Abstract
Background:
Wide-awake hand surgery is useful for tendon reconstruction because surgeons can observe the actual movement of the reconstructed tendons during the surgery. We hypothesized that accurate ultrasound-guided injection of local anesthetics into the sensory nerves contributes to reliable analgesia with a relatively small amount of anesthetic.
Methods:
We enrolled 8 patients who underwent forearm tendon transfer. Three patients underwent reconstruction of flexor tendon ruptures in zones 4 and 5, 3 underwent opponensplasty, and 2 underwent multiple tendon transfers according to Brand’s procedure. All patients underwent ultrasound-guided injection of ropivacaine to each sensory nerve branch of the upper arm and forearm and into the subfascial layer of the forearm. The mean amount of total ropivacaine was 193 mg.
Results:
In 7 of the 8 patients, we confirmed adequate active contraction of the flexor or extensor muscles during surgery. The expected active motion of the flexor pollicis longus was not found in 1 patient during surgery because the effect of the anesthetic had spread too widely, involving the motor branch of the median nerve. Two patients required additional infiltration of 2–3 mL of local anesthetic because of local wound pain. All patients gained satisfactory function of the transferred tendons after the surgery, and no remarkable perioperative complications related to local anesthetic systemic toxicity occurred.
Conclusions:
Selective administration of an anesthetic to the sensory nerve branches and subfascial layer enables the performance of wide-awake forearm tendon surgery. The ultrasound-guided injection technique provides safe and effective regional anesthesia for wide-awake surgery.
The usefulness of wide-awake surgery with infiltration of local anesthetics has been widely reported.1,2 The ability of the hand surgeon to observe active movement of the fingers intraoperatively is a great advantage in terms of predicting the postsurgical function of the hand. The most frequently reported technique of wide-awake surgery involves subcutaneous infiltration of a local anesthetic based on anatomical landmarks, and the surgical site is usually limited to the area distal to the wrist joint. A large amount of local anesthetic may be required when the surgical site extends to the forearm, as in tendon reconstruction surgery. Lalonde and Wong1 described that wide-awake surgery at the forearm requires up to 500 mg (200 mL) of epinephrine-containing lidocaine.
The use of a large amount of local anesthetics is associated with a substantial risk of local anesthetic systemic toxicity. Cardiac arrest because of local anesthetic toxicity is a rare but serious complication.3,4 The maximum dose of epinephrine-containing lidocaine for local anesthesia is usually 4–7 mg/kg. The maximum dose of ropivacaine in healthy adults is 3 mg/kg.
Regional anesthesia under ultrasound guidance is effective because of the ability to observe the nerves, needles, and spread of the local anesthetic in real time.5,6 Barrington and Kluger7 reported that ultrasound-guided regional anesthesia is associated with a lower risk of local anesthetic systemic toxicity based on an analysis of approximately 20,000 cases. Real-time observation is considered to be useful for avoidance of nerve injury and intravascular injection of the local anesthetic, making regional anesthesia a safer procedure.5 Ultrasonography allows for identification of the location of the branching site of the superficial branch of the radial nerve and dorsal sensory branch of the ulnar nerve in the forearm.
We hypothesized that sufficient analgesia for wide-awake forearm tendon surgery can be obtained without local anesthetic toxicity with the use of accurate ultrasound-guided injection into each sensory nerve to the skin, interosseous membrane, and fascia of the upper extremity. The purpose of this study was to evaluate the effectiveness of ultrasound-guided selective sensory nerve block for wide-awake forearm tendon reconstruction.
MATERIALS AND METHODS
We enrolled 8 consecutive patients who underwent tendon transfer or tendon graft surgery at the forearm in our department from February 2013 to April 2014. Three of the 8 patients underwent tendon graft or tendon transfer for flexor tendon injuries in zone 4 or 5, 3 underwent opponensplasty of the thumb for carpal tunnel syndrome, and 2 underwent tendon transfer according to Brand’s procedure for posterior interosseous nerve palsy. Each patient underwent ultrasound-guided anesthetic injection 1 hour before surgery. The peripheral nerves in the upper extremities were examined using an ultrasound unit (LOGIQ P6; General Electric, Fairfield, Conn.) with a 16-MHz linear matrix probe. A 23-gauge, 70-mm needle was used for injection. All cutaneous nerves were carefully blocked using the in-plane method of ultrasound guidance. We selected one of the several injection patterns depending on the operative procedure performed. The anesthetic method used for each procedure is described below.
