Abstract
Background
Empirical literature indicates that the therapeutic alliance explains a modest but reliable proportion of variance in predicting alcohol-related outcomes among individuals in treatment for alcohol use disorders (AUDs). Hartzler and colleagues (2011) showed in the COMBINE data set that alcohol abstinence self-efficacy is a potentially important statistical mediator of the relationship between the alliance and client outcomes.
Methods
The purpose of this study was to replicate this finding in the Project MATCH data set. We used total alliance ratings on the Working Alliance Inventory and tested both client and therapist ratings in mediation analyses.
Results
We found that posttreatment self-efficacy accounted for the effect of therapist and client ratings of alliance (measured at session 2) on posttreatment drinking outcomes (drinks per drinking day and alcohol-related problems). In addition, we found a moderation effect of treatment, such that the association between the client’s rating of the alliance and self-efficacy changes was positive for individuals in the cognitive behavioral treatment group but negative for those receiving motivation enhancement or Twelve-Step Facilitation.
Conclusions
This study reaffirms the importance of the therapeutic alliance and self-efficacy in predicting AUD outcomes. Future research should examine changes in the therapeutic alliance throughout treatment and how these changes are related to self-efficacy and AUD treatment outcomes over time.
Keywords: Therapeutic Alliance, Abstinence Self-Efficacy, Alcohol Use Disorder, Alcohol Treatment Outcomes, Project MATCH
The therapeutic alliance has long been viewed in the psychotherapy literature as an important variable in the behavior change process and is currently considered a major “common factor” in psychotherapy outcomes (Wampold, 2010), including psychological treatments for alcohol use disorder (AUD). The therapeutic alliance centers on the quality of the collaborative relationship between the therapist and patient. Several components between the therapist and patient are thought to constitute the therapeutic alliance, including sharing common goals, completing tasks, building trust, nonjudgment, empathy, and having positive feelings toward one another (Summers and Barber, 2003). There is wide agreement that the alliance is a significant treatment process variable in AUD treatment (as well as treatments for other substance use disorders) and a predictor of client outcomes (Meier et al., 2005).
Connors and colleagues (1997) stimulated research on the therapeutic alliance in AUD treatment in their analyses of data from Project MATCH (Project Matching Alcoholism Treatments to Client Heterogeneity; Project MATCH Research Group, 1997). Briefly, Project MATCH was a national (United States) multisite clinical trial (Project MATCH Research Group, 1997) that involved the random assignment of outpatient and inpatient clients with AUD to one of the three 12-week treatment conditions. Results from the Connors and colleagues (1997) study showed that among the outpatient sample rating of the alliance at treatment session 2 by either the client or the therapist (as measured by total scores on the Working Alliance Inventory [WAI]; Horvath and Greenberg, 1989) predicted both greater treatment engagement and positive drinking-related outcomes during and following treatment. However, in the aftercare sample, the client ratings of alliance were unrelated to drinking outcomes, and therapist ratings of alliance only predicted percentage of days abstinent during and following treatment. Although the effect sizes were not large, the findings from Connors and colleagues (1997) inspired additional research on therapeutic alliance in AUD treatment.
Connors and colleagues (1997) found little evidence of a treatment-by-alliance interaction in predicting treatment engagement or drinking outcomes. Ilgen and colleagues (2006) reasoned that it might be useful to look within treatments in investigations of the utility of the alliance in predicting client outcomes. Further, Ilgen and colleagues (2006) hypothesized that client self-efficacy (to sustain abstinence from alcohol) would moderate any effects of the alliance, because individuals who are lower in self-efficacy tend to be more influenced by external factors, including their therapist (Bandura, 1997). In particular, they hypothesized that stronger alliance would be especially beneficial for clients with low self-efficacy. Analyses of the Project MATCH outpatient data confirmed this hypothesis by demonstrating a significant interaction between early treatment alliance and self-efficacy in predicting 1-year percentage of days abstinent and drinks per drinking day [DDD], but only for the therapists’ ratings of the alliance (Ilgen et al., 2006).
Although Ilgen and colleagues (2006) found that self-efficacy moderated the effects of alliance, there are also good reasons to hypothesize that changes in self-efficacy mediate the association between alliance and AUD treatment outcomes. For example, Hartzler and colleagues (2011) used data from the COMBINE study (COMBINE Study Research Group, 2003) to test whether changes in alcohol abstinence self-efficacy mediated the relationship between client ratings of the therapeutic bond (1 component of the therapeutic alliance as measured by the WAI) and client outcomes. Results indicated that changes in self-efficacy significantly mediated the association between client ratings of therapeutic bond and percentage drinking days, alcohol consequences, and psychiatric functioning at 12-month follow-up, but only for those who received only the “combination behavioral intervention” (no medical management and no medications, including placebo).
Altogether, the literature to date illustrates the importance of the therapeutic alliance in explaining a modest but consistent proportion of variance in predicting alcohol use and related outcomes of AUD treatment, independent of multiple other predictors. Furthermore, alcohol abstinence self-efficacy has emerged in recent research as a potentially important construct in the relationship between the alliance and alcohol-related outcomes. These initial findings concerning self-efficacy have important implications for advancing the understanding of the alliance–AUD patient outcomes relationship, as well as for clinical practice in demonstrating that the negative relationship between client self-efficacy and treatment outcome may be compensated for to some degree by a strong therapeutic alliance, at least as the therapist perceives it. Accordingly, the purpose of this study was to investigate further the alcohol abstinence self-efficacy statistical mediation effect by replicating and extending the Hartzler and colleagues (2011) study in the Project MATCH outpatient sample. In the study reported here, a multivariate parallel process growth model was derived from the studies cited in this paper as well as in the general literature on AUD clinical course and outcome (McKay, 2009), and this model was tested on each of 3 outcome variables: PDD, DDD, and negative alcohol-related consequences.
