Abstract
Background
The burden of orthopaedic trauma in the developing world is substantial and disproportionate. SIGN Fracture Care International is a nonprofit organization that has developed and made available to surgeons in resource-limited settings an intramedullary interlocking nail for use in the treatment of femoral and tibial fractures. Instrumentation also is donated with the nail. A prospectively populated database collects information on all procedures performed using this nail. Given the challenging settings and numerous surgeons with varied experience, it is important to document adequate alignment and union using the device.
Questions/purposes
The primary aim of this research was to assess the adequacy of operative reduction of closed diaphyseal femur fractures using the SIGN interlocking intramedullary nail based on radiographic images available in the SIGN database. The secondary aims were to assess correlations between postoperative alignment and several associated variables, including fracture location in the diaphysis, degree of fracture site comminution, and time to surgery. The tertiary aim was to assess the functionality of the SIGN database for radiographic analyses.
Methods
A review of the prospectively populated SIGN database was performed for patients with a diaphyseal femur fracture treated with the SIGN nail, which at the time of the study totaled 32,362 patients. After study size calculations, a random number generator was used to select 500 femur fractures for analysis. Exclusion criteria included open fractures and those without radiographs during the early postoperative period. The following information was recorded: location of the fracture in the diaphysis; fracture classification (AO/Orthopaedic Trauma Association [OTA] classification); degree of comminution (Winquist and Hansen classification); time from injury to surgery; and patient demographics. Measurements of alignment were obtained from the AP and lateral radiographs with malalignment defined as deformity in either the sagittal or coronal plane greater than 5°. Measurements were made manually by the four study authors using on-screen protractor software and interobserver reliability was assessed.
Results
The frequency of malalignment greater than 5° observed on postoperative radiographs was 51 of 501 (10%; 95% CI, 6.5–11.5), and malalignment greater than 10° occurred in eight of 501 (1.6%) of the femurs treated with this nail. Fracture location in the proximal or distal diaphysis was strongly correlated with risk of malalignment, with an odds ratio (OR) of 3.7 (95% CI, 1.5–9.3) for distal versus middle diaphyseal fractures and an OR of 4.7 (95% CI, 1.9–11.5) for proximal versus middle fractures (p < 0.001). Time from injury to surgery greater than 4 weeks also was strongly correlated with risk of malalignment (p < 0.001). Inherent fracture stability, based on fracture site comminution as per the Winquist and Hansen classification (Class 0–1 stable versus 2–4 unstable) showed an OR of 2.3 (95% CI, 1.2–4.3) for malalignment in unstable fractures. Interobserver reliability showed agreement of 88% (95% CI, 83–93) and mean kappa of 0.81 (95% CI, 0.65–0.87). The SIGN database of radiographic images was found to be an excellent source for research purposes with 92% of reviewed radiographs of acceptable quality.
Conclusions
The frequency of malalignment in closed diaphyseal femoral fractures treated with the SIGN nail closely approximated the incidence reported in the literature for North American trauma centers. Increased time from injury to surgery was correlated with increased frequency of malalignment; as humanitarian distribution of the SIGN nail increases, local barriers to timely care should be assessed and improved as possible. Prospective clinical study with followup, despite its inherent challenges in the developing world, would be of great benefit in the future.
Level of Evidence
Level III, therapeutic study.
