Abstract
Background
Lactoferrin, an iron-binding glycoprotein which belongs to the transferrin family, has been shown to promote bone growth. However, reports regarding effects of lactoferrin on bone regeneration during distraction osteogenesis are limited. Our study was designed to investigate the effect of bovine lactoferrin treatment on bone formation of the distracted callus.
Questions/purposes
We asked whether bovine lactoferrin enhances bone formation of the distraction callus as determined by (1) radiographic and histologic appearances; (2) dual-energy x-ray absorptiometry (DXA) analysis of bone mineral composition and bone mineral density; (3) micro-CT measures of trabecular architecture; and (4) biomechanical strength of the healing bone. Additionally, serology, reverse transcription (RT)-PCR, and immunohistochemistry were used to explore the possible mechanisms of bovine lactoferrin use on bone formation during distraction osteogenesis.
Methods
Unilateral tibial osteodistraction was performed on 80 New Zealand White rabbits with a distraction rate of 1 mm per day for 10 days. Animals then were divided randomly into two groups: (1) vehicle and (2) bovine lactoferrin. At 4 and 8 weeks after completion of distraction, the animals were sacrificed. Lengthened tibias and serum samples were obtained and subjected to radiologic, DXA, micro-CT, histologic, and biomechanical examinations, and serum, RT-PCR and immunohistochemical analyses.
Results
Radiologic, DXA, micro-CT, histologic, and biomechanical examinations indicated that bovine lactoferrin treatment not only accelerated bone formation at early stages of distraction osteogenesis but also promoted bone consolidation at late stages. The ultimate force of the distracted calluses was increased by 37% (118.8 ± 6.65 N in the lactoferrin group and 86.5 ± 5.47 N in the vehicle group; p < 0.001) and 84% (384.8 ± 18.4 N in the lactoferrin group and 209.0 ± 15.2 N in the vehicle group; p < 0.001) at 4 and 8 weeks, respectively. Moreover, serum analysis showed that bovine lactoferrin treatment significantly increased serum levels of bone alkaline phosphatase and decreased serum levels of tartrate resistant acid phosphatase 5b. In addition, RT-PCR and immunohistochemical analyses suggested that bovine lactoferrin treatment induced a lower receptor activator of nuclear factor-kappaB (RANK) ligand/osteoprotegerin (RANKL/OPG) ratio in the distracted callus.
Conclusions
The results of our study suggest that bovine lactoferrin treatment could promote bone regeneration during distraction osteogenesis in the rabbit. The results indicate that the OPG/RANKL/RANK system might be a major mechanism for increased bone formation and decreased bone resorption in distraction osteogenesis with bovine lactoferrin treatment.
Clinical Relevance
Oral administration of bovine lactoferrin may provide a feasible approach for promoting osteogenesis during distraction osteogenesis.
Introduction
Distraction osteogenesis is characterized by the formation of new bone between two osteotomized bone segments which are separated by gradual traction. As a well-established surgical technique, distraction osteogenesis has been widely used in the treatment of limb-length discrepancies, bone defects after trauma, infection, tumor resection, and in various structural bone deformities [1]. Distraction osteogenesis consists of three stages: the latency stage after osteotomy and application of the external fixator; the distraction stage in which the separated bone ends are gradually and continuously distracted; and the consolidation stage [14, 15]. Although distraction osteogenesis has revolutionized the treatment of many orthopaedic conditions, one major limitation of the technique is that the completed process (when new bone formation and consolidation reach a level of sufficient strength for weightbearing) requires a period of months to years [26].
Various approaches have been studied to accelerate the process of bone formation and consolidation in distraction osteogenesis including low-intensity pulsed ultrasound [5], systemic use of bisphosphonates [10] and parathyroid hormone [17], local application of various potent bone anabolic agents such as BMPs [22, 23], VEGF [25], transforming growth factor-β [29], basic fibroblast growth factor [16], IGF-1 [30], and platelet-rich plasma [20], and local transplantation of bone mesenchymal stem cells [28, 31] and gene therapy [12]. However, the effects of these approaches on distraction osteogenesis remain controversial and none of the interventions has proven to be clinically effective. Therefore, a new approach is needed to promote bone formation during distraction osteogenesis.
Lactoferrin is an 80 kDa iron-binding glycoprotein which belongs to the transferrin family. Lactoferrin is present in many physiologic exocrine secretions, especially in milk and colostrum, and in the secondary granules of neutrophils [7]. In healthy individuals, serum levels of lactoferrin, which are predominantly neutrophil-derived, are 2 to 7 g/mL; thus, inflammation can lead to a higher local concentration of lactoferrin [19]. As an iron chelator, lactoferrin has antimicrobial activity. It also affects cell proliferation and differentiation [34], endothelial cell adhesion [18], myelopoiesis [2], embryonic development [33], cytokine and chemokine production [6], regulation of the inflammatory response [21], and modulation of the immune system [27].
Lactoferrin also was reported to promote bone growth [24]. It can promote bone formation by stimulating proliferation and differentiation of osteoblasts and by inhibiting osteoblast apoptosis. However, it can inhibit bone resorption by reducing osteoclast formation.
Owing to the dual functions of lactoferrin on bone metabolism, we designed our study to investigate the effects of orally administered bovine lactoferrin on tibial distraction osteogenesis in a rabbit model. We asked whether bovine lactoferrin enhances bone formation of the distraction callus as determined by (1) radiographic and histologic appearances; (2) dual-energy x-ray absorptiometry (DXA) analysis of bone mineral composition and bone mineral density; (3) micro-CT measures of trabecular architecture; and (4) biomechanical strength of the healing bone. Additionally, serology, reverse transcription (RT)-PCR, and immunohistochemistry were used to explore the possible mechanisms of bovine lactoferrin on bone formation during distraction osteogenesis.
