Abstract
Background
Chinese herbal products (CHPs) have been frequently used among patients with chronic diseases including hypertension; however, the co-prescription pattern of herbal formulae and single herbs remain uncharacterized. Thus, this large-scale pharmacoepidemiological study evaluated the frequency and co-prescription pattern of CHPs for treating hypertension in Taiwan from 2003 to 2009.
Methods
The database of traditional Chinese medicine (TCM) outpatient claims was obtained from the National Health Insurance in Taiwan. Patients with hypertension during study period were defined according to diagnostic codes in the International Classification of Disease Ninth Revision, Clinical Modification. The frequencies and percentages of herbal formula and single herb prescriptions for hypertension were analyzed. We also applied association rules to evaluate the CHPs co-prescription patterns.
Results
The hypertension cohort included 154,083 patients, 123,240 patients of which (approximately 80 %) had used TCM at least once. In total, 81,582 visits involving CHP prescriptions were hypertension related; Tian-Ma-Gou-Teng-Yin and Dan Shen (Radix Salvia Miltiorrhizae) were the most frequently prescribed herbal formula and single herb, respectively, for treating hypertension.
Conclusions
This study elucidated the utilization pattern of CHPs for treating hypertension. Future studies on the efficacy and safety of these CHPs and on drug–herb interactions are warranted.
Keywords: Complementary and alternative medicine, Traditional Chinese products, Hypertension, National Health Insurance Research Database, Traditional Chinese medicine
Background
Hypertension, a major medical and public health concern affecting approximately 972 million adults worldwide, is the main risk factor for cardiovascular, brain, and kidney diseases [1]. In addition, hypertension is consistently accompanied by other metabolic diseases, such as diabetes mellitus and lipid abnormalities, the incidence of which has increased recently [2, 3]. Moreover, hypertension causes a loss of 92 million disability adjusted life years and is responsible for 7.6 million excess deaths yearly [4]. Thus, antihypertensive drugs are primarily used to control blood pressure, thereby preventing the occurrence or progression of cardiovascular diseases and other complications. Despite the prevalence of hypertension and its associated complications, the control of this disease is inadequate. Although several antihypertensive drugs, such as diuretics, beta-blockers, calcium-channel blockers, and angiotensin-converting enzyme or angiotensin II receptor blockers, are available currently, a systolic/diastolic blood pressure level of <140/90 mmHg, defined in the Seventh Report of the Joint National Committee (JNC7) in 2003 and reaffirmed in the JNC8 in 2013, was achieved in no more than 25 % of patients undergoing treatment for hypertension worldwide [5]. Furthermore, the clinical applications of antihypertensive drugs are limited by numerous adverse side effects, such as dizziness, headache, orthostatic hypotension, and decreased sexual function [6]. Notably, complementary and alternative therapies have become increasingly popular for treating hypertension [7], particularly traditional Chinese medicine (TCM) [8], because of their potential efficacy and few side effects [9, 10]. In addition to numerous published cases and randomized trials, an increasing number of experimental studies have revealed multiple antihypertensive and protective mechanisms of TCM [10]. In addition, various meta-analyses and systemic reviews have recently evaluated the effectiveness of TCM for hypertension [11].
TCM, including acupuncture, traumatology manipulative therapies, and decoction, plays a crucial role in health care in Taiwan and other Asian or Western countries. Chinese herbal products (CHPs), a modern form of decoctions in which herbal formulae and single herbs are concentrated into granulated compounds, are widely prescribed by TCM physicians because of their convenience and quality. According to TCM theory, TCM physicians evaluate patient conditions to prescribe one or more herbal formulae combined with several single herbs for each prescription. However, the CHPs used for treating hypertension and their co-prescription patterns remain not fully elucidated.
The National Health Insurance (NHI) program has been reimbursing claims for CHPs, including single herbs or herbal formulae, in Taiwan since 1995. By using the National Health Insurance Research Database (NHIRD), we analyzed the CHPs prescribed for treating hypertension and their co-prescription patterns in Taiwan. The results are a reference from which clinical practitioners can understand the medicinal demands and preferences of TCM users with hypertension and thereby provide reliable information about CHP use.
Methods
Data source
The NHI program of Taiwan, executed in 1995, reimburses both Western medicines and CHPs. Approximately 99 % of Taiwan residents were included into the program by the end of 2010 [12]. The electronic database of all claims obtained from the NHIRD website involved medical record files containing patient sex and date of birth, date of medical visits, medical care facilities and specialties, drugs, management and treatment, transferred identification number, and three major diagnoses coded according to the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) format. The data regarding patient identity and institutions are cryptographically scrambled to protect personal privacy. Thus, the NHIRD offers an optimal platform for understanding the utilization pattern of CHPs prescribed by licensed TCM physicians among the hypertension patient population in Taiwan.
We analyzed a sample of one million randomly selected patients from among the 22 million beneficiaries of the NHI program in Taiwan, determining the prevalence of prescribed CHPs in patients with hypertension from 2003 to 2009. This study adhered to strict confidentiality guidelines according to regulations for personal electronic data protection and was approved by the Ethics Review Board of Chang Gung Memorial Hospital, Chia-Yi Branch (103-7691B).
Study subjects
The study cohort comprised patients diagnosed with hypertension (ICD-9-CM codes: 401–405) three or more times within one year from 2003 to 2009; information was obtained from Western and TCM outpatient visit records. All hypertension-related medical records were analyzed during the study period. In the hypertension cohort, patients who had at least one TCM outpatient clinical visit from 2003 to 2009 were defined as TCM users; among the TCM users, those who had used CHPs were defined as CHP users, whereas those with no TCM outpatient records were defined as non-TCM users. In addition, we obtained the prescription files containing the CHP prescription records corresponding to patient outpatient visits that involved a hypertension diagnosis to assess the corresponding CHP co-prescriptions for hypertension.
