Summary:
Lymphedema is a chronic debilitating disease, affecting a considerable part of the population; it results from impairment of the lymphatic system. It is highly prevalent among patients subjected to axillary and groin nodal dissection after surgery for breast cancer, abdominopelvic surgery, and lymphadenectomy after melanoma surgery. Interestingly, among the surgical treatment options for lymphedema, groin lymph node transfer is gaining popularity; however, in some cases, dissection at this site can cause significant morbidity, including possible development of iatrogenic lymphedema. To avoid these complications, new donor nodal groups are being proposed (eg, submental or supraclavicular). We have used the greater omentum as a lymph node and lymph vessel donor site. Dissection of the omentum is easy to perform and can even be done in patients who have undergone previous abdominal surgeries. We present refinements in the surgical technique for free omentum transfer in the management of secondary lymphedema: the first free omental flap dissection performed laparoscopically and the use of a primary flap as the recipient pedicle of a free greater omentum flap for anatomical repair after chest osteoradionecrosis and simultaneous functional repair of chronic lymphedema.
Lymphedema is a chronic disease that affects a considerable part of the population, and it is caused by impairment of the lymphatic system. Sentinel node biopsy1 has reduced its incidence, but this procedure still fails to support long-term results.
Lymph node transfer is gaining popularity in lymphedema surgery. However, dissection of the groin nodes can lead to iatrogenic lymphedema, which has determined the proposal of using neck donor nodal groups.2,3 Interestingly, the free greater omentum (FGO) flap is another resource that provides lymph nodes for lymphedema treatment. We present refinements in FGO flap transfer for lymphedema.
PATIENTS AND METHODS
CASE 1
A 45-year-old woman was evaluated for right lower-limb lymphedema. She had been diagnosed with lupus erythematosus 30 years ago, and she had undergone kidney transplantation after renal failure secondary to lupus nephropathy 9 years ago. Secondary lymphedema developed 1 year after kidney transplantation.
Nonoperative measures did not improve the patient’s clinical situation. The patient’s body mass index (BMI) was 35.52. The preoperative circumference difference between the lower extremities was 83.7 cm. (The measurements were taken at the supramalleolar circumference and 10, 20, and 30 cm proximal to the malleoli.) Lymphoscintigraphy showed a normal sequence in the left lower extremity and dermal backflow with no lymph nodes in the right leg. Secondary lymphedema of the right lower limb (stage III according to the International Society of Lymphology [ISL] staging) was diagnosed. Lymphovenous anastomoses were performed without success. Later, FGO flap transfer was done in January 2013 under general anesthesia.
A surgical gastroenterologist dissected the flap laparoscopically, taking special care while dissecting the gastroepiploic vessels, which was guided by a plastic surgeon. The extraction of the flap from the abdomen was performed with special attention dedicated to avoiding lesions of the vascular pedicle (Fig. 1). The left gastroepiploic vessels were finally anastomosed to the right superficial circumflex iliac system. The flap was placed under Scarpa’s fascia, and the distal portion was exposed through a window of skin to evaluate the postoperative viability.
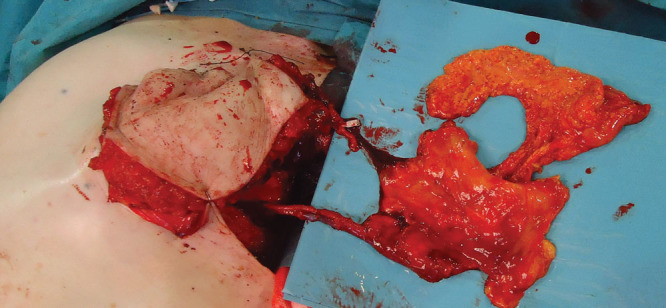
Fig. 1.

View of the greater omentum flap during the process of extraction from the abdominal cavity following laparoscopic dissection.
CASE 2
A 69-year-old woman had undergone surgery for left breast cancer (Halsted radical mastectomy) 33 years ago. Radiotherapy and chemotherapy had also been administered, but the information regarding the type of chemotherapeutic agents used was absent. Four years after surgery, the patient had presented with fourth rib exposure due to osteoradionecrosis. She had also developed lymphedema of the left upper limb, but the date of onset could not be estimated. Clinical rehabilitation had been done irregularly. The patient’s medical history included idiopathic epilepsy, Parkinson’s disease, and depressive disorder. She was living in a residence for disabled patients.