Materials and Methods
Animals
Eighty adult male New Zealand White rabbits (2.5–3.0 kg) were used in our study. All animals were housed separately in standard cages in a temperature-controlled room (20°–22° C), with free access to food and water. All procedures of the study design were approved by the Animal Ethics Committee of Sichuan University.
Distraction Procedures and Intervention Protocol
A longitudinal incision was made on the skin of the medial aspect of the right tibia of the rabbit. After the muscles had been carefully separated from the periosteum, the anterior medial surface of the tibia was exposed. Four titanium half-pins (1.5 mm diameter × 40 mm length) were inserted in the tibial shaft perpendicular to its long axis across both cortices after predrilling the bone holes with a burr. Then a custom-made titanium external distractor was secured to the four titanium half-pins. A transverse osteotomy was made using an ultrafine drill-bit under constant irrigation between the second and third half-pins, just below the tibiofibular junction. Finally, the periosteum, muscles, and skin were sutured, respectively. Distraction was commenced 7 days after surgery at a rate of 0.5 mm every 12 hours for 10 days. In total, each tibia was lengthened by 10 mm.
After surgery, the rabbits were randomly divided in two groups: the vehicle (n = 36) and the bovine lactoferrin (n = 36) (Fig. 1). From the beginning of distraction until the rabbits were euthanized, the bovine lactoferrin-treated rabbits received, orally via intubation, bovine lactoferrin (Wako Pure Chemicals Industries Ltd; Osaka, Japan) that was dissolved in 0.9% physiologic saline at the designed dose (85 mg/kg) every day, according to a previous study [9], while the rabbits in the vehicle group received, orally via intubation, a dose of 1 mL/kg daily with 0.9% physiologic saline. Eighteen animals in each group were sacrificed with an overdose of pentobarbital (150 mg/kg) at 4 weeks and 8 weeks after completion of distraction, at which time the lengthened tibias and serum samples were obtained.
Fig. 1.
A schema of our study design and the number of animals involved at each stage is shown. DXA = dual dual-energy x-ray absorptiometry; RT-PCT = reverse transcription-polymerase chain reaction.
Radiographic and DXA Examinations
AP view radiographs of the lengthened tibias were used to qualitatively evaluate macroscopic evidence of bone formation and sclerosis. The lengthened tibias were placed on a customized platform and the x-ray unit (DENSOMAT; Gendex™ Dental Systems, Hatfield, PA, USA) was positioned 30 cm from samples. The machine settings were fixed at 46 kV and 7 mA, with a 0.06-ms exposure time.
After radiographic documentation, the distractor was carefully removed and the lengthened tibias were stripped of soft tissues. Bone mineral density and composition were measured using DXA analysis (Lunar iDXA™; GE Healthcare Lunar, Fairfield, CT, USA) under the small-animal scan mode. The lengthened tibias were placed in deionized water in the same position used for radiographic scans. To record bone mineral composition and density, a region of interest was drawn to include only the mineralized tissue in the distraction gap. The same region of interest (midshaft tibia) of the nonoperated contralateral tibia was measured as a normal control.
Micro-CT Analysis
Before micro-CT analysis, specimens were dissected between the second and third pin holes, which included approximately 5 mm of the proximal and distal original bone and approximately 10 mm of the distracted callus. The specimens were placed in a 17-mm-diameter holder filled with 70% ethanol and subjected to examination at a resolution of 10 μm using a μ-CT 80 scanner (55 kV, 145 mA, 700 ms integration time; Scanco Medical, Bassersdorf, Switzerland). We obtained more than 1000 images with a resolution of 2048 × 2048 pixels of the scanned region. The region of interest was defined as the distracted area located between the two ends of the fractured bone. In the region of interest, the medullary canal volume was excluded from evaluation; after segmentation, the following parameters were calculated in the new-formed bone tissues according to a previous study [8]: bone volume fraction, trabecular number, trabecular thickness, and trabecular separation. The bone volume fraction represented the portion of mineralized tissue, while trabecular number, thickness, and separation provided detailed information regarding the amount, thickness, and organization of trabeculae.
Histologic Examination
Histologic examination also was conducted to qualitatively evaluate bone formation and remodeling of the distracted callus. Specimens were fixed overnight in 4% paraformaldehyde solution and then rapidly decalcified in 14.5% EDTA buffer (pH = 7.2) for 6 weeks at room temperature. After decalcification, the specimens were washed, dehydrated in gradient alcohol, embedded in paraffin wax, and cut into sections (5 μm in thickness) through the long axis with a SP1600 microtome (Leica Biosystems, Wetzlar, Germany). Finally, the sections were stained with hematoxylin and eosin and examined qualitatively under light microscopy (Eclipse 80i; Nikon, Tokyo, Japan).
Biomechanical Assessment
A three-point bending test was chosen for biomechanical assessment of the distracted calluses, using an electronic materials testing system (Instron® 5566; Instron®, Norwood, MA, USA). Briefly, a specimen was placed on its posterior surface, resting on a supported bending apparatus with two supports that lay 10 mm apart. The tested specimen area was defined as the region of the distracted callus. Using a loading nose at the mid-point between the two supports, a force then was exerted on the distracted callus at a rate 5 mm/minute until failure. Specimens were kept moist throughout testing with 4% paraformaldehyde solution. Force versus displacement was recorded during testing and the ultimate force was taken as the force at the point of fracture of the specimen.
Serum Analysis
Serum levels of bone alkaline phosphatase (BALP) and tartrate-resistant acid phosphatase 5b (TRAP 5b) were measured to assess systemic bone turnover after distraction osteogenesis with bovine lactoferrin treatment. The serum samples were stored at −80° C until analysis. Total BALP and TRAP 5b levels were examined in the serum samples to study the biochemical markers of bone turnover. Serum levels of BALP and TRAP 5b were measured by ELISA (rabbit BALP and TRAP5b ELISA kits; R&D, Minneapolis, MN, USA), according to the manufacturer’s instructions.
