Abstract
Introduction:
Children are more risk-prone group of the population and low birth weight (LBW) is the leadingcause of newborns’ mortality and morbidity. LBW is defined as child's birth weight lower than 2500 g. Many maternal and fetal factors are determined as risk factors of LBW. This study tries to detect related factors to LBW and effect of them on children's growth pattern up to sixth month of life in Health centers of Urmia city, Iran.
Materials and Methods:
A cross-sectional study was carried out in Urmia city using registered data from mothers’ documents. All related data such age and weight of infants, mothers’ age, gestational age (GA) at the time of delivery, time gap between two pregnancies, past history of abortion, prenatal care history, systemic and underlying diseases, hemoglobin of mothers during pregnancy, and pattern of infant's growth up to sixth month of age were registered in a questionnaire. All registered data were transferred to SPSS 15 software and analyzed.
Results:
Mean ± SD of birth weight was 3071 ± 625.66 g. There was a significant relationship between birth weight and mother's age (P < 0.001) and weight (P < 0.001). Children of mothers younger than 18 years had much birth weights. There was a significant relationship between birth weight and GA during delivery (P < 0.001). Children of preterm labor had lower birth weights. In twins, LBW was more prevalent (P < 0.001).
Conclusion:
Our results show that LBW is related to multiple causes and that most of them are preventable with educational programs and also strict and regular prenatal care. Decreasing incidence of LBW children can be achieved by cooperation between different parts of health and clinical systems.
Keywords: Children, growth pattern, low birth weight
INTRODUCTION
Children are the most valuable property of mankind and also are the most vulnerable part of the population.[1] Birth weight is one of the most important health indicators of development in every country as one of the main factors for normal growth and development and even survival of newborns and infants.[2] Based on World Health Organization (WHO)'s definition, low birth weight (LBW) defines as a child with birth weight lower than 2500 g.[3] From 120 million reported child birth annually worldwide, 20 million are LBWs. LBW is the cause of 70% of newborns’ mortality, especially in developing countries. Based on the 2002 report of WHO, the prevalence of LBW is approximately 10% in Asia and 9% in Iran. In a report from Kohgiluye Boyerahmad province, Iran, mortality due to LBW and prematurity were 5% and 35%, respectively.[4,5]
LBW is a result of preterm labor (PL) or intrauterine growth retardation (IUGR). Approximately 15.5% of all births, or more than 20 million infants worldwide, are born with LBW. The level of LBW in developing countries (16.5%) is more than double the level in developed regions (7%).[6] More than 95% of LBW babies are born in developing countries.[2] In Iran, the rate of LBW is different from 8.5[7] to 9.1[8] in different provinces of the country. LBW not only is the leading cause of mortality but also results in disability, increased risk of infections and hematological and nutritional diseases.[7]
There are several causing factors for LBW: Nutritional status and pattern of weight gaining on mother during pregnancy, history of obstetric complications such as abortion or another child with LBW, chronic underlying diseases in mother, alcohol use and smoking. Other factors are prenatal care, hemoglobin (Hb) and hematocrit (Hct) level of mother during pregnancy, socioeconomic situation, mother's activity during pregnancy and demographic factors (age, weight,…) and so on.[9,10]
An LBW child can have several problems, especially in developing countries except psychological consequences; high cost of care and treatment of such children for parents (that are usually from low socioeconomic layers of community) can be catastrophic. LBW is the leading cause of mortality in newborns,[11] designing a study to determine risk factors of LBW can help health system authorities to prevent it and lower its mortality and morbidity. As there are many risk factors involved in LBW, it is important to find the prevalent regional factors to have a broad picture for designing educational programs or policy making. This study tries to detect LBW-related factors and their effect on children's growth pattern up to sixth month of life in Health centers of Urmia city, Iran.
MATERIALS AND METHODS
This was a cross-sectional study carried out on information obtained from registered documents of 250 families which were under supervision and follow up in the health centers of Urmia city and its related villages in 2011. Documents were selected randomly. Four health centers from four areas of Urmia city were selected and 54 completed questionnaires were obtained from each center, which were chosen randomly. All related data such as age and weight of infants, mothers’ age, gestational age (GA) at the time of delivery, time gap between two pregnancies, past history of abortion, prenatal care history, systemic and underlying diseases, Hb of mothers during pregnancy, and pattern of infant's growth up to six months of age were registered in a questionnaire. All infants with malformation and also cases of still birth were excluded from the study. LBW based on international definition was birth weight under 2500 g, very LBW (VLBW) was under 1500 g, definition of preterm labor was delivery before 37 weeks of pregnancy. All data were transferred to SPSS-15 software and analyzed using t-test (to compare GA and child number in pregnancy with birth weight) and Chi-square test to compare gender and history of bleeding with birth weight). A P value of < 0.05 was considered statistically significant.
