Abstract
Background:
The thought of having a surgery can be stressful for everyone. Providing the necessary information to the patient can help both the patient and the treatment team. This study was conducted to compare the effectiveness of face-to-face verbal training and educational pamphlets on the readiness of patients for undergoing non-emergency surgeries.
Materials and Methods:
The study was a before–after randomized clinical trial. 90 patients scheduled to undergo non-emergency surgery who referred to Shahrekord Ayatollah Kashani Hospital in 2013 were distributed randomly and gradually into two experimental groups (group of face-to-face verbal training and group of educational pamphlet) and one control group. Dependent variable of the study was pre-surgery readiness. Data analysis was carried out by using SPSS statistical software. Statistical analysis were analysis of variance (ANOVA) and correlation test.
Results:
Results showed that the mean scores of pre-surgery readiness in both interventional groups were significantly higher than that in the control group after the intervention (P < 0.05). However, there was no significant difference between the two experimental groups (P > 0.05).
Conclusions:
Each of the methods of face-to-face verbal education and using the pamphlet could be equally effective in improving the readiness of the patients undergoing surgery. Therefore, in environments where the health care providers are facing with the pressure of work and lack of sufficient time for face-to-face verbal training, suitable educational pamphlets can be used to provide the necessary information to patients and prepare them for surgery.
Keywords: Face to face, pamphlet, patient training, pre-surgery, readiness
INTRODUCTION
Millions of major and minor emergency and non-emergency surgeries are performed in Iran annually. Surgeries on patients have useful and sometimes harmful effects. The main goal of surgery is to rescue patients from physical and psychological suffering with minimum damage and cost and also help in making the patients ready sooner for performing their responsibilities and roles in the society or at least to reduce their dependence on the family and society.[1] Positive or negative impact of non-emergency surgeries on patients is sometimes enough for the patients to recall these events in their speeches as before and after surgery.[2] In order to obtain the most positive outcome from surgeries, with the least harm and adverse effects on the patient, the role of patients’ physical and mental readiness and their companions’ decisions is very important.[1] On the other hand, investigation on the increased complaints in medical law enforcement authorities has shown that the most common forms of negligence have been reported as lack of mental readiness or the patient's physical pre-surgery readiness. Moreover, it is possible that the patients’ and their companions’ expectations from the surgery have been untrue or the required readiness for surgery has not been achieved in a better way by the patients. It has been observed many times that before surgery the patients have no correct assumption of the type of disease, alternative forms of treatment, or have unreasonable expectations of surgery. In some situations, patients or their companions have led the surgeon to surgery with false expectations.
Surgery can be stressful for anyone. Providing the necessary information to the patient can assist both the patient and the treatment team. Understanding that what and why something is going to happen will lead to greater patient cooperation in the treatment process. Studies have shown that pre-surgery training has been very effective in reducing stress, pain, and anxiety in patients after surgery.[2,3] In a meta-analysis of 68 studies, 20% improvement has been reported in the outcomes after surgery for patients trained before surgery.[2]
Undergoing surgery is a special and stressful situation that can decrease the learning capability with a focus on the training provided.[3] Available evidences suggest that patients do not obtain the necessary information for pre-surgery readiness and post-surgery care.[1,2] It should be noted that it is possible to accomplish this by interaction and effective communication to establish a relationship between the physician, nurse, and the patient. The study results indicated that medical team does not have enough time for training patients.[4,5] On the other hand, in the study of Hekmatpou et al., it has been reported that patients forgot about 80% of what their physicians told them and almost 50% of the information that was remembered by them was not correct. Therefore, choosing an effective training method is vital in these situations.[5] The question is that in such a stressful situation, which approach could be more appropriate for training and creating a pre-surgery readiness for surgery candidates. Face-to-face verbal learning has been considered as the gold standard for patient training.[4] However, one of its disadvantages is that it is time consuming. Studies have shown that most of the information received by patients during the verbal in-person counseling have not been understood or have been forgotten. Educational written methods have been proposed, such as educational pamphlets as teaching aids along with face-to-face training. Written information is a key technique for training the patients in order to attract their participation in the treatment process.
