Abstract
Though exempted from national bans of tobacco smoking in hospitals, some psychiatric facilities have voluntarily gone 100% smoke free with little reported difficulty in clinical management. The impact of smoking restrictions on psychiatric patients’ thoughts about quitting smoking, however, is not known. This study investigates changes in thoughts about quitting smoking for patients hospitalized in a smoke-free psychiatric inpatient facility. Participants were 100 smokers recruited from a university-based adult inpatient psychiatry unit. The present study focused on participants’ reported desire to quit smoking, their expectancy of success and anticipated difficulty with quitting, and their smoking abstinence goal. Assessments were conducted at hospital intake and shortly before hospital discharge. Follow-up assessments were conducted by phone at 1 week, 1 month, and 3 months posthospitalization to measure smoking behavior. Although no cessation treatment was provided in this observational study, from admission to discharge, participants reported an increased expectancy of success with quitting and a decreased expectancy of difficulty with staying quit. They also were more likely to endorse a smoking-related goal. Psychiatric diagnosis was not related to thoughts about abstinence. Furthermore, participants’ thoughts about abstinence at discharge were significantly related to their subsequent smoking behavior. Hospitalization in a smoke-free environment is associated with increases in patients’ expectancies about quitting and staying smoke free.
Introduction
Rates of tobacco use are two to three times higher among individuals with psychiatric disorders relative to the general population (Lasser et al., 2000). Individuals with psychiatric disorders are estimated to make up 44%–46% of the U.S. tobacco market (Grant, Hasin, Chou, Stinson, & Dawson, 2004; Lasser et al., 2000). Particularly high rates of tobacco use have been reported among individuals with psychotic disorders, depression, and substance use disorders (Rohde, Lewinsohn, Brown, Gau, & Kahler, 2003).
In 1992, the Joint Commission on Accreditation of Healthcare Organizations (1992) banned smoking in all U.S. hospitals. Psychiatric inpatient units were exempt from this nationwide policy because of promoted beliefs that these patients need to smoke and fears that bans would lead to greater difficulty in patient management, use of restraint, as-needed medication use, and against-medical-advice discharges (e.g., Beemer, 1993; Ryabik, Lippman, & Mount, 1995; Taylor et al., 1993). The National Alliance on Mental Illness advocated strongly against smoking bans, promoting the argument for patients’ inalienable right to smoke (Psychiatric News, 1994). The culture of smoking, which has been a central part of the operation of psychiatric inpatient facilities throughout their history, has impeded efforts to transition to smoke-free policies, and to date, their implementation is fragmented and varies from complete smoking bans to various smoking allowances (Lawn & Pols, 2005).
Despite hesitations to ban smoking, experience consistently has shown these fears to be unwarranted. Among psychiatric hospitals that have elected to instate 100% smoking bans, few difficulties have been reported. A review of 22 studies involving smoking bans in psychiatric populations reported no major long-standing troublesome effects in terms of unrest or compliance (El-Guebaly, Cathcart, Currie, Brown, & Gloster, 2002). Another review of 26 studies reported that staff in the psychiatric facilities anticipated more smoking-related problems than occurred, and overall there were no increases in aggression, use of seclusion, discharge against medical advice, or as-needed medication use following the smoking bans (Lawn & Pols, 2005). The present study was designed to explore another potential consequence of hospitalization in a smoke-free environment: the consequential changes in patients’ thoughts about abstinence. For some patients, hospitalization in a smoke-free facility may provide an ideal and perhaps otherwise rare opportunity for an extended period of smoking abstinence, which may affect their thoughts about quitting smoking.
Thoughts about quitting smoking, such as confidence in one’s ability to successfully quit, may play a vital role in smoking behavior and relapse. Self-efficacy expectations, or one’s belief in his or her ability to change, have been proposed as the cornerstone of human agency (Bandura, 1977, 1997). Several theoretical models of smoking relapse support this assertion and highlight efficacy expectations as the key to explaining effortful behaviors (e.g., Marlatt & Gordon, 1985; Niaura, 2000). Empirical studies demonstrate that more confident individuals are more likely to try to quit smoking on their own or with treatment cessation interventions (Brod & Hall, 1984; Zentner & Borland, 1995), are more likely to quit successfully (Carey & Carey, 1993), and are less likely to relapse (e.g., Baer & Lichtenstein, 1988; DiClemente, 1981; Gwaltney et al., 2001).
