Abstract
Background and Aims:
Today Glasgow coma scale (GCS) is the most well-known and common score for evaluation of the level of consciousness and outcome predict after traumatic brain injuries in the world. Regarding to some advantages of the full outline of unresponsiveness (FOUR) score over GCS in intubated patients, we’re going to compare the precision of these two scores in predicting the outcome predict in intubated patients.
Methods:
This research was a diagnostic-based study, which was conducted prospectively on 80 patients with Traumatic brain injury who were intubated and admitted to Intensive Care Unit (ICU) of Educational Hospitals of Mazandaran University of Medical Science during February 2013 to August 2013. The scores of FOUR and GCS were measured by the researcher in the first 24 h of admission in ICU. The information's recorded in the check list including the mortality rate of early and late inside of the hospital interred to excel. The findings were analyzed using SPSS software, through descriptive statistics and regression logistic.
Results:
The results showed of 80 patients 21 patients (20%) were female and 59 patients (80%) were male. The age average of the samples was 33.80 ± 12.60 ranging from 16 to 60 years old. 21 patients (26.2%) died during treatment. Of 21 patients, 15 patients died during first 14 days (18.7%) and 6 patients died after 14 years (7.5%). The area under curve (AUC) of FOUR score in early mortality was 0.90 (C1 = 0.95, 0.88–0.90). The amount AUC for GCS was 0.80 (C1 = 0.95, 0.78–0.84), which in delayed mortality it was ordered as 0.86 (C1 = 0.95, 0.84–0.90) and 0.89 (C1 = 0.95, 0.78–0.88).
Conclusion:
The research results indicated that FOUR score is more exact and more practical in intubated patients regarding lack of verbal response factor in early mortality prediction in GCS. Hence, it is recommended for health professionals to use the FOUR score to predict the early outcome of intubated patients with traumatic brain injuries.
Keywords: Full outline of unresponsiveness, Glasgow coma scale, Intensive Care Unit, mortality, traumatic brain injuries
INTRODUCTION
Trauma brain injury (TBI) is one of the death reasons in the worldwide. It is estimated that 1.5 million people die due to TBI each year, and millions of people need emergency treatment cause of TBI. Unfavorable consequences of TBI is about 20%.[1,2] Determining the severity of TBI is the first guideline for treatment and outcome of trauma.[3,4] The most common tool to determine of severity of brain trauma is Glasgow coma scale (GCS).[5]
This score was invented by Tizad and Janet on 1974. Many studies suggested that GCS provides the first care policy and prediction of the first outcome, mortality and morbidity.[5,6] Although GCS is a suitable score for determining the TBI severity, it has some limitations.[5,6,7]
The limitations of GCS made Wijdicks et al. to create a new score called full outline of unresponsiveness (FOUR) in order to more comprehensive examination of the patient.[8] FOUR provides the complementary information like brain stem reflex, visual following and respiratory pattern, which are not included by GCS.[8] One of the characteristics of FOUR that emphasized by its inventors is that FOUR needs no verbal response and hence it is more practical for critical intubated patients.[9,10] Verbal response factor in GCS is a sources of some persona decision among clinicians’ and nurses in examination of intubated patients. This limitation commonly leads to record of lower GCS scores. Regarding these, there is a question that does the endotracheal tube affects on predicting the outcome by the scores FOUR and GCS?
Some researchers conducted a study in order to compare the prediction abilities of FOUR and GCS in patients with TBI.[8,11,12] Although as our knowledge no studies was found in scientific data banks about comparing these two scores in patients with endotracheal tubes.
Hence, the researcher aimed to compare the prediction abilities of FOUR and GCS in intubated and nonintubated patients to answer this important question that does the endotracheal tube effect on the prediction precision of these two scores, FOUR and GCS?
METHODS
Design and sampling
This study was conducted on 80 patients with TBI in Intensive Care Unit (ICU) of the hospitals of Mazandaran University of Medical Science during February 2013 to August 2013. The number of samples was based on Fugate et al. (B), and sampling method was convenience method. Of 92 patients with TBI admitted during our study 80 were included based on inclusion and exclusion criteria. The inclusion criteria were as following: having TBI, age over 16 and below 65,[6,13,14] at least 24 h being in ICU[15] and having endotracheal tube. Furthermore, the exclusion criteria of the study included patients with abnormal background, drug abusing and taking sedative medicine before score measurements.
In this study, GCS and FOUR scores were measured by the researcher 15 min difference from each other (FOUR and GCS) in ICU within the first 24 h of admission. Then, injury outcome including early (average death cases before 14 days) and delayed mortality (14 days after admission) were recorded and registered.