Educational pamphlet is a useful and cheap educational tool that is readily available to patients and can be read and reread quickly and directly by the patients without having the fear of being asked questions by the healthcare providers in face-to-face verbal training. In addition, educational pamphlets reduce the time spent by the healthcare providers and the medical team.[6,7] Henney and colleagues have shown that patients were satisfied with received written information and the patients trained by educational pamphlets were more satisfied with the treatment.[2] Harwood quoted from Winman thus: 75% of patients have a tendency to use the pamphlet and consider it as a valuable method and 80% of them read the pamphlets.[7] Therefore, how patients responds to information provided depends on the method of providing information.[8] The findings of several studies have shown that using pamphlets has been effective in increasing the knowledge of patients,[1,8] and a sense of competency and readiness of parents for vaccinations.[9] Review of the existing literature shows that the outcomes of face-to-face verbal training were compared with the outcomes of training through the pamphlet as a teaching aid along with face-to-face training. In this regard, various research findings have been different. Some studies considered pamphlets to be more effective as a complement to face-to-face training.[3,10] Some studies have reported no difference on using pamphlet and whether or not to use it in comparison to face-to-face verbal training.[11,12] In some studies, the use of pamphlets did not have any effect on the increase of knowledge of patients or changing patients’ attitude. The possible reason could be not understanding the content of the pamphlets.[13,14,15] For example, in the clinical trial study of Venmans and colleagues entitled “Acceptability and impact of educational pamphlets about the infection on 200 patients with non-insulin dependent diabetes in two rural and urban centers in the Netherlands,” the findings have shown that there was no significant difference in the level of knowledge and attitudes of patients in the experimental group. Pamphlet content being not understandable has been proposed as a possible cause.[13] Due to the time-consuming nature of face-to-face training and it not being common in the routine pre-surgery care, there is no evidence about the impact of the pamphlets alone compared with face-to-face training. Therefore, making decisions in choosing the best approach for pre-surgery training of patients requires research-based scientific evidences in comparing these two methods. This study was conducted with the aim of comparing the effectiveness of training through pamphlet with face-to-face training on the rate of pre-surgery readiness of the patients.
MATERIALS AND METHODS
The study was a before–after randomized clinical trial. The study population included candidate patients undergoing non-emergency surgeries of herniorrhaphy, cholecystectomy, and nephrectomy after being referred to the surgery rooms of Shahrekord Kashani Hospital in 2013. All surgeries were performed under general anesthesia by a surgeon and an anesthesiologist. The sample size, based on a previous study,[8] was calculated as 25 people, which was finalized as 30 subjects for each group in this study. A total of 90 samples were enrolled in the study based on the inclusion criteria by using easy and gradual sampling method. Inclusion criteria were as follows: Age 20–65 years, no history of previous surgery, undergoing non-emergency surgery, no history of any family member having undergone the same surgery, not having an obvious mental health problem, having the ability to communicate verbally, willingness to cooperate in the research, being literate (patient or one of the close relatives), and staying in the hospital from the afternoon of the day before surgery. The dependent variable of the study was pre-surgery readiness. This variable was measured in three ways: (1) knowledge level of the patient before, during, and after surgery about readiness (as pre- and post-intervention); (2) patient's self-assessment of acquired readiness before surgery (as pre- and post-intervention); and (3) readiness of patients based on the standard checklist of surgery room (only after intervention). It was performed by the researcher-made method based on medical and surgery textbook contents. Patient's level of knowledge was assessed by a questionnaire containing 26 questions about the readiness before, during, and after herniorrhaphy surgery, 26 questions about cholecystectomy surgery, and 27 questions about prostatectomy surgery (4-choice and true and false questions). Patient's self-assessment questionnaire about the readiness before surgery contained 22 questions. One part was graded as a Likert's type from quite favorable to unfavorable and the other part as yes or no. Surgery room standard checklist for the patient readiness included 22 questions with yes or no responses. This checklist included items such as: Having pre-surgery tests, radiography, ECG, appropriate coverage of the patient, counseling before surgery, having a companion, fasting, informing the physician about the medication at home before surgery, obtaining informed consent, not having ornaments, emptying the bladder before surgery, etc. This checklist is used routinely in hospitals on arrival of the patients to the surgery room for surgery. Content validity was used to determine the validity of the tools. The tools were given to surgery and nursing specialists and all the needed corrections were carried out based on their comments. In order to estimate the reliability of the tools, Cronbach's alpha coefficient was used for the multiple-choice questions. The obtained values were α =0.71 for 4-choice questions of patient's knowledge assessment questionnaire and α =0.75 for Likert's type questions of patient's self-assessment questionnaire on acquired readiness. Richardson coefficient estimated the reliability of yes/no and correct/wrong questions of patient's knowledge assessment questionnaire as 0.79, yes/no questions of patient's self-assessment of acquired readiness before surgery as 0.78, and the standard checklist of surgery rooms for readiness of the patient as 0.80.
