome) and hydrotic ectodermal dysplasia (Clouston syndrome).[4,5] In this case report, we are describing two different management approaches of two Christ Siemen Touraine syndrome cases.
Case Reports
Case 1
A 7-year-old patient reported to our department with a complaint of multiple missing teeth. Detailed case history revealed that he was intolerant to heat and did not sweat. Extraoral examination revealed sparse hair, prominent chin, protuberant, and everted lips. Skin was dry and rough, and his nails were rough and brittle. Intraoral examination revealed hypodontia of lower arch and anodontia of the upper arch [Figure 1]. Skin biopsy revealed decreased number of sweat glands, and orthopantomogram (OPG) showed congenitally missing teeth and tooth bud of two permanent incisors.
Figure 1.

Case 1: Clinical features
Our treatment plan was to give a removable partial denture in the upper and complete denture in lower arch [Figure 2].
Figure 2.
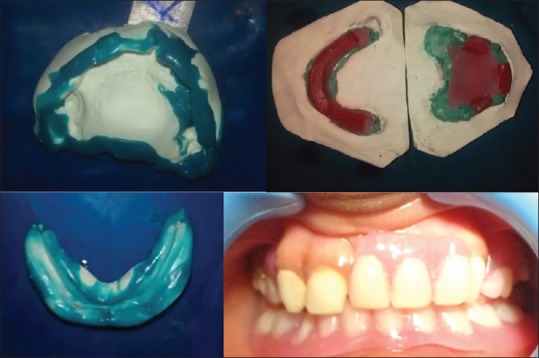
Case 1: Prosthetic rehabilitation
Case 2
A 5-year-old patient reported to the pediatric and preventive dentistry department with a complaint of lower space maintainer getting dislodged continuously. Detailed case history revealed the child to have been diagnosed with Christ Siemens Touraine syndrome. Thorough clinical examination revealed features such as sparse hair, dry and rough skin and a lack of tolerance to heat and inability to sweat normally. Intraoral examination revealed that the factors that prevented the space maintainer from being seated are a highly retroclined lower lip resting on the lower arch and lingually tipped lower molar bilaterally rendering the clasps of the space maintainer unable to engage the molars. OPG revealed congenitally missing teeth and presence of the maxillary incisors and first molar on all quadrants in the secondary dentition [Figure 3].
Figure 3.

Case 2: Prosthetic rehabilitation using removable partial denture in the upper arch and fixed partial denture in lower arch
Our treatment plan was to give a removable space maintainer in the upper arch and to convert the removable space maintainer to a fixed one in the lower arch. The lower molars were banded, and the removable space maintainer was trimmed and attached to an orthodontic wire, which was soldered onto the bands.
Discussion
In many cases, dentists are the first to identify this condition as the patients report with multiple missing teeth. Hence, dentists play an important role in the diagnosis and management of ectodermal dysplasia.[5,6] Prosthetic rehabilitation is the mainstay in the pediatric dental setup.[7] The method of prosthetic rehabilitation is chosen based on the features and the characteristics of each individual case.[8]
In the first case, a removable space maintainer was chosen as the feature of the patient was ideal for such a line of management and implants were not considered due to the age of the patient. In the second case, a fixed space maintainer was chosen in the lower due to the constant displacement of the fixed space maintainer by the lower lip and disengagement of clasps from the lower molars. The function and esthetics of both cases were successfully restored in both cases.
Implants were not considered in both cases taking into consideration the age of the patient. Implants are not the ideal prosthetic solution in growing maxilla and mandible. The possibility of a tooth bud developing at a later stage cannot be ruled out, and implants would hamper such a development.
The prosthetic management of both cases achieved multiple goals such as:
Restoring masticatory function
Enhancing the esthetics
Elevating the confidence of the patients
Improved the lower vertical height of the face
Reduced the angular folds of lip drastically reducing the possibility of fungal infections
Improved the patients’ quality-of-life.
Once the patients attain complete craniofacial growth, an implant-supported prosthesis shall be placed which is the ideal long-term dental management of Christ Siemens Touraine syndrome.
Conclusion
As the dentist is the first to meet the child in most cases, in depth knowledge about the features of ectodermal dysplasia is imperative and intricate understanding of the treatment modalities is essential from the clinicians’ side. The successful management of such cases will ensure the functional and esthetic requirement of the patient and thereby increase the self-esteem of the child.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Ranjan V. Ectodermal dysplasia – A case report and review of literature. [Last accessed on 2015 Jan 15];J Dentofacial Sci. 2013 2:27–30. Available from: http\\www.journalofdentofacialscience.com. [Google Scholar]
- 2.Kayalvizhi G, Neeraja R. Christ-siemens – Touraine syndrome with self-mutilation habit: An unusual presentation. Int J Clin Pediatr Dent. 2009;2:52–5. doi: 10.5005/jp-journals-10005-1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jain D, Jain S, Kumar A, Rahangdate T. Hypohidrotic ectodermal dysplasia: Prosthetic and endodontic management. Int J Clin Pediatr Dent. 2010;3:63–7. doi: 10.5005/jp-journals-10005-1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bala S, Nikhil M, Chugh A, Narwal A. Prosthetic rehabilitation of a child suffering from hypohidrotic ectodermal dysplasia with complete anodontia. Int J Clin Pediatr Dent. 2012;5:148–50. doi: 10.5005/jp-journals-10005-1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Srivastava VK. Ectodermal dysplasia: A case report. Int J Clin Pediatr Dent 201. 4:269–70. doi: 10.5005/jp-journals-10005-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deshmukh S, Prashanth S. Ectodermal dysplasia: A genetic review. Int J Clin Pediatr Dent. 2012;5:197–202. doi: 10.5005/jp-journals-10005-1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh T, Singh R, Singh GP, Singh JP. Hypohidrotic ectodermal dysplasia: A felicitous approach to esthetic and prosthetic management. Int J Clin Pediatr Dent. 2013;6:140–5. doi: 10.5005/jp-journals-10005-1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ohno K, Ohmori I. Anodontia with hypohidrotic ectodermal dysplasia in a young female: A case report. Pediatr Dent. 2000;22:49–52. [PubMed] [Google Scholar]


