Abstract
Background
Communication, impulse control and motivation can all be affected by Bipolar Disorder (BD) making consistent parenting more difficult than for parents without mental health problems. Children of parents with BD (CPB) are at significantly increased risk of a range of mental health issues including Attention Deficit Hyperactivity Disorder (ADHD), anxiety, depression, substance use, and sleep disorders. Furthermore, CPB are also at elevated risk for BD compared to the general population. This paper describes the rationale and protocol for a pilot randomised controlled trial (RCT) designed to assess the feasibility and acceptability of a new online intervention providing interactive psychoeducational information and parenting support for parents with BD.
Methods and design
This article describes a single-blind randomised controlled trial comparing an Integrated Bipolar Parenting Intervention (IBPI) in addition to treatment as usual (TAU) with TAU alone. Participants will be recruited from across the UK from mental health services and through self-referral. The primary outcome of the study is the feasibility and acceptability of IBPI as indicated by recruitment to target, use of the intervention site, and retention to follow-up. Parents with BD allocated to the IBPI condition will have access to the intervention for 16 weeks. Effect size estimates will be obtained with respect to child behaviour, parenting skills and measures of parental mental health using measures taken at baseline (0), and at 16, 24, 36, and 48 weeks post randomization.
Discussion
This is the first randomised controlled trial of an integrated bipolar disorder parenting intervention. The benefits and challenges of delivering this online intervention, and evaluation using online RCT methodology are discussed.
Trial registration
Current Controlled Trials ISRCTN75279027 Registered 12 August 2013
Background
Bipolar Disorder (BD), which has a prevalence rate of approximately 1 to 1.5 % [1] is characterised by recurrent periods of high mood (mania) and low mood (depression). Difficulties with work-related performance, financial issues, social/leisure activities and social/family relationships are common [2], though positive experiences of BD have also been identified [3]. Overall, BD tends to have a significant negative impact on the individual, family, and society, with an estimated annual financial cost in England alone of £5.2 billion [4].
Many individuals with mental health problems are also parents. An Australian study estimated that 23 % of children live in families with at least one parent with a mental health illness and 20 % of users of mental health services have dependent children [5]. The Royal College of Psychiatrist’s report ‘Parents as patients: supporting the needs of patients who are parents and their children’ [6] has highlighted the potential impact of parental mental health issues on children, especially severe mental illness, such as bipolar disorder. Parenting can be a particular challenge for parents who are living with bipolar disorder, as there can be difficulties with sleep/wake cycles, impulse control, motivation and communication [7,8] which can impact on their ability to consistently engage in adaptive parenting.
There is now consistent evidence that children of parents with BD (CPB) are vulnerable to a wide range of behavioural and emotional conditions including Attention Deficit Hyperactivity Disorder (ADHD), anxiety, depression, substance use, and sleep disorders, in addition to higher rates of BD compared to the general population [9-11]. However, it is possible that parenting programmes, designed to help parents to encourage desirable behaviour and cope with challenging behaviour in their children may be effective in enhancing the confidence and skills of bipolar parents, and in doing so, can help ameliorate these vulnerabilities. Parenting programmes are delivered in a range of formats from group settings to online and typically build on parenting strengths rather than highlighting weaknesses. There is evidence that such programmes can effectively reduce child problem behaviours including conduct, antisocial behaviour and attention deficit disorders [12-14].
A particular parenting programme (Triple P), developed by one of the authors (MS) has been shown to be effective in reducing problem behaviours and in improving both parenting skills and parental wellbeing [15]. In addition, there is evidence that in depressed mothers Triple P led to reductions in both maternal depression and in problem behaviour in their children [16]. Although there are Triple P studies which have included teenagers, the majority of trials have focussed on parents of pre-teenage children typically aged 2–3 to 9–11 [15].
There is a high demand for both structured psychological interventions for mental health issues [17] as recommended by National Institute for Clinical Excellence [18] and for community based parenting support [19,20]. However many individuals struggle to access either of these types of intervention due to lack of suitably trained therapists. The internet (currently used by 73 % of the UK population [21]) provides an alternative to face to face interventions offering the potential to deliver self-management help flexibly (at the time and location chosen by the client), cheaply and without the stigma that some people feel is associated with seeking support from mental health services [22].
A pilot study by our team has shown that providing simple psychoeducational information on BD along with an early online version of the Triple P Positive Parenting Program led to significant improvements in child behaviour and parenting [23]. The present study builds on this work using a new interactive self-management site for BD developed for the study and integrated with the most recent version of Triple P Online, [24] to provide a web-based integrated bipolar parenting intervention (IBPI).