Confounding factors were controlled by applying exclusion and inclusion criteria[Tables 1 and 2].
Table 1.
Birth weight–based demographic variables
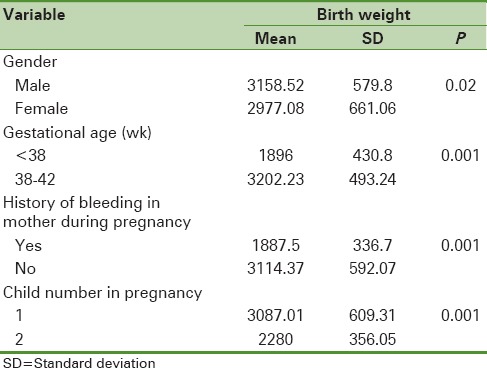
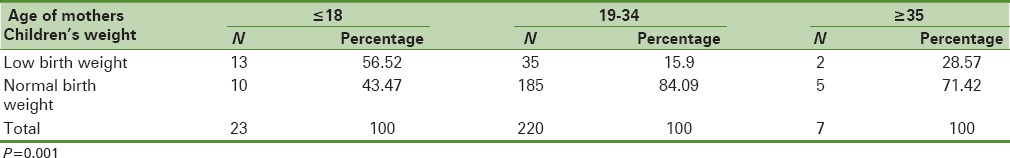
Table 2.
Association of low birth weight with mothers’ age
RESULTS
Two hundred and fifty infants were included in this study; 120 (48%) were female and 130 (52%) were male. Data show that 20.1% of infants had birth weight under 2500 g (LBW) and 79.9% were more than 2500 g. A 75.8% of females were weighed more than 2500 g and 24.2 were under 2500 g. These data were 83.2% and 16.3% for male infants, respectively. Mean grade of birth weight was 3071 (±625.66) g totally. Mean weight (kg), delivery rate and gap between present and previous delivery for mothers (years) were 63.07 (±13.09), 4.31 (±2.24) and 3.36 (±1.05), respectively.[Table 1]
Twenty-three infants (9.2%) were delivered from mothers under the age of 18 and 7 infants (2.8%) from mothers older than 35 years. The rest of the children's mothers (220 mothers (88%)) were between 18 and 35 years of age. A 63.2% of mothers had been experiencing their first pregnancy, 24.4% second pregnancy, 9.6% third, and 7% forth and more. The gap between two pregnancies was more than 4 years in 69.1% of mothers, 3 years in 8.51%, and 2 years and lower in 22.34% of mothers.[Table 2]
Ninety percent of deliveries occurred between 38 and 42 weeks of GA; only 10% of deliveries were under 38 weeks. A 97.2% of the participants were home makers and 2.8% were working; 7.2% illiterate, 29.6% elementary school, 32.4% guidance school, 23.6% diploma holders, and 7.2% had academic degrees.
Data showed that 3.2% of mothers had bleeding during pregnancy and 9.2% had some problems such as edema, systolic blood pressure over 140 mmHg and albominuria. Hb was in normal range in 90.4%; only 4% had a history of abortion.
A 54.4% of participants had normal weight before pregnancy, 7.2% were underweight[body mass index (BMI ≤ 18.5)], and 38.4% were overweight (BMI ≥ 25).
Height-to-weight index of infants in 12.8% was under 3rd percentile, 54% between 3rd and 50th percentiles, and 29.6% between 50th and 97th percentiles.
In Chi-square analysis, there was a significant relationship between birth weight and gender of infants (P = 0.02).
In t-test analysis, there was a significant relationship between birth weight and mother's age (P < 0.001) and weight (P < 0.001). Mothers younger than 18 years had more birth weights. Mothers categorized as underweight had children with LBWs. There was no significant correlation between birth weight and gap between two pregnancies (P = 0.115).
There was a significant relationship between birth weight and GA during delivery (P < 0.001). preterm labor children had LBWs. In twins, LBW was more prevalent (P < 0.001). There was no significant correlation between birth weight and history of abortion, mother's work, and mother's level of graduation.