Evidence suggests that self-efficacy is context and time specific (e.g., Gwaltney et al., 2002; Gwaltney, Shiffman, & Sayette, 2005). That is, efficacy expectations may be shaped and changed by direct life experiences. The present study explicitly investigates the changes in efficacy expectations that are associated with smoking abstinence related to psychiatric hospitalization in a smoke-free environment.
Commitment to abstinence, generally operationalized as holding a specific goal to achieve abstinence, has been shown to be related to cessation of addictive behavior and maintenance of sobriety. Commitment to abstinence has predicted better abstinence outcomes and less likelihood of relapse at long-term follow-up in treatment studies for alcohol, opiates, cocaine, and tobacco (Hall, Havassy, & Wasserman, 1990, 1991; Morgenstern, Bux, Labouvie, Blanchard, & Morgan, 2002).
The primary objective of the present study was to examine whether smoking abstinence, as a consequence of psychiatric hospitalization in a smoke-free facility, was associated with changes in participants’ thoughts about quitting smoking. The particular thoughts measured concerned participants’ efficacy expectancies regarding success with quitting smoking and perceived difficulty with remaining smoke free after a quit attempt. Thoughts regarding patients’ commitment to abstinence were operationalized in terms of desire to quit smoking and having a specific abstinence goal. Demographic, tobacco-related, and psychiatric factors associated with changes in thoughts about abstinence were explored. Finally, we examined the impact of patients’ thoughts about abstinence on subsequent smoking behavior following hospital discharge. The present investigation was based on a larger study investigating psychiatric patients’ return to smoking after a smoke-free hospitalization (Prochaska, Fletcher, Hall, & Hall, 2006).
Method
Participants and recruitment
Participants were 100 (60 male, 39 female, 1 transgender) patients recruited from a university-based adult inpatient psychiatry unit with a complete smoking ban located in the San Francisco Bay area. Patients who were aged 18 years or older, smoked more than 100 cigarettes over their lifetime, and smoked one or more cigarettes in the week prior to hospitalization were eligible to participate. Patients who were non-English speaking or had severe agitation, cognitive deficits, or homicidal ideation were excluded from the study. Individuals who had plans to move out of the area were excluded because of the longitudinal design of the 3-month study.
Participants were recruited from the inpatient unit within 48 hr of admission. Clinical staff provided a brief overview of the study. Patients interested in learning more about the study met with research staff to confirm eligibility. Research staff provided a complete description of the study and obtained informed consent. The study was designed in compliance with HIPAA regulations, and all procedures involving human subjects were approved by the Institutional Review Board of the University of California, San Francisco. Assessments were conducted during hospital admission; before discharge; and at 1 week, 1 month, and 3 months posthospitalization. A total of 161 patients admitted to the unit during the recruitment period were identified as smokers. Of those, 20 did not meet study inclusion criteria and 26 were discharged before they could be recruited. A total of 115 patients were approached regarding the study; of those patients, 93% (107) agreed to hear details about the study, and 87% (100) elected to participate and provided informed consent. Follow-up assessments were completed by 90% of the sample.
Procedures
The first on-unit assessment was conducted generally within 48 hr of patients’ admission. The second on-unit assessment was conducted prior to patients’ discharge. Smoking was not permitted during the hospitalization. The outside rooftop area was non-smoking, and patients rarely received off-ward privileges other than to this controlled outside area. Visitors were told they could not bring cigarettes and were searched as needed. Follow-up assessments were conducted by phone at 1 week, 1 month, and 3 months posthospitalization. The full set of measures administered in these assessments has been described in detail previously (Prochaska et al., 2006). Only the measures relevant for the purposes of the present study are described here. Participants were paid US$10 for the on-unit assessment, $5 for each of the follow-up assessments, and $10 for travel for biochemical verification to confirm nonsmoking status when reported at the follow-up assessments. Participants who completed all assessments received an additional $10 bonus.