The participants were examined after referral to the physician and included in the surgery list. Initially, citing the research purpose, the researcher obtained written consent from the participants for participating in the study. To investigate the patients’ knowledge about the readiness before, during, and after surgery, multiple-choice questions based knowledge test and patient's self-assessment of readiness before surgery based on the Likert's criteria were used. Then, the samples were distributed by using randomized distribution method in two groups (face-to-face verbal training group and training through pamphlet group) and one control group. Intervention in the training group through the pamphlet was administered 1 week before the surgery, during visits to the physician (in the office or clinic), and when they were included in the list of physician's surgeries. The required pamphlet was prepared with the items related to the disease, pre-surgery readiness, location of surgery, type of anesthesia, post-surgery care in the hospital, self-care at home, and frequently asked questions by the patients before the surgery, along with the answers in plain and understandable language for the patients. This pamphlet was prepared by two nursing faculty members by using reference books and was approved by surgeons and anesthesiologists. The approved pamphlet was given to patients of this group by the physician. Then, they were asked to read the desired pamphlet. Intervention in the face-to-face verbal training group was performed in such a way that the patients in this group had been visited the night before the surgery by a physician (surgeon) and an anesthesiologist. Physician gave the necessary training to the patient as face-to-face verbal training about disease, pre-surgery readiness, location of surgery, type of anesthesia, post-surgery care at the hospital, and self-care at home, similar to what was given in the pamphlet. Then, the physician answered the questions of patients regarding surgery. In the third group (control group) was adopted the regular routine method. On the morning of surgery, the patient was re-examined for knowledge of readiness before, during, and after surgery by using multiple-choice knowledge test and patient's self-assessment of pre-surgery readiness based on the Likert's criteria. Patient's readiness for surgery was also evaluated according to the surgery room checklist. This study was approved by the Ethics Committee of the Vice Chancellor of Research of Shahrekord University of Medical Sciences. For ethical considerations, the study goals were described to the patients and their consent to participate in the research was obtained. SPSS software version 16, analysis of variance (ANOVA) test, and Pearson and Spearman correlation coefficients were used for analysis of the obtained data. Level of significance was considered at P < 0.05.
RESULTS
Regarding demographic variables, the research findings showed that the mean age of the study samples was 42 years with a standard deviation of 3.6, 84.6% of the subjects were married, and the majority of them had under diploma level of education (68%). In this study, the pre-surgery readiness in the investigated samples was assessed by using three tools: Knowledge test and patient's self-assessment of pre-surgery readiness, and checklist of surgery rooms. Kolmogorov–Smirnov test results showed that data relating to each of the three dependent variables (level of pre-surgery readiness of patients based on knowledge test, patient's self-assessment, and checklist of surgery rooms) had a normal distribution (P > 0.05). Kolmogorov–Smirnov test results with several samples also showed that the basic readiness level in the three groups before surgery based on the knowledge test had no significant difference, while the results of ANOVA test showed that there was significant difference between the mean scores of patients’ knowledge after the intervention in the three groups. Mean scores of patients’ knowledge in the intervention groups were significantly higher than in the control group. Scheffe test results showed that this difference was related to the control group and there was no significant difference between intervention groups (P > 0.05)[Table 1]. With regard to the patient's self-assessment of pre-surgery readiness, ANOVA test results showed that there was a significant difference in the mean scores after the intervention in the three groups as the mean score of readiness for the patients in the intervention groups was significantly more than that in the control group (P < 0.05). Based on the results of Scheffe test, this difference was due to the control group and there was no significant difference between the experimental groups (P > 0.05)[Table 2]. In relation to the checklist of surgery room readiness, ANOVA test results showed significant difference between the obtained mean scores in the three groups, and the intervention groups had significantly more readiness according to the surgery room checklist in comparison with the control group (P < 0.05). Scheffe test results showed that the obtained difference was related to the control group and there was no significant difference between the obtained mean score from the checklist of surgery room in the intervention groups (P > 0.05)[Table 3]. Regarding the relationship between demographic characteristics of the investigated samples and the dependent variables of research, Spearman correlation test showed that there was no significant relationship between the pre-surgery readiness based on knowledgeof the patients, patients’ self-assessment of pre-surgery readiness, and the checklist of surgery room, and the type of surgery, level of education, marital status, gender, place of residence, and the patient's occupation. Pearson correlation test also showed no significant relationship between age and pre-surgery readiness (P > 0.05).