This paper describes the rationale and protocol for a pilot randomised controlled trial (RCT) of IBPI designed to assess how feasible it is to implement an online parenting intervention for parents with BD. The study will therefore evaluate as primary outcomes, recruitment into the study and consent to participate, retention to the intervention and to follow-up assessments (both arms). The trial will also provide preliminary estimates of the impact of the intervention on child behaviour, parenting skill and confidence, parental mood (including time to further mood episodes) and family functioning.
Method
This trial is conducted by a multidisciplinary team of researchers, clinicians, service users, and a statistician across academic institutions and NHS Trusts in the United Kingdom. This study was reviewed and approved by the UK NHS Ethics Committee process (REC ref: 12/NW/0749).
Objective
To determine the feasibility and acceptability of an online integrated parenting intervention for bipolar disorder compared with treatment as usual.
Main research questions:
To demonstrate feasibility of recruitment and consenting procedures, adherence to intervention and retention to both arms of the trial across assessment, intervention and 16, 24, 36 and 48 week follow up periods.
To provide parameter estimates of clinical outcomes with respect to, child behaviour, parenting skills, mood, and family functioning.
Trial design
A rater-blind randomised controlled trial which compares sixteen weeks of access to an online integrated bipolar parenting intervention (IBPI) plus treatment as usual (TAU) with TAU alone. The trial is based in the United Kingdom. Randomisation will be carried out by the independent Clinical Trials Unit at The Christie NHS Foundation Trust, Manchester.
Sample size
The chief purpose of this trial is to evaluate the feasibility and acceptability of providing IBPI, thus a formal power calculation for a test comparing treatment groups is not appropriate.
The primary outcome, to demonstrate feasibility, will be recruitment into the trial and the proportion of completers of the intervention and of assessments at 16, 24, 36 and 48 weeks follow-up. Thirty participants per group, i.e. 60 in total, is sufficient to reliably determine the primary feasibility outcomes for the trial. We therefore aim to recruit N = 100 across both arms of the study to allow for a potential drop-out rate of up to 35-40 % based on an average of attrition rates across 4 relevant studies of web-based interventions for affective and/or parenting issues [20,24-26].
Recruitment
Participants will be recruited in two ways:
Clinician Referral Route
Seventeen National Health Service (NHS) Trusts across the UK are taking part in this study. Community mental health teams, out-patient clinics, GP surgeries, primary care mental health teams and voluntary services will identify potential participants. Care coordinators, research nurses and research development officers will be approached in order to contact potential participants in the first instance. When recruiting in community mental health teams and voluntary services, a member of the research team will present an outline of the study and will provide written material about the study. Potential participants will be offered a participant information sheet by their care co-ordinators or the research team, outlining the study and their role should they wish to take part.
-
2.
Self-Referral Routes
The study will be advertised in the media using social networks, such as Facebook, Twitter, relevant online forums and via adverts in local press. Posters and leaflets will be distributed in both NHS and non NHS sites such as relevant third sector bases (i.e. mental health organisations and parenting advice or children’s centres) to maximise participant access. There will be a significant focus on online recruitment. Due to the nature of the study, it is assumed that potential participants seeking advice online are more likely to engage with such an intervention.
Clinicians will be informed of a participant’s involvement in the study subject to participant consent. If a participant does not wish for their primary or secondary care clinician to be informed about their involvement in the study, this does not prevent their participation as long as they consent to their clinician being contacted should they be a significant risk to themselves or others during the study. Figure 1 gives an outline of the participant flow through the study.
Figure 1.
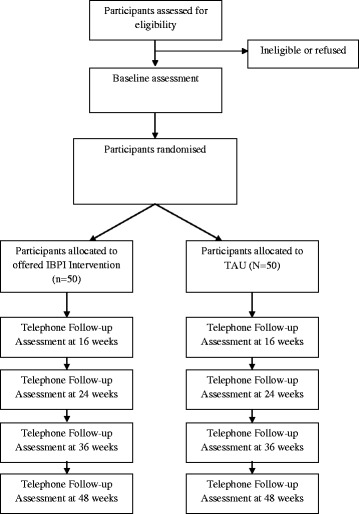
CONSORT diagram showing design of the study
Participants will be asked to express an interest in the study which will act as a ‘run in period’ before consent, so that any potential drop outs occur prior to consent to minimise attrition during the trial [24]. This should also ensure that participants are providing informed consent and are fully committed and motivated to take part in the study before randomisation.