Assessments
The following measures were completed at the first on-unit assessment: Smoking History Questionnaire (Hall et al., 1990) assessed years of smoking, age first smoked, daily smoking behavior, and previous quit attempts. The Fagerström Test for Nicotine Dependence (FTND) (Heatherton, Kozlowski, Frecker, & Fagerström, 1991), a nine-item measure, assessed smoking behaviors indicative of physical dependence. The Computerized Diagnostic Interview Schedule-IV (CDIS; Robins, Cottler, Bucholz, & Compton, 1995) assessed demographic information and Diagnostic and Statistical Manual of Mental Disorders (4th edition) clinical diagnoses of unipolar depression, bipolar depression, anxiety disorders, psychotic disorders, and substance use disorders. The Secondhand Tobacco Smoke Exposure Survey, a six-item measure adapted for the present study, assessed participants’ exposure to second-hand smoke at work, at home, and in social situations. The Stages of Change Scale (DiClemente et al., 1991), a five-item measure, assessed readiness to quit smoking and categorized the smokers into one of the three pre-action stages (precontemplation, contemplation, and preparation). The Commitment to Abstinence Scale (Hall et al., 1990) assessed participants’ desire to quit smoking, expectancy of success, and anticipated difficulty quitting. Each construct was assessed with a single item, and responses were made on 10-point Likert scales. An additional item assessed participants’ smoking abstinence goal. For the purposes of analyses, the goals were categorized into one of three groups: (a) having no goal in mind, (b) intermediate goal (e.g., short-term abstinence, smoking in a controlled manner), or (c) goal of complete abstinence. The measure has demonstrated significant associations with other motivational measures in a sample of depressed outpatient smokers (Prochaska et al., 2004). Chart review documented patients’ length of stay on the unit and use of nicotine replacement therapy during the hospital stay.
Prior to their discharge from the hospital, most of the participants completed the Commitment to Abstinence Scale (Hall et al., 1990) for a second time. Some participants were discharged before the experimenter could conduct the second assessment (e.g., during the evening or weekend). For analyses, changes in patients’ thoughts about abstinence between hospital admission and discharge were calculated by subtracting scores at admission from scores reported before hospital discharge.
Follow-up assessments were conducted by phone at 1 week, 1 month, and 3 months after discharge. These assessments measured the timing of patients’ first cigarette following hospital discharge, as well as the total number of cigarettes smoked in the 7 days prior to each follow-up assessment. Reports of complete abstinence in the past 7 days were verified by having participants come in for an expired-air carbon monoxide (CO) sample using a Bedfont Smokerlyzer with a cut-off of CO≤10 ppm. Quit attempts, defined as abstinence for at least 24 hr, not including rehospitalization, also were assessed.
Data analyses
Analyses were conducted using SPSS version 14.0. Changes in thoughts about abstinence between admission and hospital discharge were tested with chi-square and paired-samples t tests. One-way analyses of variance (ANOVAs), regression, and chi-square tests were used to examine the relationship between changes in thoughts about abstinence and psychiatric diagnoses, demographic, and smoking variables, and also to test the associations between patients’ thoughts about abstinence at discharge and subsequent smoking behavior.
Results
Participant characteristics
The sample was demographically diverse: 68% were White, 9% Hispanic, 7% Asian American, and 4% Black; 12% reported another racial category, including multiracial. The mean age of the sample was 38.7 years (SD=11.9). Most participants (71%) were privately insured; 29% were insured through Medicare/Medi-Cal, and 1% were self-pay. Patients were hospitalized on average 7.5 days (SD=5.6). Additional sample characteristics have been described previously (Prochaska et al., 2006).
