Abstract
Objective
Presentation of the diagnostic and surgical treatment methods of our extrauterine intrauterine device (IUD) cases.
Material and Methods
We retrospectively evaluated the data of 21 extrauterine IUD cases at our clinic between 2008 and 2010. The symptoms, diagnostic methods, and surgical treatments were evaluated.
Results
A total of 14 copper and seven levonorgestrel (LNG) IUDs were used. IUD had been inserted during lactation in 71.4% of the patients. The reasons for presentation of patients were unintended pregnancy in 19.05%, pelvic pain in 19.05%, and pelvic pain with vaginal bleeding in 23.8%. IUD in two patients were located the retroperitoneal area. IUD string had not been visible during routine follow-up in 38.1% of the patients. Laparoscopy was performed in 14 patients and laparotomy was performed for dense adhesions in seven patients.
Conclusion
Extrauterine IUDs can present with various clinical symptoms. Ultrasonography and X-Ray are sufficient for the diagnosis. Surgical removal is needed to prevent possible complications, and the preferred surgical technique in appropriate patients is laparoscopy.
Keywords: Extrauterine IUD, surgery, contraception
Introduction
Intrauterine devices (IUDs) are highly effective reversible contraceptive devices commonly used throughout the world. Globally, they are the second most common contraceptive method (14%) following sterilization (21%) (1). They are also frequently used in Turkey (20.2%). The most common types are the copper-releasing IUD and the Levonorgestrel-releasing IUD (LNG-IUD) systems.
There are various complications with respect to IUD use (0.2–3.6/1000 applications), among which uterine perforation is a serious complication. Most uterine perforations are observed in IUD’s inserted during lactation (2, 3). Other important complications are lower midline abdominal pain, organ perforation, strangulation, infection, and infertility. The adhesions that can gradually develop with intra-abdominal IUD’s are the most important cause of additional morbidity (4). This complication has been reported both with LNG-IUDs (Mirena, Shering Plough, Germany) and copper IUDs (TCu-380A). Prevention and early diagnosis are the most important factors to avoid this complication. Therefore, it is necessary to see the IUD string immediately after insertion or in the first week with vaginal examination and to perform a check with ultrasonography in all patients. Surgical intervention is frequently required in uterine perforation.
We aim to present our clinical experience with the symptoms, diagnostic methods, and surgical treatment of extra-uterine IUDs in this retrospective study.
Material and Methods
We retrospectively evaluated the patient charts of females with an extrauterine IUD and who had undergone laparotomy or laparoscopy at Adıyaman University Faculty of Medicine Training and Research Hospital, Department of Obstetrics and Gynecology between 2008 and 2014.
We first performed a search using the “IUD with no visible string at the cervical os” code (530.583) of the International Classification of Disease and Related Health Problems-10 (ICD-10) codes that have been adapted to Turkish. Following the evaluation of the data, the patients were divided into two groups as intrauterine and extrauterine IUDs. Patients who had an intrauterine IUD where no string was visible and that was removed with a simple vaginal procedure or hysteros-copy were excluded from the study. We found a total of 21 extrauterine IUD cases. Patient data were evaluated through review of the patient charts and the hospital system records. All patients underwent surgery after going through a similar evaluation process. A gynecological examination was performed first and IUD was evaluated with transvaginal ultrasonography when the string could not be seen. Anteroposterior and lateral pelvic X-rays were obtained to support the diagnosis. None of the patients in the study underwent magnetic resonance imaging (MRI) or computed tomography (CT) scans. Patients who received a preliminary diagnosis of extrauterine IUD were prepared for laparoscopic surgery. Laparotomy with a Pfannenstiel incision was performed for patients who could not undergo laparoscopy. All surgical procedures were performed under general anesthesia.