RT-PCR Analysis
Total RNA was isolated from the distracted calluses using TRIzol® reagent (Life Technologies, Grand Island, NY, USA), according to the manufacturer’s protocol, and the RNA then was reverse transcribed into complementary DNA. The specific primers used for PCR were: forward primer 5′-AACCCCAGAGCGAAATAC-3′ and reverse primer 5′-AAGAATGCCTCCTCACAC-3′ for osteoprotegerin (OPG); forward primer 5′-GGTTCCCATAAAGTGAGTCTGT-3′ and reverse primer 5′-TTAAAAGCCCCAAAGTATGTT-3′ for receptor activator of nuclear factor-kappaB ligand (RANKL); forward primer 5′-TCACCATGGATGATGATATCGC-3′; and reverse primer 5′-CGTGCTCGATGGGGTACTTCA-3′ for β-actin. The PCR reaction was performed using an Applied Biosystems® ABI Prism 7300 system (Life Technologies) and the PCR products were fractionated using 1% agarose gel electrophoresis. The comparative Ct method was used to calculate the relative expression levels, with the levels of each target gene normalized to β-actin.
Immunohistochemical Analysis
Expression of OPG and RANKL in the distraction gap were further detected by immunohistochemistry. Primary antibodies against OPG and RANKL were obtained from Abcam® plc (Cambridge, UK). Immunohistochemical staining of OPG and RANKL was performed according to the manufacturer’s suggested instructions. In brief, tissue sections were washed in phosphate-buffered saline and immersed in 0.3% Tween™ 20 (Thermo Fisher Scientific Inc, Grand Island, NY, USA) for 1 hour. Slides then were incubated with the primary antibody. After washing in phosphate buffered saline, sections were incubated with the horseradish peroxidase-labeled secondary antibody (Abcam® plc). Color (brown) development was performed using 0.5 mg/mL 3,3′-diaminobenzidine tetrahydrochloride. Negative control staining was performed using phosphate buffered saline instead of the primary antibody.
Statistical Analyses
All results, expressed as mean ± SD, were performed using SPSS 17.0 (SPSS Inc, Chicago, IL, USA). For the parameters of micro-CT and biomechanical assessment, one-way ANOVA was performed to detect differences between the groups. Comparisons were significant when p was less than 0.05.
Results
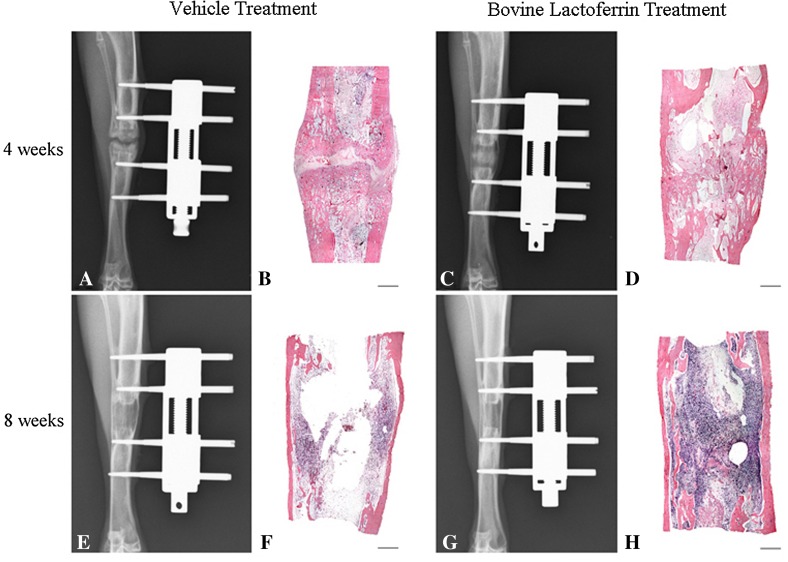
Radiographic results revealed that at 4 weeks, there were two sclerotic zones proximally and distally adjacent to the central radiolucent zone in the vehicle group, while the central radiolucent zone was already undetectable in the bovine lactoferrin group (Fig. 2). At 8 weeks, the lengthened tibial segment in both groups showed a tubular bone structure with a new cortex. However, compared with the vehicle group, the radiodensity and cortex of the distracted calluses were much higher and thicker in the bovine lactoferrin group (Fig. 2).
Fig. 2A–H.
A representative (A) AP radiograph and (B) a histologic photomicrograph of distracted calluses at 4 weeks for the vehicle group are shown. (C) The AP radiograph and (D) photomicrograph for the bovine lactoferrin group at 4 weeks also are shown. A representative (E) AP radiograph and (F) a photomicrograph for the vehicle group at 8 weeks are shown. (G) The AP radiograph and (H) photomicrograph for the bovine lactoferrin group at 8 weeks also are shown. (Stain, hematoxylin & eosin; bar = 1 mm).
Histologic evaluation of optical imaging revealed that at 4 weeks bone formation was sparse and focal defects were seen in the distracted calluses of the vehicle group, while the distraction gap of the bovine lactoferrin group was partially bridged with trabacular bone (Fig. 2). At 8 weeks, complete bony continuity and recanalization of the marrow cavity were observed in the distraction gap of both groups. However, a more thick and robust structure was found in the newly formed cortical bone at the lengthening site of the bovine lactoferrin group, whereas a thinner, more fragile structure was observed in the vehicle group (Fig. 2).
