Abstract
Study Objective
Primary: To examine the relationship between relative timing of puberty with bone mineral density (BMD) in a group of adolescent girls; Secondary: To determine if family history of breast cancer was associated with bone mineral density.
Design/Setting/Participants
Longitudinal study of girls recruited between 6 and 7 years of age seen every 6 months for 5 years, and subsequently seen annually. BMD of the lumbar spine was measured by dual-energy X-ray absorptiometry (DXA) at mean age of 12.5 years; age- and race-specific Z-scores (BMDz) were calculated. Age of pubertal onset was determined by the first occurrence of breast stage 2, and participants were categorized into race-specific early, on-time and late puberty onset groups.
Main Outcome Measures
BMDz by timing of pubertal onset, and by family history of breast cancer.
Results
DXA scans were performed on 227 study participants, and a second scan was performed on 114 two years later. Age of onset of puberty was inversely correlated with BMDz, r=−0.31 (p<0.0001). There was no association between BMDz and family history of breast cancer.
Conclusions
Earlier timing of puberty was associated with higher BMD. The high shared variance of BMD and timing of pubertal onset implies an underlying biologic basis.
Keywords: bone density, puberty, breast cancer
INTRODUCTION
Puberty is a period of rapid change in both breast tissue and bone. The pathways involved in their development are complex and share several biologic factors, including insulin-like growth factor-1 (IGF-1) and the sex steroids. Associations have been reported independently between high bone mineral density (BMD) and an increased risk of breast cancer,1–4 as well as earlier age of menarche and an increased risk of breast cancer.5–7 Puberty represents a window of susceptibility for breast cancer.8 Further examination of the relationship between pubertal timing and BMD could provide important insights into breast cancer pathogenesis.
Peak bone mass and density in women are largely established during puberty. It has been reported that nearly 40% of total body bone mineral accrual occurs in the two years before and two years after peak height velocity during the pubertal growth spurt.9,10 Peak bone mineral content and density are reached in young women by 18 to 20 years of age.9
The purpose of this study was to examine the relationship between relative timing of puberty and BMD in a group of adolescent girls, and determine if family history of breast cancer was associated with BMD during puberty.
METHODS
The participants in the study were a subset of a larger cohort of girls enrolled in a longitudinal epidemiologic study of pubertal maturation, as part of the Cincinnati site of the Breast Cancer and the Environment Research Program (BCERP). The projects of the BCERP have been conducted through three sites: Mount Sinai School of Medicine, Kaiser Permanente of Northern California, and Cincinnati Children’s Hospital Medical Center/University of Cincinnati College of Medicine. Study aims and design have been described in detail elsewhere.11 To summarize, the participants at the Cincinnati site were recruited through public and parochial schools in the greater Cincinnati metropolitan area as well as through the Breast Cancer Registry of Greater Cincinnati. Participants were recruited between 6 and 7 years of age, and the enrollment process at the Cincinnati site lasted 19 months. Girls were seen every six months between 2004 and 2010, and thereafter every 12 months, with a visit window of 4 weeks. This study was approved by the Institutional Review Board of Cincinnati Children’s Hospital Medical Center. Informed consent was obtained from parents or guardians, and assent from participants.
There were 227 study participants included in these analyses. 143 girls were white, and 84 girls were black. A limited number of female staff were trained and certified in assessment of pubertal maturation, utilizing the criteria established by Marshall and Tanner for breast maturation, with palpation.12
Family history of breast cancer was gathered from a questionnaire administered to the parent/guardian in years 1 and 5 of the study. The parent/guardian was asked which first and second degree biological relatives of the participant had been diagnosed with breast cancer.
BMD was determined at the lumbar spine via dual-energy X-ray absorptiometry (DXA), on the Hologic QDR 4500A. Technicians were certified in performing these scans by the International Society for Clinical Densitometry. Calibration of the DXA scanner was assessed by daily scanning of a phantom, which would immediately indicate any machine malfunction. The coefficient of variability (CV) of the phantom scan results were calculated monthly and monitored for any change in machine performance over time. The mean longitudinal CV over a period of 3 years (n=971 scans) of the spine phantom was 0.4%. DXA results were standardized for age and race, and lumbar spine results were reported as BMD z-scores (BMDz). Of note, DXA was performed only at the Cincinnati site.
Statistical analysis
The age of pubertal onset was determined by the first occurrence of breast stage 2 or above during the study. We categorized study participants into race-specific early, on-time and late onset groups using the sample percentiles of 20% and 80%, yielding three groups- early (20%), on-time (60%), and late (20%). We compared the BMD z-score from the initial DXA scan between the three pubertal onset groups, and in separate analyses, the participants’ family history of breast cancer, using one-way ANOVA. Linear regression equations were used to model the relationship between the BMD z-score with the age of pubertal onset group, adjusted for participant’s pubertal stage at the time of the DXA scan, race and family history of breast cancer; these analyses were conducted separately for BMDz results from the initial and the subsequent DXA scans. Rank-based Spearman’s correlations were reported for BMD z-score with the age of pubertal onset group.
