Abstract
Background
Nicotine dependence (ND) is a key construct that organizes physiological and behavioral symptoms associated with persistent nicotine intake. Measurement of ND has focused primarily on cigarette smokers. Thus, validation of brief instruments that apply to a broad spectrum of tobacco product users is needed.
Methods
We examined multiple domains of ND in a longitudinal national study of the United States population, the United States National Epidemiological Survey of Alcohol and Related Conditions (NESARC). We used methods based in item response theory to identify and validate increasingly brief measures of ND that included symptoms to assess ND similarly among cigarette, cigar, smokeless, and poly tobacco users.
Results
Confirmatory factor analytic models supported a single, primary dimension underlying symptoms of ND across tobacco use groups. Differential Item Functioning (DIF) analysis generated little support for systematic differences in response to symptoms of ND across tobacco use groups. We established significant concurrent and predictive validity of brief 3- and 5- symptom indices for measuring ND.
Conclusions
Measuring ND across tobacco use groups with a common set of symptoms facilitates evaluation of tobacco use in an evolving marketplace of tobacco and nicotine products.
Keywords: Nicotine Dependence, Poly-Tobacco Use, Item Response Theory, Tobacco
1. INTRODUCTION
Nicotine dependence (ND) has been described as a combination of neurobiological symptoms and learned behaviors associated with repeated self-administration of nicotine (Collins and Marks, 1991; Edwards and Gross, 1976). For the past half century, knowledge about tobacco use and ND has come primarily from research conducted among cigarette users (United States Department of Health and Human Services (USDHHS), 2014). However, in recent years, tobacco products have diversified into new and different forms, and poly-use of these products is becoming increasingly common (USDHHS, 2014). Tobacco products differ in nicotine content, route of administration, constituent ingredients and constituents, and behavioral patterns of persistent use and thus cigarette-focused instruments may not effectively reflect ND among non-cigarette product users (De Leaon et al., 2014; Fant et al., 2009). The extent that the occurrence and severity of symptoms of ND (e.g., tolerance, withdrawal) are similar or different across tobacco products (e.g., cigarettes versus non-combustible tobacco products) is currently unknown; therefore, there is an urgent need to examine the utility and validity of ND measures across users defined by different tobacco products.
In clinical practice and many research purposes, the diagnosis and treatment of ND relies on definitions in both the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; (American Psychiatric Association, 1994) and the International Classification of Diseases (Organization, 2008). Both classification systems use the 7 primary domains identified by Edwards and Gross (1976) and Collins and Marks (1991): (1) physiological tolerance, (2) evidence of characteristic withdrawal symptoms, (3) impaired control over tobacco use, (4) unsuccessful attempts to quit, (5) spending a great deal of time using tobacco, (6) prioritizing tobacco use over other activities, and (7) using tobacco despite physical or psychological health consequences. The DSM-IV and ICD-10 do not represent an exhaustive representation of domains of ND and efforts to expand definitions under the DSM-V (American Psychiatric Association, 2013) to include social consequences and craving or refine aspects of ND in self-report instruments continue to evolve (Piper et al., 2008). The NESARC developed 22 symptoms that fit into the seven DSM-IV domains and proposed additional symptoms that may also inform the ND construct. NESARC measured use of multiple tobacco-use products, making it well suited to investigate this set of ND domains across products.
The overarching aim of this project was to establish a parsimonious set of symptoms that efficiently and effectively measures ND across users of different tobacco products. We set out to identify a reduced set of questions that would make it easier for researchers and clinicians to assess ND for users of different types of tobacco products and poly-users. One such study that could benefit from identification of ND questions that are valid across different tobacco products is the Population Assessment of Tobacco and Health (PATH) Study, which is a nationally representative longitudinal cohort study of tobacco use and health outcomes within the United States population (National Institutes of Health and Food and Drug Administration, 2014) that includes a set of NESARC ND symptoms in its baseline survey. Using the entire set of questions from the NESARC study, we leverage the psychometric tools of item response theory to formalize commonalities and differences in symptom “signatures” among users of different tobacco products. A secondary goal was to identify and remove any symptom domains that were sensitive to product characteristics. Third, we examined whether the reduced set of symptoms would be a valid and efficient measure of ND to replicate in other national studies examining tobacco use.
2. METHODS
2.1 Symptoms of nicotine dependence
We examined Past Year symptoms of ND in a US cohort using the NESARC study data. We utilized wave 1 (W1: n= 43,093) conducted in 2001–2002 and wave 2 (W2: n=34,653) conducted in 2004–2005. We organized the 22 ND symptoms assessed by the NESARC Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS) into groups that either reflected specific DSM-IV criteria or had similar content. Initial groupings included Tolerance (2 symptoms), Withdrawal Syndrome (8 potential symptoms), Use for Withdrawal Relief (1 symptom), Use Upon Waking (1 symptom), Use After Temporary Abstinence (1 symptom), Used More Than Intended (1 symptom), Desire to Quit/Difficulty Quitting (2 symptoms), Loss of Control (1 symptom), Difficulty Refraining (1 symptom), Give Up Activity (2 symptoms), and Use Despite Health Consequences (2 symptoms). High symptom intercorrelations led us to collapse desire to quit/difficulty quitting symptoms (2 symptoms; r=0.83), and to collapse Give Up Activities symptoms (2 symptoms; r=0.76). We created a single symptom for the presence of the withdrawal syndrome using the DSM-IV criteria of endorsement of 4 of 8 symptoms and reporting impairment. The thirteen remaining symptoms were then organized into 8 multi-symptom domains: tolerance (2 symptoms); withdrawal (2 symptoms: Withdrawal Syndrome, Withdrawal Relief); use after temporary abstinence (2 symptoms); using more than intended (1 symptom); difficulty quitting (1 symptom); loss of control (2 symptoms -1 Diff. Refrain, 1 Loss of Control); giving up activities due to use (1 symptom); and consequences of use (2 symptoms).