Study variables
Patient demographic characteristics were investigated to determine the main independent variables affecting TCM use in the hypertension cohort. In addition to patient sex, patient age was categorized into three groups: <45, 45–65, >65 years. The monthly insurance salaries of patients were grouped into four levels: NT$0, NT$1–NT$15,840, NT$15,841–NT$25,000, >NT$25,000. Urban levels in this study were divided into four strata according to the location of NHI registration. Level 1 referred to the most urbanization and level 4 indicated the least urbanization. We also included the following clinical, potential comorbidities related to hypertension from the NHIRD as independent variables: ischemic heart disease (ICD-9-CM codes: 410–414), cardiovascular disease (ICD-9-CM codes: 430–438), atherosclerosis (ICD-9-CM code: 440), hyperlipidemia (ICD-9-CM code: 272), and type II diabetes mellitus (ICD-9-CM code: 250).
Traditional Chinese medicine
TCM, comprising CHPs, acupuncture, and traumatology manipulative therapies, has developed over the past millennia and is most widely adopted by patients in Taiwan. Prescriptions by TCM physicians based on the patients’ varying signs and symptoms may comprise one or more herbs (formulae). Chinese herbal drugs or formulae are manufactured as powder or fine granules that can be easily mixed in a single prescription. Information regarding reimbursed CHPs, including the name of each CHP, the proportion of each constituent, the date and period of drug approval, the code, and the manufacturer name, were obtained from the Department of Chinese Medicine and Pharmacy website.
Statistical analysis
Drug registration numbers from the Department of Chinese Medicine and Pharmacy website were linked to the outpatients visit records of the hypertension cohort. Database software, SAS Version 9.2 (SAS Institute Inc., Cary, NC, USA), was used for data linkage and descriptive statistic analysis of drug utilization pattern, including frequencies, percentages, average daily dose(g), and average use duration(days) of herbal formulae or single herbs for treating hypertension. In general, TCM physicians prescribe one or more herbal formulae including several single herbs to treat patients. In this study, the association rules of data mining were applied to assess the co-prescriptions of CHPs for hypertension. The support factor was the proportion of the co-prescriptions of medications A and B among all prescriptions, and the confidence factor was the proportion of the co-prescriptions of medications A and B among all prescriptions containing medication A (Fig. 1). We used 0.5 % as the minimum support factor and 30 % as the minimum confidence factor [13].
Fig. 1.
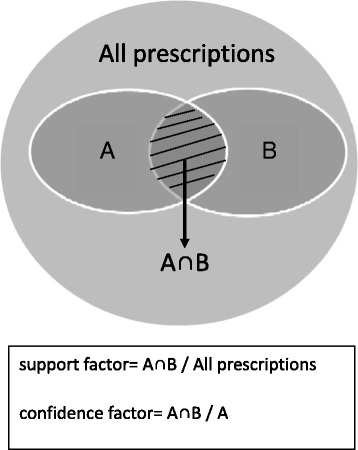
Basic Concepts and Algorithms of Association rules
Results
In this study, we identified 154,083 patients who had visited the outpatient department for hypertension three or more times within one year during the study period among the study cohort of one million randomly sampled patients. Table 1 shows a summary of the patient characteristics. Of these patients, 123,240 patients (approximately 80 %) used TCM at least once, and 116,070 patients used CHPs. Female patients used TCM more frequently than did male patients. The peak age of the patients receiving TCM treatment ranged between 45 to 65 years (47.4 %). In addition, patients with comorbidities such as metabolic diseases, including diabetes mellitus or hyperlipidemia, were more likely to consider TCM treatment.
Table 1.
Characteristics of Hypertension population from one million random sampling cohort of the NHIR database
| Characteristics | Non-TCM Users | TCM users | CHP users | |||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| Age | ||||||
| <45 | 3802 | 12.3 | 18768 | 15.2 | 17653 | 15.2 |
| 45-65 | 12790 | 41.5 | 58453 | 47.4 | 55219 | 47.6 |
| >65 | 14251 | 46.2 | 46019 | 37.3 | 43198 | 37.2 |
| Gender | ||||||
| Female | 11509 | 37.3 | 64826 | 52.6 | 61594 | 53.1 |
| Male | 19334 | 62.7 | 58414 | 47.4 | 54476 | 46.9 |
| Insurance salaries(NTD$/month) 1 | ||||||
| 0 | 5965 | 19.3 | 21891 | 17.8 | 20485 | 17.7 |
| 1-15840 | 5653 | 18.3 | 18185 | 14.8 | 16980 | 14.6 |
| 15841-25000 | 12882 | 41.8 | 57967 | 47.0 | 55006 | 47.4 |
| >25000 | 6343 | 20.6 | 25197 | 20.4 | 23599 | 20.3 |
| Urban Level 2 | ||||||
| 1 | 9069 | 29.4 | 35622 | 28.9 | 33226 | 28.6 |
| 2 | 13023 | 42.2 | 55239 | 44.8 | 52063 | 44.9 |
| 3 | 5538 | 18.0 | 20546 | 16.7 | 19486 | 16.8 |
| 4 | 3213 | 10.4 | 11833 | 9.6 | 11295 | 9.7 |
| Comorbidity with hypertension(ICD-9-CM) | ||||||
| Ischemic Heart Disease (410–414) | 9607 | 31.1 | 41603 | 33.8 | 39237 | 33.8 |
| Cardiovascular disease (430–438) | 7466 | 24.2 | 27218 | 22.1 | 25592 | 22.1 |
| Atherosclerosis(440) | 931 | 3.0 | 3814 | 3.1 | 3616 | 3.1 |
| Hyperlipidemia (272) | 11476 | 37.2 | 52627 | 42.7 | 49629 | 42.8 |
| Type II Diabetes Mellitus(250) | 9773 | 31.7 | 39936 | 32.4 | 37514 | 32.3 |
| Total | 30843 | 123240 | 116070 | |||
1. NTD, New Taiwan dollar 1USD≒30NTD
2. 1:most urbanization; 4:least urbanization
Table 2 presents the estimated prevalence of hypertension (15.4 %) in Taiwan from 2003 to 2009, indicating that the prevalence increased with an increase in age for both sexes. The prevalence of hypertension was 2.5 %, 32.7 %, and 67.6 % in women and 4.1 %, 32.6 %, and 60.8 % in men aged <45, 45–65, and > 65 years, respectively.