Introduction
There is an increasing epidemic of trauma in the developing world, and musculoskeletal morbidity takes a substantial and disproportionate human and economic toll [1, 5]. One of the most devastating and common traumatic injuries in the developing world is the long bone fracture. Until recently, the best option available for many long bone fractures in this setting was a substantial period of immobilization and traction, because there was limited access to the orthopaedic surgical resources considered common in the developed world [4]. SIGN Fracture Care International (also known as the Surgical Implant Generation Network, or SIGN), a nonprofit organization, has developed and donated an intramedullary and interlocked prosthesis known as the SIGN nail. This nail is designed for use in the femur and the tibia without the need for fluoroscopic imaging and allows for low-cost intramedullary fixation in resource-limited settings [14]. Implants and related materials are donated to affiliated hospital sites where SIGN-trained surgeons can treat long bone fractures with SIGN intramedullary prostheses without concern for device-related costs [14]. Training is didactic and practical and is done through either a site visit by a volunteer visiting a SIGN surgeon educator or through a surgeon visiting a SIGN educator regionally or at the SIGN headquarters in Richland, Washington. SIGN currently has greater than 250 sites in more than 50 countries where SIGN nails have become a mainstay of treatment used by local surgeons [14]. The SIGN nails have been approved by the FDA and have shown good clinical results in small clinical series [7, 12, 13]. The SIGN standard nail was designed and began use in 1999 and is a solid stainless steel nail with a 9° proximal bend and 1.5° distal bend, offered in 8 mm to 12 mm diameters and 280 mm to 420 mm lengths [14]. It is a utilitarian design and is used in the femur, tibia, and humerus in antegrade and retrograde approaches. Using a specially designed proximal jig and extended aiming arm, the nail is designed to be interlocked proximally and distally without fluoroscopic imaging [7, 14]. The nail is designed and manufactured in-house by SIGN in Richland, Washington, and the standard nail has now been joined by several other implants including the fin nail (which uses distal flanges in lieu of distal interlocked screws), a pediatric nail, and hip nails.
The SIGN standard nail has been used in more than 100,000 operations performed around the world [14]. The SIGN organization, its implants, and the many surgeons in low and middle-income countries now using their techniques and equipment have effectively and dramatically changed the treatment paradigm for long-bone fractures and serve as an example of successful disruptive innovation [6]. In the developing world where resources are limited, traditional clinical research using standard followup and clinical outcomes is extraordinarily difficult, if not impossible, and research in these countries is severely underrepresented in the literature [9]. Although logistically challenging, it is worth critically examining the outcomes of the SIGN nail thus far. Without predictable and standardized multicenter long-term clinical outcomes available, the best available objective postoperative evaluation tool for assessment of quality of surgical care in the SIGN database is the use of postoperative radiographs.
We therefore sought to assess the adequacy of operative reduction of closed diaphyseal femur fractures using the SIGN interlocking intramedullary nail. The secondary aims were to assess correlations between postoperative alignment and several associated variables, including fracture location in the diaphysis, degree of fracture site comminution, and time to surgery. The tertiary aim was to assess the functionality of the SIGN database for the purpose of retrospective radiographic analyses.
Materials and Methods
Study Design and Setting
A retrospective analysis of closed diaphyseal femur fractures was performed using the SIGN database. This online database was started in 2003 and is a prospectively populated clinical care database with anonymized data of nearly all patients treated with the SIGN nail. It includes patient demographics, specifications of the implant used, and preoperative and postoperative radiographs. The database currently has entries for greater than 75,000 patients [14]. It is one of the largest fracture or injury treatment databases focusing on low- and middle-income countries, and its completeness and clinical relevance have served as a model for other international trauma databases [2]. SIGN surgeons are required to upload preoperative and postoperative radiographs for their hospital to receive free replacement SIGN implants. For the purposes of this study, all anonymous data were accessed remotely from computers based at our institutions and using a secure login. Research ethics board approval was obtained at our institutions and there were no risks to patients in the study because all data were retrospective and already anonymous.
Participants and Study Subjects
Inclusion criteria included diaphyseal femur fractures (AO/Orthopaedic Trauma Association [OTA] classification 32) [8] and patients treated with the standard SIGN nail. Exclusion criteria included open fractures and patients who did not have postoperative radiographs or whose radiographs were not adequate for assessment. A total of 32,362 patients in the database at the time of the study met the inclusion criteria and exclusion criteria of open fractures. The exclusion criterion of appropriate imaging had to be applied after sampling because of the variability in uploaded imaging in the database.
Randomization
The study by Ricci et al. [11], which examined postoperative malalignment after intramedullary nailing of 374 femur fractures at a trauma center in the United States, served as a guide in the development of the study method. In determining sample size, we assumed a prevalence of malalignment of at least 8%, and that in a worst-case scenario 25% of radiographs would be unsuitable for analysis. With these conditions, the selected sample size of 500 gave probabilities between 0.89 and 1.00 of obtaining a CI half-width between 3% and 4%. Using a random number generator, 500 femur fractures of the available 32,362 closed diaphyseal femur fractures from the SIGN surgery database were sampled.
