Abstract
Sleep deficiency, which can be caused by acute sleep deprivation, chronic insufficient sleep, untreated sleep disorders, disruption of circadian timing, and other factors, is endemic in the U.S., including among professional and non-professional drivers and operators. Vigilance and attention are critical for safe transportation operations, but fatigue and sleepiness compromise vigilance and attention by slowing reaction times and impairing judgment and decision-making abilities. Research studies, polls, and accident investigations indicate that many Americans drive a motor vehicle or operate an aircraft, train or marine vessel while drowsy, putting themselves and others at risk for error and accident. In this chapter, we will outline some of the factors that contribute to sleepiness, present evidence from laboratory and field studies demonstrating how sleepiness impacts transportation safety, review how sleepiness is measured in laboratory and field settings, describe what is known about interventions for sleepiness in transportation settings, and summarize what we believe are important gaps in our knowledge of sleepiness and transportation safety.
Keywords: Biological rhythm, circadian; drowsiness; fatigue; homeostatic sleep-wake regulation; hours of work; individual differences; sleep inertia; sleep-wake propensity
FATIGUE, TIREDNESS, SLEEPINESS, DROWSINESS: WHAT DOES IT MEAN FOR TRANSPORTATION SAFETY?
While many Americans complain about their sleep, few consider it a serious health or safety issue. However, sleep deficiency, which may be caused by acute sleep deprivation, chronic insufficient sleep duration, sleep disorders (such as sleep apnea), disruption of circadian timing, or other factors, is endemic in our society (National Center on Sleep Disorders Research, 2011). A National Sleep Foundation (NSF) “Sleep in America” poll found that one third of adults report sleeping 7 or fewer hours per night, and 15% of adults report sleeping 6 hours or less per night (National Sleep Foundation, 2002). In addition to people whose insufficient sleep is due to restricting their time in bed, individuals with sleep disorders (frequently undiagnosed) and other medical conditions often have poor quality, unrestful sleep that leads them to be sleepy during the daytime. This has important consequences for transportation safety. The 2003 National Highway Traffic Safety Administration (NHTSA) National Survey of Distracted and Drowsy Driving found that more than 40% of working-age drivers reported having fallen asleep while driving at least once, with 8% reporting having done so in the previous 6 months (Royal, 2003); NHTSA extrapolated these findings to 7.5 million drivers nodding off while driving each month. The NHTSA findings are supported by a poll conducted by the National Sleep Foundation (NSF). In their 2009 annual Sleep in America poll, NSF found that 54% of the respondents reported driving while drowsy within the past year and 28% reported actually falling asleep while driving within the past year (National Sleep Foundation, 2009). The findings from these surveys help explain data from the 100-Car Naturalistic Driving Study, where 22–24% of crashes and near-crashes were associated with signs of drowsiness, and driver drowsiness contributed to a 4- to 6-fold increase in crash/near-crash risk (Klauer, Dingus, Neale, Sudweeks, & Ramsey, 2006). Americans are sleepy and this puts them at risk for transportation accidents (Czeisler, 2015).
Vigilance and attention are critical for safe transportation operations, but fatigue and sleepiness compromise vigilance and attention by slowing reaction times, increasing the likelihood of lapses of attention, and impairing judgment and decision-making (Budnick, Lerman, Baker, Jones, & Czeisler, 1994). Fatigue and sleepiness also increase distractibility (Anderson & Horne, 2006), and together these factors decrease operator efficiency and increase the risk of operator error. Such performance impairments have important consequences for the efficiency and safety of transportation operations (Philip & Åkerstedt, 2006). Transportation workers, like most US workers, fail to obtain sufficient sleep on work nights, making them vulnerable to fatigue-related performance decrements and errors. However, sleepiness and fatigue pose special problems for transportation operators, whether professional or non-professional. The operation of a transportation vehicle is typically a routine, highly-over-learned task with minimal novelty, operators are usually in a sedentary position, in many modes of transportation operators are in dim light or near darkness, and the routine tasks performed by transportation operators are especially vulnerable to momentary lapses of attention or slowed reaction times. Even the loss of just an hour of sleep, such as occurs during the spring transition from Standard Time to Daylight Savings Time, is associated with a 6–11% increase in traffic accidents (Coren, 1996; Monk, 1980; Varughese & Allen, 2001). This sensitivity to such a small change suggests that the drivers involved in those traffic accidents do not habitually obtain enough sleep, making it impossible for them to compensate for the loss of that extra hour of sleep and leaving them extremely vulnerable to the lapses of attention and associated performance deficits. More than half of Americans admit having driven a vehicle while drowsy in the past year (National Sleep Foundation, 1999, 2000, 2002, 2005), with nearly a fifth reporting having fallen asleep at the wheel. While NHTSA reports suggest that only a small proportion of crashes are due to drowsiness or falling asleep at the wheel (National Highway Traffic Safety Administration, 2008), there is evidence that drowsy driving is a more widespread problem (Hanowski, Wierwille, & Dingus, 2003; Klauer et al., 2006). In fact, the National Transportation Safety Board found that fatigue was the leading cause of fatal-to-the-driver heavy truck crashes in the United States (National Transportation Safety Board, 1990), and an analysis of 15 years of passenger vehicle crash data by the AAA Foundation for Traffic Safety estimated that 15–20% of fatal crashes involved a drowsy driver (Tefft, 2012, 2014); see Table 1. Thus, sleep loss and the resulting sleepiness impacts on attention have important implications for transportation safety (Czeisler, 2015).
Table 1. Estimates of Crashes Involving a Drowsy Driver in the US During the Years 1989–2013.
Government estimates of drowsy driving related crashes range from 1.4% to 3.2%, with an estimated 2.5% of all fatal crashes involving a drowsy driver (National Highway Traffic Safety Administration, 2011). These estimates have been called into question by studies which find the numbers for drowsy driving related crashes to be much higher [see e.g. (Tefft, 2014) who report that 6% of all crashes and 21% of fatal crashes involve a drowsy driver]. Explanations for these discrepancies may include methodological differences, different data sets, and different definitions of fatigue relatedness between the studies. Adding to the difficulty of estimating fatigue relatedness in crashes is that accident reports in different accident locations may code fatigue in different ways (or not at all), training of local investigators in recognizing hallmarks of drowsy driving is inconsistent, unreliable self-reports from involved drivers, and the lack of objective ways to determine driver impairment due to fatigue.
| Estimates of crashes involving a drowsy driver | ||||||||
|---|---|---|---|---|---|---|---|---|
| Study/report | all crashes | injury crashes |
fatal crashes |
Study type | Data collected |
Number of crashes included in analysis |
Source | Notes |
| Crashes and Fatalities Related to Driver Drowsiness/Fatigue | 0.9% (1 – 4%) * |
1.4% | 3.6% | statistical summary / review | 1989–1993 | 6,300,000 crashes annually |
Knipling & Wang, 1994 | * based on the paper's review of other studies |
| Revised estimates of the U.S. drowsy driver crash problem size based on General Estimates System case review | 1.2 – 1.6% | case review | 1989–1993 | 6,300,000 crashes annually | Knipling & Wang, 1995 | Knipling & Wang updated their earlier estimate | ||
| The role of driver inattention in crashes; new statistics from the 1995 Crashworthiness Data System | 2.6% * | investigation | 1995 | 4,536 | Wang et al. 1996 | * crashes in which a vehicle was towed from the scene | ||
| An On-Road Study to Investigate Fatigue in Local/Short Haul Trucking | 20.8% * | field study | 1997 | 77 ** | Hanowski et al. 2003 | * near-crashes where fatigue was present ** number driver-at-fault near-crashes |
||
| The Impact of Driver Inattention on Near-Crash/Crash Risk: An Analysis Using the 100-Car Naturalistic Driving Study | 16 – 22% * | field study | 2001–2004 | 82 ** (761) *** |
Klauer et al. 2006 (DOT HS 810 594) | * crashes / near-crashes ** number of crashes *** number of near-crashes |
||
| Predicting daytime and nighttime drowsy driving crashes based on crash characteristic models | 15–33% | investigation | 2001–2003 | 1,773 | Masten et al. 2006 | |||
| Report to Congress on the Large Truck Crash Causation Study | 11.6% * | investigation | 2001–2003 | 967 | Federal Motor Carrier Safety Administration, 2005 (MC-R/MC-RAI) | * of crashes where the critical reason was assigned to the truck (includes all non-performance errors: driver fell asleep, was disabled by a heart attack or seizure, or other physical impairment) | ||
| National Motor Vehicle Crash Causation Survey: Report to Congress | 3.2% * | investigation | 2005–2007 | 5,471 ** | National Highway Traffic Safety Administration, 2008 (DOT HS 811 059) | * of driver-at-fault crashes ** out of 6,950 ivestigated crashes |
||
| Traffic Safety Facts | 1.4% * | 2.2% | 2.5% | statistical summary | 2005–2009 | 5,895,000 (5-year average) |
National Highway Traffic Safety Administration, 2011 (DOT HS 811 449) | |
| Prevalence of Motor Vehicle Crashes Involving Drowsy Drivers, United States, 1999–2004 | 7.0%* (3.9%) * † |
13.1%** (7.7%)** † |
16.5% (3.6 %) † |
investigation | 1999–2008 | 47,597 | Tefft BC., 2012 | * crashes in which a vehicle was towed from the scene ** resulted in hospital admission † value based on original non-imputed data |
| Prevalence of Motor Vehicle Crashes Involving Drowdy Drivers, United States, 2009–2013 | 6% * | 13% ** | 21% | investigation | 2009–2013 | 14,268 *** | Tefft BC., 2014 | * crashes in which a vehicle was towed from the scene ** resulted in hospital admission *** out of 21,292 investigated crashes |
Note: This table is meant as an overview of reports/estimates of drowsy driving, and does not attempt to cover all studies reporting drowsy driving statistics during the time period.
21ST CENTURY SOCIETAL CHANGES AND IMPACTS ON FATIGUE IN TRANSPORTATION
Several factors in the late 20th and early 21st century have resulted in greater levels of fatigue among people in the US and other industrialized societies. While shift work was once mainly done by public safety, healthcare, and manufacturing workers, today more workers in all industries (including financial services, retail and food services) are required to do their jobs at night. Estimates of shift work frequency vary, but the Bureau of Labor Statistics estimates that nearly 10% of workers work on the night shift or on irregular or rotating shift schedules (Bureau of Labor Statistics, 2005), accounting for more than 12 million people in the US (Bureau of Labor Statistics, 2012). Working at night or on a rotating schedule impacts medical and social aspects of the worker’s life (Monk, 2000). In fact, the disruption caused by shift work is recognized as a circadian rhythm sleep disorder in both the International Classification of Sleep Disorders (Diagnostic Classification Steering Committee, 1995) and the DSM-IV (American Psychiatric Association, 2000). Even workers who choose to work at night because of higher pay or to accommodate childcare or other family demands report that working at night has negative influences on their health and safety (Barton, 1994; Novak & Auvil-Novak, 1996). While there are numerous adverse health consequences of shift work (Davis, Mirick, & Stevens, 2001; De Bacquer et al., 2009; Drake, Roehrs, Richardson, Walsh, & Roth, 2004; Fischer et al., 2001; Fujino et al., 2006; Ha & Park, 2005; Kawachi et al., 1995; Knutsson, Hallquist, Reuterwall, Theorell, & Åkerstedt, 1999; Kubo et al., 2006; Lin, Hsiao, & Chen, 2009; Monk, 2000; Schernhammer et al., 2001; Vener, Szabo, & Moore, 1989), it is the risk of accidents while at work (Mitler et al., 1988) and while commuting (Drake et al., 2004; Novak & Auvil-Novak, 1996) that have the greatest and most immediate impacts on transportation. This increased accident risk is largely due to the insufficient sleep experienced by most night and rotating shift workers, as they attempt to sleep during the day when an extended and consolidated bout of sleep is difficult to achieve. This results in shorter average sleep durations for night workers than reported by day workers (Drake et al., 2004; Garde, Hansen, & Hansen, 2009; Grundy et al., 2009; Luckhaupt, S.E., 2012). Compounding the impact of shift work schedules are the extended work hours of many shift workers either at their primary job or at second jobs, and longer commuting times. In fact, while the average commute time in the US is 25.1 minutes (McKenzie & Rapino, 2011), more than a third of Americans have a commute time that is longer than half an hour (McKenzie & Rapino, 2011), and 7.5% commute an hour or longer on a regular basis (estimated to be nearly 1 million night workers). In a recent survey of transportation workers by the National Sleep Foundation (2012), train operators and pilots reported significantly longer commutes than other transportation and non-transportation workers.
As individuals and families spend more time working, the available time for personal, family, and household activities is reduced. Because many such activities are not optional, individuals often choose to forgo sleep to accomplish them. The availability of round-the-clock grocery stores, fitness centers, and restaurants makes daily life easier for shift workers and those with long work hours or other demands on their time, but also makes it easier to push those chores into the night, displacing sleep. In addition, with the availability of 24-hour television and internet, it is easy to pursue social activities and entertainment during the night. In fact, one quarter of Americans admit that they chronically sleep less than needed (National Sleep Foundation, 2000), despite the fact that most recognize that this adversely affects their performance. It is therefore not surprising that nearly 40% of adults 30 to 64 years old reported daytime sleepiness so severe that it interfered with work and social functioning at least a few days each month (National Sleep Foundation, 2002).
CAUSES AND CONSEQUENCES OF SLEEPINESS AND FATIGUE
Cognitive functioning is modulated by many factors (see Table 2), including the sleep-wake homeostat (elapsed time awake) and the phase (timing) of the endogenous circadian pacemaker (the biological clock). The sleep-wake homeostat contributes an approximately linear decline to cognitive function and alertness with increasing time awake (Dijk, Duffy, & Czeisler, 1992; Johnson et al., 1992), while the circadian pacemaker contributes a rhythmic variation in cognitive functioning and alertness over the course of the 24-hour day (Dijk et al., 1992; Johnson et al., 1992). Under normal conditions (awake during the day and sleeping at night) in well-rested individuals, the sleep-wake homeostat and the circadian timing system interact to produce a relatively stable level of cognitive functioning and alertness across a ~16 hour wake episode (Dijk et al., 1992). However, in individuals who are not fully rested, there can be a dip in alertness and performance in the afternoon relative to the morning or early evening (Lenné, Triggs, & Redman, 1997; Moller, Kayumov, Bulmash, Nhan, & Shapiro, 2006; Reimer, D'Ambrosio, & Coughlin, 2007).
Table 2.
Factors That Influence Fatigue and Sleepiness
Circadian Rhythmicity (biological time of day)
|
Sleep Inertia
|
Time Awake
|
Sleep-Wake History
|
Time-on-Task
|
Medications and Medical Conditions
|
Circadian Timing
Circadian rhythms, i.e., biological rhythms oscillating with an approximate cycle length of twenty-four hours (from the Latin words: circa--about and dies--a day), are present at all levels of biological complexity from unicellular organisms to humans. Circadian rhythms are endogenous (i.e., internally generated), self-sustaining oscillations; therefore, rhythmicity continues even in the absence of periodic external time cues (such as sunlight-darkness or sleep and wakefulness). In humans, many physiological processes, including body temperature, hormone secretion, renal and cardiac function, subjective alertness, sleep-wake behavior, and performance vary according to the time of day (Allan & Czeisler, 1994; Cajochen, Khalsa, Wyatt, Czeisler, & Dijk, 1999; Cajochen, Wyatt, Czeisler, & Dijk, 2002; Czeisler, 1978; Czeisler, Buxton, & Khalsa, 2005; Czeisler & Gooley, 2007; Czeisler & Jewett, 1990; Czeisler & Klerman, 1999; Dijk & Czeisler, 1994; Dijk et al., 2002; Dijk, Neri, et al., 2001; El-Hajj Fuleihan et al., 1997; Horowitz, Cade, Wolfe, & Czeisler, 2003; Johnson et al., 1992; Khalsa, Conroy, Duffy, Czeisler, & Dijk, 2002; Scheer, Hilton, Mantzoros, & Shea, 2009; Van Cauter & Buxton, 2001; Waldstreicher et al., 1996; Wyatt, Dijk, Ritz-De Cecco, Ronda, & Czeisler, 2006). Circadian rhythms in alertness and performance are generated by the same light-sensitive cluster of neurons (the suprachiasmatic nuclei) that drive circadian rhythms of body temperature and other physiologic functions (Boivin & Czeisler, 1998; Czeisler, 1995; Czeisler, Chiasera, & Duffy, 1991; Czeisler & Gooley, 2007; Czeisler et al., 1990; Czeisler & Khalsa, 2000; Czeisler et al., 1989; Czeisler & Wright Jr., 1999; Duffy, Kronauer, & Czeisler, 1996; Jewett, Kronauer, & Czeisler, 1991, 1994; Jewett et al., 1997; Shanahan & Czeisler, 1991; Shanahan, Kronauer, Duffy, Williams, & Czeisler, 1999; Shanahan, Zeitzer, & Czeisler, 1997). This biological clock also plays a major role in the timing and architecture of sleep (Czeisler et al., 2005; Czeisler & Dijk, 2001; Czeisler & Gooley, 2007; Czeisler & Khalsa, 2000; Dijk & Lockley, 2002; Khalsa et al., 2002; Münch, Silva, Ronda, Czeisler, & Duffy, 2010; Saper, Scammell, & Lu, 2005). Spontaneous sleep duration, level of sleepiness, rapid eye movement (REM) sleep, and both the ability and the tendency to sleep vary markedly with circadian phase (or biological time of day) and interact with a homeostatic process to regulate sleep propensity and daytime alertness and neurocognitive performance (Czeisler et al., 2005; Czeisler & Dijk, 2001; Czeisler & Gooley, 2007; Czeisler, Weitzman, Moore-Ede, Zimmerman, & Knauer, 1980; Czeisler, Zimmerman, Ronda, Moore-Ede, & Weitzman, 1980; Dijk & Czeisler, 1994, 1995; Dijk, Duffy, Riel, Shanahan, & Czeisler, 1999; Dijk, Shanahan, Duffy, Ronda, & Czeisler, 1997; Khalsa et al., 2002; Van Dongen & Dinges, 2005; Wyatt, Ritz-De Cecco, Czeisler, & Dijk, 1999). The overall circadian rhythm promotes alertness and waking during the daytime, and promotes sleep at night. These day-night circadian variations in sleep-wake propensity (Dijk et al., 1992; Johnson et al., 1992) severely compromise the alertness and performance of workers who try to remain awake at night to work. Studies from a variety of occupations show consistently that night workers make more mistakes (Bjerner, Holm, & Swensson, 1955), have more occupational accidents and injuries (Drake et al., 2004; Smith, Folkard, & Poole, 1994; Smith, Colligan, & Tasto, 1982), and have a greater risk of a fatal occupational injury (Åkerstedt, Fredlund, Gillberg, & Jansson, 2002; Folkard, 2008) than do day workers. In fact, the circadian timing system not only produces lower levels of alertness during the night than in the day, but actually sends the strongest biological drive for sleep in the late night/early morning hours (e.g., ~3:00–6:00 am).
This day-night rhythm in alertness also impacts the performance of early morning workers and interferes with the ability to sleep during the daytime. The net consequence of these direct and indirect effects is an increased rate of drowsy driving related accidents especially during the latter half of the night and on the commute home after a night shift as compared to the day (National Highway Traffic Safety Administration, 2000; Drake et al., 2004; Folkard & Tucker, 2003; Novak & Auvil-Novak, 1996). In fact, the temporal distribution of motor vehicle crashes attributed to drowsy driving shows a major peak in the late night and early morning hours (e.g., ~3–6 am) (National Transportation Safety Board, 1990; Harris, 1977; Horne & Reyner, 1995; Langlois, Smolensky, Hsi, & Weir, 1985; Mitler et al., 1988; Pack et al., 1995), and an FRA review of main-track collisions found a peak accident occurrence at 4–5 am (Collision Analysis Working Group, 2006). In a recent poll of workers in a variety of transportation modes, they were significantly more likely than non-transportation workers to report working irregular schedules (National Sleep Foundation, 2012) and to have shift start times during the late evening or early morning hours, factors that are likely to contribute to disruption of their circadian rhythms and increase the risk of errors and accidents.