2.2 Overview of Data Analytic Plan
We established four mutually exclusive past year tobacco-user groups: cigarette only users (n=9305), cigarette and cigar users (n=581), cigar only users (n=538), and smokeless tobacco users with or without other forms of tobacco (n=615). W2 included 8289 tobacco users of whom 356 were successful quitters (i.e. no tobacco use for ≥ 12-months). Item response models (IRM) were used to detail symptom responses among the four tobacco use groups. Prior to fitting IRM we evaluated model assumptions that symptoms measured a single common construct of ND. When covariation among symptoms arises from inclusion of multiple symptoms to assess the same domain of the ND construct (i.e. 2 tolerance or 2 withdrawal symptoms), the estimated relationships of symptoms with the primary single common construct of ND can be affected. Understanding any significant covariation within multi-symptom domains is important in selecting an IRM that can accommodate violations of this local independence assumption. To evaluate the significance of covariation within multi-symptom domains, we used a series of bifactor models to organize covariance of all symptom responses using a primary factor to reflect a single dimension of nicotine dependence while also allowing secondary factors to account for additional covariation within multi-symptom domains. We used full information maximum likelihood confirmatory factor analysis (Cai, 2010) and the Metropolis-Hastings Robbins-Monro (MH-RM) algorithm implemented in the ‘mirt’ package (Chalmers, 2012). Fit to a single primary factor of ND was compared to fit to a series of bifactor models of ND that added covariation within multi-symptom domains. We evaluated increasingly complex bifactor models that accounted for either a minimum of three multi-symptom domains (Tolerance, Withdrawal, Use After Temporary Abstinence) or a maximum of five-multi-symptom domains (three multi-symptom domains plus either loss of control and/or consequences). We used model-fit indices including AIC, BIC, and -2log likelihood to guide evaluations. We selected an IRM model based in Testlet Response Theory (Wainer et al., 2007). In this context, all symptoms are believed to measure a single primary dimension of ND and the ‘testlets’ are the groupings of symptoms within multi-symptom domains. This IRM allows comparison of symptom endorsements and evaluation of brief symptom indices for use across tobacco use groups. To evaluate validity we compared observed W1 ND symptom counts with concurrent quantity of product use, and also assessed predictive validity of W1 ND assessment on quit success by W2. We then used symptom characteristics from these analyses to select reduced sets of symptoms that could be used to assess ND equitable across all tobacco-use groups.
2.3. Bayesian Item Response Model
We fit an IRM that accommodated non-normal distributions of ND and included testlets to account for variability within multi-symptom domains. Although confirmatory bifactor models supported assumptions that all symptoms reflect a single primary dimension of ND, the models also suggested that additional variability remained within multi-symptom domains. We selected an IRM that included testlets, or groupings of symptoms that belong to these multi-symptom domains. Each testlet is modeled with a random effect term to adjust for this additional source of covariation that would otherwise violate local independence assumptions of other IRM models. By adding random effects to reflect significant variability within multi-symptom domains, IRM with testlets were used to evaluate the measurement equality of ND symptom reports from each tobacco use group. We evaluated (1) the relative strength of association (i.e., discrimination) between each symptom and levels of ND; (2) the ability to map each symptom within identified levels of ND (i.e., severity threshold). Finally, a series of models isolated and compared each ND symptom report from each tobacco use group in Differential Item Functioning (DIF) analyses. Using methods described by Wang and colleagues (2008) and SCORIGHT software (Wang et al., 2005), we obtained Markov Chain Monte Carlo (MCMC) generated samples from the posterior distribution of each of the model parameters separately for each symptom and each tobacco use group. Significant DIF in the discrimination (‘a’ parameter) and/or severity (‘b’ parameter’) was interpreted when differences between pairs of posterior values sampled from each group were >0 in 95% of 10,000 draws.
3. RESULTS
3.1 Descriptive analyses
The analytical sample of adults who used tobacco within the last 12 months was identified at W1. Demographic characteristics of the W1 sample and the rate of W2 re-interviews are detailed by each demographic subgroup in Table 1. At W2, the percentage of re-interviews was lower among 1) those 18–25 and 65+ relative to other age groups, 2) Asian relative to other racial groups, and 3) those with less than high school education relative to other levels of education attainment. Importantly, rates of re-interview were similar among the tobacco-use groups.
Table 1.
Demographics at Wave 1 and the percent respondents missing assessments at Wave 2 within demographic subgroups.
| Variable | Wave 1 | Wave 2 | ||
|---|---|---|---|---|
| n | Sample % | n | % Missing at W2 | |
| Age Group | ||||
| 18–29 | 8666 | 20.1% | 6719 | 22.5% |
| 30–39 | 8942 | 20.8% | 7299 | 18.4% |
| 40–49 | 8458 | 19.6% | 7146 | 15.5% |
| 50–64 | 8822 | 20.5% | 7485 | 15.2% |
| 65+ | 8205 | 19.0% | 6004 | 26.8% |
| Gender | ||||
| Male | 18518 | 43.0% | 14564 | 21.4% |
| Female | 24575 | 57.0% | 20089 | 18.3% |
| Race | ||||
| White | 31825 | 73.9% | 25791 | 19.0% |
| Black/Afr.American | 8404 | 19.5% | 6680 | 20.5% |
| Asian | 1312 | 3.0% | 942 | 28.2% |
| American Indian | 1304 | 3.0% | 1032 | 20.9% |
| Hawaiian/Pacific | 248 | 0.6% | 208 | 16.1% |
| Ethnicity | ||||
| Hispanic/Latino | 8308 | 19.3% | 6356 | 23.5% |
| Not Hispanic/Latino | 34785 | 80.7% | 28297 | 18.7% |
| Education | ||||
| < High School | 7849 | 18.2% | 5744 | 26.8% |
| GED/High School | 12547 | 29.1% | 9955 | 20.7% |
| Some/Two-year College | 12663 | 29.4% | 10474 | 17.3% |
| Bachelors Degree | 5251 | 12.2% | 4389 | 16.4% |
| Some/Graduate Degree | 4783 | 11.1% | 4091 | 14.5% |
| Examined Tobacco Use Groups | ||||
| Cigarette ONLY | 9305 | 21.6% | 7446 | 20.0% |
| Cigarette and Cigar ONLY | 581 | 1.3% | 447 | 23.1% |
| Cigar ONLY | 538 | 1.2% | 436 | 19.0% |
| Smokeless WITH/WITHOUT OTHER FORMS | 615 | 1.4% | 513 | 16.6% |
| Other/Non-Users | 32054 | 74.4% | 25811 | 19.5% |
Note: Percent Missing at W2 reflects the number of wave 1 respondents within each demographic subgroup observed at wave 2 (row percents)
3.2 Domains of nicotine dependence symptoms among tobacco use groups
All 13 symptoms were expected to be related to a single underlying dimension of ND. Five of the eight domains included symptom pairs with conceptual overlap and potentially significant local dependence (see section 2.1). CFA was used to evaluate the improvement in model fit when grouping symptom pairs within domains using a series of bifactor models. Table 2 lists the model fit indices and available model degrees of freedom (df) that reflect the number of unique response patterns observed in each tobacco-use group, minus one (Chalmers, 2012).