Participants who express an interest in the study, either through self-referral or team referral routes, will be contacted by the IBPI team by telephone to complete a pre-screen form to assess their likely eligibility and be given information regarding the study. If they confirm their wish to participate they will be emailed a participant information pack and web link directing them to consent online. The online link will take the participant to the study website consent screens, each presenting a single clause of the consent form. A consent button is used for each page to ensure there is clear consent to the study as a whole before proceeding to a final screen in which the individual provides their name, email address and telephone number to permit data validation, confirm identity and facilitate contact as required to support assessments. Online registration data will be stored on the secure study database. Once registered, each participant will be provided with login information for both bipolar and parenting modules.
Inclusion/exclusion criteria
Potential participants must meet the inclusion criteria of:
Structured Clinical Interview for DSM-IV Axis I Disorders (SCID) verified diagnosis of bipolar disorder (I, II or Not Otherwise Specified) [27]
Have at least one child aged 3 to 10 years
Have an average of at least 10 h face-to-face contact with this child each week
Have access to the internet
Sufficient understanding of written and spoken English in order to provide consent, engage with interviews, complete measures and use the intervention
Exclusion criteria:
Absence of inclusion criteria
Have a primary diagnosis of alcohol or other substance misuse
Unable or unwilling to provide informed consent
Parent currently receiving an evidence based structured parenting intervention and/or intensive psychotherapy
The index child currently in receipt of intensive structured psychological therapy and/or currently the subject of child protection proceedings
Outcome measures
To evaluate the feasibility and acceptability of delivering the IBPI intervention the following data will be evaluated: levels of recruitment into the trial; retention of participants in both arms of the study and adherence to and completion of the intervention (website useage).
Structured Clinical Interview for DSM-IV at baseline will be used to confirm bipolar diagnosis and to provide sociodemographic information. Measures of clinical outcome will be recorded at baseline and follow-ups to provide an indication of the effectiveness of the intervention on child behaviour, and parenting skills and confidence. Secondary outcomes are levels of self-reported affective mood symptoms and time to mood episodes and family functioning. All observer-rated follow-up assessments are conducted by telephone, all self-report assessments are completed online.
Feasibility and acceptability outcomes
The primary outcome of the study is the feasibility and acceptability of IBPI. Feasibility will be measured by recruitment to target and retention to follow-up as well as absence of untoward incidents associated with IBPI. Acceptability will be measured by adherence to intervention through website usage data (pattern and frequency of module access).
Measurement of primary clinical outcomes
Hypotheses are that IBPI will improve i) Child Behaviour as perceived by the parents and measured by the Strengths and Difficulties Questionnaire (SDQ) [28] and Eyberg Child Behavior Inventory (ECBI) [29]; and ii) Parenting Skills and confidence as measured by the Parenting Scale (PS3) [30], Parenting Sense of Competency Scale (PSOC) [31,32] and Parenting Stress Index (PSI) [33].
Measurement of secondary outcomes
Hypotheses are that IBPI will improve; i) Self-reported symptoms of mania and depression (Internal States Scale (ISS) [34] Centre for Epidemiologic Studies Depression Scale (CES-D) [35] and the Altman Rating Scale (AMRS) [36]; ii) Observer rated time to relapse and mood symptoms (Structured Clinical Interview for DSM-IV-TR AXIS 1 DISORDERS - LIFE (SCID-LIFE) [37], Hamilton Depression Rating Scale (HAM-D) [38], Bech-Rafaelsen Mania Scale (MAS) [39]; iii) family coherence measured by the Confusion, Hubbub and Order Scale (CHAOS) [40].
Schedule of assessments
The first follow up assessment occurs 16 weeks from randomisation. See Table 1 for more details on specific assessments and follow up periods. Online assessment measures will be delivered via the LimeSurvey open source questionnaire system (https://www.limesurvey.org/en/). At each online assessment point, participants will be sent an email asking them to follow the link provided to complete the measures. The research team web developer (RP) will monitor the completion of questionnaires and send reminder emails on a regular basis. In the event that email contacts do not elicit a response, the team will make telephone calls to facilitate the completion of measures where such support may be required.
Table 1.
