Abstract
Background
To produce population-level, year- and age-specific risk estimates of first time nonmedical use of prescription stimulants among young people in the United States.
Methods
Data are from the National Surveys on Drug Use and Health 2004–2012; a nationally representative probability sample survey administered each year. Subpopulations included youths aged 12 to 21 years (n=240,160) who had not used prescription stimulants nonmedically prior to their year of survey assessment. A meta-analytic approach was used to produce population-level age-, year-, and cohort-specific risk estimates of first time nonmedical use of prescription stimulants.
Results
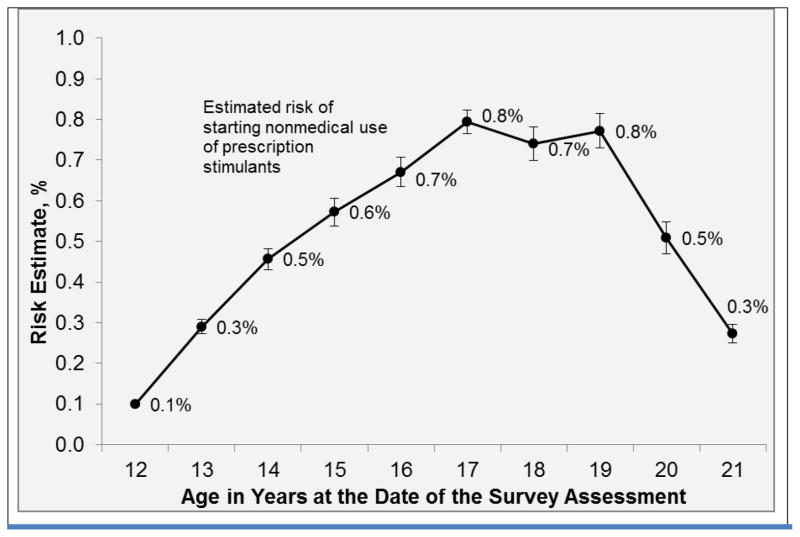
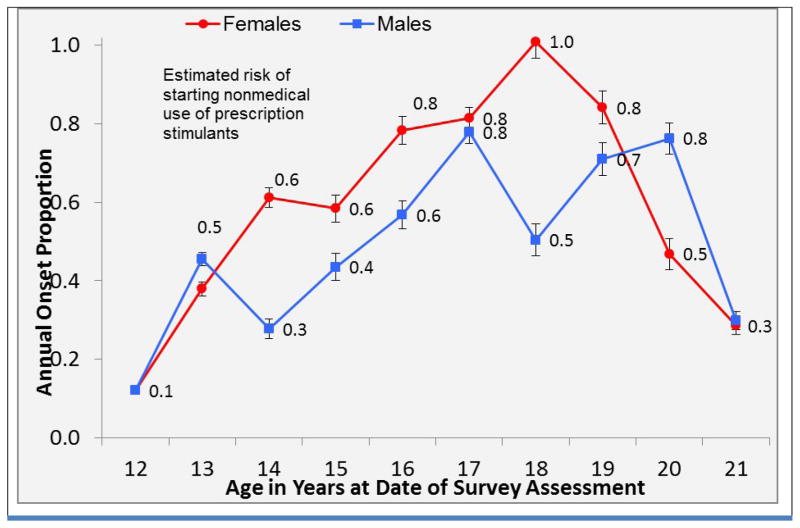
Peak risk of starting nonmedical use of prescription stimulants was concentrated between ages 16 and 19 years, when an estimated 0.7% to 0.8% of young people reported nonmedical use of these medicines for the first time in the past twelve months. Smaller risk estimates ranging from 0.1% to 0.6% were observed at ages 12 to 15 years and 20 to 21 years. Compared with males, females were more likely to have started nonmedical use of prescription stimulants (odds ratio = 1.35; 95% CI, 1.13–1.62), particularly between the ages of 14 and 19. Females showed a peak annual incidence rate of 1% at age 18, while males the same age showed an incidence rate of 0.5%.