Description of Experiment, Treatment, or Surgery
All patients underwent treatment of their femoral fractures with a standard SIGN intramedullary nail inserted without the use of fluoroscopic imaging.
Variables, Outcome Measures, Data Sources, and Bias
Patient case data were accessed through the password-protected and anonymous SIGN online surgical database. Significant variability existed for image quality owing to quality of the radiographs and/or the uploaded image, which usually was a digital photograph taken of the radiograph. Postoperative radiographs were assessed and the following information analyzed and recorded: adequacy of radiographs (ie, the ability to assess the radiograph and make planned measurements); location of diaphyseal femur fracture (proximal versus middle versus distal third); fracture classification (AO/OTA classification) [8]; degree of comminution (Winquist and Hansen classification) [16]; antegrade versus retrograde nail; and alignment of the femur or fracture in the coronal and sagittal planes. Adequate reduction was defined as angles of 5° or less in the coronal and sagittal planes. Measurements were made using an on-screen protractor (Screen Protractor; Iconico Inc, New York, NY, USA) on the AP and lateral radiographs (Fig. 1). The on-screen protractor has extendable protractor arms and varying degrees of translucency, such that the protractor origin can be placed over the fracture site and the arms extended longitudinally along the axes of the femur proximal and distal to the fracture, and this therefore allows it to be used through an overlay technique on any digital radiographic image on screen.
Fig. 1.
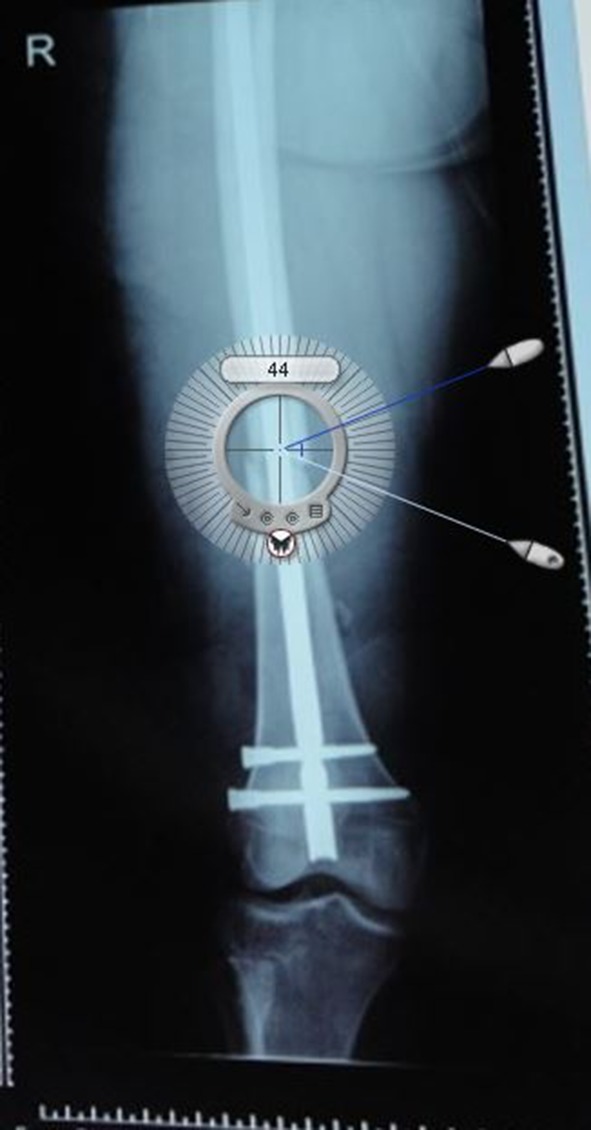
A representative postoperative image from the SIGN database shows a femur with the overlying image of the on-screen protractor used to measure angulation in our study.
Statistical Analysis and Study Size
The study sample size of 500 was divided by the four authors who each acted as independent raters, each planning for assessment of 125 independent femur fractures. To ensure standardization and reproducibility, interobserver reliability was assessed. Previous study of multirater alignment measurements in the femur showed an intraclass correlation coefficient (ICC) of 0.90 [10]. Based on these results we eschewed intraoberver analysis and performed sample size analysis for the interobserver reliability using the ICC of 0.90 and our total of four individual and independent raters to find that 25 cases reviewed by all four raters would allow an appropriate calculation of interobserver reliability. A total of 25 unique and random femur fractures were anonymized and read by all four study authors to allow for calculation of interobserver reliability. A multiple linear regression model and odds ratio (OR) calculations were used to assess the correlation between radiographic malalignment and the patient, fracture, and technique variables. Chi-square and Student’s t-test analyses also were performed.
