Abstract
Local agencies that enforce housing policies can partner with the health care system to target pediatric asthma care. These agencies retain data that can be used to pinpoint potential clusters of high asthma morbidity. We sought to assess whether the density of housing code violations in census tracts—the in-tract asthma-relevant violations (such as the presence of mold or cockroaches) divided by the number of housing units—was associated with population-level asthma morbidity and could be used to predict a hospitalized patient’s risk of subsequent morbidity. We found that increased density in housing code violations was associated with population-level morbidity independent of poverty, and that the density explained 22 percent of the variation in rates of asthma-related emergency department visits and hospitalizations. Children who had been hospitalized for asthma had 1.84 greater odds of a revisit to the emergency department or a rehospitalization within twelve months if they lived in the highest quartile of housing code violation tracts, compared to those living in the lowest quartile. Integrating housing and health data could highlight at-risk areas and patients for targeted interventions.
Child asthma morbidity is not constant across populations.1-3 There are deep, potentially preventable disparities in its distribution.4-6 Social and environmental factors, such as substandard housing conditions, perpetuate asthma-related disparities and contribute to excess morbidity.7-10 Interventions that improve housing conditions also improve health, especially for people with diseases such as asthma.11-16 Given the clear relationship of housing and health, it follows that policy makers focused on housing policy and housing quality could share a common purpose with those who focus on the health of populations and patients.
Such a shared purpose among the housing and health sectors, coupled with shared expertise and data, could facilitate a deeper characterization of social and environmental risks and enable a more targeted, collaborative approach to the provision of population- and patient-level care. Improved health outcomes at a reduced cost could result from these sectors’ adoption of innovative approaches to risk assessment, approaches that rely on preexisting and potentially important data that are not routinely used to make health care decisions.17,18
National data sets such as those from the US census and variables such as the percentage of vacant or renter-occupied homes within a geographic area19 have been used to understand variability in health outcomes across populations.20,21 However, local data sets may provide additional granularity, which could facilitate a deeper understanding of variation in morbidity.
Many jurisdictions collect data on the enforcement of housing ordinances or codes designed to maintain healthy housing conditions for community residents.22,23 In Greater Cincinnati, housing inspectors respond to tenants’ or neighbors’ complaints about housing conditions such as the presence of pests or mold. If violations are identified, inspectors work with tenants, landlords, and the courts to remediate conditions. Information about violations becomes part of the public record.24
Data on code violations have been used across large areas (populations of about 130,000) to assess associations with allergic sensitization to certain environmental exposures.23 Using the data for smaller areas such as census tracts could be even more meaningful in understanding local disparities. Data could also be efficiently brought into patients’ electronic health records to inform and improve clinical care.18,25-28
Marketers, political campaigns, and—increasingly—public health practitioners use this type of contextual or geographic data to identify populations to whom they can target outreach efforts such as mailings and canvassing. Similar data could inform and improve care delivery at the population and patient levels.
Patients at high risk are often concentrated within neighborhoods that expose residents to potentially harmful risks.5,23,29-33 However, health care providers often fail to make use of geomarkers—which we define as any objective, contextual, or geographic measure that informs additional assessments and interventions for patients who are affected by chronic illnesses that are sensitive to the surrounding environment.
To explore this concept further, we sought to calculate a census-tract-based housing code violation density geomarker from local data. We also sought both to assess the correlation and association of that density with rates of asthma-related emergency department (ED) visits and hospitalizations at the census-tract level across a population sample, and to determine whether that density would be predictive of a patient’s risk of revisiting the ED or being rehospitalized following an index hospitalization—the first in a series—related to asthma.
Study Data And Methods
A retrospective cohort of the 4,355 children ages 1–16 who visited the ED or were hospitalized for asthma at Cincinnati Children’s Hospital Medical Center in the period January 2009–December 2012 was used. Subjects were identified using an asthma-specific encounter diagnosis—International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), 493.XX—within hospital billing data. The patients’ home addresses were geocoded and mapped to the corresponding 2010 census tract.19
The population-level analysis focused on this cohort’s 8,736 ED visits and hospitalizations during the study period. The patient-level analysis used a subset of the cohort: the 1,531 children who were hospitalized. We determined whether these patients revisited the ED or were rehospitalized for asthma within twelve months.