Conclusions
Peak annual incidence rates for nonmedical use of prescription stimulants were observed between the ages of 16 and 19 years. There is reason to initiate interventions during the earlier adolescent years to prevent youths from starting nonmedical use of prescription stimulants.
Keywords: adolescent, nonmedical use, stimulant
1. INTRODUCTION
Many nationally representative studies reporting past-year and lifetime prevalence rates for nonmedical use of stimulants do not differentiate between first time nonmedical use and nonmedical use that persists years after onset (i.e., use of prescription stimulants that were not prescribed to the user or that the user took only for the experience or feeling they caused). Past-year and lifetime prevalence rates for nonmedical use are informative, but ultimately may convey more information about persistence in nonmedical use than the timing of initiation among youth. To produce reliable age-specific incidence rates for nonmedical use (i.e., peak ages of onset), it is necessary to separate first-time users from sporadic or persistent nonmedical users by excluding the latter from the sample, or by separately analyzing data from these two different types of users (Austic et al., in press; Deandrea et al., 2013; Harris et al., 2008; Meier et al., 2012). The present study is one of only a few to estimate peak age of onset for nonmedical use (Austic et al., in press; Deandrea et al., 2013; Meier et al., 2012), and is the only nationally representative study to produce age-specific incidence rates for nonmedical use of stimulants among young people in the United States (US). Age-specific incidence rates for youth provide crucial information needed to design timely and effective primary prevention initiatives because they identify ages of lower risk directly preceding ages of peak risk for starting to misuse another person’s prescription or misuse one’s own prescription without a physician’s knowledge (Deandrea et al., 2013).
Nationally representative studies such as the Monitoring the Future have been criticized for lack of specificity in questions asked about different types of prescription stimulants (e.g., just asking about stimulants prescribed to treat attention deficit/hyperactivity disorder (ADHD; Rabiner, 2013). Since 1999, the National Survey on Drug Use and Health (NSDUH) has used a confidential multi-item nonmedical stimulant use assessment featuring color photographs of different formulations of prescription stimulants including but not limited to ADHD medication (Substance Abuse and Mental Health Services Administration (SAMHSA), 2014). While the NSDUH is not without limitations (Boyd and McCabe, 2008), NSDUH estimates are strong relative to available alternatives. Each year the NSDUH is administered to a new nationally representative sample of the US population and asks about past-year and lifetime nonmedical use of a broad range of prescription stimulants. In contrast with studies reporting mean age of onset (see results from the 2012a NSDUH study, SAMHSA, 2013a), the present study uses a meta-analytic approach that treats each NSDUH year’s independent sample – from 2004 to 2012 – as a separate study to identify peak ages at which young people in the US are most likely to start nonmedical use of prescription stimulants (i.e., first time nonmedical use in the past-year; Austic et al., in press; Deandrea et al., 2013; Harris et al., 2008; Meier et al., 2012). Based on epidemiological estimates previously published, it was anticipated that the present study would identify a peak risk for first time nonmedical use of prescription stimulants starting during the early college years (McCabe et al., 2014; McCabe and West, 2013).
2. METHODS
2.1. Study setting and data collection
Data are from the 2004 through 2012 National Survey on Drug Use and Health (NSDUH) with annual independently drawn nationally representative probability samples of US community residents age 12 years or older. The NSDUH sampling frames include youth who drop out of school and youth who attend school. Participation levels for 12 to 25 year old participants were acceptable, at 70% or better during the years under study (SAMHSA, 2014). Before any interviews were conducted, all consent processes and survey questions were approved by Research Triangle Institute institutional review boards for the protection of human subjects.
2.2. Study sample
Pooled across years, a total of 250,910 respondents aged 12 to 21 years participated in the 2004 through 2012 NSDUH, and were included in public use files. In the present sample, the mean size of age groups (± standard deviation) was 24,007±3,606 and the mean size of year groups was 26,675±770. A confidential multi-item nonmedical stimulant use assessment with color photographs of prescription stimulant compounds identified the newly incident nonmedical users of prescriptions stimulants.
