Abstract
Introduction
The advent of “personalized medicine” has been driven by technological advances in genomics. Concentration at the subcellular level of a patient’s cancer cells has meant inevitably that the “person” has been overlooked. For this reason, we think there is an urgent need to develop a truly personalized approach focusing on each patient as an individual, assessing his/her unique mental dimensions and tailoring interventions to his/her individual needs and preferences. The aim of this study was to develop and test the psychometric properties of the ALGA-Breast Cancer (ALGA-BC), a new multidimensional questionnaire that assesses the breast cancer patient’s physical and mental characteristics in order to provide physicians, prior to the consultation, with a patient’s profile that is supposed to facilitate subsequent communication, interaction, and information delivery between the doctor and the patient.
Methods
The specific validation processes used were: content and face validity, construct validity using factor analysis, reliability and internal consistency using test–retest reliability, and Cronbach’s alpha correlation coefficient. The exploratory analysis included 100 primary breast cancer patients and 730 healthy subjects.
Results
The exploratory factor analysis revealed eight key factors: global self-rated health, perceived physical health, anxiety, self-efficacy, cognitive closure, memory, body image, and sexual life. Test–retest reliability and internal consistency were good. Comparing patients with a sample of healthy subjects, we also observed a general ability of the ALGA-BC questionnaire to discriminate between the two.
Conclusion
The ALGA-BC questionnaire with 29 items is a valid instrument with which to obtain a patient’s profile that is supposed to help physicians achieve meaningful personalized care which supplements biological and genetic analyses.
Keywords: personalized medicine, patient–physician communication, questionnaire validation, patient preferences
Introduction
According to the personalized medicine approach, appropriate and optimal therapies are mainly based on the analysis of the patient’s genome. Medicine, however, is broader than subcellular characteristics, and the patient as a person is the pivotal focus. Focus on the diverse consequences associated with the illness itself is critical to optimal patient care.1,2 In particular, along with assessing his/her biological and clinical characteristics, it is important to give attention to each patient as an individual, assessing unique mental dimensions and tailoring interventions to them. According to this vision, the patient should not only be evaluated organically and technically, but also at the psychological, cognitive, emotional, and social levels which are often significantly disrupted when receiving a diagnosis of serious life-threatening diseases such as cancer. A main component of this new approach to personalized medicine should include optimization of communication between the physician and the patient3 which is fundamental to realizing a shared decision-making model. In order to achieve effective communication, to provide understandable information, and to increase patient understanding so that shared decision making can occur, it is necessary for physicians to have consistent knowledge about the individual patient they are working with. When a physician is knowledgeable about the patient’s physical, psychological, emotional, social, and cognitive status, it is easier to format the structure of the communication/relationship. In studying the benefits associated with high-quality patient/physician communication, Detmar et al4 researched the potential value of communication during medical visits, finding that when the physician was provided with health-related quality of life data from the patient, effective communication was facilitated and more relevant issues were discussed. Other studies have shown the benefits of quality patient/physician communication, reporting that women have been found to feel less anxious and depressed when they feel as if their physician had offered adequate information about their health status.5 In addition, women who have positive experiences with physicians and receive satisfactory information are less likely to refuse conventional medicine and experience less decisional conflict, regret, and psychological distress than the others.6
There is a need for a reliable, ready-to-use patient-profiling tool to be used before the first encounter with a patient which sets the style and informs the communication tone, language, and content of all subsequent doctor–patient discussions. Such a tool will be based on a new multidimensional questionnaire that assesses the breast cancer patient’s physical and mental characteristics in order to provide physicians, prior to the consultation, with a patient’s profile that is supposed to facilitate subsequent communication, interaction, and information delivery between the doctor and the patient.
Two main benefits of constructing a validated questionnaire and a subsequent patient-profiling tool can be identified. On the clinical side, it will serve to optimize information delivery from doctors to patients: doctors, having a patient profile, can rapidly adjust the content and the level of verbal information to the patient’s needs and level of understanding. On the research side, the same tool can be used to automatically identify, through advanced algorithms, the possible clinical trials in which the patient could be enrolled.
Aims
The present study was aimed to develop and validate a new questionnaire for breast cancer patients, which qualitatively and quantitatively assesses the overall physical, psychological, and cognitive status of the patient after the diagnosis. Differently from the existing questionnaires, this questionnaire is not intended to be standalone, but to be the core of the future planned computerized profiling tool that will automatically analyze the individual patients’ answers to generate a patient’s profile. Such a profile should then help the physician to tailor his/her communication style and content in order to meet the patient’s needs and preferences.
This questionnaire is intended to be: 1) short, simple, and user-friendly; 2) psychometrically sound with good validity and reliability; 3) useful both in research and clinical practice; 4) sufficiently sensitive to reliably quantify physical, psychological, and cognitive characteristics of breast cancer patients; and 5) suitable to be administered online so that the patient’s answers can be immediately analyzed by the future dedicated profiling tool. The new questionnaire has been named ALGA-Breast Cancer (ALGA-BC) and is reported, in English and Italian, in Table 1.
Table 1.
The validated version (Italian) and translation in English of the ALGA-BC questionnaire
| Factors | Questions (English version) | Questions (Italian version) | Possible answers | Reversequestions | ||||
|---|---|---|---|---|---|---|---|---|
| GSRH | Compared to others your age, would you say your health is … | Rispetto alla sua età, considera il suo stato di salute come … | Very poor | Poor | Neither poor nor good | Good | Very good | Reverse |
| In general, would you say your health is … | In generale, considera il suo stato di salute come … | Very poor | Poor | Neither poor nor good | Good | Very good | Reverse | |
| Perceived physical health (in the last 4 weeks) | Did you feel tired? | Si è sentito stanco? | Never | Rarely | Sometimes | Often | Always | |
| Did you feel weak? | Si è sentito debole? | Never | Rarely | Sometimes | Often | Always | ||
| Did pain interfere with your daily activities? | La fatica ha interferito con le sue attività quotidiane? | Never | Rarely | Sometimes | Often | Always | ||
| How often were you limited in doing either your work or other daily activities? | Si è sentito limitato nello svolgere il suo lavoro o le atre attività quotidiane? | Never | Rarely | Sometimes | Often | Always | ||
| Did you experience pain? | Ha avuto dolore? | Never | Rarely | Sometimes | Often | Always | ||
| Did you have trouble sleeping? | Ha avuto difficoltà a dormire? | Never | Rarely | Sometimes | Often | Always | ||
| How often were you limited in pursuing your hobbies or other leisure time activities? | Si è sentito limitato nel praticare i suoi passatempi o altre attività di divertimento o svago? | Never | Rarely | Sometimes | Often | Always | ||
| Did you need to rest? | Ha avuto bisogno di riposo? | Never | Rarely | Sometimes | Often | Always | ||
| Anxiety | How anxious do you feel AT THE MOMENT? | Quanto si sente ansioso in questo momento? | Not anxious at all | A little | Moderately | Very anxious | Extremely anxious | |
| How anxious do you USUALLY feel? | Quanto si sente ansioso di solito? | Not anxious at all | A little | Moderately | Very anxious | Extremely anxious | ||