Table 2.
Patient number and estimated prevalence of hypertension in Taiwan from one million random sampling cohort of the NHIR database 2003-2009
| Age/gender | All | Female | Male | |||
|---|---|---|---|---|---|---|
| All | 154083 | 15.4 % | 76335 | 15.1 % | 77748 | 15.7 % |
| <45 | 22570 | 3.3 % | 8561 | 2.5 % | 14009 | 4.1 % |
| 45-65 | 71243 | 32.6 % | 36066 | 32.7 % | 35177 | 32.6 % |
| >65 | 60270 | 64.2 % | 31708 | 67.6 % | 28562 | 60.8 % |
Between 2003 and 2009 in Taiwan, 81,582 hypertension-related outpatient visits involved CHP prescriptions by TCM physicians. Table 3 presents the most frequently prescribed herbal formulae and single herbs during these outpatient visits and includes data on the frequency of prescriptions, average daily doses, and average prescription durations. The most commonly prescribed herbal formula for hypertension was Tian-Ma-Gou-Teng-Yin (27.5 %), followed by Gou-Teng-San (12.5 %), Xue-Fu-Zhu-Yu-Tang (9.2 %), Jia-Wei-Xiao-Yao-San (7.8 %), and Zhi-Bo-Di-Huang-Wan (6.1 %). Moreover, Dan Shen (Radix Salvia Miltiorrhizae) (17.1 %) was the most commonly prescribed single herb for patients with hypertension, followed by Gou Teng (Ramulus Uncariae cum Uncis) (10.4 %), Ge Gen (Radix Puerariae) (8.4 %), and Niu Xi (Radix Achyranthis Bidentatae) (6.4 %).
Table 3.
Top ten herbal formulae and single herb prescribed by traditional Chinese medicine doctors for Hypertension (n = 81,582)
| Frequency of prescription n (%) | Average daily dose (g) | Average duration for prescription (days) | ||
|---|---|---|---|---|
| Herbal formulae | ||||
| Tian-Ma-Gou-Teng-Yin | 22,403 | 27.5 % | 9.7 | 10.4 |
| Gou-Teng-San | 10,211 | 12.5 % | 7.6 | 9.2 |
| Xue-Fu- Zhu-Yu-Tang | 7,540 | 9.2 % | 7.7 | 10.7 |
| Jia-Wei-Xiao-Yao-San | 6,342 | 7.8 % | 7.1 | 11.4 |
| Zhi-Bo-Di-Huang-Wan | 4,999 | 6.1 % | 6.4 | 11.6 |
| Qi-Ju-Di-Huang-Wan | 4,828 | 5.9 % | 4.9 | 12.7 |
| Long-Dan-Xie-Gan-Tang | 4,589 | 5.6 % | 8.4 | 10.2 |
| Liu-Wei-Di-Huang-Wan | 4,058 | 5.0 % | 6.8 | 11.0 |
| Zhi-Gan-Cao-Tang | 3,834 | 4.7 % | 8.0 | 11.5 |
| Shu-Jing-Huo-Xue-Tang | 3,661 | 4.5 % | 5.2 | 11.8 |
| Single Herb | ||||
| Dan Shen (Radix Salvia Miltiorrhizae) | 13,970 | 17.1 % | 2.3 | 11.3 |
| Gou Teng (Ramulus Uncariae cum Uncis) | 8,492 | 10.4 % | 2.0 | 10.4 |
| Ge Gen (Radix Puerariae) | 6,846 | 8.4 % | 1.9 | 10.4 |
| Niu Xi (Radix Achyranthis Bidentatae) | 5,230 | 6.4 % | 2.3 | 11.9 |
| Xia Ku Cao (Spica Prunellae Vulgaris) | 4,964 | 6.1 % | 2.2 | 10.8 |
| Da Huang (Radix et Rhizoma Rhei) | 4,964 | 6.1 % | 1.0 | 10.8 |
| Du Zhong (Cortex Eucommiae) | 4,576 | 5.6 % | 1.7 | 11.9 |
| Tian Ma (Rhizoma Gastrodiae Elatae) | 4,284 | 5.3 % | 1.7 | 10.9 |
| Chuan Qi (Radix Notoginseng) | 4,189 | 5.1 % | 3.0 | 10.5 |
| Shan Zha (Crataegi Fructus) | 4,173 | 5.1 % | 1.8 | 10.8 |
According to the association rules in Table 4, the most commonly prescribed combination of two herbal formulae for hypertension was Tian-Ma-Gou-Teng-Yin and Xue-Fu-Zhu-Yu-Tang (support factor, 2.64 %). The most commonly prescribed combination of a herbal formula and a single herb for treating hypertension was Tian-Ma-Gou-Teng-Yin and Dan Shen (support factor, 5.11 %). In addition, TCM physicians frequently prescribed Tian-Ma-Gou-Teng-Yin in combination with other herbal formulae, such as Xue-Fu-Zhu-Yu-Tang, Zhi-Bo-Di-Huang-Wan, Qi-Ju-Di-Huang-Wan, and Long-Dan-Xie-Gan-Tang, or with another single herb, such as Dan Shen, Ge Gen, and Xia Ku Cao (Spica Prunellae Vulgaris). The most commonly prescribed combination of two single herbs was Tian Ma (Rhizoma Gastrodiae Elatae) and Gou Teng (support factor, 2.28 %). Moreover, physicians frequently prescribed Dan Shen in combination with other single herbs, such as Ge Gen, Chuan Qi (Radix Notoginseng), Gou Teng, and Shan Zha (Crataegi Fructus) for treating hypertension.