Schedule of assessments
| Time point | Type of outcome | Outcome measures | Measuring change in |
|---|---|---|---|
| • Baseline | Feasibility | Recruitment and retention to follow-up | N/A |
| • 16, 24, 36, 48-weeks post randomization | N/A | ||
| • During intervention | Adherence to intervention and website usage | ||
| • 16-weeks post randomization | Acceptability | N/A | |
| • Baseline, | Primary Clinical | SDQ | Child Behaviour |
| • End of intervention (16 weeks), and | ECBI | Child Behaviour | |
| PS3 | Parenting | ||
| • 24-, 36-, and 48- weeks post randomization. | PSOC | Parenting | |
| PSI | Parenting | ||
| Via online survey | Secondary Clinical | ISS | Parent symptoms |
| CES-D | Parent symptoms | ||
| AMRS | Parent symptoms | ||
| CHAOS | Parent symptoms | ||
| • Baseline, | Secondary Clinical | SCID-LIFE | Parent symptoms |
| • 24- and 48-weeks post randomization. | HAM-D | Parent symptoms | |
| MAS | Parent symptoms | ||
| Via phone interview with RA |
Integrated bipolar parenting intervention
An 8 module intervention will be provided to parents offering self-management strategies for bipolar disorder (see Table 2). This is programmed based on the Drupal open source content management system written in PHP with a MySQL database. All modules were developed in partnership with service users with lived experience of bipolar disorder and parenting. The modules listed below cover a range of aspects of living with bipolar disorder all providing a mixture of information, video clips from professionals and service users and self-evaluation exercises. Each module topic is presented in the context of both bipolar disorder and parenting – for instance the ‘benefits and challenges’ module looks at how bipolar mood experiences can have both positive and negative impacts on parenting.
Table 2.
List of IBPI modules
| Bipolar Modules | Triple P Modules | |
|---|---|---|
| 1 | What is bipolar disorder? | What is positive parenting? |
| 2 | Benefits and challenges | Encouraging desirable behaviour |
| 3 | Managing emotions | Teaching new skills and behaviour |
| 4 | Knowing yourself | Managing misbehaviour |
| 5 | Mood monitoring | Dealing with disobedience |
| 6 | Playing to your strengths | Preventing problems by planning ahead |
| 7 | Planning for yourself | Making shopping fun |
| 8 | Finding support and final thoughts | Raising confident competent kids |
After each bipolar module the participant is offered access to the linked parenting module from the Level 4 Triple P online intervention [24]. Both elements of the IBPI intervention share interactive and multimedia features including: video clips, interactive exercises, self-evaluation exercises. Both also share a normalising, self‐regulatory focus to specifically avoid stigmatising or blaming participants.
Each module will typically last around 30 mins and it is anticipated that parents will cover around 1 module per week. Each parent allocated to the intervention arm of the trial has access to the intervention for 16 weeks. Participants are offered modules in the order noted above as they follow logically from one to the next. However, this order of module completion is not obligatory so participants can select modules as they wish and return to those which they find most useful.
Analysis
Feasibility outcomes
The primary purpose of the study is to evaluate the feasibility and acceptability of delivering IBPI therefore a formal power calculation comparing treatment groups is not required. We anticipate that approximately 60 % of subjects will complete the assessment. With 100 subjects recruited across both treatment arms, this proportion will be estimated with 95 % confidence limts +/−9.6 %. The corresponding limits for the estimated proportion within each treatment arm will be +/− 13.6 %
Feasibility is a binary outcome. A simple logistic regression analysis will be used to estimate the probabilities of completion of follow-up in each group at each assessment point, and the differences between the two. Acceptability will be evaluated by analysis of web useage data. Pattern and frequency of module access will be explored through time to access the site from account creation, number of views of each module, order of viewing of modules and number of specific page views.
Clinical and functional outcomes
Clinical and functional outcomes consist of repeated measurements. These will be taken at weeks 0, 16, 24, 36 and 48 following randomisation for most measures, except SCID-LIFE, HAM-D and MAS which will be recorded a 0, 24,and 48 weeks (but assessment of episodes covers all the weeks from the previous assessment). Records on participants who drop out of the study before week 48 will be incomplete. Analysis of measurements and dropout times will include checks that groups are balanced with respect to age, gender, level of education and use of services, and control for these as required, followed by linear modelling with correlated errors for the repeated measurements and linked logistic regression models for the probability of dropout conditional on the repeated measurements prior to dropout [41]. In order to inform the design of a definitive trial, these analyses will investigate which patient characteristics affect the repeated measurement outcomes and/or the probability of dropout.
To determine how well IBPI worked for those who did not drop-out, the main clinical outcome measure is D, the difference in SDQ and PS pre- and post-intervention. The corresponding primary analysis will be a two-sample t-test comparing values of D in the two groups. Post-intervention, it is hypothesised that participants who received IBPI will have a greater D than those receiving assessments only. We will also explore website usage data.