| Self-efficacy | Can you handle unforeseen situations thanks to your resourcefulness? | Ritiene di essere in grado di saper affrontare situazioni impreviste grazie alla sua intraprendenza? | Never | Rarely | Sometimes | Often | Always | Reverse |
| Are you confident that you could deal efficiently with unexpected events? | Ritiene di essere in grado di saper affrontare in modo efficace eventi imprevisti? | Never | Rarely | Sometimes | Often | Always | Reverse | |
| Are you certain that you can accomplish your goals? | E’ sicuro di poter realizzare i suoi obiettivi? | Never | Rarely | Sometimes | Often | Always | Reverse | |
| Can you manage to solve difficult problems if you try hard enough? | Riesce a risolvere problemi difficili se ci prova abbastanza seriamente? | Never | Rarely | Sometimes | Often | Always | Reverse | |
| Can you remain calm when facing difficulties because you can rely on your coping abilities? | Ritiene di essere in grado di saper restare calmo nell’affrontare le difficoltà, perché ha fiducia nelle sue capacità di fronteggiarle? | Never | Rarely | Sometimes | Often | Always | Reverse | |
| If someone opposes you, can you find the means and ways to get what you want? | Se qualcuno la contrasta, riesce a trovare il modo o il sistema per ottenere ciò che vuole? | Never | Rarely | Sometimes | Often | Always | Reverse | |
| Cognitive closure | When you face a problem, do you decide what to do without hesitation and without thinking too much? | Quando deve risolvere un problema, non ci pensa troppo sopra e decide senza esitare? | Never | Rarely | Sometimes | Often | Always | Reverse |
| Do you prefer to decide for the first available solution, rather than reflecting for a long time on a decision? | Preferisce decidere per la prima soluzione disponibile, piuttosto che riflettere a lungo sulla decisione da prendere? | Never | Rarely | Sometimes | Often | Always | Reverse | |
| When you resolve a problem, do you try to not lose time by considering the different points of view? | Quando deve risolvere un problema, in genere non perde tempo a considerare i diversi punti di vista? | Never | Rarely | Sometimes | Often | Always | Reverse | |
| Memory (in the last 4 weeks) | Did you experience completely forgetting to do things you said you would do, and things you planned to do? | Le capita di dimenticare completamente di fare cose che avrebbe dovuto fare o che ha in progetto di fare? | Never | Rarely | Sometimes | Often | Always | |
| Did you forget when something happened; for example, whether it was yesterday or last week? | Ha dimenticato quando si è verificato un certo avvenimento (per esempio se è accaduto ieri oppure la settimana scorsa)? | Never | Rarely | Sometimes | Often | Always | ||
| When talking to someone, did you forget what you have just said? Maybe saying “what was I talking about?” | Parlando con qualcuno, le è capitato di dimenticare ciò che ha appena detto? Dicendo, ad esempio, “di che cosa stavamo parlando”? | Never | Rarely | Sometimes | Often | Always | ||
| Did you check whether you have remembered to do something that you should have done? | Ha controllato se ha fatto ciò che avrebbe dovuto fare? | Never | Rarely | Sometimes | Often | Always | ||
| Body image (in the last 4 weeks) Sexual life (in the last 4 weeks) | Did you find it difficult to look at yourself naked? | Ha avuto difficoltà a guardarsi nudo? | Never | Rarely | Sometimes | Often | Always | |
| Have you been dissatisfied with your body? | Si è sentito insoddisfatto del suo corpo? | Never | Rarely | Sometimes | Often | Always | ||
| To what extent were you sexually active? (with or without intercourse) | In che misura è stato sessualmente attivo (con o senza rapporti sessuali completi)? | Never | Rarely | Sometimes | Often | Always | Reverse | |
| To what extent were you interested in sex? | In che misura ha provato interesse per il sesso? | Never | Rarely | Sometimes | Often | Always | Reverse | |
Note: The last column indicates which are the questions whose scores must be reversed for the analysis.
Abbreviations: ALGA-BC, ALGA-Breast Cancer; GSRH, global self-rated health.
Once validated in breast cancer patients, the ALGA-BC questionnaire will be tested in a sample of healthy subjects, in order to verify if the same factors can be found in the two samples, and if their results are similar or not.
Methods
The development and validation of the ALGA-BC questionnaire occurred in two separate phases (the development procedure and the validation procedure) involving a sample of 100 breast cancer patients. The study was approved by the ethical committee of the hospital were the study was conducted.
The method used for the two steps is described in detail below.
Subjects
Patients recruited for the development and validation of the new questionnaire were drawn from the breast cancer unit of the European Institute of Oncology in Milan, Italy. In order to have a homogenous sample, only the women aged between 18 and 70 years diagnosed with primary breast cancer who had undergone radical surgery between January and October 2014 were consecutively asked to participate in the study. Patients with recurrent breast cancer or with overt psychiatric illness which would interfere with the measurement of psychological variables were excluded from the study (Table 2 for the demographic characteristics of the two samples). The sample size of 100 was determined accordingly to Rattray and Jones7 and Terwee et al.8 Patients included in the study were planned to answer the questionnaire before their first encounter with the medical oncologist.
Table 2.
Demographic characteristics of the two samples (breast cancer patients versus healthy subjects)
| Patients
|
Controls
|
|||
|---|---|---|---|---|
| n | % | n | % | |
| Age | ||||
| <20 years | 1 | 1 | 4 | 1 |
| 20–24 years | 0 | 0 | 72 | 10 |
| 25–29 years | 1 | 1 | 103 | 14 |
| 30–39 years | 13 | 13 | 172 | 24 |
| 40–49 years | 29 | 29 | 171 | 23 |
| 50–60 years | 35 | 35 | 150 | 21 |
| >60 years | 20 | 20 | 58 | 8 |
| Marital status | ||||
| Single | 7 | 7 | 214 | 29 |
| Unmarried partner | 7 | 7 | 111 | 15 |
| Married | 67 | 67 | 357 | 49 |
| Separated or divorced | 12 | 12 | 42 | 6 |
| Widow | 7 | 7 | 6 | 1 |
| Educational level | ||||
| Elementary school | 10 | 10 | 0 | 0 |
| Middle school | 13 | 13 | 6 | 1 |
| High school | 52 | 52 | 71 | 55 |
| University | 23 | 23 | 398 | 10 |
| PhD/specialization | 2 | 2 | 255 | 35 |
A sample of 730 healthy volunteers were randomly selected from the general population. To be included in study, healthy subjects must have been aged between 18 and 70 years and to be healthy (no acute or chronic illness at the moment of the evaluation and no past history of cancer). Healthy subjects also filled out the questionnaire using online survey software and were tested during the same period as cancer patients.
Phase 1: development of the instrument and item pool
The aim of the development phase was to build a questionnaire which included both physical and mental aspects that can play a relevant role in coping with the diagnosis of cancer, or can be altered as a result of receiving the diagnosis. In particular, we wanted to investigate the perceived health and physical state, as well as the psychological and cognitive aspects essential to creating a broad personal patient profile.
Content validity
To achieve content validity and identify representative and relevant items, a literature review was conducted in MEDLINE, searching for validated questionnaires assessing physical, psychological, and cognitive aspects related to breast cancer. In addition, results from informal interviews with breast cancer patients and medical oncologists were used to delineate the most relevant elements which emerge after a cancer diagnosis, and how they influence the patient’s daily life and the way in which she interacts with her physician and elaborates the information provided.
The research group, consisting of experienced psychologists knowledgeable in psychometrics and medical oncologists, created the initial pool of items by using questions carefully selected from a number of validated psychological questionnaires (see the next paragraph) on the basis of their own knowledge and the patient interviews. The items were thereafter evaluated by an expert panel consisting of clinical and cognitive psychologists, medical oncologists, nurses, and breast cancer patients referred for treatment at the European Institute of Oncology. The expert panel was asked to suggest additional items for the item pool if they found any domains or concerns that were not covered. Fifteen randomly selected patients were encouraged to suggest new questions if they thought there were concerns missing at the time of data collection. During the initial and validation phases, patients were also asked for comments on the questionnaires’ readability and understandability. Patients who participated in the informal interviews were the same who were asked to suggest new questions and to evaluate the existing ones. These patients were then excluded from the final questionnaire testing.
