The Home Oxygen Program in British Columbia began as a small, centralized program clerically managed by the Ministry of Health in British Columbia. A pilot program launched in the mid-1990s, however, demonstrated the feasibility and myriad benefits of managing the program locally. Approximately seven years later, the pilot’s model and recommendations were implemented in British Columbia’s five health authorities, and the program has grown to include many clients. This article describes the development of the program from its infancy to its present-day success, focusing on regionalization and its incumbent challenges.
Keywords: British Columbia, Home oxygen, Home Oxygen Program, Medical eligibility, Oxygen provider, Regional, Regionalized, Registered respiratory therapist, Request for proposal, Vancouver Coastal Health
Abstract
Since its inception in the 1980s, the Home Oxygen Program in British Columbia was centrally managed by the Ministry of Health. Initially a small program with few clients across the province, it soon became a large program with many clients and increasing expenditures. A pilot program started in Victoria (British Columbia) in 1996 demonstrated that managing the program locally could offer better client care, better contract management and significant cost savings. In 2002, the pilot’s model and recommendations were implemented in British Columbia’s five health authorities. The present review details the experiences of regionalizing the program in the Vancouver Coastal Health authority. After fine adjustments to the model were developed and new contracts and criteria changes made, better care for clients was provided than the previous centralized model at a reduced cost to the taxpayer.
Abstract
Depuis sa création en 1980, le ministère de la Santé gérait le programme de fourniture d’oxygène à domicile de la Colombie-Britannique. Ce programme, qui se limitait au départ à quelques clients dans la province, a vite pris de l’envergure pour inclure de nombreux clients et s’associer à des dépenses croissantes. En 1996, un programme pilote lancé à Victoria (Colombie-Britannique) a démontré que sa gestion locale pouvait assurer de meilleurs soins aux patients, une meilleure gestion des contrats et d’importantes économies. En 2002, le modèle du projet pilote et les recommandations ont été mises en œuvre dans les cinq régies régionales de la Colombie-Britannique. La présente analyse détaille les expériences de régionalisation du programme au sein de la régie régionale Vancouver Coastal Health. Après des réglages de précision, de nouveaux contrats et des modifications aux critères, les clients ont profité de meilleurs soins que dans le cadre du modèle centralisé antérieur, à moindre coût pour le contribuable.
Home oxygen therapy has been provided in the British Columbia (BC) public health care system for almost 40 years, following four randomized controlled trials from 1980 to 2004. These studies showed the importance of providing home oxygen therapy to individuals with chronic obstructive pulmonary disease (COPD) with poor oxygenation on room air (1–4). The studies found a remarkable reduction in mortality when oxygen was provided to individuals with COPD with hypoxemia. For example, in the Nocturnal Oxygen Therapy Trial group (1), subjects with a resting partial pressure of arterial oxygen (PaO2) <55 mmHg with only nocturnal oxygen treatment had a 1.94 times higher mortality rate than those who used continuous oxygen. In comparison, male subjects in the Medical Research Council Working Party study (2) with a resting PaO2 40 mmHg to 60 mmHg had 11.9% annual mortality rate while treated with oxygen versus 29.4% annual mortality rate in the control (no treatment) group. Based on the results of these studies, domiciliary oxygen therapy became a popular treatment regimen to improve both the life expectancy and quality of life of individuals with COPD. Criteria for the use of home oxygen therapy in BC are based on these studies, among others (1-6).
Although the studies, recommendations and criteria are based on recommendations for the treatment of COPD, not all clients using oxygen therapy in BC have COPD. Because “there is limited evidence concerning the efficacy of home oxygen in other respiratory diseases… it is presumed to be effective based on the COPD data for hypoxemic patients with other respiratory diseases such as pulmonary hypertension and fibrosis” (7). Aside from young children, BC medical criteria for home oxygen are generally applied to individuals with hypoxemia and of all ages, regardless of diagnosis or prognosis.
METHODS
Because the present article was written as an internal evaluation of the Home Oxygen Program (HOP), it did not require research ethics board approval from Vancouver Coastal Health (VCH). The article was written with a historical perspective spanning >12 years to present (Table 1). The data, including client volumes, lengths of stay, diagnoses and cost, were collected from the VCH program’s database, financial reports and program records.
