Abstract
Background
Previous studies have mostly focused on the effects of specific constituents of beverages and foods on the risk of esophageal cancer (EC). An increasing number of studies are now emerging examining the health consequences of the high temperature of beverages and foods. We conducted a meta-analysis to summarize the evidence and clarify the association between hot beverages and foods consumption and EC risk.
Methods
We searched the PubMed, Embase, and Web of Science databases for relevant studies, published before May 1, 2014, with the aim to estimate the association between hot beverage and food consumption and EC risk. A random-effect model was used to pool the results from the included studies. Publication bias was assessed by using the Begg test, the Egger test, and funnel plot.
Results
Thirty-nine studies satisfied the inclusion criteria, giving a total of 42,475 non-overlapping participants and 13,811 EC cases. Hot beverage and food consumption was significantly associated with EC risk, with an odds ratio (OR) of 1.82 (95% confidence interval [CI], 1.53–2.17). The risk was higher for esophageal squamous cell carcinoma, with a pooled OR of 1.60 (95% CI, 1.29–2.00), and was insignificant for esophageal adenocarcinoma (OR: 0.79; 95% CI: 0.53–1.16). Subgroup analyses suggests that the association between hot beverage and food consumption and EC risk were significant in Asian population (OR: 2.06; 95% CI: 1.62-2.61) and South American population (OR: 1.52; 95% CI: 1.25-1.85), but not significant in European population (OR: 0.95; 95% CI: 0.68-1.34).
Conclusions
Hot beverage and food consumption is associated with a significantly increased risk of EC, especially in Asian and South American populations, indicating the importance in changing people’s dietary habits to prevent EC.
Keywords: Hot, Beverage, Food, Esophageal cancer, Meta-analysis
Background
Esophageal cancer (EC) is the eighth most common cancer in the world and ranks six among all cancers in mortality [1]. Many studies have shown that dietary habits are significantly correlated with the occurrence of EC [2,3], most of which linking specific constituents of beverages and foods to EC. For example, Polyphenols in green tea was found to inhibit esophageal tumorigenesis [4], whereas maté infusion and caffeine appeared to induce mutagenic effects [5]. An increasing number of studies have investigated the possible relationship between the temperature of beverages and foods and EC risk [6-8], since recurrent thermal injuries to the esophageal mucosa owing to the consumption of hot drinks or foods has long been considered a risk factor for EC [9].
Hot beverage consumption could substantially increase the intraesophageal temperature, depending on the initial drinking temperature. An animal study showed that the structure and the function of the esophageal epithelium were damaged by heat stress even [10]. However, epidemiological evidence on the causal relationship between the temperature of beverages and foods and EC is not well established. Research on the relationship was often done as a component of larger studies that focused on specific beverage or food gradients, and the results varied greatly across studies. Some studies found no association between hot beverages and foods and EC risk [11-13], arguing that the oral cavity could modulate the heat, and the temperature could fall too rapidly to cause injury to the esophageal mucosa [14]. But many other studies reported that the intake of hot beverages and foods increased EC risk [11,15,16].
In 2009, Islami and colleagues [9] reviewed fifty nine studies and found that over half of the studies showed statistically significant increased risk of EC associated with higher temperature of beverage and food intake. However, the authors did not use quantitative techniques to compute summary estimates of the risk, and the review is outdated. Therefore, we conducted this meta-analysis to ascertain the association between hot beverage and food consumption and EC risk more precisely, relying on all available evidence up-to-date, and to identify the potential factors affecting this association.
Methods
Search strategy
This meta-analysis was conducted according to the checklist of the Meta-Analysis of Observational Studies in Epidemiology Guideline [17]. We searched PubMed, Embase, and Web of Science databases from inception to May 1, 2014 for all epidemiological studies on hot beverage and food consumption in relation to EC risk, using the string ‘(esophageal OR oesophageal) AND (cancer OR carcinoma OR neoplasm) AND (tea OR maté OR coffee OR beverage OR liquid OR alcohol OR food OR diet)’. In addition, we scrutinized the reference lists from retrieved articles to identify other relevant studies.
Inclusion criteria
Studies were considered eligible for inclusion if they met the following criteria: (1) the study was a case–control or cohort study design, (2) it was published in English, (3) the exposure was hot beverage or food consumption, (4) the outcome of interest was EC, and (5) the study reported the odds ratio (OR) or relative risk (RR) with 95% confidence intervals (CIs) for the association between hot beverages or foods and EC risk or provided sufficient data to calculate them.
Date extraction
We extracted the following data from each retrieved article: name of first author, publication year and country of study, study design, specific outcomes, characteristics of study population, number of cases and participants, exposure type, exposure measurement, outcome assessment, comparison categories, OR or RR and corresponding 95% CI, and confounding factors adjusted in the analyses. Data from included studies were independently extracted by two authors (Y.W.C and Y.C), and disagreements were resolved through discussion with the third reviewer (Z.X.L).
Quality assessment
Two independent reviewers (Y.W.C and C.Y) evaluated the quality of the included studies by the Newcastle-Ottawa Scale [18], which was a nine-point scale that allocated points based on the selection process (0-4points), the comparability (0–2 points), and the assessment of outcomes of study participants (0-3points). We assigned scores of 0–3, 4–6, and 7–9 for low, moderate, and high quality of studies, respectively.
Statistical analysis
Random-effects model was used to estimate the summary ORs or RRs for the association between hot beverage and food consumption and EC risk. Taking the subjectivity of differentiating between hot and very hot into account, we used the specific OR for standardized category (hot and very hot) versus reference category (cold and warm) of beverage and food consumption. We defined exposure as hot beverages and foods (standardized category, preference for high-temperature foods and drinks, often consuming of them) versus non-hot beverages and foods (all other combinations). If studies had partly overlapped subjects, only the one with a larger sample size was selected for the analysis. If a study reported results for different beverages and foods separately, those beverage/food specific results were regarded as separate reports on the relationship between temperature and EC risk. One study [11] contained 4 kinds of drinks, and was, therefore, accounted as four independent reports. Another study [19] reporting tea, water and food was regarded as three reports. Two studies [13,20] conducted in two different areas of China were considered as two reports respectively, and another study [16] including two large multicenter case–control studies was treated as two reports.
Statistical heterogeneity among studies was evaluated using the I2 statistic, where values of 25%, 50% and 75% represent cut-off points for low, moderate and high degrees of heterogeneity, respectively [21]. To assess the heterogeneity across all included studies, the study location (Asia, South America, Europe, Africa), study setting (population-based, hospital based), study quality (≥7,<7),type of EC (esophageal squamous cell carcinoma (ESCC), esophageal adenocarcinoma (EAC)), and sample size (≥1000,<1000) were further examined using meta-regression. In sensitivity analyses, we conducted leave-one-out analyses [22] for each study to examine the magnitude of influence of each study on pooled risk estimates. Subgroup analyses by age, sex, study location, hot beverage and food categories, study quality, smoking and alcohol intake, study setting, outcome assessment and exposure assessment were conducted to examine the robustness of the primary results. Publication bias was assessed using the Begg test [23], the Egger test [24] and funnel plot. All statistical analyses were performed using STATA version 11.0 (Stata Corp, College Station, Texas, USA). All tests were two sided with a significance level of 0.05.
