Abstract
Angiosarcoma is a malignant neoplasm of endothelial cells of blood vessels, representing 2% of all sarcomas. The occurrence of angiosarcoma in the oral cavity is a rare. In general management includes resection and wide-field postoperative radiation therapy. The risk of local-regional failure and distant relapse is still a cause of worry. Herewith, a case of angiosarcoma of mandible in a female patient is presented, who presented with small, innocent-looking mass, which became a highly destructive malignant tumor within few days.
Keywords: Angiosarcoma, jaw, mandible, oral cavity
INTRODUCTION
Angiosarcoma is a malignant mesenchymal neoplasm of endothelial cells of blood vessels, representing 2% of all sarcomas with skin and soft tissue being the most common sites.[1] In head and neck region, it affects scalp and facial soft tissue. Angiosarcoma of the oral cavity is extremely rare. Clinically, it appears as red, blue or purple nodular mass.[2] As angiosarcoma of oral cavity is extremely rare, this may result diagnostic challenge, misclassification and inefficient management. Management includes complete surgical resection, followed by wide-field postoperative radiotherapy. Prognosis depends upon factors such as depth of tumor invasion, tumor diameter, local regional spread, distant metastasis, positive margins on surgical tumor resection and tumor recurrence.[3]
Herewith, a case of angiosarcoma of left mandible in a female patient is presented, who presented with small, innocent-looking mass, which became a highly destructive malignant tumor within few days.
CASE REPORT
A 52-year-old female reported to the department of oral medicine and radiology with a gingival growth in the left mandible since 1-month. History of the presenting illness revealed that initially the growth was small in size, but now rapidly progressed to the present size since few days. The growth was associated with difficulty in mastication, speech, swallowing and frequent bleeding. There was no history of fever, trauma and similar swelling elsewhere in the body, with noncontributory past medical or dental and family history.
On general examination, the patient was of normal built and height. Extraorally, a diffuse, soft, and slightly tender swelling was present involving left body of the mandible. A solitary, nontender left submandibular lymph node was palpable, which was firm in consistency. Intraorally, an exophytic, nodular, sessile mass was seen involving the gingival and alveolar mucosa in the mandibular left right posterior region, with approximate size of 4 cm × 5.5 cm. The overlying mucosa was pink to reddish with areas of yellowish necrotic slough. On palpation, the mass was soft to firm in consistency and was slightly tender, with variable amount of bleeding on probing [Figure 1a].
Figure 1.

(a) Solitary, exophytic, nodular mass involving the mandibular left right posterior region, with approximate size of 4 cm × 5.5 cm, at the time offirst reporting. (b) Patient's mouth full of growth, after few days
Based on the history and clinical examination, a provisional diagnosis of benign aggressive neoplasm of left mandible was made. Routine investigations, including complete blood count, serum urea and electrolyte, and urinalysis were all within normal limits.
On conventional lateral oblique view, mild erosion of the alveolar crest was seen [Figure 2a]. Patient was advised computed tomography (CT) scan. By the time patient reported after CT scan, her mouth was full of growth due to huge increase in the size of mass [Figure 1b].
Figure 2.
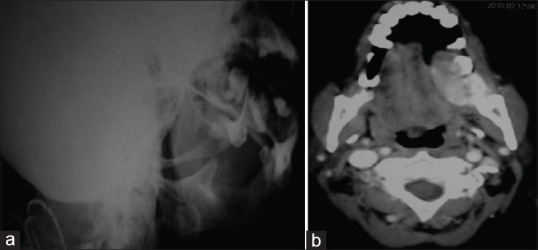
(a and b) On conventional lateral oblique view, mild erosion of the alveolar crest was seen. Axial computed tomography scan showing a single large, homogeneous, enhancing, soft tissue density lesion in the left mandibular posterior region, which showed enhancement on contrast administration, with the tongue displaced to opposite side with aggressive bone destruction of body of mandible on left side
Axial CT examination revealed a large, homogeneous, enhancing, soft tissue density lesion in the left mandibular posterior region, which showed enhancement on contrast administration, with the tongue displaced to opposite side with aggressive bone destruction of body of mandible on left side [Figure 2b]. The chest radiograph did not show any abnormality.