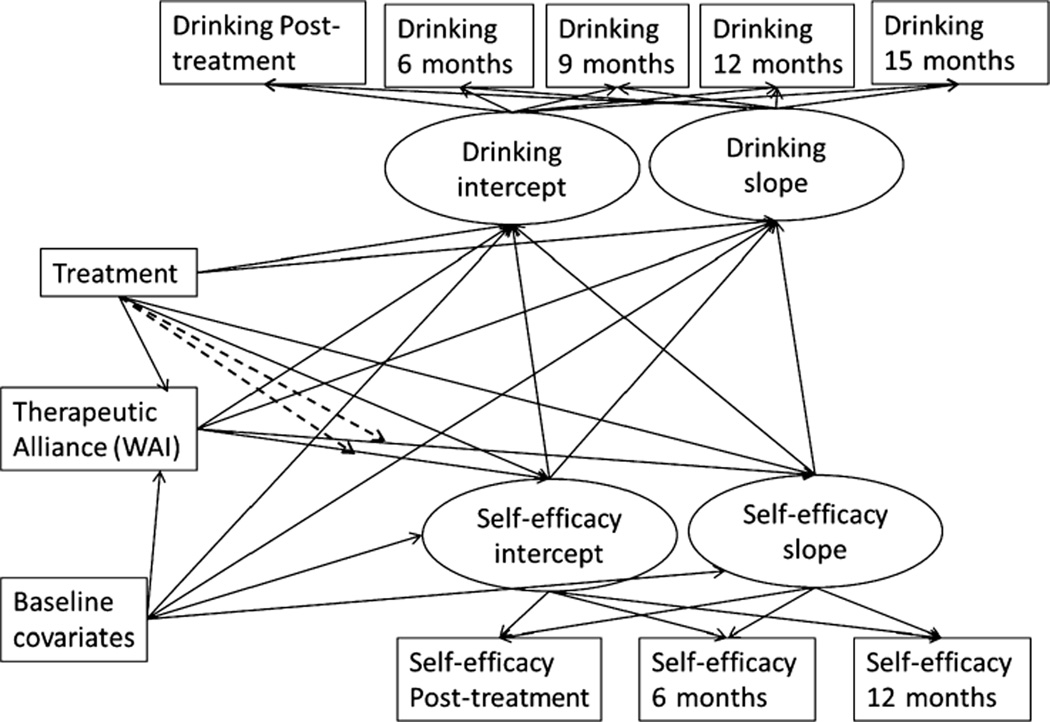
The hypothesized theoretical model is presented in Fig. 1. As can be seen in Fig. 1, treatment condition was hypothesized to have direct effects on the therapeutic alliance, abstinence self-efficacy from 3 months (immediately after treatment completion, “self-efficacy intercept”) to 12 months following treatment completion, and drinking outcomes from 3 months (“drinking intercept”) to 12 months following treatment completion. In this regard, participants in the Motivational Enhancement Therapy (MET) condition were predicted to report the strongest levels of alliance, due to MET’s more explicit emphasis on the therapeutic relationship as a vehicle of change (Miller and Rose, 2009). In addition, participants in the Cognitive Behavioral Therapy (CBT) condition were hypothesized to show the highest levels of self-efficacy. This prediction followed from CBT’s explicit emphasis on building skills to change behavior, which in turn enhances self-efficacy to make and sustain such changes. Treatment condition also was hypothesized to moderate the association between alliance and self-efficacy. The alliance change in self-efficacy relationship was expected to be positive and strongest among participants in the CBT group, because of CBT’s emphasis on building that expectation and behavioral skills to substantiate it. In this regard, we hypothesized that in CBT, the course of drinking-related self-efficacy is more sensitive to client-reported alliance than it is in MET or Twelve-Step Facilitation (TSF), which do not place as explicit an emphasis on developing drinking-related behavioral self-efficacy as CBT does. Consistent with a number of previous studies, both the therapeutic alliance and self-efficacy were predicted to have direct effects on client outcomes. The statistical mediation effect of central interest was the alliance–self-efficacy outcomes relationship. However, the treatment alliance–self-efficacy outcomes statistical mediation effect was also tested. It is important to note that this study provides an extension of Connors and colleagues (1997) and Hartzler and colleagues (2011) in 3 main ways. First, we examined a new drinking outcome while retaining 2 of 3 drinking outcomes identical to those of Hartzler and colleagues (percent days drinking [PDD] and alcohol-related negative consequences). Second, Connors and colleagues (1997) tested treatment effects as part of their statistical models but used an omnibus test approach in doing so. In the current study, 2 planned contrasts comparing respective pairs of treatment conditions were tested. Third, both Hartzler and colleagues (2011) and Connors and colleagues (1997) tested 1-year outcomes, whereas in the current study, all of the longitudinal data were including in the model, as represented in our testing for the significance of the slope of self-efficacy and alcohol-related outcomes, respectively, over time.
Fig. 1.
Hypothesized parallel process growth model of drinking and self-efficacy, predicted by therapeutic alliance and treatment, as well as the treatment-by-alliance moderation effect (indicated by dashed lines).
MATERIALS AND METHODS
This secondary data analysis was conducted using data from Project MATCH. A total of 1,726 participants were recruited from 9 different sites across the United States and were randomized to 1 of 3 treatment conditions for AUDs: CBT (Kadden et al., 1992), MET (Miller et al., 1992), or TSF (Nowinski et al., 1992). Among the full sample, 952 were outpatients and 774 were aftercare clients. This study only examined data from the outpatient arm, because previous studies using Project MATCH data have found that the alliance predicts client outcomes more reliably in the outpatient sample (Connors et al., 1997), and subsequent research investigating the effects of the alliance and self-efficacy on outcomes has used the outpatient Project MATCH sample (Ilgen et al., 2006). Eligibility criteria for participants in Project MATCH’s outpatient arm included a current DSM-III-R diagnosis of Alcohol Abuse or Dependence, actively drinking during the 3 months preceding study entrance, being at least 18 years of age, and having at least a 6th grade reading level. Assessment time points included baseline, 3 months (immediately posttreatment), 6 months (3 months posttreatment), 9, 12, and 15 months (12 months posttreatment). More detailed information about the study design and procedures is in Project MATCH Research Group (1993).
Participants
The full outpatient sample included 952 participants, 27.7% female, 80% non-Hispanic White, 35.5% married, average age of 38.9 (SD = 10.7), and average years of education of 13.4 (SD = 2.2). Only participants who had all available data for the covariates (described later) were included in the analyses for this study, which reduced the sample size to n = 755 (79% of full outpatient sample) for the WAI Client models and n = 743 (78% of full outpatient sample) for the WAI Therapist models (given greater missing data for WAI Therapist scores). Individuals’ data in these subsamples used for the current analyses had no significant difference in client demographics between the WAI Client models and the WAI Therapist models.
Measures
Project MATCH involved the administration of an extensive battery of measures. These have been described in detail in several of the major publications from Project MATCH (e.g., Project MATCH Research Group, 1997). The analyses completed for this study and reported in this paper included data from a baseline demographic questionnaire, the Alcohol Abstinence Self-Efficacy Scale (AASE; DiClemente et al., 1994), the WAI (Horvath and Greenberg, 1989), the Form 90 (Miller, 1996), and the Drinker Inventory of Consequences (DrInC; Miller et al., 1995). The WAI was administered during the second treatment session. The AASE was measured at baseline and 3-, 9-, and 15-month follow-ups, which corresponded to immediately posttreatment (3 months), 6 months posttreatment (9-month follow-up), and 12 months posttreatment (15-month follow-up). The Form 90 and DrInC were measured in 90-day intervals at baseline and 3-, 6-, 9-, 12-, and 15-month follow-ups, which corresponded to posttreatment (3 months), 3 months posttreatment (6-month follow-up), 6 months posttreatment (9-month follow-up), 9 months posttreatment (12-month follow-up), and 12 months posttreatment (15-month follow-up).
The 3-, 9-, and 15-month follow-up interviews (Connors et al., 1994) were considered major participant evaluation points by the Project MATCH Research Group and included the majority of baseline assessments, blood and urine samples, and collateral interviews (i.e., interviews with individuals who were familiar with the participants’ drinking). Overall, assessments were conducted with more than 90% of the participants completing the assessments across each of the originally scheduled follow-up points. The focus of this study was participant drinking and other information collected at the baseline assessment, therapeutic alliance during treatment, self-efficacy following treatment, and drinking data during the first year posttreatment.
Baseline Covariates
A number of variables were included as baseline covariates given the known association between these measures and drinking outcomes in prior analyses of the Project MATCH data. Specifically, we included demographic variables of education and gender, baseline readiness to change (as defined by scores on the University of Rhode Island Change Assessment [URI-CA] scale; DiClemente and Hughes, 1990), baseline alcohol dependence severity (as defined by scores on the Alcohol Dependence Scale [ADS]; Skinner and Horn, 1984), percent of treatment sessions attended, and baseline levels of self-efficacy (as measured by the AASE; DiClemente et al., 1994) and drinking outcomes, as measured by the Form 90 (Miller, 1996) and DrInC (Miller et al., 1995).