Time Awake
Without sleep, alertness and neurocognitive performance exhibit a steady deterioration, onto which a rhythmic circadian variation is superimposed (Boivin et al., 1997; Cajochen et al., 1999; Cajochen et al., 2002; Chee et al., 2008; Czeisler et al., 2005; Czeisler & Dijk, 2001; Czeisler, Dijk, & Duffy, 1994; Czeisler & Gooley, 2007; Czeisler & Khalsa, 2000; Dijk & Czeisler, 1994, 1995; Dijk et al., 1992; Dijk, Duffy, & Czeisler, 2000; Dijk et al., 1999; Dorrian, Rogers, & Dinges, 2005; Jewett, 1997; Jewett, Borbély, & Czeisler, 1999; Jewett, Wyatt, et al., 1999; Johnson et al., 1992; Klein et al., 1993; Wright Jr., Hull, & Czeisler, 2002; Wyatt et al., 1999). This is the so-called “sleep-wake homeostat”, a process by which sleepiness increases with longer durations of waking, and some or all of that sleepiness is then dissipated during the following sleep episode. A schematic of this process is illustrated in the upper panel of Figure 1. Acute sleep deprivation impairs judgment (Anderson & Dickinson, 2009; Babkoff, Zukerman, Fostick, & Ben Artzi, 2005; Killgore et al., 2007); cognitive performance (Doran, Van Dongen, & Dinges, 2001; Durmer & Dinges, 2005; Goel, Rao, Durmer, & Dinges, 2009; Ratcliff & Van Dongen, 2009); memory (Turner, Drummond, Salamat, & Brown, 2007); reaction time (Anderson, Wales, & Horne, 2010; Cajochen et al., 1999; Dorrian et al., 2005; Lim & Dinges, 2008); visual-perceptual ability (Anderson, Wales, et al., 2010; Horowitz et al., 2003; Kendall, Kautz, Russo, & Killgore, 2006; Rogé, Pébayle, El Hannachi, & Muzet, 2003; Russo et al., 2005; Santhi, Horowitz, Duffy, & Czeisler, 2007); distractibility (Anderson & Horne, 2006; Anderson, Wales, et al., 2010) and ability to focus attention (Anderson, Wales, et al., 2010; Turner et al., 2007), and increases the instability of waking neurobehavioral functions (Anderson, Wales, et al., 2010; Doran et al., 2001; Goel, Rao, et al., 2009) and the probability of eyelid closure and risk of loss of situational awareness, even when the eyes remain open (Anderson, Wales, et al., 2010). In fact, 24 hours of sustained wakefulness (missing a single night of sleep) has been shown to greatly impair neurobehavioral performance (Bocca & Denise, 2006; Cajochen et al., 1999; Venkatraman, Chuah, Huettel, & Chee, 2007) to an extent that is comparable to a level of 0.10 percent blood alcohol concentration (Hack, Choi, Vijayapalan, Davies, & Stradling, 2001). Ironically, instead of slowing response times to preserve accuracy, many sleep deprived individuals increase speed at the expense of making more mistakes (i.e., become ‘fast and sloppy’) and take greater risks (Horowitz et al., 2003; McKenna, Dicjinson, Orff, & Drummond, 2007). These neurobehavioral impairments associated with sleep loss are accompanied by changes in regional brain activity (Chee et al., 2006; Chee et al., 2008; Drummond et al., 2005; Drummond, Gillin, & Brown, 2001; Drummond et al., 2000; Drummond et al., 1999; Thomas et al., 2000). The instability of the waking state due to sleep loss is associated with the occurrence of so-called “micro-sleep” episodes (i.e., brief, involuntary sleep episodes < 15 seconds long) and sleep attacks (i.e., involuntary sleep episodes >15 seconds long) (Chee et al., 2008; Durmer & Dinges, 2005; Lim & Dinges, 2008), both of which can be classified as attentional failures (Barger et al., 2006; Lockley et al., 2004). The impact of 48 hours of sleep loss on neurobehavioral performance is even more severe, degrading the ability to sustain attention and vigilance (Babkoff, Mikulincer, Caspy, & Kempinski, 1988; Durmer & Dinges, 2005; Jewett, 1997; Van Dongen, Maislin, Mullington, & Dinges, 2003) and to withhold automatic responses and inhibit inappropriate responses (Drummond, Paulus, & Tapert, 2006).
Figure 1. Accumulation and Dissipation of Homeostatic Sleep Pressure in Three Conditions with Varying Durations of Waking and Sleep.
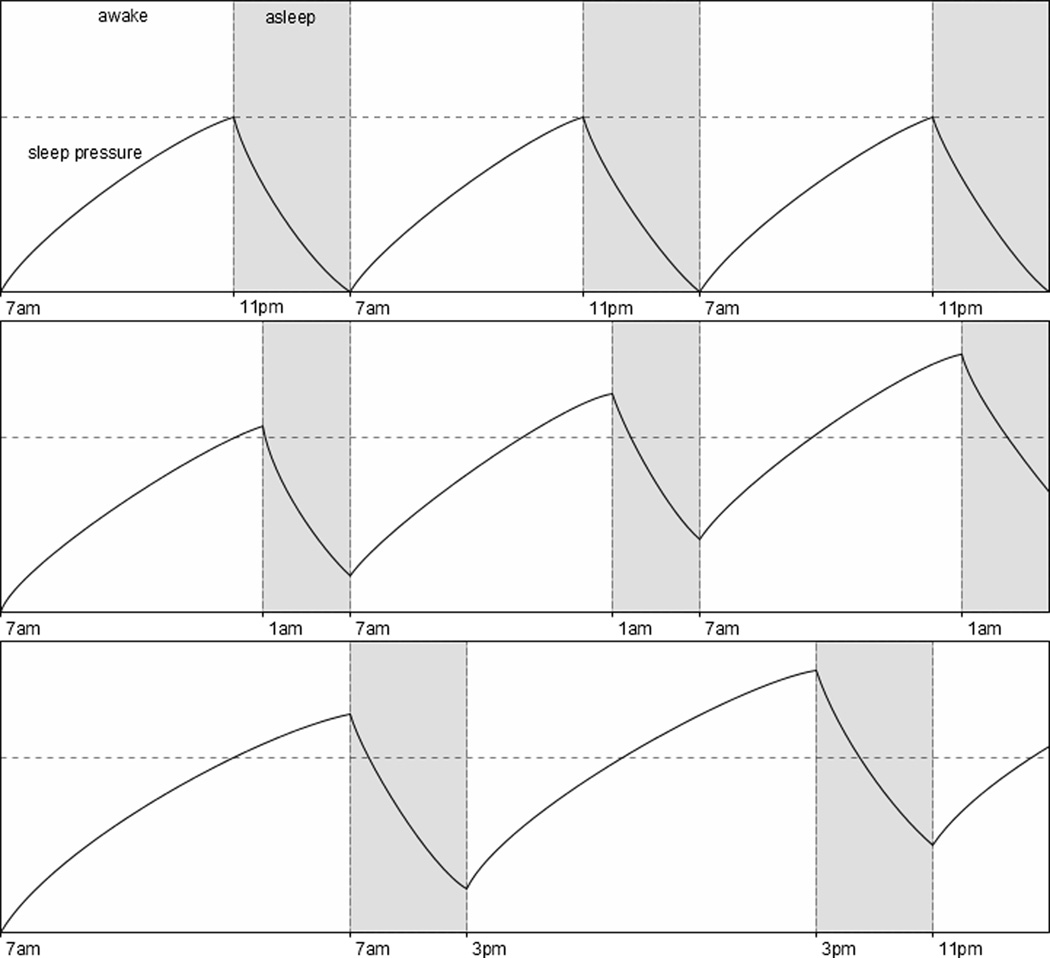
Horizontal axis: time; vertical axis: level of sleep pressure; shaded areas: sleep episodes; dashed horizontal line: typical level of sleep pressure accumulated at the end of a 16-hour waking day in someone who began the day fully rested.
Upper panel-Normal condition: Sleep pressure accumulates during the 16 hours of waking and fully dissipates during the 8 hours of nocturnal sleep. Middle panel-Chronic Sleep Restriction: Sleep pressure accumulates during the 18 hours of waking to a level slightly higher than in the normal condition (indicated by the dashed horizontal line), but due to sleep being restricted to 6 hours per night, sleep pressure does not dissipate completely, leading the next waking day to begin at an elevated level; this process continues and sleep pressure keeps building up over subsequent days. Lower panel-Acute Sleep Deprivation: Sleep pressure accumulates to such a high level during the 24 hours of waking that the following 8 hour sleep opportunity is not sufficient to bring it back to baseline. Because this recovery sleep episode occurs during the daytime when the quality of sleep is reduced, this further limits the ability of this sleep episode to bring sleep pressure back to baseline levels.
Insufficient Sleep
Equally relevant to transportation safety are the alertness and performance decrements associated with chronic partial sleep loss. Nightly sleep curtailment (also called chronic partial sleep deprivation) leads to the accumulation of a sleep “debt”, which negatively affects health and performance (Balkin, Rupp, Picchioni, & Wesensten, 2008). Multiple nights of insufficient sleep have detrimental effects on alertness, vigilance, psychomotor skills, postural stability and mood (Belenky et al., 2003; Cohen et al., 2010; Czeisler, 2003; Durmer & Dinges, 2005; Johnson, 1982; Mander et al., 2010; Naitoh, 1976; Taub & Berger, 1973; Van Dongen & Dinges, 2003; Van Dongen et al., 2003; Wilkinson, 1965). Subjective measures of stress, tiredness, sleepiness, irritability, hostility, distractibility, mood disturbances and the frequency of complaints increase, while sociability, optimism, judgment, and the ability to acquire new information decrease under chronic sleep loss (Anderson & Horne, 2006; Dinges et al., 1997; Haack & Mullington, 2005; Killgore, Balkin, & Wesensten, 2006; Killgore et al., 2007; Rupp, Wesensten, & Balkin, 2010). The impacts of insufficient sleep on performance are cumulative, and objective measures of performance, including reaction time and memory, worsen with each successive day that insufficient sleep is obtained (Belenky et al., 2003; Cain, Silva, Münch, Czeisler, & Duffy, 2010; Lee et al., 2009; Silva, Cain, et al., 2010; Silva, Wang, Ronda, Wyatt, & Duffy, 2010; Van Dongen et al., 2003). In laboratory studies, participants limited to 4 h in bed for two nights (Drake et al., 2001) or 6 h in bed for a week showed performance decrements comparable to 24 h of continuous wakefulness (Van Dongen et al., 2003).
Laboratory studies indicate that recovery from sleep loss is complex, that not all aspects of performance recover at the same rate, and recovery from a week of insufficient sleep (such as experienced during the work week by many workers) takes longer than a night or two of extended weekend sleep (Banks, Van Dongen, & Dinges, 2007; Lamond et al., 2007; Silva, Cain, et al., 2010). Thus, work schedules that cause chronic sleep restriction may generate a deterioration of performance that becomes progressively greater with additional weeks of sleep curtailment. Despite intermittent opportunities for recovery sleep on days off, individuals exposed to such schedules become progressively more vulnerable to the adverse effects of sleep loss. Furthermore, numerous studies demonstrate that subjectively, most individuals are unaware of their level of impairment from chronic sleep loss (Lee et al., 2009; Silva, Wang, et al., 2010). This poses an additional challenge to regulators and managers in safety-critical operations, because nearly half of the US working population (Gertler & DiFiore, 2009, 2011) spends fewer than 7h in bed per night, and such individuals are not aware of their level of impairment due to sleepiness and fatigue.
Interactions Between Time Awake, Circadian Time, and Recent Sleep-Wake History on Sleepiness
The impact of how long an individual has been awake on their alertness and performance interacts with their recent sleep-wake history and the time of day in a complex manner. For a given duration of wakefulness, the decline in performance associated with that duration of waking will depend on what time the wake episode began, being steeper if waking began earlier than usual or ends later than usual (Cajochen et al., 2002; Silva, Wang, et al., 2010; Wyatt et al., 1999). In addition, the rate of performance decline during typical wake durations (13–18 h) is greater if the individual has a chronic sleep debt (Cohen et al., 2010; Lee et al., 2009; Silva, Wang, et al., 2010; Thomas, Raslear, & Kuehn, 1997). These non-linear interactions are even greater when waking exceeds that of a typical waking day (>20h) (Cohen et al., 2010) or when the wake episode occurs during the biological nighttime (Cohen et al., 2010; Lee et al., 2009; Silva, Wang, et al., 2010). This latter example underlies the increased risk for drowsy driving crashes (Åkerstedt, Peters, Anund, & Kecklund, 2005) among workers commuting home after a night shift; this is an especially vulnerable time because the strong circadian drive for sleep is enhanced by the additional sleepiness resulting from having remained awake for an extended time all night (Lee et al., 2009; Silva, Wang, et al., 2010). Compounding the impact of attempting to remain awake all night at an adverse biological time, the typical night shift worker sleeps in the morning following work. This is a biological time at which it is difficult to sustain sleep for an extended duration, and night workers typically report shorter sleep durations than their day worker counterparts (Garde et al., 2009; Luckhaupt, S.E., 2012), resulting in greater levels of sleepiness on the following night. Furthermore, unlike the day worker who wakes on average 2–3 h before reporting to work (National Sleep Foundation, 2008), night workers are typically awake longer than day workers before reporting to work, resulting in the end of their work occurring after more than 12 h awake, even further reducing their ability to remain alert throughout the night shift and increasing the risk of an accident while at work or while commuting home. Nearly 10% of American workers work on the night shift or on irregular or rotating shift schedules (Bureau of Labor Statistics, 2005), accounting for approximately 12.5 million people (Bureau of Labor Statistics, 2012), and most workers drive to and from work (McKenzie & Rapino, 2011). An Australian study indicated that of work-related motor vehicle crashes, nearly 75% occurred during a commute (Boufous & Williamson, 2006). In a survey study of 635 nurses at a large metropolitan hospital in the US, we found that the odds of reporting nodding off driving to or from work in the previous year was 3.9 times higher for rotating shift workers and 3.6 times higher for night nurses compared to nurses who worked only days or evenings (Gold et al., 1992), and near-miss accidents were 2.5 times more likely to be reported by the shift workers. The increased motor vehicle crash risk from drowsy driving impacts not only those millions of shift workers who drive during their working hours or commute to and from work each night, but also impacts other drivers on the road, particularly those driving to work in the morning while night shift workers are driving home.
Sleep Inertia
Sleep inertia is a period of time immediately upon awakening during which alertness and performance are impaired, such that normal waking levels are not yet met (Balkin & Badia, 1988; Lubin, Hord, Tracy, & Johnson, 1976). It has been reported that both subjective alertness and cognitive performance are significantly impaired upon awakening even in subjects who are not sleep deprived and who are awakened at their habitual wake time (Achermann, Werth, Dijk, & Borbély, 1995; Jewett, Wyatt, et al., 1999; Wertz, Ronda, Czeisler, & Wright Jr., 2006). Previous investigations have reported varying durations of sleep inertia effects (Achermann et al., 1995; Jewett, Wyatt, et al., 1999; Federal Aviation Administration, 2010; Webb & Agnew, 1964). While most studies only measure sleep inertia over the first 20–30 minutes after awakening (Silva & Duffy, 2008; Scheer, Shea, Hilton, & Shea, 2008), studies which continue assessments up to two hours show that performance often does not plateau until an hour or more after awakening (Achermann et al., 1995; Jewett, Wyatt, et al., 1999), with the duration and impairment effects of sleep inertia being related to the duration of wakefulness preceding the sleep episode (Dinges, Orne, Whitehouse, & Orne, 1987), the sleep stage just before awakening (Cavallero & Versace, 2003; Dinges, Orne, & Orne, 1985; Silva & Duffy, 2008), and the circadian time at which awakening occurs (Scheer, Shea, Hilton, & Shea, 2008; Silva & Duffy, 2008). Sleep inertia is of greatest concern for transportation in cases where operators are on-call and/or may be required to report for duty shortly after awakening, and has been implicated in aviation accidents and errors where flight crew have napped for extended durations in flight (Transportation Safety Board of Canada, 2012; Gokhale, 2010).
Medication Use/Medical Conditions that Impact Sleepiness
Sleepiness is a frequent side effect of prescription medications, including some anti-depressants, statins, anti-hypertensives, hypnotics, anti-anxiety medications, pain management medications, anti-epileptic agents, muscle relaxants and medications to block stomach-acid secretion. Many common over-the-counter drugs also have side-effects that include sleepiness, including diphenhydramine, an anti-histamine sold for treating allergy symptoms but also the active ingredient in many over-the-counter sleeping pills sold in the U.S. Stimulants and drugs of abuse can also have a profound effect on the ability to sustain alertness and performance. Caffeine is the most widely used psycho-active agent in the world, fueling our 24/7 society. Because caffeine antagonizes the actions of adenosine (Dunwiddie & Masino, 2001), a neuromodulator that mediates the sleep-inducing effects of prolonged wakefulness (Porkka-Heiskanen et al., 1997), it can temporarily increase alertness while not reducing any sleep debt. While caffeine and other wake-promoting compounds may improve alertness, they cannot substitute for sleep, and may interfere with sleep when the opportunity for sleep arises (Drake, Roehrs, Shambroom, & Roth, 2013; LaJambe, Kamimori, Belenky, & Balkin, 2005). In a study of fatal-to-the-driver truck crashes, the National Transportation Safety Board found that plasma caffeine levels were highest in drivers involved in fatigue-related crashes (1990, 1995). They interpreted those findings as indicating that the sleepiest drivers were taking caffeine to try to (unsuccessfully) combat their fatigue. Alcohol, another major drug of abuse, is a central nervous system depressant that increases sleep propensity during wakefulness but disrupts sleep consolidation after sleep onset. Even low doses of alcohol synergistically interact with sleep loss to greatly increase sleep propensity (Roehrs, Beare, Zorick, & Roth, 1994; Vakulin et al., 2007), degrade driving performance and increase crash risk in a driving simulator (Banks, Catcheside, Lack, Grunstein, & McEvoy, 2004; Horne, Reyner, & Barrett, 2003; Howard et al., 2007; Vakulin et al., 2007) and on the road (Philip, Vervialle, Le Breton, Taillard, & Horne, 2001). Healthy professional drivers who were awake for 18 to 21 hours and were exposed to legal low-dose alcohol (blood alcohol concentration of 0.03 g/dL) had significantly more attentional failures and greater variation in both lane position and speed in a driving simulator than they did when their blood alcohol concentration exceeded 0.05 g/dL—a level associated with significantly increased risk of a motor vehicle crash (Howard et al., 2007).
Many medical conditions disrupt sleep, leading to increased daytime sleepiness. Arthritis, peripheral vascular disease, and other conditions with pain disrupt sleep, causing sleep fragmentation and reducing the time spent in the deepest stages of sleep. Patients with gastroesophageal reflux disease, heartburn, and chronic obstructive pulmonary disease experience sleep disruption associated with the supine position assumed for sleep. Restless legs syndrome (RLS), which the National Institutes of Health estimates to affect 5–15%of Americans (National Heart, Lung, and Blood Institute, 2010), makes it difficult to initiate sleep due to unpleasant feelings in the legs. Patients with RLS typically experience symptoms in the evening or at night and while quietly resting, and the symptoms only dissipate when the legs are moved. RLS is strongly associated with periodic limb movements of sleep (PLMS), in which the leg or arm muscles twitch or jerk during sleep, leading to sleep disruption and fragmentation once sleep is initiated (Allen et al., 2003).
Obstructive sleep apnea (OSA) is a common sleep disorder in which the supine posture of sleep, combined with the reduction in muscle tone during sleep, result in partial or complete airway obstruction. While healthy individuals have occasional airway obstructions during sleep, people with OSA have frequent (>10–15 times per hour of sleep) obstructions that are associated with hypoxia and brief arousals to reopen the airway. These frequent arousals fragment sleep and can lead to daytime sleepiness, although not all individuals with OSA report daytime sleepiness. In general, vigilance and the ability to sustain attention are degraded in patients with OSA. Reaction times in patients with mild to moderate OSA have been reported to be comparable to or worse than those of a young adult with a blood alcohol concentration of 0.080 g/dL (Powell et al., 1999). Untreated patients with OSA perform much more poorly in a driving simulator (in terms of lane deviations, tracking errors, off-road events and collisions with obstacles) and are 6 to 10 times (i.e., about 500% to 1,000%) more likely to have an actual motor vehicle crash than people without OSA (Findley et al., 1995; Findley & Bonnie, 1988; Findley, Fabrizio, Thommi, & Suratt, 1989; Findley, Levinson, & Bonnie, 1992; Findley, Unverzagt, & Suratt, 1988; Findley, Weiss, & Jabour, 1991; George, 2004; George, Boudreau, & Smiley, 1996; George, Nickerson, Hanly, Millar, & Kryger, 1987; Hack et al., 2001; Schwartz, 1991; Teran-Santos, Jimenez-Gomez, & Cordero-Guevara, 1999). OSA is a concern for operators in all modes of transportation, and in two surveys of railway T&E workers, sleep apnea was reported by 6–8% of the respondents (Gertler & DiFiore, 2009, 2011), likely to be an underestimate of the true prevalence due to the demographic characteristics of the T&E workforce and the prevalence of OSA among other worker groups (Rajaratnam et al., 2011; Barger et al., 2015). A recent screening program of nearly 20,000 commercial drivers found that more than 20% had OSA (Berger et al., 2012). Recent NTSB accident reports include undiagnosed or untreated sleep apnea in the operator as possible contributing factors to accidents (National Transportation Safety Board, 2002, 2011b). Because of the strong association between obesity and OSA, and the fact that many individuals with OSA are not aware of it (Howard et al., 2004; Pavlova, Duffy, & Shea, 2008), screening of obese individuals for OSA in safety-sensitive occupations is strongly recommended (Ancoli-Israel, Czeisler, George, Guilleminault, & Pack, 2008; Talmage, Hudson, Hegmann & Thiese, 2008), so that those individuals can be treated to avoid both the safety hazards and the medical consequences of OSA (Czeisler, 2015). A 2004 study estimated that the cost of treating all patients in the US with OSA would be worthwhile considering the cost savings from reducing motor vehicle accidents (Sassani et al., 2004).
Duration of Work
Duration of work shift can have an impact on error and accident risk, although the impact of work duration is difficult to separate from the impact of time awake. The number of consecutive work hours; the number of consecutive days of work; the time of day and the frequency of rest breaks have all been found to influence the risk of error and accident (Dembe, Erickson, Delbos, & Banks, 2005; Folkard & Lombardi, 2006; Loomis, 2005; Rogers, Hwang, Scott, Aiken, & Dinges, 2004). A meta-analysis found that the relative risk of injury or accident is more than doubled after 12-hours of work (Folkard & Lombardi, 2006), and increases with the duration of time since the last break. Rogers and colleagues found that the risk of error was three times higher when nurses worked shifts of 12.5 hours or longer, and increased work duration, overtime and working more than 50 hours in a week also increased the risk of error (Rogers et al., 2004). Overtime after long shifts further increased the risk of error (Rogers et al., 2004). A 12-hour night shift combines the effects of extended work hours with work at adverse circadian time, and this combination increases the risk of fatigue related error and accident at work and on the commute home. Long work hours also result in reduced opportunity for recovery sleep, and increase the risk of error and accident when such shifts are worked on successive days. Similar increases in error or accident risk with prolonged task performance have also been shown for non-commercial drivers (Philip, Taillard, Quera-Salva, Bioulac, & Åkerstedt, 1999).
Given that full time employees on 12-hour schedules work 50 to 100 fewer days per year than do full time employees on 8-hour work schedules, such schedules are often quite popular among workers (Thomas, Schwartz, & Whitehead, 1994). When workers experienced with both 8- and 12-hour night shifts were asked which shift resulted in fatigue which decreased their performance at work, 80 percent of respondents felt that the 12-hour workday resulted in the least efficient performance due to fatigue (Tepas & Mahan, 1986). In addition, studies of conversions from 8-hour to 12-hour shifts in a power plant and a natural gas utility conducted by NIOSH researchers have demonstrated that introduction of 12-hour shifts results in consistent declines in performance and alertness and increased fatigue, especially for those on the 12-hour night shift (Lewis et al., 1986; Rosa & Bonnet, 1995; Rosa et al., 1990; Rosa & Colligan, 1995). A follow-up study in the same facility 3.5 years after imposition of the 12-hour shift schedule demonstrated that the declines in performance and alertness attributable to the extra 4 hours on shift were still apparent, with no improvement due to adaptation (Rosa & Colligan, 1995).