Based on the history of sudden increase in size of growth and clinical presentation of the lesion, and imaging features, a provisional diagnosis of aggressive vascular lesion, mostly the sarcoma of mandible was considered. The patient was referred to department of oral and maxillofacial surgery for the biopsy and further management and resection of the lesion with hemimandibulectomy under planned elective tracheostomy and carotid artery ligation was done. And the excised specimen was sent for histopathological examination [Figure 3a].
Figure 3.
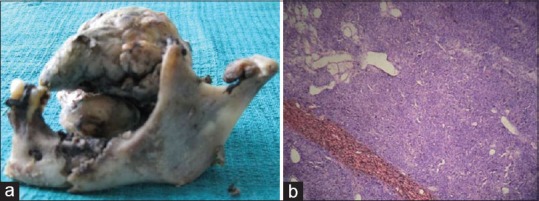
(a and b) Resected mass along with hemi mandible. Histopathologically, anaplastic endothelial cells arranged in sheets and alveolar pattern, with rampant mitotic activity (H and E, ×40)
Histopathological examination revealed a tumor mass underneath normal or mildly hyperplastic, ulcerated epithelium. The mass comprised anaplastic endothelial cells arranged in sheets and alveolar pattern, with rampant mitotic activity. The neoplastic cells showed diffusely infiltrative and perithelial distribution, with anatomizing channels [Figure 3b]. The histopathological diagnosis of high-grade anaplastic angiosarcoma was made. Unfortunately, the patient died after few days, because of cardiac arrest and respiratory complications,
DISCUSSION
Angiosarcoma of jaw has a predilection for elderly individuals when compared to angiosarcoma elsewhere in the body, which has predilection for children and young adults.[1] It occurs in both male and female equally. Clinically, the intraoral angiosarcoma appears as round or ovoid bluish nodular painless mass. The overlying surface may be ulcerated or intact, with tendency of spontaneous bleeding.[2] The present case showed similar findings. The differential diagnosis may include pyogenic granuloma, hemangioma, Kaposi's sarcoma, melanoma and metastatic lesions. Occasionally, angiosarcoma mimic periodontal disease and may be misdiagnosed as reactive lesions such as pyogenic granuloma.[4] The period of time for the presence of symptoms of angiosarcoma of the head and neck is short.
The exact etiology is unknown, certain risk factors has been documented such as chronic lymph edema, radiotherapy, vinyl chloride exposure, trauma and telangiectatic skin lesions.[5]
Diagnosis of angiosarcoma is established by histopathological examination which shows multiple vascular anastomoses, with solid necrotic or hemorrhagic areas. The neoplastic vessels present atypical endothelium with prominent hyper chromatic nuclei and can be classified in high or low grade based on their microscopic appearance.[6] However, immunohistochemical staining with CD34, Ulex europaeus agglutinin I and factor VIII antigen is often required. Factor VIII-like antigen is synthesized in vascular endothelial cells and CD34 is specifically stained in vascular endothelial cells.[7]
Management includes radical surgery with sufficient margins, followed by radiotherapy (4000–5000 rads) as the treatment of choice. Chemotherapy has a low impact on the disease. Fukushima et al. reported favorable results with the use of recombinant interleukin 2, combined with surgery.[6] Free margins are the best prognostic factor for avoiding recurrence. Cervical metastasis occurs in 10–15% of cases and distal metastasis to bone, liver, lungs or skin occurs in 30% of patients during the first 24 months of the disease.[5]