Self-Efficacy
The Confidence subscale of the AASE (DiClemente et al., 1994) was used to assess client confidence to abstain from alcohol in 20 different high-risk situations (e.g., “When I am feeling depressed”) via self-report ratings on a 5-point Likert-type scale (1 = Not at all likely to abstain; 5 = Extremely likely to abstain). The internal consistency reliabilities for the AASE ranged from α = 0.93 at baseline to α = 0.97 at the 12-month follow-up. AASE confidence scores at 3, 9, and 15 months were used as indicators in the latent growth model of self-efficacy.
Drinking Outcomes
The Form 90 was used to measure alcohol consumption (i.e., quantity/frequency) at baseline and at all follow-up assessments. As described by the Project MATCH Research Group (1997), Form 90 is administered by in-person interview to obtain retrospective self-reports of daily alcohol consumption. The Form 90 data were used to derive 2 measures of alcohol consumption that were the primary dependent variables in this study. The first, PDD, was defined in Project MATCH as the percentage of the total number of days in an interval in which the individual reported alcohol consumption. PDD is a measure of the frequency of drinking. DDD is a measure of drinking intensity or severity and in Project MATCH was defined as the average number of drinks per drinking occasion. In the Project MATCH data, the Form 90 data were summarized on a monthly basis; if an individual was abstinent for an entire month, then his/her DDD was zero for that month (Project MATCH Research Group, 1997). Consistent with prior Project MATCH publications, we transformed the PDD and DDD variables, using arcsine and square root transformations, respectively. We used the PDD and DDD at 3-, 6-, 9-, 12-, and 15-month follow-ups as indicators in the latent growth models of drinking outcomes. The DrInC (Miller et al., 1995) assessed alcohol-related consequences. Clients reported on a 4-point scale (1 = never, 4 = daily or almost daily) the frequency of 50 alcohol-related consequences (e.g., “My marriage or love relationship has been harmed by my drinking”). Internal consistency of DrInC in this sample ranged from α = 0.93 at baseline to α = 0.96 at the 12-month follow-up. We used the DrInC scores at 3-, 6-, 9-, 12-, and 15-month follow-ups as indicators in the latent growth models of drinking outcomes.
Therapeutic Alliance
The WAI (Horvath and Greenberg, 1989) includes paired therapist and client Likert-type ratings (1 = Never to 7 = Always) on 36 items (e.g., “We respect each other”) that are used to generate total alliance scores and subscales for therapeutic bond, goals, and tasks. The total WAI scores, as reported by the client and the therapist, were included as predictors of self-efficacy and drinking outcomes in separate models (i.e., WAI Client model and WAI Therapist model). For this study, we used the WAI scores from the second session of treatment. In this regard, although therapeutic alliance data were collected following multiple sessions of treatment in MATCH, about 95% of those data were collected following Session 2. However, Meier and colleagues’ (2005) review showed that the early alliance is positively related to substance use disorder treatment outcomes. The internal consistency of the client total score was α = 0.72, and the therapist total score was α = 0.71.
Analysis Plan
The associations between therapeutic self-efficacy, and drinking outcomes over time were assessed within a structural equation modeling framework using a parallel process growth model (Cheong et al., 2003; MacKinnon, 2008) to assess the association between self-efficacy (across the 3-, 9-, and 15-month follow-ups) and drinking outcomes over time (across the 3-, 6-, 9-, 12-, and 15-month follow-ups). Baseline measures of all outcomes and additional covariates, described earlier, were included as predictors of alliance, self-efficacy, and drinking outcomes. The moderating effects of treatment were investigated within the context of the larger model using interaction terms with continuous variables included in the interaction as mean-centered variables as recommended by Aiken and West (1991). Two contrast vectors were created to account for variance related to treatment condition. In the first contrast, individuals in the MET condition received a code (“score”) of + 1, TSF participants were coded −1, and CBT participants were coded 0. This contrast highlighted MET’s more explicit emphasis on the therapeutic relationship as noted earlier. In the second contrast, participants in the CBT group were coded +1, those in MET group were coded −1, and individuals in the TSF group were coded 0, reflecting CBT’s emphasis on building the skills that underlie perceptions of self-efficacy to abstain from alcohol, as cited earlier. This emphasis is particularly apparent when compared to MET, which is designed to impart self-efficacy but includes no explicit skill-building exercises to do so. Finally, mediation effects were examined using the products of coefficient approach with bootstrapping (1,000 bootstrapped samples) to obtain 95% confidence intervals of the mediated effects (MacKinnon, 2008).
All models were tested using Mplus version 7.1 (Muthén and Muthén, 2012). We were specifically interested in testing the moderation effects and mediating paths, but we were also ultimately concerned with achieving acceptable model fit. Model fit was evaluated by chi-square values, the root mean square error of approximation (RMSEA; Browne and Cudeck, 1993), and the comparative fit index (CFI; Bentler, 1990). Models with nonsignificant chi-square, RMSEA less than 0.06, and CFI greater than 0.95 were considered a good fit to the observed data (Hu and Bentler, 1999). Models with RMSEA lower than 0.08 and CFI greater than 0.90 were considered an acceptable fit to the observed data.
RESULTS
Descriptive Analyses
Correlations between primary study measures indicated that therapeutic alliance, as rated by clients and therapists, was not associated with baseline self-efficacy, but was significantly correlated with 3-month (posttreatment) and 9-month self-efficacy (in effect, both time points represent change in self-efficacy); 3-, 6-, 9-, and 12-month PDD; and 6-month DDD. Therapeutic alliance, as reported by the client, was also inversely correlated with 9-month DDD, whereas therapeutic alliance, as reported by the therapist, was also inversely correlated with 15-month PDD and 3-, 6-, 9-, and 12-month DDD. Posttreatment self-efficacy at all follow-ups was also significantly related to all follow-up drinking outcomes. Correlations and descriptive statistics for the baseline and 3- and 15-month time points are provided in Table 1; additional correlations are available upon request.
Table 1.
Correlations Between Some of the Primary Study Variables (Not Including Covariates and Not Including all Time Points)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1.WAI Client | 1.00 | |||||||||||||
| 2. WAI Therapist | 0.25* | 1.00 | ||||||||||||
| 3. AASE baseline | −0.03 | 0.00 | 1.00 | |||||||||||
| 4. AASE 3 months | 0.11* | 0.13* | 0.24* | 1.00 | ||||||||||
| 5. AASE 15 months | 0.06 | 0.05 | 0.21* | 0.38* | 1.00 | |||||||||
| 6. PDD baseline | 0.00 | 0.01 | −0.07* | −0.09* | −0.13* | 1.00 | ||||||||
| 7. PDD 3 months | −0.11* | −0.14* | −0.14* | −0.34* | −0.23* | 0.22* | 1.00 | |||||||
| 8. PDD 15 months | −0.07 | −0.09 | −0.12* | −0.23* | −0.43* | 0.31* | 0.43* | 1.00 | ||||||
| 9. DDD baseline | 0.02 | 0.00 | −0.06 | −0.02 | −0.03 | −0.02 | −0.01 | −0.11* | 1.00 | |||||
| 10. DDD 3 months | −0.06 | −0.09* | −0.10* | −0.27* | −0.18* | 0.04 | 0.56* | 0.18* | 0.25* | 1.00 | ||||
| 11. DDD 15 months | −0.05 | −0.07 | −0.08* | −0.18* | −0.34* | 0.02 | 0.19* | 0.41* | 0.27* | 0.34* | 1.00 | |||
| 12. DrlnC baseline | 0.09* | 0.09* | −0.16* | −0.04 | −0.06 | 0.13* | 0.03 | −0.11* | 0.38* | 0.13* | 0.04 | 1.00 | ||
| 13. DrlnC 3 months | −0.03 | −0.03 | −0.18* | −0.22* | −0.16* | 0.08 | 0.24* | −0.02 | 0.25* | 0.33* | 0.15* | 0.48* | 1.00 | |
| 14. DrlnC 15 months | 0.01 | 0.13* | −0.16* | −0.16* | −0.37* | 0.07 | 0.23* | 0.26* | 0.19* | 0.28* | 0.41* | 0.36* | 0.55* | 1.00 |
| Mean (SD) |
211.5 (24.2) |
191.7 (24.6) |
2.96 (0.8) |
3.46 (0.9) |
3.44 (1.1) |
66% (30%) |
19% (30%) |
27% (35%) |
13.4 (7.8) |
3.7 (6.4) |
5.0 (6.2) |
45.4 (21.5) |
32.4 (24.3) |
28.0 (22.9) |
p < 0.05. WAI, Working Alliance Inventory; AASE, Alcohol Abstinence Self-Efficacy Scale; PDD, percent drinking days; DDD, drinks per drinking day; DrlnC, Drinker Inventory of Consequences.