TABLE 1.
Timelines, initiatives and details of the Home Oxygen Program (HOP) in British Columbia (BC)
| Year/date | Initiative | Details |
|---|---|---|
| Circa 1980 | HOP began in BC | Few clients, basic equipment |
| Circa 1996 | Centralized HOP: program review | Expenditures were skyrocketing; challenging to run the program efficiently in current state |
| November 1996 | Pilot project | Victoria, BC. One RRT hired to assess clients at home in place of the provider’s RRT. Remainder of BC continued in current state |
| April 22, 1999 | Recommendations to Ministry of Health | Pilot program findings in letter to Ministry of Health (35% of clients no longer eligible and were discontinued). Letter recommends regionalization of HOP across BC |
| May 2002 | Regionalization across BC | Each health authority required to operate their own HOP based on Victoria’s model; assumed existing contracts with oxygen providers; staff hired and began assessing existing clients. |
| December 2002 | Request for proposal | Provincial request for proposal; new service model based on pilot; primary and secondary provider (80%/20% of business) |
| July 2003 | Providers awarded | New contract started. Transitioned clients to successful providers |
| 2003 | Medical criteria revision | Collaborative effort across BC |
| March 2004 | VCH HOP review | All existing VCH clients were assessed; 16% fewer clients (no longer eligible and were discontinued) |
| 2007 | Medical criteria revision | Collaborative effort across BC |
| 2008 | Request for proposal | Provincial request for proposal. Primary and secondary model (70%/30%); encouraged new technology, fewer deliveries. Transitioned clients to successful providers |
| July 2008 | Providers awarded | New contract started. Transitioned clients to successful providers |
| 2012 | Medical criteria revision | Collaborative effort across BC |
| 2013 | Contract extension | Four-year term with existing providers until 2017 |
RRT Registered respiratory therapist; VCH Vancouver Coastal Health
BACKGROUND
BC’s HOP was once a centralized program operated by clerical staff from the Ministry of Health and a medical consultant. All applications from across BC were sent to a single location and adjudicated for eligibility on an approximately weekly basis. Physicians requested funding approval on behalf of his or her patient, supported with clinical data showing hypoxemia. Oxygen litre flow, hours of use per day and the equipment needed were also requested by the physicians. The program sent approved applications to an oxygen provider for set-up in the client’s home. The provider also needed to make arrangements for oxygen deliveries as needed, and have the client regularly assessed by a registered respiratory therapist (RRT).
Funding was for an indefinite period of time because the physician was expected to follow up with the client, adjust oxygen therapy or discontinue treatment as needed, with most changes requiring approval from the HOP. Each application or change often took considerable effort and time and, not surprisingly, HOP clients often remained on oxygen for many months or years longer than they would have been eligible for. Each oxygen provider had their own contracted monthly rates based on where the client resided and the equipment type provided (concentrators, cylinder sizes, regulators, liquid oxygen), which, along with providing receipts for every delivery, made reconciling invoices time challenging.
Despite their expertise in home oxygen therapy, the oxygen provider’s RRTs had limited latitude in scope of practice. They assessed the client and made suggestions to change the flow of oxygen or equipment, but were unable to make any changes without the physician’s order. One further concern with this model was the potential conflict of interest if the company’s RRT suggested changes, which resulted in an increase in the funding requirement.
This general model persisted for many years. Soon, more and more clients enrolled in the program, making it more challenging, complex and, of course, more expensive to manage. Fundamental program changes were in order.
Pilot project
With the Ministry of Health’s approval, the Capital Regional District (CRD) of Victoria, BC, initiated a pilot project in November 1996 to manage how home oxygen was provided within the city. There were 444 HOP clients at the time and a steady number of applications per week. A full-time RRT was hired to assess clients in their homes, and a respirologist consultant was retained to provide medical support.
During the home assessments, it was discovered that some clients did not require any intervention, while many other clients needed changes. Oxygen flows were titrated immediately, and equipment was removed or added shortly after contacting the oxygen provider. Other clients clearly no longer met eligibility requirements for the program, and were discontinued within a few days after discussions with the client and the medical consultant. The client’s physician was then notified.