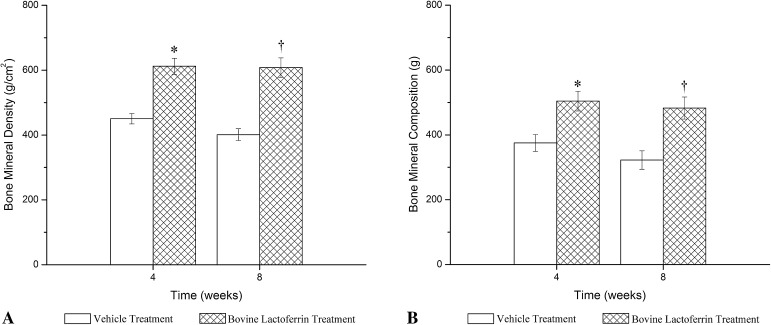
DXA examinations of the distracted calluses revealed that from 4 to 8 weeks, bone mineral density values of the regenerated zone remained stable in the bovine lactoferrin group (612.0 ± 24.6, 608.0 ± 30.0, respectively; 95% CI, −31.29 to 39.29; p = 0.81), but decreased in the vehicle group (450.5 ± 16.2, 401.0 ± 18.3, respectively; 95% CI, 27.25–71.75; p = 0.001). Moreover, bone mineral density values of the bovine lactoferrin group increased by 35.8% at 4 weeks (612.0 ± 24.6, 450.5 ± 16.2, respectively; 95% CI, −188.29 to −134.71; p < 0.001) (Fig. 3A) and by 51.6% at 8 weeks compared with values of the vehicle group (608.0 ± 30.0, 401.0 ± 18.3, respectively; 95% CI, −238.97 to −175.03; p < 0.001) (Fig. 3A). The bone mineral composition values measured by DXA were similar to the density results (Fig. 3B); however, no differences were detected between groups in the density or composition results of the nonoperated contralateral tibia (data not shown).
Fig. 3A–B.
Bone mineral (A) density (g/cm2) and (B) composition (g) values of the distracted calluses measured by DXA for the two groups at 4 and 8 weeks are shown. Data are expressed as mean ± SD; *p < 0.05; †p < 0.05; DXA = dual-energy x-ray absorptiometry.
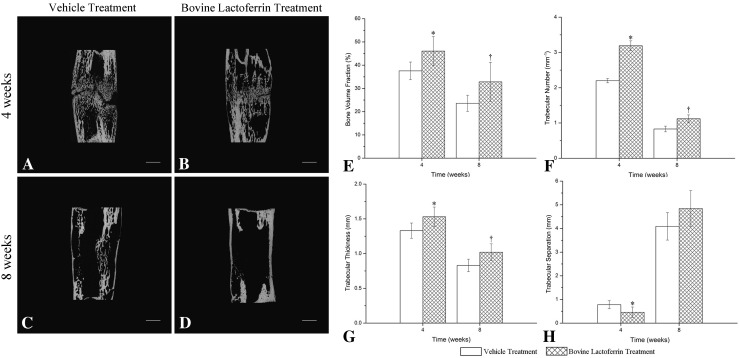
Representative three-dimensional reconstructed images of the distracted calluses from both groups indicated microstructural differences in the distraction gap between the two groups (Fig. 4A–D). Moreover, there were differences in the quantitative results of the distracted calluses from micro-CT analysis between the two groups. At 4 weeks, the data from the vehicle group were: bone volume fraction (37.55% ± 3.81%), trabecular number (2.20 ± 0.06 mm−1), trabecular thickness (1.33 ± 0.11 mm), and trabecular separation (0.78 ± 0.17 mm). In contrast, the bovine lactoferrin group showed increased values of bone volume fraction (46.06% ± 6.26%, 37.55% ± 3.81%, respectively; 95% CI, −15.17 to −1.84; p = 0.017) (Fig. 4E), trabecular number (3.19 ± 0.14 mm−1, 2.20 ± 0.06 mm−1, respectively; 95% CI, −1.13 to −0.85; p < 0.001) (Fig. 4F), and trabecular thickness (1.53 ± 0.14 mm, 1.33 ± 0.11 mm, respectively; 95% CI, −0.35 to −0.03; p = 0.025) (Fig. 4G), and a decrease in trabecular separation (0.46 ± 0.22, 0.78 ± 0.17 mm, respectively; 95% CI, 0.06–0.57; p = 0.019 (Fig. 4H). At 8 weeks, values of bone volume fraction, trabecular number, and trabecular thickness also were higher in the bovine lactoferrin group than in the vehicle group (p < 0.05, respectively), but trabecular separation levels did not differ between the two groups (p = 0.085) (Fig. 4E–H).
Fig. 4A–H.
The coronal micro-CT slices through the center of the distracted calluses are shown for (A) vehicle treatment and (B) bovine lactoferrin treatment at 4 weeks, and (C) vehicle treatment and (D) bovine lactoferrin treatment at 8 weeks. Bar = 1 mm. The quantitative results of micro-CT analysis at 4 and 8 weeks are expressed as (E) bone volume fraction, (F) trabecular number, (G) trabecular thickness, and (H) trabecular separation. The error bars mark the SD.