The relevance of work duration in transportation is illustrated in a 2000 FMCSA Federal Register proposed rule. In that document, Chart 5 shows data from 1991–1996 on the relative risk of a fatigue-related truck crashes with increased hours driving ("Hours of service of drivers; driver rest and sleep for safe operations," 2000). Those data show that the relative risk of a fatigue-related crash increases sharply after 8–10 hours driving, and there was a 15-fold increase in the risk after 13 hours of driving compared to 1 hour of driving.
Distractions, and Interaction of Sleepiness with Distraction
Driver/operator distraction is a major safety concern in all modes of transportation. Distractions compromise safety by taking the operator’s attention away from their operational environment (the road/track ahead, their instruments), and even when such distractions are brief, if they occur at critical moments they can have serious consequences. Distractions become even more of a concern in high-speed operating conditions where the time for responding to operational challenges is shorter. Recent laboratory research has shown that distractibility markedly increases when individuals are fatigued (Anderson & Horne, 2006; Anderson, Wales, et al., 2010), and the authors concluded that sleepy individuals may actually seek out distractions, perhaps in an attempt to remain awake and/or due to an inability to suppress their responses to distractions. A video study of long and short-haul truck drivers found that when drowsy, drivers spent less time visually scanning their environment but spent more time adjusting their position, conversing with a passenger, and scratching their face or head (Barr, Yang, Hanowski, & Olson, 2011). The National Transportation Safety Board has found distractions, typically from cell phone usage or text messaging, to be a contributing factor in a series of recent major accidents in all modes of transportation, causing deaths, injuries, and millions in damage (2011a, 2011b, 2011c).
Sleep-Wake Transitions and Automatic Behavior
Individuals struggling to stay awake under conditions of elevated sleep pressure—whether due to acute sleep deprivation, chronic sleep restriction, or repeated interruption of sleep (due to external interruptions or the presence of a sleep disorder)—are not always able to do so. Sleep deprivation greatly increases the risk that an individual will succumb to the increased sleep pressure when their brain initiates an involuntary transition from sleep to wakefulness. This transition is initiated by the ventrolateral preoptic (VLPO) area of the hypothalamus, which has been identified as the brain’s “sleep switch” (Saper, Fuller, Pedersen, Lu, & Scammell, 2010; Saper et al., 2005). These classic consequences of chronic sleep loss are particularly evident while doing a routine task like driving (Strohl et al., 1998). In a condition of chronic sleep deprivation, even when work (or wakefulness) is scheduled during an appropriate circadian phase, the probability of a sleep-related performance failure while working or driving is markedly increased. Of course, once an individual has lost the struggle to stay awake and makes the transition from wakefulness to sleep—however briefly—driving performance is much worse than that of a drunk driver, as the individual is unresponsive to the environment throughout the duration of the microsleep episode or the sleep attack. In addition to outright falling asleep, sometimes drowsy individuals linger in an intermediate state between sleep and wakefulness. In this situation, which probably represents a transitional state in which part of the brain is asleep while part of the brain remains awake (Vyazovskiy et al., 2011), the operator of a motor vehicle may maintain full pressure on the accelerator and proceed for a considerable distance, even negotiating gradual turns and exhibiting goal-directed behavior, but fail to heed stop signals or respond appropriately to traffic conditions in a timely manner. This intermediate state, which has been termed automatic behavior syndrome, is characterized by the ability to perform some aspects of operating the vehicle (maintaining pressure on the accelerator, and in some cases turning the steering wheel), but doing so without appropriate situational awareness or judgment (Guilleminault, Billiard, Montplaisir, & Dement, 1975; Guilleminault, Phillips, & Dement, 1975). In the case of a motor vehicle driver, this can result in driving toward the flashing hazard lights of a disabled or public safety vehicle in the breakdown lane. A striking example of apparent automatic behavior was documented when the husband of a motorist who was nearly driven off the highway by a drowsy driver called 911 to report the drowsy driver and then videotaped the drowsy driver as she drove for 30 minutes on U.S. Interstate 25 in Denver (ABC 7News Denver, 2007).
METHODS FOR ASSESSMENT OF FATIGUE AND SLEEPINESS IN THE LABORATORY AND IN THE FIELD
We currently do not have good measures of individual sleep need, or ways to assess a person’s level of sleep deficiency. Sleepiness is a subjective feeling, but the deficits from insufficient sleep can be objectively assessed in a variety of ways. Findings from neuroimaging studies suggest that sleep deprivation particularly affects the prefrontal cortex, a brain region associated with alertness, attention and higher order cognitive functions (Thomas et al., 2000). Fluorodeoxyglucose positron emission tomography (PET) studies of subjects who performed a serial addition/subtraction task revealed that 24 h of sleep deprivation reduced regional cerebral metabolic rate in the prefrontal cortex (Thomas et al., 2000). Functional magnetic resonance imaging (fMRI) studies similarly revealed that during performance of serial subtraction tests, prefrontal cortical activation decreased after 35 h of sleep deprivation; in contrast, during performance of verbal learning and divided attention tests, prefrontal activation increased (Drummond & Brown, 2001). The increases were associated with increases in subjective sleepiness, and may represent cerebral compensation for the effects of sleep deprivation (Drummond et al., 2000). People who are sleep deprived exhibit cognitive deficits that resemble those observed in patients with prefrontal cortical lesions. These deficits include impaired planning abilities (Harrison & Horne, 1999, 2000), flatness of speech (Harrison & Horne, 1997), and increased perseveration [e.g., (Harrison & Horne, 1997, 1999; Horne, 1988)]. The extent of the effects of sleep deprivation seems to depend on the complexity of the task (Chee & Choo, 2004). FMRI studies have shown multiple changes in both cortical activation and deactivation that accompany performance in various tasks under conditions of sleep deprivation (Chee & Choo, 2004). These fMRI changes are thought to underlie both the observed deterioration and conservation of performance in tasks of varying complexity.
A variety of tests are used to determine the cognitive impairments associated with sleep loss. One of the most widely used, in both laboratory and field settings, is the psychomotor vigilance task (PVT; Dinges & Powell, 1985; Kribbs, Pack, & Dinges, 1994; Lamond, Dawson, & Roach, 2005). The PVT is a test of visual reaction time (RT) in which the subject is asked to maintain the fastest possible RTs to a simple visual stimulus for several minutes. PVT performance has been shown to decline with duration of wakefulness (Wyatt, Cajochen, Ritz-De Cecco, Czeisler, & Dijk, 2004), and to show an interaction between circadian and wake-dependent factors (Cain et al., 2010; Silva, Wang, et al., 2010; Wyatt et al., 1999). Tests of cognitive throughput (Dijk et al., 1992; Gillooly, Smolensky, Albright, Hsi, & Thorne, 1990; Johnson et al., 1992; Klein, Wegmann, Athanassenas, Hohlweck, & Kuklinski, 1976; Monk & Carrier, 1997; Wyatt et al., 2004), attentional selection (Santhi et al., 2007), executive function (Cain, Silva, Chang, Ronda, & Duffy, 2011; Lingenfelser et al., 1994; McCarthy & Waters, 1997; Stenuit & Kerkhofs, 2008), and short-term memory (Wright Jr. et al., 2002; Wyatt et al., 2004; Wyatt et al., 1999) are also used in studies of sleep loss. In addition to these general types of performance, specific types of job-relevant performance assessments have also been used in the controlled laboratory setting, including performance driving an automobile (Howard, Gora, Swann, & Pierce, 2002; Vakulin et al., 2007) or train simulator (Thomas et al., 1997).
EEG measures can also be used to determine relative sleepiness by recording waking EEG signals and examining them with spectral analysis. An advantage of EEG is that it can be collected continuously while the individual being monitored is performing other tasks, although there are many practical and technical difficulties with using it in field settings. With prolonged wakefulness, EEG activity in lower frequencies increases (especially over more frontal brain regions; Aeschbach et al., 1997; Cajochen et al., 1999), with prominent increases in delta and theta frequencies (Aeschbach et al., 1999; Åkerstedt & Gillberg, 1990) that are associated with performance failures in the laboratory (Makeig & Jung, 1996) and in the field (Cabon, Coblentz, Mollard, & Fouillot, 1993; Torsvall & Åkerstedt, 1987). Eye movements are also used as an index of relative sleepiness, as it has been known for many years that slow rolling eye movements (SEM) and prolonged eyelid closure are both associated with the onset of sleep and are increased during quiet wakefulness when the individual has been awake for a long time (Åkerstedt & Gillberg, 1990; Aserinsky & Kleitman, 1955; Santamaria & Chiappa, 1987).
Laboratory studies suggest that ocular and oculomotor measures may be more reliably related to impaired vigilance and behavioral lapses than EEG measures of drowsiness (Dinges, Mallis, Maislin & Powell, 1998). Changes in the frequency, amplitude and duration of blinks, and episodes of slow eye closure occur in response to sleep deprivation and during the biological nighttime (Åkerstedt et al., 2005; Caffier, Erdmann, & Ullsperger, 2003; Johns, Tucker, Chapman, Crowley, & Michael, 2007). An increase in the percentage of time the eyes are at least 80% closed (PERCLOS) has been reported in drowsy participants during task performance, and correlates well with vigilance and simulated driving tasks in the laboratory (Mallis, Maislin, Powell, Konowal, & Dinges, 1999; Research & Standards, 1998; Dinges, Mallis, Maislin & Powell, 1998; Wierwille & Ellsworth, 1994). While controlled laboratory studies have shown that PERCLOS can closely track performance lapses, use of camera-based PERCLOS technology in real-world settings has encountered problems, including the ability to function in bright or highly variable lighting conditions, and in operators wearing sunglasses or eyeglasses. However, in the fatigued state, failure in the performance of a visual task such as driving is caused not only when the eyelids are closed, but can also occur when the eyelids are open by a process of visual suppression or neglect (Anderson, Chang, Sullivan, Ronda, & Czeisler, 2013; Anderson, Wales, et al., 2010; Chapman, Johns, & Crowley, 2006). In fact, the performance-related dangers of drowsiness begin well before long eyelid closures occur. Some reports suggest that the velocity and amplitude of eyelid movements may provide useful indicators of drowsiness, and that the use of multiple eyelid closure metrics may improve the prediction of drowsiness (Caffier et al., 2003; Johns et al., 2007). A few studies conducted in driving simulators (Åkerstedt et al., 2005; Howard et al., 2002; Phipps-Nelson, Redman, & Rajaratnam, 2011; Shin, Sakai, & Uchiyama, 2011), as well as small field studies (Ftouni et al., 2013; Lee et al., 2012) have reported that measures of eyelid velocity and amplitude are associated with driving impairments, and thus may be a promising tool for real-time detection of drowsiness in operational settings.
SUBJECTIVE FATIGUE AND SLEEPINESS: POOR ESTIMATES OF OBJECTIVE DEFICITS IN ATTENTION AND PERFORMANCE
The impact of sleep loss on performance and attention can be measured with a variety of objective tests, as outlined above. However, as noted, many of those methods require specialized equipment and/or take the operator’s attention away from the task at hand. For this reason, subjective assessments of sleepiness have been advocated as measures of potential performance impairment. While there is evidence that in general both subjective and objective measures of sleepiness change in parallel, this is not always the case especially with chronic sleep loss. Moreover, individuals routinely underestimate their level of sleepiness, degree of impairment from sleepiness, and potential for a sleepiness-related accident.
Laboratory studies indicate that individuals can typically perceive a change in their level of sleepiness when sleep is acutely curtailed (Duffy, Willson, Wang, & Czeisler, 2009). However, they are far less accurate in estimating their sleep-related impairments under conditions of chronic partial sleep loss (Silva, Cain, et al., 2010; Silva, Wang, et al., 2010). For example, in a 14-day chronic sleep restriction study subjective sleepiness ratings showed an acute response to the first night of sleep restriction, but only small further increases on subsequent days, even though performance continued to decline each subsequent day (Van Dongen et al., 2003). Another study found performance to be independent of subjective sleepiness in both acute and chronic sleep deprivation conditions, suggesting that objective and subjective measures represent distinct entities that should not be assumed to be equivalent (Franzen, Siegle, & Buysse, 2008). And studies in our laboratory that involve many days of sleep disruption or sleep restriction have found that while objectively assessed performance continues to decline over subsequent days of partial sleep loss, subjective assessments of alertness decline initially (typically only on the first or second day after sleep loss) but then level off and no longer parallel the objective deficits in performance (Silva, Cain, et al., 2010; Silva, Wang, et al., 2010). It may be that individuals can perceive large changes in response to sleep loss when they begin at a high level of alertness, but they are less able to perceive more gradual changes due to chronic sleep loss. In general, most individuals are poor judges of their fatigue-related performance impairment. Complicating this, drowsiness is often not a uniform state but can come and go in waves (Thorpy & Billiard, 2011). When fatigued, small areas of the sleepy brain can transiently go “off-line” and show sleep-like activity, while the individual overall remains awake but in an impaired state (Vyazovskiy et al., 2011). This so-called “local sleep” becomes more and more likely with longer durations of wakefulness (Hung et al., 2013). This may underlie the observation that while sleepy individuals can often mask their feeling of drowsiness temporarily by changing some aspect of their environment (activity level, temperature, noise level; Thorpy & Billiard, 2011), such strategies provide only temporary relief, and as wakefulness continues the strategies become more and more ineffective (Schwarz et al., 2012).
While additional research is warranted to understand individual differences in the subjective-objective sleepiness disconnect and whether individuals can be trained to be better judges of their actual sleep-related vulnerabilities, the existing evidence indicates that subjective sleepiness ratings are not an appropriate tool for measuring objective performance and alertness levels, at least in real-world settings where variations in environmental factors are difficult or impossible to control and where the use of stimulants may mask although not reverse performance impairments due to sleep loss (Buxton et al., 2010).
INDIVIDUAL DIFFERENCES IN RESPONSE TO SLEEP LOSS
Inter-individual differences play an important role in the response to chronic and acute sleep loss (Van Dongen, Baynard, Maislin, & Dinges, 2004; Van Dongen et al., 2003). LeProult et al. (2003) reported that there were stable individual differences in the response to acute sleep deprivation but that objective and subjective measurements of the response to sleep deprivation were unrelated. Thus, individuals who have the subjective perception that they are highly susceptible to the effects of sleep deprivation are not necessarily the same individuals who show the largest performance impairments during sleep deprivation. Similarly, the study of Frey et al. (2004) found that no individual was particularly vulnerable or resistant to all the effects of sleep deprivation. Rather, sleep deprivation effects were task dependent, as was also shown previously by Van Dongen and colleagues (2004). Van Dongen has also reported that individual responses to sleep deprivation and sleep restriction have trait-like characteristics (Van Dongen, Doran, & Dinges, 2000; Van Dongen, Baynard, et al., 2004; Van Dongen, Maislin, & Dinges, 2004; Van Dongen, Olofsen, Dinges, & Maislin, 2004). They found that when subjects were brought back to the laboratory for repeat visits, the same ones remained particularly vulnerable while others remained resistant to the adverse effects of sleep loss on cognitive performance (Van Dongen, Baynard, et al., 2004). While all the subjects had more lapses of attention after a night without sleep, the stable individual trait differences accounted for 67% to 92% of the variance in the performance decrement induced by sleep loss, and persisted even when participants were either well rested (12 hours in bed each night for a week) or sleep restricted (6 hours in bed each night for a week) before they stayed awake all night (Van Dongen, Baynard, et al., 2004).
Differences in Vulnerability to Sleep Loss Due to Recent Sleep-Wake History
As described above, the ability to sustain attention, maintain cognitive performance and prevent attentional failures deteriorates when the sleep of individuals with habitual sleep durations in the ~8 hour range is restricted to 7 or fewer hours per night for many nights in a row (Belenky et al., 2003; Dinges, 2004; Policy, 2006; Van Dongen et al., 2003). However, there is also evidence from sleep extension studies suggesting individuals who habitually sleep 8 hours or fewer per night may actually have a chronic sleep debt, and that individuals with habitually short sleep durations may not reflect true underlying sleep “need” (Dinges, 2005; Klerman & Dijk, 2005; Roehrs, Timms, Zwyghuizen-Doorenbos, & Roth, 1989; Wehr et al., 1993). In both cases, when such individuals were brought into the laboratory for sleep extension, they performed significantly better after sleep extension than they had at baseline, suggesting that they had a chronic sleep debt. It is not only the duration of recent sleep that can make an individual vulnerable to subsequent sleep loss, but the regularity of their recent sleep can also contribute. Whether sleep irregularity is due to shift work, transmeridien travel, or social jet lag (Wittmann, Dinich, Merrow, & Roenneberg, 2006), it can lead to changes in circadian timing which in turn can impact resiliency to sleep loss (Committee on Sleep Medicine Research Board on Health Sciences Policy, 2006). Given the widespread amount of short sleep among the general population, many individuals may be vulnerable to even modest (additional) amounts of sleep loss due to their chronic insufficient sleep. This concept is supported by studies that examined the number of traffic accidents following the switch to daylights savings time in the spring. The springtime change is associated with a one-hour loss of sleep, yet this modest change results in 6–11% more traffic accidents in the days immediately following the daylight savings time transition, suggesting that the affected drivers may have had an underlying vulnerability to even such a modest amount of sleep loss (Coren, 1996; Monk, 1980; Varughese & Allen, 2001). Both acute and chronic sleep loss, whether caused by work schedules, family responsibilities, social activities or health problems, will degrade tolerance and increase performance vulnerability to any subsequent sleep loss. Moreover, recent studies suggest that an 8–10 hour recovery sleep is not sufficient to return the performance levels of individuals who have recently had chronic sleep loss back to baseline (Banks, Van Dongen, Maislin, & Dinges, 2010). Thus, individuals who obtain less sleep than needed during the work week may not be able to make up for that sleep loss by extending their sleep on the weekend.
Age-Related Differences in the Vulnerability to Sleep Loss
There are reports of a ‘global slowing’ in cognitive function associated with aging. This has been reported in attentional tasks, where the average reaction times of older subjects tend to be longer than the average reaction times of young adult subjects. This loss of speed has been attributed to not only a ‘global slowing’ but also a reduction in attentional resources with age. In one study the performance of young and older adults were compared in a full attention and divided attention task (Anderson, 1999). There was an overall increase in reaction time in both the full and the divided attention tasks in the older subjects. However, not all tasks show a performance impairment in older adults relative to younger adults. A number of studies which have examined the neurophysiological basis of age-related changes in cognitive functioning show that the differences between young and older adults are not simple, and the same cognitive task can engage different brain regions in younger and older adults (Grady et al., 1994; Grady et al., 1998). In particular, in older adults regions of the brain associated with higher order cognitive functions seem to be activated in order to preserve performance in some cognitive tasks. Data from highly screened older adults suggest that the reported impact of aging on cognition may be due less to aging per se than to consequences of aging on health and sleep. In fact, several laboratory studies have demonstrated that healthy older adults without sleep disorders maintain their attention and performance better when acutely or chronically sleep deprived than do young adults (Adam, Rétey, Khatami, & Landolt, 2006; Bonnet, 1989; Bonnet & Rosa, 1987; Buysse et al., 1993; Duffy et al., 2009; Silva, Wang, et al., 2010). We and others have hypothesized that the common age-related changes in homeostatic sleep-wake regulation that disrupt sleep at night may also make it less likely that a healthy older adult falls asleep in response to acute or chronic sleep loss (Carrier, Land, Buysse, Kupfer, & Monk, 2001; Dijk & Duffy, 1999; Dijk, Duffy, & Czeisler, 2001). However, very healthy older individuals without sleep disorders are rare, and while older drivers are less likely to report driving when drowsy or dozing off behind the wheel than younger adults (National Sleep Foundation, 2003), 15% of those age 65+ reported doing so within the past year in a scientific poll conducted by the National Sleep Foundation.
Young adults are especially vulnerable to the impacts of sleep loss. This is likely due in part to their strong homeostatic sleep-wake regulation and the insufficient sleep they regularly obtain. More than half of adolescent drivers reported that they had driven drowsy during the past year in a National Sleep Foundation survey, with 15% of 10th, 11th and 12th graders reporting driving drowsy at least once per week (National Sleep Foundation, 2006). Drowsy driving, when combined with the relative inexperience and risk-taking behavior of young drivers, results in a greater likelihood of motor vehicle crash. The potential impact of insufficient sleep on teen crash risk has been highlighted in a recent paper by Vorona and colleagues. They examined crash data from two adjacent counties in Virginia where high school start times differed by nearly 1.5 hours and found that in the county with the earlier school start times (assumed to be associated with reduced sleep duration), crash rates were about 10% higher on weekdays during the school year among teenage drivers, but did not differ among adult drivers (Vorona et al., 2014). In fact, teenage drivers are overrepresented in fatal crashes, with a NHTSA study finding that even though drivers age 15–20 represented only 6.3% of total drivers, they were involved in 18% of the police-reported crashes and in 13.8% of the fatal crashes (National Highway Traffic Safety Administration, 2005b). Teen drivers are 4 times more likely than older drivers to have a motor vehicle crash (Insurance Institute for Highway Safety, 2006), and motor vehicle crashes injure approximately 450,000 teenagers each year (National Highway Traffic Safety Administration, 2005b) and are the leading cause of death for 16–20 year olds (National Highway Traffic Safety Administration, 2005a, 2005b).