2.3. Study medication items and risk groups
One audio-enhanced, computer-assisted self-interview module provided the following prompt:
“We are not interested in your use of over-the-counter stimulants such as Dexatrim or No-Doz that can be bought in drug stores or grocery stores without a doctor’s prescription. Card C shows pictures of some different types of prescription stimulants and lists the names of some others. These pictures show only pills, but we are interested in your use of any form of prescription stimulants that were not prescribed for you or that you took only for the experience or feeling they caused.”
Respondents were asked first about their nonmedical use of three classes of stimulants: (1) methamphetamine, Desoxyn®, or Methedrine®; (2) prescription diet pills such as amphetamines, Benzedrine®, Biphetamine®, Fastin®, or Phentermine; and (3) Ritalin® or methylphenidate. Then they were asked whether they had used any stimulant from the list: Cylert®; Dexedrine®; Dextroamphetamine; Didrex®; Eskatrol®; Ionamin®; Mazanor®; Obedrin-LA®; Plegine®; Preludin®; Sanorex®; and Tenuate (SAMHSA, 2013a). If they indicated they had used any of these drugs, they were asked which one(s). In addition, respondents were asked if they had “ever, even once, used any type of prescription stimulant that was not prescribed to you or that you took only for the experience or feeling it caused.” If they answered, “yes” to this question, they were asked how old they were the first time this happened, and asked to name any other prescription stimulants they had used nonmedically.
Newly incident users were identified by comparing each individual’s age on the date of assessment with the age they reported first using any type of prescription stimulant that was not prescribed to them or that they took “only for the experience or feeling it caused.” The estimates herein are based upon a subpopulation of 240,160 respondents aged 12 to 21 years whose self-report assessment indicated that they had never engaged in nonmedical use of prescription stimulants before the year in which they were assessed for the NSDUH; 10,750 (4.3%) did not contribute to the study estimates for incidence of use because they had already initiated such use before the year in which they were surveyed. In other words, as of the date of assessment, subpopulations in the estimation sample either were never users (who were still at risk for starting use in a later year) or were newly incident users (who had just started to use for the first time).
2.4. Data analysis
Year- and age-specific incidence rates were estimated with weighting and survey estimation appropriate for the NSDUH complex survey data (Stata, version 13). The meta-analysis summary estimates reported are not simple means, as frequently reported in annual NSDUH reports; they were calculated using a random effects meta-analysis software program that weights each year by the inverse of its variance (Harris et al., 2008). Standard errors for the estimates were all relatively small (< 0.1) because of the large NSDUH samples.
Stratum-specific estimates of cumulative incidence proportion can be calculated as a ratio of the number of newly incident users divided by the sum of the number of ‘never users’ plus the number of newly incident users. With age as a marker of cohort membership, the result is a set of year-by-year and age by age risk estimates, which makes it possible to trace the experience of individual cohorts over time without a repeated measures survey design (Kroutil, 2010). For example, one cohort sampled was aged 12 in 2004, aged 13 in 2005, and aged 14 in 2006.
Previous publications describe in detail the approach used to identify newly incident users, past-onset users, and never users (Deandrea et al., 2013; Meier et al., 2012). Additional logistic regression analyses were conducted to predict the probability of subpopulations starting to engage in nonmedical use of prescription stimulants for the first time based on race or sex based on findings from past studies demonstrating race/ethnicity and sex differences in lifetime and past year nonmedical use of prescription stimulants (McCabe et al., 2014; McCabe and West, 2013).
3. RESULTS
3.1. Newly incident user characteristics
Table 1 describes the study sample and reports unweighted frequencies and weighted proportions for subgroupings of newly incident users based on demographic characteristics. The main study estimates given in Table 2 are weighted proportions of newly incident prescription stimulant users. These estimates include a tracing of individual cohorts, age-specific patterns, and age-year-cohort patterns of concentrated risk. For example, an estimated 0.4% of respondents who were aged 14 years in 2004 started nonmedical use of prescription stimulants in the previous year. The US population cohort of 14 year olds in 2004 was newly sampled in 2005 when the cohort passed their 15th birthdays. The risk estimate for this new sample of respondents, aged 15 years in 2005, was 0.8%. Examining the cells in Table 2 by age and year, this cohort’s risk estimate for starting nonmedical use of prescription stimulants was 0.8% at age 16 in 2006, and peaked to 1.1% (around 1 in 100) at age 18 years in 2008 (i.e., 1.1% was the largest observed value in that population cohort’s series of estimates from 2004 through 2011), and then dropped to 0.4% at age 21 in 2011.