Demographics and Description of Study Population
All patients were skeletally mature and underwent surgery for treatment of a diaphyseal femoral fracture. Because of the clinical setting(s), not all patients were treated for acute fractures. We also examined the effect of different treatment groups on clinical outcomes. Patients were grouped into four treatment groups based on clinical context to address our second research question (time to surgery variable): (1) acute: patients who received acute fracture care with the SIGN nail within 4 weeks of injury; (2) subacute: delayed treatment–patients who received their SIGN nail more than 4 weeks from the time of injury but less than 6 months and did not have a nonunion or another attempt at definitive treatment using a different surgical technique; (3) nonunion: treatment for a nonunion with date of injury more than 6 months from the SIGN nail; and (4) deformity: surgical treatment for well-established malunion or chronic deformity correction.
A total of 537 femur fractures were divided and analyzed by the four authors. Five hundred patients were assigned originally and because several patients had bilateral femur fractures, extra fractures were added to the study group. An additional 25 femur fractures were analyzed by all four authors for the purpose of assessing interobserver reliability. Of the 537 total femur fractures assessed, 36 (7%) either were mislabeled as femur fractures or did not have any available postoperative radiographs. There were eight femur fractures in which the radiographs were of such poor quality that measurement of postoperative alignment was impossible, leading to a total of 42 (8%) without imaging. Therefore, approximately 92% of the femur fractures had adequate imaging for assessment. The study population had a mean age of 33 years (range, 13–90 years), and was 77% male and 33% female. Treatment groups of the fractures were 71% (356/501) acute fractures, 14% (68/501) subacute, 13% (67/501) nonunions, and 2% (10/501) deformities or malunions. Fracture locations in the diaphysis were 89% (448/501) middle, 5% (26/501) proximal, and 5% (27/501) distal (Table 1). The fractures were classified according to the AO/OTA classification [8] and the most common class of fracture in the group was the simple transverse type, with more than 1/3 of all fractures in the study sample (Table 2).
Table 1.
Demographics of the study group
| Patient demographics | Number | Proportion |
|---|---|---|
| Total patients | 501 | |
| Male | 386 | 77% |
| Female | 115 | 23% |
| Average age (years) | 32.8 | |
| Treatment group demographics | ||
| Acute | 356 | 71% |
| Subacute | 68 | 14% |
| Nonunion | 67 | 13% |
| Deformity | 10 | 2% |
| Injury characteristics | ||
| Location (diaphyseal femur fracture) | ||
| Proximal | 26 | 5% |
| Middle | 448 | 89% |
| Distal | 27 | 5% |
| Winquist & Hansen classification | ||
| 0 | 185 | 37% |
| 1 | 144 | 29% |
| 2 | 63 | 13% |
| 3 | 51 | 10% |
| 4 | 39 | 8% |
Table 2.
