Abstract
Objective
This review answered two questions: (a) what types of specialty medical settings are implementing models for treating depression, and (b) do models for treating depression in specialty medical settings effectively treat depression symptoms?
Method
We searched Medline/Pubmed to identify articles, published between January 1990 and May 2013, reporting on models for treating depression in specialty medical settings. Included studies had to have adult participants with comorbid medical conditions recruited from outpatient, nonstandard primary care settings. Studies also had to report specific, validated depression measures.
Results
Search methods identified nine studies (six randomized controlled trials, one nonrandomized controlled trial and two uncontrolled trials), all representing integrated care for depression, in three specialty settings (oncology, infectious disease, neurology). Most studies (N=7) reported greater reductions in depression among patients receiving integrated care compared to usual care, particularly in oncology clinics.
Conclusions
Integrated care for depression in specialty medical settings can improve depression outcomes. Additional research is needed to understand the effectiveness of incorporating behavioral and/or psychological treatments into existing methods. When developing or selecting a model for treating depression in specialty medical settings, clinicians and researchers will benefit from choosing specific components and measures most relevant to their target populations.
Keywords: Integrated care, Depression, Cancer, HIV/AIDS, Multiple sclerosis
1. Introduction
Of the 15.2 million adults in the United States who experience a major depressive episode each year, 37% seek care only from a primary care provider [1], indicating a clear need for mental health care in medical settings [2,3]. One way to address this need is through models that integrate depression treatment with general medical care [4–8]. In primary care settings, such programs usually include systematic screenings for depression and direct access to depression treatments, as well as the use of medication treatment algorithms (e.g., Sequenced Treatment Alternatives to Relieve Depression) [9,10]. These programs may also include depression care managers who serve as patients’ mental health points of contact and work to coordinate care by consulting with physicians and specialty mental health providers. Depression care managers may also provide psychotherapy or other low-intensity behavioral treatments [6,7].
A recent meta-analysis found that one specific model of care, collaborative care for depression, effectively treats depression when implemented in primary care settings [11]. However, not all patients with depression are managed in primary care settings; some patients, including those with chronic medical conditions, must be managed in specialty medical settings. The joint management of depression and chronic medical conditions is important because individuals with chronic medical conditions are more likely to develop depression than those without such conditions [12]. Furthermore, the relationship between depression and chronic medical conditions is bidirectional [12]. Chronic medical conditions can lead to depression through biological changes (e.g., vascular depression) or through the negative psychosocial consequences of managing disease (e.g., loss of functioning, role disruptions) [13]. At the same time, depression can exacerbate chronic medical conditions, for example, depression is associated with insulin resistance [14], and individuals with depression are more sedentary [15] and less likely to adhere to chronic illness self-management behaviors than individuals without depression [12,16,17].
Given the bidirectional relationship between depression and chronic medical conditions, it is reasonable to hypothesize that patients would benefit from models of care that treat depression in specialty medical settings. However, to our knowledge, no reviews describe the efficacy or effectiveness of such programs. Therefore, this review provides preliminary answers to two questions: (a) what types of specialty medical settings are implementing models for treating depression, and (b) do models for treating depression in specialty medical settings effectively treat depression symptoms?
2. Materials and methods
2.1. Search strategy
One author and a research assistant conducted a search in PubMed/Medline using the following major search terms: Depression or Depressive Disorder in addition to any of the following MeSH terms alone or in combination: Delivery of Health Care; Delivery of Health Care, Integrated; Rehabilitation; Patient-Centered Care; Health Promotion; Recreation Therapy and Cooperative Behavior. All results were imported into RefWorks (a reference manager).
2.2. Selection strategy
Two authors independently reviewed articles identified during the initial search using RefWorks and the following inclusion criteria. All abstracts/articles had to (a) be published in a peer-reviewed journal between January 1, 1990, and May 22, 2013; (b) be written in English; (c) include adult (aged 18+) participants with a medical condition; (d) include participants recruited from an outpatient, non-mental-health setting, including specialty medical or nonstandard primary care settings (e.g., primary care specifically for individuals with HIV); (e) report a quantitative measure of depression severity as an outcome and (f) define and assess depression using standardized structured interviews [e.g., Patient Health Questionnaire-9 (PHQ-9); 18] or by specific cutoff scores on validated depression-symptom scales. If the article met these criteria, it was further assessed as a “model of care.” A model of care was defined as an inclusive, intentional, systematic approach grounded in theory and directed at a desired outcome [19]. Given the nascent area of the literature, we chose to include studies conducted in any specialty medical setting. Reviewers also applied the following exclusion criteria: (a) studies could not solely measure the effectiveness of specific interventions (e.g., a randomized controlled trial of cognitive behavior therapy), and (b) studies could not be prevention or screening studies, reviews, meta-analyses, dissertations, reports, meeting abstracts or case studies. The same two authors discussed results and any questions regarding inclusion/exclusion criteria, occasionally seeking a third opinion until consensus. Given the nascent area of this research, we did not include medical specialty search terms (e.g., oncology) in order to keep results as inclusive as possible.