The diagnosis and treatment of angiosarcoma presents challenges and hence it is crucial to perform a thorough history and physical examination with a high clinical suspicion. The overall prognosis is poor. Mortality results from either extensive local disease or distant metastasis to organs such as lungs. In the present case, patient had localized disease without distant metastasis. The poor prognosis has been correlated with multifocal disease, positive surgical margins, size of the tumor (>5 cm of external diameter of the tumor), mitotic rate (>3 HPF), depth of invasion (>3 mm), local regional recurrence and distant metastases.[8] In our patient, delay on the part of patient placed her at significant risk for reduced survival, especially given the size of her tumor at second time reporting after CT. The tumor is often so extensive at diagnosis that complete surgical resection of the tumor may not be feasible. Even with optimal local regional treatment, the likelihood of a local recurrence in the radiation field or distant metastases through hematogenous spread is quite high.[9]
CONCLUSION
The relative rarity of its occurrence in the oral cavity, as well as resemblance of its clinical, radiographic and histopathological features to other benign and malignant conditions, poses a diagnostic challenge to the clinicians. Expanding nodular or papule type lesions that bruise or bleed for a prolonged period of time should raise concerns about an underlying malignancy and should be promptly investigated.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Fisher C. Soft tissue tumor. In: LeBoit PM, Burg G, Weedon D, Sarasin A, editors. World Health Organization Classification of Tumours. Pathology and Genetics of Skin Tumours. Lyon: IARC Press; 2006. pp. 230–62. [Google Scholar]
- 2.Triantafillidou K, Lazaridis N, Zaramboukas T. Epithelioid angiosarcoma of the maxillary sinus and the maxilla: A case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:333–7. doi: 10.1067/moe.2002.126022. [DOI] [PubMed] [Google Scholar]
- 3.Florescu M, Simionescu C, Margaritescu C, Georgescu CV. Gingival angiosarcoma: Histopathologic and immunohistochemical study. Rom J Morphol Embryol. 2005;46:57–61. [PubMed] [Google Scholar]
- 4.Abdullah BH, Yahya HI, Talabani NA, Alash NI, Mirza KB. Gingival and cutaneous angiosarcoma. J Oral Pathol Med. 2000;29:410–2. doi: 10.1034/j.1600-0714.2000.290807.x. [DOI] [PubMed] [Google Scholar]
- 5.Loudon JA, Billy ML, DeYoung BR, Allen CM. Angiosarcoma of the mandible: A case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:471–6. doi: 10.1016/s1079-2104(00)70127-2. [DOI] [PubMed] [Google Scholar]
- 6.Fukushima K, Dejima K, Koike S, Tei G, Asano J, Ueda M, et al. A case of angiosarcoma of the nasal cavity successfully treated with recombinant interleukin-2. Otolaryngol Head Neck Surg. 2006;134:886–7. doi: 10.1016/j.otohns.2005.03.053. [DOI] [PubMed] [Google Scholar]
- 7.Wong KF, So CC, Wong N, Siu LL, Kwong YL, Chan JK. Sinonasal angiosarcoma with marrow involvement at presentation mimicking malignant lymphoma: Cytogenetic analysis using multiple techniques. Cancer Genet Cytogenet. 2001;129:64–8. doi: 10.1016/s0165-4608(01)00431-9. [DOI] [PubMed] [Google Scholar]
- 8.Kharkar V, Jadhav P, Thakkar V, Mahajan S, Khopkar U. Primary cutaneous angiosarcoma of the nose. Indian J Dermatol Venereol Leprol. 2012;78:496–7. doi: 10.4103/0378-6323.98086. [DOI] [PubMed] [Google Scholar]
- 9.Mendenhall WM, Mendenhall CM, Werning JW, Reith JD, Mendenhall NP. Cutaneous angiosarcoma. Am J Clin Oncol. 2006;29:524–8. doi: 10.1097/01.coc.0000227544.01779.52. [DOI] [PubMed] [Google Scholar]