As a result of this consultation, three questions about sexual life were added to the original pool of items. The expert panel also gave recommendations for changes to improve clarity and the logical order of the items. The development process resulted in 38 questions about physical and mental status selected, though mostly modified and reformulated, from the following existing and validated questionnaires: European Organization for Research and Treatment of Cancer Quality of Life Questionnaire – Core (EORTC QLQ-C30);9 European Organization for Research and Treatment of Cancer Quality of Life Questionnaire – Breast (EORTC QLQ-BR23);10 Center of Epidemiologic Studies Depression Scale (CES-D);11 Everyday Memory Questionnaire – Revised (EMQ-R);12 General Self-Efficacy Scale (GSE);13 and Need for Cognitive Closure Scale.14
As a final step, the content validity of the questionnaire was evaluated using the content validity index (CVI). A first draft of the instrument in the form of CVI was sent to 20 psychologists and clinical oncologists who were asked to answer using a four-point scale ranging from 1 to 4 (not relevant to highly relevant). According to recommendations in the literature, a level of 0.80 or greater was used as a criterion for demonstrating content validity.15,16 Items receiving a rating less than 0.80 were revised.
Face validity
To determine the face validity, patients were given an evaluation form assessing the questionnaire in terms of feasibility, readability, and consistency of style and formatting. The patients’ preference for completing the questionnaire using an electronic device (iPad) instead of paper-and-pencil support was also assessed.
Phase 2: construct validity and internal consistency reliability
Construct validity answers the question of whether or not the items of an instrument consistently, and with sufficient precision, measure the construct they are supposed to measure.17,18
The sample for factor analysis included 100 Italian women operated for newly diagnosed primary breast cancer who were able to respond to the questionnaire and who expressed their willingness to participate in the study. Patients filled out the questionnaire on an iPad after signing the informed consent form and immediately before their first encounter with the medical oncologist, during which they received the proposal for the subsequent courses of treatment, based on targeted chemotherapy and/or endocrine therapy and/or radiotherapy. When completing the questionnaire, patients were not aware of their final (post-surgical) diagnosis. A psychologist was in attendance to answer any questions from the patient during the questionnaire completion.
Most of the questions referred to the last 2 or 4 weeks (as indicated in the questionnaire), except those regarding “state-trait anxiety”, “self efficacy”, and “cognitive closure” which are supposed to be almost stable along time (Figure 1 for a flowchart of the data collection).
Figure 1.
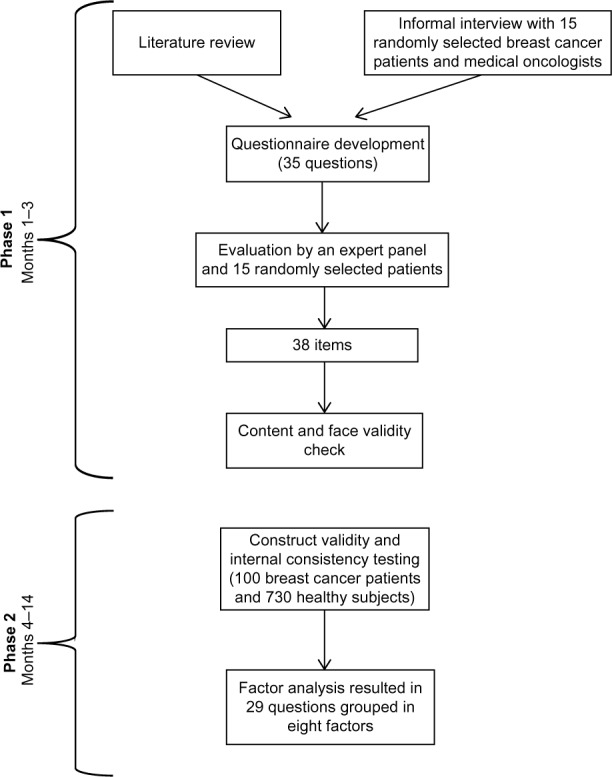
The research process starting from the development of the questionnaire to data collection and analysis.
In a future study, the results will be automatically processed according to a scoring system and then forwarded by Internet to the physician ahead of the interview with the patient.
In order to assess the factor structure of the core item set, principal components analysis with varimax rotation was performed. A principal factors method, which entails no distributional assumptions, was used to fit the common factor model to the data. A rotated principal factors extraction was performed on all items to estimate the number of factors to retain.19–22
The scree plot of ordered eigenvalues of a correlation matrix was used to decide the appropriate number of factors extracted. Items were eliminated based on low factor loading. Loading magnitudes were considered unacceptably low if they were less than 0.50.23
Next, scores were calculated for each participant by summing the item scores identified for each factor and dividing by the total number of items.
Internal consistency analysis was performed separately on items comprising each of the factors identified evaluating Cronbach’s alpha.
To evaluate the goodness of fit between the models and data, we used fit indices, including the standardized root-mean-square residuals, comparative fit index, and root mean square error of approximation (RMSEA) that indicates the amount of unexplained variance. A sufficient model fit was defined as the standardized root-mean-square residual of 0.08 or less, comparative fit index of 0.90 or greater, and RMSEA of 0.06 or less.
Predictions for discriminative and divergent validity were made based on a literature review. Differences were evaluated between patient age groups, level of education, marital status, the presence of children (ie, if a woman had ever given birth to any children), a past history of cancer diseases, and the presence of past or present psychological treatments. One-way analysis of variance tests were used to investigate the relationships between scores and the above sociodemographic variables. Residuals from full models, investigating factor variations, were checked to assess normal distribution.
Finally, we checked if the scores of factors obtained considering cancer cases were significantly different between patients and healthy subjects (individuals with no history of cancer diseases who completed the same version of the questionnaire) and also if factors obtained analyzing the controls’ responses separately were different from the ones obtained including only cancer patients.
Results
Patient sociodemographics
Data were analyzed using the statistical software SAS, version 9.2.
Forty-four percent of the 100 patients included in the study were aged less than 50 years. Most of the subjects were married or lived with a partner (74%), had children (84%), and had attended high school (75%). Sixteen of them had received or were receiving psychological treatment at the moment of evaluation. For 90 of them it was the first diagnosis of cancer, while ten had already had a previous cancer.
The sample of healthy subjects included 730 volunteers, who completed the questionnaire online, and of whom 293 (40%) were women. The majority of the controls (n=522, 72%) were 50 years old or older (14% were young adults, 30 or less years old), had a university degree (n=653, 45%), and were married or lived with a partner (n=468, 64%). Half of the sample had children, and a quarter (25%, n=186) had asked at least once in their life for psychological counseling (Table 2 for a summary of the demographic characteristics of the two samples).
Content validity
The total ALGA-BC scale showed good content validity (CVI =0.96).
Face validity
Ninety-six percent of respondents found the questions easy to answer and clearly understandable. They also found the appearance and layout acceptable, each parameter being evaluated at 3 or 4 on a Likert scale of 1–4.
After this first evaluation phase, all the 38 initial items were included in the questionnaire.
Construct validity
The Bartlett’s test of sphericity,9,24,25 used to verify the assumption that variances are equal across groups or samples, was highly significant (P=0.006), indicating that the distribution of data met the psychometric criteria for exploratory factor analysis to proceed. The scree test of eigenvalues plotted against factors suggested an eight-factor solution, explaining 98% of the variance. The measure of sampling adequacy is good (0.76).