Results
Literature search
The search identified a total of 3780 unique articles from PubMed, Google scholar, and Web of Science databases, of which 189 articles were identified as potentially relevant. After retrieving and reviewing the full text, we determined that 39 studies met our inclusion criteria. The process of study selection is shown in Figure 1.
Figure 1.
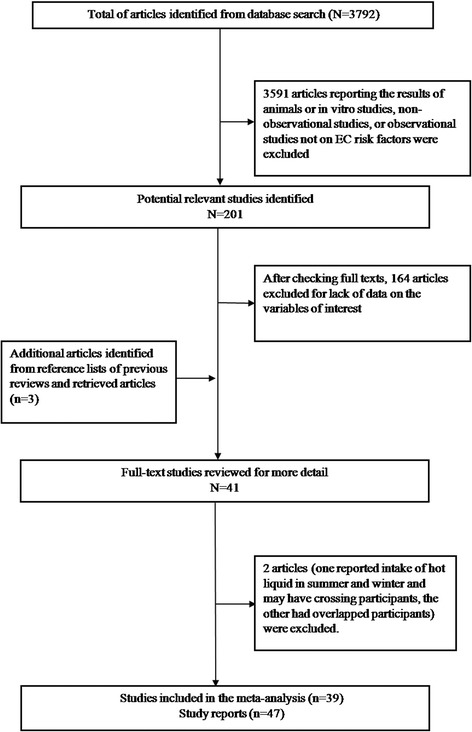
Study selection process.
Study characteristics
Table 1 shows the main characteristic of the 39 included studies. These studies were published between 1979 and 2014, all of which with case–control design. The sample sizes of studies ranged from 143 to 4,118 with a total of 42,475 subjects. The number of EC cases diagnosed in the studies ranged from 47 to 1,310, with a total of 13,811 reported EC cases. Seventeen studies were conducted in China [13,19,20,25-38], six in Uruguay [11,16,39-42], three in Argentina [11,16,43], three in Brazil [11,16,44], three in Paraguay [11,16,45], three in India [46-48], three in Iran [15,49,50], two in British [8,51], one in Australia [12], one in Sweden [7], one in Greece [6], one in Kenya [52], and one in Japan [53]. Thirty studies reported results for men and women together, four reported the results for men and women separately, and three reported results for men only and two for women only. Three studies reported results separately by type of EC. Two studies were deemed high quality, 36 moderate quality studies, and one low quality study. The average quality score for all included studies was 5.00.
Table 1.
Characteristics of studies included in the meta-analysis
| Study source | Study design | Sex | Age at baseline(years) | No of cases | No of participants | Exposure assessment | Outcome assessment | Exposure categories used in meta-analysis | Adjustment for confounders | Quality assessment |
|---|---|---|---|---|---|---|---|---|---|---|
| Islami et al., [15], northern Iran | Population based case–control | F/M | Cases:64.5 ± 10.1 controls:64.3 ± 10.4 | 300 | 871 | Interviews | Endoscopy and biopsy samples | Tea: hot/very hot vs. warm | Ethnicity, daily vegetable intake, alcohol consumption, tobacco or opium use, duration of residence in rural areas, education level, and car ownership | 7 |
| Lin et al., [35],Southern China | Hospital based case–control | F/M | Cases:54.5 ± 4.9 controls:52.5 ± 3.7 | 213 | 426 | FFQ | Endoscopically and histologically confirmed | Beverage: hot/very hot vs. lukewarm | Age, sex, educational status, smoking, drinking, body mass index, vegetable and fruit | 6 |
| Rolon et al., [45], Paraguay | Hospital based case–control | F/M | ≤45:33 46–55:89 56–65:188 ≥ 66:202 | 131 | 512 | Interviews | Cytology, histology, or radiology | Maté: very hot vs. warm/hot | design variables, lifetime cigarette consumption, and lifetime alcohol consumption | 6 |
| Stefani et al., [41], Uruguay | Hospital based case–control | F/M | 40-89 | 166 | 830 | Questionnaire | Histologically verified | Maté: hot/very hot vs. warm | NR | 6 |
| Castelletto et al., [43], Argentina | Hospital based case–control | F/M | ≤54:80 55–64:129 65–74:127 ≥ 75:57 | 131 | 393 | Questionnaire | Histological diagnosis | Maté: hot/very hot vs. warm | Education, average number of cigarettes/day, alcohol consumption (ml/day), the design variables | 6 |
| Castellsagu´e et al., [11], south America | Hospital based case–control | F/M | 64.0(mean) | 830 | 2609 | Interviews with structured questionnaire | Histologically confirmed or a cytological or radiological diagnosis | Maté, tea, coffee, coffee with milk: hot/very hot vs. cold/warm | Age group, hospital, residency, years of education, average number of cigarettes/day, average amount of pure ethanol/day and gender | 6 |
| Ibiebele et al., [12], Australia | Population based case–control | F/M | 18-79 | 521 | 1965 | FFQ | Registries | Tea/coffee: hot/very hot vs. lowest | Age, gender; cumulative history of smoking in pack years, lifetime mean alcohol intake; heartburn and acid reflux symptoms, body mass index, educational status, aspirin use in previous 5 years, total fruit and vegetable intake and total energy intake in kilojoules | 6 |
| Szyman´ska et al., [44], Latin America | Hospital based case–control | F/M | NR | 71 | 228 | Lifestyle questionnaire | ICD-O classification | Maté: hot/very hot vs. cold/warm | NR | 5 |
| Chen et al., [26], Southern China | Hospital based case–control | F/M | Cases:54.6 ± 6 controls:54.0 ± 7 | 87 | 267 | Self-designed structured questionnaire | Histologically confirmed | Tea: hot/very hot vs. warm | NR | 5 |
| Sewram et al., [42], Uruguay | Hospital based case–control | F/M | 35-85 | 295 | 685 | Questionnaire | Registries | Maté: very hot vs. warm/hot | Amount consumed, and duration of mate´ consumption | 5 |
| Tang et al., [19], China | Hospital based case–control | F/M | 61 ± 11.4 | 359 | 739 | Structured questionnaire | Medical records and pathology reports | Tea, water, food: high vs. low or mild | Age, gender, education level, body mass index, smoking status, alcohol drinking, family history of cancer in first-degree relatives, daily intake of vegetables and daily intake of fruit | 6 |
| Stefani et al., [40], Uruguay | Hospital based case–control | F/M | 40-89 | 234 | 702 | Questionnaire | Microscopically confirmed | Maté: hot/very hot vs. warm | NR | 5 |
| Wu et al., [20], China | Population based case–control | F/M | NR | 665 | 2000 | Pretested standardized epidemiologic questionnaire | registry | Tea: high vs. normal | NR | 5 |
| Sharp et al., [8], England and Scotland | Population based case–control | F | <75(<80in Trent) | 156 | 312 | Interviews | Histologically confirmed | Tea/coffee: hot/burning hot vs. warm | NR | 5 |
| Terry et al., [7], Sweden | Population based case–control | F/M | <80 | 189 | 1004 | interviews | Histologically confirmed | Tea/coffee: hot/very hot vs. cold/lukewarm | Age, gender, body mass index, cigarette smoking, socioeconomic status presence of Gastro-oesophageal reflux symptoms, frequency quartiles of hot beverage consumption, and quartiles of alcohol, fruit and vegetables, and energy consumption | 5 |
