Introduction
Acute stroke is an emergency and early diagnosis is critical for prompt implementation of potentially lifesaving interventions. Computed tomography (CT) is often the initial imaging modality used in the evaluation of stroke in the acute care setting. A non-contrast CT scan of the head is widely used to quickly identify intracranial hemorrhage and signs of cerebral ischemia or other radiographic contraindications to thrombolytic therapy (e.g. obvious parenchymal hypodensity or intracerebral hemorrhage (ICH)). More specific and subtle CT findings may also contribute to triaging patients to acute stroke interventions, even when the scan is otherwise normal. The hyperdense middle cerebral artery (HDMCA) sign may help persuade a practitioner to triage a patient to acute intervention, even in setting of otherwise normal imaging(1). The sensitivity and specificity of this sign is rater dependent, and can easily be confused with other non-stroke specific findings such as vascular calcifications(2). Even so, its utility is clear, and identifying other objective information on head CT correlated with presence of an acute stroke may similarly assist practitioners in better identifying acute stroke and expediting life saving interventions.
Acute stroke imaging is often interpreted at the point of care by radiologists or stroke practitioners utilizing Picture Archival and Communication (PACS) systems. Images are stored in Digital Imaging and Communications in Medicine (DICOM) standard format and viewed using various DICOM viewers(3).
In acute stroke, clinical gaze deviation to the side of the involved hemisphere and opposite to the side of paralysis, Prévost's sign, has been well noted in clinical practice and in the literature(4). The finding of eye deviation on clinical exam has been found to correlate with diagnosis of stroke in particular cohorts(5). Over recent years, rapid imaging evaluation has been performed more and more in an effort to optimize door to needle times in stroke. Often, this is done before a complete patient history has even been obtained, making imaging the first objective data obtained on the stroke code patient.
Conjugate gaze deviation seen on neuroimaging is also a common finding in acute stroke, as practitioners are trained to look at the CT scan for numerous acute stroke findings. Data on diagnostic and predictive utility of this eye deviation found on initial head CTs or magnetic resonance imaging (MRIs) is available for particular cohorts and diagnostic groups. This conjugate eye deviation finding as applied in the acute stroke code imaging evaluation, the “DeyeCOM sign”, may have significant implications in the emergency care of stroke patients, especially if the remainder of the CT scan does not show significant findings consistent with cerebral ischemia. Analogous to the HDMCA sign, this sign may augment a clinician's history and physical exam to help guide acute management of potential stroke patients even earlier in the evaluation period. In this analysis, we evaluated the stroke code CT imaging of acute stroke code patients to determine the diagnostic and predictive utility of the “DeyeCOM sign” in our acute stroke code patient cohort.
Methods
This analysis included review of all adult acute stroke code patients from a prospectively collected, Investigational Review Board (IRB) approved, registry of consecutive patients entered into the University of California, San Diego (UCSD) Specialized Programs of Translational Research in Acute Stroke (SPOTRIAS) database, and seen at one of our core UCSD facilities, from January 2007 to December 2013.
Patients were excluded from the analysis if initial head CT scan was not available, or if significant motion artifact precluded the ability to determine angle of eye deviation (using the lenses as a reference point). Patients whose lenses were not present on at least one CT scan image were likewise excluded. Eye deviation was then determined for both globes from the non-contrast head CT obtained at the time of initial clinical presentation. Films were reviewed and angles scored by a single reader, who was blinded to patient data including final diagnosis. The DICOM images were viewed using IMPAX software, and the angle of eye deviation was determined by drawing three intersecting lines. The first line was drawn anterioposteriorly through the midline nasal structures; the second line was perpendicular to the midline; and the third line was drawn through the horizontal axis of each lens. The angle of deviation was then calculated for each orbit (Figure 1). Conjugate angles >5 degrees (OD/OS) as noted on initial non-contrast head CT were defined as presence of the “DeyeCOM sign”. All other variations such as no eye deviation, lone eye deviation or disconjugate eye deviation, for the purpose of this primary analysis, were considered as having an absence of the “DeyeCOM sign”. This finding was recorded for each patient's scan and analyzed with the remainder of clinical information previously collected in the SPOTRIAS database. Data included demographics, medical history, risk factors, onset to CT time, Emergency Department (ED) arrival to CT time, glucose, pre-stroke modified Rankin Score (mRS), baseline National Institutes of Health Stroke Scale (NIHSS), final primary diagnosis (where stroke was defined as ischemic stroke or ICH) and 90-day mRS outcome.