2.3. Study characteristics
The authors used RefWorks to identify and remove duplicate abstracts and abstracts published before 1990. Abstracts were then divided among reviewers for review. Full articles were reviewed if abstracts lacked sufficient information on inclusion and exclusion criteria. Data were collected on study design, participant characteristics (e.g., comorbid medical conditions), model characteristics and depression outcomes.
3. Results
3.1. Trial flow and study characteristics
The original search resulted in 1115 abstracts (Fig. 1). Nine articles were identified for study inclusion: six randomized controlled trails (RCTs), one nonrandomized controlled trial and two uncontrolled trials (Table 1). All studies identified their interventions as “collaborative care models,” but no study provided enough information to determine whether the model of care met criteria for the foundational components of Collaborative Care as described by the Advancing Integrated Mental Health Solutions (AIMS) Center at the University of Washington (http://aims.uw.edu/collaborative-care/principles-collaborative-care). Therefore, the models assessed in this review are best described as integrated care models (i.e., models that integrate mental and medical services but do not meet all the criteria of Collaborative Care or do not provide enough information to make that determination). In addition, it should be noted that two articles described different follow-up time points of the same study [20,21]. Dwight and colleagues [22] described pilot work for those two studies [20,21], but because the pilot focused on a specific population (women), we considered it a distinct program for the purposes of this review.
Fig. 1.
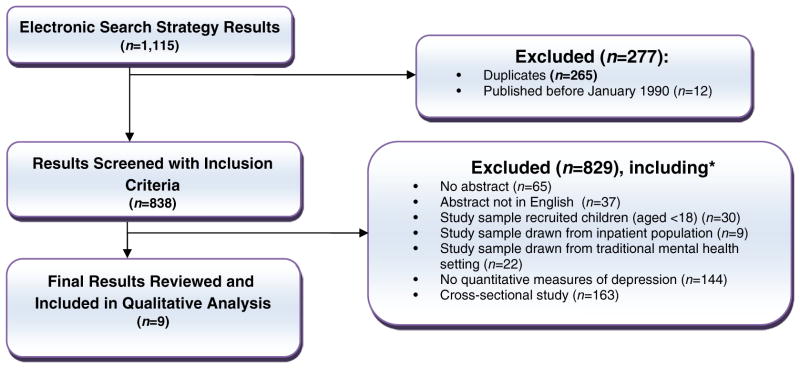
Trial flow. *This box provides a sample of exclusion criteria; therefore, samples do not equal 829.
Table 1.
Study designs and outcomes.
| Authors | Location | Year | Study name | Chronic condition studied |
Sample size | Sample size of those who completed all assessments |
Clinical setting | Study design | Program duration |
Depression- specific outcome measures |
Empirical support |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cancer | |||||||||||
| Dwight et al. [22] | Los Angeles, CA | 2005 | Multifaceted Oncology Depression Program (pilot for Ell et al.) | Breast or cervical cancer and major depressive disorder, dysthymia or persistent depressive symptoms at baseline and 1-month follow-up | 55 | 36 | Public-sector oncology clinics | RCT | 8 weeks | PHQ-9 | ITT: Significantly more participants had a 50% decrease in depressive symptoms in integrated vs. usual care at month 8 (37% vs. 12%) |
| Ell et al. [20,21] | Los Angeles, CA | 2008; 2011 (1-year follow-up) | Alleviating Depression Among Patients with Cancer (ADAPt-c) | Cancer and major depressive disorder or dysthymia | 472 | Month 6: ADAPT-c=166, enhanced usual care=152; month 12: ADAPT-c=144, enhanced usual care=114; month 24: ADAPT-c=111, enhanced usual care=99 | Outpatient oncology clinic | RCT | Up to 12 months | PHQ-9; Antidepressant medication prescription rates | ITT: Significantly more participants had a 50% decrease in depressive symptoms in integrated vs. enhanced usual care at months 12 (63% vs. 50%) and 24 (46% vs. 32%), but not at months 6 or 18. Significantly more participants achieved a 5-point decrease on PHQ-9 at months 12 (72.2% vs. 59.7%), 18 (69% vs. 55%) and 24 (54% vs. 37%) in integrated vs. enhanced usual care, but not at month 6. Significantly higher percentage of participants were in remission (PHQ-9 <5) in integrated vs. enhanced usual care only at month 18 (44% vs. 34%). Significantly higher percentage of participants were prescribed antidepressant medication in integrated vs. enhanced usual care only at month 12 (9% vs. 33%). |