Based on Chi-square test pattern of growth in the first 6 months of life was related to birth weight (P < 0.001).
In children with birth weight more than 2500 g growth indexes was between 50th and 97th percentiles in 38.9%, between 3rd and 50th in 58.4%, and under 3rd in 2.6%; for LBW children (birth weight < 2500 g)–0.5%, 53%, and 46.5%, respectively.
DISCUSSIONS
LBW is the leading cause of mortality in newborns and infants and with congenital malformations are major causes of morbidity[6]
Based on World Health Organization (WHO) reports, female children are at more risk of LBW.[12,13] In the present study, we found that the prevalence of LBW was more in female rather than male children significantly. Studies by Delaram in Shehrekord[7] and Rafii in Arak[8] concluded similar results in Iran but Roudbari in Zahedan[14] did not find significant difference between gender and LBW prevalence.
Mothers between 18 and 35 years of age had lowest prevalence of LBW in their children. The highest prevalence was for mothers younger than 18 years but was not significant in over 35 years old (of course, prevalence was more in 13–49 year olds). Low parity in our >35 years old mothers and observing appropriate gap between two pregnancies in this group can be the cause of compensation of high age risk, because in most of the studies, mother's high age is a risk factor for LBW.[1]
In our study, mothers in first pregnancy had highest percentage of LBW children; this result is concomitant with Delgad et al.'s work[12] in Brazil. Then in our study, first pregnancy was a strong risk factor that needs more attention by health system authorities.
The most important risk factor in all studies and also in our study was preterm labor.[13] The results of studies showed that many risk factors as women younger than 20 years, low maternal weight < 50 kg, and smoking during pregnancy, can be the reason of preterm labor and preterm labor is the most risk factors in morbidity and mortality of children.[15] We did not find relationship between mothers’ level of education and LBW; but Gisselman et al., found such relationship.[16] This discrepancy can be due to increasing knowledge of mothers about pregnancy in our study, after frequent educational programs are implemented for pregnant mothers in Iran's health centers.
In our study, similar to Eghbalian[12] and Minagawa[17] studies no relationship between LBW and mothers’ work was found while Choudhary et al., in India[18] resulted that 71.4% of mothers engaged as laborer gave birth to LBW babies as compared with others. Also they showed that duration of day-time rest taken by mothers of LBW newborns 76.5% belonged to mothers who took less than 1 h day-time rest as compared with only 7.1% newborns whose mothers took the rest for 90 min or more. The difference between our study and Choudhary could be related to the design of study, which in Choudhary study was more focused on the types of work but we only asked about working or not working. Another possible cause is the considerable difference between the prevalence of LBW in India and Iran. Based on WHO statistics, the prevalence of LBW in India is approximately 30%, whereas in our country it is approximately 8.5%.
Our study also has found significant relationship between LBW and mothers’ age (P < 0.001), pre-pregnancy mothers’ weight (P < 0.001), GA (P < 0.001), and children's gender (P = 0.02). There was no relationship between LBW and mothers’ work, level of education, and history of abortion.
The statistics showed that the rate of LBW in Iran is better than the mean rate in our region as based on WHO report, the mean LBW of western Asian countries is 15.4%.[2] The results of our study punctuates on the potential risk factors of LBW. Pregnancy in high ages is an important risk factor. The age of marriage in Iran has been increased during the past decade; then educational programs during marriage consultations should be designed to encourage couples (especially who married at older ages) to bear a child soon because of maternal and fetal complications. Also mothers should be educated on the optimal weight before and during pregnancy. Due to national programs implementation in health and clinical centers of the country under supervision of Iranian Ministry of Health, the mothers at any level of education are educated on the necessary issues, which a pregnant woman must know. Family physician program is held in most of rural areas in the country and spreading the same to urban areas, will play an important role in face-to-face education and controlling risk factors of LBW.
Although this study included approximately 250 participants, results give a broader regional perspective on the situation of risk factors in Urmia city and province and highlight the educational needs for this region. The differences between cultures and socioeconomic situations cause some risk factors more important than other. We could not control them and another limitation in this study was that some of our needed information was unregistered in documents so we invited mothers and completed the questionnaire.