| Lubin et al., 2014, South America, [16] | Case–control | F/M | 35-85 | 1310 | 4118 | Questionnaire | Medical records | Maté: hot/very hot vs. warm vs. | NR | 5 |
| Wang et al. [37], China | Population based case–control | F/M | Mean: cases 61.51 controls 60.75 | 355 | 763 | Structured questionnaire | Pathologically diagnosed | Food: hot vs. warm | Age (continuous), marital status and education years | 7 |
| Phukan et al., [47], India | Hospital based case–control | F/M | Case:55.0 ± 8.1 control:54.5 ± 7.8 | 502 | 1511 | Investigation | Histopathologically confirmed | Food: hot vs. moderate | Education, income, chewing betel nut and tobacco, smoking, and alcohol use | 4 |
| Wu et al., [13], China | Population based case–control | F/M | <50: 67 50–59:219 60–69: 428 70–79:295 ≥ 80:53 | 531 | 1062 | Pre-tested standardized questionnaires | Cancer registration database | Food: hot vs. normal | NR | 4 |
| Gao et al., [29], China | Population based case–control | F/M | 30-74 | 902 | 2454 | Structured questionnaire | Registry | Hot soup or porridge: hot/burning hot vs. cold/neither cold nor hot | Age, education, birthplace, tea drinking, cigarette smoking, alcohol drinking and consumption of preserved foods, vegetables and fruit | 6 |
| Hu et al., [32], China | Hospital based case–control | F/M | 35-69 | 196 | 588 | Interviews | Histopathologically confirmed | Gruel: hot/scalding vs. lowest | Smoking, alcohol, income and occupation | 4 |
| Garidou et al., [6], Greece | Hospital based case–control | F/M | <60: 79 60–69:103 ≥ 70: 117 | 99 | 299 | Questionnaire | Histologically confirmed | Preferrable temperature: very hot vs. cold to hot | Gender, age, birthplace, schooling, height, analgesics, coffee drinking, alcohol intake, tobacco smoking and energy intake | 4 |
| Cheng et al., [51], British | Population based case–control | F | Cases:65.9 controls:65.3 | 74 | 148 | Questionnaire and interview | Histologically confirmed | Preference tea or coffee: hot very/burning hot/hot vs. warm | NR | 4 |
| Hanaoka et al., [53], Japan | Hospital based case–control | M | Under 85 years old | 141 | 282 | Structured questionnaire | Confirmed histologically by biopsy examination | Preference for high = temperature food and drink: like vs. dislike | Alcohol consumption (g/week) | 4 |
| Srivastava et al., [48], India | Case–control | F/M | NR | 170 | 340 | Pretested. Semi-structured questionnaires | Endoscopic, radiological and histopathological assessments | Food: hot vs. warm | NR | 4 |
| Stefani et al., [39], Uruguay | Hospital based case–control | F/M | 40-49:45 50–59:120 60–69:207 70–79:183 80–89:45 | 200 | 600 | Questionnaire | Newly diagnosed and microspically confirmed | Maté temperature: hot/very hot vs. warm | NR | 5 |
| Cheng et al., [27], Hong Kong of China | Case–control | F/M | <45:40 45–54:246 55–64: 722 65–74:696 > =75: 294 | 400 | 1998 | Interviews with structured questionnaire | Histologically confirmed diagnoses | Preference for hot drinks or soups: yes vs. no | Adjusted for age and education, place of birth, green leafy vegetables, pickled vegetables, citrus fruits, tobacco and alcohol | 4 |
| Gao et al., [30], China | Population based case–control | F/M | 30-74 | 653 | 1965 | Structured, standardized questionnaire | Registry | Burning-hot fluids:yes vs. no | NR | 5 |
| Cook-mozaffari et al., [49], Iran | Case–control | F/M | NR | 344 | 1032 | Questionnaire | Registry | Drinking of hot tea: yes vs. no | NR | 4 |
| Guo et al.,[31], China | Nested case–control | F/M | 40-69 | 640 | 3840 | Structured questionnaires | X-ray films and cytological, pathological, surgical specimens | Hot liquid:≥1 vs.0 | Years of smoking and cancer history in first degree relatives | 6 |
| Ke et al., [34], China | Hospital based case–control | F/M | 29-82 | 1064 | 2168 | Questionnaires and FFQ | Histologically confirmed | Hot Congou drinkers vs. non-hot Congou drinkers | NR | 5 |
| Patel et al., [52], Kenya | Hospital based case–control | F/M | Mean:56.1 | 159 | 318 | Questionnaires | NR | Take hot beverages: yes/no | NR | 4 |
| Hung et al., [33], Taiwan of China | Case–control | M | Mean:62.4 | 267 | 697 | Interviews according to standardized questionnaire | Histologically confirmed | Hot drink or soup: 3+ time per day vs. <3 time per day | Adjusted for age, educational levels, ethnicity, source of hospital, smoking, alcohol drinking and areca nut chewing | 4 |
| Chen et al., [25], Taiwan of China | Hospital based case–control | M | 40-50:284 51–60::291 61–70 :314 > 70:209 | 274 | 922 | Interviews | Newly histologically diagnosed | Hot drink or soup: > = 1 time/d vs. <1time/d | Adjusted for age, educational levels, ethnicity, source of hospital, smoking, alcohol drinking, and areca nut chewing | 4 |
| Gao et al., [28],China | Case–control | F/M | 51-65 | 600 | 2114 | Questionnaires | Histologically confirmed | Scalding hot food: daily vs. weekly/never/monthly/seldom | NR | 4 |
| Sun et al., [36],China | Population based case–control | F/M | Cases:61.21 ± 8.95 Controls:60.84 ± 8.90 | 250 | 1000 | Questionnaires | Cancer registration database | Hot foods: often vs. sometimes | NR | 6 |
| Yang et al., [38], China | Case–control | F/M | Cases:58.1 (8.5) Controls:57.9 (8.8) | 185 | 370 | Questionnaires | Histologically diagnosed within half a year | Hot foods: often vs. Rarely/occasionally | NR | 6 |
| Jessri et al., [50], Iran | Hospital based case–control | F/M | 40-75 | 47 | 143 | Structured pre-tested questionnaires | Histologically-confirmed | Food and beverages temperature: hot vs. warm/cold | NR | 4 |
| Khan et al., [46], India | Case–control | F/M | Case:54.3(7.6) Control:58.1(8.3) | 100 | 200 | Questionnaires | Histologically-confirmed | Degree of hotness: hot vs. warm | NR | 3 |
Age presents the range with Mean (SD). Abbreviations: NR = not reported; F = female; M = male.