Children were excluded if they lived outside the area served by the Cincinnati Area Geographic Information System (CAGIS), a data repository that was the source for our primary predictor of residential housing code violations. This part of Greater Cincinnati is an urban region of 113 census tracts that collectively contained 63,095 children ages 1–16 and 171,296 residential housing units. The urban region is marked by high rates of poverty and substandard housing: The median household income for the city of Cincinnati reported by the US census for 2008–12 was $33,708, and more than half of the city’s housing units were built before 1950.19
Cincinnati Children’s Hospital Medical Center manages nearly 95 percent of all asthma-related hospitalizations in Hamilton County, which includes Greater Cincinnati.34
OUTCOMES AND PREDICTORS
We calculated the population-level utilization rate outcome variable by dividing all ED visits and hospitalizations within a census tract by the number of children ages 1–16 who lived within that tract. This was then converted to a rate, measured per 1,000 children, and averaged over the study period.
Patient-level outcomes were assessed for the subcohort of children with a hospitalization in the study period. ED revisits and rehospitalizations were captured by ICD-9-CM codes for asthma discharge diagnoses within hospital billing data (493.XX). Patients were identified as either having had or not having had an asthma-related ED revisit or rehospitalization within twelve months of the index hospitalization.
Predictors for both population- and patient-level analyses included housing-related geographic data (geomarkers) that were publicly available. The primary predictor was the locally derived residential housing code violation density. It was constructed from data collected by Greater Cincinnati health, property maintenance, and building departments and tracked in the Cincinnati Area Geographic Information System.
Violation data were extracted for the period 2008–12. This period was thought to be relevant to the 2009–12 patient cohort since it included the year before the first encounter for any patient included in our analyses.
The 11,371 specific violations were chosen a priori based on evidence of their relevance to asthma morbidity. The violations that were chosen, included in the calculation of housing code violation density, and geocoded were related to pests (for example, cockroaches and rodents), mold, and water damage.35,36
We calculated the housing code violation density for each census tract. The numerator was the number of residential housing code violations; the denominator was the number of residential housing units (homes or apartments). The density was converted to a rate, measured per 1,000 housing units, and averaged over the study period. This yielded a continuous variable that was available across all included census tracts.
For the patient-level analysis, we linked geocoded patients to their census tract’s housing code violation density value. We chose quartile cutoff points that placed approximately 25 percent of the hospitalized patients in our study in one of the following four groups for housing code violation density: low, low medium, high medium, and high. This was done, in part, to simulate a use of the data that could be more easily adapted to clinical settings.
We tested two variables as alternatives to housing code violation density: the census tracts’ percentages of vacant homes and of renter-occupied homes. In both cases, the denominator was the number of housing units in the census tract. Both variables were obtained from the 2008–12 American Community Survey (ACS) conducted by the Census Bureau.19 For our patient-level analysis, we also chose quartile cutoff points to distribute patients equally among the four risk categories noted above.
COVARIATES
The percentage of people within a census tract with incomes below the federal poverty level was obtained from the ACS and used as a covariate in our population-level analyses.19 For our patient-level analyses, a census tract’s poverty was categorized in much the same way as our primary and secondary predictors, distributing patients among the four risk groups noted above.
Patients’ demographic characteristics, obtained from their electronic health records, were age, sex, race, and insurance status. Age was treated as a continuous variable. Race was defined as white, African American, or multiracial or other. Insurance was defined as private or public.
ANALYSIS
Geographic information systems software was used to map housing code violations and patterns of use of the ED and hospital. We mapped all visits and hospitalizations as well as ED revisits and rehospitalizations. Mapping made it possible to visualize both the region and one illustrative neighborhood—Avondale—with a high concentration of both code violations and asthma-related morbidity.
Population-level census-tract correlations between each housing geomarker (housing code violation density and vacancy and renter rates) and utilization rates were assessed using Spearman correlation coefficients. We used robust regression models to assess associations between predictors and utilization rates after we adjusted for census-tract poverty.
Patient-level associations between each geomarker and a patient’s risk of revisiting the ED or being rehospitalized for asthma were assessed using the Mantel-Haenszel test for trend and generalized estimating equations regression to account for clustering at the census-tract level. Relationships between a patient’s demographic characteristics and his or her risk of an ED revisit or rehospitalization for asthma were assessed using chi-square tests and logistic regression.