We obtained satisfactory Cronbach’s alphas, greater than 0.70 (for factor 3), and higher than 0.90 for factors 1 and 7. Deleting an item from the analysis would not substantially improve the overall Cronbach’s for any scale. These values indicate a good reliability of the test.
Finally, an excellent average inter-item correlation greater than 0.40 was found.
Substantive interpretation of the pattern of factor loadings resulted in the labels “global self-rated health”, “perceived physical health”, “anxiety”, “self efficacy”, “cognitive closure”, “memory”, “body image”, and “sexual life”, keeping 29 items out of the initial 38.
The eight factors are explained as follows:
Factor 1: “global self-rated health”. This factor includes two items that focus on how patients consider their health status in general and relatively to their age.26 Measures of global self-rated health have been proved to have significant clinical value in cancer care.27
Factor 2: “perceived physical health” (eight items). These items focus on fatigue, weakness, physical limitations, pain, and sleep problems concomitant to the illness. It has been observed that patients who report more perceived health problems after a cancer diagnosis have more posttraumatic stress symptoms and a compromised health-related quality of life.28,29
Factor 3: “anxiety”. These two items investigate the state anxiety (anxiety about a specific event) versus trait anxiety (anxiety as a personal characteristic) perceived by patients.30 Anxiety associated with cancer may increase feelings of pain, cause nausea and vomiting, and interfere with the ability to sleep and with the patient’s quality of life in general. It can also alter the patient’s cognitive abilities, such as memory and attention, reducing her ability to understand information given by the physician.31–33 In cancer patients, feelings of anxiety may increase or decrease at different times so the variation between the reference point (usual level of anxiety) and the actual level of anxiety is important to understanding the real status of the patient and how it varies along time.
Factor 4: “self efficacy” (six items). This factor refers to “a broad and stable sense of personal competence to deal effectively with a variety of stressful situations”.34 Individuals possessing a high level of self-efficacy are optimistic and self-confident in their own coping abilities when confronted with life stressors such as a diagnosis of cancer. A strong sense of self-efficacy was found to be generally correlated with better health. On the contrary, a low sense of self-efficacy is associated with depression and anxiety.35,36 This makes the dimension of self-efficacy crucial in the context of cancer care.
Factor 5: “cognitive closure”. This factor includes three items investigating the individual’s tendency to seek out information when they have to make a decision.37,38 Cognitive closure is a dispositional construct that is referred to as a latent variable manifested through several different aspects including the desire for predictability, the discomfort with ambiguity, and close-mindedness. In medical contexts, cognitive closure is related to the patient’s preference for the amount of information she wishes to receive about illness, treatment, etc. The assessment of cognitive closure might thus assist the physician in his/her decision on how much information should be best provided in order for the patient to make an informed choice.
Factor 6: “memory”. This factor is made up of four items that explore the mnestic abilities of patients. Difficulties in the ability to remember, think, and concentrate are often reported by breast cancer patients as a consequence of treatment or because of the excessive level of stress and worries.39 Next to the immediate impact of impairments in memory on the quality of life, memory and concentration problems might also result in the patient’s lowered chance of actively participating in the medical and treatment-decision process.40 By previously informing the physician about the patient’s memory and attention problems, he/she might be able to adjust his/her way of communicating with the patient, thus ensuring shared decision making.
Factor 7. In breast cancer patients, own body image may often change due to physical and psychological reasons, worsening women’s living.41 This factor (two items), called “body image”, investigates the level of acceptance and satisfaction the patient has regarding her body.
Factor 8: “sexual life”. These two items ask for the recent general interest in sex and the extent to which patients have been sexually active. Investigating body image and sexual problems might be especially important in breast cancer patients, as these dimensions are strongly influenced by changes in female bodies resulting from surgery, radiotherapy, and chemotherapy.42
Finally, analyzing the sample of healthy subjects separately, the factor “anxiety” disappeared, while another factor, called “rumination”, emerged. Rumination indicates the tendency to compulsively focus attention on negative thoughts, instead of searching for solutions. Rumination is similar to worry except it focuses on bad feelings and experiences from the past, whereas worry is concerned with potential bad events in the future. Rumination is usually associated with anxiety and other negative emotional states.
Most of the questions referred to the last 2 or 4 weeks (as indicated in the questionnaire), except those regarding the “self efficacy” and the “cognitive closure” factors which are supposed to be almost stable along time.
Descriptive analyses of the scores by sociodemographic variables are provided in Table 3 with results of analysis of variance tests. As it can be observed, “perceived physical health” scores were significantly lower for “at least university” than for high school (P=0.02), indicating that higher education contributes to a better perception of physical conditions; “anxiety” was significantly higher for mothers than for women without children (P=0.007); “memory”, “anxiety”, and “body image” scores were significantly higher for women with a history of psychological treatments (P=0.015, P=0.003, and P=0.007, respectively); “global self-rated health” was borderline significantly better among the ten women with a history of cancer than in others; and “cognitive closure” looked greater at older ages (P=0.02).
Table 3.
Median and interquartile range of factors
| n | Variable | Median | Lower quartile | Upper quartile | P-values | |
|---|---|---|---|---|---|---|
| Marital status | ||||||
| Married/living with partners | 74 (74%) | Physical state | 2.88 | 2.38 | 3.38 | |
| Self-efficacy | 3.00 | 2.17 | 3.67 | |||
| Memory-attention | 1.75 | 1.25 | 2.50 | |||