Table 1.
Comparison of the mean scores of pre-surgery readiness of patients after the intervention in the three groups based on the questions of knowledge test

Table 2.
Comparison of the mean scores of patient self-assessment of pre-surgery readiness after the intervention in the three groups based on the checklist of patient self-assessment
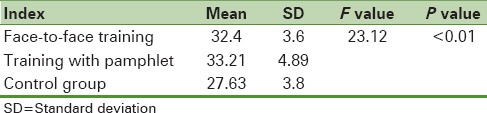
Table 3.
Comparison of the mean scores of pre-surgery readiness after the intervention in the three groups based on the checklist of surgery room

DISCUSSION AND CONCLUSION
In the present study, the level of patients’ knowledge base and their initial self-assessment of pre-surgery readiness were identical and at a low level. This issue showed that routine visit of the surgeon (in clinic or office) has failed to be effective in increasing the knowledge and patients’ feeling of readiness for surgery. Therefore, it is required that the patients receive appropriate and necessary information. This finding was similar to the findings from other studies in this field reporting that patients are unable to gain the expected data.[1,2] The present study findings also showed that training of the patients before surgery by face-to-face verbal method or through the pamphlet could be equally effective in increasing the knowledge and patient self-assessment of pre-surgery readiness, and also, readiness of the patient for surgery according to the checklist of surgery room. No similar study was found comparing the impact of face-to-face verbal training with training through educational pamphlet alone. Previous studies have investigated the impact of combined training of face to face along with the pamphlet or other methods such as computer and internet compared with face-to-face training alone. In those studies that used providing written information such as pamphlets, or a computer and internet as a method of training, similar findings were obtained and approved the same as the present study (e.g., the study of Klein and colleagues entitled “Investigation of positive impact of training through a pamphlet in creating a feeling of adequacy and maternal readiness for the care after vaccination of children”[9] and the study of Humphris and colleagues investigating the effect of this instructional method in increasing knowledge of people with cancer[10]). Effectiveness of this educational method has also been supported in other studies as follows: In changing the attitude toward treatment and increasing adherence in depressed patients in Japan,[16] increasing the patients’ knowledge about screening of colorectal cancer,[17] increasing the knowledge and understanding of mothers about electroencephalography in Turkey,[18] and increasing the knowledge of patients about oral cancer in Italy.[19] In the previous studies, face-to-face training had increased the level of patients’ knowledge. However, training through internet[20] or by video tutorial[21] has had more impact in increasing the patients’ knowledge. In addition, patients’ self-assessment of readiness in the study of Felley[8] and patients’ knowledge level in the study of Keulers and colleagues[11] after training with the combined method of face-to-face training and pamphlets have been found to be more than that obtained in face-to-face training alone. In the study of Henney[2] and also in the study of Hong,[4] training the patients undergoing surgeries of ear, nose, and throat by pamphlets was found to increase the retention rate of information in the patients. A systematic review conducted by Venmas and colleagues[13] of the impact of providing written information to patients has found that it creates a sense of personal satisfaction in patients from the received information, increases physicians’ satisfaction in reducing the time taken for training, and increases the patients’ compliance with the treatment. The studies of Little and colleagues[14] and Wetzels and colleagues[15] have reported that educational pamphlets have no effect on attitude, knowledge, or patients’ performance. The authors have stated that one of the reasons for the ineffectiveness of pamphlets in those studies could be the items present in the pamphlet not being understandable. Therefore, it is necessary to be considered sufficient time and attention to provide educational pamphlets.