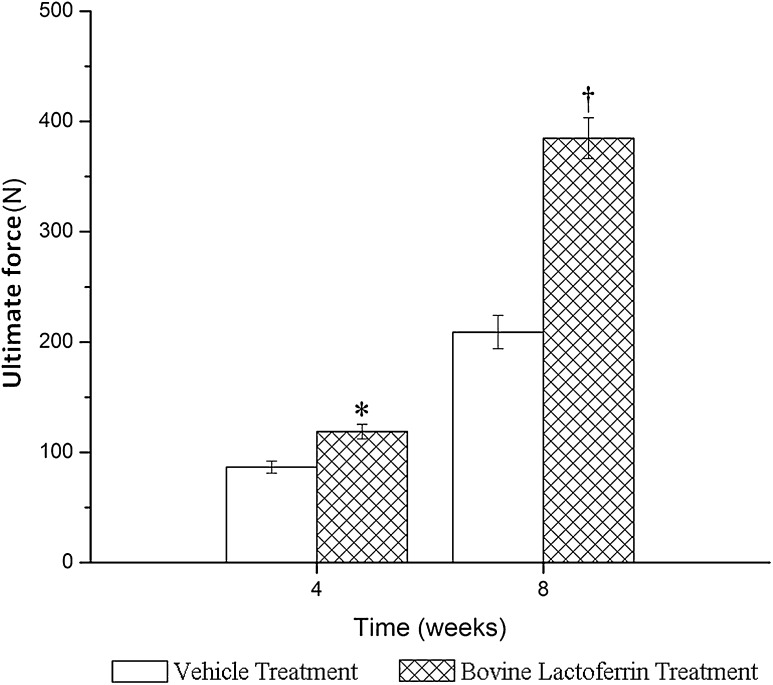
At 4 weeks, the mean value of ultimate force of the distracted calluses in the bovine lactoferrin group was 118.8 ± 6.65 N, which was approximately 1.37-fold greater than that in the vehicle group (118.8 ± 6.65, 86.5 ± 5.47, respectively; 95% CI, −40.16 to −24.50; p < 0.001) (Fig. 5). Similarly, the mean value of ultimate force in the bovine lactoferrin group at 8 weeks remained higher (1.84-fold) compared with the vehicle group (384.8 ± 18.4, 209.0 ± 15.2, respectively; 95% CI, −197.53 to −154.14; p < 0.001) (Fig. 5).
Fig. 5.
The ultimate force of the distracted callus as measured during a three-point bending test is shown. Data are expressed as mean ± SD; *p < 0.05; p < 0.05.
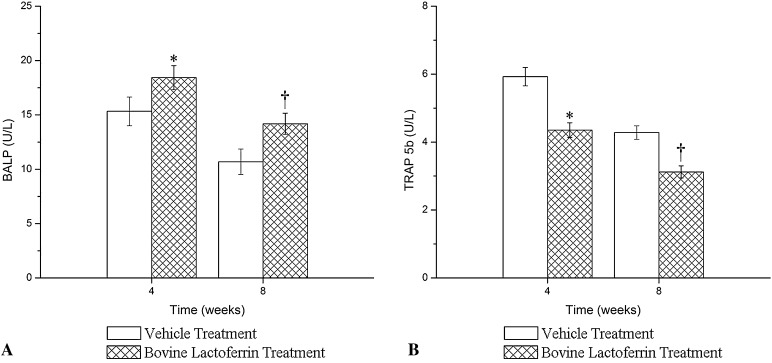
At 4 and 8 weeks compared with the vehicle group, serum levels of BALP in the bovine lactoferrin group were increased by 32.6% and 20.2% respectively (both p < 0.05), whereas serum levels of TRAP 5b in the bovine lactoferrin group were decreased by 36.3% and 37.2% respectively (both p < 0.05) (Fig. 6).
Fig. 6A–B.
The (A) effects of bovine lactoferrin treatment on serum levels of BALP and (B) TRAP 5b levels are shown. Data are expressed as mean ± SD; *p < 0.05; †p < 0.05; BALP = bone alkaline phosphatase; TRAP = tartrate resistant acid phosphatase.
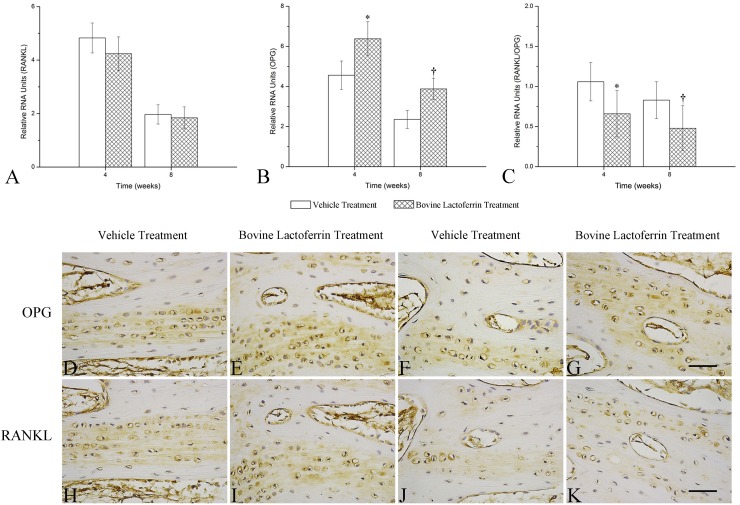
Data from RT-PCR revealed that bovine lactoferrin treatment not only increased the expression level of OPG mRNA but also slightly decreased the expression level of RANKL mRNA in the distraction gap, leading to a lower RANKL/OPG ratio in the distracted calluses of the bovine lactoferrin group compared with the vehicle group (p < 0.05) (Fig. 7A–C). Bovine lactoferrin treatment led to an increase in the number of OPG-positive staining cells in the distracted callus; however, no difference was detected regarding the number of RANKL-positive staining cells in the distraction gap between the two groups (Fig. 7D–K). These results also indicated that the RANKL/OPG ratio was decreased in the distracted calluses with bovine lactoferrin treatment, which was consistent with the data of the RT-PCR analysis.
Fig. 7A–K.