| Anxiety | 6.00 | 4.50 | 7.00 | |||
| Body image | 2.00 | 1.50 | 3.00 | |||
| Cognitive closure | 3.00 | 2.00 | 3.33 | |||
| GSRH | 2.00 | 1.50 | 2.75 | |||
| Sexual life | 3.00 | 2.00 | 4.00 | |||
| Single/divorced/widow | 26 (26%) | Physical state | 2.44 | 2.00 | 3.38 | |
| Self-efficacy | 2.83 | 2.17 | 3.50 | |||
| Memory-attention | 2.00 | 1.25 | 2.75 | |||
| Anxiety | 4.50 | 2.50 | 7.00 | |||
| Body image | 2.00 | 1.00 | 3.00 | |||
| Cognitive closure | 3.17 | 2.00 | 4.00 | |||
| GSRH | 2.00 | 1.50 | 2.25 | |||
| Sexual life | 3.50 | 3.00 | 4.50 | |||
| Educational level | ||||||
| High school | 75 (75%) | Perceived physical health | 3.00 | 2.38 | 3.50 | 0.02 |
| Self-efficacy | 3.00 | 2.17 | 3.67 | |||
| Memory | 1.75 | 1.25 | 2.50 | |||
| Anxiety | 6.00 | 3.50 | 7.00 | |||
| Body image | 2.00 | 1.00 | 3.00 | |||
| Cognitive closure | 3.00 | 2.00 | 3.67 | |||
| GSRH | 2.00 | 1.50 | 2.75 | |||
| Sexual life | 3.00 | 2.00 | 4.00 | |||
| At least university | 25 (25%) | Perceived physical health | 2.38 | 1.63 | 2.88 | |
| Self-efficacy | 2.67 | 2.00 | 3.75 | |||
| Memory | 1.88 | 1.38 | 3.13 | |||
| Anxiety | 5.25 | 4.50 | 6.50 | |||
| Body image | 2.00 | 1.50 | 2.75 | |||
| Cognitive closure | 2.67 | 2.17 | 3.83 | |||
| GSRH | 2.00 | 1.00 | 2.50 | |||
| Sexual life | 3.00 | 2.50 | 4.00 | |||
| Children | ||||||
| Yes | 84 (84%) | Perceived physical health | 2.88 | 2.25 | 3.50 | |
| Self-efficacy | 3.00 | 2.17 | 3.67 | |||
| Memory | 1.75 | 1.25 | 2.75 | |||
| Anxiety | 6.00 | 4.00 | 7.00 | 0.007 | ||
| Body image | 2.00 | 1.50 | 3.00 | |||
| Cognitive closure | 3.00 | 2.00 | 3.67 | |||
| GSRH | 2.00 | 1.50 | 2.75 | |||
| Sexual life | 3.00 | 2.00 | 4.00 | |||
| No | 16 (16%) | Perceived physical health | 2.31 | 1.56 | 3.38 | |
| Self-efficacy | 2.75 | 2.17 | 3.58 | |||
| Memory | 2.00 | 1.25 | 2.50 | |||
| Anxiety | 4.50 | 2.75 | 6.00 | |||
| Body image | 2.00 | 1.00 | 2.75 | |||
| Cognitive closure | 3.33 | 2.17 | 4.00 | |||
| GSRH | 1.63 | 1.25 | 2.25 | |||
| Sexual life | 3.25 | 2.75 | 4.00 | |||
| Psychological treatments | ||||||
| Yes | 16 (16%) | Perceived physical health | 3.06 | 2.00 | 3.75 | |
| Self-efficacy | 3.00 | 2.42 | 3.75 | |||
| Memory | 2.75 | 1.75 | 3.13 | 0.015 | ||
| Anxiety | 7.00 | 4.50 | 8.75 | 0.003 | ||
| Body image | 2.75 | 2.00 | 3.75 | 0.007 | ||
| Cognitive closure | 2.50 | 1.67 | 4.17 | |||
| GSRH | 2.25 | 1.50 | 2.63 | |||
| Sexual life | 3.50 | 3.00 | 4.00 | |||
| No | 81 (81%) | Perceived physical health | 2.75 | 2.13 | 3.38 | |
| Self-efficacy | 2.83 | 2.17 | 3.67 | |||
| Memory | 1.75 | 1.25 | 2.50 | |||
| Anxiety | 5.50 | 3.50 | 6.50 | |||
| Body image | 2.00 | 1.00 | 3.00 | |||
| Cognitive closure | 3.00 | 2.33 | 3.67 | |||
| GSRH | 2.00 | 1.50 | 2.75 | |||
| Sexual life | 3.00 | 2.00 | 4.00 | |||
| Smoking | ||||||
| Yes | 14 (14%) | Perceived physical health | 2.75 | 2.13 | 3.63 | |
| Self-efficacy | 3.00 | 2.67 | 3.50 | 0.002 | ||
| Memory | 1.75 | 1.25 | 2.50 | |||
| Anxiety | 5.75 | 3.50 | 7.00 | |||
| Body image | 2.75 | 2.00 | 4.00 | |||
| Cognitive closure | 3.50 | 3.00 | 4.33 | 0.03 | ||
| GSRH | 2.00 | 1.50 | 2.75 | |||
| Sexual life | 3.00 | 2.50 | 4.00 | |||
| No | 76 (76%) | Perceived physical health | 2.88 | 2.00 | 3.50 | |
| Self-efficacy | 3.17 | 2.17 | 3.83 | |||
| Memory | 2.00 | 1.25 | 2.75 | |||
| Anxiety | 6.00 | 4.50 | 7.00 | |||
| Body image | 2.00 | 1.50 | 3.00 | |||
| Cognitive closure | 2.67 | 2.00 | 3.67 | |||
| GSRH | 2.00 | 1.50 | 2.75 | |||
| Sexual life | 3.00 | 2.00 | 4.00 | |||
| Ex-smoker (?) | 10 (10%) | Perceived physical health | 2.75 | 2.63 | 3.00 | |
| Self-efficacy | 2.00 | 1.50 | 2.33 | |||
| Memory | 1.50 | 1.25 | 2.50 | |||
| Anxiety | 4.50 | 2.00 | 6.00 | |||
| Body image | 1.75 | 1.00 | 3.00 | |||
| Cognitive closure | 3.00 | 2.00 | 3.33 | |||
| GSRH | 1.88 | 1.50 | 2.25 | |||
| Sexual life | 3.75 | 3.00 | 4.00 | |||
| Physical activity | ||||||
| Yes | 36 (36%) | Perceived physical health | 2.69 | 2.00 | 3.38 | |
| Self-efficacy | 3.08 | 2.00 | 3.75 | |||
| Memory | 2.00 | 1.50 | 2.75 | |||
| Anxiety | 6.25 | 4.50 | 7.25 | |||
| Body image | 2.50 | 1.50 | 3.00 | |||
| Cognitive closure | 3.00 | 2.00 | 3.83 | |||
| GSRH | 1.88 | 1.25 | 2.38 | |||
| Sexual life | 3.00 | 2.50 | 3.50 | |||
| No | 64 (64%) | Perceived physical health | 2.88 | 2.25 | 3.63 | |
| Self-efficacy | 2.83 | 2.17 | 3.50 | |||
| Memory | 1.75 | 1.25 | 2.50 | |||
| Anxiety | 5.00 | 3.00 | 7.00 | |||
| Body image | 2.00 | 1.00 | 3.00 | |||
| Cognitive closure | 3.00 | 2.33 | 3.67 | |||
| GSRH | 2.00 | 1.50 | 2.75 | |||
| Sexual life | 3.00 | 2.00 | 4.00 | |||
| Personal history of cancer | ||||||
| Yes | 10 (10%) | Perceived physical health | 3.50 | 2.00 | 3.75 | |
| Self-efficacy | 3.67 | 3.17 | 3.83 | |||
| Memory | 2.75 | 1.75 | 2.75 | |||
| Anxiety | 6.50 | 4.50 | 6.50 | |||
| Body image | 2.50 | 1.50 | 4.00 | |||
| Cognitive closure | 2.67 | 2.00 | 3.00 | |||
| GSRH | 2.50 | 2.00 | 2.75 | 0.07 | ||
| Sexual life | 3.00 | 3.00 | 4.00 | |||
| No | 90 (90%) | Perceived physical health | 2.75 | 2.13 | 3.38 | |
| Self-efficacy | 2.83 | 2.17 | 3.67 | |||
| Memory | 1.75 | 1.25 | 2.50 | |||
| Anxiety | 5.50 | 4.00 | 7.00 | |||
| Body image | 2.00 | 1.50 | 3.00 | |||
| Cognitive closure | 3.00 | 2.33 | 4.00 | |||
| GSRH | 2.00 | 1.50 | 2.50 | |||
| Sexual life | 3.00 | 2.00 | 4.00 | |||
| Age | ||||||
| ≤40 years | 15 | Perceived physical health | 3.00 | 1.75 | 3.75 | |
| Self-efficacy | 3.00 | 2.00 | 3.67 | |||
| Memory | 2.00 | 1.25 | 3.50 | |||
| Anxiety | 5.00 | 2.50 | 6.50 | |||
| Body image | 2.00 | 1.50 | 2.50 | |||
| Cognitive closure | 2.67 | 2.00 | 3.33 | 0.02 | ||
| GSRH | 2.00 | 1.50 | 2.50 | |||
| Sexual life | 3.00 | 2.50 | 4.00 | |||
| 50 years | 29 | Perceived physical health | 2.75 | 2.38 | 3.50 | |
| Self-efficacy | 3.17 | 2.00 | 3.67 | |||
| Memory | 2.00 | 1.50 | 2.50 | |||
| Anxiety | 5.00 | 4.00 | 6.50 | |||
| Body image | 2.50 | 1.50 | 3.50 | |||
| Cognitive closure | 2.67 | 2.00 | 3.33 | |||
| GSRH | 2.00 | 1.25 | 2.50 | |||
| Sexual life | 3.00 | 2.00 | 3.50 | |||
| 60 years | 35 | Perceived physical health | 2.88 | 2.00 | 3.38 | |
| Self-efficacy | 2.67 | 2.17 | 3.50 | |||
| Memory | 1.63 | 1.25 | 2.50 | |||
| Anxiety | 6.00 | 4.50 | 7.00 | |||
| Body image | 2.00 | 1.00 | 3.00 | |||
| Cognitive closure | 3.33 | 2.67 | 4.00 | |||
| GSRH | 2.00 | 1.50 | 2.75 | |||
| Sexual life | 3.00 | 2.00 | 4.00 | |||
| ≥70 years | 20 | Perceived physical health | 2.75 | 2.44 | 3.50 | |
| Self-efficacy | 2.92 | 2.42 | 3.83 | |||
| Memory | 1.63 | 1.00 | 2.63 | |||
| Anxiety | 6.25 | 3.50 | 7.75 | |||
| Body image | 2.00 | 1.00 | 3.00 | |||
| Cognitive closure | 2.83 | 2.33 | 4.33 | |||
| GSRH | 1.88 | 1.25 | 2.88 | |||
| Sexual life | 3.00 | 1.50 | 4.00 | |||
Abbreviation: GSRH, global self-rated health.