We then used multivariable generalized estimating equations regression to enumerate the relationship between each housing geomarker and patients’ risk of ED revisits or rehospitalizations. A full description of this multivariable analysis is provided in online Appendix 1.37
Geocoding and mapping were conducted using ArcGIS software, version 10.1. Statistical analyses were performed using SAS software, version 9.3. This study was approved by the Institutional Review Board of Cincinnati Children’s Hospital Medical Center.
LIMITATIONS
There were limitations to this study. First, the housing code violation density variable was constructed using local administrative data. Cincinnati Area Geographic Information System serves as a data repository, and the quality and completeness of data cannot be validated.
Second, in the region we studied, as in many others, housing inspectors respond to housing complaints and only then identify potential code violations. Inspectors do not proactively assess housing conditions. Thus, the true breadth of violations is unknown.
Third, the local nature of the housing code violation density is a strength in many ways, but it clearly affects the generalizability of the measure. Nonetheless, we believe that many US jurisdictions collect similar data.
Fourth, our results may be subject to the "ecologic fallacy" of drawing conclusions about individual people in a given census tract based only on analyses of data about the entire population of that tract. However, we believe that the homogeneity of the census tracts’ populations supports such an assumption.
Finally, our sample was drawn from a single health system, and thus we could not account for children who sought care elsewhere. However, Ohio Hospital Association data suggest that the vast majority of children within Hamilton County use the Cincinnati Children’s Hospital Medical Center for hospital care. We believe that the percentage is even higher for the residents of the Greater Cincinnati area included in this study.34
Study Results
STUDY POPULATION
Between January 1, 2009, and December 31, 2012, 4,355 children collectively had 8,736 asthma-related ED visits and hospitalizations at Cincinnati Children’s Hospital Medical Center. We used all 8,736 events to calculate population-level asthma-related rates of utilization of the center’s services. The median utilization rate across the 113 census tracts in our study was 33.0 ED visits or hospitalizations per 1,000 children (range: 0.0–168.3; Exhibit 1). Across these same tracts, the median housing code violation density was 11.0 violations per 1,000 residential units (range: 0.0–120.0).
EXHIBIT 1. Characteristics Of 113 Greater Cincinnati Census Tracts And 1,531 Children From Those Tracts Hospitalized In The Period 2009–12.
| Characteristic | Number or median |
Percent or IQR |
|---|---|---|
|
| ||
| POPULATION OF CENSUS TRACT (MEDIAN) | ||
|
| ||
| Utilization rate (events per 1,000 children) | 33.0 | 21.3–47.5 |
| Housing code violation density (per 1,000 units)a | 11.0 | 6.0–20.7 |
| Vacancy rate (%)b | 18.8 | 13.5–27.2 |
| Renter rate (%)b | 59.9 | 45.3–76.8 |
| Poverty rate (%)b | 27.6 | 15.6–43.4 |
|
| ||
| PATIENTS | ||
|
| ||
| Median age (years) | 5.2 | 2.8–9.9 |
| Male | 942 | 61.7 |
| Race | ||
| White | 247 | 16.2 |
| African American | 1,204 | 78.8 |
| Multiracial or other | 77 | 5.0 |
| Insurance | ||
| Private | 413 | 27.6 |
| Public | 1,081 | 72.4 |
|
| ||
| CENSUS TRACT c | ||
|
| ||
| Housing code violation density (per 1,000 units)a | ||
| Low (<8.8) | 389 | 25.5 |
| Low medium (8.8–15.0) | 425 | 27.8 |
| High medium (15.1–23.8) | 342 | 22.4 |
| High (>23.8) | 372 | 24.3 |
| Percent of vacant homesb | ||
| Low (<14.6) | 412 | 27.0 |
| Low medium (14.6–20.1) | 382 | 25.0 |
| High medium (20.2–29.3) | 356 | 23.3 |
| High (>29.3) | 378 | 24.7 |
| Percent of renter-occupied homesb | ||
| Low (<50.6) | 392 | 25.7 |
| Low medium (50.6–65.4) | 383 | 25.1 |
| High medium (65.5–79.4) | 373 | 24.4 |
| High (>79.4) | 380 | 24.9 |
| Percent of people living in povertyb | ||
| Low (<19.7) | 402 | 26.3 |
| Low medium (19.7–34.8) | 370 | 24.2 |
| High medium (34.9–49.7) | 403 | 26.4 |
| High (>49.7) | 53 | 23.1 |
SOURCE Authors’ analysis of 2008–12 data from the Cincinnati Area Geographic Information System and the American Community Survey. NOTES An event is an asthma-related visit to the emergency department or a hospitalization at Cincinnati Children’s Hospital Medical Center. Poverty rate is the percentage of people in a census tract whose income is below the federal poverty level. IQR is interquartile range.
