Abstract
Background:
Many factors contribute to occupational injuries. However, these factors have been compartmentalized and isolated in most studies.
Objective:
To examine the relationship between work-related injuries and multiple occupational and non-occupational factors among construction workers in the USA.
Methods:
Data from the 1988–2000 National Longitudinal Survey of Youth, 1979 cohort (N = 12,686) were analyzed. Job exposures and health behaviors were examined and used as independent variables in four multivariate logistic regression models to identify associations with occupational injuries.
Results:
After controlling for demographic variables, occupational injuries were 18% (95% CI: 1.04–1.34) more likely in construction than in non-construction. Blue-collar occupations, job physical efforts, multiple jobs, and long working hours accounted for the escalated risk in construction. Smoking, obesity/overweight, and cocaine use significantly increased the risk of work-related injury when demographics and occupational factors were held constant.
Conclusions:
Workplace injuries are better explained by simultaneously examining occupational and non-occupational characteristics.
Keywords: Job exposures, Health behaviors, Multiple exposures, Occupational injuries, Workplace injuries
Background
The construction industry is a high-risk occupational injury sector in the USA. Despite injury reductions resulting from continuous intervention efforts, the construction industry reported more fatalities than any other industry in 2012.1 Although the nonfatal injury rate in the US construction industry has declined significantly over the past two decades, the rate of injuries resulting in days away from work is still 40% higher than the rate for all industries combined.2 In addition to the pain and suffering of injured workers, work-related injuries pose huge financial burdens on workers, their families, employers, communities, and the economy. It is estimated that injuries resulting from falls to a lower level in construction cost $427 million annually (2005–2008 average) for medical care alone.3 Therefore, to reduce traumatic injuries and fatalities in construction is one of the strategic goals of the National Occupational Research Agenda.4
Many factors contribute to occupational injuries. Most traditional research focuses on workplace factors. Studies have found that physically demanding jobs5–8 and working long hours and shift work9–15 increase the risk of occupational injury. Job tenure also plays a role in workplace injuries.5,16 An examination of construction occupations showed that plumbers and electricians with five or less years in their present job were significantly more likely to experience a workplace injury than their more tenured counterparts.17
Researchers have also found disparities in injury risk by race/ethnicity,18–20 gender,12,13,18 age,12,16,17,21–24 geographic region,20 and education.5 For example, Hispanic construction workers have a higher rate of occupational injuries than their non-Hispanic counterparts.25 Younger workers generally lack experience, which may also increase the risk of injury on the job.16,21
Additionally, health behaviors have been linked to workplace injuries. Several studies, including two in construction, have shown that smokers have a higher risk of occupational injury than non-smokers.17,22,26–29 Alcohol, marijuana, cocaine, and other substance abuse are associated with increased occupational injury, with studies showing a dose-response relationship.13,30 A study of unionized construction workers in Washington State showed that among 25–30 year olds, substance abusers were almost twice as likely to incur a workplace injury when compared to non substance abusers.26 Another study in France found smoking to be an injury risk factor for workers under age 30.27
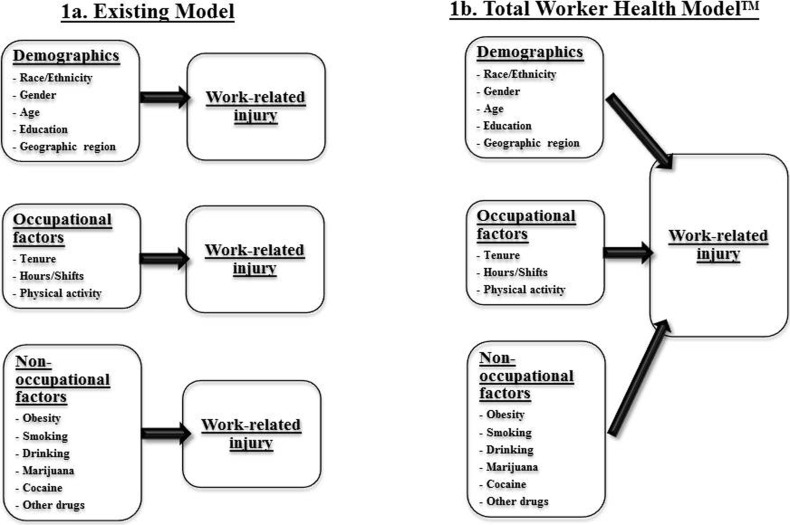
Although these studies are useful in understanding the risk factors of work-related injury, most have been compartmentalized (Fig. 1a). Following research patterns, injury prevention programs have typically focused on safety and workplace health promotion programs related to one off-the-job risk factor (e.g. smoking cessation programs). Today, a growing body of evidence supports the effectiveness of workplace interventions that integrate health protection and health promotion programs.31–33 More researchers and policymakers have recognized that occupational and non-occupational factors may contribute to worker safety and health simultaneously.34,35 In response, the National Institute for Occupational Safety and Health (NIOSH) launched the Total Worker HealthTM (TWHTM) program.36 Given the higher than average injury rates among construction workers, further exploration of workplace injuries using the TWH concept is necessary for targeting effective mitigation strategies for this high-risk worker group.
Figure 1.
Demographics, occupational factors, and non-occupational factors associated with work-related injury.