Physical examination showed a narrow thorax with malposition of the left clavicle due to a severe fracture 10 years before presentation. The patient’s BMI was 25.24, her height was 158 cm, and her weight was 62.6 kg.
Lymphedema with numbness and pitting edema of the left upper limb and hand was observed. Preoperative circumference difference between the upper extremities was 87.5 cm. Measurements were taken at the palmar crease, at the wrist, and at 10, 20, and 30 cm proximal to the wrist.
Lymphoscintigraphy showed a normal sequence in the right limb and dermal backflow in the left arm with no identification of lymph nodes.
The diagnosis was stage III (ISL) lymphedema secondary to radical mastectomy and osteoradionecrosis of the fourth and fifth ribs with associated ulcer of the chest wall.
A transverse rectus abdominis myocutaneous (TRAM) flap based on the right rectus abdominis muscle was performed following removal of the anterior portion of both ribs. Dissection of the deep inferior epigastric vessels was done to prepare a recipient vascular pedicle. Upon undermining the TRAM flap, a partial supraumbilical laparotomy was done to expose the FGO flap, which had adhered to the lesser omentum due to previous oncologic surgery.
The dissection of the right gastroepiploic vessels was performed under the surgical microscope. End-to-end anastomoses of the gastroepiploic vessels were performed to the deep inferior epigastric vessels. A portion of the omentum was placed under the superficial fascia of the inner aspect of the arm, from the axilla to the inner midline of the humerus. An end-to-end supermicrosurgical anastomosis was done between a vein of the subcutaneous tissue of the arm and a lymph vessel of the omentum (Fig. 2).
Fig. 2.
End-to-end anastomoses of the gastroepiploic vessels were done to the deep inferior epigastric vessels, and a portion of the omentum measuring 6 by 9 cm was placed under the superficial fascia of the inner aspect of the arm.
RESULTS
Eighteen months after surgery, both patients indicated a high degree of satisfaction, a lighter sensation in the affected limb, and reduction of numbness. The difference of circumference between limbs was 69 cm in the first case and 68 cm in the second case; it should be noted that the second patient suffered a left humerus fracture 5 months following the surgery, with subsequent interruption of rehabilitation for 3 months (Figs. 3, 4).
Fig. 3.

Preoperative view of the second patient presenting stage III lymphedema.
Fig. 4.

Postoperative view of the arm of the second patient 18 months after the surgery.
None of the cases reported any complications related to the donor site. Lymphoscintigraphy did not show any improvement in comparison to preoperative studies.
DISCUSSION
It is well known that the omentum is a highly vascularized intra-abdominal structure that provides an excellent tissue against inflammation and irradiation. Due to its angiogenic properties, it acts as a natural defense mechanism in peritonitis and intra-abdominal sepsis.4 The omentum can be exteriorized and lengthened based on a vascular pedicle or detached using microvascular anastomosis.5–7
The use of greater omentum node transfer in the management of chronic lymphedema presented satisfactory results as both pedicled and free flap.8–11 Drainage can be further improved by lymphovenous anastomosis between lymphatic vessels in the flap and veins in the arm. Omentum may be used to prevent lymphedema after ilioinguinal lymph node dissection12; however, this is controversial.13 There is previous literature indicating that pedicled omentum flaps have been obtained by laparoscopy, but our first case is a free flap.9 Interestingly, this can be performed in patients with previous abdominal surgeries,14 but the dissection of gastroepiploic vessels must be assisted by the reconstructive microsurgeon because the extraction of the flap may damage the pedicle.
The use of a primary flap as the recipient pedicle of a new free flap has also been published,15 but this is the first report of anatomical repair after chest osteoradionecrosis with simultaneous functional repair of chronic lymphedema.
CONCLUSIONS
The FGO flap can be a reliable and effective donor site of lymphatic tissue for lymphedema surgery. This flap can be dissected laparoscopically in order to be transferred as a free flap even in the case of prior abdominal surgeries.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the General University Hospital Gregorio Marañon.