Figure 1.
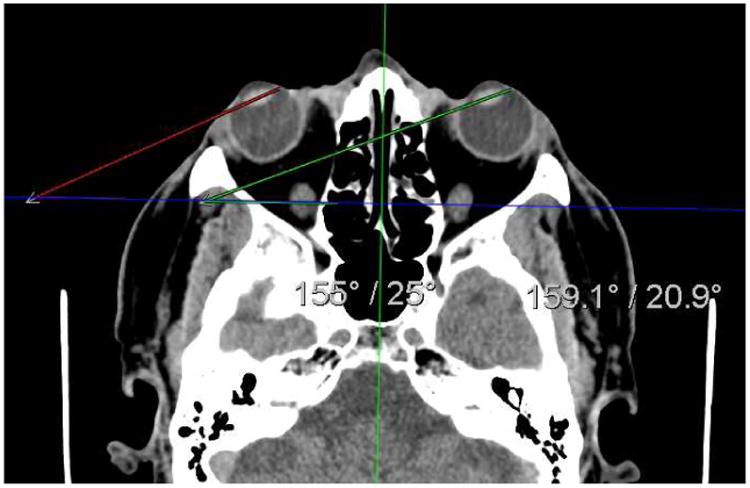
“DeyeCOM sign” on non-contrast CT scan of the head in a stroke code patient presenting to the Emergency Department. The right eye was deviated 25° and the left 20.9°.
Descriptive statistics for baseline variables and outcomes were reported by DeyeCOM sign group and differences between the groups were assessed using Fisher's Exact tests for categorical variables and Wilcoxon Rank-sum tests for continuous variables. Spearman's correlation coefficient was used to assess the correlation between the baseline NIHSS and absolute average eye deviation. Receiver operating characteristic (ROC) analyses (using pROC package in R) were conducted to assess the best cutoff of absolute average angle in predicting acute stroke (AIS, ICH) in participants with eye deviation. Empirical ROC curves were plotted and AUC calculated with 95% confidence interval via bootstrap. The significance level for all comparisons were set at p<0.05 and all statistical testing were two-sided. The statistical software R, version 3.0.3 (http://www.r-project.org) was used for all statistical analyses.
Results
Three hundred and forty two patients were included in the analysis. Of those, 106 (31%) were DeyeCOM+ (presence of the “DeyeCOM sign”) and 236 (69%) were DeyeCOM- (absence of the “DeyeCOM sign”). Age was similar in the two groups, with a mean age of 63 years overall (62.61±16.14 DeyeCOM+ vs. 63.43±15.18 DeyeCOM-; p=0.53). Overall the study population was 56% male. There was a relative higher percentage of females in the DeyeCOM+ group than the DeyeCOM- group (56/106(52.83%) in DeyeCOM+ vs. 96/236(40.68%) in DeyeCOM-; p=0.05). There was a relative higher percentage of hypertension in the DeyeCOM-group (61/106(57.55%) in DeyeCOM+ vs. 168/236 (71.19%) in DeyeCOM-; p=0.02). No other significant differences were found in baseline characteristics between groups though presence of prior central nervous system disease was marginally statistically higher in the DeyeCOM+ group (23/105(21.9%) in DeyeCOM+ vs. 31/236(13.14%) in DeyeCOM-; p=0.05). Baseline characteristics and risk factors are noted in Table 1. There was no difference in pre-stroke mRS (0-2 vs. 3-6) between groups (p=0.25).
Table 1. Baseline characteristics of the study population.