The 21 patients detected within the defined period were evaluated. Age, obstetric history, extrauterine IUD type, time of application, time until diagnosis and surgical intervention, symptoms, and surgical route used were recorded. Informed written consent was obtained from all the women. This retrospective case-series study was exempt from ethical approval by the Adıyaman University Ethics commission. We did not conduct statistical analysis.
Results
Demographic data
The demographic data revealed a mean age of 29.4 years and a mean body mass index (BMI) value of 26.9 kg/m2. Obstetric data revealed a mean gravida value of 3.6. The mean number of births by normal spontaneous vaginal delivery was 2.5, while the mean number of cesarean births was 0.4. An IUD had been used before the current one by 33.3% of the patients. The mean duration for which the previous IUD was used was 40.2 (24–48) months (Table 1).
Table 1.
Demographic characteristics of patients
| Patient | Age (years) | Gravity | Parity | BMI (kg/m2) | Number of CS | Previous IUD use | Time of total IUD use (months) | History of abdominal surgery |
|---|---|---|---|---|---|---|---|---|
| 1 | 23 | 3 | 3 | 26.4 | None | yes | 24 | no |
| 2 | 25 | 3 | 3 | 23.6 | 1 | no | 0 | no |
| 3 | 28 | 4 | 3 | 27.8 | None | yes | 48 | no |
| 4 | 26 | 2 | 2 | 26.4 | None | no | 0 | no |
| 5 | 24 | 1 | 1 | 29.1 | None | no | 0 | yes |
| 6 | 34 | 5 | 5 | 28 | 1 | no | 0 | no |
| 7 | 38 | 7 | 4 | 26.1 | None | no | 0 | no |
| 8 | 36 | 5 | 4 | 26.5 | 3 | no | 0 | no |
| 9 | 34 | 3 | 3 | 25.9 | None | no | 0 | no |
| 10 | 31 | 4 | 4 | 24.9 | 2 | yes | 30 | no |
| 11 | 30 | 2 | 2 | 24.7 | None | yes | 48 | yes |
| 12 | 23 | 2 | 2 | 28.6 | None | no | 0 | no |
| 13 | 27 | 1 | 1 | 27 | None | no | 0 | no |
| 14 | 28 | 2 | 2 | 26.2 | None | no | 0 | no |
| 15 | 35 | 6 | 4 | 29 | None | yes | 48 | no |
| 16 | 30 | 4 | 4 | 26 | None | no | 0 | no |
| 17 | 26 | 3 | 3 | 31 | None | no | 0 | no |
| 18 | 32 | 8 | 6 | 27 | None | yes | 36 | yes |
| 19 | 36 | 5 | 4 | 28 | None | yes | 48 | no |
| 20 | 28 | 5 | 3 | 24 | 1 | no | 0 | no |
| 21 | 32 | 3 | 3 | 25.4 | None | yes | 36 | no |
BMI: Body mass index; IUD: Intrauterine device; CS: Caesarean section
IUD types and important time points regarding insertion
Table 2 presents the extrauterine IUD clinical data and usage characteristics of the patients. All mislocated extrauterine IUD applications had been performed in primary health care centers. Extrauterine IUDs consisted of seven LNG-IUDs and 14 copper IUDs (TCu-380A-IUD). The mean duration between IUD insertion and diagnosis was 8.1 months (3 days-24 months). The mean duration between the last pregnancy and IUD insertion was 14.7 (2–38) months. IUD had been inserted during lactation in 15 (71.4%) patients.
Table 2.