Opponensplasty
Upper Arm
First, we blocked the cutaneous sensory nerves of the upper arm (musculocutaneous nerve, medial cutaneous nerve of the forearm, and posterior cutaneous nerve of the forearm) using approximately 2 mL of 0.750% ropivacaine for each nerve.
Middle Forearm
Second, we blocked the superficial branch of the radial nerve in the middle of the forearm. To provide analgesia to the fascia of the forearm, we injected 5–10 mL of 0.375% ropivacaine in the subfascial layer between the flexor muscle belly and the forearm fascia.
Distal Forearm
Third, we blocked the superficial palmar branch of the median and ulnar nerves approximately 3 cm proximal to the wrist joint using approximately 2 mL of 0.750% ropivacaine for each nerve.
Flexor Tendon Reconstruction at the Forearm
In addition to the anesthesia for opponensplasty indicated above, we blocked other nerves as described below.
Distal Forearm
We injected approximately 3 mL of 0.750% ropivacaine into the anterior interosseous nerve for sensory block of the periosteum in the distal one-third of the forearm for an additional surgical procedure, which included spur resection at the volar surface of the distal radius.
Brand’s Procedure
In addition to the anesthesia for flexor tendon reconstruction indicated above, we blocked other nerves as described below (Fig. 1).
Fig. 1.
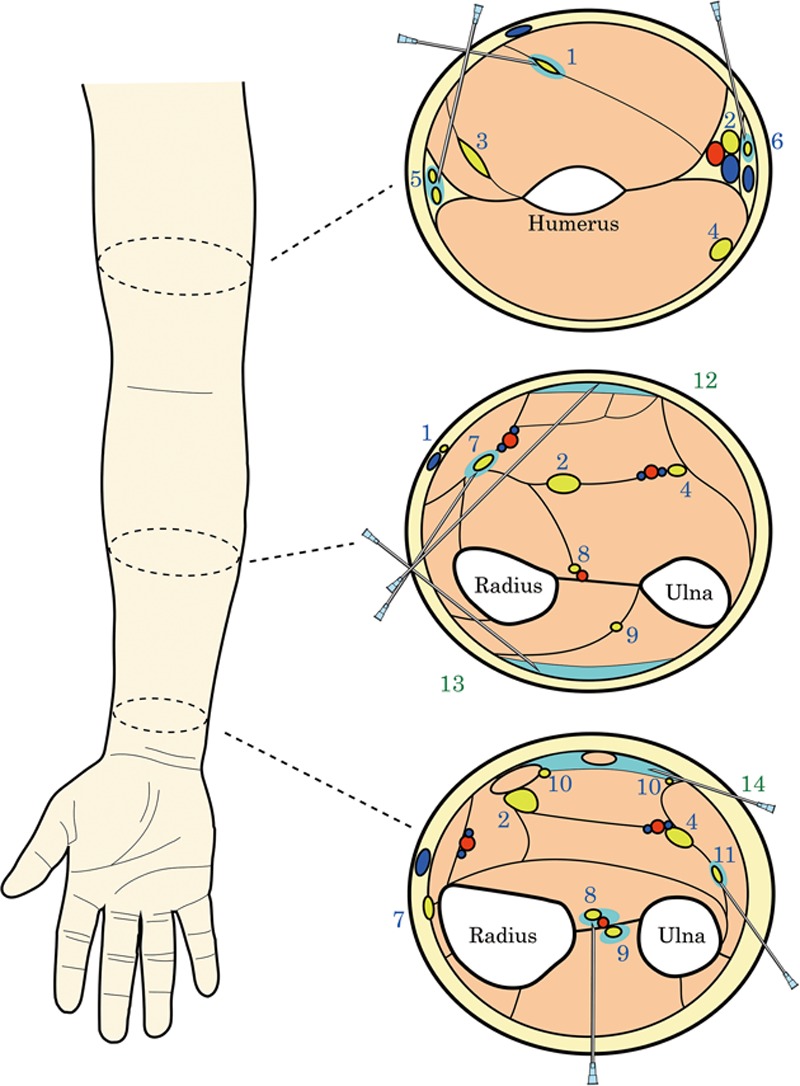
Schematic diagram of ultrasound-guided selective sensory nerves block for Brand’s procedure. There are 3 target layers for injection at the 3 upper and forearm levels. First target includes musculocutaneous (1) and 2 cutaneous [medial (6) and posterior (5)] nerves of the forearm at the distal aspect of the upper arm. The superficial branch of the radial nerve (7) and posterior branch of the ulnar nerve (11) are blocked at the level of forearm. Palmar branch of the median and ulnar nerves (10) is blocked with forearm subfascial injection technique of local anesthetic (14). Usually, these fine nerves are difficult to confirm with ultrasonograph. Second target is subfascial layer at the middle of the forearm (12, 13). Third target is anterior and posterior interosseous nerves (8, 9). This blocking site is distally located from branching site of the motor nerves. 