The effects of bovine lactoferrin treatment on (A) RANKL and (B) OPG mRNA expression and (C) RANKL/OPG ratio in the distraction gap are shown. Relative levels measured by reverse transcription-PCR are shown; error bars = SD. Immunohistochemical detection of OPG for (D) vehicle and (E) bovine lactoferrin treatments at 4 weeks, and (F) vehicle and (G) bovine lactoferrin treatments at 8 weeks are shown. RANKL expression in the distracted calluses also is shown for (H) vehicle and (I) bovine lactoferrin treatments at 4 weeks, and (J) vehicle and (K) bovine lactoferrin treatments at 8 weeks. Bar = 400 mm; RANK = receptor activator of nuclear factor-kappaB; RANKL = receptor activator of nuclear factor-kappaB ligand; OPG = osteoprotegerin.
Discussion
The purpose of our study was to investigate the effects of bovine lactoferrin treatment on bone regeneration in distraction osteogenesis. Results from radiologic, histologic, DXA, micro-CT, and biomechanical examinations revealed that at 4 weeks after completion of distraction, bovine lactoferrin treatment not only increased bone mineral density and composition but also induced better micro-CT values and biomechanical strength, indicating that bovine lactoferrin treatment accelerated bone formation at an early stage of distraction osteogenesis. At 8 weeks after completion of distraction, bovine lactoferrin treatment still increased bone mineral density and composition and also improved callus microstructure and enhanced healing strength, thus leading to qualitatively improved radiologic and histologic morphologic features of the distracted calluses. This suggests that bovine lactoferrin treatment promoted bone consolidation at a late stage of distraction osteogenesis. Overall, our study showed that oral administration of 85 mg/kg/day bovine lactoferrin could promote bone regeneration after tibial distraction osteogenesis in a rabbit model.
Our study had several potential limitations. Based on the results of a previous study [32], bovine lactoferrin is easily degraded to digestive enzymes such as pepsin or trypsin, and only 60% of the intact lactoferrin enters the intestine after oral ingestion in human beings. In our study, the degradation and the absorption ratios of bovine lactoferrin that were applied via oral administration in rabbits were not examined. However, Iigo et al. [13] reported that bovine lactoferrin was not detectable in the portal blood of mice given an oral dose of 300 mg/kg bovine lactoferrin, suggesting that the lactoferrin was less likely to be transported from the intestine into the blood thereby interacting with bone-related cells directly when administered orally. We used a dose of 85 mg/kg/day of bovine lactoferrin, according to a previous report [9], however, the actual serum concentrations of bovine lactoferrin were not measured. A third potential limitation was that systemic treatment with bovine lactoferrin was reported to induce a sharp decrease in serum levels of calcium in animals [9], thus attention should be paid to the condition of blood electrolytes if systemic application of bovine lactoferrin is used clinically. Finally, physiologic conditions are different between rabbits and humans, and predicting the effects of bovine lactoferrin on distraction osteogenesis in humans from the results of rabbits should be made cautiously.
In this study, results from radiographic and histologic examinations showed that bovine lactoferrin treatment resulted in earlier bone mineralization and better new bone formation in the distracted callus. These results might be explained by the dual effects of bovine lactoferrin on bone formation and bone resorption. According to previous studies [4, 24], bovine lactoferrin treatment not only promotes bone formation through increasing the number of osteoblasts and enhancing the ability of the osteoblasts to synthesize and mineralize the bone matrix, but also inhibits bone resorption by reducing the number of osteoclasts formed from precursor cells.
The results from DXA examination revealed that at 4 and 8 weeks after completion of distraction, bone mineral density and composition values of the bovine lactoferrin group were significantly higher than those of the vehicle group (p < 0.05, respectively). Our results were consistent with those of previous studies [4, 9, 11] which indicated that dietary lactoferrin supplementation could have a beneficial effect on postmenopausal bone loss by modulating bone formation and resorption. Based on these results, it appears that promotion of bone formation and inhibition of bone resorption by bovine lactoferrin contributed to increased bone mineral density and composition of the distracted calluses.
Moreover, results from micro-CT analyses showed that significantly higher values of bone volume fraction and trabecular number and thickness were detected in the bovine lactoferrin group compared with the vehicle group at 4 and 8 weeks after completion of distraction, whereas a significantly lower value of trabecular separation was found in the bovine lactoferrin group compared with the vehicle group at 4 weeks but not at 8 weeks after completion of distraction. Overall, our results from the micro-CT analyses suggest that the structure and spatial configuration of trabecular bone in the distraction gap were prominently promoted with bovine lactoferrin treatment.
In addition, results from biomechanical assessment revealed that when compared with the vehicle group, increased values of ultimate force of the distracted calluses were detected in the bovine lactoferrin group at 4 and 8 weeks after completion of distraction (p < 0.05, respectively). Previous studies [4, 9] showed that bovine lactoferrin increased the parameters of mechanical strength in a dose-dependent manner, and our results agreed with these findings. The above results support that oral administration of bovine lactoferrin contributed to the accelerated biomechanical strength of the distracted calluses.
To address the issue of the mechanisms involved, we measured biochemical markers of bone turnover such as BALP and TRAP 5b. Results from serum analysis showed that compared with the untreated distraction osteogenesis group, systemic treatment with bovine lactoferrin significantly increased serum levels of BALP and decreased serum levels of TRAP 5b. Our results were consistent with those of previous studies [3, 9, 11] indicating that bovine lactoferrin treatment promoted the process of distraction osteogenesis by enhancing bone formation and reducing bone resorption. To further explore the possible mechanisms, we also detected the expression level of OPG and RANKL in the distraction gap. The results of RT-PCR and immunohistochemical analysis indicated that bovine lactoferrin treatment not only increased the expression level of OPG but also slightly decreased the expression level of RANKL in the distraction gap, leading to a significantly lower RANKL/OPG ratio in the distracted calluses compared with the untreated distraction osteogenesis group. Our results agree with those of previous studies [11, 35] indicating that the OPG/RANKL/RANK system might be a major mechanism for increased bone formation and decreased bone resorption in distraction osteogenesis using bovine lactoferrin treatment.