Despite the importance of integration, the construction industry presents a challenge for occupational safety and health research. The work environment changes daily for individual workers as construction progresses and the workers move from project to project or company to company. As a result, many studies with construction workers have relied on cross-sectional data, were limited by small sample size, or lacked statistical power.16,17,26,28
The National Longitudinal Survey of Youth, 1979 cohort (NLSY79), a population-based longitudinal study, provides a valuable opportunity to explore several factors simultaneously for individuals with multiple employers or transient/sporadic employment patterns typical of construction work. Using the NLSY79 to assess injury risk among all workers, researchers have found an association between injuries and education, overtime, race/ethnicity, gender, marital status, and obesity.5,6,18,21,37 Within construction, overtime and shift work were found to be associated with an increased risk of injury.9 While these study designs may be sound, they were restricted to focus on one risk factor in one study. It remains unclear whether factors observed separately contribute jointly to work-related injuries. Therefore, to better measure the combined effects of multiple factors on occupational injury, this study concurrently examines how work-related injuries are affected by occupational and non-occupational factors among construction workers using the concept model illustrated in Fig. 1b. The model is built upon existing research and the TWH concept discussed above. It hypothesizes that job exposures, health behaviors, and other personal characteristics contribute jointly to work-related injuries. The hypothesis was tested step-by-step using multivariate logistic regression.
Methods
Data source and sample size
This study analyzed 1988–2000 data from the NLSY79, a nationally representative longitudinal survey sponsored by the US Bureau of Labor Statistics.38 The initial sample contained 12,686 young men and women aged 14 through 22 years old as of January 1979. Participants were interviewed annually from 1979 through 1994, and biennially from 1996 through the present. The NLSY79 provides detailed information on demographics, employment history, socioeconomic characteristics, and a variety of health behaviors. A work-related injury module was introduced in 1988 and included through 2000. Between 1988 and 2000 (except in 1991), survey respondents were asked whether they had experienced a work-related injury since the last interview. The information collected in the survey facilitated the tracking of work histories, health behaviors, and work-related injuries for the respondents.
The response rates of the NLSY79 were 91% and 83% in 1988 and 2000, respectively.39 Between 1988 and 2000, about 500–700 respondents per wave reported their current or most recent primary job (in any occupation) was in the construction industry. Overall, 1,625 NLSY79 respondents reported working in construction as their current or most recent primary job for at least one wave (1–2 years) during the study period — a total of 5,287 observations. Those who were employed in other industries were referred to as non-construction workers, a total of 65,751 throughout the 12-year period. Those who were not in the labor force, or did not report industry were excluded from this study.
Outcome measure
Work-related injury was the outcome measure. From 1988 to 2000, the NLSY79 respondents were asked, “Since [date of last interview], have you had an incident at any job that resulted in an injury or illness to you?” Following this question, the respondents were asked whether they missed one or more work days due to injury or illness since the last interview, not counting the day of the incident. Because very few incidents resulted in illness in construction, the term “injuries” refers to “injuries and illnesses” in the study. Injury incidence rates at each survey were calculated using the number of reported injuries in the survey as the numerator and the number of respondents who were employed and completed the injury module in that survey year as the denominator. In multivariate regression models, a dichotomous dependent variable was generated to represent participants' work-related injury status (yes/no) in the survey reference period.
Occupational factors
Occupational factors included blue-collar (e.g. carpenter, roofer, laborer) or white-collar (e.g. manager, professional, administrative) occupation; number of jobs held in the calendar year before the interview; and hours worked per day and weeks worked per year in the current or most recent job. Occupational factors also measured physical effort on the job (ranging from “all/most of the time,” to “none/almost none of the time”); and whether the job required lifting heavy loads/stooping/kneeling/crouching was categorized as “most/all of the time/5–7 days a week,” “moderate amount/some of the time/1–4 days a week,” and “rarely/none of the time/less than 1 day a week.” Job-required physical activities were composed of nine dichotomous (yes/no) measures: walk around; use hands or fingers; reach for supplies; lift up to 10 pounds; lift over 10 pounds; stoop/kneel/crouch; stand for long periods; use stairs/inclines; and hear special sounds (e.g. signals, directions). These nine measures were combined into a physical activity index ranging from zero to nine. Physical effort information was only collected in 1998 and 2000. Assuming exposures were similar for the same occupation over time, the value of physical activity was estimated by occupation and assigned to individuals based on their occupation for the years when physical activity information was not collected.
Non-occupational factors
Body mass index (BMI), smoking status, drinking status, lifetime marijuana use, and lifetime cocaine use were defined as non-occupational factors. Respondents' BMI in each wave was categorized as normal weight (BMI = 18.5–24.9), overweight (BMI = 25.0–29.9), or obese (BMI ≥ 30). Very few respondents were underweight and they were excluded from the estimations. Smoking status, lifetime marijuana use, and lifetime cocaine use were not collected in every wave; therefore, measures from the previous wave were used when the information was not collected. Smoking status included “never smoker” (fewer than 100 cigarettes in their lifetime); “former smoker” (at least 100 cigarettes in their lifetime, but were not currently smoking); and “current smoker” (smoked at least 100 cigarettes and were still smoking). Drinking status was only available in 1988, 1989, and 1994. “Heavy drinker” was defined as six or more drinks on one occasion at least four times in the past 30 days; “light drinker” included former drinkers and those who drank less than heavy drinkers; and “never drinker” included those who reported drinking no alcohol in the past 30 days.