CONCLUSIONS
Our study also has found significant relationship between LBW and mothers’ age, pre-pregnancy mothers’ weight, GA, and children's gender. Most of these causes are preventable with educational programs and strict and regular prenatal care. Decreasing incidence of LBW children can be achieved by cooperation between different parts of health and clinical systems.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.de Onis M, Blössner M, Villar J. Levels and patterns of intrauterine growth retardation in developing countries. Eur J Clin Nutr. 1998;52:5–15. [PubMed] [Google Scholar]
- 2.New York: UNICEF; 2004. United Nations Children's Fund and World Health Organization, Low Birthweight: Country, regional and global estimates. [Google Scholar]
- 3.Last GM. Dictionary of epidemiology. In: Shojaee H, Malekafzali H, editors. 4th ed. Vol. 2. Tehran, Iran: Samat Publication; 2004. pp. 230–45. [Google Scholar]
- 4.Ahmadvand AP, Jamshidi HR. 1st ed. Tehran, Iran: Ebnesina Publication; 2002. World reporting of Health; pp. 140–58. [Google Scholar]
- 5.Maghri MK, Hamid H. Prevalence of Low Birth Weight and some risk factors in Valiasr Hospital of Birjand. Journal of Birjand University Medical Science. 2003;10:12–5. [Google Scholar]
- 6.Stoll BJ, Kliegman RM. 17th ed. Philadelphia: Saunders; 2004. Overview of mortality and morbidity. Nelson Textbook of Pediatrics; pp. 519–23. [Google Scholar]
- 7.Delaram M, Hasan Poor A, Noorian K, Kazemian A. Impact of early admission in labor on maternal and neonatal outcomes in Hajar health-care center of Shahr-e-Kord, Iran. J Birjand University Medical Science. 2007;14:9–15. [Google Scholar]
- 8.Rafii M. Prevalence of Low Birth Weight and Obesity and some concomitant factors in live offspring's in 2006 and compare with 2002 result's in Arak Talleghani Hospital. Iran J Pediatr. 2007;17:47–53. [Google Scholar]
- 9.Geneva: World Health Organization; 2004. WHO Technical Consultation, ’Towards the development of a strategy for promoting optimal fetal growth, Report of a meeting (draft) [Google Scholar]
- 10.Ansari H, Zafar P, Rahiami E. Relationship between exposure pregnancy and neonatal Low Birth Weight: A Case Control Study. J Jahrom University Medical Science. 2008;6:17–26. [Google Scholar]
- 11.WHO. Low Birth weight. Mother Child Health J. 1992;2:1–13. [Google Scholar]
- 12.Delgado-Rodríguez M, Pérez-Iglesias R, Gómez-Olmedo M, Bueno-Cavanillas A, Gálvez-Vargas R. risk factors for low Birth weight: Results from a Case–Control study in southern spain. Am J Phys Antropol. 1998;105:419–24. doi: 10.1002/(SICI)1096-8644(199804)105:4<419::AID-AJPA2>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 13.Golestan M, Akhavan Karbasi S, Fallah R. Prevalence and risk factors for low birth weight in Yazd, Iran. Singapore Med J. 2011;52:730–3. [PubMed] [Google Scholar]
- 14.Roudbari M, Yaghmaei M, Soheili M. Prevalence and risk factors of low-birth-weight infants in Zahedan, Islamic Republic of Iran. East Mediterr Health J. 2007;13:838–45. [PubMed] [Google Scholar]
- 15.Ferraz EM, Gray RH, Cunha TM. Determinants of preterm delivery and intrauterine growth retardation in north-east Brazil. Int J Epidemiol. 1990;19:101–8. doi: 10.1093/ije/19.1.101. [DOI] [PubMed] [Google Scholar]
- 16.Gisselmann MD. Education, infant mortality and Low birth weight in Sweden 1973-1990: Emergence of Low birth weight paradox. Scend J Public Health. 2005;33:65–71. doi: 10.1080/14034940410028352. [DOI] [PubMed] [Google Scholar]
- 17.Minagawa AT, Biagoline RE, Fujimori E, de Oliveira IM, Moreira AP, Ortega LD. Low birth weight and prenatal maternal conditions. Rev Esc Enferm USP. 2006;40:548–54. doi: 10.1590/s0080-62342006000400014. [DOI] [PubMed] [Google Scholar]
- 18.Choudhary AK, Choudhary A, Tiwari SC, Dwivedi R. Factors associated with low birth weight among newborns in an urban slum community in Bhopal. Indian J Public Health. 2013;57:20–3. doi: 10.4103/0019-557X.111362. [DOI] [PubMed] [Google Scholar]