Symptoms, the locations and treatment of IUD, type of IUDs and special time for IUD insertion
| Patients no | Location of the IUD | Type of operation | Time from insertion to diagnosis | Time from pregnancy to insertion | Symptom(s) | Type of IUD |
|---|---|---|---|---|---|---|
| 1 | In the Douglas pouch | Laparoscopy | 7 months | 16 months | None | LNG-IUD |
| 2 | In the Douglas pouch | Laparoscopy | 12 months | 11 months | None | TCu 380 A-IUD |
| 3 | Near the uterine artery | Laparoscopy | 6 months | 8 months | None | TCu 380 A-IUD |
| 4 | Near the ovary | Laparotomy | 3 months | 4 months | Pelvic pain | TCu 380 A-IUD |
| 5 | In the Douglas pouch | Laparoscopy | 18 months | 2 months | None | TCu 380 A-IUD |
| 6 | In the Douglas pouch | Laparoscopy | 24 months | 8 months | None | TCu 380 A-IUD |
| 7 | In the Douglas pouch | Laparoscopy | 12 months | 16 months | Unintended pregnancy | TCu 380 A-IUD |
| 8 | Omentum | Laparotomy | 10 months | 24 months | Unintended pregnancy | LNG-IUD |
| 9 | Omentum | Laparotomy | 6 months | 38 months | Unintended pregnancy | LNG-IUD |
| 10 | Omentum | Laparotomy | 4 days | 36 months | Pain and bleeding | LNG-IUD |
| 11 | In the Douglas pouch | Laparoscopy | 7 days | 24 months | Pain and bleeding | LNG-IUD |
| 12 | In the Douglas pouch | Laparoscopy | 3 days | 10 months | Pelvic pain | TCu 380 A-IUD |
| 13 | In the Douglas pouch | Laparoscopy | 5 days | 8 months | Pain and bleeding | TCu 380 A-IUD |
| 14 | Retroperitoneum | Laparotomy | 6 days | 6 months | Pain and bleeding | TCu 380 A-IUD |
| 15 | In the Douglas pouch | Laparoscopy | 3 days | 22 months | Pelvic pain | LNG-IUD |
| 16 | Retroperitoneum | Laparotomy | 24 months | 18 months | Unintended pregnancy | TCu 380 A-IUD |
| 17 | Neary the ovary | Laparoscopy | 7 months | 12 months | None | TCu 380 A-IUD |
| 18 | In the Douglas pouch | Laparoscopy | 13 months | 2 months | None | TCu 380 A-IUD |
| 19 | Omentum | Laparotomy | 8 months | 36 months | None | LNG-IUD |
| 20 | Near the ovary | Laparoscopy | 6 months | 6 months | Pelvic pain | TCu 380 A-IUD |
| 21 | In the Douglas pouch | Laparoscopy | 18 months | 2 months | Pain and bleeding | TCu 380 A-IUD |
LNG-IUD: Levonorgestrel intrauterine device; TCu 380 A-IUD: Copper- Intrauterine device; IUD: Intrauterine device
Symptoms and IUD localization
Symptoms at presentation were delayed menstruation in the four patients with an unintended pregnancy, pelvic pain in four, and pelvic pain with vaginal bleeding in five. In addition, the IUD strings of eight patients had not been visible during routine follow-up. Two of the patients with delayed menstruation had undergone pregnancy termination at private centers, while two patients continued the pregnancy with an extrauterine IUD and had a normal spontaneous vaginal delivery. IUD was in the Douglas pouch and retroperitoneum in the patients who gave birth. IUD was surgically removed in the postpartum period in both patients. The retroperitoneal IUD was close to the right iliac artery bifurcation during the surgery. The surgery started as laparoscopy but was converted to laparotomy because of the IUD location and the dense adhesions.
The most common extrauterine IUD location was the Douglas pouch with 11 (52.3%) patients (Figure 1, 2). The rare location of the retroperitoneum was seen in two of our patients (Figure 3). Laparoscopic IUD removal was performed in a total of 14 (66.6%) patients. The most common reason to perform laparotomy was severe adhesions.
Figure 1.