| Strong et al. [24] | Southeast Scotland, UK | 2008 | Depression Care for People with Cancer (SMaRT oncology 1) | Cancer and major depressive disorder | 200 | 196 | Specialist cancer center | RCT | 3 months | SCL-20; remission of depression (SCL-20 <0.75 or no diagnosis via SCID) | Completer: significantly lower median SCL-20 score in integrated vs. usual care only at months 3 (1.20 vs. 1.55), 6 (1.03 vs. 1.51), and 12 (1.12 vs. 1.43); significantly greater number of participants showed at least a 50% decrease in depression symptoms in integrated vs. usual care at month 3 (53% vs. 34%); significantly more participants in remission of major depressive disorder via the SCL-20 (15% greater) and SCID (45% vs. 68%) in integrated vs. usual care. |
| Kroenke et al. [23] | Indiana | 2010 | Indiana Cancer Pain and Depression (INCPAD) trial | Cancer, cancer-related pain, and depression | 405 | Month 1: INCPAD=175, usual care=179; Month 3: INCPAD=169, usual care=166; Month 6: INCPAD=151, usual care=153; Month 12: INCPAD=134, usual care=135 | Urban and rural oncology practices | RCT | 12 months | SCL-20; PHQ-9; depression severity subscale of SF-36 | ITT: Specific findings not reported, but said to be significant. Completer: significantly greater improvements in HSCL-20 depression severity in integrated vs. usual care. Between-group effect size differences were 0.31 (1 month), 0.42 (3 months), 0.45 (6 months) and 0.41 (12 months). Greater improvements in Mental Health Inventory depression severity and diagnostic status outcomes in integrated vs. usual care. Significantly fewer participants met PHQ-9 criteria for depression in integrated vs. usual care at months 3 and 12. |
| HIV/AIDS | |||||||||||
| Adams et al. [26] | Durham, NC | 2011 | – | HIV and depression | 13 | 9 | Outpatient infectious disease clinic | Uncontrolled intervention | 12 weeks | PHQ-9 | ITT: not reported; completers: mean PHQ-9 score significantly decreased (18.33 at baseline, 11.44 at week 12) |
| Coleman et al. [27] | Boston, MA | 2012 | – | HIV/AIDS and depression | 123 | 66 | HIV Clinic with colocated psychiatric consultation service | Retrospective chart review without control group | No time limit | BDI-II; antidepressant medication prescription rates | ITT: not reported; completer: significantly lower BDI-II scores between first and last appointments (23 vs. 15.7; follow-up time varied); higher percentage of patients prescribed antidepressant medications at posttreatment compared to baseline (70% vs. 55%). |
| Pyne et al. [29] | Atlanta, GA; Houston, TX; Little Rock, AR | 2011 | HIV Translating Initiatives for Depression into Effective Solutions (HITIDES) | HIV and depression | 249 | Month 6: HITIDES=109; usual care=117; Month 12: HITIDES=105; usual care=110 | VA ambulatory specialty clinic for HIV | Single-blind RCT | Up to 12 months | Treatment response (50% decrease in SCL-20 score), remission (mean SCL-20 item score <0.5) and depression-free days; antidepressant medication prescription rates; self-report antidepressant medication adherence | Significantly greater treatment response (33% vs. 17.5%) and remission rates (22% vs. 12%) in integrated vs. usual care at month 6, but not at month 12; significantly more depression-free days in integrated vs. usual care at month 12; no significant differences in antidepressant prescription rates or adherence in integrated vs. usual care at month 6 or 12. |
| Multiple sclerosis | |||||||||||
| Patten et al. [30] | Calgary, Canada | 2007 | – | Multiple sclerosis and depression | 90 | 22 | University of Calgary multiple sclerosis clinic | Nonrandomized controlled trial | 6 months | MINI (depression diagnosis); antidepressant medication prescription rates and dose | ITT: no significant difference in percentage of patients with depression between integrated vs. usual care at month 6 (33.3% vs. 55.2%); no significant differences in percentage of patients prescribed antidepressants in integrated vs. usual care at month 6 (59.3% vs. 48.3) or the number taking an adequate dose in integrated vs. usual care at month 6 (62.5% vs. 71.4%). |
ITT, intent to treat; Completer, analyses that use only participants who completed all assessments; CES-D, Center for Epidemiologic Studies Depression Scale; MEMS, Medication event Monitoring System; HSCL-20, Hopkins Symptom Checklist-20; HRS-D, Hamilton Rating Scale-Depression; PRIME-MD, Primary Care Evaluation of Mental Disorders; –, not reported; SF-36: Short Form Health Survey.