When all 444 clients were assessed, the CRD HOP reported to the BC Ministry of Health on April 22, 1999 that the pilot “… reduced [HOP] utilization by a total of 35%”. During that time, 291 clients remained on the CRD program after <2 years since the program started. When weekly growth was taken into account, the letter stated that the reduction would actually have been 45%. The reduced use amounted to a reported savings of $150,000 in fiscal year 1998/1999. The CRD program continued in this manner while recommending expansion of their model across the province.
Regionalization
Several years after the CRD made its recommendations, in May 2002, the HOP finally regionalized and was modelled after the pilot across BC. Figure 1 shows BC’s five geographically defined health authorities: VCH, Island Health, Fraser Health, Interior Health and Northern Health. Each health authority is responsible for providing public health care to the citizens residing in their geographical boundaries. In 2006, the population of BC was approximately 4.1 million, with 1.03 million of those residing within VCH’s boundaries in the southwestern corner of BC (8). Funding was provided by the Ministry to each health authority based on previous year’s payments to the oxygen providers with no additional operational funding.
Figure 1).
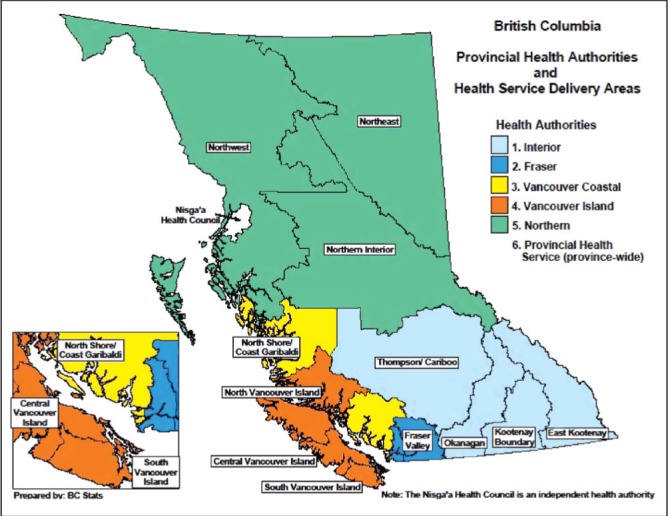
Map showing British Columbia’s health authorities
VCH appointed a program coordinator, medical consultant and three RRTs on short-term contracts to assess as many clients residing in Vancouver as soon as possible. There were 912 clients funded by the VCH HOP in May 2002. With the help of the contracted RRTs, many HOP clients were assessed at home. Following the CRD’s model, the therapists titrated oxygen flow rates and added or discontinued equipment as needed or provided a lesser expensive modality if tolerated (eg, liquid oxygen systems were more expensive than cylinder- or oxygen-conserving device systems). Of the first 191 VCH clients assessed, 45 (23%) were discontinued and 42 (22%) had equipment changed. Even with approximately 12 applications per week, by February 2003, the census showed 806 HOP clients enrolled in the program.
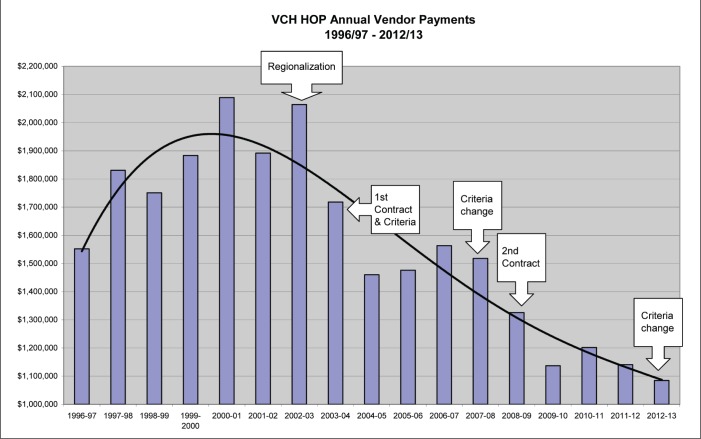
The contract RRTs’ terms ended and, soon after, VCH staff grew to include one casual and two permanent full-time RRTs, one clerk, one program coordinator and one medical consultant. By March 2004, all existing clients were assessed and the VCH HOP client population was reduced to 762. This 16% reduction equated to approximately $330,000 per year in program efficiencies in our health authority alone. Efficiencies attributed to changes in equipment also provided more program savings (Figure 2).