Hot beverage and food consumption and the risk of esophageal cancer
The results from the random-effects meta-analysis of hot beverage and food consumption and the risk of EC were shown in Figure 2. Thirty-two of 47 independent reports from 39 studies suggested a positive relation between hot beverage and food consumption and EC risk. The pooled OR was 1.77(95% CI, 1.39–2.25), with a high heterogeneity (I2 = 92.8%, p = 0.001); the pooled OR was 2.09(95% CI, 1.71–2.56, I2 = 57.8%, p = 0.008); and the pooled OR of EC risk in relation to hot beverage and food consumption was 1.73(95% CI, 1.18–2.53, I2 = 68.2%, p = 0.004).
Figure 2.
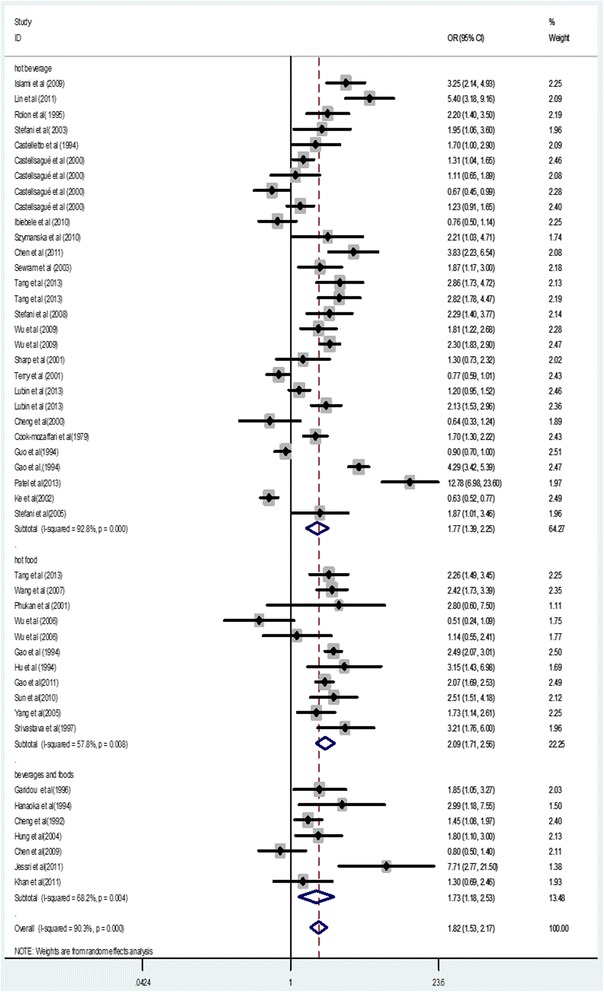
Forest plot of odds ratios from 39 studies linking hot beverage and food consumption and the risk of esophageal cancer.
Subgroup analysis
Table 2 showed the results based on subgroup analyses, which were to examine the stability of the primary results and explore the resources of potential heterogeneity. The associations between hot beverage and food consumption and the risk of EC were similarly significant in subgroup analyses, with the exception of EAC (OR = 0.79, 95% CI = 0.53–1.16, I2 = 50.30%, P = 0.110) and European population (OR = 0.95, 95% CI = 0.68–1.34, I2 = 62.40%, P = 0.031).
Table 2.
Subgroup analysis of odds ratio of hot beverages and foods and esophageal cancer
| No of reports | OR | (95% CI) | I 2 | P for heterogeneity | |
|---|---|---|---|---|---|
| Sex | |||||
| Men | 8 | 2.36 | 1.53–3.65 | 87.60% | 0.001 |
| Women | 7 | 2.45 | 1.51–3.98 | 85.60% | 0.001 |
| Combined | 37 | 1.78 | 1.49–2.16 | 89.30% | 0.001 |
| Type of EC | |||||
| ESCC | 26 | 1.60 | 1.29–2.00 | 88.70% | 0.001 |
| EAC | 4 | 0.79 | 0.53–1.16 | 50.30% | 0.110 |
| NR | 20 | 2.35 | 1.90–2.91 | 80.70% | 0.001 |
| Study quality | |||||
| Score ≥ 7 | 2 | 2.73 | 2.06–3.62 | 12.90% | 0.284 |
| Score < 7 | 45 | 1.78 | 1.49–2.14 | 90.40% | 0.001 |
| Study location | |||||
| Asia | 28 | 2.06 | 1.62–2.61 | 91.70% | 0.001 |
| South America | 13 | 1.52 | 1.25–1.85 | 66.70% | 0.001 |
| Europe | 5 | 0.95 | 0.68–1.34 | 62.40% | 0.031 |
| Africa | 1 | 12.78 | 6.95–23.5 | . | 0.001 |
| Measurement domain | |||||
| Temperature categories | 33 | 1.84 | 1.54–2.21 | 83.80% | 0.001 |
| Whether consuming or not | 5 | 2.14 | 0.94–4.88 | 98.30% | 0.001 |
| Preference | 4 | 1.44 | 0.88–2.35 | 66.30% | 0.031 |
| Frequency | 5 | 1.71 | 1.24–2.36 | 68.90% | 0.012 |
| Beverages and foods domain | |||||
| Tea | 8 | 1.88 | 1.16–3.07 | 94.30% | 0.001 |
| Mate | 10 | 1.72 | 1.43–2.07 | 47.50% | 0.046 |
| Foods | 11 | 2.09 | 1.71–2.56 | 57.80% | 0.008 |
| Others | 18 | 1.73 | 1.19–2.49 | 93.70% | 0.001 |
| Controlling age in models | |||||
| Yes | 17 | 1.6 | 1.24–2.07 | 88.50% | 0.001 |
| No | 30 | 1.98 | 1.55–2.52 | 91.30% | 0.001 |
| Controlling smoking in models | |||||
| Yes | 29 | 1.61 | 1.26–2.07 | 89.30% | 0.001 |
| No | 27 | 2 | 1.56–2.55 | 90.50% | 0.001 |
| Controlling alcohol intake in models | |||||
| Yes | 19 | 1.56 | 1.21–2.02 | 88.00% | 0.001 |
| No | 28 | 2.03 | 1.59–2.59 | 91.60% | 0.001 |
| Study setting | |||||
| Population | 14 | 1.52 | 1.07–2.16 | 94.1% | 0.001 |
| Hospital | 24 | 2.10 | 1.56–2.82 | 89.8% | 0.001 |
| NR | 9 | 1.73 | 1.44–2.06 | 59.7% | 0.040 |
| Exposure assessment | |||||
| Interview | 14 | 1.33 | 1.03–1.71 | 80.0% | 0.001 |
| Questionnaire | 33 | 2.07 | 1.67–2.57 | 91.5% | 0.001 |
| Outcome assessment | |||||
| Histology | 30 | 1.68 | 1.36–2.07 | 88.2% | 0.001 |
| Record | 17 | 1.90 | 1.50–2.41 | 86.3% | 0.001 |
Abbreviations: EC = esophageal cancer; ESCC = esophageal squamous cell carcinoma; EAC = esophageal adenocarcinoma; NR = not reported.