Discussion
This study will provide important data for the development of a future definitive IBPI trial should the results of this trial look promising. The online parenting intervention IBPI has been developed with experts in positive parenting interventions, experts in the self-management of bipolar disorder and individuals who have experience of bipolar disorder consistent with Mental Health Research Network good practice guidelines [42]. In addition, service user involvement has been a core aspect of the research process, from inception of ideas through to the development of the methodology, outcome measures and the intervention. The intervention itself promotes positive parenting and builds upon skills which parents already possess. There is currently no other known intervention which specifically provides targeted support for parents with bipolar disorder.
Strengths of the study include a focus on an intervention which integrates strategies to aid living well with bipolar disorder in the context of being a parent of young children. It also offers the potential to increase access to evidence-based support for a group who currently have limited access to psychological interventions in general and particularly to interventions which also incorporate consideration of the challenges of parenting. The diverse nature of the research and intervention development team have ensured that the intervention is grounded in lived experience of being a parent with bipolar disorder, with the addition of opinions from experts in the field. The nature of IBPI means that each parent can personalise and tailor their own intervention, allowing them to get the most out of it for their circumstances. The intervention is intended to be both flexible and appealing, acknowledging the issue of engagement. All modules can be started, paused and recommenced when convenient or when feeling able to focus on the content.
The online RCT aims to be as rigorous as a traditional RCT but reducing the impact of potentially confounding variables such as extensive contact with the research team. In line with the definition of Mathieu et al. [43] the current trial is primarily rather than fully on line (as not all of the assessments are completed online). Participation in the trial is from home and observer-rated assessments are made via the telephone consistent with this minimal contact (whilst all self-report measures are completed online). A diagnosis of bipolar disorder is verified at baseline; followed by a series of outcome measures at baseline and then at follow up time points. Evaluating IBPI online makes it possible to recruit participants nationally, and capture outcome data instantaneously. This study is recruiting from across NHS primary and secondary care settings throughout the United Kingdom and through self-referral with a focus on online recruitment. Therefore, the findings should be more representative of a group of parents with bipolar disorder who use the internet for parenting support. This means higher levels of reliability, and validity without the cost implications and resources necessary in traditional RCTs.
The weaknesses of this study would need to be addressed in a later definitive trial. However, parenting in bipolar disorder is an area where little is known about the effects of a targeted intervention. The study allows individuals to be followed up for a period of 48 weeks following the use of the IBPI intervention. Further follow-ups would be helpful to indicate more definitively whether this intervention has a sustained impact on longer term parenting and mood outcomes. As the current focus of this trial is on parents of children from 3 to 10 it will not indicate whether this integrated approach might have potential as children enter teenage years and beyond (when risk for increased psychopathology in offspring is detected [44]).
The online nature of this intervention study means that there is a lack of human contact including the absence of a therapist. This potentially puts more demands on the individual to apply self-management strategies on their own initiative. However, this might also be an advantage for some participants, particularly in the context of evidence that individuals with bipolar disorder typically place high value on autonomy [45]. It has been suggested that computer mediated studies may provide an environment which encourages socially desirable or unreliable responding [46]. However, there is contrasting evidence to suggest that such studies are equally as reliable as traditional methods of outcome data collection [47] and it has been argued that the anonymous online environment allows participants to express their opinions and feelings more freely, thus, reducing unreliable responding when completing outcome measures online [48].
In summary, if the current study indicates that IBPI is an acceptable and feasible intervention, in addition to potential clinical benefits it will be an important step towards developing evidence-based interventions for parents with bipolar disorder that have been lacking until now.
Acknowledgements
This report presents independent research commissioned by the Medical Research Council (Grant number: MR/J011886/1). We would like to thank service users who have contributed to the development of the intervention through the service user reference group and the Spectrum Centre advisory panel.
Funding
Medical Research Council Experimental Medicine for Mental Health Grant.
Footnotes
Competing interests
This trial reports on both the development and evaluation of the IBPI intervention, the latter is therefore not independent.
Rachel Calam has long standing research collaborations with staff at the Parenting and Family Support Centre, School of Psychology, University of Queensland. She has been a board member of the Triple P Research Network and is currently on the Triple P International Scientific Advisory Committee in a research capacity. The Parenting and Family Research Group at The University of Manchester and its members have no share in, ownership of, or formal relationship with, Triple P International Pty Ltd and derive no funding or royalty from it.