Tools
The checklists included the demographic information, kinds of injuries to head and consciousness level by FOUR and GCS and injury outcomes.
Glasgow coma scale GCS is a standard score in the worldwide accepted by neurologists and the most common clinical tool to determine the brain trauma severity.[5] GCS has three items including: (1) Eye or visual, (2) motor and (3) verbal, the scores is 4, 5, 6, respectively, and totally included a range of 3–15.
Full outline of unresponsiveness score has four item including (1) eye or visual, (2) motor, (3) brain stem reflex and (4) respiratory pattern. Each item scored from 0 to 4 and totally the range of sores is between 0 and 16. The validity and reliability of FOUR have been proved in Iran and abroad studies.[8,16,17]
Procedure
All patients’ families agreed by signing the consent form and the aim and procedure of the study explained for families. Furthermore, the study was delivered to the ethical committee of the University.
After taking the license from the university ethical committee, the data were collected, entered into the SPSS Inc. Released 2007. SPSS for Windows, Version 16.0. Chicago, SPSS Inc.
Statistic
Data analyzed by regression logistic test with the precision of 95%. The sensitivity and specificity of total score of GCS and FOUR were compared in prediction of early and delayed mortality among TBI patients. The receiver operating characteristic (ROC) curve was drawn and cut-off was calculated correctly then the amounts of area under curve (AUC) and cut-off were evaluated. P <0.05 considered as meaningful.
RESULTS
In this study, all study population (n = 80) were available during the study. The age range of the participants was 33.80 ± 12.60 years. 21 patients (20%) were female, and the rest were male 59 patients (80%). The causes of admission were as follow: 20 patients were admitted because of the hematoma epidural, 10 patients because of subdural, 18 by brain edema and 32 because of bleeding brain context.
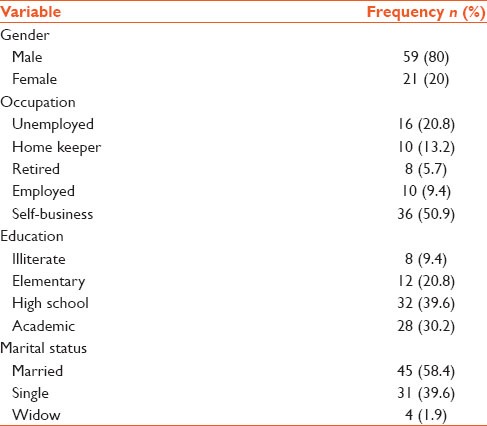
Injury kinds comprised: 42 patients had accidents by motorcycles, 28 accidents by cars and 10 patients fell off from a height as it is clear from results the accidents of motorcycles were the main reason of trauma for head [Table 1].
Table 1.
Demographic information of the samples
The severity of injury were as following: 12 patients (15%) had moderate injuries, 68 patients (85%) had severe injuries, so there wasn’t any patients with mild injuries, and most patients were in severe injury group. 21 patients died (26.2%) that of 21 patients 15 (18.7%) died before 14 days and 6 (7.5%) died after 14 days.
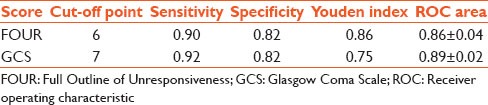
Logistic regression test showed no relation among the age, sex and reason of admission (P > 0.05), but there was a meaningful relation between the scores of FOUR and GCS. In order to compare the prediction power of these two scores, ROC curve was drowned to predict the two expected outcomes. The value of AUC for FOUR in early mortality was 0.90 (C1 = 0.95, 0.88–0.90) and for GCS it was 0.80 (C1 = 0.95, 0.78–0.84) and for delayed mortality the value of FOUR and GCS were 0.86 (C1 = 0.95, 0.84–0.90) and 0.89 (C1 = 0.95, 0.78–0.88), respectively. The sensitivity and specificity of prediction of early mortality for FOUR in cut off 4 were 0.92 and 0.87 and for GCS in cut-off 4 was 0.85 and 0.78. The sensitivity and specificity of delayed mortality for FOUR in cut-off 6 were 0.90 and 0.82 and for GCS in cut off 7 was 0.92 and 0.82. The values of the best cut-off sensitivity and specificity of Yuden index and the value of AUC were shown in Tables 2 and 3.
Table 2.
Comparison of GCS and FOUR in prediction of early mortality in intubed patients
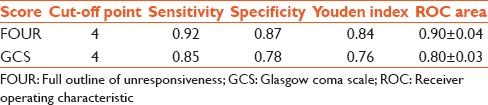
Table 3.