RESULTS
The initial DXA scans were performed in study year 6 on 227 of the 268 (84.7%) participants who remained of the original cohort; 114 of these 227 participants (50.2%) had a second scan two years later (mean 717 days). The mean age of the first DXA scan was 12.5 years. Nearly all (93.9%) were pubertal (breast stage 2 or greater), and 73.6% were breast stages 3 through 5 at the time of the first scan. There was a high correlation between BMDz scores from the first and second DXA scans in those with two scans (r=0.914, p<0.0001). Black participants had a slightly higher mean BMD z-score than white participants, but the result was not statistically significant (0.29 vs. 0.16, p = 0.40).
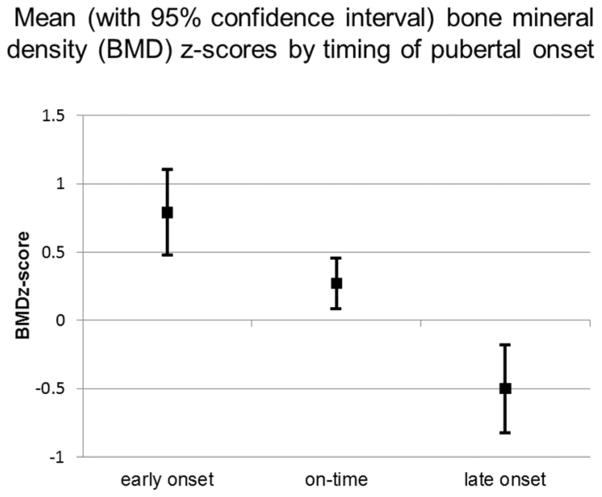
The participants were placed into three categories, based on race-specific age of pubertal onset. Among white participants, early maturers entered puberty under 7.67 years and late maturers over 9.94 years. Among black participants, early maturers entered puberty under 7.25 years and late maturers over 9.39 years of age. Our analysis revealed that age of onset of puberty was highly associated with BMDz, r=−0.32 (p<0.0001) (Figure 1). There was a strong, inverse relationship between earlier onset of puberty and higher bone density, and timing of pubertal onset accounted for 10.2% of the variance. When adjusting for pubertal stage, the amount of variance accounted by timing of pubertal onset was 7.8%. When re-examining the relationship between BMD and timing of pubertal onset, using DXA measurements obtained two years later, the association between age at onset of puberty and BMDz was still highly significant (r =−0.29, p<0.0001).
Figure 1.
There were 8% of participants who had a mother, and an additional 20% with a biologic aunt or grandmother diagnosed with breast cancer. There was no significant association of family history of breast cancer on bone mineral density (BMD z-score 0.25 vs. 0.14, p = 0.58).
DISCUSSION
This longitudinal study demonstrated earlier timing of puberty was associated with higher BMD, and relative timing of pubertal onset accounted for 10% of the variance in BMD. This study extends the evidence in the literature that BMD and age of puberty are associated. Gilsanz et al. reported that age of onset of puberty was a negative predictor of bone mass at all skeletal sites measured at the time of skeletal maturation.13 Whole body bone mineral content was 6% higher in early maturing girls compared to on-time girls. Of note, they used only the study participants at skeletal maturity, and who began and completed puberty during the protocol, which represented 10% of the cohort. This is in contrast to our study in which the retained cohort was represented, and included a larger sample size. Similarly, Jackowski et al. reported that early maturation in girls leads to the deposition of 3–4% greater total body bone mineral content at 20 years of age.14
A major limitation of our study was that our model did not examine bone density at the time of a woman’s peak bone density, which occurs in late teens or early twenties.9 This potentially may lead to confounding, as girls with later puberty may have lower BMD at younger ages, but accrue additional bone mineral content in late puberty.15 However, it is unlikely that later maturing girls will experience enough additional bone mineral to completely resolve the differences we noted. For example, although age and sexual maturation were associated with decreased tracking of BMD in a longitudinal cohort, high tracking persisted after adjusting for age and maturation effects.16 Additionally, BMD tracked highly between DXA scans performed two years apart in our pubertal cohort. Magarey et al. have reported bone mineral content increases between ages 11 and 15, at which age they have achieved 85% of their adult bone content.10 An additional DXA scan once BMD levels plateau would reinforce these findings, but we believe the high correlation noted between age of onset of puberty and BMD would remain in our participants.
There have been several studies reporting that earlier onset of puberty, as well as higher bone density, independently increase the risk of breast cancer.2–7,15 Given the high shared variance of bone density and timing of pubertal onset, and association of both to breast cancer, there likely exists a common biologic pathway. Genome-wide association studies (GWAS) have estimated that 50–85% of variance in BMD is heritable.17 Similarly, 50–80% of the variance in age of puberty can be explained by genetic factors.18 As an example of genetic explanation of a phenotypic observation, a specific gene has been identified that associates greater body mass index (BMI) and timing of puberty.19 Although our results do not conclusively link BMD and pubertal onset with a breast cancer-related gene, they have very important implications to understand mechanistic factors in breast cancer research.