Parallel Process Growth Models
The results from the parallel process growth models are provided in Tables 2–5, with Table 2 including all of the covariate effects and Tables 3–5 including the effects of WAI reporter (client or therapist) on the 3 drinking outcomes (PDD: Table 3; DDD: Table 4; or DrInC: Table 5). All 6 models provided an adequate fit to the data, particularly based on RMSEA and CFI, for example, Table 2, PDD:χ2 (85) = 177.2, p < 0.001; RMSEA = 0.038; CFI = 0.968.
Table 2.
Parallel Process Growth Model with Percent Drinking Days (PDD) as Drinking Outcome and Client-Reported Therapeutic Alliance as Predictor with All Covariate Effects Included (n = 755), χ2 (85) = 177.2, p < 0.001; RMSEA = 0.04; CFI = 0.97
| Structural Parameters—Unstandardized Estimates B (SE) |
|||||
|---|---|---|---|---|---|
| Predictor | Intercept PDD | Slope PDD | Intercept self-efficacy | Slope self-efficacy | WAI Client |
| Intercept PDD | - | - | - | - | - |
| Slope PDD | - | - | - | - | - |
| Intercept self-efficacy | −0.30 (0.05)** | 0.03 (0.03) | - | - | - |
| Slope self-efficacy | 0.25 (0.19) | −0.61 (0.22)** | - | - | - |
| Age | 0.00 (0.02) | 0.001 (0.001) | −0.004 (0.00) | −0.002 (0.00) | 0.06 (0.08) |
| Education | 0.02 (0.01) | −0.001 (0.01) | 0.02 (0.02) | 0.004 (0.01) | −1.8 (0.37)** |
| Gender | 0.06 (0.04) | −0.07 (0.04) | 0.03 (0.07) | −0.13 (00.5)** | 0.76 (2.1) |
| Motivation | −0.01 (0.01) | 0.01 (0.01) | 0.02 (0.02) | 0.03 (0.01)* | 3.6 (0.48)** |
| Alcohol Dependence Scale | −0.001 (0.002) | −0.01 (0.002)* | 0.001 (0.00) | −0.004 (0.00) | −0.10 (0.10) |
| Baseline self-efficacy | 0.05 (0.03) | −0.02 (0.02) | 0.33 (0.05)** | −0.011 (0.03) | −1.5 (1.0) |
| Baseline PDD | 0.003 (0.001)** | 0.001 (0.001) | −0.002 (0.00) | 0.00 (0.00) | 0.01 (0.03) |
| TX code 1 | 0.05 (0.03)* | −0.001 (0.02) | −0.27 (0.32) | −0.02 (0.20) | 0.23 (1.2) |
| TX code 2 | 0.003 (0.03) | 0.002 (0.02) | 0.14 (0.33) | −0.48 (0.23)* | −0.36 (1.3) |
| % Sessions | −0.27 (0.09)** | 0.07 (0.07) | 0.66 (0.14)** | −0.10 (0.09) | 13.91 (3.7)** |
| WAI Client | 0.00 (0.001) | 0.00 (0.001) | 0.004 (0.00)** | −0.001 (0.001) | - |
| TX1 × WAI | - | - | 0.001 (0.00) | 0.00 (0.001) | - |
| TX2 × WAI | - | - | 0.00 (0.00) | 0.002 (0.001)* | - |
| R2 | 0.61 | 0.82 | 0.30 | 0.17 | 0.11 |
p < 0.05
p < 0.01; PDD, percent drinking days; WAI, Working Alliance Inventory; TX1, treatment code 1 (MET = 1, TSF = −1, CBT = 0); TX2, treatment code 2 (MET = −1, TSF = 0, CBT = 1); TX1 × WAI, treatment code 1 by WAI interaction; TX2 × WAI, treatment code 2 by WAI interaction; % Sessions, % of sessions attended.
Table 5.
DrInC as Outcome and Client-Reported WAI as Predictor (n = 755), χ2 (85) = 112.95, p = 0.03; RMSEA = 0.020; CFI = 0.990; DrInC as Outcome and Therapist-Reported WAI as Predictor (n = 743), χ2 (85) = 143.20, p < 0.001; RMSEA = 0.030; CFI = 0.977
| Structural Parameters—Unstandardized Estimates B (SE) |
|||||
|---|---|---|---|---|---|
| WAI Client | Intercept DrInC | Slope DrInC | Intercept self-efficacy | Slope self-efficacy | WAI Client |
| TX code 1 | 0.15 (0.15) | 0.03 (0.12) | −0.25 (0.35) | −0.11 (0.22) | 0.26 (1.2) |
| TX code 2 | −0.14 (0.14) | −0.03 (0.13) | 0.002 (0.36) | −0.36 (0.24) | −0.34 (1.2) |
| % Sessions | −0.79 (0.51) | −0.05 (0.39) | 0.64 (0.14)** | −0.09 (0.09) | 13.9 (3.8)** |
| WAI Client | −0.002 (0.005) | −0.002 (0.004) | 0.004 (0.001)** | −0.001 (0.001) | – |
| TX1 × WAI | – | – | 0.001 (0.002) | 0.001 (0.001) | – |
| TX2 × WAI | – | – | 0.00 (0.002) | 0.001 (0.001) | – |
| R2 | 0.50 | 0.81 | 0.29 | 0.14 | 0.11 |
| WAI Therapist | Intercept DrInC | Slope DrInC | Intercept self-efficacy | Slope self-efficacy | WAI Therapist |
| TX code 1 | 0.16 (0.14) | −0.005 (0.12) | −0.20 (0.41) | 0.28 (0.28) | 3.34 (1.2)** |
| TX code 2 | −0.18 (0.14) | 0.02 (0.13) | −0.11 (0.35) | −0.03 (0.20) | 0.50 (1.2) |
| % Sessions | −1.03 (0.47)* | 0.01 (0.37) | 0.59 (0.14)** | −0.09 (0.09) | 18.27 (3.7)** |
| WAI Therapist | 0.005 (0.005) | 0.002 (0.004) | 0.004 (0.002)** | −0.001 (0.001) | – |
| TX1 × WAI | – | – | 0.001 (0.002) | −0.001 (0.001) | – |
| TX2 × WAI | – | – | 0.001 (0.002) | 0.00 (0.001) | – |
| R2 | 0.48 | 0.70 | 0.31 | 0.13 | 0.11 |
p < 0.05
p < 0.01; DrInC, Drinker Inventory of Consequences; WAI, Working Alliance Inventory; TX1, treatment code 1 (MET = 1, TSF = −1, CBT = 0); TX2, treatment code 2 (MET = −1, TSF = 0, CBT = 1); TX1 × WAI, treatment code 1 by WAI interaction; TX2 × WAI, treatment code 2 by WAI interaction; % Sessions, % of sessions attended.