| DeyeCOM+ n=106 | DeyeCOM-n=236 | p | |
|---|---|---|---|
| Age(mean±SD) | 62.6±16yrs | 63.4±15yrs | 0.5276 |
| Gender | 0.0453 | ||
| Male | 50(47.2%) | 140(59.3%) | |
| Female | 56(52.8%) | 96(40.7%) | |
| Race | 0.4674 | ||
| White | 84(79.3%) | 196(83.1%) | |
| Asian | 6(5.7%) | 14(5.9%) | |
| Pacific Islander | 3(2.8%) | 3(1.3%) | |
| Black | 12(11.3%) | 23(9.8%) | |
| Native American | 1(0.9%) | 0(0%) | |
| Ethnicity | 0.765 | ||
| Hispanic | 21(19.8%) | 43(18.2%) | |
| Non-Hispanic | 85(80.2%) | 193(81.8%) | |
| History | |||
| Hypertension | 61(57.6%) | 168(71.2%) | 0.0179 |
| Diabetes | 24(22.6%) | 50(21.2%) | 0.7775 |
| Afib | 17(16.0%) | 42(17.8%) | 0.7584 |
| Pre-stroke mRS(3-6) | 14(13.2%) | 21(8.9%) | 0.2486 |
| NIHSS(mean) | 6.85±6.9 | 5.64±7.5 | 0.0287 |
| NIHSS gaze score | |||
| Score 1-2 | 28(26.4%) | 23(9.8%) | <0.0001 |
| Times(mean) | |||
| Onset-CT | 245.5±367.2min | 353.1±730.8min | 0.1192 |
| Arrival-CT | 39.6±31.7min | 47.5±58.7min | 0.3219 |
For the overall analysis, primary clinical diagnoses are listed in Table 2. In the DeyeCOM+ group, the most common five diagnoses were acute ischemic stroke (AIS) (50.94%), transient ischemic attack (TIA) (8.49%), other (8.49%), somatization (6.6%) and ICH (5.66%). In the DeyeCOM- group, the most common five diagnoses were AIS (43.64%), TIA (14.83%), other (8.05%), somatization (9.75%) and migraine (6.36%). Using the TOAST (Trial of Org 10172 in Acute Stroke Treatment) classification(6), we found no significant differences between DeyeCOM sign groups and type of stroke (p=0.70), even when combining categories of “large vessel atherosclerosis + cardioembolic” vs. others (p=0.22). Time intervals were not different between DeyeCOM+ and DeyeCOM- groups (“Onset to CT Scan”: 245.5±367.2min vs. 353.0±730.8min; p=0.10 and “Arrival to CT Scan”: 39.6±31.7min vs. 47.5±58.7min; p=0.32) (Table 1).
Table 2. Final clinical diagnosis.
| DeyeCOM+ | DeyeCOM- | Total | |
|---|---|---|---|
| Acute ischemic stroke | 54 (50.94%) | 103 (43.64%) | 157(45.9%) |
| Arteriovenous malformations (AVM) | 0 (0%) | 1 (0.42%) | 1(0.29%) |
| Brain metastasis/tumor | 1 (0.94%) | 1 (0.42%) | 2(0.58%) |
| Encephalopathy | 2 (1.89%) | 1 (0.42%) | 3(0.88%) |
| Hyperglycemia | 1 (0.94%) | 0 (0%) | 1(0.29%) |
| Intoxication | 1 (0.94%) | 2 (0.85%) | 3(0.88%) |
| Intracerebral Hemorrhage | 6 (5.66%) | 10 (4.24%) | 16(4.68%) |
| Metabolic | 2 (1.89%) | 7 (2.97%) | 9(2.63%) |
| Migraine | 5 (4.72%) | 15 (6.36%) | 20(5.85%) |
| Other | 9 (8.49%) | 19 (8.05%) | 28(8.19%) |
| Postal ictal (seizure) | 4 (3.77%) | 10 (4.24%) | 14(4.09%) |
| Somatization/Anxiety | 7 (6.6%) | 23 (9.75%) | 30(8.77%) |
| Syncope | 4 (3.77%) | 3 (1.27%) | 7(2.05%) |
| Transient Global Amnesia | 0 (0%) | 4 (1.69%) | 4(1.17%) |
| Transient ischemic attack | 9 (8.49%) | 35 (14.83%) | 44(12.87%) |
| UNKNOWN | 0 (0%) | 2 (0.85%) | 2(0.58%) |
| Unruptured intracranial aneurysm | 1 (0.94%) | 0 (0%) | 1(0.29%) |
| Total | 106 (100%) | 236 (100%) | 342(100%) |
Baseline Emergency Department admission NIHSS and individual item scores were recorded for all patients in the study population. Total NIHSS score at time of evaluation was statistically significantly higher in patients with stroke vs. non-stroke groups groups (8.17±7.87 vs. 3.81±6.11; p<0.0001) and in the DeyeCOM+ vs. the DeyeCOM- groups (6.85±6.95 vs. 5.64±7.54; p=0.03) (Table 1). Those with DeyeCOM sign were more likely to have a positive score on NIHSS Question 2 (Gaze) (28/106(26.42%) vs. 23/236(9.75%); p<0.0001). Patients with a positive score on NIHSS Question 2 (Gaze) also were more likely to have a final diagnosis of stroke (45/173(26.01%) vs. 6/169(3.55%); p<0.0001) (Table 3). Though those with DeyeCOM sign were not more likely to have a final diagnosis of stroke overall (60/106(56.60%) vs. 113/236(47.88%); p=0.16), there was a correlation for the subset with average conjugate eye deviation ≥ 15 degrees (39/61(63.93%) vs. 113/236(47.88%); p=0.03) and a marginally significant correlation for the subset with conjugate eye deviation ≥ 25 degrees (13/18(72.22%) vs. 113/236(47.88%); p=0.05).