Matthew Sanders is the founder of Triple P and a contributory author of Triple P Online. The Triple P – Positive Parenting Program is owned by The University of Queensland (UQ). The University through its main technology transfer company, UniQuest Pty Ltd, has licensed Triple P International Pty Ltd to publish and disseminate the program worldwide. Royalties stemming from published Triple P resources are distributed to the Faculty of Health and Behavioural Sciences at UQ, Parenting and Family Support Centre, School of Psychology at UQ, and contributory authors. No author has any share or ownership in Triple P International Pty Ltd.
Authors’ contributions
SJ is the principal investigator responsible for the conduct of the study. He led the design of the research, the development of the intervention and the write-up of this paper. LW, JJ and HV are researchers responsible for recruitment and follow-up of participants: all have contributed to drafts of the current paper. PD is the statistical expert for the study. RC is the study expert in child developmental issues. RP developed the website and the online assessment procedures. DM helped develop the protocol and originally convened service user consultation groups, RL is service user lead for the project. MS is the originator of the Triple P approach and provided expert input on Triple P to the study. FL is an expert on relapse prevention. All authors have contributed to the final version of the paper. All authors read and approved the final manuscript.
Contributor Information
Steven Jones, Email: s.jones7@lancaster.ac.uk.
Laura D Wainwright, Email: l.wainwright@lancaster.ac.uk.
Jelena Jovanoska, Email: jovanosk@exchange.lancs.ac.uk.
Helen Vincent, Email: h.vincent@lancaster.ac.uk.
Peter J Diggle, Email: p.diggle@lancaster.ac.uk.
Rachel Calam, Email: rachel.calam@manchester.ac.uk.
Rob Parker, Email: r.j.parker@lancaster.ac.uk.
Rita Long, Email: r.long2@lancaster.ac.uk.
Debbie Mayes, Email: d.mayes@lancaster.ac.uk.
Matthew Sanders, Email: matts@psy.uq.edu.au.
Fiona Lobban, Email: f.lobban@lancaster.ac.uk.
References
- 1.Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, Kessler RC. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National 41 Comorbidity Survey replication. Arch Gen Psychiatry. 2007;64:543–52. doi: 10.1001/archpsyc.64.5.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Michelak EE, Yatham LN, Kolesar S, Lam RW. Bipolar disorder and quality of life: a patient-centred perspective. Qual Life Res. 2006;15:25–37. doi: 10.1007/s11136-005-0376-7. [DOI] [PubMed] [Google Scholar]
- 3.Lobban F, Taylor K, Murray C, Jones S. Bipolar disorder is a two-edged sword: a qualitative study to understand the positive edge. J Affect Disord. 2012;141:204–212. doi: 10.1016/j.jad.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 4.McCrone P, Dhanasiri S, Patel A, Knapp M, Lawton-Smith S. Paying the price: the cost of mental health care in England to 2026. London: The King's Fund; 2008. [Google Scholar]
- 5.Maybery D, Reupert A, Goodyear M, Crase L. Prevalence of children whose parents have a mental illness. Psychiat Bull. 2009;33:22–6.
- 6.Royal College of Psychiatrists . Parents as patients: supporting the needs of patients who are parents and their children. London: Royal College Report CR164; 2011. [Google Scholar]
- 7.Vance Y, Jones S, Espie J, Bentall R, Tai S. Parental communication style and family relationships in children of bipolar parents. B J Clin Psychol. 2007;47:355–9. doi: 10.1348/014466508X282824. [DOI] [PubMed] [Google Scholar]
- 8.Phelan R, Lee L, Howe D, Walter G. Parenting and mental illness: a pilot group program. Australasian Psychiat. 2006;14:399–402. doi: 10.1080/j.1440-1665.2006.02312.x. [DOI] [PubMed] [Google Scholar]
- 9.Birmaher B, Axelson D, Monk K, Kalas C, Goldstein B, Hickey MB, et al. Lifetime psychiatric disorders in school-aged offspring of parents with bipolar disorder: the Pittsburgh bipolar offspring study. Arch of Gen Psychiat. 2011;66:287–96. [DOI] [PMC free article] [PubMed]
- 10.Duffy A, Alda M, Crawford L, Milin R, Grof P. The early manifestations of BD: a longitudinal prospective study of the offspring of bipolar parents. Bipolar Disorders. 2007;9:828–38. doi: 10.1111/j.1399-5618.2007.00421.x. [DOI] [PubMed] [Google Scholar]