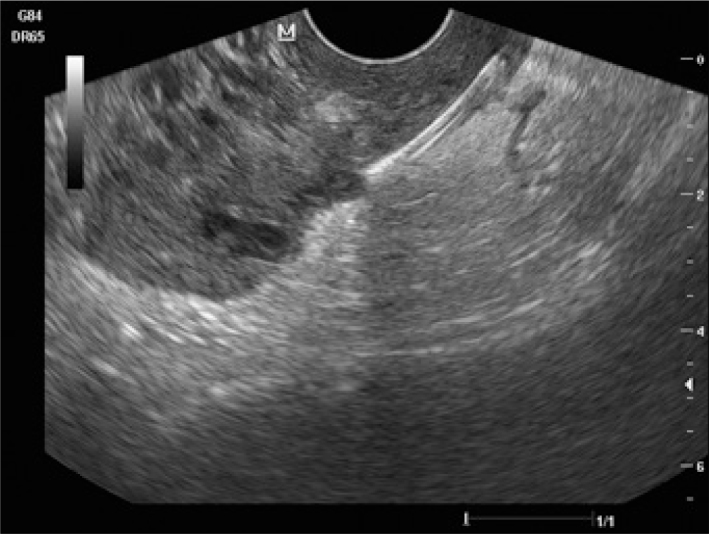
Ultrasonographic appearance of T-shaped IUD in Douglas pouch
Figure 2.

Anteroposterior abdominal X-ray demonstrating location of IUD (Coronal)
Figure 3.

Intraoperative image of IUD (Laparotomy). The IUD string is intraperitoneal but the location of the IUD body is the retroperitoneal area
Table 2 presents the treatment method, IUD type, and localization. Sixteen patients were prepared for laparoscopy under general anesthesia. The surgery was converted to laparotomy because of dense adhesions in two patients. Laparotomy had been performed in five patients because of technical equipment failure. General surgery consultation was required for dense adhesions and abscess formation in two of the patients whose surgeries were converted to laparotomy. The patient with an abscess underwent abscess drainage, and there was no additional complication during follow-up. Both patients had a TCu-380A-IUD. There was no intraoperative complication.
Discussion
IUD use is a modern contraceptive use that is commonly employed throughout the world. The low cost, long duration of effectiveness, high efficacy, reversibility, lack of systemic side effects, and coitus-independent effectiveness have led to its widespread use. However, complications such as vaginal bleeding, abdominal pain, infection, uterus perforation, and migration to adjacent organs have been reported. Complications such as uterine perforation are rare but very well defined. Some risk factors for perforation with IUD use have been reported. The postpartum period, lactation period, uterus with undiagnosed pregnancy, congenital uterine abnormality, and excessive anteflexion or retroflexion are important risk factors. The most common association is uterus perforation with an IUD inserted during the lactation period where the risk increases 10-fold (5). Uterine perforation can cause vaginal bleeding and lower abdominal pain following insertion, but several cases have no symptoms for an extended period.
Several studies have reported a period of <1 year between IUD insertion and uterine perforation diagnosis; at least 80% of these patients have been found to be in the lactation period at the time of insertion (3, 6). Similarly, 71.4% of our patients had been in the lactation period during IUD insertion. However, the diagnosis can be delayed by months or even years with an intra-peritoneal IUD. The main step in the diagnosis is suspecting an extrauterine IUD in patients where the IUD string is not seen at the cervical os during routine follow-ups or normal outpatient visits. Transvaginal ultrasonography is the best method for localization in case of suspicion. The location may be the Douglas pouch, inside the broad ligament, attached to the omentum, or the retroperitoneal area. Lateral and anteroposterior pelvic X-rays can also be obtained to support the diagnosis and for additional information on the location.
For the treatment of extrauterine IUDs, the World Health Organization recommends prompt surgical removal after diagnosis, independent of the localization and symptoms (7). Prompt decision with regard to surgery is important because adhesion formation becomes more marked and removal becomes more difficult with extrauterine IUDs as time passes. However, there are contrasting views with regard to asymptomatic patients (8). The most important complications of intra-abdominal IUDs are adhesions, intestinal obstruction, chronic pelvic pain, abscess development, and infertility (9, 10). Therefore, it is particularly important to remove IUDs in symptomatic patients. The preferred surgical route is laparoscopy because it is minimally invasive and can be used with a high success rate (11). Laparotomy should only be used in patients with significant adhesion or adjacent organ invasion.