Figure 2).
Costs from 1996 to 2012/2013. HOP Home Oxygen Program; VCH Vancouver Coastal Health
A third RRT was later hired to provide support to a separate home health program in Vancouver as a result of further program efficiencies. VCH initial oxygen utilization reviews showed:
Of 158 VCH clients in one particular sample review, 13% claimed they never used their portable oxygen.
One client used oxygen only with a small torch for welding.
Liquid oxygen for another client was kept in her closet, filled regularly by her oxygen provider (due to liquid oxygen constantly evaporating even if not used), but she never used it.
HOP RRTs went to the last known address of a client whose telephone number was not in service. The home was dilapidated, boarded and vacant. It was later discovered the client had moved to another province five years earlier with her concentrator. The money paid to the provider over the five years was refunded.
Some clients were deceased for months or years, but the surviving family members never notified the program.
Many clients’ equipment in residential facilities was stored away or used for other residents after the client passed away.
A few landlords stored, discarded or sold equipment after clients moved or were in hospital for extended periods of time.
There are more stories similar to these; however, in each case, HOP had rented the equipment not knowing the equipment was no longer used as intended.
Challenges with transition to a regional model
When the VCH RRTs reassessed the existing clients for the first time and found them to be no longer eligible for funding, many clients were relieved they no longer needed oxygen. There were, however, some long-term oxygen users who may have developed a psychological dependence on oxygen and were concerned. These clients believed that oxygen provided them with symptomatic relief. Its ongoing use was often supported by their physicians, health care staff and family, despite the client being well-oxygenated breathing room air (BC’s HOP medical eligibility does not provide oxygen for individuals with dyspnea without hypoxemia). Other clients simply wanted to have oxygen in the event something happened to them in the future (ie, in case of an exacerbation) and some clients could not believe an RRT could tell them they no longer needed oxygen when their physician told them otherwise. The following efforts were made to ease the funding discontinuation for clients who were concerned:
Some were weaned off oxygen over a number of days or weeks (reducing flow or removing equipment gradually)
Some were reassessed at a later date as a comparison, which also gave them some more time to consider their situation
Some were offered assessments in a pulmonary function laboratory
Some were recommended to pursue self-pay/extended health benefits as an option to continue receiving oxygen.
Supported by home assessments, medical evidence and medical support, the program was eventually able to press through the challenges. Before long, the stakeholders accepted the new program model.
The HOP’s view was, and remains, to never challenge the physician’s prescription for oxygen therapy; it is really a matter of who would fund it (the client, other source or HOP). Clients must initially qualify and are required to show ongoing eligibility during follow-up assessments. A prescription for oxygen was no longer considered to be funded for an indefinite period of time. These important fundamental principles were necessary for our program to be mindful of considering providing publically funded oxygen in VCH.
Requests for proposal
In December 2002, once the program model, legal terms and provider service expectations were agreed upon by the health authorities, the group published the first provincial request for proposal (RFP). The RFP required one primary and one or two secondary oxygen providers per health authority for five-year contracts. The primary provider would be awarded 80% of new HOP clients and the remainder shared with the other awarded providers. The terms of the program required equipment set up in the home within certain hours of discharge along with oxygen deliveries, 24 h/7 day service and equipment maintenance. Daily flat rates were required to simplify billing purposes and were based on the equipment provided (ie, concentrator, any portable system or a combination of both).
Within the first few postaward months, the new oxygen providers transitioned clients from the unsuccessful proponents. For VCH, the majority of clients transitioned to one of the successful companies; however, 58 remained with their original oxygen provider and paid privately. The transition period in VCH witnessed 330 clients being transitioned within a span of four months.
Before the end of the first contract term, a second provincial RFP was published in 2008 with a few changes to the service requirements. One of the significant changes was to encourage newer technology equipment (quieter concentrators, portable oxygen concentrators and home-fill systems) to help improve client experience, independence and reduce the numbers of deliveries. The model also required one primary and one secondary provider. Client transitions were again required. All but approximately 100 clients moved to successful providers in VCH, and all remaining transitioned within a matter of a few months.
The five-year term of this contract expired in July 2013 and all health authorities in BC chose to extend the contracts with the three existing providers to 2017.