Table 2.
Goodness of fit measures comparing confirmatory factor analysis models of Nicotine Dependence: Unidimensional, three multi-symptom domain bifactor, and five multi-symptom domain bifactor models are presented.
| Name | Structure | Multi-Symptom Sub-Domains | Df | AIC | BIC | logLik | X2 | df | p |
|---|---|---|---|---|---|---|---|---|---|
| Cigarette
| |||||||||
| Model A | Uni | 0 | 1159 | 98393.51 | 98579.10 | −49170.75 | |||
| Model B | Bifactor | 3 | 1153 | 97236.38 | 97464.80 | −48586.19 | 1169.12 | 6.00 | <0.01 |
| Model E | Bifactor | 5 | 1149 | 97034.38 | 97291.36 | −48481.19 | 210.00 | 4.00 | <0.01 |
|
| |||||||||
| Cigarette+Cigar
| |||||||||
| Model A | Uni | 0 | 204 | 6290.57 | 6404.06 | −3119.29 | |||
| Model B | Bifactor | 3 | 198 | 6260.30 | 6399.98 | −3098.15 | 42.27 | 6.00 | <0.01 |
| Model E | Bifactor | 5 | 194 | 6242.19 | 6399.32 | −3085.09 | 26.12 | 4.00 | <0.01 |
|
| |||||||||
| Cigar
| |||||||||
| Model A | Uni | 0 | 45 | 2383.32 | 2494.80 | −1165.66 | |||
| Model B | Bifactor | 3 | 39 | 2361.70 | 2498.91 | −1148.85 | 33.62 | 6.00 | <0.01 |
| Model E | Bifactor | 5 | 35 | 2371.20 | 2525.56 | −1149.60 | −1.49 | 4.00 | >0.99 |
|
| |||||||||
| Smokeless
| |||||||||
| Model A | Uni | 0 | 129 | 5110.52 | 5225.48 | −2529.26 | |||
| Model B | Bifactor | 3 | 123 | 5073.77 | 5215.26 | −2504.89 | 48.75 | 6.00 | <0.01 |
| Model E | Bifactor | 5 | 119 | 5071.06 | 5230.24 | −2499.53 | 10.71 | 4.00 | 0.03 |
Note: Available degrees of freedom (Df) in unidimensional model reflect the number of unique patterns of responses minus 1.
Bifactor models that reflected the grouping of symptoms within either 3 or 5 multi-symptom domains provided better fit than the unidimensional model alone. A bifactor model that included multi-symptom domains for pairs of Tolerance, Withdrawal, and Use After Temporary Abstinence symptoms, with no further multi-symptom domains for remaining symptoms, consistently produced favorable improvements in fit over a unidimensional model. Inclusion of all 5 potential symptom pairs resulted in a small, and in the case of cigar-only users, non-significant improvement in overall fit across tobacco use groups. Given marginal improvements of the more complex model and consistent improvement in fit over no mulit-symptom domains, the 3-multi-symptom domain solution was favored. All subsequent IRM of the 13 symptoms included terms to reflect three multi-symptom domains (Tolerance, Withdrawal, and Use After Temporary Abstinence) while the 7 remaining symptoms were modeled only in relation to the primary dimension of nicotine dependence.
3.3 Symptom expression across tobacco use groups
We provide a summary of DIF results in Table 3 and detail the observed frequency, IRM estimated strength of relationship with other symptoms of ND (a: discrimination), the level of ND where each symptom is likely be observed (b: severity), and results from comparison of posterior distributions across tobacco use groups in Supplementary Material1. For all analyses, we established a common metric for comparison purposes using latent scores with a mean of 0 (SD=1) to represent the average level of ND in the W1 sample. Establishing a common metric with latent scores is essential to making group comparisons that are corrected for any potential bias from DIF. Between-group comparisons using observed scores may confound interpretation in the presence of DIF. Higher observed scores may either reflect real differences in levels of ND or the higher likelihood of reporting particular symptoms. Levels of ND were 0.06 (SD=0.85) among cigarette-only users, 0.14 (SD=0.93) among cigarette+cigar users, −0.85 (SD=0.64) among cigar-only users, and −0.36 (SD=0.78) among smokeless-tobacco users. At the lowest levels of ND, symptoms observed across the tobacco-use groups included ‘wanting to stop’, ’continuing despite health problems’, ‘using just after getting up’, and ‘using tobacco just after use was not permitted.’ At the highest levels of ND, the symptoms included ‘giving up activities due to tobacco use’, ‘increasing tobacco use by 50% in the past year’, and experiencing the ‘withdrawal syndrome’ when deprived of tobacco.
Table 3.