Table 3.
PDD as Outcome and Client-Reported WAI as Predictor (n = 755), χ2 (85) = 177.2, p < 0.001; RMSEA = 0.04; CFI = 0.97; PDD as Outcome and Therapist-Reported WAI as Predictor (n = 743), χ2 (85) = 209.4, p < 0.001; RMSEA = 0.04; CFI = 0.96
| Structural Parameters—Unstandardized Estimates B (SE) |
|||||
|---|---|---|---|---|---|
| WAI Client | Intercept PDD | Slope PDD | Intercept self-efficacy | Slope self-efficacy | WAI Client |
| TX code 1 | 0.05 (0.03)* | −0.001 (0.02) | −0.27 (0.32) | −0.02 (0.20) | 0.23 (1.2) |
| TX code 2 | 0.003 (0.03) | 0.002 (0.02) | 0.14 (0.33) | −0.48 (0.23)* | −0.36 (1.3) |
| % Sessions | −0.27 (0.09)** | 0.07 (0.07) | 0.66 (0.14)** | −0.10 (0.09) | 13.91 (3.7)** |
| WAI Client | 0.00 (0.001) | 0.00 (0.001) | 0.004 (0.00)** | −0.001 (0.001) | – |
| TX1 9 WAI | – | – | 0.001 (0.00) | 0.00 (0.001) | – |
| TX2 × WAI | – | – | 0.00 (0.00) | 0.002 (0.001)* | – |
| R2 | 0.57 | 0.59 | 0.32 | 0.15 | 0.10 |
| WAI Therapist | Intercept PDD | Slope PDD | Intercept self-efficacy | Slope self-efficacy | WAI Therapist |
| TX code 1 | 0.05 (0.02)* | −0.01 (0.02) | −0.19 (0.37) | 0.38 (0.24) | 3.24 (1.2)** |
| TX code 2 | −0.002 (0.03) | 0.008 (0.02) | 0.22 (0.35) | −0.15 (0.21) | 0.39 (1.2) |
| % Sessions | −0.31 (0.08)** | 0.11 (0.06) | 0.63 (0.14)** | −0.11 (0.09) | 17.9 (3.8)** |
| WAI Therapist | 0.00 (0.001) | 0.00 (0.001) | 0.004 (0.002)** | −0.001 (0.001) | – |
| TX1 × WAI | – | – | 0.00 (0.002) | −0.002 (0.001) | – |
| TX2 × WAI | – | – | −0.001 (0.002) | 0.001 (0.001) | – |
| R2 | 0.57 | 0.59 | 0.32 | 0.15 | 0.10 |
p < 0.05
p < 0.01; PDD, percent drinking days; WAI, Working Alliance Inventory; TX1, treatment code 1 (MET = 1, TSF = −1, CBT = 0); TX2, treatment code 2 (MET = −1, TSF = 0, CBT = 1); TX1 × WAI, treatment code 1 by WAI interaction; TX2 × WAI, treatment code 2 by WAI interaction; % Sessions, % of sessions attended.
Table 4.
DDD as Outcome and Client-Reported WAI as Predictor (n = 755), χ2 (85) = 166.5, p < 0.001; RMSEA = 0.04; CFI = 0.96; DDD as Outcome and Therapist-Reported WAI as Predictor (n = 743), χ2 (85) = 190.4, p < 0.001; RMSEA = 0.041; CFI = 0.952
| Structural Parameters—Unstandardized Estimates B (SE) |
|||||
|---|---|---|---|---|---|
| WAI Client | Intercept DDD | Slope DDD | Intercept self-efficacy | Slope self-efficacy | WAI Client |
| TX code 1 | 0.18 (0.09) | 0.02 (0.08) | −0.44 (0.31) | −0.02 (0.21) | 0.24 (1.2) |
| TX code 2 | 0.10 (0.09) | −0.04 (0.08) | −0.24 (0.32) | −0.22 (0.20) | −0.35 (1.3) |
| % Sessions | −0.79 (0.33)* | 0.02 (0.25) | 0.67 (0.14)** | −0.11 (0.09) | 13.87 (3.8)** |
| WAI Client | 0.003 (0.003) | −0.001 (0.002) | 0.004 (0.00)** | −0.001 (0.001) | – |
| TX1 × WAI | – | – | 0.002 (0.001) | 0.00 (0.001) | – |
| TX2 × WAI | – | – | 0.002 (0.001) | 0.001 (0.001) | – |
| R2 | 0.71 | 0.91 | 0.30 | 0.14 | 0.11 |
| WAI Therapist | Intercept DDD | Slope DDD | Intercept self-efficacy | Slope self-efficacy | WAI Therapist |
| TX code 1 | 0.16 (0.10) | 0.04 (0.08) | −0.12 (0.33) | 0.28 (0.23) | 3.25 (1.21)** |
| TX code 2 | 0.06 (0.10) | −0.002 (0.09) | 0.12 (0.32) | −0.08 (0.19) | 0.40 (1.3) |
| % Sessions | −1.01 (0.34)** | 0.19 (0.25) | 0.63 (0.14)** | −0.12 (0.09) | 17.95 (3.8)** |
| WAI Therapist | 0.001 (0.003) | −0.003 (0.002) | 0.004 (0.002)* | −0.001 (0.001) | – |
| TX1 × WAI | – | – | 0.001 (0.002) | −0.001 (0.001) | – |
| TX2 × WAI | – | – | 0.00 (0.002) | 0.00 (0.001) | – |
| R2 | 0.70 | 0.78 | 0.31 | 0.14 | 0.10 |
p < 0.05
p < 0.01; DDD, drinks per drinking day; WAI, Working Alliance Inventory; TX1, treatment code 1 (MET = 1, TSF = −1, CBT = 0); TX2, treatment code 2 (MET = −1, TSF = 0, CBT = 1); TX1 × WAI, treatment code 1 by WAI interaction; TX2 × WAI, treatment code 2 by WAI interaction; % Sessions, % of sessions attended.
For all drinking outcomes, the association between the self-efficacy growth model and the drinking outcomes growth models was such that the intercept of self-efficacy was significantly inversely associated with the intercept of the drinking outcomes, for example, Table 2, PDD: B (SE) = −0.30 (0.05), p < 0.001, and the slope of self-efficacy was significantly inversely associated with the slope of the drinking outcomes, for example, Table 2, PDD: B (SE) = −0.61 (0.22), p = 0.005. Thus, higher self-efficacy at the end of treatment (intercept) predicted lower PDD/DDD/DrInC at the end of treatment (intercept), while increases (changes) in self-efficacy over time (slope) predicted decreases in PDD/ DDD/DrInC (slope) over time. The intercept of self-efficacy was not significantly associated with the slope (i.e., change) in drinking outcomes, and the intercepts of the drinking outcomes were not significantly associated with the slope (i.e., change) in self-efficacy.