Data from the Cincinnati Area Geographic Information System.
Data from the American Community Survey.
Quartile cutoff points were determined to place approximately 25 percent of the patients in each sample.
A subcohort of 1,531 patients were hospitalized for asthma in the study period. Within twelve months after their index hospitalization, 37 percent of these patients revisited the ED or were rehospitalized. Of the patients in this subcohort, 61.7 percent were male, 78.8 percent were African American, and 72 percent had public insurance (Exhibit 1). Their median age was 5.2 years. By design, the patients were evenly distributed across the four housing code violation density, vacancy, renter, and poverty strata.
Nearly 75 percent of the patients resided in census-defined "poverty areas"—that is, census tracts in which 20 percent or more of the residents had incomes below poverty (data not shown).38
POPULATION-LEVEL ASSESSMENTS
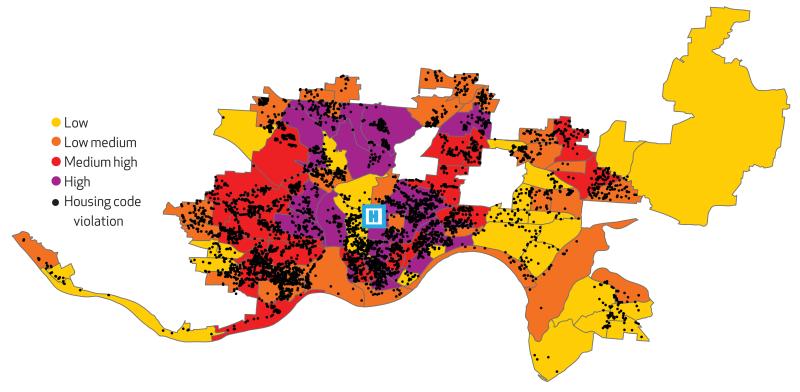
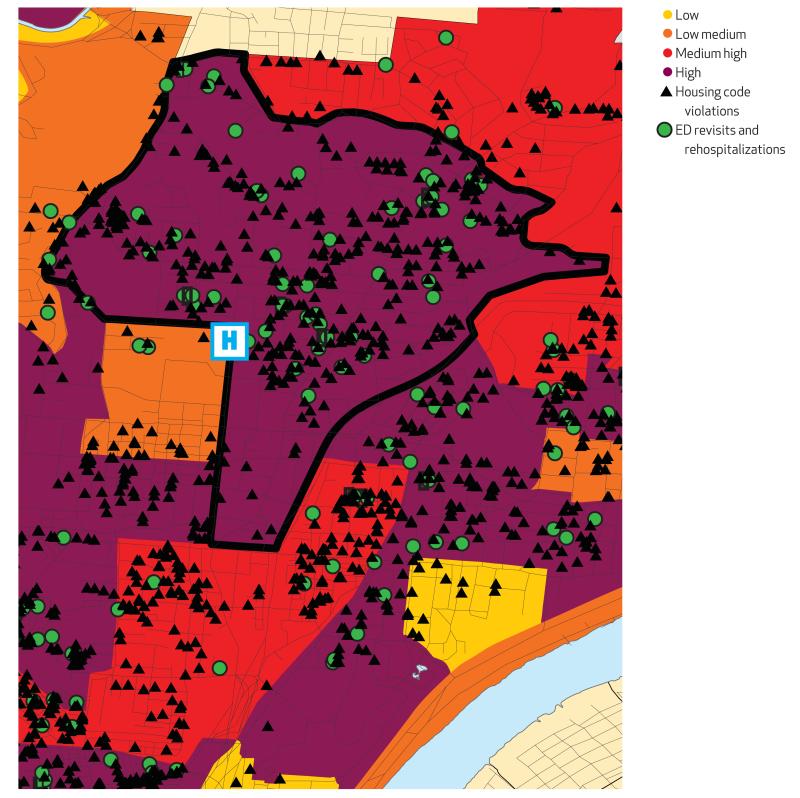
The 11,371 asthma-relevant housing code violations in the period 2008–12 appeared to cluster in census tracts with higher rates of asthma-related ED visits and hospitalizations (Exhibit 2). Avondale, a Cincinnati neighborhood that has been shown to be marked by high rates of both poverty and asthma-related morbidity,2 also demonstrated considerable overlap between the location of housing code violations and patient-level ED revisits or rehospitalizations (Exhibit 3).