Changes in thoughts about abstinence
We found no significant change in participants’ desire to quit smoking from intake to hospital discharge, t(76)=−.68, ns; however, changes in participants’ expectancies regarding quitting were statistically significant (Table 1). Specifically, participants expected to be more successful in their attempts to quit smoking, t(75)=−2.45, p<.05, and perceived less difficulty with staying smoke free following a quit attempt, t(74)=2.98, p<.01.
Table 1.
Thoughts about abstinence at admission (time 1) and discharge (time 2).
| Desire (N=75) | Expectation of success (N=76) | Expectation of difficulty (N=77) | |
|---|---|---|---|
| Time 1 | 5.7 (2.8) | 4.7 (2.8) | 7.4 (2.4) |
| Time 2 | 5.9 (3.1) | 5.4 (3.0) | 6.3 (2.7) |
| Difference between time points | ns | p<.05 | p<.01 |
Note. Values are means with standard deviations.
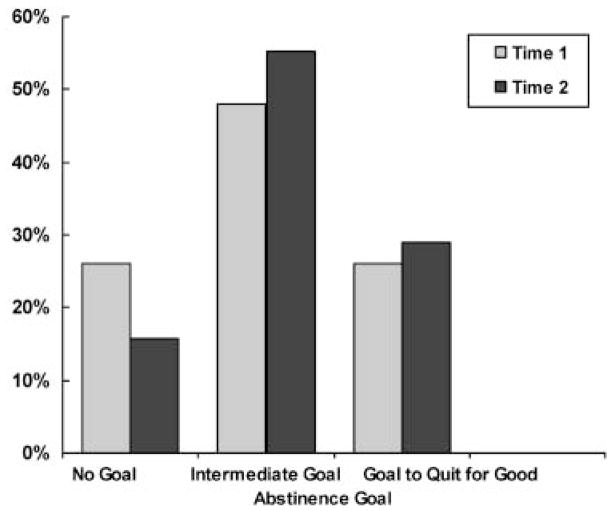
Participants’ goals related to smoking abstinence also changed significantly from intake to discharge, χ2(4)=26.94, p<.001. There was a decrease in the number of patients reporting having no abstinence goal, an increase of those identifying an intermediate goal regarding cutting back or restricting their use of tobacco, and an increase in those reporting a goal of complete abstinence (Figure 1).
Figure 1.
Goals regarding abstinence at admission (time 1) and discharge (time 2), N=76.
Moderators of change in thoughts about abstinence
Changes in participants’ thoughts about abstinence during their hospitalization were unrelated to the demographic variables assessed in the study (e.g., gender, ethnicity, education, employment). As a result, all further analyses collapsed across these variables.
Clinical diagnoses
Active psychiatric diagnoses on the CDIS-IV were major depressive disorder (55%), bipolar affective disorder (37%), post-traumatic stress disorder (37%), generalized anxiety disorder (35%), schizophrenia (8%), schizophreniform disorder (4%), alcohol dependence (34%), drug dependence (30%), nicotine dependence (83%), and nicotine withdrawal (62%). Psychiatric diagnosis was not associated with changes from admission to hospital discharge in desire to quit smoking, expectancy of success with quitting, or perceived difficulty with staying quit following a quit attempt (all p values >.345).
Smoking variables
Several smoking variables were associated with changes in participants’ thoughts about abstinence between admission and discharge. The average number of cigarettes patients smoked per day prior to hospitalization significantly predicted decreased perceived likelihood of success with quitting, F(1, 74)=5.60, p<.05. A total of 70 patients (70%) used nicotine replacement therapy during their hospitalization. Most (42) used the nicotine patch, 15 used nicotine gum, and 13 used both the patch and gum. Nicotine replacement dose was calculated as the average daily milligram dose, adjusted for the number of cigarettes participants smoked prior to hospitalization. Nicotine replacement dose significantly predicted increased feelings of success with quitting, F(1, 74)=5.07, p<.05. Participants who were exposed to more second-hand smoke in their residence had a greater increase in their expectation of difficulty with staying smoke free following a quit attempt, F(1, 72)=7.90, p<.01. Second-hand smoke exposure at work and in participants’ social environments was not related to changes in success, difficulty, or desire.