Data analysis
Rate of work-related injury was stratified by subgroups and measured by number of incident injuries per 100 observations. Unadjusted injury rates were only estimated for subgroups among construction workers. To compare differences in injury rates among these subgroups, Chi-square tests were conducted with significance defined at the P < 0.05 level. The study hypothesis was tested in four steps using multivariate logistic regression models to determine whether factors in each of the models affected work-related injuries independently or jointly: Model 1, “Industry” as an independent exposure variable; Model 2, occupational factors; Model 3, non-occupational factors; and Model 4, combination of occupational and non-occupational factors. All models were adjusted for control variables identified from descriptive analysis, including gender, race/ethnicity, education, geographic region, and survey year. Odds ratios and 95% confidence intervals (CI) were tabulated from the regression and presented in the tables. All respondents who were ever employed during the study period were included in the models. The Hosmer–Lemeshow test was applied to assess goodness-of-fit for the logistic regression models. Sampling weights from the survey were used so that the estimates could better reflect the population represented by the NLSY79. SAS SURVEY procedures40 were employed for the data analyses.
Results
Table 1 summarizes the number of respondents and work-related injuries reported in construction and non-construction in each wave between 1988 and 2000. The injury incidence rate (per 100 observations) among construction workers was 14.2% compared to 9.3% among non-construction workers in 1988. However, the incidence rates show a decline over the years as the cohort aged. During the 12-year study period, the unadjusted incidence rate for construction workers was approximately 52% higher than that for non-construction workers on average (10.8% versus 7.1%).
Table 1. Observations, work-related injuries, and injury incidence rate, construction versus non-construction, 1988–2000.
| Construction | Non-construction | |||||||||
| 95% CI | 95% CI | |||||||||
| Survey year | Observations | Injuries | Incidence ratea | Lower | Upper | Observations | Injuries | Incidence ratea | Lower | Upper |
| 1988 | 652 | 85 | 14.2% | 10.8% | 17.6% | 8,341 | 754 | 9.3% | 8.5% | 10.0% |
| 1989 | 706 | 65 | 9.2% | 6.6% | 11.8% | 8,344 | 547 | 6.6% | 6.0% | 7.3% |
| 1990 | 681 | 67 | 9.7% | 7.0% | 12.4% | 8,215 | 548 | 6.4% | 5.7% | 7.0% |
| 1992b | 536 | 57 | 10.9% | 7.8% | 13.9% | 7,100 | 505 | 7.5% | 6.8% | 8.3% |
| 1993 | 587 | 57 | 9.7% | 6.9% | 12.4% | 6,970 | 390 | 5.8% | 5.1% | 6.4% |
| 1994 | 482 | 48 | 10.9% | 7.7% | 14.2% | 6,194 | 411 | 6.9% | 6.2% | 7.7% |
| 1996b | 555 | 60 | 11.8% | 8.7% | 14.9% | 6,989 | 544 | 7.8% | 7.0% | 8.5% |
| 1998b | 536 | 57 | 12.3% | 9.0% | 15.5% | 6,917 | 498 | 7.2% | 6.5% | 7.9% |
| 2000b | 552 | 49 | 9.0% | 6.3% | 11.8% | 6,681 | 457 | 6.7% | 6.0% | 7.4% |
| Total | 5,287 | 545 | 10.8% | 9.8% | 11.8% | 65,751 | 4,654 | 7.1% | 6.9% | 7.4% |
Note:
aInjury incidence rate = number of injuries per 100 observations.
bInjury rates represent 2-year recall period. Percentages are weighted. No injury data were collected in 1991.
Injury incidence rates by demographics and non-occupational factors among construction workers are presented in Table 2. Male workers had a significantly higher injury rate than females (11.1% versus 7.7%). Hispanic workers accounted for less than 6% of the construction cohort and their injury rate was similar to that for white, non-Hispanic workers (12.8% versus 11.2%), but higher than that for black workers (6.2%). Workers with a high school education or less accounted for about three-quarters of the cohort and had a significantly higher injury rate compared to those with a higher education (11.8% versus 7.7%).
Table 2. Work-related injuries in construction, by demographics and non-occupational factors, 1988–2000.
| Injury incidence ratea | |||||
| 95% CI | |||||
| Characteristics | % of sample | Point estimate | Lower | Upper | P valueb |
| Demographics | |||||
| Gender | 0.045 | ||||
| Male | 90.8% | 11.1 | 10.1 | 12.2 | |
| Female | 9.2% | 7.7 | 4.9 | 10.4 | |
| Race/ethnicity | < 0.001 | ||||
| Hispanic | 5.6% | 12.8 | 10.2 | 15.5 | |
| Black | 10.1% | 6.2 | 4.7 | 7.7 | |
| White, non-Hispanic | 84.3% | 11.2 | 10.1 | 12.4 | |
| Birthplace | 0.495 | ||||
| Foreign-born | 3.5% | 12.3 | 7.7 | 17.0 | |
| Native-born | 96.5% | 10.8 | 9.7 | 11.8 | |
| Education | 0.001 | ||||
| High school or less | 75.9% | 11.8 | 10.6 | 12.9 | |
| Some college or above | 24.1% | 7.7 | 5.8 | 9.5 | |
| Geographic region | 0.002 | ||||
| Northeast | 18.5% | 9.5 | 7.4 | 11.7 | |
| Midwest | 26.5% | 13.6 | 11.5 | 15.8 | |
| South | 35.3% | 8.9 | 7.4 | 10.4 | |
| West | 19.8% | 11.6 | 9.3 | 13.9 | |
| Non-occupational factors | |||||
| BMIc | 0.926 | ||||
| Obese | 15.6% | 11.1 | 8.5 | 13.7 | |
| Overweight | 41.4% | 10.9 | 9.3 | 12.6 | |
| Normal weight | 43.1% | 10.6 | 9.1 | 12.1 | |
| Smoking | < 0.001 | ||||
| Current smoker | 46.5% | 13.1 | 11.4 | 14.8 | |
| Former smoker | 16.6% | 9.3 | 6.7 | 11.8 | |
| Never smoker | 36.9% | 8.6 | 7.1 | 10.1 | |
| Drinking | 0.415 | ||||
| Heavy drinker | 19.4% | 12.2 | 9.9 | 14.5 | |
| Light drinker | 59.1% | 10.5 | 9.2 | 11.7 | |
| Never drinker | 21.5% | 10.6 | 8.4 | 12.7 | |
| Lifetime marijuana use | 0.041 | ||||
| 11+ occasions | 43.3% | 12.5 | 10.8 | 14.2 | |
| 1–10 occasions | 31.8% | 9.7 | 8.0 | 11.5 | |
| Never | 24.9% | 10.0 | 8.0 | 12.0 | |
| Lifetime cocaine use | 0.031 | ||||
| 11+ occasions | 20.7% | 12.9 | 10.4 | 15.3 | |
| 1–10 occasions | 20.1% | 12.4 | 9.9 | 14.8 | |
| Never | 59.1% | 9.8 | 8.5 | 11.1 | |
| Total | 100% | 10.8 | 9.8 | 11.8 | … |
Note:
aInjury incidence rate = number of injuries per 100 observations.