Acknowledgments
On behalf of the Puberty Studies of the BCERP, we also gratefully acknowledge the study investigators and staff within the Breast Cancer and the Environment Research Centers. We also thank our community collaborators for their insight and support of our research efforts, Justin Bates for data management, and Lynn Hanrahan for clerical assistance.
Financial support: U01ES012770, U01ES019453, R21ES017315, UL1TR000077
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Fraenkel M, Novack V, Liel Y, et al. Association between bone mineral density and incidence of breast cancer. PLoS One. 2013;8:e70980. doi: 10.1371/journal.pone.0070980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grenier D, Cooke AL, Lix L, et al. Bone mineral density and risk of postmenopausal breast cancer. Breast Cancer Res Treat. 2011;126:679. doi: 10.1007/s10549-010-1138-y. [DOI] [PubMed] [Google Scholar]
- 3.Qu X, Zhang X, Qin A, et al. Bone mineral density and risk of breast cancer in postmenopausal women. Breast Cancer Res Treat. 2013;138:261. doi: 10.1007/s10549-013-2431-3. [DOI] [PubMed] [Google Scholar]
- 4.van der Klift M, de Laet CE, Coebergh JW, et al. Bone mineral density and the risk of breast cancer: The Rotterdam Study. Bone. 2003;32:211. doi: 10.1016/s8756-3282(02)00972-9. [DOI] [PubMed] [Google Scholar]
- 5.Clavel-Chapelon F, Group ENE. Differential effects of reproductive factors on the risk of pre- and postmenopausal breast cancer: Results from a large cohort of French women. Br J Cancer. 2002;86:723. doi: 10.1038/sj.bjc.6600124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garland M, Hunter DJ, Colditz GA, et al. Menstrual cycle characteristics and history of ovulatory infertility in relation to breast cancer risk in a large cohort of US women. Am J Epidemiol. 1998;147:636. doi: 10.1093/oxfordjournals.aje.a009504. [DOI] [PubMed] [Google Scholar]
- 7.Peeters PH, Verbeek AL, Krol A, et al. Age at menarche and breast cancer risk in nulliparous women. Breast Cancer Res Treat. 1995;33:55. doi: 10.1007/BF00666071. [DOI] [PubMed] [Google Scholar]
- 8.Biro FM, Deardorff J. Identifying opportunities for cancer prevention during preadolescence and adolescence: Puberty as a window of susceptibility. J Adolesc Health. 2013;52:S15. doi: 10.1016/j.jadohealth.2012.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baxter-Jones AD, Faulkner RA, Forwood MR, et al. Bone mineral accrual from 8 to 30 years of age: an estimation of peak bone mass. J Bone Miner Res. 2011;26:1729. doi: 10.1002/jbmr.412. [DOI] [PubMed] [Google Scholar]
- 10.Magarey AM, Boulton TJ, Chatterton BE, et al. Bone growth from 11 to 17 years: Relationship to growth, gender and changes with pubertal status including timing of menarche. Acta Paediatr. 1999;88:139. doi: 10.1080/08035259950170286. [DOI] [PubMed] [Google Scholar]
- 11.Biro FM, Galvez MP, Greenspan LC, et al. Pubertal assessment method and baseline characteristics in a mixed longitudinal study of girls. Pediatrics. 2010;126:e583. doi: 10.1542/peds.2009-3079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Child. 1969;44:291. doi: 10.1136/adc.44.235.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gilsanz V, Chalfant J, Kalkwarf H, et al. Age at onset of puberty predicts bone mass in young adulthood. J Pediatr. 2011;158:100. doi: 10.1016/j.jpeds.2010.06.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jackowski SA, Erlandson MC, Mirwald RL, et al. Effect of maturational timing on bone mineral content accrual from childhood to adulthood: evidence from 15 years of longitudinal data. Bone. 2011;48:1178. doi: 10.1016/j.bone.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 15.Russo J, Russo IH. Differentiation and breast cancer. Medicina (B Aires) 1997;57(Suppl 2):81. [PubMed] [Google Scholar]
- 16.Kalkwarf HJ, Gilsanz V, Lappe JM, et al. Tracking of bone mass and density during childhood and adolescence. J Clin Endocrinol Metab. 2010;95:1690. doi: 10.1210/jc.2009-2319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Richards JB, Zheng HF, Spector TD. Genetics of osteoporosis from genome-wide association studies: Advances and challenges. Nat Rev Genet. 2012;13:576. doi: 10.1038/nrg3228. [DOI] [PubMed] [Google Scholar]
- 18.Choi JH, Yoo HW. Control of puberty: Genetics, endocrinology, and environment. Curr Opin Endocrinol Diabetes Obes. 2013;20:62. doi: 10.1097/MED.0b013e32835b7ec7. [DOI] [PubMed] [Google Scholar]
- 19.Ong KK, Elks CE, Wills AK, et al. Associations between the pubertal timing-related variant in LIN28B and BMI vary across the life course. J Clin Endocrinol Metab. 2011;96:E125. doi: 10.1210/jc.2010-0941. [DOI] [PMC free article] [PubMed] [Google Scholar]