The purpose of this study was implementation and comparison of the two methods of face-to-face verbal training and pamphlets with functionality in the hospital for patients undergoing surgery in real, long-term conditions and not just in terms of research and short-term conditions. Therefore, due to the need of adequate time for reading the pamphlets by the patients, they were provided at the clinic during the last visit of the patient to the hospital before admission (2 weeks before surgery). However, providing face-to-face verbal training by the physician was not possible when the patients referred the physician's office or clinic and, merely, it was only possible in the last visit of patient before surgery by the physician at the hospital (the night before the surgery). Due to these reasons, consistency was not maintained with respect to the time of providing the two types of training to the two groups, which was one of the limitations of the study. On the other hand, patient's anxiety at the night before surgery is more than that at 2 weeks prior to surgery. Therefore, patients in the group of face-to-face training had probably higher anxiety levels at the time of training compared with the patients of pamphlet group. This might impact their learning. Therefore, this issue should be also considered. Briefly, face-to-face verbal training is given priority due to the increase of communication between healthcare providers and patients. However, given that, in the present study, face-to-face verbal training and training by educational pamphlets were equally effective in increasing the knowledge and readiness of patients before surgery. Based on the self-assessment and checklist of surgery room, it can be concluded that using pamphlets as an inexpensive and accessible method, if properly designed with all the necessary information at the patient's level of understanding and considering all the relevant data needed by the patient (disease, pre-surgery readiness, place of surgery, type of anesthesia, post-care in the hospital after surgery, self-care at home, and answers to patient's questions in the pamphlet context), might be a good alternative for face-to-face verbal training in environments where the medical team is faced with lack of time for patient training.
ACKNOWLEDGMENTS
This article has been extracted from the approved research project of Shahrekord University of Medical Sciences (No. 478). The Vice Chancellor for Research of Shahrekord University of Medical Sciences is appreciated for providing the financial help. The authors would like to thank all the participating patients in the present study and the nursing staff of surgical wards and surgery rooms of Ayatollah Kashani Hospital for their collaboration in carrying out the project.
Footnotes
Source of Support: The study is funded by Shahrekord University of Medical Sciences.
Conflict of Interest: None declared
REFERENCES
- 1.Kruzik N. Benefits of preoperative education for adult elective Surgery Patients. AORN J. 2009;90:381–7. doi: 10.1016/j.aorn.2009.06.022. [DOI] [PubMed] [Google Scholar]
- 2.Henney S, Rakhra S. Patient information in otorhinolaryngology: A prospective audit. JRSM Short Rep. 2011;2:37. doi: 10.1258/shorts.2011.011022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pokharel K, Bhattarai B, Khatiwada S. Nepalese patients’ anxiety and concerns before surgery. J Clin Anesth. 2011;23:372–8. doi: 10.1016/j.jclinane.2010.12.011. [DOI] [PubMed] [Google Scholar]
- 4.Hong J, Nguyen VT, Prose SN. Compassionate care: Enhancing physician-patient communication and education in dermatology. Part II: Patient education. J Am Acad Dermatol. 2013;68:364.e1–10. doi: 10.1016/j.jaad.2012.10.060. [DOI] [PubMed] [Google Scholar]
- 5.VahedianAzimi A, Alhani F, Hedayat K. Barriers and facilitators of patient's education: Nurses’ perspectives. Iran J Med Educ. 2013;11:620–34. [Google Scholar]
- 6.Hekmatpou D, Anoosheh M, Alhani F. Pathology of patient education: A qualitative study. Iran J Nurs. 2007;20:51–60. [Google Scholar]