EXHIBIT 2. Greater Cincinnati Census Tracts With Rates Of Asthma-Related Emergency Department Visits Or Hospitalizations, 2009–12, And 11,371 Asthma-Related Housing Code Violations, 2008–12.
SOURCE Authors’ analysis of data from the Cincinnati Children’s Hospital Medical Center and the Cincinnati Area Geographic Information System. NOTES Low is fewer than 8.8 violations per 1,000 units. Low medium is 8.8–15.0 violations. High medium is 15.1–23.8 violations. High is more than 23.8 violations.
EXHIBIT 3. Cincinnati’s Avondale Neighborhood With Asthma-Related Housing Code Violations, 2008–12, And Asthma-Related Emergency Department (ED) Revisits And Rehospitalizations Within Twelve Months Of the First (Index) Hospitalization For Children Hospitalized, 2009–12.
SOURCE Authors’ analysis of data from the Cincinnati Children’s Hospital Medical Center and the Cincinnati Area Geographic Information System. NOTES All of the Avondale neighborhood (the area within the thick black line) has a high level of violations—that is, more than 23.8 violations per 1,000 units. Volume levels are defined in the notes to Exhibit 2.
All four of the census tracts in Avondale had utilization rates in the highest risk quartile of the sample (range: 50.4–75.6 per 1,000 children; data not shown). All four also had housing code violation density values in the highest risk quartile (range: >23.8–36.3 violations per 1,000 housing units).
At the population level, housing code violation density was significantly correlated with census-tract vacancy rates (r = 0.73; p < 0.0001) and, to a lesser extent, with renter rates (r = 0.55; p < 0.0001). Each census-tract housing geomarker was also significantly correlated with rates of both census-tract poverty and asthma-related use of hospital services. The correlation coefficient between housing code violation density and poverty was 0.78, and the coefficient between the density and utilization was 0.59 (p < 0.0001 for both).
Using robust regression models, we found that housing code violation density explained 22 percent of the total variance in population-level utilization. The density remained significantly and independently associated with utilization after we adjusted for census-tract poverty (p = 0.01). Vacancy and renter rates were similarly associated with utilization at the population level after census-tract poverty was adjusted for (p = 0.04 for both).
PATIENT-LEVEL ASSESSMENTS
In the subcohort of 1,531 children, there were no significant associations between age, sex, or type of insurance and risk of an asthma-related ED revisit or rehospitalization within twelve months of the index hospitalization (Exhibit 4). However, African Americans were significantly more likely than whites to revisit the ED or be rehospitalized (38.9 percent versus 27.5 percent).
EXHIBIT 4. Bivariate Associations Between Patient- And Census-Tract-Level Characteristics And Patient-Level Risk Of An Asthma-Related Emergency Department (ED) Revisit Or Rehospitalization Within Twelve Months Of The First (Index) Hospitalization.