Table 3. DeyeCOM sign as Related to NIHSS Gaze Score, Stroke Dx and 90 day mRS.
| Stroke | No Stroke | ||
|---|---|---|---|
| NIHSS gaze score (1-2) | 45(26.01%) | 6(3.55%) | p<0.0001 |
| DeyeCOM+ | DeyeCOM- | ||
| NIHSS gaze score (1-2) | 28(26.4%) | 23(9.8%) | p<0.0001 |
| Final diagnosis stroke | 60(56.6%) | 113(47.9%) | p=0.1606 |
| 90-day mRS 3-6 | 33(34.0%) | 60(28.7%) | p=0.353 |
| 90-day mRS 3-6 (in stroke patients only) | 23(40.35%) | 43(41.35%) | p>0.99 |
For the whole cohort, worse long term outcome, as measured by dichotomized 90-day mRS (0-2 vs. 3-6), were not different overall (33/97(34.02%) in DeyeCOM+ vs. 60/209(28.71%) in DeyeCOM-; p=0.35), for the subset with conjugate eye deviation ≥ 15 degrees (22/59(37.29%) vs. 60/209(28.71%); p=0.26) or for the subset with conjugate eye deviation ≥ 25 degrees (8/17(47.06%) vs. 60/209(28.71%); p=0.17). Similar results were found for the stroke subset of the cohort (23/57(40.35%) vs. 43/104(41.35%);p>0.99) (Table 3).
ROC analyses were used to attempt to determine the best cut off for average angle of deviation in predicting acute stroke (AIS, ICH). Sensitivity and specificity were low for the overall population with DeyeCOM sign (AUC=60.40%, CI: 49.52%-71.27%); the subset with average conjugate eye deviation ≥ 15 degrees (AUC=59.97%, CI: 44.78%-75.15%); and the subset with average conjugate eye deviation ≥ 25 degrees (AUC=46.15%, CI: 15.28%-77.03%).
Discussion
In our cohort of acute stroke code patients, the frequency of DeyeCOM+ patients was 31% overall, and 35% in the patients with clinical diagnoses consistent with stroke (AIS, ICH). There were no major differences noted in risk factors, no significant differences in pre-stroke modified Rankin functional abilities, and no differences in process of care treatment times between the two groups, lending credibility to the appropriateness of the two group comparisons.
As expected, overall frequent diagnoses were AIS, TIA, somatization, other, migraine and ICH. The top five most frequent diagnoses differed between groups only in that ICH was more common in the DeyeCOM+ patients and migraine was more common in the DeyeCOM-patients. This is consistent with expectations. Although clinically the presence of gaze deviation due to seizure or post-ictal state was expected, this diagnosis was interestingly not present in the top five of either group. Although speculative, this may reassure the clinician that conjugate eye deviation in the acute setting is not frequently due to seizure. Further validation of this hypothesis is needed in other cohorts.
The NIHSS score was higher in the DeyeCOM+ than in DeyeCOM- group (6.85 vs. 5.64). This may be expected when one considers that the DeyeCOM sign may also correlate with positive scoring on particular NIHSS items, or because DeyeCOM+ patients may have a higher likelihood of stroke (and stroke patients may have a higher NIHSS than non-stroke patients). We believe each of these options is true since our data reflect that the DeyeCOM sign does correlate with subsequently scoring positive on this element on the NIHSS (p<0.0001), that the NIHSS score was higher in stroke patients than non-stroke patients (p<0.0001), and that there was a positive correlation between DeyeCOM+ patients with eye deviation ≥ 15 degrees and final stroke diagnosis (p=0.03).