bP-value represents chi-square tests comparing differences in injury rates by characteristics.
cWorkers with underweight BMI are excluded. Numbers are weighted.
In terms of non-occupational factors, approximately 47% of construction workers in this cohort were current smokers and 17% were former smokers (Table 2). Current smokers had the highest injury incidence rate (13.1%) compared to former smokers (9.3%) and never smokers (8.6%). Those who had used cocaine also had a higher rate compared to those who never used cocaine. Variation was found among workers with different BMI and drinking status, but the difference was not statistically significant.
Injury incidence rates by occupational factors in construction are reported in Table 3. Workers in blue-collar occupations and those with three or more jobs per year had higher injury rates than their counterparts, respectively. The relationship between injuries and hours or weeks worked was not linear; however, those who worked longer days and more weeks per year had a higher injury rate in general. Construction workers who expended physical effort all or most of the time on the job also had a higher injury rate than those without such efforts.
Table 3. Work-related injuries in construction, by occupational factors, 1988–2000.
| Injury incidence ratea | |||||
| 95% CI | |||||
| Occupational factors | % of sample | Point estimate | Lower | Upper | P valueb |
| Occupation | < 0.001 | ||||
| Blue-collar | 80.2% | 11.9 | 10.7 | 13.0 | |
| White-collar | 19.8% | 6.6 | 4.8 | 8.4 | |
| Number of jobs per year (mean: 2.0 jobs) | < 0.001 | ||||
| 1 job | 30.2% | 10.5 | 8.7 | 12.3 | |
| 2 jobs | 50.5% | 9.6 | 8.2 | 10.9 | |
| 3–4 jobs | 18.3% | 14.6 | 11.9 | 17.2 | |
| 5+ jobs | 0.9% | 22.4 | 8.9 | 35.9 | |
| Hours worked per day in primary job (mean: 8.7 hours) | 0.003 | ||||
| ≤ 8 hours | 62.9% | 9.4 | 8.2 | 10.6 | |
| 8.1–10 hours | 28.5% | 13.2 | 11.1 | 15.3 | |
| >10 hours | 8.6% | 12.7 | 8.9 | 16.4 | |
| Weeks worked per year (mean: 45.0 weeks) | 0.019 | ||||
| ≤ 26 weeks | 10.3% | 9.8 | 6.9 | 12.7 | |
| 27–48 weeks | 21.7% | 13.5 | 11.1 | 15.8 | |
| 49–52 weeks | 68.0% | 10.1 | 8.9 | 11.3 | |
| Physical efforts | 0.018 | ||||
| All or most of the time | 68.9% | 11.0 | 9.6 | 12.3 | |
| Some of the time | 20.7% | 10.6 | 8.1 | 13.1 | |
| None or almost none of the time | 10.3% | 5.7 | 3.1 | 8.2 | |
| Lifting/stooping/kneeling | 0.070 | ||||
| Most/all of the time/5–7 days a week | 59.7% | 11.2 | 9.9 | 12.5 | |
| Moderate amount/some of the time/1–4 days a week | 32.0% | 10.7 | 9.0 | 12.4 | |
| Rarely/none of the time/ < 1 day a week | 8.3% | 6.7 | 3.8 | 9.7 | |
| Job physical activity index (mean: 6.1) | 0.027 | ||||
| 0 | 10.6% | 6.1 | 3.5 | 8.7 | |
| 1–3 | 8.5% | 8.6 | 5.1 | 12.2 | |
| 4–6 | 17.7% | 12.2 | 9.4 | 15.0 | |
| 7–9 | 63.2% | 10.8 | 9.4 | 12.2 | |
| Total | 100% | 10.8 | 9.8 | 11.8 | … |
Note:
aInjury incidence rate = number of injuries per 100 observations.
bP value represents chi-square tests comparing differences in injury rates by occupational factors. Numbers are weighted.
Table 4 presents the results from four logistic regression models using observations in all industries. The Hosmer–Lemeshow test indicated that all four models fit the data, but Model 3 was the poorest fit (P = 0.071) and Model 4 was the best fit (P = 0.906). Controlling for demographics, construction workers were approximately 18% more likely to incur a work-related injury than their non-construction counterparts (Model 1). After occupational factors were taken into consideration, the industry differential disappeared, but all the occupational factors were significantly associated with work-related injury (Model 2). When examining non-occupational factors after controlling for demographics, the injury risk was 14% higher for construction workers compared to non-construction workers (Model 3). Obese/overweight, smoking, and cocaine use were risk factors for work-related injuries; however, drinking and marijuana use were not significant.