Genetic Basis of Individual Differences in Vulnerability to Sleep Loss
Genetic polymorphisms may account for differences in the ability of some individuals to tolerate sleep loss. A variable length tandem repeat polymorphism in the PER3 gene (PER3 5/5), found in 10–15% of the population, has been reported to confer a particular vulnerability to the performance- impairing effects of 24 hours of wakefulness (Groeger et al., 2008; Viola et al., 2007), although not to daytime performance under nighttime sleep restriction (Goel, Banks, Mignot, & Dinges, 2009). On the other hand, a haplotype of the adenosine A2A receptor gene (ADORA2A), may be associated with resistance to the effects of sleep loss on performance (Retey et al., 2006; Rupp, Wesensten, Newman, & Balkin, 2013), and more rare variants have been identified that are associated with an apparent need for less sleep (He et al., 2009; Pellegrino et al., 2014). These recent findings suggest that it may soon be possible to identify a subset of individuals who will exhibit reduced performance degradation when deprived of sleep and another subset whose performance will deteriorate markedly when they are sleep deprived. Such information could be used to identify individuals best-suited for critical and safety-sensitive tasks in situations where long-duration work episodes are unavoidable. It could also be used to identify individuals who are at greater risk for sleepiness-related errors when they do not obtain sufficient sleep so that they are deployed to tasks where sustained attention is less critical and/or can employ countermeasures strategically. While our understanding of the genetic basis of individual differences in response to sleep loss is in the early stages currently, as knowledge in this area grows it will provide the potential for this information to be used in personalized occupational medicine.
LABORATORY AND FIELD INTERVENTIONS TO REDUCE FATIGUE
Drowsiness is the intermediate state between alert wakefulness and sleep, and usually lasts only a few minutes when we are falling asleep intentionally, but can last much longer when we are struggling to stay awake, as for example when driving at night (Kecklund & Åkerstedt, 1993; Torsvall & Åkerstedt, 1987). Drowsiness is a fluctuating state of reduced awareness and impaired performance and estimated to be a contributing factor in up to 20% of road crashes (Klauer et al., 2006; Committee on Sleep Medicine Research Board on Health Sciences Policy, 2006; Tefft, 2014) and a possible contributing factor in nearly 30% of railway collisions (Collision Analysis Working Group, 2006). The primary method for monitoring sleep, sleepiness, and wakefulness uses the electroencephalogram (EEG), electrooculogram, and electromyogram (Åkerstedt, 1984; Torsvall & Åkerstedt, 1987; Torsvall, Åkerstedt, & Gillberg, 1981). Increased EEG alpha and theta activity, slow rolling eye movements (SEMs), prolonged eyelid closure duration, and changes in the rate of eyelid reopening are evident in drowsy individuals prior to sleep onset (Santamaria & Chiappa, 1987). While increased EEG theta activity is associated with behavioral lapses in the laboratory (Makeig & Jung, 1996), there are significant practical and technical difficulties in utilizing EEG as a real-time measure of drowsiness, and few studies have been able to identify relationships between EEG signs of drowsiness in operational settings (Cabon et al., 1993).
Laboratory studies suggest that ocular and oculomotor measures are related to impaired vigilance and behavioral lapses due to drowsiness (Dinges, Mallis, Maislin & Powell, 1998). Changes in the frequency, amplitude and duration of blinks and episodes of slow eye closure occur in response to sleep deprivation and during the biological nighttime (Åkerstedt et al., 2005; Anderson, Chang, Ronda, & Czeisler, 2010; C. Anderson, Wales, et al., 2010; Caffier et al., 2003; Chapman et al., 2006; Dinges & Grace, 1998; Dinges, Mallis, Maislin & Powell, 1998; Johns et al., 2007; Mallis et al., 1999), and these ocular changes correlate with decrements in vigilance and driving simulator performance in the laboratory (Akerstedt et al., 2005; Dinges, Mallis, Maislin & Powell, 1998; Howard et al., 2002; Phipps-Nelson et al., 2011; Shin et al., 2011; Wierwille & Ellsworth, 1994). For these reasons, devices have been developed to monitor ocular or oculomotor parameters in real time and provide operator feedback. These include both eyeglass-mounted systems and camera-based systems. In a recent field study carried out among Australian shift working nurses, strong associations were found between oculomotor measures of drowsiness and increased odds of self-reported adverse driving events during commutes following night shifts (Ftouni et al., 2013), and we carried out a pilot study in shift workers driving an instrumented automobile on a closed track showing associations between EEG and oculomotor measures of drowsiness and critical driving events (Lee et al., 2012). However, there remains a relative paucity of studies evaluating the ability of these ocular measures to detect impaired vigilance as a result of drowsiness, particularly in field settings. There is also insufficient information about the ability of such systems to prevent fatigue-related accidents (Balkin, Horrey, Graeber, Czeisler, & Dinges, 2011). Furthermore, these systems are being sold as safety features for drivers of non-commercial vehicles, with little evidence for their accuracy or sensitivity. Drivers of those vehicles may take greater risks in driving when they are drowsy if they believe the technology may prevent crashes.
Caffeine is used widely to ameliorate the impacts of insufficient sleep. Laboratory studies (including those in our own lab) indicate that caffeine can counteract some or all of the attentional deficits in individuals who are acutely or chronically sleep-deprived (Babkoff, French, Whitmore, & Sutherlin, 2002; Kamimori, Johnson, Thorne, & Belenky, 2005; Lieberman, Tharion, Shukitt-Hale, Speckman, & Tulley, 2002; McLellan et al., 2005; Penetar et al., 1993; Wesensten et al., 2002; Wright Jr., Badia, Myers, & Plenzler, 1997; Wyatt et al., 2004). Driving simulator studies have also found that alertness and in some cases driving ability in sleepy drivers are also improved by caffeine (De Valck, De Groot, & Cluydts, 2003; Horne & Reyner, 1996; Reyner & Horne, 1997). In a study of actual highway driving in France, Philip and colleagues found that 200 mg caffeine significantly improved middle-of-the-night driving compared with placebo (Schweitzer, Randazzo, Stone, Erman, & Walsh, 2006), returning some aspects of driving performance to daytime levels (Philip et al., 2006). An Australian case-control study of long-distance commercial drivers who had crashes found that those who reported consuming caffeine for the purpose of staying awake had a 63% reduced likelihood of crashing (Sharwood et al., 2013). While this evidence supports the use of caffeine as a countermeasure for drowsy driving and forms the basis for drowsy driving recommendations in some countries [including the UK and Australia] and US states, several US states recommend against using caffeine to promote wakefulness among drowsy drivers. The argument against caffeine as a countermeasure to drowsiness is that caffeine is only a temporary solution, it does not eliminate the need for sleep, and it may give the driver a false sense of fitness for continuing to drive. This argument is supported by an NTSB study of fatal-to-the-driver truck crashes, which found plasma caffeine levels were highest in drivers involved in fatigue-related crashes (National Transportation Safety Board, 1990, 1995). The NTSB hypothesized that the sleepiest drivers may have (unsuccessfully) resorted to more caffeine in an attempt to remain alert enough to continue driving. Furthermore, despite the evidence in support of using caffeine to counteract drowsy driving, no prior studies have assessed caffeine in the context of driving after a night shift. Caffeine’s wake promoting effects can impact and disrupt subsequent sleep, and thus it is important to understand whether it is an effective countermeasure for workers driving home after a night shift (Drake et al., 2013; LaJambe et al., 2005).
Brief naps are another countermeasure that have been promoted for reducing the impact of sleep loss on alertness and performance. There is strong evidence that a nap can be effective in reducing sleepiness (Bonnet, Gomez, Wirth, & Arand, 1995; De Valck et al., 2003; Gillberg, Kecklund, Axelsson, & Åkerstedt, 1996; J. A. Horne & Reyner, 1996; Macchi, Boulos, Ranney, Simmons, & Campbell, 2002). Sagaspe et al. found that a 30-min nap opportunity improved on-road driving performance in young adults (De Valck & Cluydts, 2001; Philip et al., 2006) but not middle aged adults (Sagaspe et al., 2007), likely due to the fact that the older drivers did not sleep as long or as deeply (Sagaspe et al., 2007). However, not all studies have found a beneficial impact of naps on driving (Lenne, Dwyer, Triggs, Rajaratnam, & Redman, 2004). Naps can produce the paradoxical effect of making the individual more impaired immediately following awakening due to sleep inertia. Laboratory studies have demonstrated that the performance impairments due to sleep inertia can last as long as 2 h after awakening (Achermann et al., 1995; Federal Aviation Administration, 2010; Jewett, Wyatt, et al., 1999; Silva & Duffy, 2008; Webb & Agnew, 1964) and can be worse than 24-h of continuous wakefulness (Wertz et al., 2006). The degree and duration of impairment from sleep inertia depends in part on the stage of sleep the individual awakens from, with deeper sleep producing more severe and long-lasting sleep inertia. For this reason, naps as a countermeasure for sleepiness should be short (15–30 minutes) so as to reduce the likelihood of severe sleep inertia upon awakening, and drivers/operators should wait before operating a vehicle to allow time for sleep inertia to dissipate. Another factor that may impact the practicality of napping for transportation operators is the availability of a suitable environment for taking a nap. Few workplaces have facilities where workers can nap, and while some individuals may be able to nap successfully in a work setting or in a vehicle, there are large individual differences in the ability to nap in such an environment (Philip et al., 2006). In one study of nighttime performance in a driving simulator, breaks alone (without sleep) reduced some time-on-task fatigue effects, but the breaks did not improve driver sleepiness (Phipps-Nelson et al., 2011). Combinations of naps and caffeine have also been tested as a countermeasure for sleepiness (Schweitzer et al., 2006), and the combination of the two has been shown to reduce driver impairments in a simulator (Reyner & Horne, 1997). While sleepy motor vehicle drivers often use strategies such as turning up the radio volume or opening a window to reduce their sleepiness, the only available scientific evidence suggests that those measures are ineffective in ameliorating drowsiness in drivers (Reyner & Horne, 1998; Schwarz et al., 2012).
Testing of countermeasures and combinations of countermeasures for operator sleepiness is an area where much more research should be conducted. At present, much of the advice that is offered to transportation operators and managers is based on small studies, or has evidence both for and against the particular countermeasure. While the best advice is for all operators to obtain sufficient sleep every night, this advice is not practical in every situation, and more research would serve the interests of operators, managers, and regulators alike.
BEST PRACTICES FOR FATIGUE REDUCTION IN TRANSPORTATION
As has been described above, alertness level depends on a number of factors with time-of the day, circadian timing, recent sleep-wake history, hours of service/duration of wake being the major contributing factors to operator sleepiness/alertness levels. Other contributing factors that can affect alertness levels include the nature of the work itself, the operational environment (i.e. the degree to which it promotes alertness or fatigue), medical problems, medications, and medication side effects. The key to preventing fatigue and sleepiness related accidents in transportation operations is to have a comprehensive Fatigue Management Plan in place that addresses all possible sources of sleepiness and fatigue, both in the workplace and outside of it. While other chapters in this volume will address this in greater detail, key features of such systems are shift schedules that consider circadian timing, duration of shifts, and time off between shifts; identifying and addressing non-work-related causes of sleepiness and fatigue; maintaining a culture where workers can report fatigue problems without fear of retribution; using available technology to detect fatigue before it causes a problem; providing resources and education for managers and workers about sleep hygiene and countermeasures for sleepiness and fatigue (see Table 3 and as an example http://www.nafmp.com/en/).
Table 3.
Elements of a Comprehensive Fatigue Management Plan
Identify causes of fatigue, both in the work environment and outside it
|
Evaluate the risk of injuries, errors, and other potential damage caused by fatigue
|
Implement measures to control risks caused by fatigue
|
Review that risk control measures work as planned
|
CHANGING ATTITUDES ABOUT SLEEP LOSS
As outlined above, insufficient or inadequate sleep has profound consequences for transportation safety. Many factors contribute to sleep deficiency, from extended work hours, rotating shift schedules, medications, undiagnosed sleep disorders, and personal choice to limit sleep time, and individuals are often poor judges of how their attention is adversely impacted by insufficient sleep. This is compounded by a culture in which lack of sleep is something many people brag about, where individuals who “need” less sleep are held up as models to emulate, and where individuals who complain of sleep deprivation are considered weak. These attitudes are not only incorrect, they are dangerous, and when they are held by managers and operators in the transportation industry and by individuals who drive automobiles on our highways they contribute to sleep-related accidents. It is important that researchers and regulators work in tandem to change such attitudes so that driving while sleepy is as socially unacceptable as driving while drunk.
PRIORITY GOALS / RESEARCH NEEDS / FUTURE DIRECTIONS
While much is understood about the causes and consequences of sleepiness and fatigue in transportation operations, there remain several knowledge gaps that we believe should be addressed. Some of these relate to understanding risks, while others relate to mitigating those risks. These areas in which more research needs to be conducted include:
Quantifying the prevalance of drowsy driving among different groups (professional vs. non-professional; young, middle-aged, older) and motor vehicle crash risk associated with drowsy driving in those cohorts.
Standardizing the information regarding motor vehicle crashes would be extremely helpful in understanding the number of drowsy driving-related crashes and being able to determine whether interventions reduce the number or severity of such crashes. This includes standards for police investigators to use in defining a crash as related to drowsy driving and national standards for compiling drowsy driving crash data.
Investigations of the impact of specific countermeasures on accident risk reduction in different transportation modes. A variety of common countermeasures, including caffeine, naps, breaks, should be tested for their ability to counteract drowsiness. Also of value will be more extensive investigations evaluating the effectiveness of countermeasures commonly adopted by operators (turning up the radio volume, opening a window) vs. sleep and circadian science-based countermeasures.
Investigations of the impact of OSA screening, testing, and treatment interventions on accident risk reduction in different transportation modes.
National standards for testing and certifying the efficacy of on-board fatigue management systems in non-commercial vehicles.
Cost-benefit investigations of fatigue reduction and management plans in different transportation modes.
Case-control evaluations of accident rate and severity in non-commercial vehicles with on-board fatigue management systems. These studies could inform whether drivers are likely to take greater risks in driving when fatigued if they have such systems available.
Investigations of individual differences in fatigue-related accident risk. Greater understanding of the source(s) of individual differences in fatigue-related accident risk could lead to personalized occupational medicine approaches, such as individually-tailored fatigue management plans that take into account individual differences in sleep need and countermeasure efficacy.
Acknowledgments
JFD is supported by NIH grant NIA-R01-AG044416 and by a grant from the William F. Milton Fund. KMZ is supported by a grant from the Finnish Work Environment Fund. CAC is supported in part by the following grants: NIH grants NHLBI-R01-HL095472, NHLBI-R01-HL94654, NHLBI-U01-HL111478, NIA-P01-AG009975, NIGMS-R01-GM105018; NASA grants NCC9–119, NASA NNX10AF47G and NASA Cooperative Agreement NCC 9-58 from the National Aeronautics and Space Administration; NSBRI-HFP02801 and NSBRI-HFP02802 from the National Space Biomedical Research Institute; FEMA EMW-2010-FP-00521 from the Federal Emergency Management Agency; and GAMS-839 from the National Football League Charities. The authors wish to thank L Preston, J Hong, J Ronda, and T Geller for assistance with manuscript preparation.
CAC has received consulting fees from or served as a paid member of scientific advisory boards for: Bose Corporations; Boston Celtics; Boston Red Sox; Citgo Inc.; Cleveland Browns; Columbia River Bar Pilots; Merck; Novartis; Purdue Pharma LP; Quest Diagnostics, Inc.; Teva Pharmaceuticals Industries Ltd.; Valero Inc.; Vanda Pharmaceuticals, Inc. Dr. Czeisler currently owns an equity interest in Lifetrac, Inc.; Somnus Therapeutics, Inc.; Vanda Pharmaceuticals, Inc. He received royalties from McGraw Hill, Penguin Press/Houghton Mifflin Harcourt, and Philips Respironics, Inc. and has received grants and research support from Cephalon Inc., National Football League Charities, Philips Respironics, ResMed Foundation, San Francisco Bar Pilots and Sysco. He is the incumbent of an endowed professorship provided to Harvard University by Cephalon, Inc. and holds a number of process patents in the field of sleep/circadian rhythms (e.g., photic resetting of the human circadian pacemaker). Since 1985, he has also served as an expert witness on various legal cases related to sleep and/or circadian rhythms, including matters involving Bombardier, Inc.; Delta Airlines; FedEx; Greyhound; Michael Jackson’s mother and children; Purdue Pharma, L.P.; United Parcel Service and the United States of America.
Footnotes
Disclosures. JFD and KMZ have no actual or potential conflicts to disclose.
Contributor Information
Jeanne F. Duffy, Division of Sleep and Circadian Disorders, Departments of Medicine and Neurology, Brigham and Women’s Hospital and Division of Sleep Medicine, Harvard Medical School
Kirsi-Marja Zitting, Division of Sleep and Circadian Disorders, Departments of Medicine and Neurology, Brigham and Women’s Hospital and Division of Sleep Medicine, Harvard Medical School.
Charles A. Czeisler, Division of Sleep and Circadian Disorders, Departments of Medicine and Neurology, Brigham and Women’s Hospital and Division of Sleep Medicine, Harvard Medical School
REFERENCE LIST
- ABC 7News Denver. Woman videotaped falling asleep while driving on I-25. 2007 Oct 18; Retrieved from http://www.thedenverchannel.com/news/14360882/detail.html. [Google Scholar]
- Achermann P, Werth E, Dijk DJ, Borbély AA. Time course of sleep inertia after nighttime and daytime sleep episodes. Archives Italiennes de Biologie. 1995;134:109–119. [PubMed] [Google Scholar]
- Adam M, Rétey JV, Khatami R, Landolt H-P. Age-related changes in the time course of vigilant attention during 40 hours without sleep in men. Sleep. 2006;29(1):55–57. doi: 10.1093/sleep/29.1.55. [DOI] [PubMed] [Google Scholar]
- Aeschbach D, Matthews JR, Postolache TT, Jackson MA, Giesen HA, Wehr TA. Dynamics of the human EEG during prolonged wakefulness: Evidence for frequency-specific circadian and homeostatic influences. Neuroscience Letters. 1997;239(2–3):121–124. doi: 10.1016/s0304-3940(97)00904-x. [DOI] [PubMed] [Google Scholar]
- Aeschbach D, Matthews JR, Postolache TT, Jackson MA, Giesen HA, Wehr TA. Two circadian rhythms in the human electroencephalogram during wakefulness. American Journal of Physiology. 1999;277(6 Pt 2):R1771–R1779. doi: 10.1152/ajpregu.1999.277.6.R1771. [DOI] [PubMed] [Google Scholar]
- Åkerstedt T. Work schedules and sleep. Experientia. 1984;40:417–422. doi: 10.1007/BF01952374. [DOI] [PubMed] [Google Scholar]
- Åkerstedt T, Fredlund P, Gillberg M, Jansson B. A prospective study of fatal occupational accidents-relationship to sleeping difficulties and occupational factors. Journal of Sleep Research. 2002;11:69–71. doi: 10.1046/j.1365-2869.2002.00287.x. [DOI] [PubMed] [Google Scholar]
- Åkerstedt T, Gillberg M. Subjective and objective sleepiness in the active individual. International Journal of Neuroscience. 1990;52(1–2):29–37. doi: 10.3109/00207459008994241. [DOI] [PubMed] [Google Scholar]
- Åkerstedt T, Peters B, Anund A, Kecklund G. Impaired alertness and performance driving home from the night shift: A driving simulator study. Journal of Sleep Research. 2005;14(1):17–20. doi: 10.1111/j.1365-2869.2004.00437.x. [DOI] [PubMed] [Google Scholar]
- Allan JS, Czeisler CA. Persistence of the circadian thyrotropin rhythm under constant conditions and after light-induced shifts of circadian phase. Journal of Clinical Endocrinology & Metabolism. 1994;79:508–512. doi: 10.1210/jcem.79.2.8045970. [DOI] [PubMed] [Google Scholar]
- Allen RP, Picchietti D, Hening WA, Trenkwalder C, Walters AS, Montplaisir J. Restless legs syndrome: Diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Medicine. 2003;4(2):101–119. doi: 10.1016/s1389-9457(03)00010-8. [DOI] [PubMed] [Google Scholar]
- Ancoli-Israel S, Czeisler CA, George CFP, Guilleminault C, Pack AI. Expert panel recommendations. Obstructive sleep apnea and commercial motor vehicle driver safety. Presented to Federal Motor Vehicle Safety Administration. 2008 Jan 1; Retrieved from http://www.fmcsa.dot.gov/sites/fmcsa.dot.gov/files/docs/Sleep-MEP-Panel-Recommendations-508.pdf.