Face validity
The questionnaire was considered easy to complete by 88% of subjects, and not too long by 72%, and the questions were judged pertinent by 85%.
Most of the subjects (87%) preferred to complete the questionnaire using an electronic device instead of using the paper-and-pencil version.
Test–retest reliability
The test–retest reliability of the instrument was calculated testing ten patients who repeated the questionnaire 2 weeks after the first administration. Test–retest reliability was 0.90 (P<0.001).
Comparison between cancer patients and healthy subjects
Comparing the scores obtained by cancer patients with those from healthy subjects, we observed, as expected, significant differences in the following factor names: perceived physical health, self-efficacy, anxiety, cognitive closure, global self-rated health, sexual life, and rumination (Table 4). All these factors were higher in patients than controls, indicating that:
patients perceive their physical health and sexual life as worse than healthy subjects do;
patients experience a higher level of anxiety and a lower level of self-efficacy compared to healthy subjects;
patients have higher cognitive closure compared to healthy subjects; and
patients ruminate more than healthy subjects.
Table 4.
Comparison between patients and healthy subjects
| Variable | Median | Lower quartile | Upper quartile | P-values |
|---|---|---|---|---|
| Cases (n=100) | ||||
| Physical state | 2.9 | 2.1 | 3.4 | 0.0003 |
| Self-efficacy | 3.0 | 2.2 | 3.7 | <0.0001 |
| Memory-attention | 1.8 | 1.3 | 2.5 | 0.197 |
| Body image | 2.0 | 1.5 | 3.0 | 0.751 |
| Cognitive closure | 3.0 | 2.0 | 3.7 | <0.0001 |
| GSRH | 2.0 | 1.5 | 2.8 | <0.0001 |
| Sexual life | 3.0 | 2.0 | 4.0 | 0.002 |
| Anxiety | 2.0 | 1.3 | 3.0 | <0.0001 |
| Rumination | 5.5 | 4.0 | 7.0 | 0.017 |
| Controls (n=730) | ||||
| Physical state | 2.5 | 2.0 | 3.0 | |
| Self-efficacy | 2.2 | 2.0 | 2.5 | |
| Memory-attention | 2.0 | 1.5 | 2.5 | |
| Body image | 2.0 | 1.5 | 3.0 | |
| Cognitive closure | 3.3 | 3.0 | 4.0 | |
| GSRH | 1.5 | 1.0 | 2.0 | |
| Sexual life | 2.5 | 2.0 | 3.0 | |
| Anxiety | 3.5 | 2.0 | 5.0 | |
| Rumination | 1.7 | 1.3 | 2.7 | |
Abbreviation: GSRH, global self-rated health.
Discussion
The present study describes the development and validation of a disease-specific questionnaire for breast cancer patients which qualitatively and quantitatively assesses the overall physical, psychological, and cognitive status of the patient.
In order to cover the relevant areas of the influence of a cancer diagnosis on physical, psychological, and cognitive domains, items were chosen from discussions with patients, suggestions by experienced health care professionals, and literature review. Being asked to provide feedback on the topics included and the readability of the questions, both patients and physicians gave a significant contribution to the preparation of the questionnaire.
Content validity was guaranteed using the CVI method, which showed a good score for the total scale,15,16 while the lack of missing data from the 100 interviewed patients indicates that the ALGA-BC questionnaire is relevant and not too difficult to complete or burdensome. Moreover, patients showed a clear preference for completing the questionnaire on the iPad, compared to the paper-and-pencil version, regardless of their age and educational level. These are encouraging and important data, considering that the electronic version is necessary for the future development of the tool, which will automatically generate the patient’s profile to be sent to physicians, perhaps in the form of a graphic report, to help them to have an immediate insight into the patient’s characteristics.
From a statistical point of view, the ALGA-BC scale shows significant evidence of validity and reliability. The item-total correlations for the total scale is high. This indicates that the 29 items included in the eight key factors measure the same concept and that none of them fulfilled the criteria for removal. These findings are confirmed by the CFAs. The CFA analyses show that the eight-factor model has strong factor loadings and satisfactory goodness-of-fit values.
In terms of psychometric characteristics, this first evaluation suggests that the ALGA-BC questionnaire is a promising instrument for breast cancer patient profiling. In fact, even if the authors are aware that the ALGA-BC questionnaire does not completely cover all the patients’ needs and concerns, the eight factors that emerged from the factor analysis represent the critical areas that are useful for physicians’ understanding of the patients’ strengths and weaknesses in order to personalize their interaction and communication style. In particular, the “global self-rated health” and the “perceived physical health” factors are useful for understanding how the patient perceives and judges her health and how she reports her physical symptoms, giving the oncologist important information that completes the objective clinical evaluation. The factors “anxiety” and “self efficacy” indicate whether the patient tends to be psychologically overwhelmed by the disease and if she shows adequate self-confidence in her coping abilities when confronted with life stressors such as the diagnosis of cancer. “Cognitive closure” informs the physician about the amount of information the patient wishes to receive about illness and treatment, while “memory” indicates if patients are able (or feel able) to remember a lot of input or not. Finally, even if it appears as a separate factor only in the healthy subjects sample, the factor “rumination” strongly indicates that patients are more prone than controls to focus attention on negative thoughts, instead of searching for positive solutions. Such information will help the physician to approach the patient according to her needs and preferences, taking into account her difficulties and limitations in order to not overload her with unsuitable or counterproductive data. The last two factors (“body image” and “sexual life”) are particularly important when a diagnosis of breast cancer occurs and need to be taken into account by physicians, who should be responsible not only for treating the disease, but also for treating the patient as an individual with specific (and often very relevant) needs and worries.
Regarding the observed influences of the sociodemographic variables, at least on some of the eight factors, they must be taken into account when generating the single patient’s profile. In particular, it appears that patients with a high educational level consider their health status better than those with lower education. We cannot exclude that the association between “educational level” and “perceived physical health” scores may reflect real differences in health, and not just the subjects’ perceptions of their physical conditions. Nevertheless, a possible explanation is that, regardless of the real differences in health among them, the patients’ knowledge about treatment options makes them more optimistic about their health status.