The results of our study showed that oral administration of bovine lactoferrin at a dose of 85 mg/kg/day could promote bone regeneration after tibial distraction osteogenesis in a rabbit model. Moreover, the OPG/RANKL/RANK system may be a major mechanism for increased bone formation and decreased bone resorption in distraction osteogenesis when bovine lactoferrin treatment is used. However, studies with different doses of bovine lactoferrin and longer treatment periods are needed to further determine the dose- and time-dependent effects of bovine lactoferrin on distraction osteogenesis.
Footnotes
The institution of one or more of the authors (JH) has received, during the study period, funding from the Foundation of Ministry of Education of China (Beijing, China).
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
The corresponding author certifies that his institution approved the animal protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Sichuan University, Chengdu, Sichuan, China.
References
- 1.Aronson J, Johnson E, Harp JH. Local bone transportation for treatment of intercalary defects by the Ilizarov technique: biomechanical and clinical considerations. Clin Orthop Relat Res. 1989;243:71–79. [PubMed] [Google Scholar]
- 2.Artym J, Zimecki M. The effects of lactoferrin on myelopoiesis: can we resolve the controversy? Postepy Hig Med Dosw (Online). 2007;61:129–150. [PubMed] [Google Scholar]
- 3.Bharadwaj S, Naidu AG, Betageri GV, Prasadarao NV, Naidu AS. Milk ribonuclease-enriched lactoferrin induces positive effects on bone turnover markers in postmenopausal women. Osteoporos Int. 2009;20:1603–1611. doi: 10.1007/s00198-009-0839-8. [DOI] [PubMed] [Google Scholar]
- 4.Blais A, Malet A, Mikogami T, Martin-Rouas C, Tome D. Oral bovine lactoferrin improves bone status of ovariectomized mice. Am J Physiol Endocrinol Metab. 2009;296:E1281–E1288. doi: 10.1152/ajpendo.90938.2008. [DOI] [PubMed] [Google Scholar]
- 5.Chan CW, Qin L, Lee KM, Zhang M, Cheng JC, Leung KS. Low intensity pulsed ultrasound accelerated bone remodeling during consolidation stage of distraction osteogenesis. J Orthop Res. 2006;24:263–270. doi: 10.1002/jor.20015. [DOI] [PubMed] [Google Scholar]
- 6.Cumberbatch M, Bhushan M, Dearman RJ, Kimber I, Griffiths CE. IL-1beta-induced Langerhans’ cell migration and TNF-alpha production in human skin: regulation by lactoferrin. Clin Exp Immunol. 2003;132:352–359. doi: 10.1046/j.1365-2249.2003.02146.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garcia-Montoya IA, Cendon TS, Arevalo-Gallegos S, Rascon-Cruz Q. Lactoferrin a multiple bioactive protein: an overview. Biochim Biophys Acta. 2012;1820:226–236. doi: 10.1016/j.bbagen.2011.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gerstenfeld LC, Sacks DJ, Pelis M, Mason ZD, Graves DT, Barrero M, Ominsky MS, Kostenuik PJ, Morgan EF, Einhorn TA. Comparison of effects of the bisphosphonate alendronate versus the RANKL inhibitor denosumab on murine fracture healing. J Bone Miner Res. 2009;24:196–208. doi: 10.1359/jbmr.081113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guo HY, Jiang L, Ibrahim SA, Zhang L, Zhang H, Zhang M, Ren FZ. Orally administered lactoferrin preserves bone mass and microarchitecture in ovariectomized rats. J Nutr. 2009;139:958–964. doi: 10.3945/jn.108.100586. [DOI] [PubMed] [Google Scholar]
- 10.Heidari P, Abbaspour A, Baghdadi T, Espandar R, Farzan M, Amanpour S, Rasouli MR, Mohagheghi MA, Amiri HR, Yasui N. Effect of risedronate on bone resorption during consolidation phase of distraction osteogenesis: a rabbit model. J Orthop Surg (Hong Kong). 2010;18:228–234. doi: 10.1177/230949901001800219. [DOI] [PubMed] [Google Scholar]
- 11.Hou JM, Xue Y, Lin QM. Bovine lactoferrin improves bone mass and microstructure in ovariectomized rats via OPG/RANKL/RANK pathway. Acta Pharmacol Sin. 2012;33:1277–1284. doi: 10.1038/aps.2012.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hu J, Qi MC, Zou SJ, Li JH, Luo E. Callus formation enhanced by BMP-7 ex vivo gene therapy during distraction osteogenesis in rats. J Orthop Res. 2007;25:241–251. doi: 10.1002/jor.20288. [DOI] [PubMed] [Google Scholar]
- 13.Iigo M, Kuhara T, Ushida Y, Sekine K, Moore MA, Tsuda H. Inhibitory effects of bovine lactoferrin on colon carcinoma 26 lung metastasis in mice. Clin Exp Metastasis. 1999;17:35–40. doi: 10.1023/A:1026452110786. [DOI] [PubMed] [Google Scholar]
- 14.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res. 1989;238:249–281. [PubMed] [Google Scholar]
- 15.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: Part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res. 1989;239:263–285. [PubMed] [Google Scholar]
- 16.Jiang X, Zou S, Ye B, Zhu S, Liu Y, Hu J. bFGF-Modified BMMSCs enhance bone regeneration following distraction osteogenesis in rabbits. Bone. 2010;46:1156–1161. doi: 10.1016/j.bone.2009.12.017. [DOI] [PubMed] [Google Scholar]