Thoughts about abstinence at discharge and future smoking behavior
Follow-up data were collected on 90% of the sample. The ten patients without follow-up data were removed from subsequent analyses. Most participants (76%) returned to smoking the same day they were discharged from the hospital. The time to first cigarette following discharge ranged from seconds to 36 days, with a median of 20 min for all participants. A one-way ANOVA demonstrated a significant association between the length of time (in minutes) that elapsed before the first cigarette smoked and participants’ reported abstinence goal at hospital discharge. For those with a goal of complete abstinence, more minutes elapsed before returning to smoking, compared with patients with no goal or those with an intermediate quitting goal, F(2, 58)=4.39, p<.05. Similarly, a significant association was found between the length of time that elapsed before the first cigarette smoked and participants’ reported desire to quit smoking at hospital discharge. Specifically, greater desire to quit smoking predicted longer latency to return to smoking following hospital discharge, F(1, 60)=8.65, p<.001.
Although all patients returned to smoking after their discharge from the hospital, the sample had a significant decline in average number of cigarettes smoked per day at the 3-month follow-up, compared with the daily average prior to hospitalization, t(75)=6.22, p<.001. Patients’ expectation of success with quitting smoking and their abstinence goals reported at hospital discharge were significantly associated with the number of cigarettes they smoked at the 3-month follow-up. Those with a greater expectation of success smoked fewer cigarettes per day on average at 3 months, r(77)=−.38, p<.01. Similarly, patients with a goal of complete abstinence smoked fewer cigarettes per day (M=5.98, SD=6.81), compared with patients with an intermediate abstinence goal (M=14.14, SD=8.08), or those with no goal (M=13.91, SD=16.16), F(2, 53)=4.73, p<.05.
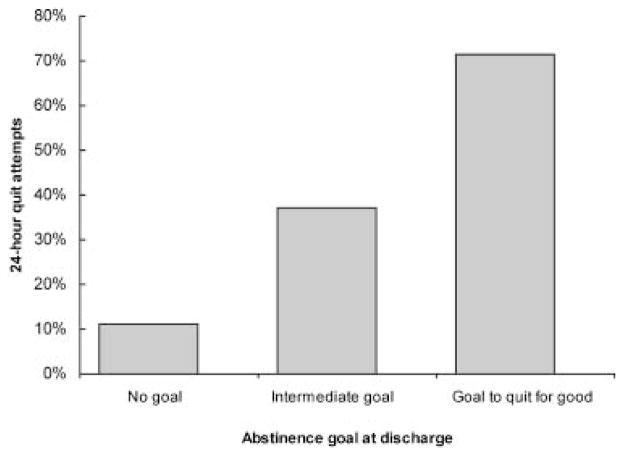
In addition to a reduced smoking rate, nearly half of the participants (48%) reported a later quit attempt after their hospital discharge. Quit attempts were defined as complete abstinence for at least 24 hr with the specific intent to quit and not because of rehospitalization. A logistic regression demonstrated a significant overall relationship in predicting later quit attempts for the following combination of variables assessed at hospital discharge: desire to quit smoking, anticipated success with quitting, and anticipated difficulty with staying smoke free after quitting, R2=.336, χ2(3)=19.06, p<.01. Participants with greater desire to quit, greater expectation of success, and less expectation of difficulty in staying quit were more likely to have a 24-hr quit attempt in the 3 months following hospital discharge. A similar, albeit weaker relationship was found when predicting later quit attempts from thoughts about abstinence reported at hospital admission, R2=.177, χ2(3)=12.09, p<.01. Finally, a chi-square analysis revealed a statistically significant association between later quit attempts and participants’ abstinence goals, χ2(2)=10.99, p<.01. Participants with a goal of complete smoking abstinence were most likely to report a later 24-hr quit attempt, compared with those with an intermediate quitting goal and those with no goal (Figure 2).
Figure 2.
Percentage of patients attempting to quit smoking following discharge.