Being mothers makes patients more vulnerable to anxiety, presumably because of the worry related to the children’s care. A previous or current psychological treatment is related to increased anxiety, worse body image perception, and a decrease in memory (that is also common in different psychological disturbances), while, when women experience a diagnosis of cancer for the second time, they tend to consider their global health better than patients who are at their first diagnosis, probably because they have already experienced similar symptoms in the past. Finally, older patients tend to show higher cognitive closure than younger patients, indicating that they need more time and more information when they have to make a decision.
Comparing breast cancer patients with healthy subjects, we observed that patients show worse perceived physical health and sexual life, lower self-efficacy, higher cognitive closure, and higher rumination than healthy subjects. These expected differences confirm that the ALGA questionnaire is a good instrument for discriminating between cancer patients and healthy subjects, at least on the examined variables.
This approach, based on patient profiling, is supposed to improve the patient–physician relationship as well as the patient’s compliance, and to increase her participation in the medical decision making. Moreover, this information is also an important predictor of the patient’s future quality of life and health, being related to the way in which the patient copes with the disease. With the help of ALGA-BC, oncologists are recommended to put their attention on the mental effects of the disease or treatment and eventually recommend the patient to refer to other specialists to cope with them.
Obviously, ALGA-BC is not intended to provide an exhaustive psychological diagnosis nor to assess the presence of psychiatric disorders that are usually assessed against the “gold standard” of diagnosis by interview or, as second best, against a proxy gold standard of another questionnaire which has proven itself for this purpose, but to generally evaluate physical, psychological, and cognitive reactions related to breast cancer. In our opinion, such a kind of assessment is an important step in achieving real personalized care for cancer patients that overcomes the limitations imposed by a purely biological and genetic approach.43 Cancer is increasingly prevalent, being a strain on the health care system and a source of significant impairment for patients. This evidence highlights the public health magnitude of cancer and the importance of efforts to characterize and address the health concerns of cancer patients. Cancer experience is a complex phenomenon that impacts all aspects of the patient’s life, including her physical, emotional, and psychological health,44 as shown by the fact that cancer patients and healthy subjects obtained significantly different scores in most of the factors. However, to date, there are no available, easy-to-use tools that directly help oncologists to understand such effects or how they can be different from one patient to the others. Not surprisingly, the need for developing the ALGA-BC questionnaire (and the related tool, which is now being developed in our lab) arose from clinical oncologists who expressed their difficulties in finding an efficient way to interact with their patients, especially during the first encounter, being pressed by time constraints that is often not fully understood or misinterpreted by the patients themselves.
Of course, the present study presents some limitations. First of all, some psychometric properties such as the responsiveness or sensitivity to change of the questionnaire were not studied. Such properties are important and must be investigated in another study. Moreover, some statistical methods such as principal component analysis need a lot of patients to be realized: so the psychometric properties of the final questionnaire (with the 29 items retained) should be studies in further studies with an adequate sample size. Finally, to assess the criterion validity, and to verify the accuracy of the instrument, results obtained by the ALGA questionnaire should be compared with those obtained by other validated questionnaires. This step has not been yet conducted due to the difficulty of asking patients to complete more than one questionnaire before their encounter with the physician and must be included in future studies.
Conclusion
Considering the increasing incidence of cancer worldwide, the limits imposed by health care systems regarding the time physicians can spend with their patients, and the need to provide improved patient care, this study provides a validated questionnaire that allows personalization of the medical approach that takes into account the patient’s physical and mental aspects, as well as the purely genetic and clinical ones. The ALGA-BC questionnaire is valid, reliable, and able to find out psychological alterations in breast cancer patients. For these reasons, we argue that it can be included in new decision support tools for physicians, to assist both in clinical practice and research.
Figure 2.
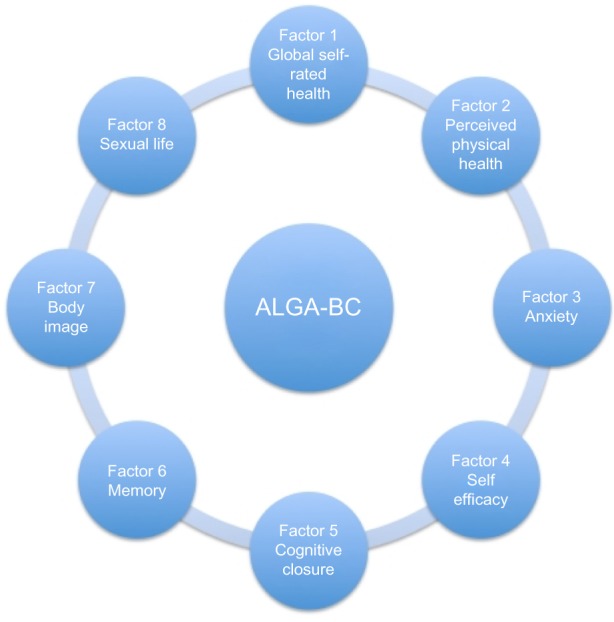
The eight factors included in the ALGA-Breast Cancer (ALGA-BC) questionnaire.
Acknowledgments
This work was supported by the European Union ICT Program (Project “p-medicine – from data sharing and integration via VPH models to personalized medicine” FP7-ICT-2009.5.3).
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Aspinall MG, Hamermesh RG. Realizing the promise of personalized medicine. Harv Bus Rev. 2007;85(10):108–117. 165. [PubMed] [Google Scholar]
- 2.Peppercorn JM, Smith TJ, Helft PR, et al. American Society of Clinical Oncology American society of clinical oncology statement: toward individualized care for patients with advanced cancer. J Clin Oncol. 2011;29(6):755–760. doi: 10.1200/JCO.2010.33.1744. [DOI] [PubMed] [Google Scholar]
- 3.Epstein RM, Franks P, Fiscella K, et al. Measuring patient-centered communication in patient-physician consultations: theoretical and practical issues. Soc Sci Med. 2005;61(7):1516–1528. doi: 10.1016/j.socscimed.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 4.Detmar SB, Muller MJ, Schornagel JH, Wever LD, Aaronson NK. Health-related quality-of-life assessments and patient-physician communication: a randomized controlled trial. JAMA. 2002;288(23):3027–3034. doi: 10.1001/jama.288.23.3027. [DOI] [PubMed] [Google Scholar]
- 5.Trudel JG, Leduc N, Dumont S. Perceived communication between physicians and breast cancer patients as a predicting factor of patients’ health-related quality of life: a longitudinal analysis. Psychooncology. 2014;23(5):531–538. doi: 10.1002/pon.3442. [DOI] [PubMed] [Google Scholar]
- 6.Citrin DL, Bloom DL, Grutsch JF, Mortensen SJ, Lis CG. Beliefs and perceptions of women with newly diagnosed breast cancer who refused conventional treatment in favor of alternative therapies. Oncologist. 2012;17(5):607–612. doi: 10.1634/theoncologist.2011-0468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rattray J, Jones MC. Essential elements of questionnaire design and development. J Clin Nurs. 2007;16(2):234–243. doi: 10.1111/j.1365-2702.2006.01573.x. [DOI] [PubMed] [Google Scholar]