With regard to other covariates included in the model, the intercepts of PDD and DrInC were consistently significantly positively associated with baseline levels of the drinking outcome, Table 2, PDD: B (SE) = 0.003 (0.001), p < 0.001, whereas the intercepts of PDD, DDD, and DrInC were consistently inversely associated with percent sessions attended, Table 2, PDD: B (SE) = −0.27 (0.09), p = 0.002. In addition, the slope of PDD was significantly inversely related to alcohol dependence scores on the ADS, Table 2: B (SE) = −0.01 (0.002), p = 0.03; however, the slopes of DDD and DrInC were not associated with ADS or any of the other covariates.
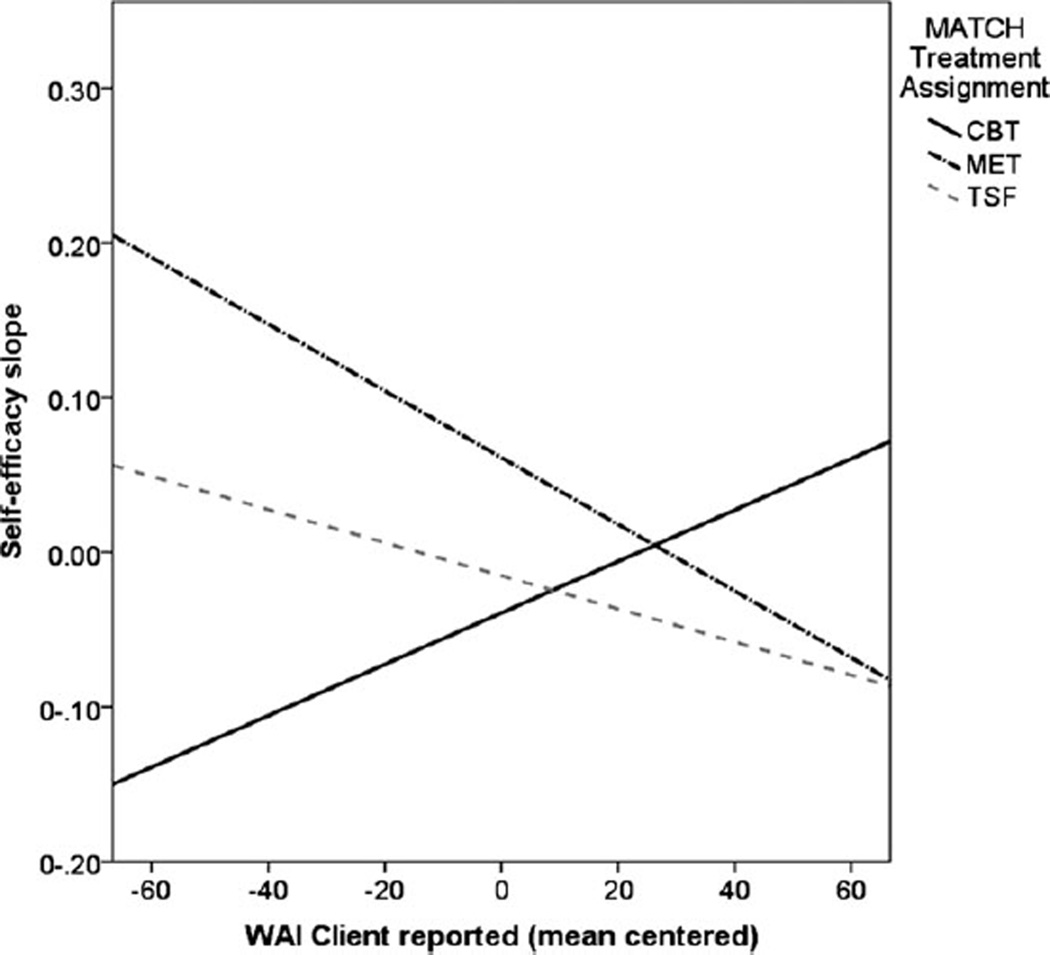
The intercepts of self-efficacy across models were consistently significantly positively associated with baseline self-efficacy, Table 2: B (SE) = 0.33 (0.05), p < 0.001, therapeutic alliance, Table 2: B (SE) = 0.004 (0.001) p = 0.007, and percent sessions attended, e.g., Table 2: B (SE) = 0.66 (0.14), p < 0.001. The slopes of self-efficacy were consistently positively associated with motivation, as measured by the URI-CA; Table 2: B (SE) = 0.03 (0.01), p = 0.03, and inversely associated with gender, Table 2: B (SE) = −0.13 (0.05), p = 0.008, indicating that greater motivation and being male (gender = 0) predicted a greater increase in self-efficacy over time. In addition, for the PDD–WAI Client model, receiving CBT compared to receiving MET (treatment code 2) was associated with less change in self-efficacy over time, Table 2: B (SE) = −0.48 (0.023), p = 0.03, but this main effect was qualified by an interaction between treatment code 2 and WAI Client in predicting the change in self-efficacy over time, Table 2: B (SE) = 0.002 (0.001), p = 0.048. An examination of this interaction using simple slopes (shown in Fig. 2) indicated that the association between WAI scores and the change in self-efficacy (slope) was significantly positive for the CBT group (simple slope standardized β = 0.26, p < 0.001), but was significantly negative for the MET and TSF groups (MET: β = −0.32, p < 0.001; TSF: β = −0.16, p < 0.001; see Fig. 2).
Fig. 2.
Interaction between client-reported therapeutic alliance and treatment condition in predicting the change in self-efficacy over time.
Finally, with respect to prediction of the WAI Client and Therapist scores, results indicated that motivation and the percent of sessions attended were consistently positively associated with the WAI Client- and Therapist-reported scores, whereas education was inversely associated with WAI Client-and Therapist-reported scores. Motivation was significantly positively associated with WAI Client scores in all models, such that greater baseline motivation (as measured by the URICA) predicted higher client ratings of therapeutic alliance. Treatment code 1 was also significantly associated with WAI Therapist scores in all models, indicating that therapists in MET, as compared to TSF, reported greater therapeutic alliance.
Mediation Results
As shown in Table 6, for the DDD and DrInC outcomes and for both therapist and client ratings of therapeutic alliance, we found support for posttreatment self-efficacy (intercept) as a significant mediator of the association between therapeutic alliance and the intercepts of the DDD and DrInC drinking outcomes. Thus, the effect of therapist and client ratings of working alliance in prediction of the intercepts of DDD and DrInC can be partially explained by self-efficacy. For all drinking outcomes (PDD, DDD, and DrInC scores) and the therapist ratings of therapeutic alliance, we found a double mediation effect, whereby both WAI therapist ratings and self-efficacy significantly mediated the association between treatment code 1 and the intercepts of the drinking outcomes. Thus, the effect of MET (coded 1) vs. TSF (coded —1) on drinking outcomes was mediated by therapist ratings of alliance and self-efficacy at the end of treatment.
Table 6.