- Anderson C, Chang AM, Sullivan JP, Ronda JM, Czeisler CA. Assessment of drowsiness based on ocular parameters detected by infrared reflectance oculography. Journal of Clinical Sleep Medicine. 2013;9(9):907–920. doi: 10.5664/jcsm.2992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson C, Chang AM, Ronda JM, Czeisler CA. Real-time drowsiness as determined by infrared reflectance oculography is commensurate with gold standard laboratory measures: a validation study. Sleep. 2010;33:A108. (Abstract Supplement) [Google Scholar]
- Anderson C, Dickinson DL. Bargaining and trust: The effects of 36-h total sleep deprivation on socially interactive decisions. Journal of Sleep Research. 2009;19:54–63. doi: 10.1111/j.1365-2869.2009.00767.x. [DOI] [PubMed] [Google Scholar]
- Anderson C, Horne JA. Sleepiness enhances distraction during a monotonous task. Sleep. 2006;29(4):573–576. doi: 10.1093/sleep/29.4.573. [DOI] [PubMed] [Google Scholar]
- Anderson C, Wales AWJ, Horne JA. PVT lapses differ according to eyes open, closed, or looking away. Sleep. 2010;33(2):197–204. doi: 10.1093/sleep/33.2.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson ND. The attentional demands of encoding and retrieval in younger and older adults: 2. Evidence from secondary task reaction time distributions. Psychology and Aging. 1999;14(4):645–655. doi: 10.1037//0882-7974.14.4.645. [DOI] [PubMed] [Google Scholar]
- Aserinsky E, Kleitman N. Two types of ocular motility occurring in sleep. Journal of Applied Physiology. 1955;8(1):1–10. doi: 10.1152/jappl.1955.8.1.1. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders - Fourth Edition (DSM-IV) Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Babkoff H, French J, Whitmore J, Sutherlin R. Single-dose bright light and/or caffeine effect on nocturnal performance. Aviation, Space, and Environmental Medicine. 2002;73(4):341–350. [PubMed] [Google Scholar]
- Babkoff H, Mikulincer M, Caspy T, Kempinski D. The topology of performance curves during 72 hours of sleep loss: A memory and search task. Quarterly Journal of Experimental Psychology. 1988;40A:737–756. doi: 10.1080/14640748808402296. [DOI] [PubMed] [Google Scholar]
- Babkoff H, Zukerman G, Fostick L, Ben Artzi E. Effect of the diurnal rhythm and 24 h of sleep deprivation on dichotic temporal order judgment. Journal of Sleep Research. 2005;14(1):7–15. doi: 10.1111/j.1365-2869.2004.00423.x. [DOI] [PubMed] [Google Scholar]
- Balkin TJ, Badia P. Relationship between sleep inertia and sleepiness: Cumulative effects of four nights of sleep disruption/restriction on performance following abrupt nocturnal awakenings. Biological Psychology. 1988;27:245–258. doi: 10.1016/0301-0511(88)90034-8. [DOI] [PubMed] [Google Scholar]
- Balkin TJ, Horrey WJ, Graeber RC, Czeisler CA, Dinges DF. The challenges and opportunities of technological approaches to fatigue management. Accident Analysis and Prevention. 2011;43(2):565–572. doi: 10.1016/j.aap.2009.12.006. [DOI] [PubMed] [Google Scholar]
- Balkin TJ, Rupp T, Picchioni D, Wesensten NJ. Sleep loss and sleepiness: Current issues. Chest. 2008;134(3):653–660. doi: 10.1378/chest.08-1064. [DOI] [PubMed] [Google Scholar]
- Banks S, Catcheside P, Lack L, Grunstein RR, McEvoy RD. Low levels of alcohol impair driving simulator performance and reduce perception of crash risk in partially sleep deprived subjects. Sleep. 2004;27(6):1063–1067. doi: 10.1093/sleep/27.6.1063. [DOI] [PubMed] [Google Scholar]
- Banks S, Van Dongen H, Dinges D. Response to sleep restriction depends upon pre-existing sleep debt. Sleep. 2007;30:A119. (Abstract Supplement) [Google Scholar]
- Banks S, Van Dongen HP, Maislin G, Dinges DF. Neurobehavioral dynamics following chronic sleep restriction: dose-response effects of one night for recovery. Sleep. 2010;33(8):1013–1026. doi: 10.1093/sleep/33.8.1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barger LK, Ayas NT, Cade BE, Cronin JW, Rosner B, Speizer FE, Czeisler CA. Impact of extended-duration shifts on medical errors, adverse events, and attentional failures. PLoS Medicine. 2006;3(12):e487. doi: 10.1371/journal.pmed.0030487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barger LK, Rajaratnam SMW, Wang W, O’Brien CS, Sullivan JP, Qadri S, Lockley SW, Czeisler CA for the Harvard Work Hours, Health and Safety Group. Common sleep disorders increase risk of motor vehicle crashes and adverse health outcomes in firefighters. Journal of Clinical Sleep Medicine. 2015 doi: 10.5664/jcsm.4534. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barr LC, Yang CYD, Hanowski RJ, Olson R. An assessment of driver drowsiness, distraction, and performance in a naturalistic setting. Washington, DC: U.S. Department of Transportation, Federal Motor Carrier Safety Administration; 2011. (DOT Publication No. FMCSA-RRR-11-010). [Google Scholar]
- Barton J. Choosing to work at night: A moderating influence on individual tolerance to shift work. Journal of Applied Psychology. 1994;79(3):449–454. doi: 10.1037/0021-9010.79.3.449. [DOI] [PubMed] [Google Scholar]
- Belenky G, Wesensten NJ, Thorne DR, Thomas ML, Sing HC, Redmond DP, Balkin TJ. Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: A sleep dose-response study. Journal of Sleep Research. 2003;12:1–12. doi: 10.1046/j.1365-2869.2003.00337.x. [DOI] [PubMed] [Google Scholar]
- Berger M, Varvarigou V, Rielly A, Czeisler CA, Malhotra A, Kales SN. Employer-mandated sleep apnea screening and diagnosis in commercial drivers. Journal of Occupational and Environmental Medicine. 2012;54(8):1017–1025. doi: 10.1097/JOM.0b013e3182572e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjerner B, Holm A, Swensson A. Diurnal variation in mental performance. A study of three-shift workers. British Journal of Industrial Medicine. 1955;12:103–110. doi: 10.1136/oem.12.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bocca ML, Denise P. Total sleep deprivation effect on disengagement of spatial attention as assessed by saccadic eye movements. Clinical Neurophysiology. 2006;117(4):894–899. doi: 10.1016/j.clinph.2006.01.003. [DOI] [PubMed] [Google Scholar]
- Boivin DB, Czeisler CA. Resetting of circadian melatonin and cortisol rhythms in humans by ordinary room light. Neuroreport. 1998;9(5):779–782. doi: 10.1097/00001756-199803300-00002. [DOI] [PubMed] [Google Scholar]
- Boivin DB, Czeisler CA, Dijk DJ, Duffy JF, Folkard S, Minors DS, Waterhouse JM. Complex interaction of the sleep-wake cycle and circadian phase modulates mood in healthy subjects. Archives of General Psychiatry. 1997;54(2):145–152. doi: 10.1001/archpsyc.1997.01830140055010. [DOI] [PubMed] [Google Scholar]
- Bonnet MH. The effect of sleep fragmentation on sleep and performance in younger and older subjects. Neurobiology of Aging. 1989;10:21–25. doi: 10.1016/s0197-4580(89)80006-5. [DOI] [PubMed] [Google Scholar]
- Bonnet MH, Gomez S, Wirth O, Arand DL. The use of caffeine versus prophylactic naps in sustained performance. Sleep. 1995;18(2):97–104. doi: 10.1093/sleep/18.2.97. [DOI] [PubMed] [Google Scholar]
- Bonnet MH, Rosa RR. Sleep and performance in young adults and older normals and insomniacs during acute sleep loss and recovery. Biological Psychology. 1987;25(2):153–172. doi: 10.1016/0301-0511(87)90035-4. [DOI] [PubMed] [Google Scholar]
- Boufous S, Williamson A. Work-related traffic crashes: A record linkage study. Accident Analysis and Prevention. 2006;38(1):14–21. doi: 10.1016/j.aap.2005.06.014. [DOI] [PubMed] [Google Scholar]
- Budnick LD, Lerman SE, Baker TL, Jones H, Czeisler CA. Sleep and alertness in a 12-hour rotating shift work environment. Journal of Occupational Medicine. 1994;36(12):1295–1300. doi: 10.1097/00043764-199412000-00010. [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics. Workers on flexible and shift schedules in May 2004. Washington, DC: U.S. Department of Labor; 2005. (DOL Publication No. USDL-05-1198). [Google Scholar]
- Bureau of Labor Statistics. The employment situation - August 2012. Washington, DC: U.S. Department of Labor; 2012. (DOL Publication No. USDL-12-1796). [Google Scholar]
- Buxton OM, Pavlova M, Reid EW, Wang W, Simonson DC, Adler GK. Sleep restriction for 1 week reduces insulin sensitivity in healthy men. Diabetes. 2010;59(9):2126–2123. doi: 10.2337/db09-0699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse DJ, Monk TH, Reynolds CF, III, Mesiano D, Houck PR, Kupfer DJ. Patterns of sleep episodes in young and elderly adults during a 36-hour constant routine. Sleep. 1993;16(7):632–637. [PubMed] [Google Scholar]
- Cabon P, Coblentz A, Mollard R, Fouillot JP. Human vigilance in railway and long-haul flight operation. Ergonomics. 1993;36(9):1019–1033. doi: 10.1080/00140139308967974. [DOI] [PubMed] [Google Scholar]
- Caffier PP, Erdmann U, Ullsperger P. Experimental evaluation of eye-blink parameters as a drowsiness measure. European Journal of Applied Physiology. 2003;89(3–4):319–325. doi: 10.1007/s00421-003-0807-5. [DOI] [PubMed] [Google Scholar]
- Cain SW, Silva EJ, Chang AM, Ronda JM, Duffy JF. One night of sleep deprivation affects reaction time, but not interference or facilitation in a Stroop task. Brain & Cognition. 2011;76(1):37–42. doi: 10.1016/j.bandc.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cain SW, Silva EJ, Munch MY, Czeisler CA, Duffy JF. Chronic sleep restriction impairs reaction time performance more in young than in older subjects. Sleep. 2010;33:A85. (Abstract Supplement) [Google Scholar]
- Cajochen C, Khalsa SBS, Wyatt JK, Czeisler CA, Dijk DJ. EEG and ocular correlates of circadian melatonin phase and human performance decrements during sleep loss. American Journal of Physiology. 1999;277:R640–R649. doi: 10.1152/ajpregu.1999.277.3.r640. [DOI] [PubMed] [Google Scholar]
- Cajochen C, Wyatt JK, Czeisler CA, Dijk DJ. Separation of circadian and wake duration-dependent modulation of EEG activation during wakefulness. Neuroscience. 2002;114(4):1047–1060. doi: 10.1016/s0306-4522(02)00209-9. [DOI] [PubMed] [Google Scholar]
- Carrier J, Land S, Buysse DJ, Kupfer DJ, Monk TH. The effects of age and gender on sleep EEG power spectral density in the middle years of life (ages 20–60 years old) Psychophysiology. 2001;38(2):232–242. [PubMed] [Google Scholar]
- Cavallero C, Versace F. Stage at awakening, sleep inertia and performance. Sleep Research Online. 2003;5(3):89–97. [Google Scholar]
- Chapman RJ, Johns MW, Crowley KE. In the drowsy state, errors of omission in a visual reaction-time test occur with eyes open or closed. Sleep. 2006;29:A364. (Abstract Supplement) [Google Scholar]
- Chee MW, Choo WC. Functional imaging of working memory after 24 hr of total sleep deprivation. Journal of Neuroscience. 2004;24(19):4560–4567. doi: 10.1523/JNEUROSCI.0007-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chee MW, Chuah LY, Venkatraman V, Chan WY, Philip P, Dinges DF. Functional imaging of working memory following normal sleep and after 24 and 35 h of sleep deprivation: Correlations of fronto-parietal activation with performance. NeuroImage. 2006;31(1):419–428. doi: 10.1016/j.neuroimage.2005.12.001. [DOI] [PubMed] [Google Scholar]
- Chee MW, Tan JC, Zheng H, Parimal S, Weissman DH, Zagorodnov V, Dinges DF. Lapsing during sleep deprivation is associated with distributed changes in brain activation. Journal of Neuroscience. 2008;28(21):5519–5528. doi: 10.1523/JNEUROSCI.0733-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen DA, Wang W, Wyatt JK, Kronauer RE, Dijk DJ, Czeisler CA, Klerman EB. Uncovering residual effects of chronic sleep loss on human performance. Science Translational Medicine. 2010;2(14):14ra13. doi: 10.1126/scitranslmed.3000458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collision Analysis Working Group. 65 main-track train collisions, 1997 through 2002: Review, analysis, findings, and recommendations. Washington, DC: Department of Transportation, Federal Railroad Administration; 2006. [Google Scholar]
- Coren S. Daylight savings time and traffic accidents. New England Journal of Medicine. 1996;334(14):924–924. doi: 10.1056/NEJM199604043341416. [DOI] [PubMed] [Google Scholar]
- Czeisler CA. Human circadian physiology: Internal organization of temperature, sleep-wake, and neuroendocrine rhythms monitored in an environment free of time cues. Palo Alto, CA: Stanford University; 1978. (Unpublished doctoral dissertation) [Google Scholar]
- Czeisler CA. The effect of light on the human circadian pacemaker. In: Waterhouse JM, editor. Circadian Clocks and Their Adjustment. Chichester (Ciba Found. Symp. 183): John Wiley and Sons, Inc.; 1995. pp. 254–302. [DOI] [PubMed] [Google Scholar]
- Czeisler CA. Quantifying consequences of chronic sleep restriction. Sleep. 2003;26(3):247–248. [PubMed] [Google Scholar]
- Czeisler CA. Duration, timing and quality of sleep are each vital for health, performance and safety. Sleep Health. 2015 doi: 10.1016/j.sleh.2014.12.008. (in press) http://dx.doi.org/10.1016/j.sleh.2014.12. [DOI] [PubMed] [Google Scholar]
- Czeisler CA, Buxton OM, Khalsa SBS. The human circadian timing system and sleep-wake regulation. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practices of Sleep Medicine. 4th ed. Philadelphia: WB Saunders Company; 2005. pp. 375–394. [Google Scholar]
- Czeisler CA, Chiasera AJ, Duffy JF. Research on sleep, circadian rhythms and aging: Applications to manned spaceflight. Experimental Gerontology. 1991;26:217–232. doi: 10.1016/0531-5565(91)90014-d. [DOI] [PubMed] [Google Scholar]
- Czeisler CA, Dijk DJ. Human circadian physiology and sleep-wake regulation. In: Takahashi JS, Turek FW, Moore RY, editors. Handbook of Behavioral Neurobiology: Circadian Clocks. New York: Plenum Publishing Co.; 2001. pp. 531–569. [Google Scholar]
- Czeisler CA, Dijk DJ, Duffy JF. Entrained phase of the circadian pacemaker serves to stabilize alertness and performance throughout the habitual waking day. In: Ogilvie RD, Harsh JR, editors. Sleep Onset: Normal and Abnormal Processes. Washington, DC: American Psychological Association; 1994. pp. 89–110. [Google Scholar]
- Czeisler CA, Gooley JJ. Sleep and circadian rhythms in humans. Cold Spring Harbor Symposia on Quantitative Biology. 2007;72:579–597. doi: 10.1101/sqb.2007.72.064. [DOI] [PubMed] [Google Scholar]
- Czeisler CA, Jewett ME. Human circadian physiology: Interaction of the behavioral rest - activity cycle with the output of the endogenous circadian pacemaker. In: Thorpy MJ, editor. Handbook of Sleep Disorders. New York: Marcel Dekker, Inc.; 1990. pp. 117–137. [Google Scholar]
- Czeisler CA, Johnson MP, Duffy JF, Brown EN, Ronda JM, Kronauer RE. Exposure to bright light and darkness to treat physiologic maladaptation to night work. New England Journal of Medicine. 1990;322:1253–1259. doi: 10.1056/NEJM199005033221801. [DOI] [PubMed] [Google Scholar]
- Czeisler CA, Khalsa SBS. The human circadian timing system and sleep-wake regulation. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 3rd ed. Philadelphia: WB Saunders Company; 2000. pp. 353–375. [Google Scholar]
- Czeisler CA, Klerman EB. Circadian and sleep-dependent regulation of hormone release in humans. Recent Progress in Hormone Research. 1999;54:97–132. [PubMed] [Google Scholar]
- Czeisler CA, Kronauer RE, Allan JS, Duffy JF, Jewett ME, Brown EN, Ronda JM. Bright light induction of strong (type 0) resetting of the human circadian pacemaker. Science. 1989;244:1328–1333. doi: 10.1126/science.2734611. [DOI] [PubMed] [Google Scholar]
- Czeisler CA, Weitzman ED, Moore-Ede MC, Zimmerman JC, Knauer RS. Human sleep: Its duration and organization depend on its circadian phase. Science. 1980;210:1264–1267. doi: 10.1126/science.7434029. [DOI] [PubMed] [Google Scholar]
- Czeisler CA, Wright KP., Jr . Influence of light on circadian rhythmicity in humans. In: Turek FW, Zee PC, editors. Neurobiology of Sleep and Circadian Rhythms. New York: Marcel Dekker, Inc.; 1999. pp. 149–180. [Google Scholar]
- Czeisler CA, Zimmerman JC, Ronda JM, Moore-Ede MC, Weitzman ED. Timing of REM sleep is coupled to the circadian rhythm of body temperature in man. Sleep. 1980;2:329–346. [PubMed] [Google Scholar]
- Davis S, Mirick DK, Stevens RG. Night shift work, light at night, and risk of breast cancer. Journal of the National Cancer Institute. 2001;93(20):1557–1562. doi: 10.1093/jnci/93.20.1557. [DOI] [PubMed] [Google Scholar]
- De Bacquer D, Van Risseghem M, Clays E, Kittel F, De Backer G, Braeckman L. Rotating shift work and the metabolic syndrome: A prospective study. International Journal of Epidemiology. 2009;38(3):848–854. doi: 10.1093/ije/dyn360. [DOI] [PubMed] [Google Scholar]
- De Valck E, Cluydts R. Slow-release caffeine as a countermeasure to driver sleepiness induced by partial sleep deprivation. Journal of Sleep Research. 2001;10(3):203–209. doi: 10.1046/j.1365-2869.2001.00260.x. [DOI] [PubMed] [Google Scholar]
- De Valck E, De Groot E, Cluydts R. Effects of slow-release caffeine and a nap on driving simulator performance after partial sleep deprivation. Perceptual and Motor Skills. 2003;96(1):67–78. doi: 10.2466/pms.2003.96.1.67. [DOI] [PubMed] [Google Scholar]
- Dembe AE, Erickson JB, Delbos RG, Banks SM. The impact of overtime and long work hours on occupational injuries and illnesses: New evidence from the United States. Occupational and Environmental Medicine. 2005;62(9):588–597. doi: 10.1136/oem.2004.016667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorpy MJ, Chairman Diagnostic Classification Steering Committee. International classification of sleep disorders: Diagnostic and coding manual. Rochester, MN: American Sleep Disorders Association; 1995. [Google Scholar]
- Dijk DJ, Czeisler CA. Paradoxical timing of the circadian rhythm of sleep propensity serves to consolidate sleep and wakefulness in humans. Neuroscience Letters. 1994;166(1):63–68. doi: 10.1016/0304-3940(94)90841-9. [DOI] [PubMed] [Google Scholar]
- Dijk DJ, Czeisler CA. Contribution of the circadian pacemaker and the sleep homeostat to sleep propensity, sleep structure, electroencephalographic slow waves, and sleep spindle activity in humans. Journal of Neuroscience. 1995;15(5):3526–3538. doi: 10.1523/JNEUROSCI.15-05-03526.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dijk DJ, Duffy JF. Circadian regulation of human sleep and age-related changes in its timing, consolidation and EEG characteristics. Annals of Medicine. 1999;31:130–140. doi: 10.3109/07853899908998789. [DOI] [PubMed] [Google Scholar]
- Dijk DJ, Duffy JF, Czeisler CA. Circadian and sleep/wake dependent aspects of subjective alertness and cognitive performance. Journal of Sleep Research. 1992;1:112–117. doi: 10.1111/j.1365-2869.1992.tb00021.x. [DOI] [PubMed] [Google Scholar]
- Dijk DJ, Duffy JF, Czeisler CA. Contribution of circadian physiology and sleep homeostasis to age-related changes in human sleep. Chronobiology International. 2000;17(3):285–311. doi: 10.1081/cbi-100101049. [DOI] [PubMed] [Google Scholar]
- Dijk DJ, Duffy JF, Czeisler CA. Age-related increase in awakenings: Impaired consolidation of nonREM sleep at all circadian phases. Sleep. 2001;24(5):565–577. doi: 10.1093/sleep/24.5.565. [DOI] [PubMed] [Google Scholar]
- Dijk DJ, Duffy JF, Riel E, Shanahan TL, Czeisler CA. Ageing and the circadian and homeostatic regulation of human sleep during forced desynchrony of rest, melatonin and temperature rhythms. Journal of Physiology (London) 1999;516.2:611–627. doi: 10.1111/j.1469-7793.1999.0611v.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dijk DJ, Lockley SW. Integration of human sleep-wake regulation and circadian rhythmicity. Journal of Applied Physiology. 2002;92:852–862. doi: 10.1152/japplphysiol.00924.2001. [DOI] [PubMed] [Google Scholar]
- Dijk DJ, Neri DF, Wyatt JK, Ronda JM, Riel E, Ritz-De Cecco A, Czeisler CA. Sleep, circadian rhythms, and performance during space shuttle missions. In: Buckey JC Jr, Homick JL, editors. The Neurolab spacelab mission: Neuroscience research in space. Houston, Texas: NASA, Lyndon B. Johnson Space Center; 2002. pp. 211–221. [Google Scholar]
- Dijk DJ, Neri DF, Wyatt JK, Ronda JM, Riel E, Ritz-De Cecco A, Czeisler CA. Sleep, performance, circadian rhythms, and light-dark cycles during two space shuttle flights. American Journal of Physiology. 2001;281:R1647–R1664. doi: 10.1152/ajpregu.2001.281.5.R1647. [DOI] [PubMed] [Google Scholar]