Table 1.
Characteristics of young people at risk of starting nonmedical use of prescription stimulants in the United States (n=240,160)a
| Characteristic | Unweighted Frequency (n=240,160) | Weighted % (n=240,160) | Newly Incident Users, Frequency (Weighted %)b (n=1,232) |
|---|---|---|---|
| ‘At risk’ individuals 12–21 years | 240,160 | 100 | 1,232 (5) |
| Newly incident users | 1,232 | 0.5 | 1,232 (100) |
| Gender | |||
| Female | 119,196 | 48.7 | 729 (56) |
| Male | 120,964 | 51.3 | 503 (44) |
| Race/ethnicityc | |||
| Non-Hispanic White | 142,397 | 58.3 | 906 (75) |
| Non-Hispanic Black | 33,950 | 15.1 | 57 (5) |
| Non-Hispanic Native American/Alaskan Native | 3,653 | 0.6 | 25 (1) |
| Non-Hispanic Native Hawaiian/Pacific Islander | 1,135 | 0.4 | 4 (<1) |
| Non-Hispanic Asian | 7,995 | 4.5 | 22 (2) |
| Non-Hispanic Multiracial | 9,124 | 1.9 | 63 (3) |
| Hispanic | 41,906 | 19.2 | 155 (13) |
| Population density | |||
| Metropolitan Statistical Area with ≥ 1million | 97,926 | 49.7 | 487 (50) |
| Metropolitan Statistical Area with < 1million | 116,383 | 41.8 | 612 (42) |
| Not in a Metropolitan Statistical Area | 25,851 | 8.5 | 133 (8) |
Data are from the US National Surveys on Drug use and Health 2004–2012; 10,750 (4.3%) individuals excluded who had previously misused stimulants.
Unweighted frequencies and weighted proportions reported.
Self-reported by respondents.
Table 2.
Risk estimates by age and year of assessment of starting nonmedical use of prescription stimulants per 100 young people in the United States (n=240,160)a
| Age in Years on Date of Survey Assessment | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | |
| 2004 | 0.1 | 0.5 | 0.4 | 1.4 | 1.3 | 0.6 | 0.8 | 1.2 | 0.7 | 0.1 |
| 2005 | 0.0 | 0.2 | 0.5 | 0.8 | 0.6 | 0.7 | 0.7 | 0.8 | 0.5 | 0.1 |
| 2006 | 0.1 | 0.2 | 0.8 | 0.8 | 0.8 | 1.3 | 0.8 | 0.4 | 0.2 | 0.3 |
| 2007 | 0.1 | 0.5 | 0.2 | 0.4 | 0.7 | 0.9 | 0.3 | 0.7 | 0.4 | 0.5 |
| 2008 | 0.1 | 0.4 | 0.7 | 0.3 | 0.7 | 0.6 | 1.1 | 0.5 | 0.1 | 0.4 |
| 2009 | 0.2 | 0.4 | 0.5 | 0.3 | 0.4 | 0.6 | 0.8 | 0.7 | 0.7 | 0.3 |
| 2010 | 0.1 | 0.2 | 0.3 | 0.5 | 0.5 | 0.7 | 0.7 | 0.9 | 0.6 | 0.2 |
| 2011 | 0.0 | 0.1 | 0.40 | 0.6 | 0.5 | 0.7 | 0.9 | 0.7 | 0.6 | 0.4 |
| 2012 | 0.1 | 0.3 | 0.5 | 0.2 | 0.5 | 0.9 | 0.6 | 1.1 | 0.8 | 0.1 |
Data are from the US National Surveys on Drug Use and Health 2004–2012; 10,750 (4.3%) individuals excluded who had previously misused stimulants. Weighted proportions are reported. Because of the large samples, all standard errors for these estimates were below 0.1%.