- 11.Jones S, Bentall R. A review of potential cognitive and environmental risk markers in children of bipolar parents. Clin Psychol Rev. 2008;28:1083–1095. doi: 10.1016/j.cpr.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 12.Sanders MR. The triple P – positive parenting program – a public health approach to parenting support. J Fam Psychol. 2008;22:506–517. doi: 10.1037/0893-3200.22.3.506. [DOI] [PubMed] [Google Scholar]
- 13.Reupert A, Maybery D. Programmes for parents with a mental illness. J Psychiatr Mental Health Nurs. 2011;18:257–264. doi: 10.1111/j.1365-2850.2010.01660.x. [DOI] [PubMed] [Google Scholar]
- 14.NICE . Antisocial behaviour and conduct disorders in children and young people: recognition, intervention and management CG158. London: National Institute for Clinical Excellence; 2013. [Google Scholar]
- 15.Nowak C, Heinrichs N. A comprehensive meta-analysis of triple P - positive parenting program using hierarchical linear modeling: effectiveness and moderating variables. Clin Child Fam Psychol Rev. 2008;11:114–144. doi: 10.1007/s10567-008-0033-0. [DOI] [PubMed] [Google Scholar]
- 16.Sanders MR, Markie-Dadds C, Tully L, Bor W. The triple P positive parenting program: a comparison of enhanced, standard, and self-directed behavioral family intervention for parents of children with early onset conduct problems. J Consult Clin Psychol. 2000;68:624–640. doi: 10.1037/0022-006X.68.4.624. [DOI] [PubMed] [Google Scholar]
- 17.Kazdin AE, Blase SL. Rebooting psychotherapy research and practice to reduce the burden of mental illness. Perspect Psychol Sci. 2011;6:21–37. doi: 10.1177/1745691610393527. [DOI] [PubMed] [Google Scholar]
- 18.NICE . Bipolar disorder: the management of bipolar disorder in adults, children and adolescents in primary and secondary care CG185. London: National Institute for Clinical Excellence; 2006. [Google Scholar]
- 19.Calam R, Sanders MR, Miller C, Sanhnani V, Carmont SA. Can technology and the media help reduce dysfunctional parenting and increase engagement with preventative parenting interventions? Child Maltreat. 2008;13:347–361. doi: 10.1177/1077559508321272. [DOI] [PubMed] [Google Scholar]
- 20.Sanders MR, Calam R, Durand M, Liversidge T, Carmont SA. Does self-directed and web-based support for parents enhance the effects of viewing a reality television series based on the triple P – positive parenting programme? J Child Psychol Psychiat. 2008;49:924–932. doi: 10.1111/j.1469-7610.2008.01901.x. [DOI] [PubMed] [Google Scholar]
- 21.World Internet Project. International Report: Fourth Edition. Retrieved from http://www.worldinternetproject.net; 2012
- 22.Dimeff LA, Paves AP, Skutch J, Woodcock EA. Shifting paradigms in clinical psychology: How innovative technologies are shaping treatment delivery. In: Barlow DH, editor. The oxford handbook of clinical psychology. New York: Oxford University Press; 2011. pp. 618–648. [Google Scholar]
- 23.Jones SH, Calam R, Sanders M, Diggle P, Dempsey R, Sadhnani V. A pilot web based positive parenting intervention to help bipolar parents to improve perceived parenting skills and child outcomes. Behav Cognitive Psychother. 2014;42:283–296. [DOI] [PubMed]
- 24.Turner KMT, Sanders MR. Triple P online [interactive internet program] Brisbane, QLD, Australia: Triple P International Pty. Ltd; 2011. [Google Scholar]
- 25.Todd N, Jones S, Hart A, Lobban F. A web-based self-management intervention for bipolar disorder ‘living with Bipolar’: a feasibility randomised controlled trial. J Affect Disord. 2014;169:21–29. doi: 10.1016/j.jad.2014.07.027. [DOI] [PubMed] [Google Scholar]
- 26.Frances J, Kay-Lambkin FJ, Baker AL, Lewin TJ, Carr VJ. Computer-based psychological treatment for comorbid depression and problematic alcohol and/or cannabis use: a randomized controlled trial of clinical efficacy. Addict. 2009;104:378–388. doi: 10.1111/j.1360-0443.2008.02444.x. [DOI] [PubMed] [Google Scholar]
- 27.First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Structured clinical interview for DSM-IV axis I disorders, research version. Washington DC: American Psychiatric Press; 1997. [Google Scholar]