Discussion
The findings indicate that psychiatric patients’ thoughts about quitting smoking changed significantly over the course of their hospitalization in a smoke-free facility. Initial overall analysis indicated no change in desire to quit but significant increases in expectancies of success with quitting and decreases in expectancies of difficulty with remaining smoke free after a quit attempt. Analysis of potential moderators identified several relevant clinical and tobacco-related factors. Changes in participants’ desire to quit and expectancy of success and difficulty with quitting were not found to differ by psychiatric diagnosis. The lack of difference is consistent with previous work with depressed outpatient smokers, which has found similar levels of motivation to quit, and success with quitting, as compared with the general population (Hall et al., 2006; Prochaska et al., 2004).
The overall analysis also indicated significant changes from admission to hospital discharge in participants’ goals related to their smoking. Specifically, participants were more likely to report a goal of intermediate or of complete abstinence versus not having any goal. These effects were robust and were consistent across gender, age, education, and other demographic variables measured in the study.
The principal motive urging this investigation of changes in thoughts about abstinence is the vital role these cognitions play in subsequent smoking behavior outcomes. Increasing efficacy beliefs and commitment to smoking abstinence is beneficial, as these factors have consistently shown a strong association with quitting smoking successfully (e.g., Carey & Carey, 1993) as well as a lesser likelihood of relapse (e.g., Gwaltney et al., 2001). Patients in the present study reported positive changes in their thoughts about abstinence, specifically abstinence efficacy beliefs and commitment to quitting smoking, and these thoughts, as measured upon discharge, were associated with longer latency to the first cigarette smoked after hospitalization, reduced smoking rate at the 3-month follow-up, and a greater likelihood of subsequent quit attempts.
The study findings help illuminate the potential advantageous effects of abstinence in a controlled hospital environment. Recent reviews demonstrate that the negative effects feared because psychiatric hospitals were going smoke free have not occurred (El-Guebaly et al., 2002; Lawn & Pols, 2005). The present study supports and extends these findings by illustrating that there may be additional advantages for patients, in terms of changes in thoughts about abstinence, as a result of a smoke-free hospitalization.
Further, these results support the importance of offering tobacco treatment for psychiatric patients. The American Psychiatric Association (2006) practice guidelines identify the inpatient hospitalization stay as an ideal opportunity to offer smokers with comorbid psychiatric disorders the same smoking cessation treatments that have been recognized as effective for smokers in the general population. In this study, although nicotine withdrawal was managed with nicotine replacement, no smoking cessation treatment was offered to patients. Even so, the results suggest that by the time of their hospital discharge, patients may have increased their readiness for considering such treatment, as evident by significantly greater confidence in and commitment to abstinence. This prospect is supported by studies indicating that smokers who have higher self-efficacy expectations are more likely to try to quit smoking or join smoking cessation treatments (Brod & Hall, 1984; Zentner & Borland, 1995). It also is important to note that providing nicotine replacement was successful in that it increased participants’ expectation of success if they were to quit smoking.
A limitation of the study is that patients were recruited from a single clinical site. However, the sample was diverse and representative of patients at the recruitment setting (Prochaska et al., 2006). Advantages of the study include the use of biochemical verification of nonsmoking status during follow-ups, an 87% participation rate, and a 90% follow-up rate.
The results of the study offer promising directions for future clinical interventions. Specifically, since self-efficacy is potentially malleable, interventions may choose to target patients’ efficacy expectations regarding smoking cessation. Treatments could incorporate goal-setting techniques designed to increase patients’ commitment to abstinence as well as coping skills and training to increase their confidence in their ability to successfully quit smoking and their commitment to abstinence. Furthermore, the study’s promising results have implications for the implementation of policies that ban smoking in psychiatric settings. Participants in the study, who were hospitalized merely 7.5 days on average and were offered no specific tobacco treatment other than nicotine replacement during their stay, nonetheless demonstrated a positive transformation in their thoughts about abstinence, which had beneficial effects on their subsequent smoking behavior in terms of reduction in the number of cigarettes smoked and later attempts at quitting.