Summary of Differential Item Function (DIF) analyses for each Nicotine Dependence (ND) symptom.
| Cigarette ONLY | Cigarette + Cigar ONLY | Cigar Only | Smokeless WITH/WITH OUT OTHER FORMS | ||||
|---|---|---|---|---|---|---|---|
| (n= 9305) | (n= 581) | (n= 538) | (n= 615) | ||||
| Nicotine Dependence Symptom | Reference | a | b | a | b | a | b |
| Mult-symptom Domain 1: Tolerance | |||||||
| Use much more to get effect | R | 0 | 0 | 0 | − | 0 | − |
| Increase use by 50 percent | R | 0 | 0 | 0 | 0 | 0 | 0 |
| Mult-symptom Domain 2: Withdrawal | |||||||
| Withdrawal syndrome | R | 0 | 0 | 0 | 0 | 0 | 0 |
| Use tobacco to keep from having withdrawal | R | 0 | 0 | 0 | + | 0 | 0 |
| Mult-symptom Domain 3: Use After Temporary Abstinence | |||||||
| Often JUST AFTER getting up | R | + | 0 | 0 | + | 0 | 0 |
| JUST AFTER use was not permitted | R | 0 | 0 | 0 | + | − | + |
| Remaining symptoms | |||||||
| Used tobacco more than you intended | R | 0 | 0 | + | 0 | 0 | 0 |
| Want to/try to stop or cut down | R | 0 | 0 | + | + | + | + |
| Chain smoking/using | R | + | − | + | 0 | + | − |
| Wake at up night to use tobacco | R | 0 | 0 | + | 0 | 0 | + |
| Give up or cut down on activities | R | 0 | 0 | + | − | 0 | 0 |
| Use tobacco despite health problem | R | 0 | + | + | + | 0 | + |
| Use tobacco despite anxious or depressed | R | 0 | 0 | 0 | 0 | 0 | 0 |
Note: The discrimination (a) and severity (b) parameters from each tobacco use group were compared to parameters from cigarette users as a reference (‘R’). Comparisons with no significant DIF have ‘0’ symbol. Comparisons where the parameter was higher in the focal group have a ‘+’ and comparisons where parameter was lower in the focal group have a ‘−‘ symbol.
3.4 Differences in symptom reports within tobacco use groups
DIF analyses evaluated each parameter within IRM designed to isolate group differences in the likelihood of symptom reports given similar levels of ND. Posterior distributions for item parameters were generated by a series of IRM that examined each symptom for each tobacco-use group. Using the model to anchor each group to the same metric for ND, we compared results to posterior distributions from cigarette-only users, the reference group (Wang, Bradlow, Wainer, and Muller, 2008). Table 3 lists the results of the DIF comparisons. Using the two posterior distributions of discrimination (a) and severity (b) item parameters from each tobacco-use group, we assessed DIF by: 1) drawing a value of each item parameter from tobacco-use group distributions; 2) drawing a corresponding value from cigarette-only users, the reference distribution; 3) comparing to see if the parameter from the cigarette-only users was larger than the value from the other tobacco-use group distribution; and 4) repeating comparisons of pairs from 10,000 draws to record an estimate of the likelihood that item parameters were higher among cigarette-only users than in other tobacco-use groups. The identified differences between item parameters were considered significant when more than 95% (suggesting higher estimates) or less than 5% (suggesting lower estimates) of comparisons between randomly drawn pairs were higher in cigarette-only users. DIF analyses were completed for the following symptom groups:
3.4.1 Tolerance
We observed no significant DIF between cigarette-only and other tobacco use groups when reporting an ‘increase in use by 50%.’ When compared to cigarette-only users, both cigar-only and smokeless user reports of ‘using much more to get an effect’ were associated with slightly lower overall levels of ND (bCigar= 1.29; bSmokeless= 1.42; bCigarette= 1.61). We did not observe significant DIF in comparisons of cigarette+cigar and cigarette-only users on either of the Tolerance symptoms.
3.4.2 Withdrawal
We did not detect differences in the strength of discrimination for Withdrawal related symptoms. We observed small DIF in one comparison in which cigar-only user reports of ‘use tobacco to keep from having withdrawal’ reflected slightly more severe levels of ND than similar reports among cigarette-only users (bCigar= 1.96; bCigarette= 1.50).
3.4.3 Use After Temporary Abstinence
Although strongly related to levels of ND in all tobacco-use groups, cigarette+cigar user reports of ‘using just after getting up’ was an even stronger indicator of ND (i.e. more discriminating) than observed in cigarette-only users. However, ‘using soon after getting up’ (bCigar= 0.34; bCigarette= −0.27; difference=0.61) and ‘just after use was not permitted’ (bCigar= 0.46; bCigarette= −0.18; difference=0.64) reflected significantly higher levels of ND among cigar-only than among cigarette-only users. Among smokeless and cigarette-only users, responses to ‘using soon after getting up’ assessed ND similarly. Smokeless users reports of needing to use ‘Just after use was not permitted’ was not as strongly related to overall levels of ND as was observed for cigarette-only users. Smokeless users who endorsed this less discriminating symptom had higher levels of ND than cigarette-only users who endorsed this symptom.
3.4.4 Remaining symptoms
Among the seven remaining symptoms, ‘using tobacco more than intended’, ‘wanting to/trying to stop or cut down’, ‘giving up activities to use tobacco’, and ‘using tobacco even though anxious or depressed’ had the least amount of DIF across tobacco use groups. Reports of ‘chain smoking’ had stronger relationships with levels of ND within each of the tobacco-use groups than within cigarette-only users. Reports of ‘using tobacco despite health problems’ was associated with slightly higher levels of ND within each of the tobacco-use groups (bCigarette+Cigar= 0.32; bCigar= 0.44; bSmokeless=0.54; bCigarette= 0.15) than within cigarette-only users. ‘Waking up at night to use tobacco’ was more strongly associated with ND among cigar-only users. This symptom was less likely to be reported by smokeless users than among cigarette-only users (bSmokeless=1.87; bCigarette= 1.33).