Mediation Model Results Including Unstandardized Estimate B (95% Confidence Interval) of the Indirect Effect
| Model | TXI→WAI→ Drinking outcome |
TX2→WAI→ Drinking outcome |
WAI→Self-Efficacy→ Drinking outcome |
TX1→WAI→Self-Efficacy→ Drinking outcome |
TX 2→WAI→Self-Efficacy→ Drinking outcome |
|---|---|---|---|---|---|
| WAI Client—PDD | |||||
| PDD intercept | 0.00 (−0.003, 0.002) | 0.00 (−0.003, 0.002) | −0.001 (−0.002, 0.00) | 0.00 (−0.004, 0.003) | 0.00 (−0.003, 0.004) |
| PDD slope | 0.00 (−0.002, 0.002) | 0.00 (−0.002, 0.003) | 0.00 (−0.001, 0.002) | 0.00 (−0.002, 0.002) | 0.00 (−0.003, 0.001) |
| WAI Therapist—PDD | |||||
| PDD intercept | −0.001 (−0.006, 0.005) | 0.00 (−0.003, 0.002) | −0.001 (−0.002, 0.00) | −0.001 (−0.01, −.001)* | 0.00 (−0.004, 0.002) |
| PDD slope | −0.001 (−0.006, 0.002) | 0.00 (−0.002, 0.001) | 0.001 (0.00, 0.002) | 0.002 (−0.001, 0.006) | 0.00 (−0.002, 0.002) |
| WAI Client—DDD | |||||
| DDD intercept | 0.001 (−0.01,0.01) | −0.001 (−0.01,0.01) | −0.005 (−0.009, −.001)* | −0.001 (−0.01,0.01) | 0.002 (−0.01, 0.006) |
| DDD slope | 0.00 (−0.007, 0.006) | 0.00 (−0.005, 0.008) | 0.001 (−0.003, 0.006) | 0.00 (−0.006, 0.007) | 0.00 (−0.009, 0.005) |
| WAI Therapist—DDD | |||||
| DDD intercept | 0.004 (−0.01, 0.03) | 0.00 (−0.007, 0.01) | −0.005 (−0.009, −.001)* | −0.01 (−0.04, −0.002)* | −0.002 (−0.02, 0.01) |
| DDD slope | −0.009 (−0.03, 0.003) | −0.001 (−0.01,0.007) | 0.002 (−0.002, 0.007) | 0.007 (−0.004, 0.03) | 0.001 (−0.006, 0.008) |
| WAI Client—DrlnC | |||||
| DrlnC intercept | −0.001 (−0.02,0.01) | 0.001 (−0.02, 0.01) | −0.005 (−0.01, −.001)* | −0.001 (−0.02,0.01) | 0.002 (−0.01, 0.02) |
| DrlnC slope | −0.001 (−0.01,0.01) | 0.001 (−0.008,0.01) | 0.002 (−0.005, 0.01) | 0.00 (−0.008, 0.01) | −0.001 (−0.01,0.007) |
| WAI Therapist—DrlnC | |||||
| DrlnC intercept | 0.016 (−0.01, 0.06) | 0.002 (−0.01, 0.02) | −0.005 (−0.01, −.001)* | −0.017 (−0.05, −.002)* | −0.003 (−0.02, 0.01) |
| DrlnC slope | 0.002 (−0.02, 0.01) | 0.000 (−0.01, 0.009) | 0.003 (−0.002, 0.01) | 0.010 (−0.005, 0.04) | 0.001 (−0.008,0.01) |
p < 0.05; PDD, percent drinking days; DDD, drinks per drinking day; DrlnC, Drinker Inventory of Consequences; WAI, Working Alliance Inventory; TX1, treatment code 1 (MET = 1, TSF = −1. CBT = 0);TX2, treatment code 2 (MET = −1,TSF = 0, CBT = 1).
DISCUSSION
The results of the current study were largely consistent with the hypotheses, and the findings replicate and extend those of recent empirical studies of the therapeutic alliance in AUD treatment, alcohol abstinence self-efficacy, and treatment outcomes. The main hypothesis concerned the replication of Hartzler and colleagues’ (2011) finding of statistical mediation of the relationship between the alliance and outcomes by alcohol abstinence self-efficacy for individuals in that study who only received the combined behavioral intervention. The results of this study showed a statistical mediation effect, with self-efficacy at the end of treatment (the intercept in the growth models) mediating the association between ratings of therapeutic alliance (client and therapist) and posttreatment (3-month) drinking outcomes, in the direction of greater alliance predicting higher self-efficacy predicting better treatment outcomes. Furthermore, this study extends the Hartzler and colleagues (2011) data in that both the client and therapist ratings of the alliance were tested, whereas Hartzler and colleagues used only client ratings in their analyses. Moreover, Hartzler and colleagues (2011) recorded only ratings of “therapeutic bond,” which is 1 of 3 WAI components, whereas this study (as well as Connors et al., 1997) used WAI total score, which is summed over items loading on its 3 components.
Connors and colleagues (1997), Hartzler and colleagues (2011), and Ilgen and colleagues (2006) tested models that included point estimates of 12-month posttreatment completion outcomes. In this study, the modeling approach took into account growth (change) in both self-efficacy and the drinking outcomes over the course of assessments at 3, 6, 9, and 12 months following treatment completion and showed (concurrent) mediation effects only for the post-treatment outcome but not for changes in drinking outcomes over time. This finding may be due to the fact that the MATCH outpatient sample showed major reductions in alcohol use and consequences from pre- to posttreatment across all treatment conditions and that maintenance of those changes was excellent. That is, on average, the participants did not show a large degree of change or growth in alcohol use or negative consequences from posttreatment to a year later (Project MATCH Research Group, 1997). Therefore, there was relatively little variability in drinking outcomes growth to explain. Nevertheless, the concurrent mediation findings for the posttreatment outcomes are clinically relevant. In this regard, there is evidence that abstinence or reduced alcohol consumption during a period an individual is engaged in outpatient treatment is positively related to healthier longer term (i.e., 3-year) drinking outcomes (Maisto et al., 2006, 2007). Furthermore, Maisto and colleagues (2008) showed that change in alcohol abstinence self-efficacy at posttreatment statistically mediates that association in the Project MATCH outpatient data.
We also found that the alliance and self-efficacy had direct effects on drinking outcomes, both in the direction of improved functioning. One possible explanation for these findings is that early treatment alliance from both the client’s and the therapist’s viewpoint reflects, at least in part, the client’s early success in working effectively toward the goal of abstaining or reducing consumption. The initial success then could initiate a reciprocal enhancing relationship between self-efficacy, control of alcohol use, and alliance over the course of treatment, which is also predictive of longer term outcomes.
We also found a “double mediation” effect, such that both WAI therapist ratings and self-efficacy significantly mediated the association between receiving MET and the intercepts of the drinking outcomes. This finding is consistent with the hypothesis that MET is an alliance-enhancing treatment approach, as least as reflected in the therapist’s rating of the alliance, and that the alliance in MET may be a vehicle of enhancing client self-efficacy to make and sustain change in alcohol use.
We found evidence for a moderation effect of treatment, but only in part as hypothesized. As Fig. 2 shows, the association between the client’s rating of the alliance and growth in self-efficacy was positive for individuals in the CBT group but negative for those receiving the other 2 treatments. The positive slope for CBT patients was as hypothesized. However, it is not clear why the client’s rating of greater alliance predicted decreases in self-efficacy in the MET and TSF conditions. This somewhat surprising finding deserves future study. Perhaps greater alliance in these treatments is working via other change mechanisms, such as change talk in the MET condition (Apodaca and Longabaugh, 2009) or increases in AA involvement in the TSF condition (Longabaugh et al., 1998). Another possibility is that the finding is spurious, or a chance result among the large number of analyses that were conducted.
There are several limitations of this study that warrant mentioning. As with all secondary data analyses, the study is limited by a research protocol that was not designed primarily to test this study’s hypotheses. In addition, it could be argued that the Project MATCH data are over 2 decades old, and thus, some of the measures may be yielding findings that are less than representative of current treatment processes and outcomes. Furthermore, the Project MATCH research design is characterized by several shortcomings, including lack of a control condition and an extensive assessment protocol that likely resulted in participant selection bias. Nevertheless, Project MATCH remains one of the largest and most research-generative AUD treatment clinical trials ever conducted in the United States. Further, the large majority of measures used in Project MATCH, including the WAI, remain state-of-the-science measures of their respective constructs. Similarly, the content of the 3 respective treatments tested in MATCH has not changed substantially. Finally, it is important to keep in mind that the statistical mediation effects found in this study concern variables all measured concurrently at the posttreatment assessment. Therefore, the temporal ordering of variables that would be observed in an actual causal mediation effect was not evident in the data.