New model Basics
The new HOP program became both a funding agency and a clinical program provided by RRTs who understood the importance of close follow-up and the benefits of direct management of a client’s oxygen therapy. Although the client’s physician or nurse practitioner is still required to provide hypoxemia data and sign the application form, once that is accomplished and the application is approved, the HOP becomes directly involved in managing oxygen therapy for the client and titrating the flows, equipment and funding, when and as needed. The signed application form serves as both an application for oxygen funding as well as a prescription for oxygen therapy with the ability for the HOP respiratory therapists to titrate to ≥90% oxygen saturation without the need to confirm with the physician first. New community-based applications (from family physicians and specialists) are usually approved by the HOP the same day they are received. Set-up is usually performed by the following working day. Acute care clients are set up within a few hours of discharge seven days a week without previous approval by the HOP. Depending on the needs of the client, an oxygen provider RRT will also assess the client at home the next business day. The first follow-up assessment by VCH HOP staff is performed within six weeks of set-up. If the client still meets criteria, oxygen will continue to be funded; if not, changes are made in a matter of days (sometimes involving addition of equipment or removal, or complete discontinuation) and the physician is made aware.
Safe use of oxygen
Unfortunately, there are some clients who choose not to follow safe practices with oxygen, resulting in many ‘near misses’, some injuries and a few deaths. All new clients are provided with verbal and written education about how to be safe with oxygen on set-up and during follow-up assessments. Some clients claim to forget or simply do not believe they will get injured. When incidents do occur, they are reported to the HOP by the client or caregiver (family, home health, home support, oxygen provider). The client is promptly re-educated about the importance of safety and reminded that a second incident will result in removal of the equipment for their safety and the safety of others. A letter is written to the client, the physician and the home health team and, on most occasions, a telephone conversation occurs with someone on the team.
In VCH, 48 safety events have been reported to the office since 2004, with three of these resulting in death. Twenty four of these events were flash fires, causing injuries to the client and/or property damage (18 in 2010 to 2011); at least two fires were sufficiently extensive to cause general evacuation of the area. This approach of reporting, ongoing educating, communicating among stakeholders and actually withdrawing oxygen when needed not only educates the client, but also educates the home health team and physicians who may be involved with future clients on oxygen and results in fewer incidents. In 2012 and 2013, there were only two reported incidents in each of those years. Although constant education to ensure safe practice with oxygen is undertaken with the goal of zero incidents, it is a challenge because the actions of clients cannot be monitored or controlled every minute of every day.
Medical eligibility criteria
The development of medical eligibility criteria was another collaborative effort between managers and medical consultants across the province. Referring to the available literature, national and global program comparisons and expertise from the medical consultants, the HOPs in BC agreed on common language and eligibility requirements of the programs. Eligibility revisions occurred in 2003, 2007 and 2012 (9).
Benefits of regionalization
Regionalization benefits all HOPs in BC through collaborative efforts, but it also offers local control and management of the program by local staff who are responsible for day-to-day operations of the program.
Benefits of regionalization include:
Continuity of care from improved liaison and communication with local community and acute health care teams. In 2011, >80% of existing HOP clients in VCH were known to home health services at one time. Fifty percent of VCH clients are currently receiving an average of 2.6 other home health services such as nursing, occupational therapy, physiotherapy, palliative care, home support, mental health and chronic disease management.
Improved communication among all stakeholders, including acute, residential and home health staff, clients, family members and physicians, enable easier access to HOP staff.
Improved electronic medical records to track clients’ needs who also receive other health services.
Improved responsiveness to the needs of existing clients.
Improved access to the program in which queries are addressed in a timely manner.
Improved knowledge of the local population and needs.
Current state
As of November 2014, there were approximately 600 HOP-funded clients in VCH, with approximately 90% residing in the urban lower mainland area. The remainder of HOP clients reside in more rural areas accessed by car, ferry or air.
Figure 2 shows the payments made to oxygen providers from 1996 to 2012/2013 for clients receiving home oxygen in the VCH area. The trend from 1996 to regionalization in 2002 (black line) shows the staggering increase in costs to run the program for VCH. Following regionalization, it is clear that the program became more cost effective due to the new service model, revision of medical eligibility criteria and negotiation of oxygen provider contracts.