Table 4.
Co-prescriptions (one to one association) of single herbs and herbal formulae for Hypertension population
| Herbal associations | Support (%) | Confidence (%) | Transaction count | Association rule |
|---|---|---|---|---|
| Single herb to single herb | 2.28 | 43.46 | 1862 | Tian Ma (Rhizoma Gastrodiae Elatae) → Gou Teng (Ramulus Uncariae cum Uncis) |
| 2.19 | 26.09 | 1785 | Ge Gen (Radix Puerariae) → Dan Shen (Radix Salvia Miltiorrhizae) | |
| 2.16 | 42.15 | 1764 | Chuan Qi (Radix Notoginseng) → Dan Shen (Radix Salvia Miltiorrhizae) | |
| 2.14 | 20.56 | 1745 | Gou Teng (Ramulus Uncariae cum Uncis) → Dan Shen (Radix Salvia Miltiorrhizae) | |
| 1.69 | 33.09 | 1380 | Shan Zha (Crataegi Fructus) → Dan Shen (Radix Salvia Miltiorrhizae) | |
| Herbal formula to herbal formula | 2.64 | 28.55 | 2151 | Xue-Fu- Zhu-Yu-Tang → Tian-Ma-Gou-Teng-Yin |
| 1.89 | 30.77 | 1538 | Zhi-Bo-Di-Huang-Wan → Tian-Ma-Gou-Teng-Yin | |
| 1.82 | 30.91 | 1486 | Qi-Ju-Di-Huang-Wan → Tian-Ma-Gou-Teng-Yin | |
| 1.60 | 28.49 | 1307 | Long-Dan-Xie-Gan-Tang → Tian-Ma-Gou-Teng-Yin | |
| Herbal formula to single herb | 5.11 | 18.61 | 4166 | Tian-Ma-Gou-Teng-Yin → Dan Shen (Radix Salvia Miltiorrhizae) |
| 2.66 | 9.68 | 2168 | Tian-Ma-Gou-Teng-Yin → Ge Gen (Radix Puerariae) | |
| 2.47 | 9.00 | 2014 | Tian-Ma-Gou-Teng-Yin → Xia Ku Cao (Spica Prunellae Vulgaris) | |
| 2.02 | 21.83 | 1645 | Xue-Fu- Zhu-Yu-Tang → Dan Shen (Radix Salvia Miltiorrhizae) | |
| 1.64 | 5.99 | 1340 | Tian-Ma-Gou-Teng-Yin → Du Zhong (Cortex Eucommiae) |
Discussion
To the best of our knowledge, this is the first large, random national-level study to document the frequency and co-prescription pattern of CHPs, including herbal formulae and single herbs, for hypertension. The results were obtained by analyzing the computerized insurance reimbursements in Taiwan. The term “hypertension” did not exist in ancient China; thus, TCM has been used to treat hypertension-related symptoms in clinical practice rather than to decrease blood pressure values. In other words, TCM physicians treat patients according to a holistic consideration of the body’s condition. The most common clinical manifestations of hypertension include dizziness, headache, fatigue, shortness of breath, lassitude in the loins and knees, memory loss, dry eyes, and palpitations [14]. TCM physicians prescribe various Chinese herbal formulae or single herbs to treat such patients by differentiating the syndromes according to the signs and symptoms caused by hypertension and TCM principles.
Because of the unsatisfactory efficacy and potential side effects of antihypertensive drugs, including dizziness, headache, orthostatic hypotension, and decreased sexual function after long term use [6],the use of TCM as an alternative therapeutic option for hypertension has been increasing in Taiwan. Although several studies on CHPs have reported their effectiveness in treating hypertension [7, 8, 15], additional studies are warranted to further investigate the safety and efficacy of CHPs and their drug interactions.
Tian-Ma-Gou-Teng-Yin, the most commonly prescribed herbal formula for hypertension in Taiwan, as reported by a previous study [16], has been demonstrated to lower blood pressure and total cholesterol, prevent the incidence of stroke in patients with hypertension, and improve clinical symptoms and quality of life [17, 18]. Several clinical studies and animal experiments have revealed that Tian-Ma-Gou-Teng-Yin decreases endothelin, angiotensin II [19], superoxide dismutase [20],and calcium gene-related peptides [21], regulates the secretions and serum concentrations of vasoactive substances [22], and enhances insulin resistance [23]. However, a review article reported that no randomized, controlled clinical trials have compared the effects of Tian-Ma-Gou-Teng-Yin with those of a placebo or no treatment. Thus, further research is warranted to establish the efficacy of Tian-Ma-Gou-Teng-Yin [24].
Gou-Teng-San is the second most commonly prescribed herbal formula for hypertension. Gou-Teng-San is often prescribed for headache and vertigo and has recently been prescribed for treating hypertension and dementia [25]. Reportedly, the antihypertensive effect of Gou-Teng-San is mediated by calcium channel antagonist action, which was demonstrated clearly in the pharmacological analysis of hirsutine, an indole alkaloid isolated from Gou Teng [26]. The other possible mechanism for the antihypertensive effect of Gou-Teng-San is the radical scavenging activity of Gou Teng, a main component herb of Gou-Teng-San, in the isolated aorta with the endothelium, reported in an experimental animal model [27].