In our analysis, DeyeCOM sign correlated with the presence of positive scoring on Question 2 (Gaze) of the NIHSS (p<0.0001), and positive scoring on Question 2 of the NIHSS correlated with the final diagnosis of stroke (p<0.0001). Though we did not see an overall correlation between the DeyeCOM sign and final diagnosis of stroke, there was a positive correlation for the group with average eye deviation ≥ 15 degrees (p=0.03). Other data sets have shown a correlation. Simon et al. found that on CT, conjugate eye deviation or lone abducting eye, reliably pointed to the affected hemisphere in AIS(7). Schwartz et al. noted that conjugate eye deviation on imaging is less common in non-stroke than in stroke, and more common in patients that went to intra-arterial procedures for stroke than those who received IV therapy(8). This implies a possible correlation between presence of eye deviation and severity of stroke (since severe strokes tend to be taken to IA procedures if they “fail IV” or if they are outside of the approved therapeutic window).
Schwartz et al. point out that deviation may be seen in non-stroke patients, as we have also found in our analysis, 43% of the time(8). Interestingly, the presence of eye deviation may also influence the final diagnosis of stroke itself as Mahajan et al noted(9). When eye deviation was present, the reliability of identifying evidence of acute stroke on CT was increased.
In order to further refine our analysis, we assessed if degree of deviation itself would correlate with a final diagnosis of stroke. Lesley et al, using known middle cerebral artery (MCA) strokes, found that though the frequency of gaze deviation was not different between MCA strokes and non-strokes, measurement of ocular gaze deviation is useful in predicting presence of acute ischemic stroke in a refined sample of known MCA stroke patients(5). We did not detect this prediction based on individual degree of eye deviation across the spectrum, but our analysis was not restricted to known MCA strokes, known large vessel strokes, or even image-proven diagnosis of stroke, and there were small sample sizes within each subgroup. Assessing whether DeyeCOM sign was more frequent based on underlying TOAST criteria was also negative overall (p=0.70) and when grouping categories of “large vessel atherosclerosis + cardioembolic” (p=0.22), though this was also likely hindered by small group sizes.
Prior investigators have shown conjugate eye deviation may predict partial or total disability in patients with acute stroke at three months compared to a prior epidemiological study cohort(10). Authors speculate that this may be due to these patients either having a larger stroke size, or perhaps due to the type of lesion portending a poorer prognosis (e.g ICH). Our analysis did not show a significant ability of the DeyeCOM sign to predict 90 day outcome of the overall cohort, or in our stroke subset. This may be due to including many different types of patients in the overall cohort, having too small of a sample size for any particular subset of interest, or simply due to a true lack of correlation. One limitation of our design includes not adjusting for the baseline NIHSS differences between groups. Adjustments were not made as it is likely that the more frequent (p<0.0001) positive scores on Question 2 (Gaze) of the NIHSS are what contributed to the increased overall NIHSS values found in the DeyeCOM+ group.
Eye deviation on CT scan may also help contribute to stroke laterality. Although beyond the scope of our analysis, the usual eyes closed position in the CT scanner, removing fixation, may result in a higher likelihood of tonic eye deviation from a non-dominant hemisphere lesion as noted by other authors(11).
Two of the largest contributions of our analysis to the literature are the strong correlation between the DeyeCOM sign and both subsequently scoring positive on the NIHSS gaze item as well as having a positive correlation with the final diagnosis of stroke. The argument that the practitioner could just eventually perform an NIHSS and find this positive on Question 2 (Gaze), (or await the results of the CT or eventual MRI to see the presence of an infarct) does not focus significantly enough on the changing patterns of acute stroke care. This preliminary evaluation demonstrated that the DeyeCOM sign can be used in addition to the clinical evaluation to reliably assess elements of clinical deficit, and for patients with deviation ≥ 15 degrees, show correlation with final diagnosis of stroke. In acute stroke, prompt diagnosis is critical. Saver et al demonstrated that patients lose 1.9 million neurons and nearly 14 billion synapses for every minute of brain ischemia(12). In current rapid care environments, there is more and more pressure to complete the stroke code evaluation as rapidly as possible. In these settings, sometimes the physical exam and complete history is actually performed after initial neuroimaging. In our own facility, this new paradigm is taking shape. As such, reliable information obtained early in the evaluation process (such as gaze deviation that correlates with subsequent NIHSS scoring elements, and even final stroke diagnosis and long term outcome) could augment the clinical decision making even in the setting of otherwise negative CT scan imaging. Further analysis, in larger cohorts and subsequent analysis plans, will help refine this hypothesis.