When Table 2 is studied year by year (row by row), 2004 (top row of Table 2) appears to be the year with the highest proportion of newly incident users across the 10 age groups (12–21 years) in a comparison of values across years (2004–2012) within each age group. When Table 2 is studied age by age (column by column), ages 16 through 19 stand out as ages with the highest proportion of newly incidence users across the years (2004–2012) in a comparison of values across age groups (12–21 years) within each year. Still, considerable variability may be observed within any given year and age group.
3.2. Meta-analysis summary estimates for newly incident users
Figure 1 shows meta-analysis summary estimates for age-specific risk of starting nonmedical use of prescription stimulants based on weighted proportions – Figure 2 shows these estimates by sex. Shown in Figure 1 are the peak risks, concentrated between age 16 and 19, and the lower age-specific risk estimates between ages 12 to 15 years and between ages 20 to 21 years. These estimates are based on all of the age-specific risk estimates given in Table 2, integrated via a standard meta-analysis for independently drawn samples (Harris et al., 2008).
Figure 1.
Meta-analysis summary estimates: Age-specific risk of starting nonmedical use of prescription stimulants Figure 1. Age-specific incidence rate estimatesa (with standard error bars) for newly incident nonmedical use of prescription stimulants. Data are from the US National Surveys on Drug Use and Health 2004–2012 (n=240,160). a Age-specific summary estimates based on meta-analysis of estimates based on weighted proportions; each year provides an independent sample.
Figure 2.
Meta-analysis summary estimates: Age-specific risk of starting nonmedical use of prescription stimulants, by sex. Age-specific incidence rate estimatesa (with standard error bars) for newly incident nonmedical use of prescription stimulants, by sex. Data are from the US National Surveys on Drug Use and Health 2004–2012 (n=240,160). a Age-specific summary estimates based on meta-analysis of estimates based on weighted proportions; each year provides an independent sample.
Figure 2 shows that the age specific risk of newly incident nonmedical prescription stimulant use was higher among females than males between the ages of 14 and 19 except at age 17, when the incidence rate was 0.8% for both males and females. Females showed a peak annual incidence rate of 1% at age 18, which was twice the rate of males at that age (0.5%).
Compared with (weighted proportions for) all other race/ethnicity groups, non-Hispanic White and Native American subpopulations were each more likely to have started nonmedical use of stimulant medicines (White odds ratio = 2.15, 95% CI, 1.81–2.54, P<0.001; Native American odds ratio = 2.31, 95% CI, 1.06–5.02, P=0.035). 1.17% (weighted proportions reported) of Native American and 0.66% of White subpopulations were newly incident nonmedical users of prescription stimulants, compared with 0.31% of subpopulations belonging to all other race/ethnicity groups (i.e., excluding White and Native American subpopulations).
3.3 Race and gender differences by subtypes of prescription stimulant compounds
Logistic regression analyses were conducted to test for race and gender differences in initiation by subtypes of prescription stimulant compounds (subtypes described in the Methods section). Results indicated that White subpopulations were more likely to initiate nonmedical use of prescription stimulants with Ritalin or methylphenidate, compared with non-White subpopulations (odds ratio, 1.95, 95% CI 1.35–2.82, P=0.001).
Females represented 48.7% of the sample (based on weighted proportions), yet 56.2% (based on weighted proportions) of the 1,232 who initiated nonmedical use of prescription stimulants in the past year. Results from logistic regression analyses indicated that the odds of starting nonmedical use of prescription stimulants were higher among females (odds ratio = 1.35; 95% CI, 1.13–1.62, P=0.001).