3.2. Data synthesis
Different patient populations may have different treatment needs; therefore, results are first presented by disease type. In the final data-synthesis section, we present information on variability in model components across disease type in order to provide information that is translatable to clinical settings (Table 2). The number of components was not necessarily associated with better models or better patient outcomes.
Table 2.
Variability in model components.
| Authors | Delivery agent | Pharmacotherapy | Rx treatment algorithm |
Stepped care plan |
Consultative approach |
Telephone follow-Up |
Patient psychoeducation |
Provider psychoeducation |
Specialty mental health referral |
Self-mgmt coaching |
Colocated psychotherapy |
Face-to-face follow-up |
Maintenance plan |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cancer | |||||||||||||
| Dwight et al. [22] | Cancer/depression clinical specialist (master’s-level social worker) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | – |
| Ell et al. [20,21] | Bilingual cancer depression clinical specialist (master’s-level social worker), supervised by psychiatrist | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ |
| Strong et al. [24] | Nurse without prior psychiatric experience, study psychiatrist | ✓ | ✗ | ✗ | ✓ | ✓ | ✓ | ✓ | – | ✓ | ✓ | ✗ | – |
| Kroenke et al. [23] | Nurse care manager; pain psychiatrist specialist | ✓ | ✓ | ✓ | – | ✓ | ✓ | – | – | – | ✗ | ✗ | – |
| HIV/AIDS | |||||||||||||
| Adams et al. [26] | Nonmedically trained care managers (social workers) supervised by psychiatrist | ✓ | ✓ | ✓ | – | ✓ | – | – | ✓ | – | ✗ | ✓ | – |
| Coleman et al. [27] | Psychiatrist, consultation–liaison fellow, administrative assistant as case manager | ✓ | ✓ | ✓ | ✓ | – | – | ✓ | ✓ | – | – | – | – |
| Pyne et al. [29] | Depression care manager (registered nurse), clinical pharmacist, psychiatrist | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | ✗ |
| Multiple sclerosis | |||||||||||||
| Patten et al. [30] | Depression care manager (psychiatric nurse with multiple sclerosis training who completed IMPACT training) and psychiatrist | ✓ | ✓ | ✓ | ✓ | – | – | – | ✓ | – | ✓ | ✓ | ✓ |
The number of components was not necessarily associated with better models or better patient outcomes. Rx, prescription; mgmt, management; ✓, included in model; ✗, not included in model; –, inclusion not reported; Consultative approach, consulting with a psychiatrist; Telephone/face-to-face follow-up, at least one telephone/face-to-face check-in after treatment initiation; Patient/provider psychoeducation, psychoeducation about depression and the target medical condition; Self-management coaching, coaching related to the target medical condition; Maintenance plan, plan developed with patients for use after treatment ends.
3.2.1. Cancer
Five studies assessed integrated care for depression in oncology settings. All five studies were RCTs with significant, positive treatment effects. With the exception of a pilot study for patients with gynecological cancers, assessed by Dwight and colleagues [22], all studies included patients with any form of cancer. Results of the pilot study, conducted by Dwight and colleagues (N=55) [22], demonstrated that, after 8 months, patients receiving integrated care for depression in an oncology clinic were significantly more likely to have a 50% decrease in depressive symptoms as measured by the PHQ-9 [18] compared to patients receiving usual care in that clinic [22]. The two studies (N=472) [20,21] based on this pilot work [22] had similar results over a longer follow-up period: after 24 months, patients receiving integrated care in an oncology clinic were significantly more likely to have a 50% decrease in depressive symptoms as measured by the PHQ-9 [18] than those receiving enhanced usual care in that clinic. (In this study, enhanced usual care included providing patients with pamphlets about depression, providing didactics on depression to treating oncologists and informing treating oncologists of a patient’s depression status.) There were no significant differences in antidepressant medication rates between integrated care and enhanced usual care at 24 months. However, antidepressant medication rates were significantly higher in the integrated care group at the 12-month follow-up. Consistent with these findings, two additional studies in oncology settings (N=405 and N=200, respectively) [23,24], with shorter follow-up time periods (12 and 6 months, respectively), found significant decreases in depression-symptom severity as measured by the Symptom Checklist-20 (SCL-20; [25]) in integrated care compared with usual care.
3.2.2. HIV/AIDS
Three studies investigated the effects of integrated care for depression in specialty settings for HIV/AIDS. Results of the two uncontrolled studies (N=13 and N=123, respectively) [26,27] found significant decreases in depression-severity scores between baseline and follow-up [measured by the PHQ-9 [18] and the Beck Depression Inventory-II (BDI-II) [28], respectively]. Notably, mean scores on the BDI-II [28] at follow-up remained above clinical cutoffs for depression in one study [27] despite the fact that patients who received integrated care were more likely to have antidepressant medication prescriptions at follow-up than at baseline. Results from the single RCT (N=249) [29] found an early difference in depression remission rates as measured by the SCL-20 [25] between integrated care and usual care, but the statistically significant difference was not sustained at the 12-month follow-up. In addition, Pyne and colleagues [29], the authors of this RCT, found no significant differences in antidepressant medication prescription rates between integrated care and usual care. However, patients receiving integrated care in this study had more depression-free days than patients in usual care.