Table 4. Multivariate logistic regression of work-related injuries (injured versus not injured), 1988–2000.
| Model 1a | Model 2b | Model 3c | Model 4d | |||||||||
| 95% CI | 95% CI | 95% CI | 95% CI | |||||||||
| Variables | Odds ratio | Lower | Upper | Odds ratio | Lower | Upper | Odds ratio | Lower | Upper | Odds ratio | Lower | Upper |
| Industry | ||||||||||||
| Construction | 1.18** | 1.04 | 1.34 | 0.91 | 0.80 | 1.04 | 1.14* | 1.00 | 1.29 | 0.89 | 0.78 | 1.02 |
| Non-construction | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Occupation | ||||||||||||
| Blue-collar | … | … | … | 1.66** | 1.51 | 1.82 | … | … | … | 1.63** | 1.48 | 1.79 |
| White-collar | … | … | … | 1.00 | 1.00 | 1.00 | … | … | … | 1.00 | 1.00 | 1.00 |
| Physical efforts | ||||||||||||
| All or most of the time | … | … | … | 2.55** | 2.21 | 2.95 | … | … | … | 2.46** | 2.13 | 2.85 |
| Some of the time | … | … | … | 1.88** | 1.63 | 2.16 | … | … | … | 1.82** | 1.58 | 2.10 |
| None or almost none of the time | … | … | … | 1.00 | 1.00 | 1.00 | … | … | … | 1.00 | 1.00 | 1.00 |
| Number of jobs per year | ||||||||||||
| 5+ jobs | … | … | … | 2.16** | 1.50 | 3.10 | … | … | … | 2.00** | 1.39 | 2.88 |
| 3–4 jobs | … | … | … | 1.28** | 1.15 | 1.42 | … | … | … | 1.25** | 1.13 | 1.39 |
| 1–2 jobs | … | … | … | 1.00 | 1.00 | 1.00 | … | … | … | 1.00 | 1.00 | 1.00 |
| Hours worked per day in primary job | ||||||||||||
| >10 hours | … | … | … | 1.15* | 1.01 | 1.31 | … | … | … | 1.15* | 1.01 | 1.31 |
| 8.1–10 hours | … | … | … | 1.03 | 0.94 | 1.13 | … | … | … | 1.03 | 0.94 | 1.13 |
| ≤ 8 hours | … | … | … | 1.00 | 1.00 | 1.00 | … | … | … | 1.00 | 1.00 | 1.00 |
| BMIe | ||||||||||||
| Obese | … | … | … | … | … | … | 1.37** | 1.24 | 1.51 | 1.34** | 1.21 | 1.48 |
| Overweight | … | … | … | … | … | … | 1.12* | 1.03 | 1.22 | 1.13* | 1.02 | 1.21 |
| Normal weight | … | … | … | … | … | … | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Smoking | ||||||||||||
| Current smoker | … | … | … | … | … | … | 1.52** | 1.40 | 1.66 | 1.38** | 1.27 | 1.51 |
| Former smoker | … | … | … | … | … | … | 1.19** | 1.06 | 1.33 | 1.16* | 1.03 | 1.30 |
| Never smoker | … | … | … | … | … | … | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Drinking | ||||||||||||
| Heavy drinker | … | … | … | … | … | … | 1.01 | 0.89 | 1.15 | 0.99 | 0.87 | 1.13 |
| Light drinker | … | … | … | … | … | … | 0.96 | 0.88 | 1.05 | 0.99 | 0.91 | 1.08 |
| Never drinker | … | … | … | … | … | … | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Lifetime marijuana use | ||||||||||||
| 11+ occasions | … | … | … | … | … | … | 1.06 | 0.96 | 1.18 | 1.10 | 0.99 | 1.21 |
| 1–10 occasions | … | … | … | … | … | … | 1.01 | 0.91 | 1.12 | 1.04 | 0.94 | 1.15 |
| Never | … | … | … | … | … | … | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Lifetime cocaine use | ||||||||||||
| 11+ occasions | … | … | … | … | … | … | 1.15* | 1.02 | 1.29 | 1.16* | 1.03 | 1.30 |
| 1–10 occasions | … | … | … | … | … | … | 1.15* | 1.03 | 1.28 | 1.16** | 1.04 | 1.30 |
| Never | … | … | … | … | … | … | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
Note:
aP value for the Hosmer–Lemeshow goodness-of-fit test = 0.163.
bP value for the Hosmer–Lemeshow goodness-of-fit test = 0.520.
cP value for the Hosmer–Lemeshow goodness-of-fit test = 0.071.
dP value for the Hosmer-Lemeshow Goodness of fit test = 0.906.
eWorkers with underweight BMI are excluded. *P < 0.05. **P < 0.01. All models are adjusted by year, gender, race, education, and geographic region. Numbers are weighted.
Model 4 accounted for both occupational and non-occupational factors while controlling for demographic characteristics. No significant difference was found between construction and non-construction workers in the fully adjusted model, but risk factors identified from Models 2 and 3 remained statistically significant and results were robust. Blue-collar workers were 63% more likely to be injured on the job when compared to white-collar workers; workers who spent all or most of the time expending physical efforts, and held five or more jobs per year at least doubled their likelihood of a work-related injury compared to their corresponding counterparts. Current smokers had a 38% higher risk of work-related injury than those who never smoked. When compared to workers with normal weight, injury risk was 34% and 13% higher for obese and overweight workers, respectively. Any cocaine use increased the risk of injury by about 16% compared to individuals who never used cocaine.