REFERENCES
- 1.Purushotham AD, Upponi S, Klevesath MB, et al. Morbidity after sentinel lymph node biopsy in primary breast cancer: results from a randomized controlled trial. J Clin Oncol. 2005;23:4312–4321. doi: 10.1200/JCO.2005.03.228. [DOI] [PubMed] [Google Scholar]
- 2.Cheng MH, Huang JJ, Huang JJ, et al. A novel approach to the treatment of lower extremity lymphedema by transferring a vascularized submental lymph node flap to the ankle. Gynecol Oncol. 2012;126:93–98. doi: 10.1016/j.ygyno.2012.04.017. [DOI] [PubMed] [Google Scholar]
- 3.Althubaiti GA, Crosby MA, Chang DW. Vascularized supraclavicular lymph node transfer for lower extremity lymphedema treatment. Plast Reconstr Surg. 2013;131:133e–135e. doi: 10.1097/PRS.0b013e318272a1b4. [DOI] [PubMed] [Google Scholar]
- 4.Collins D, Hogan AM, O’Shea D, et al. The omentum: anatomical, metabolic, and surgical aspects. J Gastrointest Surg. 2009;13:1138–1146. doi: 10.1007/s11605-009-0855-1. [DOI] [PubMed] [Google Scholar]
- 5.Liebermann-Meffert D. The greater omentum. Anatomy, embryology, and surgical applications. Surg Clin North Am. 2000;80:275–293, xii. doi: 10.1016/s0039-6109(05)70406-0. [DOI] [PubMed] [Google Scholar]
- 6.Micheau P. [The greater omentum. Its role in reconstructive plastic surgery]. Ann Chir Plast Esthet. 1995;40:192–207. [PubMed] [Google Scholar]
- 7.Ng D, Tang CB, Kadirkamanathan SS, et al. Scrotal reconstruction with a free greater omental flap: a case report. Microsurgery. 2010;30:410–413. doi: 10.1002/micr.20763. [DOI] [PubMed] [Google Scholar]
- 8.Egorov YS, Abalmasov KG, Ivanov VV, et al. Autotrans plantation of the greater omentum in the treatment of chronic lymphedema. Lymphology. 1994;27:137–143. [PubMed] [Google Scholar]
- 9.Attash SM, Al-Sheikh MY. Omental flap for treatment of long standing lymphoedema of the lower limb: can it end the suffering? Report of four cases with review of literatures. BMJ Case Rep. 2013;2013:pii:bcr2012008463. doi: 10.1136/bcr-2012-008463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ciuce C, Seddiq F, Fodor M, et al. Omental free-tissue transfer: indications and results from personal experience. Microsurgery. 2003;23:198–205. doi: 10.1002/micr.10130. [DOI] [PubMed] [Google Scholar]
- 11.Nakajima E, Nakajima R, Tsukamoto S, et al. Omental transposition for lymphedema after a breast cancer resection: report of a case. Surg Today. 2006;36:175–179. doi: 10.1007/s00595-005-3111-7. [DOI] [PubMed] [Google Scholar]
- 12.Benoit L, Boichot C, Cheynel N, et al. Preventing lymphedema and morbidity with an omentum flap after ilioinguinal lymph node dissection. Ann Surg Oncol. 2005;12:793–799. doi: 10.1245/ASO.2005.09.022. [DOI] [PubMed] [Google Scholar]
- 13.Ngan HY, Tam KF, Ng TY. Prevention of lymphoedema using omentoplasty after pelvic lymphadenectomy: a prospective randomised controlled trial. Hong Kong Med J. 2008;14(5 Suppl):43–46. [PubMed] [Google Scholar]
- 14.Karayiannakis AJ, Polychronidis A, Perente S, et al. Laparoscopic cholecystectomy in patients with previous upper or lower abdominal surgery. Surg Endosc. 2004;18:97–101. doi: 10.1007/s00464-003-9001-4. [DOI] [PubMed] [Google Scholar]
- 15.Nakayama B, Kamei Y, Toriyama K, et al. Usefulness of a first transferred free flap vascular pedicle for secondary microvascular reconstruction in the head and neck. Plast Reconstr Surg. 2002;109:1246–1253. doi: 10.1097/00006534-200204010-00006. [DOI] [PubMed] [Google Scholar]