IUDs are inserted by midwives and medical practitioners following a certification program in our country. Therefore, early follow-ups can be a problem. The lack of suspicion about perforation in the early stage can delay referrals to a gynecology specialist, and therefore the diagnosis. However, LNG-IUDs are generally inserted by obstetrics and gynecology specialists in our country. We found an extrauterine LNG-IUD in seven patients. This result indicates that the uterine perforation risk should be considered even when the insertion has been performed by a specialist.
Operator factors were not addressed in our study, and this is one of the limitations of our research. We did not have access to information regarding who performed IUD procedures; therefore, we could not address operator skill as a factor for uterine perforation and malposition of IUD.
The migration of IUD to adjacent structures following perforation has been reported with extrauterine IUDs in the literature. Bladder and iliac vein migration is particularly noteworthy (12). Therefore, migration should be considered if IUD cannot be found (13–16). Retroperitoneal IUD migration is rare but important because of the adjacent vascular structures. Consultation of the relevant specialty may be intraoperatively acquired in such cases; we requested general surgery consultation because of diffuse intestinal adhesions for two cases and abscess formation at the sigmoid colon level for one case. Abscess drainage from the abdomen was performed for our patient with abscess formation. Most of the patients were diagnosed with an extra-uterine IUD when the IUD string was not seen during routine follow-up and the patient was evaluated by ultrasonography and X-ray (17).
In conclusion, uterine perforation can present with symptoms such as lower abdominal pain and abnormal vaginal bleeding, with the IUD string not being seen during routine follow-up, or an unintended pregnancy. The combination of transvaginal ultrasound and anteroposterior/lateral X-ray is usually adequate for the diagnosis. It may be best for a specialist to perform the insertion in cases at risk such as those with a known uterine anomaly or excessive uterine anteflexion or retroflexion or patients in the lactation period. The early diagnosis of complications, such as uterine perforation, also requires the follow-up of the IUD location with postprocedure ultrasonography in several cases. In light of the data, we believe that all extrauterine IUD’s should be surgically removed (preferably by laparoscopy) to prevent complications at later stages.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Adıyaman University Faculty of Medicine Ethical Committee.
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - M.K., M.B., T.Y.; Design - M.K., M.B., T.Y.; Supervision - M.K., M.B., T.Y., MA; Resource - M.K., M.B., T.Y.; Materials - M.K., M.B., T.Y.; Data Collection & /or Processing - M.K., M.B., T.Y., D.K.; Analysis & /or Interpretation - M.K., M.B., T.Y., D.K.; Literature Search - M.K., D.K., T.Y.; Writing - M.K., T.Y.; Critical Reviews - M.K., M.B., T.Y., D.K., M.A.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.World Population Bureau. Family Planning Worldwide, 2008 Data Sheet. [29 January 2013, date last accessed]. Available from: http://www.prb.org/pdf08/fpds08.pdf.
- 2.Chi I, Feldblum PJ, Rogers SM. IUD-related uterine perforation: an epidemiologic analysis of a rare event using an international data-set. Contracept Deliv Syst. 1984;5:123–30. [PubMed] [Google Scholar]
- 3.Caliskan E, Ozturk N, Dilbaz BO, Dilbaz S. Analysis of risk factors associated with uterine perforation by intrauterine devices. Eur J Contracept Reprod Health Care. 2003;8:150–5. http://dx.doi.org/10.1080/ejc.8.3.150.155. [PubMed] [Google Scholar]
- 4.Adoni A, Ben Chetrit A. The management of intrauterine devices following uterine perforation. Contraception. 1991;43:77–81. doi: 10.1016/0010-7824(91)90128-3. http://dx.doi.org/10.1016/0010-7824(91)90128-3. [DOI] [PubMed] [Google Scholar]
- 5.Heartwell SP, Schlesselman S. Risk of uterine perforation among users of intrauterine devices. Obstet Gynecol. 1983;61:31–6. [PubMed] [Google Scholar]
- 6.Andersson K, Ryde-Blomqvist E, Lindell K, Odlind V, Milsom I. Perforations with intrauterine devices. Report from a Swedish survey. Contraception. 1998;57:251–5. doi: 10.1016/s0010-7824(98)00029-8. http://dx.doi.org/10.1016/S0010-7824(98)00029-8. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. Sexual and reproductive health. Available from: http://www.who.int/reproductivehealth/publications/maternal_perinatal_health/en/index.html.