Xue-Fu-Zhu-Yu-Tang, the third most commonly prescribed herbal formula for hypertension, is commonly prescribed for cardiovascular diseases by TCM physicians in clinical practice. Patients with hypertension typically exhibit enhanced platelet adhesion, aggregation, releasing reaction, and dysfunction in erythrocyte deformability; hence, improving erythrocyte deformability and inhibiting platelet activation might be helpful in treating patients with hypertension. The use of CHPs might improve blood rheological conditions, including coagulation, viscosity, blood flow, and deformability [10]. Certain experimental studies have demonstrated that Xue-Fu-Zhu-Yu-Tang can increase coronary blood flow, improve cardiac microcirculation, prevent platelet aggregation, and accommodate blood lipids [28, 29].
Although Jia-Wei-Xiao-Yao-San is rarely prescribed alone by TCM physicians for treating hypertension, this study revealed that it was the fourth most commonly prescribed herbal formula for hypertension. TCM physicians combined it with another herbal formula and/or single herb according to patient symptoms [30]. Moreover, previous studies have reported that Jia-Wei-Xiao-Yao-San is the most commonly used CHP for relieving menopausal symptoms, such as hot flushes, and other related symptoms, including emotional disturbances and insomnia [31, 32]. Patients with such symptoms might be at a higher risk of developing hypertension, and this may explain the frequent prescription of Jia-Wei-Xiao-Yao-San for hypertension.
As observed in Table 3, Dan Shen, the dried root and the rhizome of Salviamiltiorrhiza Bge (Labiatae), is the most frequently prescribed single herb for hypertension. Studies have reported the multiple pharmacological activities of Dan Shen in the cardiovascular system, including anti-hypertension [33], anti-thrombosis [34], anti-atherosclerosis [35],and cardioprotection [36], in addition to improved microcirculation in the brain and heart [37]. Previous studies have demonstrated that the active chemical constituents of Dan Shen, particularly, tanshinone IIA, danshensu, salvianolic acid B, lithospermicacids, and cryptotanshinone, exhibit beneficial effects in managing cardiovascular diseases [38, 39]. For over five decades, using Dan Shen products has been considered extremely safe, with no reports of any major adverse effect [40]. Although studies have reported its interactions with warfarin, salicylate, diazepam, and ginseng [41–44], no studies have reported interactions between antihypertensive drugs and Dan Shen.
Gou Teng is the second most frequently prescribed single herb for hypertension. Certain studies have reported that alkaloids are the main active pharmacological components of Gou Teng. Of these components, rhynchophylline and isorhynchophylline are the chief ingredients, which play a major role as hypotensive agents [45]. As observed in Table 4, TCM physicians often used Tian Ma in combination with Gou Teng for treating hypertension or hypertension-related symptoms. Tian Ma is also a crucial Chinese herb used for decreasing blood pressure values. Moreover, recent studies have demonstrated that it can promote a stable decrease in blood pressure, improve clinical symptoms, regulate the rennin–angiotensin system, improve insulin resistance and salt sensitivity, and decrease serum levels of total cholesterol, triglycerides, and low-density lipoprotein cholesterol [15, 46, 47].
To increase treatment efficacy and compensate for insufficiency of another single herb, TCM physicians often use two single herbs as a herb pair. Tian Ma used with Gou Teng is an example of a herb pair that increases treatment efficacy and exerts similar effects in the cardiovascular and central nervous systems. This might explain why Tian Ma and Gou Teng are the two most frequently prescribed single herbs in combination for treating hypertension.
In addition, TCM physicians often used Ge Gen to treat hypertension-related symptoms such as headache and dizziness. Previous studies have reported that Ge Gen primarily comprises isoflavonoids, such as puerarin, diadzein, and daidzin, which exhibit anti-hypertensive [48] and antithrombotic effects [49] and reduce plasma cholesterol levels [50].
TCM physicians treat patients with hypertension according to syndrome differentiation theory, and prescriptions differed among TCM physicians because of their experience and knowledge. In the present study, the co-prescription patterns of CHPs by TCM physicians differed from that of decoctions. TCM physicians prescribed a thoroughly recorded formula as the core formula and subtracted or added herbs in a decoction preparation to fit a patient’s condition according to TCM theory. When they prescribed CHPs, which are extracted and completely mixed together in the manufacturing process, TCM physicians only added single or multiple herbs into the core formula, but subtracted or changed the proportions of herbs in the finished herbal products. Thus, TCM physicians combined other formulae or herbs in each prescription to treat patients. Moreover, the NHI in Taiwan only reimburses CHPs and not decoctions, eliciting our concern that the co-prescription pattern of CHPs with a high support factor might indicate a typical practice pattern among TCM physicians in Taiwan [51]. Although 5.9 CHPs were prescribed on average during one hypertension-related TCM outpatient visit in the present study, the co-prescription of three or more Chinese herbal formulae or single herbs for hypertension had a low support factor; thus, we determined two co-prescription patterns (one to one association) in the study.
Tian-Ma-Gou-Teng-Yin and Xue-Fu-Zhu-Yu-Tang was the most commonly prescribed combination of two herbal formulae for treating hypertension, whereas Tian-Ma-Gou-Teng-Yin and Dan Shen were the most frequently prescribed combination of an herbal formula and a single herb for treating hypertension. In addition, Tian-Ma-Gou-Teng-Yin and Dan Shen were the most frequently co-prescribed herbal formula and single herb for treating hypertension. Furthermore, we could investigate the most common corresponding diagnoses or syndromes related to hypertension. As in a previous study [32], we can conduct clinical trials on the efficacy and safety of these co-prescribed CHPs according to the results of our study in the future.
Although patients with hypertension primarily seek conventional therapy, TCM is crucial in complementary and alternative medicines. In other words, most patients with hypertension who went to TCM outpatient clinical practices for treatment often had an initial hypertension diagnosis from Western medicine practitioners. Furthermore, modern TCM physicians are trained in Western medicine knowledge during undergraduate or refresher courses. Although, the therapeutic principles of TCM are based on the results of syndrome differentiation, which differs from the principles of Western medicine, TCM physicians in Taiwan must use ICD-9-CM codes in the NHI claims database to diagnose diseases during outpatient visits.