Acknowledgments
This study was supported by grants from the State of California Tobacco-Related Disease Research Program (13KT-0152) and the National Institute on Drug Abuse (NIDA; K23 DA018691) awarded to Judith Prochaska. This research also was supported by the NIDA program for Postdoctoral Training in Drug Abuse Treatment and Services Research (T32 DA-007250) and a NIDA research center grant (P50 DA009253).
Footnotes
The authors had no conflict of interest or potential competing interests with the research, including employment and consultancies for the authors and their family members.
References
- American Psychiatric Association. American Psychiatric Association practice guidelines for the treatment of patients with substance use disorders. Compendium 2006, Steering Committee on Practice Guidelines; Arlington, VA. 2006. [PubMed] [Google Scholar]
- Baer JS, Lichtenstein E. Classification and prediction of smoking relapse episodes: An exploration of individual differences. Journal of Consulting and Clinical Psychology. 1988;56:104–110. doi: 10.1037//0022-006x.56.1.104. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy. New York: Freeman; 1997. [Google Scholar]
- Beemer BR. Hospital psychiatric units: Nonsmoking policies. Journal of Psychosocial Nursing and Mental Health Services. 1993;31:12–14. doi: 10.3928/0279-3695-19930401-07. [DOI] [PubMed] [Google Scholar]
- Brod MI, Hall SM. Joiners and non-joiners in smoking treatment: A comparison of psychosocial variables. Addictive Behaviors. 1984;9:217–221. doi: 10.1016/0306-4603(84)90061-3. [DOI] [PubMed] [Google Scholar]
- Carey KB, Carey MP. Changes in self-efficacy resulting from unaided attempts to quit smoking. Psychology of Addictive Behaviors. 1993;7:219–224. [Google Scholar]
- DiClemente CC. Self-efficacy and smoking cessation maintenance: A preliminary report. Cognitive Therapy and Research. 1981;5:175–187. [Google Scholar]
- DiClemente CC, Prochaska JO, Fairhurst SK, Velicer WF, Velasquez MM, Rossi JS. The process of smoking cessation: An analysis of precontemplation, contemplation, and preparation stages of change. Journal of Consulting and Clinical Psychology. 1991;58:175–181. doi: 10.1037//0022-006x.59.2.295. [DOI] [PubMed] [Google Scholar]
- El-Guebaly N, Cathcart J, Currie S, Brown D, Gloster S. Smoking cessation approaches for persons with mental illness or addictive disorders. Psychiatric Services. 2002;53:1166–1170. doi: 10.1176/appi.ps.53.9.1166. [DOI] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Chou SP, Stinson FS, Dawson DA. Nicotine dependence and psychiatric disorders in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:1107–1115. doi: 10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- Gwaltney CJ, Shiffman S, Normal GJ, Paty JA, Kassel JD, Gnys M, et al. Does smoking abstinence self-efficacy vary across situations? Identifying context-specificity within the Relapse Situation Efficacy Questionnaire. Journal of Consulting and Clinical Psychology. 2001;69:516–527. [PubMed] [Google Scholar]
- Gwaltney CJ, Shiffman S, Paty JA, Liu KS, Kassel JD, Gnys M, et al. Using self-efficacy judgments to predict characteristics of lapses to smoking. Journal of Consulting and Clinical Psychology. 2002;70:1140–1149. doi: 10.1037//0022-006x.70.5.1140. [DOI] [PubMed] [Google Scholar]
- Gwaltney CJ, Shiffman S, Sayette MA. Situational correlates of abstinence self-efficacy. Journal of Abnormal Psychology. 2005;114:649–660. doi: 10.1037/0021-843X.114.4.649. [DOI] [PubMed] [Google Scholar]