- 8.Terwee CB, Bot SD, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42. doi: 10.1016/j.jclinepi.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 9.Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5):365–376. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- 10.Sprangers MA, Groenvold M, Arraras JI, et al. The European Organization for Research and Treatment of Cancer breast cancer-specific quality-of-life questionnaire module: first results from a three-country field study. J Clin Oncol. 1996;14(10):2756–2768. doi: 10.1200/JCO.1996.14.10.2756. [DOI] [PubMed] [Google Scholar]
- 11.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 12.Royle J, Lincoln NB. The Everyday Memory Questionnaire-revised: development of a 13-item scale. Disabil Rehabil. 2008;30(2):114–121. doi: 10.1080/09638280701223876. [DOI] [PubMed] [Google Scholar]
- 13.Schwarzer R, Jerusalem M, Weinman J, Wright S, Johnston M. Measures in Health Psychology: A User’s Portfolio. Windsor: Nfer-Nelson; 1995. Generalized self-efficacy scale; pp. 35–37. [Google Scholar]
- 14.Kruglanski AW, Atash MN, DeGrada E, Mannetti L, Pierro A, Webster DM. Psychological theory testing versus psychometric nay-saying: comment on Neuberg et al’s (1997) critique of the need for closure scale. J Pers Soc Psychol. 1997;73(5):1005–1016. doi: 10.1037//0022-3514.73.5.1005. discussion 1017–1029. [DOI] [PubMed] [Google Scholar]
- 15.Polit DF, Beck CT. The content validity index: are you sure you know what’s being reported? Critique and recommendations. Res Nurs Health. 2006;29(5):489–497. doi: 10.1002/nur.20147. [DOI] [PubMed] [Google Scholar]
- 16.Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res Nurs Health. 2007;30(4):459–467. doi: 10.1002/nur.20199. [DOI] [PubMed] [Google Scholar]
- 17.Kane M. Current concerns in validity theory. Journal of Educational Measurement. 2001;38:319–342. [Google Scholar]
- 18.DeVon HA, Block ME, Moyle-Wright P, et al. A psychometric toolbox for testing validity and reliability. J Nurs Scholarsh. 2007;39(2):155–164. doi: 10.1111/j.1547-5069.2007.00161.x. [DOI] [PubMed] [Google Scholar]
- 19.Fabrigar LR, Wegener DT, MacCallum RC, Strahan EJ. Evaluating the use of exploratory factor analysis in psychological research. Psychol Methods. 1999;4:272–299. [Google Scholar]
- 20.Horn JL. A rationale and test for the number of factors in factor analysis. Psychometrika. 1965;30:179–185. doi: 10.1007/BF02289447. [DOI] [PubMed] [Google Scholar]
- 21.Zwick WR, Velicer WF. Comparison of five rules for determining the number of components to retain. Psychol Bull. 1986;99:432–442. [Google Scholar]
- 22.Guilford JP. Factor analysis in a test-development program. Psychol Rev. 1948;55:79–94. doi: 10.1037/h0056564. [DOI] [PubMed] [Google Scholar]
- 23.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55. [Google Scholar]
- 24.Bartlett MS. Properties of sufficiency and statistical tests. (Series A).Proceedings of the Royal Statistical Society. 1937;160:268–282. [Google Scholar]
- 25.Snedecor GW, Cochran WG. Statistical Methods. 8th ed. Ames: Iowa State University Press; 1989. [Google Scholar]
- 26.DeSalvo KB, Fisher WP, Tran K, Bloser N, Merrill W, Peabody J. Assessing measurement properties of two single-item general health measures. Qual Life Res. 2006;15(2):191–201. doi: 10.1007/s11136-005-0887-2. [DOI] [PubMed] [Google Scholar]
- 27.Shadbolt B, Barresi J, Craft P. Self-rated health as a predictor of survival among patients with advanced cancer. J Clin Oncol. 2002;20(10):2514–2519. doi: 10.1200/JCO.2002.08.060. [DOI] [PubMed] [Google Scholar]
- 28.Taylor N, Absolom K, Snowden J, Eiser C, Late Effects Group Sheffield Need for psychological follow-up among young adult survivors of childhood cancer. Eur J Cancer Care (Engl) 2012;21(1):52–58. doi: 10.1111/j.1365-2354.2011.01281.x. [DOI] [PubMed] [Google Scholar]
- 29.Arden-Close E, Absolom K, Greenfield DM, Hancock BW, Coleman RE, Eiser C, Late Effects Group Sheffield Gender differences in self-reported late effects, quality of life and satisfaction with clinic in survivors of lymphoma. Psychooncology. 2011;20(11):1202–1210. doi: 10.1002/pon.1835. [DOI] [PubMed] [Google Scholar]
- 30.Spielberger CD, Gorssuch RL, Lushene PR, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Consulting Psychologists Press, Inc; 1983. [Google Scholar]
- 31.Patrick DL, Ferketich SL, Frame PS, et al. J Natl Cancer Inst Monogr. 32. 2004. National Institutes of Health State-of-the-Science Panel. National Institutes of Health State-Of-The-Science Conference Statement: symptom management in cancer: pain, depression, and fatigue, July 15–17, 2002; pp. 9–16. [DOI] [PubMed] [Google Scholar]
- 32.Singer S, Das-Munshi J, Brähler E. Prevalence of mental health conditions in cancer patients in acute care – a meta-analysis. Ann Oncol. 2010;21(5):925–930. doi: 10.1093/annonc/mdp515. [DOI] [PubMed] [Google Scholar]
- 33.Cheng KK, Yeung RM. Impact of mood disturbance, sleep disturbance, fatigue and pain among patients receiving cancer therapy. Eur J Cancer Care (Engl) 2013;22(1):70–78. doi: 10.1111/j.1365-2354.2012.01372.x. [DOI] [PubMed] [Google Scholar]
- 34.Schwarzer R, Scholz U. Cross-cultural assessment of coping resources: the general perceived self-efficacy scale. Presented at: Asian Congress of Health Psychology; August 28–29, 2000; Tokyo. [Google Scholar]
- 35.Bandura A. Self-Efficacy: The Exercise of Control. New York: Freeman; 1997. [Google Scholar]
- 36.Schwarzer R. Self-Efficacy: Thought Control of Action. Washington, DC: Hemisphere; 1992. [Google Scholar]
- 37.Shiloh S, Koren S, Zakay D. Individual differences in compensatory decision-making style and need for closure as correlates of subjective decision complexity and difficulty. Pers Individ Dif. 2001;30(4):699–710. [Google Scholar]
- 38.Webster DM, Kruglanski AW. Individual differences in need for cognitive closure. J Pers Soc Psychol. 1994;67(6):1049–1062. doi: 10.1037//0022-3514.67.6.1049. [DOI] [PubMed] [Google Scholar]
- 39.Berman MG, Askren MK, Jung M, et al. Pretreatment worry and neurocognitive responses in women with breast cancer. Health Psychol. 2014;33(3):222–231. doi: 10.1037/a0033425. [DOI] [PubMed] [Google Scholar]
- 40.Klepin HD, Geiger AM, Bandos H, et al. Cognitive factors associated with adherence to oral antiestrogen therapy: results from the cognition in the study of tamoxifen and raloxifene (Co-STAR) study. Cancer Prev Res (Phila) 2014;7(1):161–168. doi: 10.1158/1940-6207.CAPR-13-0165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Morone G, Iosa M, Fusco A, et al. Effects of a multidisciplinary educational rehabilitative intervention in breast cancer survivors: the role of body image on quality of life outcomes. Scientific World Journal. 2014;2014:451935. doi: 10.1155/2014/451935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Alacacioglu A, Ulger E, Varol U, et al. Depression, anxiety and sexual satisfaction in breast cancer patients and their partners-Izmir oncology group study. Asian Pac J Cancer Prev. 2014;15(24):10631–10636. doi: 10.7314/apjcp.2014.15.24.10631. [DOI] [PubMed] [Google Scholar]
- 43.Gorini A, Pravettoni G. P5 medicine: a plus for a personalized approach to oncology. Nat Rev Clin Oncol. 2011;8(7):444. doi: 10.1038/nrclinonc.2010.227-c1. [DOI] [PubMed] [Google Scholar]
- 44.Council NR. Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. Washington: The National Academies Press; 2008. [PubMed] [Google Scholar]