The comparison of GCS and FOUR in prediction of delayed mortality in intubed patients
DISCUSSION
In this study, TBI mainly involved the young men and active groups of the society due to their high risky behaviors, which correspond to the studies of Izadi et al.[18] and Farid et al.[15]
In the present study, most of the injury mechanisms have been caused by motor vehicles specially motorcycles which corresponds to Izadi and Jose's study.[19]
There was no meaningful difference among the patients’ age, sex, kinds of injuries and reason of admission and the outcome, which corresponds to Izard's study, but there was a significant relation between injury mechanism and outcome in Gan's study that this difference explainable with elimination of people over 60 years of age in current research.[20] Meanwhile, there was a meaningful relation between GCS and FOUR scores and trauma outcome. In the case of comparison of prediction power the FOUR has a higher curve level than GCS in early mortality as it is obvious in the AUC for FOUR was 0.90 and for GCS was 0.80. These results also were in harmony with studies of Farid et al., Akavipat et al. In this study, the difference of FOUR and GCS in the prediction of mortality was so small and was not remarkable statistically because of the difference of this study inclusion criterion to other studies. The inclusion criterion of this study was to have an endotracheal tube while there were not such criteria in other studies. However, in prediction of delayed mortality the value of FOUR was (AUC = 0.86) and the value of GCS was (AUC = 0.89), which were different mildly and were not meaningful statistically that correspond to the studies of Farid et al., Akavipat et al.[11,12,13,14,15,16,17,21]
CONCLUSION
The findings of the study suggested FOUR is more precise and more practical than GCS due to lack of ability of TBI patients for the verbal response in GCS. Totally in predicting of early mortality in intubated patients FOUR was better, although in predicting of delayed mortality, there is no meaningful difference between these two scores. Therefore, it is recommended to health professionals to use FOUR scores to predict the early mortality in intubated TBI patients and evaluate and measure it as a part of routine examination of TBI patients in 1st day of admission. The health care professionals at the time of consciousness score level changes to create a method for patients who need new and special care and improved care quality by exact prediction of severity and process of the illness. Moreover, using this score of prediction makes it possible to have exact judgments about predicting the mortality of impatiens, occupying hospital beds and the process of patients’ treatment.[22]
The limitations of this study included finding the suitable samples for this research and also taking sedative medicine by most of the patients suffering from head trauma, which was an exclusion of the study. Hence, it is recommended to continuous researches with bigger sample size and longer follow-ups.
ACKNOWLEDGMENTS
We the authors of the article are appreciate the relatives of the patients and the personnel of the ICU of Imam hospital in Sari and Razi hospital in Qaemshahr and also the authorities of Nasibeh nursing and midwifery school in Sari and the research deputy of Mazandaran university of medical sciences for his scientific support.
Footnotes
Source of Support: Mazandaran University of Medical Sciences who contributed and supported us to make the present study.
Conflict of Interest: None declared.
REFERENCES
- 1.Bruns J, Jr, Hauser WA. The epidemiology of traumatic brain injury: A review. Epilepsia. 2003;44(Suppl 10):2–10. doi: 10.1046/j.1528-1157.44.s10.3.x. [DOI] [PubMed] [Google Scholar]
- 2.Fleminger S, Ponsford J. Long term outcome after traumatic brain injury. BMJ. 2005;331:1419–20. doi: 10.1136/bmj.331.7530.1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Delney KA, Gold FL. Manegment of the multiply injured or intoxicated. In: Cooper P, Golfinos J, editors. Head Injury. 4th ed. New York: McGraw-Hill; 2000. pp. 41–62. [Google Scholar]
- 4.Valadka AB, Narayan RK. Emergency room manegment of the head injury patient. In: Narayan R, Povlishock J, editors. Neurotrauma. Newyork: McGraw-Hill; 1996. pp. 119–35. [Google Scholar]