This study has some significant limitations which are being addressed in future studies. Although of a reasonable size, with 31% DeyeCOM+ patients, the number of patients in any one category was limited. Although calculation error is possible, the straightforward angle calculation technique makes this unlikely. Some CT scanning protocols routinely exclude the lenses, which could affect the generalizability of the findings, if accurate angle calculations can not be performed. Often, the clinician does not have time to do complex angle measurements. Our center is currently performing a follow up study to determine if the same findings exist when the clinician uses only a quick visual assessment (aka “eyeballs it”) to determine presence of the DeyeCOM sign. Small subsets also likely limited our ability to find a correlation between types of stroke (large vessel, cardioembolic, etc.) with presence or absence of the DeyeCOM sign. Future studies in larger sample sizes will be done looking at larger categories, lone eye deviation, non-dominant hemisphere deviation, and source MRI images instead of CT only.
Acknowledgments
Disclosures: Supported by NIH 5P50NS044148.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Tomsick TA, Brott TG, Olinger CP, et al. Hypderdense middle cerebral artery: incidence and quantitative significance. Neuroradiology. 1989;31(4):312–5. doi: 10.1007/BF00344173. [DOI] [PubMed] [Google Scholar]
- 2.Jha B, Kothari M. Pears & Oysters: Hyperdense or pseudohyperdense MCA sign. A Damocles sword? Neurology. 2009;72:116–117. doi: 10.1212/WNL.0b013e3181a92b3b. [DOI] [PubMed] [Google Scholar]
- 3.Best DE, Horii SC, Bennett W, et al. Review of the American College of Radiology--National Electrical Manufacturers' Association standards activity. Comput Methods Programs Biomed. 1992 May;37(4):305–9. doi: 10.1016/0169-2607(92)90043-7. [DOI] [PubMed] [Google Scholar]
- 4.Prévost MJL. Deviation des yeux et de la tete dans quelques cas d'hémiplégie. Gazette Hebdomadaire de Medecine et de Chirurgie. 1865;41:649–650. [Google Scholar]
- 5.Lesley WS, Rangaswamy R, Smith KH. Predicting acute ischemic stroke by measuring degree of ocular gaze deviation (Prévost's sign) on CT. Journal of Neurointerventional Surgery. 2009;1:32–34. doi: 10.1136/jnis.2009.000281. [DOI] [PubMed] [Google Scholar]
- 6.Adams HP, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24:35–41. doi: 10.1161/01.str.24.1.35. [DOI] [PubMed] [Google Scholar]
- 7.Simon JE, Kennedy J, Pexman JH, et al. The eyes have it: conjugate eye deviation on CT scan aids in early detection of ischemic stroke. Canadian Medical Association Journal. 2003;168(11):1446–1447. [PMC free article] [PubMed] [Google Scholar]
- 8.Schwartz KM, Ahmed AT, Fugate FE, et al. Frequency of Eye Deviation in Stroke and Non-stroke Patients Undergoing Head CT. Neurocritical Care. 2012;17:45–48. doi: 10.1007/s12028-012-9717-x. [DOI] [PubMed] [Google Scholar]
- 9.Mahajan V, Minshew PT, Khoury J, et al. Eye Position Information on CT Increases the Identification of Acute Ischemic Hypoattenuation. American Journal of Neuroradiology. 2008;29:1144–46. doi: 10.3174/ajnr.A0995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tijssen CC, Schulte BP, Leyten AC. Prognostic Significance of Conjugate Eye Deviation in Stroke Patients. Stroke. 1991;22:200–202. doi: 10.1161/01.str.22.2.200. [DOI] [PubMed] [Google Scholar]
- 11.Becker E, Karnath HO. Neuroimaging of eye position reveals spatial neglect. Brain. 2010 Mar;:133, 909–14. doi: 10.1093/brain/awq011. [DOI] [PubMed] [Google Scholar]
- 12.Saver JL. Time is Brain – Quantified. Stroke. 2006;37:263–266. doi: 10.1161/01.STR.0000196957.55928.ab. [DOI] [PubMed] [Google Scholar]