- 17.Kang SY, Deshpande SS, Donneys A, Rodriguez JJ, Nelson NS, Felice PA, Chepeha DB, Buchman SR. Parathyroid hormone reverses radiation induced hypovascularity in a murine model of distraction osteogenesis. Bone. 2013;56:9–15. doi: 10.1016/j.bone.2013.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim CW, Lee TH, Park KH, Choi SY, Kim J. Human lactoferrin suppresses TNF-alpha-induced intercellular adhesion molecule-1 expression via competition with NF-kappaB in endothelial cells. FEBS Lett. 2012;586:229–234. doi: 10.1016/j.febslet.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 19.Langhorst J, Elsenbruch S, Koelzer J, Rueffer A, Michalsen A, Dobos GJ. Noninvasive markers in the assessment of intestinal inflammation in inflammatory bowel diseases: performance of fecal lactoferrin, calprotectin, and PMN-elastase, CRP, and clinical indices. Am J Gastroenterol. 2008;103:162–169. doi: 10.1111/j.1572-0241.2007.01556.x. [DOI] [PubMed] [Google Scholar]
- 20.Latalski M, Elbatrawy YA, Thabet AM, Gregosiewicz A, Raganowicz T, Fatyga M. Enhancing bone healing during distraction osteogenesis with platelet-rich plasma. Injury. 2011;42:821–824. doi: 10.1016/j.injury.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 21.Legrand D. Lactoferrin, a key molecule in immune and inflammatory processes. Biochem Cell Biol. 2012;90:252–268. doi: 10.1139/o11-056. [DOI] [PubMed] [Google Scholar]
- 22.Li G, Bouxsein ML, Luppen C, Li XJ, Wood M, Seeherman HJ, Wozney JM, Simpson H. Bone consolidation is enhanced by rhBMP-2 in a rabbit model of distraction osteogenesis. J Orthop Res. 2002;20:779–788. doi: 10.1016/S0736-0266(01)00166-8. [DOI] [PubMed] [Google Scholar]
- 23.Mizumoto Y, Moseley T, Drews M, Cooper VN, 3rd, Reddi AH. Acceleration of regenerate ossification during distraction osteogenesis with recombinant human bone morphogenetic protein-7. J Bone Joint Surg Am. 2003;85(suppl 3):124–130. doi: 10.2106/00004623-200300003-00019. [DOI] [PubMed] [Google Scholar]
- 24.Naot D, Grey A, Reid IR, Cornish J. Lactoferrin: a novel bone growth factor. Clin Med Res. 2005;3:93–101. doi: 10.3121/cmr.3.2.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ochman S, Frey S, Raschke MJ, Deventer JN, Meffert RH. Local application of VEGF compensates callus deficiency after acute soft tissue trauma: results using a limb-shortening distraction procedure in rabbit tibia. J Orthop Res. 2011;29:1093–1098. doi: 10.1002/jor.21340. [DOI] [PubMed] [Google Scholar]
- 26.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 27.Puddu P, Valenti P, Gessani S. Immunomodulatory effects of lactoferrin on antigen presenting cells. Biochimie. 2009;91:11–18. doi: 10.1016/j.biochi.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 28.Qi MC, Zou SJ, Han LC, Zhou HX, Hu J. Expression of bone-related genes in bone marrow MSCs after cyclic mechanical strain: implications for distraction osteogenesis. Int J Oral Sci. 2009;1:143–150. doi: 10.4248/IJOS.09021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rauch F, Lauzier D, Travers R, Glorieux F, Hamdy R. Effects of locally applied transforming growth factor-beta1 on distraction osteogenesis in a rabbit limb-lengthening model. Bone. 2000;26:619–624. doi: 10.1016/S8756-3282(00)00283-0. [DOI] [PubMed] [Google Scholar]
- 30.Stewart KJ, Weyand B, van’t Hof RJ, White SA, Lvoff GO, Maffulli N, Poole MD. A quantitative analysis of the effect of insulin-like growth factor-1 infusion during mandibular distraction osteogenesis in rabbits. Br J Plast Surg. 1999;52:343–350. [DOI] [PubMed]
- 31.Sun Z, Tee BC, Kennedy KS, Kennedy PM, Kim DG, Mallery SR, Fields HW. Scaffold-based delivery of autologous mesenchymal stem cells for mandibular distraction osteogenesis: preliminary studies in a porcine model. PLoS One. 2013;8:e74672. doi: 10.1371/journal.pone.0074672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Troost FJ, Steijns J, Saris WH, Brummer RJ. Gastric digestion of bovine lactoferrin in vivo in adults. J Nutr. 2001;131:2101–2104. doi: 10.1093/jn/131.8.2101. [DOI] [PubMed] [Google Scholar]
- 33.Ward PP, Mendoza-Meneses M, Mulac-Jericevic B, Cunningham GA, Saucedo-Cardenas O, Teng CT, Conneely OM. Restricted spatiotemporal expression of lactoferrin during murine embryonic development. Endocrinology. 1999;140:1852–1860. doi: 10.1210/endo.140.4.6671. [DOI] [PubMed] [Google Scholar]
- 34.Yagi M, Suzuki N, Takayama T, Arisue M, Kodama T, Yoda Y, Otsuka K, Ito K. Effects of lactoferrin on the differentiation of pluripotent mesenchymal cells. Cell Biol Int. 2009;33:283–289. doi: 10.1016/j.cellbi.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 35.Yamano E, Miyauchi M, Furusyo H, Kawazoe A, Ishikado A, Makino T, Tanne K, Tanaka E, Takata T. Inhibitory effects of orally administrated liposomal bovine lactoferrin on the LPS-induced osteoclastogenesis. Lab Invest. 2010;90:1236–1246. doi: 10.1038/labinvest.2010.80. [DOI] [PubMed] [Google Scholar]