3.5. A brief index for application across tobacco use groups
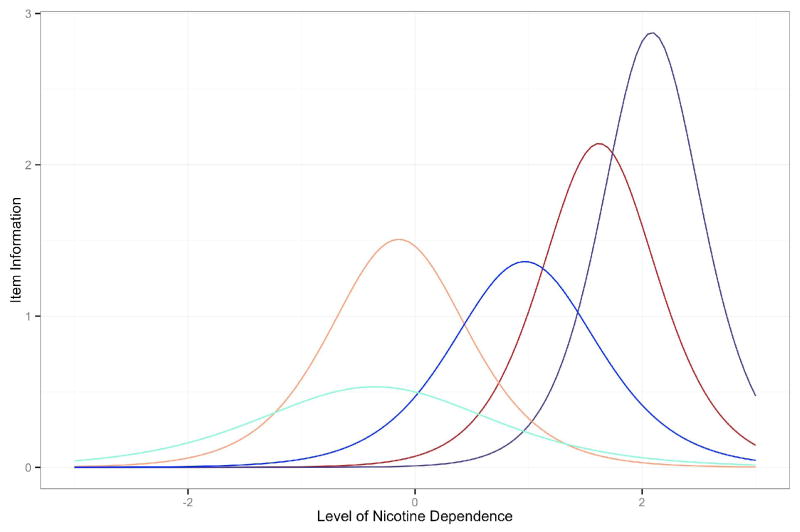
When selecting symptoms for an efficient index of ND across tobacco-use groups, we established four primary criteria. We looked to a) minimize redundancy of the content covered by symptom inquiries, b) ensure coverage of a broad range of levels of ND, c) select symptoms providing strong discrimination (information), and d) select symptoms with least DIF across use groups. Using these four guidelines, we selected a set of five symptoms; 1) ‘Want to/try stop or cut down’; 2) ‘Using just after getting up’; 3) ‘Using tobacco more than intended’; 4) ‘Using much more to get effect’; 5) ‘Nicotine withdrawal syndrome’. A plot reflecting the region of ND where each item contributes psychometric information is presented in Figure 1. We further selected a 3-symptom index using the same criteria and included symptoms 1, 2, and 4.
Figure 1.
Item Information functions for the five selected symptoms to map a broad range of Nicotine Dependence.
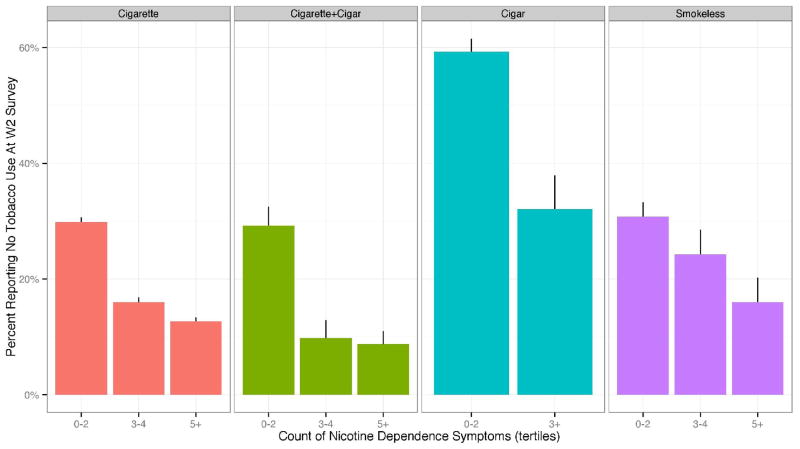
3.6. Concurrent and Predictive Validity of Extended and Brief Instruments
Concurrent use of tobacco was assessed with the questions ‘On the days that you (smoked/used snuff/chewed tobacco) during that period, about how many (cigarettes/cigars/pipe bowls of tobacco/pinches, dips or rubs/plugs, wads or chews) did you USUALLY (smoke/use) in a single day?‘ Given lack of comparability of the units of use for different products, we established an ordered grouping of Low, Medium, and High use groups based upon tertiles within each tobacco-use group. We then examined the association between observed levels of ND based upon a count of symptoms and level of tobacco use (e.g., Low, Medium, High). Using the wave 1 survey, Spearman rank correlations associating a count of the 13 ND symptoms and increasing levels of quantity were 0.38, 0.41, 0.37, and 0.42 for cigarette-only, cigarette+cigar, cigar-only, and smokeless tobacco-use groups respectively (p-values <0.01). When we examined the count of the 5-symptom ND index, correlations were 0.32, 0.35, 0.36, and 0.36, respectively. Associations were similar when using the 3-symptom index with correlations of 0.41, 0.43, 0.36, and 0.39, respectively. These significant correlations (p-values <0.01) support the concurrent validity of these indices of ND.
We hypothesized that higher levels of ND at W1 would be predictive of a decreased chance of quitting tobacco-use by the W2 assessment. The primary dependent variable was a report of no tobacco use in 12 months prior to the W2 interview. As planned covariates we included age, gender, racial/ethnic group, and education along with tobacco use group. Levels of ND scores from the raw 13-, 5-, and 3-symptom scales were classified into three-levels using W1 tertiles to facilitate comparisons of predictive validity.
Table 4 lists logistic regression model coefficients and computed odds ratios (OR). Relative to cigarette-only users, cigarette+cigar users had similar odds of quitting (OR=0.87, p>0.10). Cigar-only users (OR=4.85, p<0.01) and smokeless users (OR=1.72, p<0.01) had significantly higher odds of quitting at W2 than cigarette-only users. When added to other terms, the two dummy-coded terms comparing increasing levels of ND at W1 were consistently associated with lower odds of reporting quitting at W2. When compared to the lowest tertile, tobacco users reporting 3–4 (OR= 0.47, p<0.01) or 5+ (OR=0.36, p<0.01) of the 13 ND symptoms had significantly lower odds of quitting. We also observed significant decreases in odds of quitting when comparing increasing tertiles to the lowest tertile using the 5-symptom and 3-symptom scales (p-values < 0.01). The pattern of relationships and magnitude of association with the odds of quitting were similar for the 13-symptom, 5-symptom (A1) and 3-symptom (A2) ND indices. The two-way interaction effects of the 13-symptom (p<0.31), 5-symptom (p<0.10) and 3-symptom (p<0.16) ND indices and tobacco use group were not significant statistically.