Diet pills and Adderall were the only subtypes of stimulant medication showing sex differences. Females initiated nonmedical use of stimulants with diet pills at nearly twice the rate of males (24.1%, compared with 12.8%) (odds ratio = 2.17; 95% CI, 1.37–3.44, P=0.001) while males were more likely to initiate nonmedical use of stimulants with Adderall (25.9%, compared with 18.5% for females) (odds ratio = 1.55; 95% CI, 1.07–2.24, P=0.021).
4. DISCUSSION
In this article, the results are reported from a meta-analysis on the relationship between age and risk of starting nonmedical use of stimulants among young people in the United States. Between the ages of 12 and 21, 1,232 (5%) of the 240,160 youths surveyed who had not used prescription stimulants nonmedically prior to their year of survey assessment reported that they had begun such use for the first time in the past year. The peak years of risk for first time nonmedical use of prescription stimulants started at age 16, during the high school years, rather than during the early college years as was anticipated. Based on this study’s estimates for each year between 2004 and 2012, the average annual incidence rate across age groups (12 to 21 years) was 0.5% (around 1 in 200). Nonetheless, the peak risk was concentrated between ages 16 and 19 years, when 0.7% to 0.8% of youths started nonmedical use each year. Lower risk estimates were observed for ages 12 to 15 years and for ages 20 to 21 years, as seen in Figure 1 – a trend that may be confirmed by tracing the experience of individual cohorts across the survey years under study along the diagonal in Table 2.
Consistent with findings from other studies, White and Native American youths were at greater risk for starting to nonmedically use prescription stimulants (Kroutil et al., 2010; McCabe et al., 2014; McCabe and West, 2013). Results from this study indicated that females were at greater risk of starting to misuse their own or another person’s prescription stimulants. Notably, females showed a peak annual rate of onset of 1% (1 in 100) at age 18, compared to 0.5% (1 in 200) among 18-year-old males. Future studies could explore the possibility that this difference might be a consequence of females choosing to initiate prescription stimulants for weight loss at a higher rate than males (24.1%, compared with 12.8%). Another possibility to consider is that stimulant medication therapy for ADHD decreases subsequent risk for nonmedical use of prescription stimulants, and since males are twice as likely to receive this type of therapy, males may be less likely to start nonmedically using prescription stimulants than females (Barkley et al., 2003; Biederman et al., 1999; Kaloyanides, et al., 2007; Katusic, 2005; Mannuzza et al., 2008; McCabe, 2006; Visser et al, 2014).
A recent national report based on retrospective age of onset data collected from respondents age 12 to 49 years in the 2012 National Survey on Drug Use and Health (NSDUH) stated that the average age of onset was 22.1 years for first time stimulant nonmedical use (SAMHSA, 2013b). In contrast to research on individuals aged 12 to 49 years, for whom the latest possible age of onset is 49 years, the sample for the present study included young people aged 12 to 21 years. Perhaps more important, the present study’s focus was on newly incident nonmedical users of prescription stimulants (i.e., young people who just started to use these compounds during the year in which they were surveyed). When an analysis is based on all persons with a lifetime or recent history of drug use (e.g., those with any use in the 12 months before the assessment), the resulting estimates are based on the aggregate of experience across multiple cohorts and years. Those estimates will be higher than estimates of first time use in the past year, and will also include the experience of drug users who have been using for many years and who may not have a clear memory of the exact age of first use. One advantage of focusing on newly incident users within a younger age range (e.g., age 12 to 21) is a constrained reliance on long-term memory about age of onset many years ago. In this project, the elapsed time from initial use to the date of the interview was constrained to be less than 12 months.
Consistent with this study’s focus on newly incident use, 4.3% of the NSDUH respondents aged 12 to 21 years during 2004 to 2012 were excluded from estimates of cumulative incidence because they had engaged in nonmedical use of prescription stimulants during the years before the year in which they were surveyed (and were no longer considered at risk of newly incident use). This excluded group of lifetime nonmedical users of prescription stimulants represents roughly 1 in 25 of the young people in this nationally representative sample (not including newly incident users). While such lifetime use estimates can be important indicators of the magnitude of a problem, patterns of newly incident use more clearly highlight when the most effective time might be to prevent first use or intervene during the earliest stages of a drug dependence process (Chen et al., 2009; McCabe et al., 2007).