1, musculocutaneous nerve (lateral cutaneous nerve of the forearm); 2, median nerve; 3, radial nerve; 4, ulnar nerve; 5, posterior cutaneous nerve of the forearm; 6, medial cutaneous nerve of the forearm; 7, superficial branch of the radial nerve; 8, anterior interosseous nerve; 9, posterior interosseous nerve; 10, palmar branch of the median and ulnar nerves; 11, dorsal branch of the ulnar nerve; 12 and 13, subfascial block of the forearm; 14, block of palmar branch of the median and ulnar nerves.
Middle Forearm
We blocked the anterior and posterior interosseous nerve to achieve sensory block of the interosseous membrane using approximately 3 mL of 0.750% ropivacaine.
Distal Forearm
We injected approximately 2 mL of 0.750% ropivacaine into the dorsal branch of the ulnar nerve in the distal one-third of the forearm.
In this study, we evaluated the total amount of local anesthetic used for each patient; the active motion of the forearm muscles, which are the donor muscles of the reconstructed tendons; the presence or absence of pain during each surgery and the amount of additional local anesthetic, if required; and the presence or absence of adverse events.
RESULTS
The total amount of preoperatively injected ropivacaine was 193 ± 23 mg (37 ± 6 mL; Table 1). We confirmed active motion of the donor muscle in 7 of the 8 patients. In one case, the expected active motion of flexor pollicis longus was not observed during surgery. In this case, local anesthetic (0.75% ropivacaine 3 mL) injected for the superficial branch of the median nerve may have spread proximally along the median nerve because the blocking site was too proximally located.
Table 1.
Summary of Patients and Anesthesia
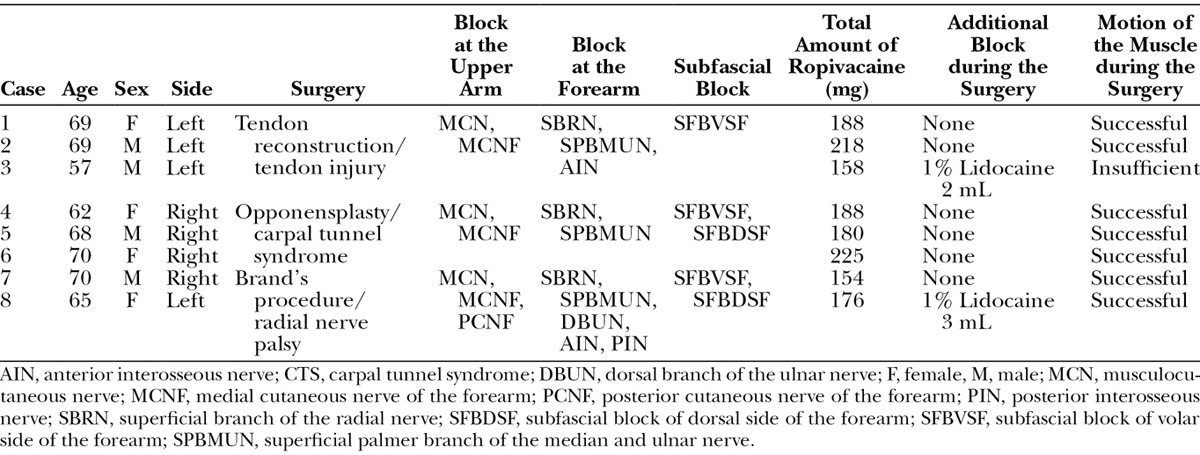
Two of the 8 patients complained of pain at the surgical site during the surgery; 2 and 3 mL of 1% lidocaine, respectively, was added by local infiltration for these 2 patients. No patients developed any particular adverse events.