AO/OTA fracture classification and risk of malalignment
| AO/OTA class | Total number | Malaligned fractures | Incidence of malalignment |
|---|---|---|---|
| 32-A1.1 | 4 | 0 | 0 |
| 32-A1.2 | 16 | 1 | 0.06 |
| 32-A1.3 | 1 | 1 | 1 |
| 32-A2.1 | 0 | 0 | 0 |
| 32-A2.2 | 63 | 8 | 0.13 |
| 32-A2.3 | 8 | 1 | 0.13 |
| 32-A3.1 | 7 | 2 | 0.29 |
| 32-A3.2 | 177 | 8 | 0.05 |
| 32-A3.3 | 10 | 1 | 0.1 |
| 32-B1.1 | 2 | 0 | 0 |
| 32-B1.2 | 25 | 3 | 0.12 |
| 32-B1.3 | 3 | 0 | 0 |
| 32-B2.1 | 3 | 0 | 0 |
| 32-B2.2 | 63 | 7 | 0.11 |
| 32-B2.3 | 4 | 0 | 0.00 |
| 32-B3.1 | 2 | 0 | 0.00 |
| 32-B3.2 | 33 | 2 | 0.06 |
| 32-B3.3 | 1 | 1 | 1.00 |
| 32-C1.1 | 6 | 1 | 0.17 |
| 32-C1.2 | 2 | 0 | 0 |
| 32-C1.3 | 3 | 0 | 0 |
| 32-C2.1 | 2 | 0 | 0 |
| 32-C2.2 | 12 | 3 | 0.25 |
| 3-C2.3 | 0 | 0 | 0 |
| 32-C3.1 | 5 | 0 | 0 |
| 32-C3.2 | 12 | 1 | 0.08 |
| 32-C3.3 | 8 | 2 | 0.25 |
| Total | 472 | 42 | 0.09 |
Results
Postoperative malalignment was observed in 10% of fractures assessed. The frequency of malalignment in either the coronal or sagittal plane greater than 5° on postoperative radiographs from all femur fractures was 51 of 501 (10%; 95% CI, 6.5–11.5). The frequency of malalignment greater than 10° was only eight of 501 (1.6%). Interobserver reliability showed agreement of 88% (95% CI, 83–93) and mean kappa of 0.81 (95% CI, 0.65–0.87).
Factors associated with malalignment included fracture location in either the proximal or distal diaphysis, degree of comminution, and time from injury to surgery greater than 4 weeks. Fracture types that had greater than average findings of postoperative malalignment included simple oblique fractures with fracture angulation greater than 30° (32-A2) and segmental fractures (32-C2). Inherent fracture stability, based on fracture site comminution per the Winquist and Hansen classification (Classes 0–1 stable versus 2–4 unstable) [16] showed an OR of 2.3 (95% CI, 1.2–4.3) for malalignment in unstable fractures (p < 0.01) (Table 3). Fracture location in the proximal or distal diaphysis was strongly correlated with risk of malalignment, with an OR of 3.7 (95% CI, 1.5–9.3) for distal versus middle diaphyseal fractures and an OR of 4.7 (95% CI, 1.9–11.5) for proximal versus middle fractures (p < 0.001) (Table 4). There was no difference in the rates of malalignment between antegrade versus retrograde nail insertion (p < 0.01). Time from injury to surgery greater than 4 weeks also was strongly correlated to risk of malalignment (p < 0.001) (Table 5). Patients receiving treatment acutely (< 4 weeks from the date of injury) had a risk of malalignment of 7%, whereas those treated subacutely (> 4 weeks) had a rate of 12%.
Table 3.
Fracture fragmentation and the risk of malalignment
| Winquist & Hansen classification | Number of fractures | Number of malaligned fractures | Incidence |
|---|---|---|---|
| 0 | 185 | 11 | 6% |
| 1 | 144 | 10 | 7% |
| 2 | 63 | 7 | 11% |
| 3 | 51 | 8 | 16% |
| 4 | 39 | 6 | 15% |
p < 0.01 = difference between Classes 0 and 1 vs 2, 3, and 4.
Table 4.
Fracture location and the risk of malalignment
| Fracture location | Number of fractures | Number of malaligned fractures | Incidence |
|---|---|---|---|
| Proximal | 26 | 7 | 27% |
| Middle | 448 | 37 | 8% |
| Distal | 27 | 7 | 26% |
p < 0.01 = difference between each fracture location.
Table 5.
Surgical timing and risk of malalignment
| Treatment group | Number of fractures | Number of malaligned fractures | Incidence |
|---|---|---|---|
| Acute | 356 | 25 | 7% |
| Subacute | 68 | 8 | 12% |
| Nonunion | 67 | 16 | 34% |
| Deformity | 10 | 2 | 20% |
p < 0.01 = difference between groups; acute = fractures treated within 4 weeks of injury; subacute = fractures treated greater than 4 weeks from injury, but less than 6 months; nonunion = fractures treated for established nonunions, greater than 6 months from injury; deformity = treatment for established malunion or chronic deformity.
The SIGN database was found to provide useful data for the purpose of retrospective radiographic research, as approximately 92% of the femur fractures had adequate imaging for assessment. However, clinical followup of fractures reviewed from the database revealed only 27% that had any charted followup in the database after discharge postsurgery. There was wide variation in followup rates between SIGN surgery sites. However, clinical followup was not found to be linked to radiographic postoperative malalignment (p = 0.15).