4.1. Limitations
Limitations of the study include the self-report character of NSDUH national sample survey data. Toxicological analysis remains beyond the scope of large nationally representative community samples on this scale and it is unclear that any drug assay would eliminate uncertainty about the age of starting nonmedical use of prescription stimulants. For example, some users would have positive urine screens due to legitimately prescribed stimulant use for approved indications (e.g., treatment for ADHD). As another potential error, some degree of survey nonparticipation raises the possibility that young people engaging in nonmedical use of prescription stimulants might not be wiling to participate in surveys of this type. Nonetheless, this source of error is constrained by focusing attention on young people who are just starting to use, most of whom may not have developed dependence problems or become disengaged from their family or from society at large within 12 to 24 months after the onset of such use (Barkley et al., 2003). In addition, a counterbalanced strength is that this survey is not restricted to young people who attend school; its sample is based on probability sampling of dwelling unit residents within each sampled community, as required for national representation of all youth. While youth in institutional settings (such as correctional and in-patient treatment facilities) were not included, each survey’s sampling frame has included youth irrespective of whether they maintain student status, have dropped out of school, are employed in the labor force, or are unemployed. These estimates are only for youth aged 12 to 21, thus findings cannot be generalized to the adult US population over age 21.
Although approximate estimates may be obtained from cross-sectional or longitudinal data using retrospective first age of use reports (as used in the present study), these limitations highlight the need for thoughtfully designed prospective studies to closely track and monitor cohort effects and annual incidence rates for substance use initiation. Error introduced by potential differences between the types of prescription stimulant compounds youth were nonmedically using year to year – versus the types of prescription stimulant compounds asked about in each year’s survey – cannot be ruled out with the present study. Finally, this study exclusively focused on nonmedical use of prescription stimulants. Future studies may use similar methods to examine initiation of illicit use of non-prescription stimulant compounds was not examined.
4.2. Conclusion
Results from this nationally representative, meta-analytic study indicate that peak annual incidence rates for nonmedical use of prescription stimulants among youth aged 12 to 21 were between the ages of 16 and 19 years. Due to the relatively low annual incidence rates observed, screening-based intervention programs may be cost prohibitive. These results draw attention to the timing of potential school-based and practice-based initiatives. If these initiatives are started in early adolescence, it may become possible to reduce the risks associated with youths starting to misuse someone else’s prescription or misuse their own prescription without a physician’s knowledge.
Highlights.
Data are from the United States National Surveys on Drug Use and Health 2004–2012.
A meta-analytic approach was used to identify ages of peak risk of initiation.
Risk estimates for nonmedical stimulant use are age-, year-, and cohort-specific.
Peak risk was concentrated between ages 16 and 19 years among young people.
Females were more likely to have started nonmedical use of prescription stimulants.
Acknowledgments
Funding Source: The development of this article was supported by National Institute on Drug Abuse grants R01DA024678, R01DA031160, R01DA016558, K05DA015799, T32DA021129, T32DA007267, and National Institutes of Health grant 2UL1TR000433-06.
Footnotes
Contributors: None (sole author manuscript).