A previous study revealed that some patients seek TCM treatment for problems other than hypertension, whereas some patients were treated for hypertension with acupuncture and traumatology manipulative therapies [16]. This might explain why only 81,582 outpatient hypertension-related visits involved CHP prescriptions by TCM physicians among the 123,240 TCM visits investigated in the present study. The prevalence of hypertension increases with age, especially when people are older than 65 years. These findings were consistent with those of a previous study [52]. However, our cohort included patients who had visited the outpatient department because of hypertension three or more times within one year alone during the study period of 2003–2009; this might have led to an underestimation of the prevalence of hypertension in Taiwan. In the present study cohort, women and patients aged 45–65 years used TCM more frequently than did men and patients in the other age groups. In addition, the patients with hypertension who experienced additional comorbidities such as metabolic diseases were more likely to consider TCM treatments.
This study had three limitations. First, we could not obtain definitive conclusions regarding the relationship between the severity of hypertension and TCM utilization. Second, apparently, TCM physicians in Taiwan use ICD-9-CM for diagnosis in clinical practice, but no reliable and suitable disease coding system exists for TCM. Several variations were observed in the prescription patterns for treating hypertension because the therapeutic principles of TCM are based on the results of syndrome differentiation. Thus, developing a coding system for TCM diagnostic classifications in the future is critical and will assist TCM research greatly. Third, NHI provided reimbursements for only finished herbal products prescribed by TCM physicians and did not include decoctions and CHPs provided by pharmacies; this might have led to the underestimation of the frequency of TCM utilization. However, this underestimation might be small because most CHPs were reimbursed.
Conclusions
This study analyzed a cohort of one million randomly sampled patients from the NHIRD from 2003 to 2009 and documented the frequency and co-prescription pattern of CHPs for hypertension in clinical practice in Taiwan. However, further research must be conducted to strengthen the available clinical evidence regarding the efficacy and safety of CHPs in improving hypertension-related mortality and morbidity as well as the drug–herb interactions.
Acknowledgments
The author's would like to thank Center of Excellence for Chang Gung Research Datalink (CORPG6D0161) for the comments and assistance in data analysis. This study was supported by a grant from Chang Gung Memorial Hospital, Chia-yi Branch, and based on the National Health Insurance Research Database provided by the Central Bureau of National Health Insurance, the Department of Health, and managed by the National Health Research Institutes. The interpretation and conclusions contained herein do not represent those of Bureau of National Health Insurance, Department of Health, or National Health Research Institutes.
Abbreviations
- CHPs
Chinese herbal products
- TCM
Traditional Chinese Medicine
- NHI
National Health Insurance
- NHIRD
National Health Insurance Research Database
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
All authors designed and conceived the study. PRY, YHC, and PCC analyzed and interpreted the data. PRY, WTS and CYW wrote the study. All authors approved the final version of submitted manuscript.
References
- 1.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–223. doi: 10.1016/S0140-6736(05)70151-3. [DOI] [PubMed] [Google Scholar]
- 2.Masuo K, Tuck ML, Lambert GW. Hypertension and diabetes in obesity. Int J Hypertens. 2011;2011:695869. doi: 10.4061/2011/695869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anagnostis P, Karagiannis A, Tziomalos K, Athyros VG, Kita M, Mikhailidis DP. Endocrine hypertension: diagnosis and management of a complex clinical entity. Curr Vasc Pharmacol. 2010;8(5):646–660. doi: 10.2174/157016110792006996. [DOI] [PubMed] [Google Scholar]
- 4.Lawes CM, Vander Hoorn S, Rodgers A. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371(9623):1513–1518. doi: 10.1016/S0140-6736(08)60655-8. [DOI] [PubMed] [Google Scholar]
- 5.MacMahon S, Alderman MH, Lindholm LH, Liu L, Sanchez RA, Seedat YK. Blood-pressure-related disease is a global health priority. Lancet. 2008;371(9623):1480–1482. doi: 10.1016/S0140-6736(08)60632-7. [DOI] [PubMed] [Google Scholar]
- 6.Yach D, Hawkes C, Gould CL, Hofman KJ. The global burden of chronic diseases: overcoming impediments to prevention and control. JAMA. 2004;291(21):2616–2622. doi: 10.1001/jama.291.21.2616. [DOI] [PubMed] [Google Scholar]
- 7.Chen KJ, Hui KK, Lee MS, Xu H. The potential benefit of complementary/alternative medicine in cardiovascular diseases. Evid Based Complement Alternat Med. 2012;2012:125029. doi: 10.1155/2012/125029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu H, Chen K. Integrative medicine: the experience from China. J Altern Complement Med. 2008;14(1):3–7. doi: 10.1089/acm.2006.6329. [DOI] [PubMed] [Google Scholar]