3.2.3. Multiple sclerosis
One study used a nonrandomized controlled trial to test integrated care for depression in a multiple sclerosis clinic (N=90) [30]. There were no significant differences in the percentage of patients with depression as measured by the Mini-International Neuropsychiatric Interview (MINI [31]) at 6-month follow-up between patients who received integrated care and those who received treatment as usual. In addition, there were no significant differences between the two groups in antidepressant medication prescription rates.
3.2.4. Intervention characteristics
As described above, all studies described models of depression care as being based on collaborative care models. Four studies cited specific collaborative care programs. Three of these four studies [20,21,30] were based on Improving Mood-Promoting Access to Collaborative Treatment (IMPACT) [32,33], one of the first large-scale collaborative care models. The remaining study that cited a specific collaborative care program [29] was based on Translation Initiatives for Depression into Effective Solutions (TIDES), a Veteran Health Administration’s collaborative care program [34,35]. Of the five remaining studies, three cited specific journal references, but not specific programs, when describing collaborative care [22–24]. The remaining two studies [26,27] did not cite references in relation to descriptions of collaborative care. No paper provided sufficient information to determine whether the model of care met the five principles of Collaborative Care presented on the AIMS website.
No studies provided information on all of the model components identified in this review (Table 2). However, all models included pharmacotherapy, and all but one model [24] included a medication treatment algorithm and a stepped-care plan. Most models included a consultative approach (i.e., consultations with psychiatrists) [20–22,24,27,29,30] and/or telephone follow-up (i.e., at least one telephone check-in after treatment initiation) [20–24,26,29]. Roughly half of the models included patient psychoeducation [20–24,29] and/or provider psychoeducation about depression and the target medical condition [20–22,24,27,29], specialty mental health referrals [20,21,26,27,29,30], self-management coaching related to the target medical condition (e.g., medication adherence) [20–22,24,29] and/or colocated psychotherapy [20–22,24,30]. Three models included face-to-face follow-up after treatment initiation [22,26,30], and only two models reported providing patients with a maintenance plan for use after treatment ended [20,21,30].
4. Discussion
All nine studies identified in our systematic search of the literature reported on integrated care models for treating depression in one of three specialty medical settings: oncology, infectious disease or neurology. Most studies provided support for the effectiveness of integrated care models for treating depression in specialty medical settings. However, depression outcomes differed based on participants’ comorbid diagnoses and/or the specialty medical setting in which the integrated care model was implemented. The studies testing integrated care for depression in oncology clinics [20–24] provided the strongest support. In contrast, the single study testing integrated care for depression in a multiple sclerosis clinic suggested that integrated care did not result in better depression outcomes. Outcomes were mixed for integrated care for depression in specialty HIV/AIDS settings; despite positive findings from uncontrolled studies [26,27], a large RCT [29] found no significant differences in the reduction of depression symptoms among patients receiving integrated care as compared to usual care.
The five studies testing integrated care for depression in oncology clinics provided the most compelling evidence for the effectiveness of integrated care. All studies found that integrated care reduced depression, and importantly, three of the five studies were large RCTs. At least two additional studies published since we conducted this review also support the effectiveness and efficacy of integrated care for depression in oncology settings. Both of these new studies provided additional tests of the Symptom Management Research Trials (SMaRT) Oncology trials. (SMaRT-1 [24] was included in the present review.) The results of SMaRT-2 (N=500) [36], an effectiveness trial of the same integrated model of depression care tested in an efficacy trial in SMaRT-1, demonstrated that individuals in integrated care were more likely to have a 50% decrease in depression severity than individuals in enhanced usual care (as measured by the SCL-20 [25]). SMaRT-3 [37] tested an integrated care model specifically for individuals with poor prognosis cancer (the model was based on the models used in SmaRT-1 and SMaRT-2). The results were similarly positive; individuals in integrated care were more likely to have a 50% decrease in depression severity than individuals in enhanced usual care (as measured by the SCL-20 [25]). Notably, treatment outcomes of the SMaRT interventions were stronger with each subsequent study despite the fact that each study was tested in more challenging settings and with sicker patients.