Conflict of Interest: No conflict declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Austic EA, McCabe SE, Stoddard SA, Epstein-Ngo QM, Boyd CJ. Age and cohort patterns of controlled medication use and misuse among adolescents: 1991–2012. J Addict Med. doi: 10.1097/ADM.0000000000000142. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkley RA, Fischer M, Smallish L, Fletcher K. Does the treatment of attention-deficit/hyperactivity disorder with stimulants contribute to drug use/abuse? A 13-Year Prospective Study. Pediatrics. 2003;111:97–109. doi: 10.1542/peds.111.1.97. [DOI] [PubMed] [Google Scholar]
- Biederman J, Wilens T, Mick E, Spencer T, Faraone SV. Pharmacotherapy of attention-deficit/hyperactivity disorder reduces risk for substance use disorder. Pediatrics. 1999;104:e20. doi: 10.1542/peds.104.2.e20. [DOI] [PubMed] [Google Scholar]
- Boyd CJ, McCabe SE. Coming to terms with the nonmedical use of prescription medications. Subst Abuse Treat Prev Policy. 2008;3:22. doi: 10.1186/1747-597X-3-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen CY, Storr CL, Anthony JC. Early-onset drug use and risk for drug dependence problems. Addict Behav. 2009;34:319–22. doi: 10.1016/j.addbeh.2008.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deandrea DC, Troost JP, Anthony JC. Toward primary prevention of extra-medical OxyContin® use among young people. Prev Med (Baltim) 2013;57:244–246. doi: 10.1016/j.ypmed.2013.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris RJ, Bradburn MJ, Deeks JJ, Harbord RM, Altman DG, Sterne JAC. Metan: fixed- and random-effects meta-analysis. Stata J. 2008;8:3–28. [Google Scholar]
- Kaloyanides KB, McCabe SE, Cranford JA, Teter CJ. Prevalence of illicit use and abuse of prescription stimulants, alcohol, and other drugs among college students: relationship with age at initiation of prescription stimulants. Pharmacotherapy. 2007;27:666–674. doi: 10.1592/phco.27.5.666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katusic SK, Barbaresi WJ, Colligan RC, Weaver AL, Leibson CL, Jacobsen SJ. Psychostimulant treatment and risk for substance abuse among young adults with a history of attention-deficit/hyperactivity disorder: a population-based, birth cohort study. J Child Adolesc Psychopharmacol. 2005;15:764–776. doi: 10.1089/cap.2005.15.764. [DOI] [PubMed] [Google Scholar]
- Kroutil L, Colliver J, Gfroerer J. Age and Cohort Patterns of Substance Use Among Adolescents. OAS Data Review (Office of Applied Studies) Substance Abuse and Mental Health Services Administratio; Rockville, MD: 2010. pp. 1–9. [Google Scholar]
- Mannuzza S, Klein RG, Truong NL, et al. Age of methylphenidate treatment initiation in children with ADHD and later substance abuse: prospective follow-up into adulthood. Am J Psychiatry. 2008;165:604–609. doi: 10.1176/appi.ajp.2008.07091465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use and diversion of prescription stimulant medication. J Psychoactive Drugs. 2006;38:43–56. doi: 10.1080/02791072.2006.10399827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT. Medical and nonmedical use of prescription stimulants: results from a national multicohort study. J Am Acad Child Adolesc Psychiatry. 2013;52:1272–1280. doi: 10.1016/j.jaac.2013.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Morales M, Cranford JA, Boyd CJ. Does early onset of non-medical use of prescription drugs predict subsequent prescription drug abuse and dependence? Results from a national study. Addiction. 2007;102:1920–1930. doi: 10.1111/j.1360-0443.2007.02015.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, West BT, Teter CJ, Boyd CJ. Trends in medical use, diversion, and nonmedical use of prescription medications among college students from 2003 to 2013: connecting the dots. Addict Behav. 2014;39:1176–1182. doi: 10.1016/j.addbeh.2014.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier EA, Troost JP, Anthony JC. Extramedical use of prescription pain relievers by youth aged 12 to 21 years in the United States: national estimates by age and by year. Arch Pediatr Adolesc Med. 2012;166:803–807. doi: 10.1001/archpediatrics.2012.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabiner DL. Stimulant prescription cautions: addressing misuse, diversion and malingering. Curr Psychiatry Rep. 2013;15:375. doi: 10.1007/s11920-013-0375-2. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: 2013a. NSDUH Series H-46, HHS Publication No. (SMA) 13-4795. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Results from the 2012 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: 2013b. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) National Survey on Drug Use and Health (NSDUH) Methodological Resource Book. Rockville, MD: 2014. [PubMed] [Google Scholar]
- Visser SN, Danielson ML, Bitsko RH, et al. Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. J Am Acad Child Adolesc Psychiatry. 2014;53:34–46. doi: 10.1016/j.jaac.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]