Sensitivity analysis and meta-regression
We excluded each study in turn and pooled the results of the remaining included studies. The positive association was not materially changed upon the exclusions, with a pooled OR range from 1.75 (95% CI, 1.47 to 2.07; P = 0.001) to 1.87(95% CI, 1.58 to 2.20; P = 0.001), which indicates that the overall result was not significantly influenced by any individual studies.
Our meta-regression analysis reveals that the study location (P = 0.001), the type of EC (P = 0.047) and sample size (P = 0.033) were significant sources of heterogeneity. Study location alone explained 34.39% of the τ2 in the meta-regression; type of EC explained 12.97%; and sample size explained 8.99%. The results were shown in Table 3.
Table 3.
Meta-regression analysis
| Variable | Coefficient | Standard error | P value | 95% CI |
|---|---|---|---|---|
| Study location | ||||
| Asia | −1.833 | 0.568 | 0.002 | −2.979–-0.688 |
| South America | −2.109 | 0.578 | 0.001 | −3.273–-0.945 |
| Europe | −2.582 | 0.607 | 0.001 | −3.807–-1.357 |
| Type of EC | −0.678 | 0.327 | 0.047 | −1.348–-0.009 |
| Sample size | −0.403 | 0.183 | 0.033 | −0.771–-0.034 |
Abbreviations: EC = esophageal cancer.
Publication bias
Visual inspection of funnel plot did not identify substantial asymmetry (see Figure 3). The Begg rank correlation test and the Egger linear regression test indicated no evidence of publication bias across included studies (Begg test Z = 0.59, P = 0.557; Egger test t = 1.58, P = 0.121).
Figure 3.
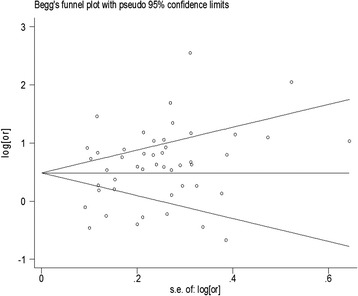
Funnel plot of hot beverages and foods and the risk of esophageal cancer.
Discussion
In this large pooled analysis of 42475 participants (13811 EC cases) from 39 case–control studies, we confirmed a positive association between hot beverage and food consumption and EC risk. Individuals who usually have beverages and food served very hot or hot were almost twice likely to develop EC than individuals who usually have beverages and foods served warm or cold. Our subgroup analyses show that the results held true across various populations despite significant heterogeneity.
Our meta-analysis shows that the consumption of hot beverages and foods are significantly associated with ESCC (OR, 1.60; 95% CI, 1.29–2.00) but not with EAC (0.79, 95% CI, 0.53–1.16). A large body of observational evidence suggests that the risk factors for ESCC and EAC may be different. For example, alcohol intake is a strong and well established risk factor for ESCC but it is not associated with EAC [54]; a high body mass index (BMI) is associated with an increased risk of EAC but a decreased risk of ESCC [55]; ESCC is strongly associated with high-level exposure to tobacco smoking in Western populations [54,56], whereas EAC is associated with gastro-esophageal reflux disease and Barrett’s esophagus [57]. More studies are needed to explore why hot beverage and food consumption is associated with an increased risk for ESCC but not EAC.
Another notable finding is that hot beverage and food consumption appears not to be a risk factor for EC in European population (OR, 0.95; 95% CI, 0.68–1.34). The result might be ascribed to the small sample size (3,728 participants and 1,039 EC cases) or the unique dietary habits of Europeans. A previous study noted that Europeans tend to add cold milk to the exposure beverages, tea or coffee before consumption [12], which may cause people say they drink hot actually only warm and result in substantial difference between the temperature perceived by drinkers and the actual temperature of their drinks.
It is conceivable that hot beverages and foods may cause thermal injury to the esophageal mucosa, and there are several biological mechanisms through which thermal injury in general could increase the risk of EC. Inflammatory processes associated with chronic irritation of the esophageal mucosa caused by local hyperthermia could stimulate the endogenous formation of reactive nitrogen species and nitrosamines [58]. This hypothesis is supported by a high rate of somatic G to A transitions in CpG dinucleotides of the TP53 gene in esophageal tumor samples from geographical areas in which drinking hot beverages is considered an important risk factor for EC [59-62]; these mutations may indicate increased nitric oxide synthase activity in tumors [63]. The barrier function of the esophageal epithelium can be impaired by thermal injury, which may increase the risk of damage from exposure to intraluminal carcinogens [10], such as polycyclic aromatic hydrocarbons. Elevated temperatures could also accelerate metabolic reaction, including those with carcinogenic substances in tobacco and alcohol [64]. In fact, the association between consuming hot drinks and the occurrence of precancerous lesions of the esophagus has been repeatedly reported [65-67]. In addition, dietary deficiencies may weaken the esophageal tissue because of the constant irritation, which may act as a predisposing factor for EC [47]. It has also been postulated that contact of hot liquid and food with the esophageal mucosa could increase gastric reflux, causing further damage from gastric acid [68]. One review proposed that the overproduction of prostaglandin E2 and leukotriene B4 as well as overexpression of their receptors are major factors in exacerbating inflammation and oxidative stress, which is the main pathogenesis associated with EAC [57]. The result from our meta-analysis of epidemiological studies is consistent with these biomedical research findings and postulations.
All the original studies used in our meta-analysis are of case–control study design, which is particularly vulnerable to potential biases (both selection bias and information bias). The included studies were conducted among different populations, mostly along with various categorizations of beverages and foods, which could confound our analysis on the specific link between the temperature of beverages and foods and the risk of EC. Lastly, the study relied on self-reported consumption of hot beverages and foods; as a result, the categorization of “hot or very hot” versus “cold or warm” is subject to reporting bias. In addition, the limited information provided in the included studies ruled out the possibility of conducting a dose–response analysis. Nonetheless, this is the first meta-analysis to systematically quantify the association between hot beverage and food consumption and EC risk, and the results of our study are of broad interest to medical science and the public since consumption of beverages such as tea, coffee, and maté are prevalent worldwide [64,69,70] and many people prefer to drink them at a high or very high temperature [15,71].
In the light of our findings, certain factors should be considered in future studies. Large prospective studies are needed to investigate the association of hot beverage and food consumption with both EC risk and the type of EC, not only because of the different ESCC and EAC risk factors but also the rapid changes in incidence of EAC [12]. In addition, measuring the actual temperature of hot beverage and food would provide dose–response data that would allow for evaluation of the relationship with EC risk more precisely. Finally, confounding factors, such as BMI, smoking, alcohol intake, and socioeconomic status, should be adjusted to allow dissection of the actual influence of hot beverage and food on EC, thereby providing provide stronger research-based evidence.
Conclusions
In summary, our meta-analysis shows that hot beverage and food consumption is associated with a significantly increase in the risk of EC, especially in Asian and South American populations. Given that hot beverages and foods are prevalent in modern society, the results of our meta-analysis have important implications for cancer etiology research as well as applications in health education and clinical practice.
Ethics approval
Ethical approval is not required for this review.