- Dijk DJ, Shanahan TL, Duffy JF, Ronda JM, Czeisler CA. Variation of electroencephalographic activity during non-rapid eye movement and rapid eye movement sleep with phase of circadian melatonin rhythm in humans. Journal of Physiology (London) 1997;505.3:851–858. doi: 10.1111/j.1469-7793.1997.851ba.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinges DF. Sleep debt and scientific evidence. Sleep. 2004;27(6):1050–1052. [PubMed] [Google Scholar]
- Dinges DF. Can habitual sleep duration harbor sleep debt? Sleep. 2005;28(10):1209–1210. doi: 10.1093/sleep/28.10.1209. [DOI] [PubMed] [Google Scholar]
- Dinges DF, Grace R. Tech Brief. PERCLOS: A valid psychophysiological measure of alertness as assessed by psychomotor vigilance. Washington, DC: U.S. Department of Transportation, Federal Highway Administration, Office of Motor Carriers; 1998. (DOT Publication No. FHWA-MCRT-98-006). [Google Scholar]
- Dinges DF, Mallis MM, Maislin G, Powell JW. Evaluation of techniques for ocular measurement as an index of fatigue and the basis for alertness management. Washington, D.C.: U.S. Department of Transportation, National Highway Traffic Safety Administration; 1998. (DOT Publication No. DOT HS 808 762). [Google Scholar]
- Dinges DF, Orne MT, Orne EC. Assessing performance upon abrupt awakening from naps during quasi-continuous operations. Behavior Research Methods Instruments & Computers. 1985;17:37–45. [Google Scholar]
- Dinges DF, Orne MT, Whitehouse WG, Orne EC. Temporal placement of a nap for alertness: Contributions of circadian phase and prior wakefulness. Sleep. 1987;10(4):313–329. [PubMed] [Google Scholar]
- Dinges DF, Pack F, Williams K, Gillen KA, Powell JW, Ott GE, Pack AI. Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4–5 hours per night. Sleep. 1997;20(4):267–277. [PubMed] [Google Scholar]
- Dinges DF, Powell JW. Microcomputer analyses of performance on a portable, simple visual RT task during sustained operations. Behavior Research Methods Instruments & Computers. 1985;17:652–655. [Google Scholar]
- Doran SM, Van Dongen HP, Dinges DF. Sustained attention performance during sleep deprivation: Evidence of state instability. Archives Italiennes de Biologie. 2001;139(3):253–267. [PubMed] [Google Scholar]
- Dorrian J, Rogers NL, Dinges DF. Psychomotor vigilance performance: Neurocognitive assay sensitive to sleep loss. In: Kushida CA, editor. Sleep Deprivation. Clinical Issues, Pharmacology, and Sleep Loss Effects. New York: Marcel Dekker; 2005. pp. 39–70. [Google Scholar]
- Drake C, Roehrs T, Shambroom J, Roth T. Caffeine effects on sleep taken 0, 3, or 6 hours before going to bed. Journal of Clinical Sleep Medicine. 2013;9(11):1195–1200. doi: 10.5664/jcsm.3170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drake CL, Roehrs T, Richardson G, Walsh JK, Roth T. Shift work sleep disorder: Prevalence and consequences beyond that of symptomatic day workers. Sleep. 2004;27(8):1453–1462. doi: 10.1093/sleep/27.8.1453. [DOI] [PubMed] [Google Scholar]
- Drake CL, Roehrs TA, Burduvali E, Bonahoom A, Rosekind M, Roth T. Effects of rapid vs slow accumulation of 8 hours of sleep loss. Psychophysiology. 2001;38:979–987. doi: 10.1111/1469-8986.3860979. [DOI] [PubMed] [Google Scholar]
- Drummond SP, Bischoff-Grethe A, Dinges DF, Ayalon L, Mednick SC, Meloy MJ. The neural basis of the psychomotor vigilance task. Sleep. 2005;28(9):1059–1068. [PubMed] [Google Scholar]
- Drummond SPA, Brown GG. The effects of total sleep deprivation on cerebral responses to cognitive performance. Neuropsychopharmacology. 2001;25(s5):s68–s73. doi: 10.1016/S0893-133X(01)00325-6. [DOI] [PubMed] [Google Scholar]
- Drummond SPA, Brown GG, Gillin JC, Stricker JL, Wong EC, Buxton RB. Altered brain response to verbal learning following sleep deprivation. Nature. 2000;403:655–657. doi: 10.1038/35001068. [DOI] [PubMed] [Google Scholar]
- Drummond SPA, Brown GG, Stricker JL, Buxton RB, Wong EC, Gillin JC. Sleep deprivation-induced reduction in cortical functional response to serial subtraction. Neuroreport. 1999;10:3745–3748. doi: 10.1097/00001756-199912160-00004. [DOI] [PubMed] [Google Scholar]
- Drummond SP, Gillin JC, Brown GG. Increased cerebral response during a divided attention task following sleep deprivation. Journal of Sleep Research. 2001;10(2):85–92. doi: 10.1046/j.1365-2869.2001.00245.x. [DOI] [PubMed] [Google Scholar]
- Drummond SPA, Paulus MP, Tapert SF. Effects of two nights sleep deprivation and two nights recovery sleep on response inhibition. Journal of Sleep Research. 2006;15:261–265. doi: 10.1111/j.1365-2869.2006.00535.x. [DOI] [PubMed] [Google Scholar]
- Duffy JF, Kronauer RE, Czeisler CA. Phase-shifting human circadian rhythms: Influence of sleep timing, social contact and light exposure. Journal of Physiology (London) 1996;495(1):289–297. doi: 10.1113/jphysiol.1996.sp021593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy JF, Willson HJ, Wang W, Czeisler CA. Healthy older adults better tolerate sleep deprivation than young adults. Journal of the American Geriatric Society. 2009;57(7):1245–1251. doi: 10.1111/j.1532-5415.2009.02303.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunwiddie TV, Masino SA. The role and regulation of adenosine in the central nervous system. Annual Review of Neuroscience. 2001;24:31–55. doi: 10.1146/annurev.neuro.24.1.31. [DOI] [PubMed] [Google Scholar]
- Durmer JS, Dinges DF. Neurocognitive consequences of sleep deprivation. Seminars in Neurology. 2005;25(1):117–129. doi: 10.1055/s-2005-867080. [DOI] [PubMed] [Google Scholar]
- El-Hajj Fuleihan G, Klerman EB, Brown EN, Choe Y, Brown EM, Czeisler CA. The parathyroid hormone circadian rhythm is truly endogenous-A general clinical research center study. Journal of Clinical Endocrinology and Metabolism. 1997;82:281–286. doi: 10.1210/jcem.82.1.3683. [DOI] [PubMed] [Google Scholar]
- Federal Aviation Administration. Advisory circular. Basics of aviation fatigue. Washington, DC: U.S. Department of Transportation; 2010. (DOT Publication No. AC 120-100). [Google Scholar]
- Federal Motor Carrier Safety Administration. Report to Congress on the large truck crash causation study. Washington, DC: U.S. Department of Transportation; 2005. (DOT Publication No. MC-R/MC-RAI). [Google Scholar]
- Federal Register. Hours of service of drivers; Driver rest and sleep for safe operations. 85. Vol. 65. Federal Register; 2000. May 2, p. 25540. (Docket No. FMCSA-97-2350; formerly FHWA-97-2350 and MC-96-28] [Google Scholar]
- Findley L, Unverzagt M, Guchu R, Fabrizio M, Buckner J, Suratt P. Vigilance and automobile accidents in patients with sleep apnea or narcolepsy. Chest. 1995;108(3):619–624. doi: 10.1378/chest.108.3.619. [DOI] [PubMed] [Google Scholar]
- Findley LJ, Bonnie RJ. Sleep apnea and auto crashes: What is the doctor to do? Chest. 1988;94(2):225–226. doi: 10.1378/chest.94.2.225. [DOI] [PubMed] [Google Scholar]
- Findley LJ, Fabrizio M, Thommi G, Suratt PM. Severity of sleep apnea and automobile crashes. New England Journal of Medicine. 1989;320(13):868–869. doi: 10.1056/nejm198903303201314. [DOI] [PubMed] [Google Scholar]
- Findley LJ, Levinson MP, Bonnie RJ. Driving performance and automobile accidents in patients with sleep apnea. Clinics in Chest Medicine. 1992;13(3):427–435. [PubMed] [Google Scholar]
- Findley LJ, Unverzagt ME, Suratt PM. Automobile accidents involving patients with obstructive sleep apnea. American Review of Respiratory Disease. 1988;138:337–340. doi: 10.1164/ajrccm/138.2.337. [DOI] [PubMed] [Google Scholar]
- Findley LJ, Weiss JW, Jabour ER. Drivers with untreated sleep apnea: A cause of death and serious injury. Archives of Internal Medicine. 1991;151:1451–1452. [PubMed] [Google Scholar]
- Fischer FM, Morata TC, Latorre MdR, Krieg EF, Fiorini AC, Colacioppo S, Cesar CLG. Effects of environmental and organizational factors on the health of shiftworkers of a printing company. Journal of Occupational and Environmental Medicine. 2001;43:882–889. doi: 10.1097/00043764-200110000-00007. [DOI] [PubMed] [Google Scholar]
- Folkard S. Shift work, safety, and aging. Chronobiology International. 2008;25(2):183–198. doi: 10.1080/07420520802106694. [DOI] [PubMed] [Google Scholar]
- Folkard S, Lombardi DA. Modeling the impact of the components of long work hours on injuries and "accidents". American Journal of Industrial Medicine. 2006 doi: 10.1002/ajim.20307. [DOI] [PubMed] [Google Scholar]
- Folkard S, Tucker P. Shift work, safety and productivity. Occupational Medicine (London) 2003;53(2):95–101. doi: 10.1093/occmed/kqg047. [DOI] [PubMed] [Google Scholar]
- Franzen PL, Siegle GJ, Buysse DJ. Relationships between affect, vigilance, and sleepiness following sleep deprivation. Journal of Sleep Research. 2008;17(1):34–41. doi: 10.1111/j.1365-2869.2008.00635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frey DJ, Badia P, Wright KP., Jr Inter- and intra-individual variability in performance near the circadian nadir during sleep deprivation. Journal of Sleep Research. 2004;13(4):305–315. doi: 10.1111/j.1365-2869.2004.00429.x. [DOI] [PubMed] [Google Scholar]
- Ftouni S, Sletten TL, Howard M, Anderson C, Lenne MG, Lockley SW, Rajaratnam SM. Objective and subjective measures of sleepiness, and their associations with on-road driving events in shift workers. Journal of Sleep Research. 2013;22:58–69. doi: 10.1111/j.1365-2869.2012.01038.x. [DOI] [PubMed] [Google Scholar]
- Fujino Y, Iso H, Tamakoshi A, Inaba Y, Koizumi A, Kubo T, Yoshimura T. A prospective cohort study of shift work and risk of ischemic heart disease in Japanese male workers. American Journal of Epidemiology. 2006;164(2):128–135. doi: 10.1093/aje/kwj185. [DOI] [PubMed] [Google Scholar]
- Garde AH, Hansen AM, Hansen J. Sleep length and quality, sleepiness and urinary melatonin among healthy Danish nurses with shift work during work and leisure time. International Archives of Occupational and Environmental Health. 2009;82(10):1219–1228. doi: 10.1007/s00420-009-0419-4. [DOI] [PubMed] [Google Scholar]
- George CF, Nickerson PW, Hanly PJ, Millar TW, Kryger MH. Sleep apnoea patients have more automobile accidents. Lancet. 1987;2:447. doi: 10.1016/s0140-6736(87)90974-3. [DOI] [PubMed] [Google Scholar]
- George CFP. Sleep. 5: Driving and automobile crashes in patients with obstructive sleep apnoea/hypopnoea syndrome. Thorax. 2004;59(9):804–807. doi: 10.1136/thx.2003.007187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George CFP, Boudreau AC, Smiley A. Simulated driving performance in patients with obstructive sleep apnea. American Journal of Respiratory and Critical Care Medicine. 1996;154(1):175–181. doi: 10.1164/ajrccm.154.1.8680676. [DOI] [PubMed] [Google Scholar]
- Gertler J, DiFiore A. Work schedules and sleep patterns of railroad train and engine service workers. Washington, D.C: U.S. Department of Transportation, Federal Railroad Administration; 2009. (DOT Publication No. DOT/FRA/ORD-09/22). [Google Scholar]
- Gertler J, DiFiore A. Work schedules and sleep patterns of railroad train and engine service employees in passenger operations. Washington, D.C: U.S. Department of Transportation, Federal Railroad Administration; 2011. (DOT Publication No. DOT/FRA/ORD-11/05). [Google Scholar]
- Gillberg M, Kecklund G, Axelsson J, Åkerstedt T. The effects of a short daytime nap after restricted night sleep. Sleep. 1996;19(7):570–575. doi: 10.1093/sleep/19.7.570. [DOI] [PubMed] [Google Scholar]
- Gillooly PB, Smolensky MH, Albright DL, Hsi B, Thorne DR. Circadian variation in human performance evaluated by the Walter Reed performance assessment battery. Chronobiology International. 1990;7(2):143–153. doi: 10.3109/07420529009056966. [DOI] [PubMed] [Google Scholar]
- Goel N, Banks S, Mignot E, Dinges DF. PER3 polymorphism predicts cumulative sleep homeostatic but not neurobehavioral changes to chronic partial sleep deprivation. PLoS ONE. 2009;4(6):e5874. doi: 10.1371/journal.pone.0005874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goel N, Rao H, Durmer JS, Dinges DF. Neurocognitive consequences of sleep deprivation. Seminars in Neurology. 2009;29(4):320–339. doi: 10.1055/s-0029-1237117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gokhale BN. Report on accident to Air India Express Boeing 737–800 aircraft VT-AXV on 22nd May 2010 at Mangalore. New Delhi: Government of India, Ministry of Civil Aviation; 2010. [Google Scholar]
- Gold DR, Rogacz S, Bock N, Tosteson TD, Baum TM, Speizer FE, Czeisler CA. Rotating shift work, sleep, and accidents related to sleepiness in hospital nurses. American Journal of Public Health. 1992;82:1011–1014. doi: 10.2105/ajph.82.7.1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grady CL, Maisog JM, Horwitz B, Ungerleider LG, Mentis MJ, Salerno JA, Haxby JV. Age-related changes in cortical blood flow activation during visual processing of faces and location. Journal of Neuroscience. 1994;14(3 Pt 2):1450–1462. doi: 10.1523/JNEUROSCI.14-03-01450.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grady CL, McIntosh AR, Bookstein F, Horwitz B, Rapoport SI, Haxby JV. Age-related changes in regional cerebral blood flow during working memory for faces. Neuroimage. 1998;8(4):409–425. doi: 10.1006/nimg.1998.0376. [DOI] [PubMed] [Google Scholar]
- Groeger JA, Viola AU, Lo JCY, von Shantz M, Archer SN, Dijk DJ. Early morning executive functioning during sleep deprivation is compromised by a PERIOD3 polymorphism. Sleep. 2008;31(8):1159–1167. [PMC free article] [PubMed] [Google Scholar]
- Grundy A, Sanchez M, Richardson H, Tranmer J, Borugian M, Graham CH, Aronson KJ. Light intensity exposure, sleep duration, physical activity, and biomarkers of melatonin among rotating shift nurses. Chronobiology International. 2009;26(7):1443–1461. doi: 10.3109/07420520903399987. [DOI] [PubMed] [Google Scholar]
- Guilleminault C, Billiard M, Montplaisir J, Dement WC. Altered states of consciousness in disorders of daytime sleepiness. Journal of the Neurological Sciences. 1975;26:377–393. doi: 10.1016/0022-510x(75)90209-9. [DOI] [PubMed] [Google Scholar]
- Guilleminault C, Phillips R, Dement WC. A syndrome of hypersomnia with automatic behavior. Electroencephalography and Clinical Neurophysiology. 1975;38:403–413. doi: 10.1016/0013-4694(75)90264-3. [DOI] [PubMed] [Google Scholar]
- Ha M, Park J. Shiftwork and metabolic risk factors of cardiovascular disease. Journal of Occupational Health. 2005;47(2):89–95. doi: 10.1539/joh.47.89. [DOI] [PubMed] [Google Scholar]
- Haack M, Mullington JM. Sustained sleep restriction reduces emotional and physical well-being. Pain. 2005;119(1–3):56–64. doi: 10.1016/j.pain.2005.09.011. [DOI] [PubMed] [Google Scholar]
- Hack MA, Choi SJ, Vijayapalan P, Davies RJ, Stradling JR. Comparison of the effects of sleep deprivation, alcohol and obstructive sleep apnoea (OSA) on simulated steering performance. Respiratory Medicine. 2001;95(7):594–601. doi: 10.1053/rmed.2001.1109. [DOI] [PubMed] [Google Scholar]
- Hanowski RJ, Wierwille WW, Dingus TA. An on-road study to investigate fatigue in local/short haul trucking. Accident Analysis and Prevention. 2003;35(2):153–160. doi: 10.1016/s0001-4575(01)00098-7. [DOI] [PubMed] [Google Scholar]
- Harris W. Fatigue, circadian rhythm, and truck accidents. In: Mackie R, editor. Vigilance Theory, Operational Performance, and Physiological Correlates. New York: Plenum; 1977. pp. 133–146. [Google Scholar]
- Harrison Y, Horne JA. Sleep deprivation affects speech. Sleep. 1997;20(10):871–877. doi: 10.1093/sleep/20.10.871. [DOI] [PubMed] [Google Scholar]
- Harrison Y, Horne JA. One night of sleep loss impairs innovative thinking and flexible decision making. Organizational Behavior and Human Decision Processes. 1999;78(2):128–145. doi: 10.1006/obhd.1999.2827. [DOI] [PubMed] [Google Scholar]
- Harrison Y, Horne JA. The impact of sleep deprivation on decision making: A review. Journal of Experimental Psychology. 2000;6(3):236–249. doi: 10.1037//1076-898x.6.3.236. [DOI] [PubMed] [Google Scholar]
- He Y, Jones CR, Fujiki N, Xu Y, Guo B, Holder JL, Jr, Fu YH. The transcriptional repressor DEC2 regulates sleep length in mammals. Science. 2009;325(5942):866–870. doi: 10.1126/science.1174443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horne JA. Sleep loss and "divergent" thinking ability. Sleep. 1988;11(6):528–536. doi: 10.1093/sleep/11.6.528. [DOI] [PubMed] [Google Scholar]
- Horne JA, Reyner LA. Sleep related vehicle accidents. British Medical Journal. 1995;310:565–567. doi: 10.1136/bmj.310.6979.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horne JA, Reyner LA. Counteracting driver sleepiness: Effects of napping, caffeine, and placebo. Psychophysiology. 1996;33(3):306–309. doi: 10.1111/j.1469-8986.1996.tb00428.x. [DOI] [PubMed] [Google Scholar]
- Horne JA, Reyner LA, Barrett PR. Driving impairment due to sleepiness is exacerbated by low alcohol intake. Occupational and Environmental Medicine. 2003;60(9):689–692. doi: 10.1136/oem.60.9.689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz TS, Cade BE, Wolfe JM, Czeisler CA. Searching night and day: A dissociation of effects of circadian phase and time awake on visual selective attention and vigilance. Psychological Science. 2003;14(6):549–557. doi: 10.1046/j.0956-7976.2003.psci_1464.x. [DOI] [PubMed] [Google Scholar]
- Howard ME, Desai AV, Grunstein RR, Hukins C, Armstrong JG, Joffe D, Pierce RJ. Sleepiness, sleep-disordered breathing, and accident risk factors in commercial vehicle drivers. American Journal of Respiratory and Critical Care Medicine. 2004;170(9):1014–1021. doi: 10.1164/rccm.200312-1782OC. [DOI] [PubMed] [Google Scholar]
- Howard ME, Gora J, Swann P, Pierce R. Alpha and theta activity and slow eye closure are related to driving performance in professional drivers. Sleep. 2002;25:A148. (Abstract Supplement) [Google Scholar]
- Howard ME, Jackson ML, Kennedy GA, Swann P, Barnes M, Pierce RJ. The interactive effects of extended wakefulness and low-dose alcohol on simulated driving and vigilance. Sleep. 2007;30(10):1334–1340. doi: 10.1093/sleep/30.10.1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung CS, Sarasso S, Ferrarelli F, Riedner B, Ghilardi MF, Cirelli C, Tononi G. Local experience-dependent changes in the wake EEG after prolonged wakefulness. Sleep. 2013;36(1):59–72. doi: 10.5665/sleep.2302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Insurance Institute for Highway Safety. Fatality facts 2005: Teenagers. Retrieved from http://www.iihs.org/iihs/topics/t/teenagers/fatalityfacts/teenagers/2005. [Google Scholar]
- Jewett ME. Models of circadian and homeostatic regulation of human performance and alertness. Cambridge, MA: Harvard University; 1997. (Unpublished doctoral dissertation) [Google Scholar]
- Jewett ME, Borbély AA, Czeisler CA. Biomathematical modeling workshop, May 18–21, 1999. Journal of Biological Rhythms. 1999;14(6):429–630. [Google Scholar]
- Jewett ME, Kronauer RE, Czeisler CA. Light-induced suppression of endogenous circadian amplitude in humans. Nature. 1991;350:59–62. doi: 10.1038/350059a0. [DOI] [PubMed] [Google Scholar]
- Jewett ME, Kronauer RE, Czeisler CA. Phase-amplitude resetting of the human circadian pacemaker via bright light: A further analysis. Journal of Biological Rhythms. 1994;9(3–4):295–314. doi: 10.1177/074873049400900310. [DOI] [PubMed] [Google Scholar]
- Jewett ME, Rimmer DW, Duffy JF, Klerman EB, Kronauer RE, Czeisler CA. Human circadian pacemaker is sensitive to light throughout subjective day without evidence of transients. American Journal of Physiology. Regulatory, Integrative, and Comparative Physiology. 1997;273:R1800–R1809. doi: 10.1152/ajpregu.1997.273.5.r1800. [DOI] [PubMed] [Google Scholar]
- Jewett ME, Wyatt JK, Ritz-De Cecco A, Khalsa SB, Dijk DJ, Czeisler CA. Time course of sleep inertia dissipation in human performance and alertness. Journal of Sleep Research. 1999;8:1–8. doi: 10.1111/j.1365-2869.1999.00128.x. [DOI] [PubMed] [Google Scholar]
- Johns MW, Tucker A, Chapman R, Crowley K, Michael N. Monitoring eye and eyelid movements by infrared reflectance oculography to measure drowsiness in drivers. Somnologie. 2007;11:234–242. [Google Scholar]
- Johnson LC. Sleep deprivation and performance. In: Webb WB, editor. Biological Rhythms, Sleep, and Performance. New York: John Wiley & Sons Ltd; 1982. pp. 111–141. [Google Scholar]
- Johnson MP, Duffy JF, Dijk DJ, Ronda JM, Dyal CM, Czeisler CA. Short-term memory, alertness and performance: A reappraisal of their relationship to body temperature. Journal of Sleep Research. 1992;1:24–29. doi: 10.1111/j.1365-2869.1992.tb00004.x. [DOI] [PubMed] [Google Scholar]