The results of Pyne and colleagues’ [29] large RCT of integrated care for depression in a specialty HIV clinic were also notable. Specifically, the authors did not find lasting differences in depression outcomes between integrated care and usual care. However, the lack of difference between integrated care and usual care was not attributed to poor improvement in both groups but rather to improvement in both groups. The fact that both groups were screened for depression suggests that such screenings may be a relatively cost-effective way to improve depression outcomes in some specialty medical settings. It must also be noted that Pyne and colleagues [29] conducted their work in the Veterans Affairs (VA) health care system. VA provides comprehensive physical and mental health care to Veterans, often at no or low cost. Therefore, simply screening for depression may not improve outcomes outside integrated health care systems like VA (e.g., settings where patients lack access to affordable mental health treatment).
Among the studies in the present review, a greater number of model components was not necessarily associated with positive outcomes. Similarly, a recent meta-analysis of Collaborative Care programs found that the most effective programs used only four or five components of collaborative care [11]. It is also of note that all programs in this review relied on one specific component of care: pharmacotherapy to treat depression. Fewer studies included behavioral treatments for depression, suggesting room for additional work integrating such treatments into models for treating depression in specialty medical settings. As suggested by others, low-intensity treatments, provided by individuals without advanced degrees, may provide one way to incorporate behavioral treatments into integrated care models for depression without increasing costs [6,7].
There are some methodological concerns related to the studies included in this review. First, comparisons of results across studies were limited because of the different lengths of follow-up time periods and variations in the methods used to assess depression outcomes. For example, one study described the percentage of participants without clinically diagnosed depression at follow-up [30], whereas other studies reported mean change in scores on different measures of depressive symptoms [e.g., 26], and other studies reported the percentage of participants who achieved at least a 50% decrease in depressive symptoms over the course of the study [e.g., 24]. A third, related methodological concern is that few studies reported a priori primary outcomes. Therefore, it is unclear whether studies reported different outcome measures based on different theoretical explanations for the effects of the care models or if the differences were due to the selective reporting of significant results.
In addition, it is not clear which depression outcome is most important — reducing depression symptoms may be as beneficial as eliminating depression symptoms, depending upon comorbid conditions or other situational factors. Similarly, while clinical remission of a depressive syndrome may be the goal of clinical practice, the absence of a depression diagnosis may be too stringent a criterion for studies that are time limited and involve chronic medical conditions with symptoms that overlap with the somatic and cognitive features of depression. Further, even when there is a clinically significant reduction in depressive symptoms, residual symptoms of mood disorders frequently persist and are amenable to continued medication adjustments and psychotherapeutic interventions [38]. Future work on models of care for treating depression in specialty medical settings should tease apart these issues. For example, including a priori rationales for primary out-come measures will ease comparisons across studies and help clinicians and scientists accurately interpret the findings of individual studies.
Other limitations include the fact that many studies had small sample sizes, and three of the nine studies were reports from the same research group. As with other literature reviews, biases towards publishing only positive outcomes may also have affected conclusions. In addition, some studies [29] relied heavily on research staff, and therefore, the findings may not generalize to routine care settings. Nevertheless, given the dearth of work in this area, the current review offers important preliminary information on models of care for treating depression in specialty medical settings.
5. Conclusion
Results of this review suggest that integrated care for depression in specialty medical settings can improve depression outcomes. However, optimal models of integrated care for depression may differ across specialty medical settings and among comorbid medical conditions. Additional research is needed on how to incorporate behavioral or psychological treatments for depression into integrated care models for depression. Results also suggest that when developing models for treating patients with depression and chronic medical conditions (e.g., Parkinson’s disease and other neurological conditions), clinicians and researchers will benefit from thoughtfully selecting the specific components and outcomes that provide the greatest impact for their patient population.
Acknowledgments
The authors would like to thank Aimee Nguyen for assistance with the literature search and Sonora Hudson for assistance with formatting the manuscript.
Footnotes
Funding acknowledgment: This material is the result of work supported with resources and the use of facilities at the Houston Veterans Affairs (VA) Health Services Research and Development (HSR&D) Center for Innovations in Quality, Effectiveness and Safety (CIN13-413) at the Michael E. DeBakey VA Medical Center. It was also supported by the Methods of Optimal Detection in Parkinson’s disease grant (NIH-R01 MH069666). In addition, it was supported by the VA Office of Academic Affiliations and VA HSR&D Service in conjunction with a VA HSR&D Advanced Fellowship Program.
Disclosure: conflicts of interest: none
Contributor Information
Jessica Y. Breland, Email: breland@stanford.edu.
Joseph Mignogna, Email: joseph.mignogna@va.gov.
Lea Kiefer, Email: lea.kiefer@va.gov.
Laura Marsh, Email: laura.marsh2@va.gov.