Acknowledgements
We thank all the authors of the studies included in our meta-analysis.
Funding
No funding was received for this systematic review.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
YWC, CY, SYC and ZXL designed the study. YWC, CY, HLS and HSB carried out the data collection. YWC, CY, YQT and YG performed the statistical analyses. YWC, CY, GY, HLS and XXY drafted the manuscript. All authors read and approved the final manuscript.
Contributor Information
Yawen Chen, Email: cyw2013shuxue@hotmail.com.
Yeqing Tong, Email: tongyeqing9999@sina.com.
Chen Yang, Email: julianmitz@163.com.
Yong Gan, Email: scswj2008@163.com.
Huilian Sun, Email: hl_sun_health@163.com.
Huashan Bi, Email: bihuashan@yeah.net.
Shiyi Cao, Email: 313704102@qq.com.
Xiaoxv Yin, Email: hnyinxiaoxv@126.com.
Zuxun Lu, Email: zuxunlu@yahoo.com.
References
- 1.Kamangar F, Dores GM, Anderson WF. Patterns of cancer incidence, mortality, and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol. 2006;24(14):2137–2150. doi: 10.1200/JCO.2005.05.2308. [DOI] [PubMed] [Google Scholar]
- 2.Andrici J, Eslick GD. Mate consumption and the risk of esophageal squamous cell carcinoma: a meta-analysis. Dis Esophagus. 2013;26(8):807–816. doi: 10.1111/j.1442-2050.2012.01393.x. [DOI] [PubMed] [Google Scholar]
- 3.Yu X, Bao Z, Zou J, Dong J. Coffee consumption and risk of cancers: a meta-analysis of cohort studies. BMC Cancer. 2011;11:96. doi: 10.1186/1471-2407-11-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morse MA, Kresty LA, Steele VE, Kelloff GJ, Boone CW, Balentine DA, et al. Effects of theaflavins on N-nitrosomethylbenzylamine-induced esophageal tumorigenesis. Nutr Cancer. 1997;29(1):7–12. doi: 10.1080/01635589709514595. [DOI] [PubMed] [Google Scholar]
- 5.Candreva EC, Keszenman DJ, Barrios E, Gelos U, Nunes E. Mutagenicity induced by hyperthermia, hot mate infusion, and hot caffeine in Saccharomyces cerevisiae. Cancer Res. 1993;53(23):5750–5753. [PubMed] [Google Scholar]
- 6.Garidou A, Tzonou A, Lipworth L, Signorello LB, Kalapothaki V, Trichopoulos D. Life-style factors and medical conditions in relation to esophageal cancer by histologic type in a low-risk population. Int J Cancer. 1996;68(3):295–299. doi: 10.1002/(SICI)1097-0215(19961104)68:3<295::AID-IJC5>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 7.Terry JL P, Wolk A, Nyrén O. Drinking hot beverages is not associated with risk of oesophageal cancers in a Western population. Br J Cancer. 2001;84:120–121. doi: 10.1054/bjoc.2000.1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sharp L, Chilvers CE, Cheng KK, McKinney PA, Logan RF, Cook-Mozaffari P, et al. Risk factors for squamous cell carcinoma of the oesophagus in women: a case–control study. Br J Cancer. 2001;85(11):1667–1670. doi: 10.1054/bjoc.2001.2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Islami F, Boffetta P, Ren J-S, Pedoeim L, Khatib D, Kamangar F. High-temperature beverages and foods and esophageal cancer risk-A systematic review. Int J Cancer. 2009;125(3):491–524. doi: 10.1002/ijc.24445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tobey NA, Sikka D, Marten E, Caymaz-Bor C, Hosseini SS, Orlando RC. Effect of heat stress on rabbit esophageal epithelium. Am J Physiol. 1999;276(6 Pt 1):G1322–1330. doi: 10.1152/ajpgi.1999.276.6.G1322. [DOI] [PubMed] [Google Scholar]
- 11.Castellsague X, Munoz N, De Stefani E, Victora CG, Castelletto R, Rolon PA. Influence of mate drinking, hot beverages and diet on esophageal cancer risk in South America. Int J Cancer. 2000;88(4):658–664. doi: 10.1002/1097-0215(20001115)88:4<658::AID-IJC22>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 12.Ibiebele TI, Taylor AR, Whiteman DC, van der Pols JC. Eating habits and risk of esophageal cancers: a population-based case–control study. Cancer Causes Control. 2010;21(9):1475–1484. doi: 10.1007/s10552-010-9576-8. [DOI] [PubMed] [Google Scholar]
- 13.Wu M, Zhao JK, Hu XS, Wang PH, Qin Y, Lu YC, et al. Association of smoking, alcohol drinking and dietary factors with esophageal cancer in high- and low-risk areas of Jiangsu Province, China. World J Gastroenterol. 2006;12(11):1686–1693. doi: 10.3748/wjg.v12.i11.1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Steiner PE. The etiology and histogenesis of carcinoma of the esophagus. Cancer. 1956;9(3):436–452. doi: 10.1002/1097-0142(195605/06)9:3<436::AID-CNCR2820090303>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 15.Islami F, Pourshams A, Nasrollahzadeh D, Kamangar F, Fahimi S, Shakeri R, et al. Tea drinking habits and oesophageal cancer in a high risk area in northern Iran: population based case–control study. BMJ. 2009;338:b929. doi: 10.1136/bmj.b929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lubin JH, De Stefani E, Abnet CC, Acosta G, Boffetta P, Victora C, et al. Mate drinking and esophageal squamous cell carcinoma in South America: pooled results from two large multicenter case–control studies. Cancer Epidemiol Biomarkers Prev. 2014;23(1):107–116. doi: 10.1158/1055-9965.EPI-13-0796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 18.Wells G SB OCD, Peterson J, Welch V, Losos M. The Newcastle - Scale for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm
- 19.Tang L, Xu F, Zhang T, Lei J, Binns CW, Lee AH. High temperature of food and beverage intake increases the risk of oesophageal cancer in Xinjiang, China. Asian Pac J Cancer Prev. 2013;14(9):5085–5088. doi: 10.7314/APJCP.2013.14.9.5085. [DOI] [PubMed] [Google Scholar]
- 20.Wu M, Liu AM, Kampman E, Zhang ZF, Van’t Veer P, Wu DL, et al. Green tea drinking, high tea temperature and esophageal cancer in high- and low-risk areas of Jiangsu Province, China: a population-based case–control study. Int J Cancer. 2009;124(8):1907–1913. doi: 10.1002/ijc.24142. [DOI] [PubMed] [Google Scholar]