Discussion
This study analyzed work-related injuries among construction workers during a 12-year period using data from the NLSY79. On average, construction workers in this cohort were 52% more likely to experience occupational injury compared to non-construction workers (Table 1). However, the industrial difference was reduced after controlling for demographics, and negated when occupational factors were considered. The results support the study hypothesis that work-related injury is associated with both occupational and non-occupational factors after controlling for demographics. Although non-occupational factors alone may not be sufficient to predict work-related injuries, the study suggested that including non-occupational factors may explain work-related injury risk to a greater extent.
The findings show that job exposures were major determinants of work-related injuries, consistent with previous studies in different settings.6,9–11,14–16 In addition to the factors that have been studied in prior research (i.e. occupation, job physical demands, and hours worked),6,9–11,15,41,42 this study found that the injury risk doubled for workers holding five or more jobs per year compared to those with one or two jobs. This indicates that worksite inexperience due to changing jobs frequently may be a risk factor for work-related injuries. Considering that the construction workforce is typically mobile, enhancing safety and health training for new workers should be a priority. This study also confirmed that smoking, obesity/overweight, and cocaine use significantly increased the risk of work-related injury when demographics and occupational factors were held constant.
There are several limitations that should be considered when interpreting the results of this study. The reference period for injury information changed during the study period, and was relatively long in later survey waves. In addition, the respondents were only asked whether they had a work-related injury since their last interview, but were not asked how many injuries they sustained during the recall period. This has not only increased recall bias, but also made it more difficult to tabulate injury rates. The information about past substance use in this cohort could be less accurate since the use of drugs is illegal, and both alcohol and smoking are stigmatized, possibly leading to systematic biases in responses.43 Moreover, while the NLSY79 provides a detailed job history, the measurement of workplace hazards that directly affect work-related injuries is limited. Further research should investigate the association between work-related injuries and specific working conditions using different approaches. Finally, this study only focused on the incidence of work-related injuries; ongoing workplace influences on chronic illnesses and the consequences of work-related injuries were not considered. More studies should be conducted using the NLSY79 or alternative data sources.
This study has several strengths. Work-related injuries in the study were estimated from a nationally representative data source. Using self-reported occupational injury as the outcome measure may reduce possible injury underreporting based on data from employers and workers' compensation.44,45 The repeated measure is particularly valuable for safety and health research on mobile construction workers. In addition, the validity and reliability of the NLSY79 have been tested by the NLS Technical Review Committee,46 and the NLSY79 data have been used in many published studies.9,47,48 Moreover, this study is one of few studies examining the relationship between work-related injuries and multiple occupational and non-occupational risk factors simultaneously. The findings could enhance our understanding of the Total Worker HealthTM concept — a strategy to prevent work-related injuries and illnesses and advance worker health and well-being.36
Conclusion
This study adds to research on workplace injuries in the context of individual construction workers during a 12-year period. The findings indicate that the difference between industries is mainly explained by jobsite exposures. Four occupational risk factors (i.e. blue-collar occupations, job physical efforts, multiple jobs per year, and longer working hours) accounted for the elevated injury rate in the construction industry. The results also suggest that smoking, obesity/overweight, and cocaine use directly or indirectly increase the likelihood of work-related injuries. Therefore, integrating workplace injury prevention and health promotion may be more effective than separate programs for improving worker safety and health.
Acknowledgements
The authors are grateful to Rosemary Sokas for her review and valuable comments, and Alissa Fujimoto for her contributions to this manuscript.
Disclaimer Statements
Contributors Xiuwen Sue Dong: study design, data interpretation, and writing manuscript; Xuanwen Wang: data manipulation and analysis, and writing manuscript; Julie Largay: literature review, writing and editing manuscript.
Funding This study was funded by the NIOSH grant U60OH009762. The contents of this study are solely the responsibility of the authors and do not necessarily represent the official views of NIOSH.
Conflicts of interest There are no conflicts of interest.
Ethics approval This study has been approved by the CPWR IRB.
References
- 1.US Bureau of Labor Statistics. Census of fatal occupational injuries [Internet]. Washington, DC: US Bureau of Labor Statistics; 2013 [cited 2014 Mar 1]. Available from: http://www.bls.gov/iif/oshcfoi1.htm.
- 2.US Bureau of Labor Statistics. Survey of Occupational Injuries and Illnesses [Internet]. Washington, DC: US Bureau of Labor Statistics; 2013 [cited 2014 Mar 1]. Available from: http://www.bls.gov/iif/oshcdnew.htm.
- 3.Occupational Safety and Health Administration. Workers' compensation costs of falls in construction: data from 38 states reporting to the National Council on Compensation Insurance (NCCI) [Internet]. Washington, DC: Occupational Safety and Health Administration; 2012. Available from: http://www.osha.gov/doc/topics/residentialprotection/workerscomp.ppt.
- 4.NORA Construction Sector Council. National construction agenda for occupational safety and health research and practice in the U.S. construction sector. Atlanta, GA: CDC; 2008. Available from: http://www.cdc.gov/niosh/programs/const/goals.html.