- Kamimori GH, Johnson D, Thorne D, Belenky G. Multiple caffeine doses maintain vigilance during early morning operations. Aviation, Space, and Environmental Medicine. 2005;76(11):1046–1050. [PubMed] [Google Scholar]
- Kawachi I, Colditz GA, Stampfer MJ, Willett WC, Manson JE, Speizer FE, Hennekens CH. Prospective study of shift work and risk of coronary heart disease in women. Circulation. 1995;92(11):3178–3182. doi: 10.1161/01.cir.92.11.3178. [DOI] [PubMed] [Google Scholar]
- Kecklund G, Åkerstedt T. Sleepiness in long distance truck driving: An ambulatory EEG study of night driving. Ergonomics. 1993;36(9):1007–1017. doi: 10.1080/00140139308967973. [DOI] [PubMed] [Google Scholar]
- Kendall AP, Kautz MA, Russo MB, Killgore WD. Effects of sleep deprivation on lateral visual attention. International Journal of Neuroscience. 2006;116(10):1125–1138. doi: 10.1080/00207450500513922. [DOI] [PubMed] [Google Scholar]
- Khalsa SB, Conroy DA, Duffy JF, Czeisler CA, Dijk DJ. Sleep- and circadian-dependent modulation of REM density. Journal of Sleep Research. 2002;11:53–59. doi: 10.1046/j.1365-2869.2002.00276.x. [DOI] [PubMed] [Google Scholar]
- Killgore WD, Balkin TJ, Wesensten NJ. Impaired decision making following 49 h of sleep deprivation. Journal of Sleep Research. 2006;15(1):7–13. doi: 10.1111/j.1365-2869.2006.00487.x. [DOI] [PubMed] [Google Scholar]
- Killgore WD, Killgore DB, Day LM, Li C, Kamimori GH, Balkin TJ. The effects of 53 hours of sleep deprivation on moral judgment. Sleep. 2007;30(3):345–352. doi: 10.1093/sleep/30.3.345. [DOI] [PubMed] [Google Scholar]
- Klauer SG, Dingus TA, Neale VL, Sudweeks JD, Ramsey DJ. The impact of driver inattention on near-crash/crash risk: An analysis using the 100-car naturalistic driving study data. Washington, D.C.: U.S. Department of Transportation, National Highway Traffic Safety Administration; 2006. (DOT Publication No. HS 810 594). [Google Scholar]
- Klein KE, Wegmann H-M, Athanassenas G, Hohlweck H, Kuklinski P. Air operations and circadian performance rhythms. Aviation, Space, and Environmental Medicine. 1976;47:221–230. [PubMed] [Google Scholar]
- Klein T, Martens H, Dijk DJ, Kronauer RE, Seely EW, Czeisler CA. Chronic non-24-hour circadian rhythm sleep disorder in a blind man with a regular 24-hour sleep-wake schedule. Sleep. 1993;16:333–343. doi: 10.1093/sleep/16.4.333. [DOI] [PubMed] [Google Scholar]
- Klerman EB, Dijk DJ. Interindividual variation in sleep duration and its association with sleep debt in young adults. Sleep. 2005;28:1253–1259. doi: 10.1093/sleep/28.10.1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knipling RR, Wang J-S. Research note: Crashes and fatalities related to driver drowsiness/fatigue. Washington D.C.: U.S. Department of Transportation, National Highway Traffic Safety Administration; 1994. [Google Scholar]
- Knipling RR, Wang J-S. Revised estimates of the US drowsy driver crash problem size based on general estimates system case reviews; Presented at the 39th Annual Association for the Advancement of Automotive Medicine Conference; Chicago, IL. 1995. Oct, [Google Scholar]
- Knutsson A, Hallquist J, Reuterwall C, Theorell T, Åkerstedt T. Shiftwork and myocardial infarction: A case-control study. Occupational and Environmental Medicine. 1999;56:46–50. doi: 10.1136/oem.56.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kribbs NB, Pack AI, Dinges DF. Modification of physiological sleep tendency with a prior performance task. Sleep Research. 1994;23:129. [Google Scholar]
- Kubo T, Ozasa K, Mikami K, Wakai K, Fujino Y, Watanabe Y, Tamakoshi A. Prospective cohort study of the risk of prostate cancer among rotating-shift workers: Findings from the Japan collaborative cohort study. American Journal of Epidemiology. 2006;164(6):549–555. doi: 10.1093/aje/kwj232. [DOI] [PubMed] [Google Scholar]
- LaJambe CM, Kamimori GH, Belenky G, Balkin TJ. Caffeine effects on recovery sleep following 27 h total sleep deprivation. Aviation, Space, and Environmental Medicine. 2005;76(2):108–113. [PubMed] [Google Scholar]
- Lamond N, Dawson D, Roach GD. Fatigue assessment in the field: Validation of a hand-held electronic psychomotor vigilance task. Aviation, Space, and Environmental Medicine. 2005;76(5):486–489. [PubMed] [Google Scholar]
- Lamond N, Jay SM, Dorrian J, Ferguson SA, Jones C, Dawson D. The dynamics of neurobehavioural recovery following sleep loss. Journal of Sleep Research. 2007;16(1):33–41. doi: 10.1111/j.1365-2869.2007.00574.x. [DOI] [PubMed] [Google Scholar]
- Langlois PH, Smolensky MH, Hsi BP, Weir FW. Temporal patterns of reported single-vehicle car and truck accidents in Texas, USA during 1980–1983. Chronobiology International. 1985;2:131–140. doi: 10.3109/07420528509055552. [DOI] [PubMed] [Google Scholar]
- Lee JH, Wang W, Silva EJ, Chang AM, Scheuermaier KD, Cain SW, Duffy JF. Neurobehavioral performance in young adults living on a 28-h day for 6 weeks. Sleep. 2009;32(7):905–913. doi: 10.1093/sleep/32.7.905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee ML, Howard ME, Horrey WJ, Liang Y, Anderson C, Shreeve MS, Czeisler CA. Ocular measurement of drowsiness and driving impairment in shift-workers. Sleep. 2012;35(Abstract Supplement):A68. [Google Scholar]
- Lenné MG, Dwyer F, Triggs TJ, Rajaratnam S, Redman JR. The effects of a nap opportunity in quiet and noisy environments on driving performance. Chronobiology International. 2004;21(6):991–1001. doi: 10.1081/cbi-200035956. [DOI] [PubMed] [Google Scholar]
- Lenné MG, Triggs TJ, Redman JR. Time of day variations in driving performance. Accident Analysis and Prevention. 1997;29(4):431–437. doi: 10.1016/s0001-4575(97)00022-5. [DOI] [PubMed] [Google Scholar]
- Leproult R, Colecchia EF, Berardi AM, Stickgold R, Kosslyn SM, Van Cauter E. Individual differences in subjective and objective alertness during sleep deprivation are stable and unrelated. American Journal of Physiology: Regulatory, Integrative, and Comparative Physiology. 2003;284:R280–R290. doi: 10.1152/ajpregu.00197.2002. [DOI] [PubMed] [Google Scholar]
- Lewis PM, Swaim DJ, Rosa RR, Colligan MJ, Booth RJ, Swint MJ. Evaluation of the 12-hour shift schedule at the Fast Flux test facility. (DOE Publication No. NTIS DE87000243) Washington, D.C.: U.S. Department of Energy; 1986. [Google Scholar]
- Lieberman HR, Tharion WJ, Shukitt-Hale B, Speckman KL, Tulley R. Effects of caffeine, sleep loss, and stress on cognitive performance and mood during U.S. Navy SEAL training. Psychopharmacology. 2002;164(3):250–261. doi: 10.1007/s00213-002-1217-9. [DOI] [PubMed] [Google Scholar]
- Lim J, Dinges DF. Sleep deprivation and vigilant attention. Annals of the New York Academy of Sciences. 2008;1129:305–322. doi: 10.1196/annals.1417.002. [DOI] [PubMed] [Google Scholar]
- Lin YC, Hsiao TJ, Chen PC. Shift work aggravates metabolic syndrome development among early-middle-aged males with elevated ALT. World Journal of Gastroenterology. 2009;15(45):5654–5661. doi: 10.3748/wjg.15.5654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lingenfelser T, Kaschel R, Weber A, Zaiser-Kaschel H, Jakober B, Kuper J. Young hospital doctors after night duty: Their task-specific cognitive status and emotional condition. Medical Education. 1994;28:566–572. doi: 10.1111/j.1365-2923.1994.tb02737.x. [DOI] [PubMed] [Google Scholar]
- Lockley SW, Cronin JW, Evans EE, Cade BE, Lee CJ, Landrigan CP, Czeisler CA. Effect of reducing interns' weekly work hours on sleep and attentional failures. New England Journal of Medicine. 2004;351(18):1829–1837. doi: 10.1056/NEJMoa041404. [DOI] [PubMed] [Google Scholar]
- Loomis D. Long work hours and occupational injuries: New evidence on upstream causes. Occupational and Environmental Medicine. 2005;62(9):585. doi: 10.1136/oem.2005.021014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubin A, Hord DJ, Tracy ML, Johnson LC. Effects of exercise, bedrest and napping on performance decrement during 40 hours. Psychophysiology. 1976;13:334–339. doi: 10.1111/j.1469-8986.1976.tb03086.x. [DOI] [PubMed] [Google Scholar]
- Luckhaupt SE. Short sleep duration among workers -- United States, 2010. Morbidity and Mortality Weekly Report (MMWR) 2012;61(16):281–285. [PubMed] [Google Scholar]
- Macchi MM, Boulos Z, Ranney T, Simmons L, Campbell SS. Effects of an afternoon nap on nighttime alertness and performance in long-haul drivers. Accident Analysis and Prevention. 2002;34(6):825–834. doi: 10.1016/s0001-4575(01)00089-6. [DOI] [PubMed] [Google Scholar]
- Makeig S, Jung TP. Tonic, phasic, and transient EEG correlates of auditory awareness in drowsiness. Cognitive Brain Research. 1996;4(1):15–25. doi: 10.1016/0926-6410(95)00042-9. [DOI] [PubMed] [Google Scholar]
- Mallis MM, Maislin G, Powell JW, Konowal NM, Dinges DF. PERCLOS predicts both PVT lapse frequency and cumulative lapse duration. Sleep. 1999;22(Abstract Supplement):A419. [Google Scholar]
- Mander BA, Reid KJ, Baron KG, Tjoa T, Parrish TB, Paller KA, Zee PC. EEG measures index neural and cognitive recovery from sleep deprivation. Journal of Neuroscience. 2010;30(7):2686–2693. doi: 10.1523/JNEUROSCI.4010-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten SV, Stutts JC, Martell CA. Predicting daytime and nighttime drowsy driving crashes based on crash characteristic models; Presented at the 50th Annual Association for the Advancement of Automotive Medicine Conference; Chicago, IL. 2006. Oct, [Google Scholar]
- May CD, Dean DA, II, Jewett ME. A revised definition of core body temperature phase that incorporates both state variables of a limit-cycle human circadian pacemaker model improves model stability at low circadian amplitudes; Presented at the 8th Society for Research on Biological Rhythms Meeting; Jacksonville, FL. 2002. May, [Google Scholar]
- McCarthy ME, Waters WF. Decreased attentional responsivity during sleep deprivation: Orienting response latency, amplitude, and habituation. Sleep. 1997;20(2):115–123. doi: 10.1093/sleep/20.2.115. [DOI] [PubMed] [Google Scholar]
- McKenna BS, Dicjinson DL, Orff HJ, Drummond SP. The effects of one night of sleep deprivation on known-risk and ambiguous-risk decisions. Journal of Sleep Research. 2007;16(3):245–252. doi: 10.1111/j.1365-2869.2007.00591.x. [DOI] [PubMed] [Google Scholar]
- McKenzie B, Rapino M. Commuting in the United States: 2009. American Community Survey Reports. Washington, DC: U.S. Department of Commerce, Economics and Statistics Administration, U.S. Census Bureau; 2011. (Publication No. ACS-15) [Google Scholar]
- McLellan TM, Kamimori GH, Bell DG, Smith IF, Johnson D, Belenky G. Caffeine maintains vigilance and marksmanship in simulated urban operations with sleep deprivation. Aviation, Space, and Environmental Medicine. 2005;76(1):39–45. [PubMed] [Google Scholar]
- Mitler MM, Carskadon MA, Czeisler CA, Dement WC, Dinges DF, Graeber RC. Catastrophes, sleep, and public policy: Consensus report. Sleep. 1988;11:100–109. doi: 10.1093/sleep/11.1.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moller HJ, Kayumov L, Bulmash EL, Nhan J, Shapiro CM. Simulator performance, microsleep episodes, and subjective sleepiness: Normative data using convergent methodologies to assess driver drowsiness. Journal of Psychosomatic Research. 2006;61(3):335–342. doi: 10.1016/j.jpsychores.2006.04.007. [DOI] [PubMed] [Google Scholar]
- Monk TH. Traffic accident increases as a possible indicant of desynchronosis. Chronobiologia. 1980;7:527–529. [PubMed] [Google Scholar]
- Monk TH. Shift Work. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 3rd ed. Philadelphia: W.B. Saunders Company; 2000. pp. 600–605. [Google Scholar]
- Monk TH, Carrier J. Speed of mental processing in the middle of the night. Sleep. 1997;20(6):399–401. doi: 10.1093/sleep/20.6.399. [DOI] [PubMed] [Google Scholar]
- Münch M, Silva EJ, Ronda JM, Czeisler CA, Duffy JF. EEG sleep spectra in older adults across all circadian phases during NREM sleep. Sleep. 2010;33(3):389–401. doi: 10.1093/sleep/33.3.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naitoh P. Sleep deprivation in human subjects: A reappraisal. Waking and Sleeping. 1976;1:53–60. [Google Scholar]
- National Center on Sleep Disorders Research. National Institutes of Health Sleep Disorders Research Plan. Bethesda, MD: U.S. National Institutes of Health; 2011. [Google Scholar]
- National Heart, Lung and Blood Institute. Who is at risk for Restless Legs Syndrome? 2010 Nov 1; Retrieved from http://www.nhlbi.nih.gov/health/health-topics/topics/rls/atrisk.
- National Highway Traffic Safety Administration. Traffic safety facts 1999: A compilation of motor vehicle crash data from the fatality analysis reporting system and the general estimates system. Washington, D.C.: U.S. Department of Transportation; 2000. (DOT Publication No. DOT HS 809 100) [Google Scholar]
- National Highway Traffic Safety Administration. Traffic safety facts 2004: A compilation of motor vehicle crash data from the fatality analysis reporting system and the general estimates system. Washington, D.C.: U.S. Department of Transportation; 2005a. (DOT Publication No. DOT HS 809 919) [Google Scholar]
- National Highway Traffic Safety Administration. Traffic safety facts. 2004 Data.. Young Drivers. Washington, D.C.: U.S. Department of Transportation; 2005b. (DOT Publication No. DOT HS 809 918) [Google Scholar]
- National Highway Traffic Safety Administration. National motor vehicle crash causation survey: Report to Congress. Washington, D.C.: U.S. Department of Transportation; 2008. (DOT Publication No. DOT HS 811 059) [Google Scholar]
- National Highway Traffic Safety Administration. Traffic safey facts. Crash Stats. Drowsy Driving. Washington, D.C.: U.S. Department of Transportation; 2011. (DOT Publication No. DOT HS 811 449) [Google Scholar]
- National Sleep Foundation. Executive summary of the 1999 "Sleep in America" poll. Washington, D.C.: National Sleep Foundation; 1999. [Google Scholar]
- National Sleep Foundation. Executive summary of the 2000 Omnibus "Sleep in America" poll. Washington, D.C.: National Sleep Foundation; 2000. [Google Scholar]
- National Sleep Foundation. Executive summary of the 2002 "Sleep in America" poll. Washington, DC: National Sleep Foundation; 2002. [Google Scholar]
- National Sleep Foundation. Executive summary of the 2003 "Sleep in America" poll. Washington, D.C.: National Sleep Foundation; 2003. [Google Scholar]
- National Sleep Foundation. Executive summary of the 2005 "Sleep in America" poll. Washington D.C.: National Sleep Foundation; 2005. [Google Scholar]
- National Sleep Foundation. 2006 "Sleep in America" poll. Washington, D.C.: National Sleep Foundation; 2006. Summary of Findings. [Google Scholar]
- National Sleep Foundation. 2008 "Sleep in America" poll: Summary of findings. Washington, D.C.: National Sleep Foundation; 2008. [Google Scholar]
- National Sleep Foundation. 2009 "Sleep in America" poll: Summary of findings. Washington, D.C.: National Sleep Foundation; 2009. [Google Scholar]
- National Sleep Foundation. Executive Summary of the 2012 "Sleep in America" poll: Transportation Workers' Sleep. Washington, D.C.: National Sleep Foundation; 2012. [Google Scholar]
- National Transportation Safety Board. Safety study: Fatigue, alcohol, other drugs, and medical factors in fatal-to-the-driver heavy truck crashes. Washington, D.C.: U.S. National Transportation Safety Board; 1990. (NTSB Publication No. NTSB/SS-90/01) [Google Scholar]
- National Transportation Safety Board. Factors that affect fatigue in heavy truck accidents. Washington, D.C.: U.S. National Transportation Safety Board; 1995. NTSB Publication No. NTSB/SS-95/01. [Google Scholar]
- National Transportation Safety Board. Railroad accident report. Collision of two Canadian National/Illinois Central Railway trains near Clarkston, Michigan, November 15, 2001. Washington, DC: U.S. National Transportation Safety Board; 2002. (NTSB Publication No. NTSB/RAR-02/04) [Google Scholar]
- National Transportation Safety Board. Highway accident report. Truck-tractor semitrailer median crossover collision with 15-passenger vehicle. Munfordville, Kentucky, May 26, 2010. Washington, DC: U.S. National Transportation Safety Board; 2011a. (NTSB Publication No. NTSB/HAR-11/02) [Google Scholar]
- National Transportation Safety Board. Marine accident report. Collision of tankship Eagle Otome with cargo vessel Gull Arrow and subsequent collision with the Dixie Vengeance tow. Sabine-Nieches Canal, Port Arthur, Texas, January 23, 2010. Washington, DC: U.S. National Transportation Safety Board; 2011b. (NTSB Publication No. NTSB/MAR-11/04) [Google Scholar]
- National Transportation Safety Board. Railroad accident brief. Accident No. DCA-09-MR-004. Massachusetts Bay Transportation Authority (MBTA), Boston, MA, May 8, 2009. Washington, DC: U.S. National Transportation Safety Board; 2011c. (NTSB Publication No. NTSB/RAB-11/06) [Google Scholar]
- Novak RD, Auvil-Novak SE. Focus group evaluation of night nurse shiftwork difficulties and coping strategies. Chronobiology International. 1996;13(6):457–463. doi: 10.3109/07420529609020916. [DOI] [PubMed] [Google Scholar]
- Pack AI, Pack AM, Rodgman E, Cucchiara A, Dinges DF, Schwab CW. Characteristics of crashes attributed to the driver having fallen asleep. Accident Analysis and Prevention. 1995;27(6):769–775. doi: 10.1016/0001-4575(95)00034-8. [DOI] [PubMed] [Google Scholar]
- Pavlova MK, Duffy JF, Shea SA. Polysomnographic respiratory abnormalities in asymptomatic individuals. Sleep. 2008;31(2):241–248. doi: 10.1093/sleep/31.2.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellegrino R, Kavakli IH, Goel N, Cardinale CJ, Dinges DF, Kuna ST, Pack AI. A novel BHLHE41 variant is associated with short sleep and resistance to sleep deprivation in humans. Sleep. 2014;37(8):1327–1336. doi: 10.5665/sleep.3924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penetar D, McCann U, Thorne D, Kamimori G, Galinski C, Sing H, Belenky G. Caffeine reversal of sleep deprivation effects on alertness and mood. Psychopharmacology. 1993;112:359–365. doi: 10.1007/BF02244933. [DOI] [PubMed] [Google Scholar]
- Philip P, Akerstedt T. Transport and industrial safety, how are they affected by sleepiness and sleep restriction? Sleep Medicine Reviews. 2006;10(5):347–356. doi: 10.1016/j.smrv.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Philip P, Taillard J, Moore N, Delord S, Valtat C, Sagaspe P, Bioulac B. The effects of coffee and napping on nighttime highway driving: A randomized trial. Annals of Internal Medicine. 2006;144(11):785–791. doi: 10.7326/0003-4819-144-11-200606060-00004. [DOI] [PubMed] [Google Scholar]
- Philip P, Taillard J, Quera-Salva MA, Bioulac B, Akerstedt T. Simple reaction time, duration of driving and sleep deprivation in young versus old automobile drivers. Journal of Sleep Research. 1999;8(1):9–14. doi: 10.1046/j.1365-2869.1999.00127.x. [DOI] [PubMed] [Google Scholar]
- Philip P, Vervialle F, Le Breton P, Taillard J, Horne J. Fatigue, alcohol and serious road crashed in France: Factorial study of national data. British Medical Journal. 2001;322:829–830. doi: 10.1136/bmj.322.7290.829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phipps-Nelson J, Redman JR, Rajaratnam SM. Temporal profile of prolonged, night-time driving performance: Breaks from driving temporarily reduce time-on-task fatigue but not sleepiness. Journal of Sleep Research. 2011;20(3):404–415. doi: 10.1111/j.1365-2869.2010.00900.x. [DOI] [PubMed] [Google Scholar]
- Committee on Sleep Medicine Research. Board on Health Sciences Policy. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington, D.C.: Institute of Medicine of the National Academies; The National Academies Press; 2006. [PubMed] [Google Scholar]
- Porkka-Heiskanen T, Strecker RE, Thakkar M, Bjorkum AA, Greene RW, McCarley RW. Adenosine: A mediator of the sleep-inducing effects of prolonged wakefulness. Science. 1997;276:1265–1268. doi: 10.1126/science.276.5316.1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell NB, Riley RW, Schechtman KB, Blumen MB, Dinges DF, Guilleminault C. A comparative model: Reaction time performance in sleep-disordered breathing versus alcohol-impaired controls. Laryngoscope. 1999;109:1648–1654. doi: 10.1097/00005537-199910000-00019. [DOI] [PubMed] [Google Scholar]
- Rajaratnam SM, Barger LK, Lockley SW, Shea SA, Wang W, Landrigan CP, Czeisler CA. Sleep disorders, health, and safety in police officers. Journal of the American Medical Association. 2011;306(23):2567–2578. doi: 10.1001/jama.2011.1851. [DOI] [PubMed] [Google Scholar]