Table 4.
Results from separate logistic regression models predicting point abstinence from tobacco use at wave 2 using wave 1 count of observed symptoms of nicotine dependence.
| Levels of Nicotine Dependence | Effect | S.E | OR | Lower 95% CI | Upper 95% CI | p |
|---|---|---|---|---|---|---|
| Tobacco Groupa | ||||||
| Cigarette | Reference | |||||
| Cigarette+Cigar | −0.14 | 0.13 | 0.87 | 0.67 | 1.12 | 0.28 |
| Cigar | 1.58 | 0.11 | 4.85 | 3.93 | 5.99 | <0.01 |
| Smokeless | 0.54 | 0.11 | 1.72 | 1.39 | 2.12 | <0.01 |
| With Thirteen Symptom Scale | ||||||
| Dependence.Group - 3-4:0-2 | −0.76 | 0.07 | 0.47 | 0.41 | 0.53 | <0.01 |
| Dependence.Group - 5+:0-2 | −1.03 | 0.07 | 0.36 | 0.31 | 0.41 | <0.01 |
| With Five Symptom Scale (A1) | ||||||
| Dependence.Group.A1 - 1-2:0 | −0.79 | 0.06 | 0.45 | 0.40 | 0.51 | <0.01 |
| Dependence.Group.A1 - 3+:0 | −1.21 | 0.09 | 0.30 | 0.25 | 0.35 | <0.01 |
| With Three Symptom Scale (A2) | ||||||
| Dependence.Group.A2 - 1-2:0 | −0.84 | 0.06 | 0.43 | 0.38 | 0.48 | <0.01 |
| Dependence.Group.A2 - 3:0 | −1.22 | 0.13 | 0.30 | 0.23 | 0.38 | <0.01 |
Note:
Logistic regression models adjusted for age, gender, racial/ethnic group, and education. Five symptom scale (A1): 1) want to stop/cut down; 2) Use soon after getting up; 3) use more than intended; 4) ever use much more than usual to get effect; 5) nicotine withdrawal. Three-symptom scale (A2) includes symptoms 1, 2, and 4. Interaction between Tobacco Group and Dependence Group was not significant.
4. DISCUSSION
In this analysis of data from the NESARC, we developed and compared three hierarchical indices of ND and identified a parsimonious and psychometrically sound 3-symptom index (’want to/try stop or cut down’; ’using just after getting up’; and ‘using much more to get effect’). Across tobacco-use groups, this index had similar predictive and concurrent validity with the two longer indices. The 3-item index also significantly correlated with quantity of products consumed and predicted successful cessation at Wave 2, independent of demographic covariates. The categorization of severity of ND was not substantially different from that obtained using the longer indices.
Overall, levels of ND were lowest among cigar-only users and highest among cigarette-only smokers and users of both cigarettes and cigars. We observed similar patterns of symptoms across tobacco-use groups with similar levels of ND. The similarity in patterns of symptoms was particularly notable for cigar only users who typically have distinctly intermittent use patterns when compared to cigarette-only smokers. The lowest levels of ND were associated with a persistent desire to quit and use soon after being restricted from tobacco use. The highest levels of ND were associated with giving up activities to use tobacco and experience of the full withdrawal syndrome when deprived of tobacco. These patterns of symptoms across increasing levels of ND were consistent with previous examinations of the continuum of ND (Saha et al., 2010; Strong et al., 2003). Two symptoms, ‘use just after getting up’ and ‘use despite health problems’ were associated with low levels of ND in the current study while in previous studies, similar symptoms were associated with high levels of ND (Strong et al., 2003, 2011). Previous studies included response options with narrowed time frames (e.g., smoking within 5 minutes of waking) and severe conditions (e.g., difficulty breathing, problems with your heart) as referents that may have raised levels of ND associated with these more severe manifestations of these domains. The ND symptoms in the current study provided a broad range of measurement of ND and had significant concurrent association across tobacco-use groups. Observed moderate correlations between levels of ND and quantity of tobacco consumed were similar across groups and were consistent with other investigations of cigarette users and smokeless users (Ebbert et al., 2012; Ferketich et al., 2007; Hatsukami et al., 1999; Shiffman et al., 2004). Furthermore, this study offers much needed validation of ND and quantity of tobacco consumed among cigar users where little comparative studies are available (Henningfield et al., 1999). Given more common patterns of intermittent use than cigarette-only users, we expected and observed lower overall levels of ND among cigar-only users. Despite different patterns of use, each of the ND instruments provided evidence of predictive validity that was similarly strong across all tobacco-use groups. This is notable given that past studies using ND measures to predict cessation outcomes have demonstrated limited associations (Breslau and Johnson, 2000).
We did not detect systematic group differences in measurement of ND, particularly when examining physiological symptoms reflecting Tolerance and Withdrawal. When we did observe significant DIF, it was generally confined to behavioral symptoms. For example, asking about the need to use tobacco ‘just after use was not permitted’ yielded slightly different information among non-cigarette users as compared to cigarette-only users. This may be due to difference in typical use patterns across tobacco-use groups (e.g., more time in between use of cigars than cigarettes), and the fact that smoke-free workplaces do not proscribe smokeless tobacco use. When behavior reflected in a symptom might be influenced by product specific factors other than ND, we observed a shift in the severity of ND reflected by the symptom. The shift in severity suggested that the behavior was still associated with ND in non-cigarette users, but was associated with slightly higher levels of ND than the same symptom observed among cigarette-only users. Alternatively, when behaviors may not reflect ND as consistently within non-cigarette users, we observed weakened discrimination estimates. Despite these differences, we were able to identify a majority of ND symptoms that were consistent across tobacco-use groups, which were used to generate shortened scales.