In conclusion, the findings of this study largely replicated and extended the Hartzler and colleagues (2011) results and reaffirm the modest but consistent relationship between the therapeutic alliance and AUD outcomes and its mediation by self-efficacy. Because of the stability of this finding, it seems important in future research to determine how the alliance relates to self-efficacy more precisely over time in their contribution to longer term AUD treatment outcomes.
REFERENCES
- Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Thousand Oaks, CA: Sage; 1991. [Google Scholar]
- Apodaca TR, Longabaugh R. Mechanisms of change in motivational interviewing: a review and preliminary evaluation of the evidence. Addiction. 2009;104:705–715. doi: 10.1111/j.1360-0443.2009.02527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Self-Efficacy: The Exercise of Control. New York: W.H. Freeman; 1997. [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. In: Alternative ways of assessing model fit, in Testing Structural Equation Models. Bollen KA, Long JS, editors. Newbury Park, CA: Sage Publications; 1993. pp. 136–162. [Google Scholar]
- Cheong JW, McKinnon D, Khoo ST. A latent growth modeling approach to mediation analysis. Struct Equ Modeling. 2003;10:238–262. doi: 10.1207/S15328007SEM1002_5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COMBINE Study Research Group. Testing combined pharmacotherapies and behavioral interventions for alcohol dependence (the COMBINE study): a pilot feasibility study. Alcohol Clin Exp Res. 2003;27:1123–1131. doi: 10.1097/01.ALC.0000078020.92938.0B. [DOI] [PubMed] [Google Scholar]
- Connors GJ, Allen JP, Cooney NL, Di Clemente CC, Tonigan JS, Anton R. Assessment issues and strategies in alcoholism treatment matching research. J Stud Alcohol. 1994;12(Suppl):92–100. doi: 10.15288/jsas.1994.s12.92. [DOI] [PubMed] [Google Scholar]
- Connors GJ, Carroll KM, DiClemente CC, Longabaugh R, Donovan DM. The therapeutic alliance and its relationship to alcoholism treatment participation and outcome. J Consult Clin Psychol. 1997;65:588–598. doi: 10.1037//0022-006x.65.4.588. [DOI] [PubMed] [Google Scholar]
- DiClemente CC, Carbonari JP, Montgomery RPG, Hughes SO. The alcohol abstinence self-efficacy scale. J Stud Alcohol Drugs. 1994;55:141–148. doi: 10.15288/jsa.1994.55.141. [DOI] [PubMed] [Google Scholar]
- DiClemente CC, Hughes SO. Stages of change profiles in outpatient alcoholism treatment. J Subst Abuse. 1990;2:217–235. doi: 10.1016/s0899-3289(05)80057-4. [DOI] [PubMed] [Google Scholar]
- Hartzler B, Witkiewitz K, Villarroel N, Donovan D. Self-efficacy change as a mediator of associations between therapeutic bond and one-year outcomes in treatments for alcohol dependence. Psychol Addict Behav. 2011;25:269–278. doi: 10.1037/a0022869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvath AO, Greenberg LS. The development of the Working Alliance Inventory. In: Greenberg LS, Pinsof WM, editors. The Psychotherapeutic Process: A Research Handbook. New York: Guilford Press; 1989. pp. 529–556. [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- Ilgen M, Tiet Q, Finney J, Moos RH. Self-efficacy, therapeutic alliance, and alcohol-use disorder treatment outcomes. J Stud Alcohol Drugs. 2006;67:465–472. doi: 10.15288/jsa.2006.67.465. [DOI] [PubMed] [Google Scholar]
- Kadden R, Carroll K, Donovan D, Cooney N, Monti P, Abrams D, Litt M, Hester R. Cognitive-behavioral coping skills therapy manual (Project MATCH Monograph Series No. 3) Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1992. [Google Scholar]
- Longabaugh R, Wirtz PW, Zweben A, Stout RL. Network support for drinking, Alcoholics Anonymous and long-term matching effects. Addiction. 1998;93:1313–1333. doi: 10.1046/j.1360-0443.1998.93913133.x. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP. Introduction to Statistical Mediation Analysis. Mahweh, NJ: Erlbaum; 2008. [Google Scholar]
- Maisto SA, Clifford PR, Stout RL, Davis CM. Drinking in the year after treatment as a predictor of three-year drinking outcomes. J Stud Alcohol Drugs. 2006;67:823–832. doi: 10.15288/jsa.2006.67.823. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Clifford PR, Stout RL, Davis CM. Moderate drinking in the first year after treatment as a predictor of three-year outcomes. J Stud Alcohol Drugs. 2007;68:419–427. doi: 10.15288/jsad.2007.68.419. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Clifford PR, Stout RL, Davis CM. Factors mediating the association between drinking in the first year after alcohol treatment and drinking at three years. J Stud Alcohol Drugs. 2008;69:728–737. doi: 10.15288/jsad.2008.69.728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR. Continuing care research: what we have learned and where we are going. J Subst Abuse Treat. 2009;36:131–145. doi: 10.1016/j.jsat.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier PS, Barrowclough C, Donmall MC. The role of the therapeutic alliance in the treatment of substance misuse: a critical review of the literature. Addiction. 2005;100:304–316. doi: 10.1111/j.1360-0443.2004.00935.x. [DOI] [PubMed] [Google Scholar]
- Miller WR. Form 90: Structured Assessment Interview for Drinking and Related Behaviors: Test Manual (NIH Publication No. 96-4004) Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1996. [Google Scholar]
- Miller WR, Rose GS. Toward a theory of motivational interviewing. Am Psychol. 2009;64:527–537. doi: 10.1037/a0016830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. The drinker inventory of consequences (DrInC): An instrument for assessing adverse consequences of alcohol abuse (NIH Publication No. 95-3911) Bethesda, MD: 1995. [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivational Enhancement Therapy Manual: A Clinical Research Guide for Therapists Treating Individuals with Alcohol Abuse and Dependence (NIH Publication No. 94-3723) Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1992. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 7th edn. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- Nowinski J, Baker S, Carroll K. Twelve-Step Facilitation Therapy Manual: A Clinical Research Guide for Therapists Treating Individuals with Alcohol Abuse and Dependence (NIH Publication No. 94-3722) Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1992. [Google Scholar]
- Project MATCH Research Group. Project MATCH (Matching Alcoholism Treatment to Client Heterogeneity): rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcohol Clin Exp Res. 1993;17:1130–1145. doi: 10.1111/j.1530-0277.1993.tb05219.x. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: project MATCH posttreatment drinking outcomes. J Stud Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- Skinner HA, Horn JL. Alcohol Dependence Scale: User’s Guide. Toronto: Addiction Research Foundation; 1984. pp. 1–38. [Google Scholar]
- Summers RF, Barber JP. Therapeutic alliance as a measurable psychotherapy skills. Acad Psychiatry. 2003;27:160–165. doi: 10.1176/appi.ap.27.3.160. [DOI] [PubMed] [Google Scholar]
- Wampold BE. The Basics of Psychotherapy. Washington, DC: American Psychological Association; 2010. [Google Scholar]