Table 2 shows the percentage of VCH clients with specific disease. Note how the percentage of palliative oxygen-dependent clients increased from 10% in 2004 to 22% at present. Although it is difficult to pinpoint the reasons for this trend, it could be due, in part, to the encouragement of more home deaths for palliative clients rather than hospitalization. Supporting this trend, we understandably observe a drop in our client’s length of stay due to the increasing number of palliative clients on home oxygen. Considering all new clients, currently only 50% remain on the program approximately 90 days after starting home oxygen. In comparison, in 2010, it took 165 days before 50% of new clients were discontinued and, in 2006, it was 450 days.
TABLE 2.
Comparison of diagnoses in 2013, 2010, 2006 and 2004
| Home Oxygen Program clients, % | ||||
|---|---|---|---|---|
|
| ||||
| Diagnosis | 2013 | 2010 | 2006 | 2004 |
| Chronic obstructive pulmonary disease | 35 | 39 | 58 | 58 |
| Cancer-related illness | 22 | 21 | 4 | 10 |
| Cardiac-related illness (eg, heart failure) | 12 | 13 | 9 | 10 |
| Other (eg, pneumonia, fibrosis) | 31 | 27 | 29 | 22 |
CONCLUSIONS AND RECOMMENDATIONS
BC’s experiences in the redevelopment of the HOP shows how considerable effort from the health authorities and cooperation from oxygen providers can result in long-lasting and profound positive changes in how home oxygen is delivered. This model also shows how RRTs can provide improved client care, service, access, responsiveness, continuity of care, communication and program control in a highly cost-effective manner. As a result of the outstanding work performed by HOP managers, RRTs and contract support staff across BC to redesign services, review eligibility criteria and regularly assess clients, financial trends and other measurements mentioned in the present review were generally realized across all of BC’s HOPs. Although the HOP has been successfully operating in this manner for 18 years (counting the pilot project), the present article does not intend to suggest that our model is the best practice in providing publicly funded home oxygen programs in Canada.
A more in-depth review of VCH’s client enrollment in the HOP is needed for long-term planning of the program due to the growth of the elderly population in our society and the prevalence of COPD, cancers and other diseases causing hypoxemia.
Footnotes
DISCLOSURES: The author has no financial disclosures or conflicts of interest to declare.
REFERENCES
- 1.Nocturnal Oxygen Therapy Trial Group. Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease: A clinical trial. Ann Intern Med. 1980;93:391. doi: 10.7326/0003-4819-93-3-391. [DOI] [PubMed] [Google Scholar]
- 2.Long term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema. Report of the Medical Research Council Working Party. Lancet. 1981;1:681. [PubMed] [Google Scholar]
- 3.Eaton T, Lewis C, Young P, et al. Longterm oxygen therapy improves health related quality of life. Respir Med. 2004;98:285. doi: 10.1016/j.rmed.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 4.Chaouat A, Weitzenblum E, Kessler R, et al. A randomized trial of nocturnal oxygen therapy in chronic obstructive pulmonary disease patients. Eur Respir J. 1999;14:1002. doi: 10.1183/09031936.99.14510029. [DOI] [PubMed] [Google Scholar]
- 5.Cranston JM, Crockett A, Moss J, et al. Domiciliary oxygen for chronic obstructive pulmonary disease. Cochrane Collaboration. Wiley Library Online. < http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD001744.pub2/full> (Accessed October 10, 2013). [Google Scholar]
- 6.O’Donnell D, Aaron S, Bourbeau J, et al. Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease – 2007 update. Can Respir J. 2007;14(Suppl B):5B–32B. doi: 10.1155/2007/830570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sandberg D, Fleetham J. Home oxygen therapy in British Columbia. BC Med J. 2013;55(3):149–52. [Google Scholar]
- 8.BC Stats 2012. Socio-Economic Profile Vancouver Coastal Health. < www.bcstats.gov.bc.ca/statisticsbysubject/SocialStatistics/SocioEconomicProfilesIndices/Profiles.aspx> (Accessed October 10, 2013).
- 9.Vancouver Coastal Health. Home Oxygen. < www.vch.ca/your_health/healthtopics/home_oxygen/home_oxygen> (Accessed October 10, 2013).