- 21.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 22.Wallace BC, Schmid CH, Lau J, Trikalinos TA. Meta-analyst: software for meta-analysis of binary, continuous and diagnostic data. BMC Med Res Methodol. 2009;9:80. doi: 10.1186/1471-2288-9-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–1101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- 24.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen YK, Lee CH, Wu IC, Liu JS, Wu DC, Lee JM, et al. Food intake and the occurrence of squamous cell carcinoma in different sections of the esophagus in Taiwanese men. Nutrition. 2009;25(7–8):753–761. doi: 10.1016/j.nut.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 26.Chen Z, Chen Q, Xia H, Lin J. Green tea drinking habits and esophageal cancer in southern China: a case–control study. Asian Pac J Cancer Prev. 2011;12(1):229–233. [PubMed] [Google Scholar]
- 27.Cheng KK, Day NE, Duffy SW, Lam TH, Fok M, Wong J. Pickled vegetables in the aetiology of oesophageal cancer in Hong Kong Chinese. Lancet. 1992;339(8805):1314–1318. doi: 10.1016/0140-6736(92)91960-G. [DOI] [PubMed] [Google Scholar]
- 28.Gao Y, Hu N, Han XY, Ding T, Giffen C, Goldstein AM, et al. Risk factors for esophageal and gastric cancers in Shanxi Province, China: a case–control study. Cancer Epidemiol. 2011;35(6):e91–99. doi: 10.1016/j.canep.2011.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gao YT, McLaughlin JK, Blot WJ, Ji BT, Dai Q, Fraumeni JF., Jr Reduced risk of esophageal cancer associated with green tea consumption. J Natl Cancer Inst. 1994;86(11):855–858. doi: 10.1093/jnci/86.11.855. [DOI] [PubMed] [Google Scholar]
- 30.Gao YT, McLaughlin JK, Gridley G, Blot WJ, Ji BT, Dai Q, et al. Risk factors for esophageal cancer in Shanghai, China. II. Role of diet and nutrients. Int J Cancer. 1994;58(2):197–202. doi: 10.1002/ijc.2910580209. [DOI] [PubMed] [Google Scholar]
- 31.Guo W, Blot WJ, Li JY, Taylor PR, Liu BQ, Wang W, et al. A nested case–control study of oesophageal and stomach cancers in the Linxian nutrition intervention trial. Int J Epidemiol. 1994;23(3):444–450. doi: 10.1093/ije/23.3.444. [DOI] [PubMed] [Google Scholar]
- 32.Hu J, Nyren O, Wolk A, Bergstrom R, Yuen J, Adami HO, et al. Risk factors for oesophageal cancer in northeast China. Int J Cancer. 1994;57(1):38–46. doi: 10.1002/ijc.2910570108. [DOI] [PubMed] [Google Scholar]
- 33.Hung HC, Huang MC, Lee JM, Wu DC, Hsu HK, Wu MT. Association between diet and esophageal cancer in Taiwan. J Gastroenterol Hepatol. 2004;19(6):632–637. doi: 10.1111/j.1440-1746.2004.03346.x. [DOI] [PubMed] [Google Scholar]
- 34.Ke L, Yu P, Zhang ZX, Huang SS, Huang G, Ma XH. Congou tea drinking and oesophageal cancer in South China. Br J Cancer. 2002;86(3):346–347. doi: 10.1038/sj.bjc.6600054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lin J, Zeng R, Cao W, Luo R, Chen J, Lin Y. Hot beverage and food intake and esophageal cancer in southern China. Asian Pac J Cancer Prev. 2011;12(9):2189–2192. [PubMed] [Google Scholar]
- 36.Sun X, Chen W, Chen Z, Wen D, Zhao D, He Y. Population-based case–control study on risk factors for esophageal cancer in five high-risk areas in China. Asian Pac J Cancer Prev. 2010;11(6):1631–1636. [PubMed] [Google Scholar]
- 37.Wang JM, Xu B, Rao JY, Shen HB, Xue HC, Jiang QW. Diet habits, alcohol drinking, tobacco smoking, green tea drinking, and the risk of esophageal squamous cell carcinoma in the Chinese population. Eur J Gastroenterol Hepatol. 2007;19(2):171–176. doi: 10.1097/MEG.0b013e32800ff77a. [DOI] [PubMed] [Google Scholar]
- 38.Yang CX, Wang HY, Wang ZM, Du HZ, Tao DM, Mu XY, et al. Risk factors for esophageal cancer: a case–control study in South-western China. Asian Pac J Cancer Prev. 2005;6(1):48–53. [PubMed] [Google Scholar]
- 39.De Stefani E, Boffetta P, Deneo-Pellegrini H, Ronco AL, Correa P, Mendilaharsu M. The role of vegetable and fruit consumption in the aetiology of squamous cell carcinoma of the oesophagus: a case–control study in Uruguay. Int J Cancer. 2005;116(1):130–135. doi: 10.1002/ijc.20950. [DOI] [PubMed] [Google Scholar]
- 40.De Stefani E, Boffetta P, Ronco AL, Deneo-Pellegrini H, Correa P, Acosta G, et al. Exploratory factor analysis of squamous cell carcinoma of the esophagus in Uruguay. Nutr Cancer. 2008;60(2):188–195. doi: 10.1080/01635580701630487. [DOI] [PubMed] [Google Scholar]
- 41.De Stefani E, Deneo-Pellegrini H, Ronco AL, Boffetta P, Brennan P, Munoz N, et al. Food groups and risk of squamous cell carcinoma of the oesophagus: a case–control study in Uruguay. Br J Cancer. 2003;89(7):1209–1214. doi: 10.1038/sj.bjc.6601239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sewram V, De Stefani E, Brennan P, Boffetta P. Mate consumption and the risk of squamous cell esophageal cancer in uruguay. Cancer Epidemiol Biomarkers Prev. 2003;12(6):508–513. [PubMed] [Google Scholar]
- 43.Castelletto R, Castellsague X, Munoz N, Iscovich J, Chopita N, Jmelnitsky A. Alcohol, tobacco, diet, mate drinking, and esophageal cancer in Argentina. Cancer Epidemiol Biomarkers Prev. 1994;3(7):557–564. [PubMed] [Google Scholar]
- 44.Szymanska K, Matos E, Hung RJ, Wunsch-Filho V, Eluf-Neto J, Menezes A, et al. Drinking of mate and the risk of cancers of the upper aerodigestive tract in Latin America: a case–control study. Cancer Causes Control. 2010;21(11):1799–1806. doi: 10.1007/s10552-010-9606-6. [DOI] [PubMed] [Google Scholar]
- 45.Rolon PA, Castellsague X, Benz M, Munoz N. Hot and cold mate drinking and esophageal cancer in Paraguay. Cancer Epidemiol Biomarkers Prev. 1995;4(6):595–605. [PubMed] [Google Scholar]
- 46.Khan NA, Teli MA, Mohib-Ul Haq M, Bhat GM, Lone MM, Afroz F. A survey of risk factors in carcinoma esophagus in the valley of Kashmir, Northern India. J Cancer Res Ther. 2011;7(1):15–18. doi: 10.4103/0973-1482.80431. [DOI] [PubMed] [Google Scholar]
- 47.Phukan RK, Chetia CK, Ali MS, Mahanta J. Role of dietary habits in the development of esophageal cancer in Assam, the north-eastern region of India. Nutr Cancer. 2001;39(2):204–209. doi: 10.1207/S15327914nc392_7. [DOI] [PubMed] [Google Scholar]