- 5.The Brain Trauma Foundation. The American Association of neurological surgeons. The joint section on neurotrauma and critical care. Glasgow coma scale score. J Neurotrauma. 2000;17:563–71. doi: 10.1089/neu.2000.17.563. [DOI] [PubMed] [Google Scholar]
- 6.Signorini DF, Andrews PJ, Jones PA, Wardlaw JM, Miller JD. Predicting survival using simple clinical variables: A case study in traumatic brain injury. J Neurol Neurosurg Psychiatry. 1999;66:20–5. doi: 10.1136/jnnp.66.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andrews PJ, Sleeman DH, Statham PF, McQuatt A, Corruble V, Jones PA, et al. Predicting recovery in patients suffering from traumatic brain injury by using admission variables and physiological data: A comparison between decision tree analysis and logistic regression. J Neurosurg. 2002;97:326–36. doi: 10.3171/jns.2002.97.2.0326. [DOI] [PubMed] [Google Scholar]
- 8.Wijdicks EF, Bamlet WR, Maramattom BV, Manno EM, McClelland RL. Validation of a new coma scale: The FOUR score. Ann Neurol. 2005;58:585–93. doi: 10.1002/ana.20611. [DOI] [PubMed] [Google Scholar]
- 9.Akavipat P. Endorsement of the FOUR score for consciousness assessment in neurosurgical patients. Neurol Med Chir (Tokyo) 2009;49:565–71. doi: 10.2176/nmc.49.565. [DOI] [PubMed] [Google Scholar]
- 10.Knaus WA, Wagner DP, Zimmerman JE, Draper EA. Variations in mortality and length of stay in intensive care units. Ann Intern Med. 1993;118:753–61. doi: 10.7326/0003-4819-118-10-199305150-00001. [DOI] [PubMed] [Google Scholar]
- 11.Akavipat P, Sookplung P, Kaewsingha P, Maunsaiyat P. Prediction of discharge outcome with the full outline of unresponsiveness (FOUR) score in neurosurgical patients. Acta Med Okayama. 2011;65:205–10. doi: 10.18926/AMO/46633. [DOI] [PubMed] [Google Scholar]
- 12.Eken C, Kartal M, Bacanli A, Eray O. Compartion of the full outline of unresponsivness score coma scale and the Glascow coma scale in an emergency setting papulation. Emerg Med. 2009;16:29–36. doi: 10.1097/MEJ.0b013e32830346ab. [DOI] [PubMed] [Google Scholar]
- 13.Ritchie PD, Cameron PA, Ugoni AM, Kaye AH. A study of the functional outcome and mortality in elderly patients with head injuries. J Clin Neurosci. 2000;7:301–4. doi: 10.1054/jocn.1999.0198. [DOI] [PubMed] [Google Scholar]
- 14.Leih-Lai MW, Theodorou AA, Sarnaik AP, Meert KL, Moylan PM, Canady AI. Limitation of the Glascow coma scale in predicting outcome in childeren with traumatic brain injury. Pediatrics. 1992;120:195–9. doi: 10.1016/s0022-3476(05)80426-3. [DOI] [PubMed] [Google Scholar]
- 15.Farid S, Darshan P, Rekha L. The four score predicts outcome in after traumatic brain injury. Neuocrit Care. 2011;15:250–6. [Google Scholar]
- 16.Stead LG, Wijdicks EF, Bhagra A, Kashyap R, Bellolio MF, Nash DL, et al. Validation of a new coma scale, the FOUR score, in the emergency department. Neurocrit Care. 2009;10:50–4. doi: 10.1007/s12028-008-9145-0. [DOI] [PubMed] [Google Scholar]
- 17.Iyer VN, Mandrekar JN, Danielson RD, Zubkov AY, Elmer JL, Wijdicks EF. Validity of the FOUR score coma scale in the medical intensive care unit. Mayo Clin Proc. 2009;84:694–701. doi: 10.4065/84.8.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Izadi avanji F, Fakharian E, Masoodi Alavi N. Outcome of factors related to traumatic brain injuries among the patients hospitalized in intensive care unit? KAUMS Journal (FEYZ) 2010;14(2):112–119. URL http://feyzkaumsacir/browsephpa_code=A-10-1-749&slc_lang=fasid=1 . [Google Scholar]
- 19.Joosse P, Smit G, Arendshorst RJ, Soedarmo S, Ponsen KJ, Goslings JC. Outcome and prognostic factors of traumatic brain injury: A prospective evaluation in a Jakarta University hospital. J Clin Neurosci. 2009;16:925–8. doi: 10.1016/j.jocn.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 20.Gan BK, Lim JH, Ng IH. Outcome of moderate and severe traumatic brain injury amongst the elderly in Singapore. Ann Acad Med Singapore. 2004;33:63–7. [PubMed] [Google Scholar]
- 21.Fugate JE, Rabinstein AA, Claassen DO, White RD, Wijdicks EF. The FOUR score predicts outcome in patients after cardiac arrest. Neurocrit Care. 2010;13:205–10. doi: 10.1007/s12028-010-9407-5. [DOI] [PubMed] [Google Scholar]
- 22.Soleimani MA, Masoudi R, Bahrami N, Qorbani M, Sadeghi T. Predicting mortality rate of patients in critical care unit using APACHE-II index. J Gorgan Uni Med Sci. 2010;11:64–9. [Google Scholar]