DISCUSSION
This study has demonstrated the effectiveness of ultrasound-guided selective sensory nerve block for wide-awake forearm tendon transfer. Although 2 patients required additional local anesthesia (2–3 mL of 1% lidocaine), complete analgesia was achieved in the other 6 patients during the surgery. The expected active motion of the flexor pollicis longus was not observed in 1 patient who underwent surgical tendon reconstruction. We consider that this failure can be avoided by careful selection of the block site. The total amount of preoperatively injected ropivacaine ranged from 154 to 225 mg, which is smaller than that described by Lalonde and Wong.1 They mentioned that common hand surgery requires up to 200 mg of lidocaine and that 300 mg of anesthetic is required for extensor indicis proprius-to-extensor pollicis longus tendon transfer. They also reported that up to 200 mL of 0.25% lidocaine (500 mg) with epinephrine is required for forearm tendon transfers, and that bupivacaine is added to elongate the analgesia time. We consider that this dose may be associated with a potential risk of local anesthetic systemic toxicity in a specific patient population. No adverse events, such as nerve injury or local anesthetic systemic toxicity, were observed in the current series. We consider ultrasound-guided selective sensory nerve block to be a potentially promising technique. Because sufficient analgesia is obtained approximately 30 minutes after anesthetic injection, we conducted the injection 1 hour before surgery.
This selective sensory nerve block procedure involves 3 separate layers that are blocked to successfully achieve analgesia before forearm surgery. First, the forearm derma is innervated by 7 cutaneous nerves: the medial, lateral, and posterior cutaneous nerves of the forearm; the dorsal branches of the radial and ulnar nerves; and the palmar superficial branches of the median and ulnar nerves. Because the cutaneous branches of these nerves overlap one another, it is necessary to block all branches coursing to the area of the surgical incision. These fine peripheral nerves can be clearly observed with a high-frequency ultrasound probe. We successfully blocked each of these nerves individually with approximately 2 mL of 0.75% ropivacaine under ultrasound guidance. Second, we blocked the forearm fascia by injecting the subfascial layer. The details regarding the innervation of the forearm fascia have not been well clarified. We consider this subfascial block in the middle third of the forearm to be adequate for achieving analgesia during creation of the fascial incision.6 Analgesia of the interosseous membrane was achieved by blocking the anterior and posterior interosseous nerves at the middle aspect of the forearm. This block site should be located distal to the branching site of the motor nerves.8 Thus, it is possible to avoid motor nerve block by performance of sequential, selective sensory nerve blocks (Figs. 2, 3).
Fig. 2.
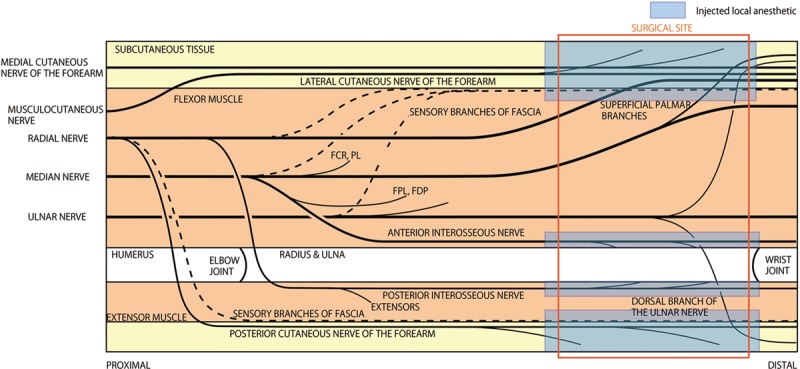
Infiltration of local anesthetic based on the anatomical landmark. Large amount of local anesthetic is required. FCR indicates flexor carpi radialis; FDP, flexor digitorum profundus; FPL, flexor pollicis longus; PL, palmaris longus.
Fig. 3.