References
- 1.(SAMHSA) SAaMHSA. More than one third of adults with major depressive episode did not talk to a professional. National Survey on Drug Use and Health Data Spotlight. 2014 [Google Scholar]
- 2.Goodrich DE, Kilbourne AM, Nord KM, Bauer MS. Mental health collaborative care and its role in primary care settings. Curr Psychiatry Rep. 2013;15:383. doi: 10.1007/s11920-013-0383-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levey SM, Miller BF, Degruy FV., III Behavioral health integration: an essential element of population-based healthcare redesign. Transl Behav Med. 2012;2:364–71. doi: 10.1007/s13142-012-0152-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grazier KL, Smith JE, Song J, Smiley ML. Integration of depression and primary care: barriers to adoption. J Prim Care Commun Health. 2014;5:67–73. doi: 10.1177/2150131913491290. [DOI] [PubMed] [Google Scholar]
- 5.Katon W, Von Korff M, Lin E, Simon G. Rethinking practitioner roles in chronic illness: the specialist, primary care physician, and the practice nurse. Gen Hosp Psychiatry. 2001;23:138–44. doi: 10.1016/s0163-8343(01)00136-0. [DOI] [PubMed] [Google Scholar]
- 6.Richards DA. Access and organization: putting low intensity interventions to work in clinical services. In: Bennett-Levy J, Richards D, Farrand P, Christensen H, Griffiths K, Kavanagh D, Klein B, editors. Oxford guide to low intensity CBT interventions. Oxford, UK: Oxford University Press; 2010. pp. 19–33. [Google Scholar]
- 7.Richards DA. Collaborative care: the effective organization of treatment for depression. In: Bennett-Levy J, Richards D, Farrand P, Christensen H, Griffiths K, Kavanagh D, Klein B, editors. Oxford guide to low intensity CBT interventions. Oxford, UK: Oxford University Press; 2010. pp. 121–8. [Google Scholar]
- 8.Unutzer J, Harbin H, Shoenbaum M, Druss B. The collaborative care model: an approach for integrating physical and mental health care in Medicaid health homes. Centers for Medicare & Medicaid Services, the Center for Health Care Strategies and Mathematica Policy Research; 2013. [Google Scholar]
- 9.Fava M, Rush AJ, Trivedi MH, Nierenberg AA, Thase ME, Sackeim HA, et al. Background and rationale for the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study. Psychiatr Clin North Am. 2003;26:457–94. doi: 10.1016/s0193-953x(02)00107-7. [DOI] [PubMed] [Google Scholar]
- 10.Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163:1905–17. doi: 10.1176/ajp.2006.163.11.1905. [DOI] [PubMed] [Google Scholar]
- 11.Thota AB, Sipe TA, Byard GJ, Zometa CS, Hahn RA, McKnight-Eily LR, et al. Collaborative care to improve the management of depressive disorders: a community guide systematic review and meta-analysis. Am J Prev Med. 2012;42:525–38. doi: 10.1016/j.amepre.2012.01.019. [DOI] [PubMed] [Google Scholar]
- 12.Katon WJ. Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues Clin Neurosci. 2011;13:7–23. doi: 10.31887/DCNS.2011.13.1/wkaton. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Detweiler-Bedell JB, Friedman MA, Leventhal H, Miller IW, Leventhal EA. Integrating co-morbid depression and chronic physical disease management: identifying and resolving failures in self-regulation. Clin Psychol Rev. 2008;28:1426–46. doi: 10.1016/j.cpr.2008.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kan C, Silva N, Golden SH, Rajala U, Timonen M, Stahl D, et al. A systematic review and meta-analysis of the association between depression and insulin resistance. Diabetes Care. 2013;36:480–9. doi: 10.2337/dc12-1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhai L, Zhang Y, Zhang D. Sedentary behaviour and the risk of depression: a meta-analysis. Br J Sports Med. 2014:1–6. doi: 10.1136/bjsports-2014-093613. http://dx.doi.org/10.1136/bjsports-2014-093613. [DOI] [PubMed]
- 16.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–7. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 17.Gonzalez JS, Batchelder AW, Psaros C, Safren SA. Depression and HIV/AIDS treatment nonadherence: a review and meta-analysis. J Acquir Immune Defic Syndr. 2011;58:181–7. doi: 10.1097/QAI.0b013e31822d490a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davidson P, Halcomb E, Hickman L, Phillips J, Graham B. Beyond the rhetoric: what do we mean by a ‘model of care’? Aust J Adv Nurs. 2006;23:47–55. [PubMed] [Google Scholar]