Discussion
The disproportionate human and economic toll of traffic injuries in low- and middle-income countries, with the majority of the world’s traumatic morbidity and mortality, was emphasized with the WHO and the United Nations declaring 2011 to 2020 the “Decade of Action for Road Safety” [17]. An unfortunate irony of the growth in musculoskeletal trauma in the developing world has been a worsening mismatch with inadequate health resources, and the SIGN organization has brought an innovative approach to their humanitarian mission of providing modern intramedullary nail technology to those who need it most. SIGN has had great clinical success thus far, but they also have had the foresight to develop and manage a database that allows robust pre- and postoperative patient information in the form of radiographs, allowing for the assessment of radiographic outcomes. The primary purpose of our study was to assess the adequacy of femoral fracture reduction through assessment of postoperative radiographic alignment, with a secondary goal of assessment for risk factors for postoperative malalignment.
A general limitation of the study was the variability and variable quality of the data available owing to the multicenter and multisurgeon nature of the SIGN database and the variability in their radiographic resources and image capture. The veracity of certain subjective elements of the database (ie, data fields entered directly by the surgical team) is difficult to assess, and we therefore sought to use the most objective part of the database: the radiographs. The most significant clinical weakness of the study was that it was not truly assessing the clinical outcome of the surgical intervention but only the immediate radiographic outcome. We could not account for true radiographic or clinical healing, infection, or other surgical complications. In the absence of those data, we thought postoperative radiographs were the best available objective measurement available that would allow comparison of alignment results using the SIGN nail with that using more sophisticated technology in North American trauma centers. Based on our assessment of radiographs in this study, we found that there was a small but substantial proportion (42 of 537; 8%) of logged cases that did not include proper orthogonal imaging or had poor quality images uploaded to the database that precluded full assessment. A potential source of bias in our study would be the understandable exclusion of fractures without adequate imaging for assessment. An important point to emphasize to SIGN surgeons in the future is the importance of taking and uploading representative coronal and sagittal images of postoperative radiographs. One possible limitation or source of bias could be the nature of the measurements of alignment or our multiple raters, although this potential limitation is likely not significant based on the findings by Owen et al. [10] when measuring femoral alignment among various raters. They reported very strong intra- and interobserver reliabilities in the assessment of malalignment of diaphyseal femur fractures with an ICC of 0.90 for varus and valgus angulation correlation, even among nonexperts, using a measurement protocol similar to the one used in our study; they concluded that a 5° measurement exceeded the variability in measurement. Our findings reflected similar results, with interobserver reliability showing agreement of 88% (95% CI, 83%–93%) and a mean kappa of 0.81 (95% CI, 0.65–0.87).
Using the most conservative definition of malalignment in the femur being anything greater than 5°, the SIGN nail showed an overall malalignment rate of 10%. In comparison, Ricci et al. [11] reported a malalignment rate of approximately 9% at a North American trauma center. When considering that the majority of the SIGN surgeries were performed without the benefit of fluoroscopy and in settings that are far from ideal from the perspective of developed countries, alignment results so closely approximating those of a Level I trauma center are a strong endorsement of the SIGN nail and instrumentation system. To properly compare the malalignment rate reported by Ricci et al. [11] with the rate for the SIGN nail, we must compare similar fracture and patient demographic groups. Treatment of femur fractures at a North American trauma center is almost exclusively performed during the first 4 weeks postinjury and most will be treated within hours to days. The same cannot be said for the SIGN cohort, many of whom experienced substantial delays to surgery. We found the frequency of malalignment in fractures treated during the first 4 weeks postinjury to be 7%. This was a more fitting comparison group and indicated that the SIGN nail had excellent immediate postoperative radiographic outcomes that were comparable to those found at a Level I trauma center in the United States, where Ricci et al. [11] reported postoperative malreduction in 9% of their study group, or 7% of stable fractures and 12% of unstable fractures. One likely factor in the impressively low frequency of malalignment in SIGN surgeries is that although the surgery can be performed without fluoroscopic imaging, the majority of the surgeries are performed using some measure of open reduction. Despite the use of adjunctive open reduction, infection rates in SIGN surgeries are within the acceptable norm and are more influenced by fracture characteristics and the use of preoperative antibiotics [19, 20].