Our approach reduced a broad set of ND symptoms into a minimum set of 3 symptoms that satisfactorily represent the ND construct. These 3 symptoms are: ’want to/try stop or cut down’; ’using just after getting up’; and ‘using much more to get effect’. These domains provided symptoms with strong psychometric properties (e.g., information functions, minimal DIF) across tobacco-use groups and maintained concurrent relationships with tobacco use and predictive associations with tobacco use cessation. This minimal set of 3 symptoms provides a new tool for measuring ND in the population. Support for this parsimonious and psychometrically sound metric across tobacco-use groups underscores its utility in measuring tobacco use in an evolving marketplace of tobacco and nicotine products.
These results add to a growing literature that demonstrates the benefit of using methods based in item response theory to understand the tobacco use phenotype. This is accomplished by assessing the development, course, and differential expression of ND symptom under varied tobacco-use patterns and products. These methods also enabled identification of overlap among symptoms as opportunities for increasing the reliability of measures (Conway et al., 2010; Courvoisier and Etter, 2008; McBride et al., 2010; Saha et al., 2010), for selecting symptoms to generate an efficient short-form (Strong et al., 2012), for enabling consistent measurement across important demographic groups (Strong et al., 2003; Yamada et al., 2009), evaluating measurement of ND across critical developmental periods (Liu et al., 2013; Rose and Dierker, 2010a, 2010b), enabling pooling of studies using common symptoms (Rose et al., 2013), and for signaling the need for developing new symptom questions (Reise and Waller, 2009). Item response models are flexible in that they allow assessment of covariates when estimating levels of ND, a facility that may be used to address questions about user-characteristics and development of ND when mutually exclusive groupings may be difficult to establish a priori (Wainer et al., 2007). The current study extends existing research by establishing measurement of ND across tobacco use groups.
4.1 Limitations
The current study has several limitations including a truncated distribution of ND among cigar users that compromised our ability to evaluate a broad range of symptoms in this use group. We also had limited ability to refine the definition of cigar use, which did not allow assessment of potential differences between filtered cigar and large cigar users. We had small sample sizes for analysis of groups other than the smokers, and incomplete assessment of dependence/addiction items that were limited to DSM-IV/ICD-10 constructs. Additionally, we did not have a biological marker of nicotine exposure that could be linked to levels of reported tobacco use, which could have been informative for assessing ND. Finally, we were limited by the poor representation of symptoms at the lower range of the ND continuum. The available symptoms may best measure ND among established tobacco-users and may not be sensitive to early progression to regular tobacco use or escalating use patterns. More work will be needed among youth, in which the level of ND and the diversity of tobacco products and behaviors may be different in comparison to established adult smokers. The current study relied upon interviews first fielded in 2001–2002 and was unable to assess the diversity of tobacco products available in the current marketplace when examining ND symptoms. However, some of these limitations will be resolved with results from the PATH Study, which includes multiple measures of ND, biological samples collected from adults, and assessments of youth and adults at varying points along the tobacco-use trajectory. Replication of our results in this national sample is needed before this index can be disseminated widely.
4.2 Conclusion
We evaluated thirteen, five, and three ND symptom indices that demonstrated concurrent and predictive utility across tobacco-use groups in a multi-wave US national sample. We found little support for meaningful differences in symptoms of ND across different tobacco use groups. The concurrent and predictive validity of each of the brief sets of ND symptoms was supported. We established a set of parsimonious symptom domains that can be used to generate efficient and effective measurement of ND across users of different tobacco products.
Supplementary Material
Figure 2.
Rates of abstinence at Wave 2 among tobacco use groups.
Highlights.
We evaluate measurement of Nicotine Dependence across types of tobacco.
We found support for a common continuum of Nicotine Dependence across use groups.
We identified a short scale of Nicotine Dependence.
We found assessment of Nicotine Dependence to be similar in cigar only smokers.
Acknowledgments
Funding: This project has been funded with Federal funds from the National Institute on Drug Abuse, National Institutes of Health, and the Food and Drug Administration, Department of Health and Human Services, under Contract No. HHSN271201100027C. In addition, Drs. Strong, Pierce, Messer, Hartman, and Ms. White were partially supported on National Cancer Institute (1R01CA172058-01) and UC Tobacco-Related Disease Research Program grants (21XT-0076; 21RT-0135). The role of Drs. Hoffman, Pharris-Ciurej, Conway, Compton, and Ms. Green on this paper were through their involvement on contract No. HHSN271201100027C. They had no involvement in the cited grants.
Footnotes
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Contributors: Drs. Strong, Pierce, Messer and Conway designed the study. Dr. Strong conducted analyses in consultation with Dr. Messer and Ms. White. Drs. Hartman, Messer, Pierce, Hoffman, Pharris-Ciurej, Conway, Compton and Ms. Green and Ms. White made significant contributions to the background research, preparation, and drafting the manuscript. All authors participated in reviewing the data and editing of the final manuscript.
Conflict of Interest statement: Author W.M. Compton declares retirement account stock holdings in Pfizer, a manufacturer of tobacco cessation products. All other authors declare no conflicts of interest.