- 20.Ell K, Katon W, Xie B, Lee PJ, Kapetanovic S, Guterman J, et al. One-year postcollaborative depression care trial outcomes among predominantly Hispanic diabetes safety net patients. Gen Hosp Psychiatry. 2011;33:436–42. doi: 10.1016/j.genhosppsych.2011.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ell K, Xie B, Quon B, Quinn DI, Dwight-Johnson M, Lee PJ. Randomized controlled trial of collaborative care management of depression among low-income patients with cancer. J Clin Oncol. 2008;26:4488–96. doi: 10.1200/JCO.2008.16.6371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dwight-Johnson M, Ell K, Lee PJ. Can collaborative care address the needs of low-income Latinas with comorbid depression and cancer? Results from a randomized pilot study. Psychosomatics. 2005;46:224–32. doi: 10.1176/appi.psy.46.3.224. [DOI] [PubMed] [Google Scholar]
- 23.Kroenke K, Theobald D, Wu J, Norton K, Morrison G, Carpenter J, et al. Effect of telecare management on pain and depression in patients with cancer: a randomized trial. JAMA. 2010;304:163–71. doi: 10.1001/jama.2010.944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Strong V, Waters R, Hibberd C, Murray G, Wall L, Walker J, et al. Management of depression for people with cancer (SMaRT oncology 1): a randomised trial. Lancet. 2008;372:40–8. doi: 10.1016/S0140-6736(08)60991-5. [DOI] [PubMed] [Google Scholar]
- 25.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL). A measure of primary symptom dimensions. Mod Probl Pharmacopsychiatry. 1974;7:79–110. doi: 10.1159/000395070. [DOI] [PubMed] [Google Scholar]
- 26.Adams J, Pollard RS, Sikkema KJ. Feasibility of integrated depression care in an HIV clinic. Psychiatr Serv. 2011;62:804. doi: 10.1176/appi.ps.62.7.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Coleman SM, Blashill AJ, Gandhi RT, Safren SA, Freudenreich O. Impact of integrated and measurement-based depression care: clinical experience in an HIV clinic. Psychosomatics. 2012;53:51–7. doi: 10.1016/j.psym.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 28.Beck A, Steer R, Brown G. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 29.Pyne JM, Fortney JC, Curran GM, Tripathi S, Atkinson JH, Kilbourne AM, et al. Effectiveness of collaborative care for depression in human immunodeficiency virus clinics. Arch Intern Med. 2011;171:23–31. doi: 10.1001/archinternmed.2010.395. [DOI] [PubMed] [Google Scholar]
- 30.Patten SB, Newman S, Becker M, Riddell C, Metz L. Disease management for depression in an MS clinic. Int J Psychiatry Med. 2007;37:459–73. doi: 10.2190/PM.37.4.h. [DOI] [PubMed] [Google Scholar]
- 31.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [quiz 34–57] [PubMed] [Google Scholar]
- 32.Hunkeler EM, Katon W, Tang L, Williams JW, Jr, Kroenke K, Lin EH, et al. Long term outcomes from the IMPACT randomised trial for depressed elderly patients in primary care. BMJ. 2006;332:259–63. doi: 10.1136/bmj.38683.710255.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Unutzer J, Katon W, Callahan CM, Williams JW, Jr, Hunkeler E, Harpole L, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288:2836–45. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 34.Luck J, Hagigi F, Parker LE, Yano EM, Rubenstein LV, Kirchner JE. A social marketing approach to implementing evidence-based practice in VHA QUERI: the TIDES depression collaborative care model. Implement Sci. 2009;4:64. doi: 10.1186/1748-5908-4-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rubenstein LV, Chaney EF, Ober S, Felker B, Sherman SE, Lanto A, et al. Using evidence-based quality improvement methods for translating depression collaborative care research into practice. Fam Syst Health. 2010;28:91–113. doi: 10.1037/a0020302. [DOI] [PubMed] [Google Scholar]
- 36.Sharpe M, Walker J, Holm Hansen C, Martin P, Symeonides S, Gourley C, et al. Integrated collaborative care for comorbid major depression in patients with cancer (SMaRT Oncology-2): a multicentre randomised controlled effectiveness trial. Lancet. 2014;384:1099–108. doi: 10.1016/S0140-6736(14)61231-9. [DOI] [PubMed] [Google Scholar]
- 37.Walker J, Hansen CH, Martin P, Symeonides S, Gourley C, Wall L, et al. Integrated collaborative care for major depression comorbid with a poor prognosis cancer (SMaRT Oncology-3): a multicentre randomised controlled trial in patients with lung cancer. Lancet Oncol. 2014;15:1168–76. doi: 10.1016/S1470-2045(14)70343-2. [DOI] [PubMed] [Google Scholar]
- 38.Dobkin RD, Menza M, Allen LA, Gara MA, Mark MH, Tiu J, et al. Cognitive-behavioral therapy for depression in Parkinson’s disease: a randomized, controlled trial. Am J Psychiatry. 2011;168:1066–74. doi: 10.1176/appi.ajp.2011.10111669. [DOI] [PMC free article] [PubMed] [Google Scholar]