- 9.Wang J, Xiong X. Control strategy on hypertension in chinese medicine. Evid Based Complement Alternat Med. 2012;2012:284847. doi: 10.1155/2012/284847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xiong X, Yang X, Liu Y, Zhang Y, Wang P, Wang J. Chinese herbal formulas for treating hypertension in traditional Chinese medicine: perspective of modern science. Hypertens Res. 2013;36(7):570–579. doi: 10.1038/hr.2013.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang J, Xiong X. Evidence-based chinese medicine for hypertension. Evid Based Complement Alternat Med. 2013;2013:978398. doi: 10.1155/2013/978398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Insurance BNH. The national health insurance annual statistical report. Bureau of National Health Insurance: Taipei, Taiwan; 2010. [Google Scholar]
- 13.Chen TJ, Chou LF, Hwang SJ. Application of a data-mining technique to analyze coprescription patterns for antacids in Taiwan. Clin Ther. 2003;25(9):2453–2463. doi: 10.1016/S0149-2918(03)80287-4. [DOI] [PubMed] [Google Scholar]
- 14.Wang LY, Li Y, Li N, Ding Y, Shi NN, Yan XJ. Study on TCM syndrome distribution of 1508 cases of hypertension patients with clinical epidemiology. China Journal of Traditional Chinese Medicine and Pharmacy. 2010;12:1960–1963. [Google Scholar]
- 15.Xiong X, Yang X, Liu W, Chu F, Wang P, Wang J. Trends in the treatment of hypertension from the perspective of traditional chinese medicine. Evid Based Complement Alternat Med. 2013;2013:275279. doi: 10.1155/2013/275279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tsai DS, Chang YS, Li TC, Peng WH. Prescription pattern of Chinese herbal products for hypertension in Taiwan: A population-based study. J Ethnopharmacol 2014:155(3);1534-40. [DOI] [PubMed]
- 17.Zhang Q, Zhang ZM, Li BY. Clinical study of tianmagouteng drinks treat 120 patients with hypertension. J Tradit Chin Med. 2008;10:1487–1489. [Google Scholar]
- 18.Liu WP, Xing ZH, Lin ZZ. Effect of Tianmagouteng decoction on the quality of life in patients with essential hypertension. Chinese Journal of Rehabilitation. 2003;01:20–21. [Google Scholar]
- 19.Lin ZZ, Xing ZH, Cai CL, Tan HY, Zhang C. Effects of tianma gouteng decoction on the plasma endothelin of patients with primary hypertension of hyperactivity of the liver yang. Chinese Journal of Clinical Rehabilitation. 2004;27:5992–5993. [Google Scholar]
- 20.Zhang Z, Lin ZZ, Jia SP. The clinical observation for the therapeutic effect of Tianmagouteng Decoction on the plasma level of malondic aldehyde among patients with hypertension. Journal of Hebei North University (Medical Edition) 2006;03:22–23. [Google Scholar]
- 21.Wu YS, Gao XF, Li SL. The exploration on the treatment of Tianma Gouteng YIn for ET CGRP in primary hypertension. Liaoning Journal of Traditional Chinese Medicine. 1998;05:13. [Google Scholar]
- 22.Wang S, Chen Y, He D, He L, Yang Y, Chen J, et al. Inhibition of vascular smooth muscle cell proliferation by serum from rats treated orally with Gastrodia and Uncaria decoction, a traditional Chinese formulation. J Ethnopharmacol. 2007;114(3):458–462. doi: 10.1016/j.jep.2007.08.039. [DOI] [PubMed] [Google Scholar]
- 23.Zhang L. The effects of Tianmagouteng Decoction (TD) on insulin resistance in patients with essential hypertension. J Tradit Chin Med. 2008;06:717–720. [Google Scholar]
- 24.Zhang HW, Tong J, Zhou G, Jia H, Jiang JY. Tianma Gouteng Yin Formula for treating primary hypertension. Cochrane Database Syst Rev. 2012;6 doi: 10.1002/14651858.CD008166.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Watanabe H, Zhao Q, Matsumoto K, Tohda M, Murakami Y, Zhang SH, et al. Pharmacological evidence for antidementia effect of Choto-san (Gouteng-san), a traditional Kampo medicine. Pharmacol, Biochem Behav. 2003;75(3):635–643. doi: 10.1016/S0091-3057(03)00109-6. [DOI] [PubMed] [Google Scholar]
- 26.Yano S, Horiuchi H, Horie S, Aimi N, Sakai S, Watanabe K. Ca2+ channel blocking effects of hirsutine, an indole alkaloid from Uncaria genus, in the isolated rat aorta. Planta Med. 1991;57(5):403–405. doi: 10.1055/s-2006-960134. [DOI] [PubMed] [Google Scholar]
- 27.Goto H, Shimada Y, Tanigawa K, Sekiya N, Shintani T, Terasawa K. Effect of Uncariae ramulus et Uncus on endothelium in spontaneously hypertensive rats. Am J Chin Med. 1999;27(3–4):339–345. doi: 10.1142/S0192415X99000380. [DOI] [PubMed] [Google Scholar]
- 28.Song J, Chen WY, Wu LY, Zheng LP, Lin W, Gao D, et al. A microarray analysis of angiogenesis modulation effect of Xuefu Zhuyu Decoction on endothelial cells. Chin J Integr Med. 2012;18(7):502–506. doi: 10.1007/s11655-012-1143-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang QY, Wang QL, Su JF XDB, Cai GX, Li Y. Angiogenesis effects of XuefuZhuyu Decoction and VEGF protein expression of rats with acutemyocardial ischemia. Chin J Info TCM. 2011;02:53–54. [Google Scholar]
- 30.Shih WT, Yang YH, Chen PC. Prescription patterns of chinese herbal products for osteoporosis in taiwan: a population-based study. Evid Based Complement Alternat Med. 2012;2012:752837. doi: 10.1155/2012/752837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang YH, Chen PC, Wang JD, Lee CH, Lai JN. Prescription pattern of traditional Chinese medicine for climacteric women in Taiwan. Climacteric. 2009;12(6):541–547. doi: 10.3109/13697130903060081. [DOI] [PubMed] [Google Scholar]