Disclaimer: The views and opinions expressed in this presentation are those of the authors only and do not necessarily represent the views, official policy or position of the US Department of Health and Human Services or any of its affiliated institutions or agencies.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic And Statistical Manual Of Mental Disorders. 5. American Psychiatric Publishing; Arlington, VA: 2013. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Breslau N, Johnson EO. Predicting smoking cessation and major depression in nicotine-dependent smokers. Am J Public Health. 2000;90:1122–1127. doi: 10.2105/ajph.90.7.1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai L. A two-tier full information item factor analysis model with applications. Psychometrika. 2010;75:581–612. [Google Scholar]
- Chalmers PR. mirt: a multidimensional item response theory package for the R environment. J Stat Softw. 2012;48:1–29. [Google Scholar]
- Collins AC, Marks MJ. Progress towards the development of animal models of smoking-related behaviors. J Addict Dis. 1991;10:109–126. doi: 10.1300/J069v10n01_08. [DOI] [PubMed] [Google Scholar]
- Conway KP, Levy J, Vanyukov M, Chandler R, Rutter J, Swan GE, Neale M. Measuring addiction propensity and severity: the need for a new instrument. Drug Alcohol Depend. 2010;111:4–12. doi: 10.1016/j.drugalcdep.2010.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courvoisier D, Etter JF. Using item response theory to study the convergent and discriminant validity of three questionnaires measuring cigarette dependence. Psychol Addict Behav. 2008;22:391–401. doi: 10.1037/0893-164X.22.3.391. [DOI] [PubMed] [Google Scholar]
- Ebbert JO, Severson HH, Danaher BG, Schroeder DR, Glover ED. A comparison of three smokeless tobacco dependence measures. Addict Behav. 2012;37:1271–1277. doi: 10.1016/j.addbeh.2012.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards G, Gross MM. Alcohol dependence: provisional description of a clinical syndrome. BMJ. 1976;1:1058–1061. doi: 10.1136/bmj.1.6017.1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferketich AK, Wee AG, Shultz J, Wewers ME. A measure of nicotine dependence for smokeless tobacco users. Addict Behav. 2007;32:1970–1975. doi: 10.1016/j.addbeh.2007.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatsukami DK, Jensen J, Boyle R, Grillo M, Bliss R. Characteristics of smokeless tobacco users seeking treatment. Addict Behav. 1999;24:551–557. doi: 10.1016/s0306-4603(98)00092-6. [DOI] [PubMed] [Google Scholar]
- Henningfield JE, Fant RV, Radzius A, Frost S. Nicotine concentration, smoke pH and whole tobacco aqueous pH of some cigar brands and types popular in the United States. Nicotine Tob Res. 1999;1:163–168. doi: 10.1080/14622299050011271. [DOI] [PubMed] [Google Scholar]
- Liu LC, Hedeker D, Mermelstein RJ. Modeling nicotine dependence: an application of a longitudinal IRT model for the analysis of adolescent nicotine dependence syndrome scale. Nicotine Tob Res. 2013;15:326–333. doi: 10.1093/ntr/nts125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride O, Strong DR, Kahler CW. Exploring the role of a nicotine quantity-frequency use criterion in the classification of nicotine dependence and the stability of a nicotine dependence continuum over time. Nicotine Tob Res. 2010;12:207–216. doi: 10.1093/ntr/ntp196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health, and Food and Drug Administration. PATH Population of Tobacco and Helath. 2014 from http://www.pathstudyinfo.nih.gov/UI/HomeMobile.aspx.
- Reise SP, Waller NG. Item response theory and clinical measurement. Annu Rev Clin Psychol. 2009;5:27–48. doi: 10.1146/annurev.clinpsy.032408.153553. [DOI] [PubMed] [Google Scholar]
- Rose JS, Dierker LC. DSM-IV nicotine dependence symptom characteristics for recent-onset smokers. Nicotine Tob Res. 2010a;12:278–286. doi: 10.1093/ntr/ntp210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose JS, Dierker LC. An item response theory analysis of nicotine dependence symptoms in recent onset adolescent smokers. Drug Alcohol Depend. 2010b;110:70–79. doi: 10.1016/j.drugalcdep.2010.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose JS, Dierker LC, Hedeker D, Mermelstein R. An integrated data analysis approach to investigating measurement equivalence of DSM nicotine dependence symptoms. Drug Alcohol Depend. 2013;129:25–32. doi: 10.1016/j.drugalcdep.2012.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha TD, Compton WM, Pulay AJ, Stinson FS, Ruan WJ, Smith SM, Grant BF. Dimensionality of DSM-IV nicotine dependence in a national sample: an item response theory application. Drug Alcohol Depend. 2010;108:21–28. doi: 10.1016/j.drugalcdep.2009.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Waters A, Hickcox M. The nicotine dependence syndrome scale: a multidimensional measure of nicotine dependence. Nicotine Tob Res. 2004;6:327–348. doi: 10.1080/1462220042000202481. [DOI] [PubMed] [Google Scholar]
- Steinberg L, Thissen D. Using effect sizes for research reporting: examples using item response theory to analyze differential item functioning. Psychol Methods. 2006;11:402–415. doi: 10.1037/1082-989X.11.4.402. [DOI] [PubMed] [Google Scholar]
- Strong DR, Kahler CW, Ramsey SE, Brown RA. Finding order in the DSM-IV nicotine dependence syndrome: a Rasch analysis. Drug Alcohol Depend. 2003;72:151–162. doi: 10.1016/s0376-8716(03)00201-1. [DOI] [PubMed] [Google Scholar]
- Strong DR, Schonbrun YC, Schaffran C, Griesler PC, Kandel D. Linking measures of adult nicotine dependence to a common latent continuum and a comparison with adolescent patterns. Drug Alcohol Depend. 2012;120:88–98. doi: 10.1016/j.drugalcdep.2011.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Team, R. C. R: A Language And Environment For Statistical Computing. R Foundation for Statistical Computing; Vienna, Austria: 2014. [Google Scholar]
- United States Department of Health and Human Services. The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 2014. [Google Scholar]
- Wainer H, Bradlow ET, Wang X. Testlet Response Theory and Its Applications. Cambridge University Press; New York, NY: 2007. [Google Scholar]
- Wang X, Bradlow ET, Wainer H, Muller ES. A Bayesian method for studying dif: a cautionary tale filled with surprises and delights. J Educ Behav Stat. 2008;33:363–384. [Google Scholar]
- World Health Organization. ICD-10: International Statistical Classification Of Diseases And Related Health Problems. 10. WHO; New York, NY: 2008. Rev. ed. [Google Scholar]
- Yamada H, Acton GS, Tsoh JY. Differential item functioning of the English and Chinese versions of the Fagerstrom Test for Nicotine Dependence. Addict Behav. 2009;34:125–133. doi: 10.1016/j.addbeh.2008.09.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.