- 28.Goodman R. Psychometric Properties of the strengths and difficulties questionnaire. J Am Acad Child Adol Psychiat. 2001;40:1337–45. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- 29.Eyberg SM, Pincus D. Eyberg child behavior and sutter-eyberg student behavior inventory – revised: professional manual. Odessa, FL: Psychological Assessment Resource; 1999. [Google Scholar]
- 30.Arnold DS, O’Leary SG, Wolff LS, Acker MM. The parenting scale: a measure of dysfunctional parenting in discipline situations. Psychol Assess. 1993;5:137–144. doi: 10.1037/1040-3590.5.2.137. [DOI] [Google Scholar]
- 31.Gibaud-Wallston J, Wandersaman LP. Development and utility of the parenting sense of competence scale. Toronto: Paper presented at the meeting of the American Psychological Association; 1978. [Google Scholar]
- 32.Johnston C, Mash EJ. A measures of parenting satisfaction and efficacy. J Clin Child Psychol. 1989;18:167–175. doi: 10.1207/s15374424jccp1802_8. [DOI] [Google Scholar]
- 33.Abidin RR. Parenting stress index, manual. 3. Charlottesville, VA: Pediatric Psychology Press; 1990. [Google Scholar]
- 34.Bauer MS, Crits-Christoph P, Ball WA, Dewees E, McAllister T, Alahi P, Cacciola J, Whybrow PC. Independent assessment of manic and depressive symptoms by self-rating. Scale characteristics and implications for the study of mania. Arch Gen Psych. 1991;48:807–12. doi: 10.1001/archpsyc.1991.01810330031005. [DOI] [PubMed] [Google Scholar]
- 35.Radloff LS. The use of the centre for epidemiologic studies depression scale in adolescents and young adults. J Youth Adol. 1991;20:149–66. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- 36.Altman E, Hedeker D, Peterson JL, Davis JM. A comparative evaluation of three self-rating scales for acute mania. Biol Psychiat. 2001;50:468–71. [DOI] [PubMed]
- 37.Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC. The longitudinal interval follow-up evaluation. A comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44:540–8. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- 38.Hamilton M. A rating scale for depression. J Neurol Psychiatry. 1960;23:59–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bech P, Rafaelsen OJ, Kramp P, Bolwig TG. The mania rating scale: scale construction and inter-observer agreement. Neuropharmacol. 1978;17:430–431. doi: 10.1016/0028-3908(78)90022-9. [DOI] [PubMed] [Google Scholar]
- 40.Matheny AP, Wachs TD. Bringing order out of chaos: psychometric characteristics of the confusion, hubbub and order scale. J App Dev Psychol. 1995;16:429–444. doi: 10.1016/0193-3973(95)90028-4. [DOI] [Google Scholar]
- 41.Diggle PJ, Heagerty P, Liang K-Y, Zeger SL. Analysis of longitudinal data. second. Oxford: Oxford University Press; 2002. [Google Scholar]
- 42.Network MHR. Service user involvement in the UK mental health research network. London: MHRN; 2005. [Google Scholar]
- 43.Mathieu M, McGeechan K, Barratt A, Herbert R. Internet-based. Randomized controlled trials: a systematic review. J Am Med Inform Assoc. 2013;20:568–576. doi: 10.1136/amiajnl-2012-001175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Duffy A, Horrocks J, Doucette S, Keown-Stoneman C, McCloskey S, Grof P. The developmental trajectory of bipolar disorder. Br J Psychiat. 2014;204:122–128. doi: 10.1192/bjp.bp.113.126706. [DOI] [PubMed] [Google Scholar]
- 45.Van der Gucht E, Morriss R, Lancaster G, Kinderman P, Bentall RP. Psychological processes in bipolar affective disorder: negative cognitive style and reward processing. Br J Psychiat. 2009;194:146–151. doi: 10.1192/bjp.bp.107.047894. [DOI] [PubMed] [Google Scholar]
- 46.Potosky D, Bobko P. Computer versus paper-and-pencil administration mode and response distortion in noncognitive selection tests. J App Psychol. 1997;82:293–299. doi: 10.1037/0021-9010.82.2.293. [DOI] [PubMed] [Google Scholar]
- 47.Chinman M, Young AS, Schell T, Hassell J, Mintz J. Computer-assisted self-assessment in persons with severe mental illness. J Clin Psychiat. 2004;65:1343–51. doi: 10.4088/JCP.v65n1008. [DOI] [PubMed] [Google Scholar]
- 48.Richman WL, Kiesler S, Weisband S, Drasgow F. A meta-analytic study of social desirability distortion in computer-administered questionnaires, traditional questionnaires, and interviews. J Appl Psychol. 1999;84:754–75. doi: 10.1037/0021-9010.84.5.754. [DOI] [Google Scholar]