- Hall SM, Havassy BE, Wasserman DA. Commitment to abstinence and acute stress in relapse to alcohol, opiates, and nicotine. Journal of Consulting and Clinical Psychology. 1990;58:175–181. doi: 10.1037//0022-006x.58.2.175. [DOI] [PubMed] [Google Scholar]
- Hall SM, Havassy BE, Wasserman DA. Effects of commitment to abstinence, positive moods, stress, and coping on relapse to cocaine use. Journal of Consulting and Clinical Psychology. 1991;59:526–532. doi: 10.1037//0022-006x.59.4.526. [DOI] [PubMed] [Google Scholar]
- Hall SM, Tsoh J, Prochaska JJ, Eisendrath S, Rossi JS, Redding CA, et al. Treatment for cigarette smoking among depressed mental health outpatients: A randomized clinical trial. American Journal of Public Health. 2006;96:1808–1814. doi: 10.2105/AJPH.2005.080382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Joint Commission on Accreditation of Healthcare Organizations. Accreditation manual for hospitals. Oakbrook Terrace, IL: Author; 1992. [Google Scholar]
- Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: A population-based prevalence study. The Journal of the American Medical Association. 2000;284:2606–2610. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- Lawn S, Pols R. Smoking bans in psychiatric inpatient settings? A review of the research. Australian and New Zealand Journal of Psychiatry. 2005;39:866–885. doi: 10.1080/j.1440-1614.2005.01697.x. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Gordon JR. Relapse prevention. New York: Guilford; 1985. [Google Scholar]
- Morgenstern J, Bux D, Labouvie E, Blanchard KA, Morgan TJ. Examining mechanisms of action in 12-step treatment: The role of 12-step cognitions. Journal of Studies on Alcohol. 2002;63:665–672. doi: 10.15288/jsa.2002.63.665. [DOI] [PubMed] [Google Scholar]
- Niaura R. Cognitive social learning and related perspectives on drug craving. Addiction. 2000;95:S155–S163. doi: 10.1080/09652140050111726. [DOI] [PubMed] [Google Scholar]
- Prochaska JJ, Fletcher L, Hall SE, Hall SM. Return to smoking following a smoke-free psychiatric hospitalization. The American Journal on Addictions. 2006;15:15–22. doi: 10.1080/10550490500419011. [DOI] [PubMed] [Google Scholar]
- Prochaska JJ, Rossi JS, Redding CA, Rosen AB, Tsoh JY, Humfleet GL, et al. Depressed smokers and stage of change: Implications for treatment interventions. Drug and Alcohol Dependence. 2004;76:143–151. doi: 10.1016/j.drugalcdep.2004.04.017. [DOI] [PubMed] [Google Scholar]
- Psychiatric News. Mental illness advocacy group battling hospital smoking ban in New York. Vol. 1994. Philip Morris; 1994. Sep 16, Bates No. 2071540448. Retrieved from http://legacy.library.ucsf.edu. [Google Scholar]
- Robins LN, Cottler L, Bucholz K, Compton W. Diagnostic Interview Schedule for DSM-IV. St. Louis, MO: Department of Psychiatry, Washington University School of Medicine; 1995. [Google Scholar]
- Rohde P, Lewinsohn PM, Brown RA, Gau JM, Kahler CW. Psychiatric disorders, familial factors, and cigarette smoking. I: Associations with smoking initiation. Nicotine & Tobacco Research. 2003;5:85–98. doi: 10.1080/1462220031000070507. [DOI] [PubMed] [Google Scholar]
- Ryabik BM, Lippman SB, Mount R. Implementation of a smoking ban on a locked psychiatric unit. General Hospital Psychiatry. 1995;16:200–204. doi: 10.1016/0163-8343(94)90102-3. [DOI] [PubMed] [Google Scholar]
- Taylor NE, Rosenthal RN, Chabus B, Levine S, Hoffman AS, Reynolds J, et al. The feasibility of smoking bans on psychiatric units. General Hospital Psychiatry. 1993;15:36–40. doi: 10.1016/0163-8343(93)90089-7. [DOI] [PubMed] [Google Scholar]
- Zentner L, Borland R. The roles of temptation strength and self-efficacy in predicting smoking cessation attempts. Behaviour Change. 1995;12:191–195. [Google Scholar]