- Ratcliff R, Van Dongen HPA. Sleep deprivation affects multiple distinct cognitive processes. Psychonomic Bulletin & Review. 2009;16(4):742–751. doi: 10.3758/PBR.16.4.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reimer B, D'Ambrosio LA, Coughlin JF. Secondary analysis of time of day on simulated driving performance. Journal of Safety Research. 2007;38(5):563–570. doi: 10.1016/j.jsr.2007.07.002. [DOI] [PubMed] [Google Scholar]
- Retey JV, Adam M, Gottselig JM, Khatami R, Durr R, Achermann P, Landolt HP. Adenosinergic mechanisms contribute to individual differences in sleep deprivation-induced changes in neurobehavioral function and brain rhythmic activity. Journal of Neuroscience. 2006;26(41):10472–10479. doi: 10.1523/JNEUROSCI.1538-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reyner LA, Horne JA. Suppression of sleepiness in drivers: Combination of caffeine with a short nap. Psychophysiology. 1997;34(6):721–725. doi: 10.1111/j.1469-8986.1997.tb02148.x. [DOI] [PubMed] [Google Scholar]
- Reyner LA, Horne JA. Evaluation of "in-car" countermeasures to sleepiness: Cold air and radio. Sleep. 1998;21(1):46–50. [PubMed] [Google Scholar]
- Roehrs T, Beare D, Zorick F, Roth T. Sleepiness and ethanol effects on simulated driving. Alcoholism - Clinical and Experimental Research. 1994;18(1):154–158. doi: 10.1111/j.1530-0277.1994.tb00896.x. [DOI] [PubMed] [Google Scholar]
- Roehrs T, Timms V, Zwyghuizen-Doorenbos A, Roth T. Sleep extension in sleepy and alert normals. Sleep. 1989;12(5):449–457. doi: 10.1093/sleep/12.5.449. [DOI] [PubMed] [Google Scholar]
- Rogé J, Pébayle T, El Hannachi S, Muzet A. Effect of sleep deprivation and driving duration on the useful visual field in younger and older subjects during simulator driving. Vision Research. 2003;43:1465–1472. doi: 10.1016/s0042-6989(03)00143-3. [DOI] [PubMed] [Google Scholar]
- Rogers AE, Hwang WT, Scott LD, Aiken LH, Dinges DF. The working hours of hospital staff nurses and patient safety. Health Affairs. 2004;23(4):202–212. doi: 10.1377/hlthaff.23.4.202. [DOI] [PubMed] [Google Scholar]
- Rosa RR, Bonnet MH. Performance and alertness on 8 h and 12 h rotating shifts at a natural gas utility. Ergonomics. 1995;36(10):1177–1193. doi: 10.1080/00140139308967987. [DOI] [PubMed] [Google Scholar]
- Rosa RR, Bonnet MH, Bootzin RR, Eastman CI, Monk T, Penn PE, Walsh JK. Intervention factors for promoting adjustment to nightwork and shiftwork. Occupational Medicine. 1990;5(2):391–415. [PubMed] [Google Scholar]
- Rosa RR, Colligan MJ. Application of a portable test battery in the assessment of fatigue in laboratory and worksite studies of 12-hour shifts. Work, Environment, Health. 1995;18(2):113–115. [PubMed] [Google Scholar]
- Royal D. National survey of distracted and drowsy driving attitudes and behavior: 2002. Washington, D.C.: U.S. Department of Transportation, National Highway Traffic Safety Administration; 2003. (DOT Publication No. DOT HS 809 566). [Google Scholar]
- Rupp TL, Wesensten NJ, Balkin TJ. Sleep history affects task acquisition during subsequent sleep restriction and recovery. Journal of Sleep Research. 2010;19(2):289–297. doi: 10.1111/j.1365-2869.2009.00800.x. [DOI] [PubMed] [Google Scholar]
- Rupp TL, Wesensten NJ, Newman R, Balkin TJ. PER3 and ADORA2A polymorphisms impact neurobehavioral performance during sleep restriction. Journal of Sleep Research. 2013;22(2):160–165. doi: 10.1111/j.1365-2869.2012.01062.x. [DOI] [PubMed] [Google Scholar]
- Russo MB, Kendall AP, Johnson DE, Sing HC, Thorne DR, Escolas SM, Redmond DP. Visual perception, psychomotor performance, and complex motor performance during an overnight air refueling simulated flight. Aviation, Space, and Environmental Medicine. 2005;76(7 Suppl):C92–C103. [PubMed] [Google Scholar]
- Sagaspe P, Taillard J, Chaumet G, Moore N, Bioulac B, Philip P. Aging and nocturnal driving: Better with coffee or a nap? A randomized study. Sleep. 2007;30(12):1808–1813. doi: 10.1093/sleep/30.12.1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santamaria J, Chiappa KH. The EEG of drowsiness in normal adults. Journal of Clinical Neurophysiology. 1987;4:327–382. doi: 10.1097/00004691-198710000-00002. [DOI] [PubMed] [Google Scholar]
- Santhi N, Horowitz TS, Duffy JF, Czeisler CA. Acute sleep deprivation and circadian misalignment associated with transition onto the first night of work impairs visual selective attention. PLoS ONE. 2007;2(11):e1233. doi: 10.1371/journal.pone.0001233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saper CB, Fuller PM, Pedersen NP, Lu J, Scammell TE. Sleep state switching. Neuron. 2010;68(6):1023–1042. doi: 10.1016/j.neuron.2010.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saper CB, Scammell TE, Lu J. Hypothalamic regulation of sleep and circadian rhythms. Nature. 2005;437(7063):1257–1263. doi: 10.1038/nature04284. [DOI] [PubMed] [Google Scholar]
- Sassani A, Findley LJ, Kryger M, Goldlust E, George C, Davidson TM. Reducing motor-vehicle collisions, costs, and fatalities by treating obstructive sleep apnea syndrome. Sleep. 2004;27(3):453–458. doi: 10.1093/sleep/27.3.453. [DOI] [PubMed] [Google Scholar]
- Scheer FA, Hilton MF, Mantzoros CS, Shea SA. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proceedings of the National Academy of Sciences of the United States of America. 2009;106(11):4453–4458. doi: 10.1073/pnas.0808180106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheer FA, Shea TJ, Hilton MF, Shea SA. An endogenous circadian rhythm in sleep inertia results in greatest cognitive impairment upon awakening during the biological night. Journal of Biological Rhythms. 2008;23(4):353–361. doi: 10.1177/0748730408318081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schernhammer ES, Laden F, Speizer FE, Willett WC, Hunter DJ, Kawachi I, Colditz GA. Rotating night shifts and risk of breast cancer in women participating in the nurses' health study. Journal of the National Cancer Institute. 2001;93(20):1563–1568. doi: 10.1093/jnci/93.20.1563. [DOI] [PubMed] [Google Scholar]
- Schwartz WJ. Further evaluation of the tetrodotoxin-resistant circadian pacemaker in the suprachiasmatic nuclei. Journal of Biological Rhythms. 1991;6(2):149–158. doi: 10.1177/074873049100600205. [DOI] [PubMed] [Google Scholar]
- Schwarz JF, Ingre M, Fors C, Anund A, Kecklund G, Taillard J, Akerstedt T. In-car countermeasures open window and music revisited on the real road: Popular but hardly effective against driver sleepiness. Journal of Sleep Research. 2012;21(5):595–599. doi: 10.1111/j.1365-2869.2012.01009.x. [DOI] [PubMed] [Google Scholar]
- Schweitzer PK, Randazzo AC, Stone K, Erman M, Walsh JK. Laboratory and field studies of naps and caffeine as practical countermeasures for sleep-wake problems associated with night work. Sleep. 2006;29(1):39–50. doi: 10.1093/sleep/29.1.39. [DOI] [PubMed] [Google Scholar]
- Shanahan TL, Czeisler CA. Light exposure induces equivalent phase shifts of the endogenous circadian rhythms of circulating plasma melatonin and core body temperature in men. Journal of Clinical Endocrinology and Metabolism. 1991;73:227–235. doi: 10.1210/jcem-73-2-227. [DOI] [PubMed] [Google Scholar]
- Shanahan TL, Kronauer RE, Duffy JF, Williams GH, Czeisler CA. Melatonin rhythm observed throughout a three-cycle bright-light stimulus designed to reset the human circadian pacemaker. Journal of Biological Rhythms. 1999;14:237–253. doi: 10.1177/074873099129000560. [DOI] [PubMed] [Google Scholar]
- Shanahan TL, Zeitzer JM, Czeisler CA. Resetting the melatonin rhythm with light in humans. Journal of Biological Rhythms. 1997;12(6):556–567. doi: 10.1177/074873049701200610. [DOI] [PubMed] [Google Scholar]
- Sharwood LN, Elkington J, Meuleners L, Ivers R, Boufous S, Stevenson M. Use of caffeinated substances and risk of crashes in long distance drivers of commercial vehicles: Case-control study. British Medical Journal. 2013;346:f1140. doi: 10.1136/bmj.f1140. [DOI] [PubMed] [Google Scholar]
- Shin D, Sakai H, Uchiyama Y. Slow eye movement detection can prevent sleep-related accidents effectively in a simulated driving task. Journal of Sleep Research. 2011;20(3):416–424. doi: 10.1111/j.1365-2869.2010.00891.x. [DOI] [PubMed] [Google Scholar]
- Silva EJ, Cain SW, Munch MY, Wang W, Ronda JM, Czeisler CA, Duffy JF. Recovery of neurobehavioral function in a group of young adults following chronic sleep restriction. Sleep. 2010;33:A103–A104. (Abstract Supplement) [Google Scholar]
- Silva EJ, Duffy JF. Sleep inertia varies with circadian phase and sleep stage in older adults. Behavioral Neuroscience. 2008;122(4):928–935. doi: 10.1037/0735-7044.122.4.928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva EJ, Wang W, Ronda JM, Wyatt JK, Duffy JF. Circadian and wake-dependent influences on subjective sleepiness, cognitive throughput, and reaction time performance in older and young adults. Sleep. 2010;33(4):481–490. doi: 10.1093/sleep/33.4.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith L, Folkard S, Poole CJM. Increased injuries on night shift. Lancet. 1994;344:1137–1139. doi: 10.1016/s0140-6736(94)90636-x. [DOI] [PubMed] [Google Scholar]
- Smith MJ, Colligan MJ, Tasto DL. Health and safety consequences of shift work in the food processing industry. Ergonomics. 1982;25:133–144. doi: 10.1080/00140138208924933. [DOI] [PubMed] [Google Scholar]
- Stenuit P, Kerkhofs M. Effects of sleep restriction on cognition in women. Biological Psychology. 2008;77(1):81–88. doi: 10.1016/j.biopsycho.2007.09.011. [DOI] [PubMed] [Google Scholar]
- Strohl KP, Blatt J, Council F, Georges K, Kiley J, Kurrus R, Willis D. Drowsy driving and automobile crashes: Reports and recommendations. Washington, DC: U.S. Department of Transportation, National Highway Traffic Safety Administration; and U.S. Department of Health and Human Services, National Heart, Lung, and Blood Institute; 1998. Publication No. DOT HS 808 707). [Google Scholar]
- Talmage JB, Hudson TB, Hegmann KT, Thiese MS. Consensus criteria for screening commercial drivers for obstructive sleep apnea: evidence of efficacy. Journal of Occupational and Environmental Medicine. 2008;50:324–329. doi: 10.1097/JOM.0b013e3181617ab8. [DOI] [PubMed] [Google Scholar]
- Taub JM, Berger RJ. Performance and mood following variations in the length and timing of sleep. Psychophysiology. 1973;10:559–570. doi: 10.1111/j.1469-8986.1973.tb00805.x. [DOI] [PubMed] [Google Scholar]
- Tefft BC. Prevalence of motor vehicle crashes involving drowsy drivers, United States, 1999–2008. Accident Analysis and Prevention. 2012;45:180–186. doi: 10.1016/j.aap.2011.05.028. [DOI] [PubMed] [Google Scholar]
- Tefft BC. Prevalence of Motor Vehicle Crashes Involving Drowsy Drivers, United States, 2009–2013. Washington DC: AAA Foundation for Traffic Safety; 2014. [DOI] [PubMed] [Google Scholar]
- Tepas DI, Mahan RP. Work shift preference, morningness-eveningness, and sleep. Sleep Research. 1986;15:287. [Google Scholar]
- Teran-Santos J, Jimenez-Gomez A, Cordero-Guevara J the Cooperative Group Burgos-Santander. The association between sleep apnea and the risk of traffic accidents. New England Journal of Medicine. 1999;340(11):847–851. doi: 10.1056/NEJM199903183401104. [DOI] [PubMed] [Google Scholar]
- Thomas GR, Raslear TG, Kuehn GI. The effects of work schedule on train-handling performance and sleep of locomotive engineers: A simulator study. Washington, D.C.: U.S. Department of Transportation, Federal Railroad Administration; 1997. (DOT Publication No. DOT/FRA/ORD-97-09). [Google Scholar]
- Thomas H, Schwartz E, Whitehead DC. Eight versus 12-hour shifts: Implications for emergency physicians. Emergency Medicine. 1994;23(5):1096–1100. doi: 10.1016/s0196-0644(94)70109-1. [DOI] [PubMed] [Google Scholar]
- Thomas M, Sing H, Belenky G, Holcomb H, Mayberg H, Dannals R, Redmond D. Neural basis of alertness and cognitive performance impairments during sleepiness. I. Effects of 24 h of sleep deprivation on waking human regional brain activity. Journal of Sleep Research. 2000;9:335–352. doi: 10.1046/j.1365-2869.2000.00225.x. [DOI] [PubMed] [Google Scholar]
- Thorpy MJ, Billiard M, editors. Sleepiness: causes, consequences and treatment. Cambridge: Cambridge University Press; 2011. [Google Scholar]
- Torsvall L, Åkerstedt T. Sleepiness on the job: Continuously measured EEG changes in train drivers. Electroencephalography and clinical Neurophysiology. 1987;66:502–511. doi: 10.1016/0013-4694(87)90096-4. [DOI] [PubMed] [Google Scholar]
- Torsvall L, Åkerstedt T, Gillberg M. Age, sleep and irregular workhours: A field study with electroencephalographic recordings, catecholamine excretion and self-ratings. Scandinavian Journal of Work, Environment and Health. 1981;7:196–203. doi: 10.5271/sjweh.3112. [DOI] [PubMed] [Google Scholar]
- Transportation Safety Board of Canada. Aviation Investigation Report: Pitch excursion, Air Canada Boeing 767–333, C-GHLQ, North Atlantic Ocean, 55°00'N 029°00'W, 14 January 2011. Ottawa, O.N.: Transportation Safety Board of Canada; 2012. (TSB Publication No. A11F0012) [Google Scholar]
- Turner TH, Drummond SPA, Salamat JS, Brown GG. Effects of 42 hr of total sleep deprivation on component processes of verbal working memory. Neuropsychology. 2007;21(6):787–795. doi: 10.1037/0894-4105.21.6.787. [DOI] [PubMed] [Google Scholar]
- Vakulin A, Baulk SD, Catcheside PG, Anderson R, van den Heuvel CJ, Banks S, McEvoy RD. Effects of moderate sleep deprivation and low-dose alcohol on driving simulator performance and perception in young men. Sleep. 2007;30(10):1327–1333. doi: 10.1093/sleep/30.10.1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Cauter E, Buxton OM. Circadian modulation of endocrine secretion. In: Takahashi JS, Turek FW, Moore RY, editors. Handbook of Behavioral Neurobiology: Volume 12 Circadian Clocks. New York: Kluwer Academic/Plenum Publishing; 2001. pp. 685–714. [Google Scholar]
- Van Dongen HP, Doran SM, Dinges DF. Performance during sleep deprivation: Evidence for state instability and trait vulnerability. Sleep. 2000;23:A245–A246. (Abstract Supplement) [PubMed] [Google Scholar]
- Van Dongen HPA, Baynard MD, Maislin G, Dinges DF. Systematic interindividual differences in neurobehavioral impairment from sleep loss: evidence of trait-like differential vulnerability. Sleep. 2004;27:423–433. [PubMed] [Google Scholar]
- Van Dongen HPA, Dinges DF. Sleep debt and cumulative excess wakefulness. Sleep. 2003;26(3):249. [Google Scholar]
- Van Dongen HPA, Dinges DF. Circadian Rhythms in Sleepiness, Alertness, and Performance. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practices of Sleep Medicine. 4th ed. Philadelphia: W.B. Saunders; 2005. pp. 435–443. [Google Scholar]
- Van Dongen HPA, Maislin G, Dinges DF. Dealing with inter-individual differences in the temporal dynamics of fatigue and performance: importance and techniques. Aviation, Space, and Environmental Medicine. 2004;75(3 Suppl):A147–A154. [PubMed] [Google Scholar]
- Van Dongen HPA, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: Dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26(2):117–126. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- Van Dongen HPA, Olofsen E, Dinges DF, Maislin G. Mixed-model regression analysis and dealing with interindividual differences. Methods in Enzymology. 2004;384:139–171. doi: 10.1016/S0076-6879(04)84010-2. [DOI] [PubMed] [Google Scholar]
- Varughese J, Allen RP. Fatal accidents following changes in daylight savings time: The American experience. Sleep Medicine. 2001;2:31–36. doi: 10.1016/s1389-9457(00)00032-0. [DOI] [PubMed] [Google Scholar]
- Vener KJ, Szabo S, Moore JG. The effect of shift work on gastrointestinal (GI) function: A review. Chronobiologia. 1989;16:421–439. [PubMed] [Google Scholar]
- Venkatraman V, Chuah YM, Huettel SA, Chee MW. Sleep deprivation elevates expectation of gains and attenuates response to losses following risky decisions. Sleep. 2007;30(5):603–609. doi: 10.1093/sleep/30.5.603. [DOI] [PubMed] [Google Scholar]
- Viola AU, Archer SN, James LM, Groeger JA, Lo JCY, Skene DJ, Dijk DJ. PER3 polymorphism predicts sleep structure and waking performance. Current Biology. 2007;17:1–6. doi: 10.1016/j.cub.2007.01.073. [DOI] [PubMed] [Google Scholar]
- Vorona RD, Szklo-Coxe M, Lamichhane R, Ware JC, McNallen A, Leszczyszyn D. Adolescent crash rates and school start times in two central Virginia counties, 2009–2011: A follow-up study to a southeastern Virginia study, 2007–2008. Journal of Clinical Sleep Medicine. 2014;10(11):1169–1177. doi: 10.5664/jcsm.4192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vyazovskiy VV, Olcese U, Hanlon EC, Nir Y, Cirelli C, Tononi G. Local sleep in awake rats. Nature. 2011;472(7344):443–447. doi: 10.1038/nature10009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldstreicher J, Duffy JF, Brown EN, Rogacz S, Allan JS, Czeisler CA. Gender differences in the temporal organization of prolactin (PRL) secretion: Evidence for a sleep-independent circadian rhythm of circulating PRL levels - a clinical research center study. Journal of Clinical Endocrinology and Metabolism. 1996;81(4):1483–1487. doi: 10.1210/jcem.81.4.8636355. [DOI] [PubMed] [Google Scholar]
- Wang J-S, Knipling RR, Goodman MJ. The role of driver inattention in crashes; new statistics from the 1995 crashworthiness data system; Presented at the 40th Annual Association for the Advancement of Automotive Medicine Conference; Vancouver, British Columbia, Canada. 1996. Oct, [Google Scholar]
- Webb WB, Agnew H. Reaction time and serial response efficiency on arousal from sleep. Perceptual and Motor Skills. 1964;18:783–784. doi: 10.2466/pms.1964.18.3.783. [DOI] [PubMed] [Google Scholar]
- Wehr TA, Moul DE, Barbato G, Giesen HA, Seidel JA, Barker C, Bender C. Conservation of photoperiod-responsive mechanisms in humans. American Journal of Physiology. 1993;265:R846–R857. doi: 10.1152/ajpregu.1993.265.4.R846. [DOI] [PubMed] [Google Scholar]
- Wertz AT, Ronda JM, Czeisler CA, Wright KP., Jr Effects of sleep inertia on cognition. Journal of the American Medical Association. 2006;295(2):163–164. doi: 10.1001/jama.295.2.163. [DOI] [PubMed] [Google Scholar]
- Wesensten NJ, Belenky G, Kautz MA, Thorne DR, Reichardt RM, Balkin TJ. Maintaining alertness and performance during sleep deprivation: Modafinil versus caffeine. Psychopharmacology. 2002;159(3):238–247. doi: 10.1007/s002130100916. [DOI] [PubMed] [Google Scholar]
- Wierwille WW, Ellsworth LA. Evaluation of driver drowsiness by trained raters. Accident Analysis and Prevention. 1994;26(5):571–581. doi: 10.1016/0001-4575(94)90019-1. [DOI] [PubMed] [Google Scholar]
- Wilkinson RT. Sleep deprivation. In: Edholm OG, Bacharach AL, editors. The Physiology of Human Survival. New York: Academic Press; 1965. pp. 399–430. [Google Scholar]
- Wittmann M, Dinich J, Merrow M, Roenneberg T. Social jetlag: Misalignment of biological and social time. Chronobiology International. 2006;23(1–2):497–509. doi: 10.1080/07420520500545979. [DOI] [PubMed] [Google Scholar]
- Wright KP, Jr, Badia P, Myers BL, Plenzler SC. Combination of bright light and caffeine as a countermeasure for impaired alertness and performance during extended sleep deprivation. Journal of Sleep Research. 1997;6:26–35. doi: 10.1046/j.1365-2869.1997.00022.x. [DOI] [PubMed] [Google Scholar]
- Wright KP, Jr, Hull JT, Czeisler CA. Relationship between alertness, performance, and body temperature in humans. American Journal of Physiology: Regulatory, Integrative, and Comparative Physiology. 2002;283:R1370–R1377. doi: 10.1152/ajpregu.00205.2002. [DOI] [PubMed] [Google Scholar]
- Wyatt JK, Cajochen C, Ritz-De Cecco A, Czeisler CA, Dijk DJ. Low-dose repeated caffeine administration for circadian-phase-dependent performance degradation during extended wakefulness. Sleep. 2004;27(3):374–381. doi: 10.1093/sleep/27.3.374. [DOI] [PubMed] [Google Scholar]
- Wyatt JK, Dijk DJ, Ritz-De Cecco A, Ronda JM, Czeisler CA. Sleep facilitating effect of exogenous melatonin in healthy young men and women is circadian-phase dependent. Sleep. 2006;29:609–618. doi: 10.1093/sleep/29.5.609. [DOI] [PubMed] [Google Scholar]
- Wyatt JK, Ritz-De Cecco A, Czeisler CA, Dijk DJ. Circadian temperature and melatonin rhythms, sleep, and neurobehavioral function in humans living on a 20-h day. American Journal of Physiology: Regulatory, Integrative, and Comparative Physiology. 1999;277:R1152–R1163. doi: 10.1152/ajpregu.1999.277.4.r1152. [DOI] [PubMed] [Google Scholar]