Fracture characteristics noted to have increased frequency of angular malalignment included fractures in the proximal or distal diaphysis, of increased degree of comminution, and those of the subacute treatment group who were treated greater than 4 weeks from their date of injury. Ricci et al. [11] found similar results, with proximal and distal fracture location and comminution being risk factors for malalignment. The increased frequency of malalignment in patients treated more than 4 weeks from the date of injury is potentially indicative of operative issues associated with waiting for treatment. There is limited literature on risks of malalignment in this patient group, but the increased complexity and challenges involved in surgery for delayed union and aseptic nonunion in the femur is well documented [3, 15]. There are some centers in the developing world where such waits are common and the result of myriad factors. These findings should act as a reminder and impetus to ensure that centers around the world have access to intramedullary fixation for acute treatment of diaphyseal femur fractures. Of the variables found to be independently linked to malalignment, timing of surgery is the variable that we have the most control over as surgeons and surgical care advocates.
The SIGN nail and SIGN database show great promise and very encouraging results. Although the quality of the data in the database was generally good and has been shown to be valid for retrospective research and analysis [19], it could be improved. Our results show that most uploaded images were adequate, but not all. Most concerning is the relatively low rate of clinical followup information in the database, although in our study, lack of followup was not found to be linked to postoperative malalignment. It is important that the data populating the database be as accurate as possible. Appropriate orthogonal images make appropriate assessment much easier and more accurate. To facilitate postmarket research and evaluation, the improvement of data can and should be stressed. SIGN and its affiliated surgeons and hospitals continue to innovate in this realm as well, working on providing incentives for followup documentation. A recent prospective study highlighted, through meticulous followup, the various barriers to clinical followup in many developing regions, but also that clinicians and the SIGN database were capturing the patients with complications as these patients were more likely to return for followup appointments [18]. Developing trauma databases and registries in low- and middle-income countries is challenging, and although the SIGN surgery database is not a replacement for a proper registry, it is a valid and important aid in coordinating trauma care and resources in developing future registries [2, 19].
The frequency of malalignment in femoral fractures treated with the SIGN intramedullary nail closely approximated the incidence reported by Ricci et al. [11] for a North American trauma center. Independent risk factors for radiographic malalignment included the acuity of surgical treatment, degree of comminution, and location of the fracture in the diaphysis. The SIGN database was found to be a satisfactory resource for the purpose of retrospective radiographic research. This study provides support for the continued and expanded use of SIGN implants throughout the developing world and highlights an example of an organization that is using innovation in technology and care delivery to meet an overwhelming challenge. Future prospective clinical study with documented clinical outcomes would be of great benefit, and greater clinical and research resources are needed in the developing world as they deal with the growing problem of musculoskeletal trauma.
Acknowledgments
We thank Lewis Zirkle MD and the SIGN organization for providing access to their database. We also thank William Petrcich MSc and Timothy Ramsay PhD of the Ottawa Hospital Research Institute who provided invaluable methodologic and statistical guidance, analysis, and input. We also acknowledge and thank the many surgeons and surgical teams around the world who contribute to the orthopaedic care of patients in under-resourced regions and to the SIGN database.
Footnotes
One of the authors (SC) has received research support funding from the Orthopaedic Trauma Association in the form of a Peer-Reviewed Resident Research Grant supporting this research.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This study was performed at the Division of Orthopaedic Surgery, University of Ottawa, Ottawa, Ontario, Canada.