- 5.Pergamit MR, Krishnamurty P. Multiyear nonfatal work injury rates. Monthly Labor Rew. 2006:35–8. [Google Scholar]
- 6.Descatha A, Dale AM, Jaegers L, Herquelot E, Evanoff B. Self-reported physical exposure association with medial and lateral epicondylitis incidence in a large longitudinal study. Occup Env Med. 2013;70:670–3. doi: 10.1136/oemed-2012-101341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Richard JB, Thélot B, Beck F. [Injuries in France: trends and risk factors] Rev Epidemiol Sante Publique. 2013;61((3)):205–12. doi: 10.1016/j.respe.2012.10.007. French. [DOI] [PubMed] [Google Scholar]
- 8.Dawson DA. Heavy drinking and the risk of occupational injury. Accid Anal and Prev. 1994;26((5)):655–65. doi: 10.1016/0001-4575(94)90027-2. [DOI] [PubMed] [Google Scholar]
- 9.Dong XS. Long workhours, work scheduling and work-related injuries among construction workers in the United States. Scand J Work Environ Health. 2005;31:329–35. doi: 10.5271/sjweh.915. [DOI] [PubMed] [Google Scholar]
- 10.Dembe AE, Erickson JB, Delbos RG, Banks SM. The impact of overtime and long work hours on occupational injuries and illnesses: new evidence from the United States. Occup Env Med. 2005;62:588–97. doi: 10.1136/oem.2004.016667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nakata A. Effects of long work hours and poor sleep characteristics on workplace injury among full-time male employees of small- and medium-scale businesses. J Sleep Res. 2011;20:576–84. doi: 10.1111/j.1365-2869.2011.00910.x. [DOI] [PubMed] [Google Scholar]
- 12.Lombardi DA, Wirtz A, Willetts JL, Folkard S. Independent effects of sleep duration and body mass index on the risk of a work-related injury: evidence from the US National Health Interview Survey (2004–2010) Chronobiol Int. 2012;29((5)):556–64. doi: 10.3109/07420528.2012.675253. [DOI] [PubMed] [Google Scholar]
- 13.Shipp EM, Tortolero SR, Cooper SP, Baumler EG, Weller NF. Substance use and occupational injuries among high school students in south Texas. Am J Drug Alcohol Abuse. 2005;31((2)):253–65. [PubMed] [Google Scholar]
- 14.Dembe AE, Erickson JB, Delbos RG, Banks SM. Nonstandard shift schedules and the risk of job-related injuries. Scand J Work Environ Health. 2006;32((3)):232–40. doi: 10.5271/sjweh.1004. [DOI] [PubMed] [Google Scholar]
- 15.Salminen S. Shift work and extended working hours as risk factors for occupational injury. Ergon Open J. 2010;3:14–18. [Google Scholar]
- 16.Bena A, Giraudo M, Leombruni R, Costa G. Job tenure and work injuries: a multivariate analysis of the relation with previous experience and differences by age. BMC Public Health. 2013;13:869–77. doi: 10.1186/1471-2458-13-869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chau N, Mur JM, Benamghar L, Siegfried C, Dangelzer JL, Francais M et al. Relationships between certain individual characteristics and occupational injuries for various jobs in the construction industry: a case–control study. Am J Ind Med. 2004;45:84–92. doi: 10.1002/ajim.10319. [DOI] [PubMed] [Google Scholar]
- 18.Berdahl TA. Racial/ethnic and gender differences in individual workplace injury risk trajectories: 1988–1998. Am J Public Health. 2008;98:2258–63. doi: 10.2105/AJPH.2006.103135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Robinson JC. Exposure to occupational hazards among Hispanics, Blacks, and Non-Hispanic Whites in California. Am J Public Health. 1989;79:629–30. doi: 10.2105/ajph.79.5.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Richardson DB, Loomis D, Bena J, Bailer AJ. Fatal occupational injury rates in southern and non-southern states, by race and Hispanic ethnicity. Am J Public Health. 2004;94:1756–61. doi: 10.2105/ajph.94.10.1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Price JM. Risk assessment in the work environment of adolescents and their attainment of occupational injury or illness as young adult workers [Internet]. Law, Policy, and Society Dissertations. Paper 18. 010 Jan 1 [cited 2014 Mar 1]. Available from: http://iris.lib.neu.edu/cgi/viewcontent.cgi?article = 1016&context = law_pol_soc_diss.
- 22.Motamedzade M, Faghih MA, Golmohammadi R, Faradmal J, Mohammadi H. Effects of physical and personal risk factors on sick leave due to musculoskeletal disorders. Int J Occup Saf Ergon. 2013;19((4)):513–21. doi: 10.1080/10803548.2013.11077012. [DOI] [PubMed] [Google Scholar]
- 23.Chau N, Gauchard GC, Siegfried C, Benamghar L, Dangelzer JL, Français M et al. Relationships of job, age, and life conditions with the causes and severity of occupational injuries in construction workers. Int Arch Occup Environ Health. 2004;77:60–6. doi: 10.1007/s00420-003-0460-7. [DOI] [PubMed] [Google Scholar]
- 24.Mitchell OS. The relation of age to workplace injuries. Monthly Labor Rev. 1988;111((7)):9–13. [Google Scholar]
- 25.Dong XS, Fujimoto A, Ringen K, Men Y. Fatal falls among Hispanic construction workers. Accid Anal Prev. 2009;41((5)):1047–52. doi: 10.1016/j.aap.2009.06.012. [DOI] [PubMed] [Google Scholar]
- 26.Pollack ES, Franklin GM, Fulton-Kehoe D, Chowdhury R. Risk of job-related injury among construction laborers with a diagnosis of substance abuse. J Occup Environ Med. 1998;40:573–7. doi: 10.1097/00043764-199806000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Chau N, Bhattacherjee A, Kunar BM. Relationship between job, lifestyle, age and occupational injuries. Occup Med. 2009;59:114–9. doi: 10.1093/occmed/kqp002. [DOI] [PubMed] [Google Scholar]