- 48.Srivastava M, Kapil U, Chattopadhyay TK, Shukla NK, Sundaram KR, Sekaran G, et al. Nutritional factors in carcinoma oesophagus: a case–control study. Asia Pac J Clin Nutr. 1997;6(2):96–98. [PubMed] [Google Scholar]
- 49.Cook-Mozaffari PJ, Azordegan F, Day NE, Ressicaud A, Sabai C, Aramesh B. Oesophageal cancer studies in the Caspian Littoral of Iran: results of a case–control study. Br J Cancer. 1979;39(3):293–309. doi: 10.1038/bjc.1979.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jessri M, Rashidkhani B, Hajizadeh B, Gotay C. Macronutrients, vitamins and minerals intake and risk of esophageal squamous cell carcinoma: a case–control study in Iran. Nutr J. 2011;10:137. doi: 10.1186/1475-2891-10-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cheng KK, Sharp L, McKinney PA, Logan RF, Chilvers CE, Cook-Mozaffari P, et al. A case–control study of oesophageal adenocarcinoma in women: a preventable disease. Br J Cancer. 2000;83(1):127–132. doi: 10.1054/bjoc.2000.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Patel K, Wakhisi J, Mining S, Mwangi A, Patel R. Esophageal cancer, the topmost cancer at MTRH in the Rift Valley, Kenya, and its potential risk factors. ISRN Oncol. 2013;2013:503249. doi: 10.1155/2013/503249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hanaoka T, Tsugane S, Ando N, Ishida K, Kakegawa T, Isono K, et al. Alcohol consumption and risk of esophageal cancer in Japan: a case–control study in seven hospitals. Jpn J Clin Oncol. 1994;24(5):241–246. [PubMed] [Google Scholar]
- 54.Freedman ND, Murray LJ, Kamangar F, Abnet CC, Cook MB, Nyren O, et al. Alcohol intake and risk of oesophageal adenocarcinoma: a pooled analysis from the BEACON Consortium. Gut. 2011;60(8):1029–1037. doi: 10.1136/gut.2010.233866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lindkvist B, Johansen D, Stocks T, Concin H, Bjorge T, Almquist M, et al. Metabolic risk factors for esophageal squamous cell carcinoma and adenocarcinoma: a prospective study of 580,000 subjects within the Me-Can project. BMC Cancer. 2014;14:103. doi: 10.1186/1471-2407-14-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Holmes RS, Vaughan TL. Epidemiology and pathogenesis of esophageal cancer. Semin Radiat Oncol. 2007;17(1):2–9. doi: 10.1016/j.semradonc.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 57.Chen X, Yang CS. Esophageal adenocarcinoma: a review and perspectives on the mechanism of carcinogenesis and chemoprevention. Carcinogenesis. 2001;22(8):1119–1129. doi: 10.1093/carcin/22.8.1119. [DOI] [PubMed] [Google Scholar]
- 58.Mirvish SS. Role of N-nitroso compounds (NOC) and N-nitrosation in etiology of gastric, esophageal, nasopharyngeal and bladder cancer and contribution to cancer of known exposures to NOC. Cancer Lett. 1995;93(1):17–48. doi: 10.1016/0304-3835(95)03786-V. [DOI] [PubMed] [Google Scholar]
- 59.Breton JSF, Abbas A, Marnay J, Arsene D, Lechevrel M. Simultaneous use of DGGE and DHPLC to screen TP53 mutations in cancers of the esophagus and cardia from a European high incidence area (Lower Normandy, France) Mutagenesis. 2003;18:299–306. doi: 10.1093/mutage/18.3.299. [DOI] [PubMed] [Google Scholar]
- 60.Firouzeh Biramijamal AA, Parvin M, Hermann-Josef G, Reet K, Monica H. Unusual profile and high prevalence of p53 mutations in esophageal squamous cell carcinomas from Northern Iran. Cancer Res. 2001;61:3119–3123. [PubMed] [Google Scholar]
- 61.Putz A, Hartmann AA, Fontes PR, Alexandre CO, Silveira DA, Klug SJ, et al. TP53 mutation pattern of esophageal squamous cell carcinomas in a high risk area (Southern Brazil): role of life style factors. Int J Cancer. 2002;98(1):99–105. doi: 10.1002/ijc.10128. [DOI] [PubMed] [Google Scholar]
- 62.Sepehr A, Taniere P, Martel-Planche G, Zia’ee AA, Rastgar-Jazii F, Yazdanbod M, et al. Distinct pattern of TP53 mutations in squamous cell carcinoma of the esophagus in Iran. Oncogene. 2001;20(50):7368–7374. doi: 10.1038/sj.onc.1204912. [DOI] [PubMed] [Google Scholar]
- 63.Wang LD, Zhou Q, Feng CW, Liu B, Qi YJ, Zhang YR, et al. Intervention and follow-up on human esophageal precancerous lesions in Henan, northern China, a high-incidence area for esophageal cancer. Gan To Kagaku Ryoho. 2002;29(Suppl 1):159–172. [PubMed] [Google Scholar]
- 64.Loria D, Barrios E, Zanetti R. Cancer and yerba mate consumption: a review of possible associations. Rev Panam Salud Publica. 2009;25(6):530–539. doi: 10.1590/S1020-49892009000600010. [DOI] [PubMed] [Google Scholar]
- 65.Munoz N, Crespi M, Grassi A, Qing WG, Qiong S, Cai LZ. Precursor lesions of oesophageal cancer in high-risk populations in Iran and China. Lancet. 1982;1(8277):876–879. doi: 10.1016/S0140-6736(82)92151-1. [DOI] [PubMed] [Google Scholar]
- 66.Munoz N, Victora CG, Crespi M, Saul C, Braga NM, Correa P. Hot mate drinking and precancerous lesions of the oesophagus: an endoscopic survey in southern Brazil. Int J Cancer. 1987;39(6):708–709. doi: 10.1002/ijc.2910390609. [DOI] [PubMed] [Google Scholar]
- 67.Wahrendorf J, Chang-Claude J, Liang QS, Rei YG, Munoz N, Crespi M, et al. Precursor lesions of oesophageal cancer in young people in a high-risk population in China. Lancet. 1989;2(8674):1239–1241. doi: 10.1016/S0140-6736(89)91850-3. [DOI] [PubMed] [Google Scholar]
- 68.Ghadirian P. Thermal irritation and esophageal cancer in northern Iran. Cancer. 1987;60(8):1909–1914. doi: 10.1002/1097-0142(19871015)60:8<1909::AID-CNCR2820600840>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 69.Kuriyama S, Shimazu T, Ohmori K, Kikuchi N, Nakaya N, Nishino Y, et al. Green tea consumption and mortality due to cardiovascular disease, cancer, and all causes in Japan: the Ohsaki study. JAMA. 2006;296(10):1255–1265. doi: 10.1001/jama.296.10.1255. [DOI] [PubMed] [Google Scholar]
- 70.Organization FaA: food balance sheets. http://www.fao.org/.
- 71.Cheng KK, Day NE. Nutrition and esophageal cancer. Cancer Causes Control. 1996;7(1):33–40. doi: 10.1007/BF00115636. [DOI] [PubMed] [Google Scholar]