- 7.Harwood A, Harrison EJ. How readable are orthodontic patient information leaflets? J Orthod. 2004;31:210–9. doi: 10.1179/146531204225022425. [DOI] [PubMed] [Google Scholar]
- 8.Felley C, Perneger TV, Goulet I, Rouillard C, Azar-Pey N, Dorta G, et al. Combined written and oral information prior to gastrointestinal endoscopy compared with oral information alone: A randomized trial. BMC Gastroenterol. 2008;8:1–7. doi: 10.1186/1471-230X-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klein NP, Kissner J, Aguirre A, Sparks R, Campbell S, Edwards KM, et al. Differential maternal responses to a newly developed vaccine information pamphlet. Vaccine. 2009;28:323–8. doi: 10.1016/j.vaccine.2009.10.046. [DOI] [PubMed] [Google Scholar]
- 10.Humphris GM, Ireland RS, Field EA. Immediate knowledge increase from an oral cancer information leaflet in patients attending a primary health care facility: A randomised controlled trial. Oral Oncol. 2001;37:99–102. doi: 10.1016/s1368-8375(00)00069-5. [DOI] [PubMed] [Google Scholar]
- 11.Keulers BJ, Welters CF, Spauwen PH, Houpt P. Can face-to-face patient education be replaced by computer-based patient education? A randomised trial. Patient Educ Couns. 2007;67:176–82. doi: 10.1016/j.pec.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 12.Strömberg A, Dahlström U, Fridlund B. Computer-based education for patients with chronic heart failure. A randomised, controlled, multicenter trial of the effects on knowledge, compliance and quality of life. Patient Educ Couns. 2006;64:128–35. doi: 10.1016/j.pec.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 13.Venmans LM, Gorter KJ, Baard KP, Rutten GE, Hak E. Acceptability and effects of an educational leaflet on infections in type 2 diabetes patients: A randomized controlled trial in primary care. Prim Care Diabetes. 2007;1:135–42. doi: 10.1016/j.pcd.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 14.Little P, Rumsby K, Kelly J, Watson L, Moore M, Warner G, et al. Information leaflet and antibiotic prescribing strateg ies for acute lower respiratory tract infection. JAMA. 2005;22:3029–35. doi: 10.1001/jama.293.24.3029. [DOI] [PubMed] [Google Scholar]
- 15.Wetzels R, Wensing M, Van Weel C, Grol R. A consultation leaflet to improve an older patient's involvement in general practice care: A randomized trial. Health Expect. 2005;8:286–94. doi: 10.1111/j.1369-7625.2005.00354.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sawamura K, Ito H, Koyama A, Tajima M, Higuchi T. The effect of an educational leaflet on depressive patients’ attitudes toward treatment. Psychiatry Res. 2010;177:184–7. doi: 10.1016/j.psychres.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 17.Smith SG, Wolf MS, Obichere A, Raine R, Wardle J, von Wagner C. The development and testing of a brief (’gist-based’) supplementary colorectal cancer screening information leaflet. Patient Educ Couns. 2013;93:619–25. doi: 10.1016/j.pec.2013.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arhan E, Serdaroglu A, Soysal S, Ozcelik A, Gucuyener K, Demir E. Assessment of mother’ knowledge and perceptions of electroencephalography and determination of the short-term effect of an informational leaflet. Epilepsy Behav. 2009;15:491–5. doi: 10.1016/j.yebeh.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 19.Petti S, Scully C. Oral cancer knowledge and awareness: Primary and secondary effects of an information leaflet. Oral Oncol. 2007;43:408–15. doi: 10.1016/j.oraloncology.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 20.Heikkinen K, Helena LK, Taina N, Anne K, Sanna S. A comparison of two educational interventions for the cognitive empowerment of ambulatory orthopaedic surgery patients. Patient Educ Couns. 2008;73:272–9. doi: 10.1016/j.pec.2008.06.015. [DOI] [PubMed] [Google Scholar]
- 21.Rossi M, McClellan R, Chou L, Davis K. Informed consent for ankle fracture surgery: Patient comprehension of verbal and videotaped information. Foot Ankle Int. 2004;25:756–62. doi: 10.1177/107110070402501011. [DOI] [PubMed] [Google Scholar]