- 28.Zheng L, Xiang H, Song X, Wang Z. Nonfatal unintentional injuries and related factors among male construction workers in central China. Am J Ind Med. 2010;53:588–95. doi: 10.1002/ajim.20833. [DOI] [PubMed] [Google Scholar]
- 29.Sacks JJ, Nelson DE. Smoking and injuries: an overview. Prev Med. 1994;23:515–20. doi: 10.1006/pmed.1994.1070. [DOI] [PubMed] [Google Scholar]
- 30.Trucco M, Rebolledo P, González X, Correa A, Bustamante M. [Recent alcohol and drug consumption in victims of work related accidents] Rev Med Chil. 1998;126((10)):1262–1267. Spanish. [PubMed] [Google Scholar]
- 31.Pronk NP.Integrated worker health protection and promotion programs: overview and perspectives on health and economic outcomes J Occup Environ Med. 20135512 Suppl):S30–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thakur JS, Bains P, Kar SS, Wadhwa S, Moirangthem P, Kumar R et al. Integrated healthy workplace model: an experience from North Indian industry. Indian J Occup Environ Med. 2012;16((3)):108–13. doi: 10.4103/0019-5278.111750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ovbiosa-Akinbosoye OE, Long DA. Factors associated with long-term weight loss and weight maintenance: analysis of a comprehensive workplace wellness program. J Occup Environ Med. 2011;53((11)):1236–42. doi: 10.1097/JOM.0b013e31823401db. [DOI] [PubMed] [Google Scholar]
- 34.Schulte PA, Wagner GR, Ostry A, Blanciforti LA, Cutlip RG, Krajnak KM et al. Work, obesity, and occupational safety and health. Am J Public Health. 2007;97((3)):428–36. doi: 10.2105/AJPH.2006.086900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Craig BN, Congleton JJ, Kerk CJ, Amendola AA, Gaines WG. Personal and non-occupational risk factors and occupational injury/illness. Am J Ind Med. 2006;49((4)):249–60. doi: 10.1002/ajim.20290. [DOI] [PubMed] [Google Scholar]
- 36.National Institute for Occupational Safety and Health. Total worker health [Internent]. Atlanta, GA: Centers for Disease Control and Prevention; 2014. Available from: http://www.cdc.gov/NIOSH/twh/
- 37.Lin T, Verma SK, Courtney TK. Does obesity contribute to non-fatal occupational injury? Evidence from the National Longitudinal Survey of Youth. Scand J Work Environ Health. 2013;39:268–75. doi: 10.5271/sjweh.3347. [DOI] [PubMed] [Google Scholar]
- 38.US Bureau of Labor Statistics. National longitudinal surveys: the NLSY79 [Internet]. 2013 Jun 12 [cited 2014 Mar 1]. Available from: http://www.bls.gov/nls/nlsy79.htm.
- 39.US Bureau of Labor Statistics. National longitudinal surveys: National Longitudinal Survey of Youth 1979: retention & reasons for noninterview [Internet]. Table 2 [cited 2014 June 29]. Available from: https://www.nlsinfo.org/content/cohorts/nlsy79/intro-to-the-sample/retention-reasons-noninterview.
- 40.SAS Institute Inc [Internet] SAS/STAT® 9.2 user's guide. Cary, NC: SAS Institute Inc.; 2009 [cited 2014 Mar 1]. Available from: http://support.sas.com/documentation/cdl/en/statugintroduction/61750/PDF/default/statugintroduction.pdf.
- 41.Caruso CC, Hitchcock EM, Dick RB, Russo JM, Schmit JM. Atlanta, GA: National Institute for Occupational Safety and Health; 2004. Overtime and extended work shifts: recent finding on illnesses, injuries, and health behaviors. (DHHS (NIOSH) Publication No. 2004–143). [Google Scholar]
- 42.Dong XS, Wang X, Daw C, Ringen K. Chronic diseases and functional limitations among older construction workers in the United States: a 10-year follow-up study. J Occup Environ Med. 2011;53((4)):372–80. doi: 10.1097/JOM.0b013e3182122286. [DOI] [PubMed] [Google Scholar]
- 43.Brener ND, Billy JOG, Grady WR. Assessment of factors affecting the validity of the self-reported health risk behavior among adolescents: evidence from the scientific literature. J Adolesc Health. 2003;33:436–57. doi: 10.1016/s1054-139x(03)00052-1. [DOI] [PubMed] [Google Scholar]
- 44.Leigh JP, Marcin JP, Miller TR. An estimate of the U.S. Government's undercount of nonfatal occupational injuries. J Occup Environ Med. 2004;46:10–18. doi: 10.1097/01.jom.0000105909.66435.53. [DOI] [PubMed] [Google Scholar]
- 45.Azaroff LS, Levenstein C, Wegman DH. Occupational injury and illness surveillance: conceptual filters explain underreporting. Am J Public Health. 2002;92:1421–9. doi: 10.2105/ajph.92.9.1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Center for Human Resource Research. Columbus, OH: Ohio State University; 2001. NLSY79 user's guide: a guide to the 1979–2000 National Longitudinal Survey of Youth data. [Google Scholar]
- 47.Besen E, Pransky G. Trajectories of productivity loss over a 20-year period: an analysis of the National Longitudinal Survey of Youth. Scand J Work Environ Health. 2014;40((4)):380–9. doi: 10.5271/sjweh.3433. [DOI] [PubMed] [Google Scholar]
- 48.Dembe AE, Yao X, Wickizer TM, Shoben AB, Dong XS. A novel method for estimating the effects of job conditions on asthma and chronic lung disease. J Asthma. 2014;51((8)):799–807. doi: 10.3109/02770903.2014.917183. [DOI] [PubMed] [Google Scholar]