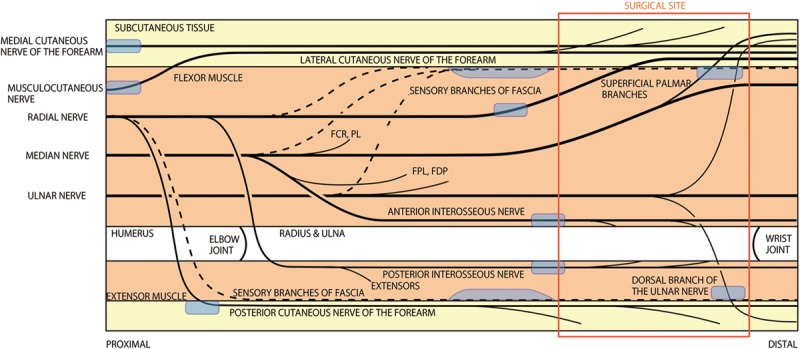
Selective sensory nerve block for Brands’ procedure. FCR indicates flexor carpi radialis; FDP, flexor digitorum profundus; FPL, flexor pollicis longus; PL, palmaris longus.
Although the selective sensory nerve block technique described herein is a technically demanding and complicated procedure, we consider that the limited doses of anesthetic agents required allow for the safe and effective performance of forearm tendon surgery. Further clinical trials are warranted to design a more accurate and reliable approach for wide-awake surgery.
In conclusion, ultrasound-guided selective sensory nerve block is a promising procedure for wide-awake forearm tendon surgery. The total amount of local anesthetic can be reduced with the use of ultrasound-guided injection to each sensory nerve to the skin, subcutaneous tissue, fascia, and interosseous membrane of the forearm.
Footnotes
Presented at the 69th Annual Meeting of the American Society for Surgery of the Hand, September 18–20, 2014, Boston, Mass.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Lalonde DH, Wong A. Dosage of local anesthesia in wide awake hand surgery. J Hand Surg Am. 2013;38:2025–2028. doi: 10.1016/j.jhsa.2013.07.017. [DOI] [PubMed] [Google Scholar]
- 2.Bezuhly M, Sparkes GL, Higgins A, et al. Immediate thumb extension following extensor indicis proprius-to-extensor pollicis longus tendon transfer using the wide-awake approach. Plast Reconstr Surg. 2007;119:1507–1512. doi: 10.1097/01.prs.0000256071.00235.d0. [DOI] [PubMed] [Google Scholar]
- 3.Chazalon P, Tourtier JP, Villevielle T, et al. Ropivacaine-induced cardiac arrest after peripheral nerve block: successful resuscitation. Anesthesiology. 2003;99:1449–1451. doi: 10.1097/00000542-200312000-00030. [DOI] [PubMed] [Google Scholar]
- 4.Klein SM, Pierce T, Rubin Y, et al. Successful resuscitation after ropivacaine-induced ventricular fibrillation. Anesth Analg. 2003;97:901–903. doi: 10.1213/01.ANE.0000075839.18073.37. [DOI] [PubMed] [Google Scholar]
- 5.Griffin J, Nicholls B. Ultrasound in regional anaesthesia. Anaesthesia. 2010;65(Suppl 1):1–12. doi: 10.1111/j.1365-2044.2009.06200.x. [DOI] [PubMed] [Google Scholar]
- 6.Marhofer P, Schrögendorfer K, Wallner T, et al. Ultrasonographic guidance reduces the amount of local anesthetic for 3-in-1 blocks. Reg Anesth Pain Med. 1998;23:584–588. doi: 10.1016/s1098-7339(98)90086-4. [DOI] [PubMed] [Google Scholar]
- 7.Barrington MJ, Kluger R. Ultrasound guidance reduces the risk of local anesthetic systemic toxicity following peripheral nerve blockade. Reg Anesth Pain Med. 2013;38:289–297. doi: 10.1097/AAP.0b013e318292669b. [DOI] [PubMed] [Google Scholar]
- 8.Liu J, Pho RW, Pereira BP, et al. Distribution of primary motor nerve branches and terminal nerve entry points to the forearm muscles. Anat Rec. 1997;248:456–463. doi: 10.1002/(SICI)1097-0185(199707)248:3<456::AID-AR19>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]