- 32.Lai JN, Hwang JS, Chen HJ, Wang JD. Finished herbal product as an alternative treatment for menopausal symptoms in climacteric women. J Altern Complement Med. 2005;11(6):1075–1084. doi: 10.1089/acm.2005.11.1075. [DOI] [PubMed] [Google Scholar]
- 33.Kang DG, Yun YG, Ryoo JH, Lee HS. Anti-hypertensive effect of water extract of danshen on renovascular hypertension through inhibition of the renin angiotensin system. Am J Chin Med. 2002;30(1):87–93. doi: 10.1142/S0192415X02000107. [DOI] [PubMed] [Google Scholar]
- 34.Shen Y, Li Y. Zhong yao yao li xue. Shanghai: Shanghai ke xue ji shu chu ban she; 1997. pp. 128–129. [Google Scholar]
- 35.Wu YJ, Hong CY, Lin SJ, Wu P, Shiao MS. Increase of vitamin E content in LDL and reduction of atherosclerosis in cholesterol-fed rabbits by a water-soluble antioxidant-rich fraction of Salvia miltiorrhiza. Arterioscler, Thromb, Vasc Biol. 1998;18(3):481–486. doi: 10.1161/01.ATV.18.3.481. [DOI] [PubMed] [Google Scholar]
- 36.Cao CM, Xia Q, Zhang X, Xu WH, Jiang HD, Chen JZ. Salvia miltiorrhiza attenuates the changes in contraction and intracellular calcium induced by anoxia and reoxygenation in rat cardiomyocytes. Life Sci. 2003;72(22):2451–2463. doi: 10.1016/S0024-3205(03)00142-5. [DOI] [PubMed] [Google Scholar]
- 37.Yu GR. [Clinical and experimental study on the effect of Salvia miltiorrhiza on microcirculation and 2,3 diphosphoglyceric acid in patients with coronary heart disease] Zhong Xi Yi Jie He Za Zhi. 1988;8(10):596–598. [PubMed] [Google Scholar]
- 38.Chan P, Liu IM, Li YX, Yu WJ, Cheng JT. Antihypertension Induced by Tanshinone IIA Isolated from the Roots of Salvia miltiorrhiza. Evid Based Complement Alternat Med. 2011;2011:392627. doi: 10.1093/ecam/nep056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lam FF, Yeung JH, Chan KM, Or PM. Relaxant effects of danshen aqueous extract and its constituent danshensu on rat coronary artery are mediated by inhibition of calcium channels. Vascul Pharmacol. 2007;46(4):271–277. doi: 10.1016/j.vph.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 40.Cheng TO. Cardiovascular effects of Danshen. Int J Cardiol. 2007;121(1):9–22. doi: 10.1016/j.ijcard.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 41.Jinping Q, Peiling H, Yawei L, Abliz Z. Effects of the aqueous extract from Salvia miltiorrhiza Bge on the pharmacokinetics of diazepam and on liver microsomal cytochrome P450 enzyme activity in rats. J Pharm Pharmacol. 2003;55(8):1163–1167. doi: 10.1211/0022357021602. [DOI] [PubMed] [Google Scholar]
- 42.Gupta D, Jalali M, Wells A, Dasgupta A. Drug-herb interactions: unexpected suppression of free Danshen concentrations by salicylate. J Clin Lab Anal. 2002;16(6):290–294. doi: 10.1002/jcla.10057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chan TY. Interaction between warfarin and danshen (Salvia miltiorrhiza) Ann Pharmacother. 2001;35(4):501–504. doi: 10.1345/aph.19029. [DOI] [PubMed] [Google Scholar]
- 44.Cheng TO. Herbal interactions with cardiac drugs. Arch Intern Med. 2000;160(6):870–871. doi: 10.1001/archinte.160.6.870. [DOI] [PubMed] [Google Scholar]
- 45.Song CQ, Fan Y, Huang WH, Wu DZ, Hu ZB. Different hypotentive effects of various active constituents isolated from Uncaria rhynchophylla. Chin Tradit Herb Drugs. 2000;10:44–46. [Google Scholar]
- 46.Jiang JY, Wang XZ, Luo SS. Effect of banxia baizhu tianma decoction on the left ventricular hypertrophy of hypertrophied myocardium in spontaneously hypertensive rat. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2010;30(10):1061–1066. [PubMed] [Google Scholar]
- 47.Wu QF, Wen MX, Lan DH. Effect of Banxia baizhu tianma decoctionon insulin resistance and blood lipid inhypertensive patients with abundant phlegm-dampness syndrome. Fujian Zhong Yi Xue Yuan Xue Bao. 2007;02:8–10. [Google Scholar]
- 48.Sun XH, Ding JP, Li H, Pan N, Gan L, Yang XL, et al. Activation of large-conductance calcium-activated potassium channels by puerarin: the underlying mechanism of puerarin-mediated vasodilation. J Pharmacol Exp Ther. 2007;323(1):391–397. doi: 10.1124/jpet.107.125567. [DOI] [PubMed] [Google Scholar]
- 49.Choo MK, Park EK, Yoon HK, Kim DH. Antithrombotic and antiallergic activities of daidzein, a metabolite of puerarin and daidzin produced by human intestinal microflora. Biol Pharm Bull. 2002;25(10):1328–1332. doi: 10.1248/bpb.25.1328. [DOI] [PubMed] [Google Scholar]
- 50.Yan LP, Chan SW, Chan AS, Chen SL, Ma XJ, Xu HX. Puerarin decreases serum total cholesterol and enhances thoracic aorta endothelial nitric oxide synthase expression in diet-induced hypercholesterolemic rats. Life Sci. 2006;79(4):324–330. doi: 10.1016/j.lfs.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 51.Hsieh SC, Lai JN, Lee CF, Hu FC, Tseng WL, Wang JD. The prescribing of Chinese herbal products in Taiwan: a cross-sectional analysis of the national health insurance reimbursement database. Pharmacoepidemiol Drug Saf. 2008;17(6):609–619. doi: 10.1002/pds.1611. [DOI] [PubMed] [Google Scholar]
- 52.Kaplan NM, Victor RG. Hypertension in the population at large. 11. Philadelphia: Wolters Kluwer; 2014. Hypertension in the population at large; p. 1. [Google Scholar]