- 8.Markovitch O, Klein Z, Gidoni Y, Holzinger M, Beyth Y. Extrauterine mislocated IUD: is surgical removal mandatory? Contraception. 2002;66:105–8. doi: 10.1016/s0010-7824(02)00327-x. http://dx.doi.org/10.1016/S0010-7824(02)00327-X. [DOI] [PubMed] [Google Scholar]
- 9.Rao RP. Lost intrauterine devices and their localization. J Reprod Med. 1978;20:195–9. [PubMed] [Google Scholar]
- 10.Ohana E, Sheiner E, Leron E, Mazor M. Appendix perforation by an ıntrauterine contraceptive device. Eur J Obstet Gynecol Reprod Biol. 2000;88:129–31. doi: 10.1016/s0301-2115(99)00142-6. http://dx.doi.org/10.1016/S0301-2115(99)00142-6. [DOI] [PubMed] [Google Scholar]
- 11.Demir SC, Cetin MT, Ucunsak IF, Atay Y, Toksoz L, Kadayifici O. Removal of intra-abdominal intrauterine device by laparoscopy. Eur J Contracept Reprod Health Care. 2002;1:20–3. http://dx.doi.org/10.1080/713604287. [PubMed] [Google Scholar]
- 12.Roy KK, Banerjee N, Sinha A. Laparoscopic removal of translocated retroperitoneal IUD. Int J Gynaecol Obstet. 2000;71:241–3. doi: 10.1016/s0020-7292(00)00213-7. http://dx.doi.org/10.1016/S0020-7292(00)00213-7. [DOI] [PubMed] [Google Scholar]
- 13.Farouk K, Afridi Z, Farooq M, Qureshi I. Urological complications of ntrauterine contraceptive device. Journal of Postgraduate Medical Institute. 2007;21:260–5. [Google Scholar]
- 14.Yalcin V, Demirkesen O, Alici B, Onol B, Solok V. An unusual presentation of a foreign body in the urinary bladder: a migrant intrauterine device. Urol Int. 1998;61:240–2. doi: 10.1159/000030338. http://dx.doi.org/10.1159/000030338. [DOI] [PubMed] [Google Scholar]
- 15.Demirci D, Ekmekcioglu O, Demirtas A, Gulmez I. Big bladder stones around an intravesical migrated intrauterine device. Int Urol Nephrol. 2003;35:495–6. doi: 10.1023/b:urol.0000025624.15799.8d. http://dx.doi.org/10.1023/B:UROL.0000025624.15799.8d. [DOI] [PubMed] [Google Scholar]
- 16.Kassab B, Audra P. The migrating intrauterine device. Case report and review of the literature. Contracept Fertil Sex. 1999;27:696–700. [PubMed] [Google Scholar]
- 17.Ozgun MT, Batukan C, Serin IS, Ozcelik B, Basbug M, Dolanbay M. Surgical management of intra-abdominal mislocated intrauterine devices. Contraception. 2007;75:96–100. doi: 10.1016/j.contraception.2006.09.011. http://dx.doi.org/10.1016/j.contraception.2006.09.011. [DOI] [PubMed] [Google Scholar]