References
- 1.Beveridge M, Howard A. The burden of orthopaedic disease in developing countries. J Bone Joint Surg Am. 2004;86:1819–1822. doi: 10.2106/00004623-200408000-00029. [DOI] [PubMed] [Google Scholar]
- 2.Clough JF, Zirkle LG, Schmitt RJ. The role of SIGN in the development of a global orthopaedic trauma database. Clin Orthop Relat Res. 2010;468:2592–2597. doi: 10.1007/s11999-010-1442-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Finkemeier CG, Chapman MW. Treatment of femoral diaphyseal nonunions. Clin Orthop Relat Res. 2002;398:223–234. doi: 10.1097/00003086-200205000-00031. [DOI] [PubMed] [Google Scholar]
- 4.Gosselin RA, Heitto M, Zirkle LG. Cost-effectiveness of replacing skeletal traction by interlocked intramedullary nailing for femoral shaft fractures in a provincial trauma hospital in Cambodia. Int Orthop. 2009;33:1445–1448. doi: 10.1007/s00264-009-0798-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gosselin RA, Spiegel DA, Coughlin R, Zirkle LG. Injuries: the neglected burden in developing countries. Bull World Health Organ. 2009;87:246. doi: 10.2471/BLT.08.052290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hansen E, Bozic KJ. The impact of disruptive innovations in orthopaedics. Clin Orthop Relat Res. 2009;467:2512–2520. doi: 10.1007/s11999-009-0865-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ikem IC, Ogunlusi JD, Ine HR. Achieving interlocking nails without using an image intensifier. Int Orthop. 2007;31:487–490. doi: 10.1007/s00264-006-0219-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audigé L. Fracture and dislocation classification compendium–2007: Orthopaedic Trauma Association Classification, Database and Outcomes Committee. J Orthop Trauma. 2007;21(10 suppl):S1–S133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 9.Noordin S, Wright JG, Howard AW. Global relevance of literature on trauma. Clin Orthop Relat Res. 2008;466:2422–2427. doi: 10.1007/s11999-008-0397-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Owen JL, Stephens D, Wright JG. Reliability of radiographic measurement of fracture angulation in children with femoral shaft fractures. Can J Surg. 2007;50:115–118. [PMC free article] [PubMed] [Google Scholar]
- 11.Ricci WM, Bellabarba C, Lewis R, Evanoff B, Herscovici D, Dipasquale T, Sanders R. Angular malalignment after intramedullary nailing of femoral shaft fractures. J Orthop Trauma. 2001;15:90–95. doi: 10.1097/00005131-200102000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Sekimpi P, Okike K, Zirkle L, Jawa A. Femoral fracture fixation in developing countries: an evaluation of the Surgical Implant Generation Network (SIGN) intramedullary nail. J Bone Joint Surg Am. 2011;93:1811–1818. doi: 10.2106/JBJS.J.01322. [DOI] [PubMed] [Google Scholar]
- 13.Shah RK, Moehring HD, Singh RP, Dhakal A. Surgical Implant Generation Network (SIGN) intramedullary nailing of open fractures of the tibia. Int Orthop. 2004;28:163–166. doi: 10.1007/s00264-003-0535-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.SIGN Fracture Care International. Available at: http://signfracturecare.org/. Accessed May 3, 2014.
- 15.Webb LX, Winquist RA, Hansen ST. Intramedullary nailing and reaming for delayed union or nonunion of the femoral shaft: a report of 105 consecutive cases. Clin Orthop Relat Res. 1986;212:133–141. [PubMed] [Google Scholar]
- 16.Winquist RA, Hansen ST., Jr Comminuted fractures of the femoral shaft treated by intramedullary nailing. Orthop Clin North Am. 1980;11:633–648. [PubMed] [Google Scholar]
- 17.World Health Organization. Decade of Action for Road Safety 2011–2020: global launch. http://www.who.int/roadsafety/publications/decade_launch/en/. Accessed March 21, 2015.
- 18.Young S, Banza LN, Hallan G, Beniyasi F, Manda KG, Munthali BS, Dybvik E, Engesæter LB, Havelin LI. Complications after intramedullary nailing of femoral fractures in a low-income country. Acta Orthop. 2013;84:460–467. doi: 10.3109/17453674.2013.850014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Young S, Lie SA, Hallan G, Zirkle LG, Engesæter LB, Havelin LI. Low infection rates after 34,361 intramedullary nail operations in 55 low- and middle-income countries: validation of the Surgical Implant Generation Network (SIGN) online surgical database. Acta Orthop. 2011;82:737–743. doi: 10.3109/17453674.2011.636680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Young S, Lie SA, Hallan G, Zirkle LG, Engesæter LB, Havelin LI. Risk factors for infection after 46,113 intramedullary nail operations in low- and middle-income countries. World J Surg. 2013;37:349–355. doi: 10.1007/s00268-012-1817-4. [DOI] [PMC free article] [PubMed] [Google Scholar]