| Characteristic | Rate of ED revisit or rehospitalization (%) |
Odds ratioa | 95% CIa |
|---|---|---|---|
|
| |||
| PATIENT LEVEL | |||
|
| |||
| All | 36.5 | _b | _b |
| Age (years) | |||
| 1–3.9 | 37.1 | Ref | Ref |
| 4–9.9 | 37.7 | 1.19 | (0.93, 1.51) |
| 10–16 | 39.1 | 0.98 | (0.75, 1.29) |
| Sex | |||
| Female | 36.0 | Ref | Ref |
| Male | 36.8 | 1.04 | (0.84, 1.28) |
| Race | |||
| White | 27.5 | Ref | Ref |
| African American | 38.9 | 1.66 | (1.22, 2.25) |
| Multiracial or other | 28.6 | 1.08 | (0.60, 1.92) |
| Insurance | |||
| Private | 38.7 | Ref | Ref |
| Public | 35.7 | 0.88 | (0.70, 1.11) |
|
| |||
| CENSUS-TRACT LEVEL | |||
|
| |||
| Housing code violation density (per 1,000 units)c | |||
| Low | 31.9 | Ref | Ref |
| Low medium | 35.5 | 1.10 | (0.96, 1.27) |
| High medium | 37.4 | 1.28 | (1.02, 1.60) |
| High | 41.7 | 1.52 | (1.21, 1.91) |
| Vacancy rate (%)d | |||
| Low | 32.0 | Ref | Ref |
| Low medium | 35.9 | 1.08 | (0.88, 1.32) |
| High medium | 39.6 | 1.27 | (1.10, 1.46) |
| High | 39.2 | 1.27 | (1.05, 1.55) |
| Renter rate (%)d | |||
| Low | 33.4 | Ref | Ref |
| Low medium | 35.0 | 1.08 | (0.84, 1.38) |
| High medium | 39.4 | 1.29 | (0.98, 1.69) |
| High | 38.4 | 1.12 | (0.91, 1.39) |
| Poverty rate (%)d | |||
| Low | 34.6 | Ref | Ref |
| Low medium | 35.4 | 1.00 | (0.74, 1.35) |
| High medium | 36.7 | 1.09 | (0.81, 1.47) |
| High | 39.7 | 1.20 | (0.90, 1.61) |
SOURCE Authors’ analysis of 2008–12 data from the Cincinnati Area Geographic Information System and the American Community Survey. NOTE CI is confidence interval.
Unadjusted logistic or generalized estimating equations regression.
Not applicable; odds ratios cannot be calculated for the entire sample.
Data from the Cincinnati Area Geographic Information System. Quartile cutoff points were determined to place approximately 25 percent of the patients in each sample.
Data from the American Community Survey. Quartile cutoff points were determined to place approximately 25 percent of the patients in each sample.
Our primary predictor for hospital utilization—the census tract’s housing code violation density—was associated with patient-level risk of an ED revisit or a rehospitalization in a graded fashion (Exhibit 4). That is, within twelve months of theindex hospitalization, 31.9 percent of those in the low risk group had a subsequent visit or hospitalization, as did 35.5 percent in the low medium, 37.4 percent in the high medium, and 41.7 percent in the high risk group (p = 0.005 for the graded relationship). Those in the highest risk group had significantly increased odds of return compared to those at lowest risk (odds ratio:1.52).
At the patient level, risk of a subsequent ED visit or hospitalization was also significantly increased for those in the highest risk group by census-tract vacancy rate, compared to those in the lowest risk group (OR: 1.27) (Exhibit 4). Neither renter rate (p = 0.4) nor poverty rate (p = 0.14) had a significant effect, however.
Appendix 1 provides a detailed illustration of our multivariable approach to patient-level outcome assessment within the subcohort.37 After we adjusted for both census-tract poverty and patient demographic characteristics, we found that, relative to those at the lowest housing code violation density risk, those at high medium risk had 1.54 greater odds (95% confidence interval: 1.15, 2.06) of an ED revisit or a rehospitalization, and those at the highest risk had 1.84 greater odds (95% CI: 1.36, 2.48). Vacancy rate was also independently associated with a patient’s risk of an ED revisit or a rehospitalization, but renter rate was not.
Discussion
Density of housing code violations was significantly associated with population-level rates of children’s asthma-related ED visits and hospitalizations, independent of poverty. Moreover, it was significantly and independently associated with patient-level risk of an asthma-related ED revisit or hospitalization after an index hospitalization for asthma.
Given the pervasive nature of childhood asthma morbidity, especially in impoverished urban settings, being able to rapidly identify those at high risk for future morbidity would be a powerful addition to care delivery. The use of contextual geographical data could augment care processes and target scarce resources to those most likely to benefit from intervention.
There has been growing interest in the use of biomarkers to guide, improve, and personalize clinical care. Biomarkers have been defined as "any substance, structure or process that can be measured in the body or its products and influence or predict the incidence of outcome or disease."39 We tested a novel concept, the geomarker, contextual or geographic data that could provide insight into a patient’s social or environmental risks in such a way that could influence or predict the incidence of outcome or disease.
Given the importance of context and geography on acute manifestations of asthma, contextual and geographical data used for geomarkers have the potential to complement models of personalized medicine, which have generally focused on genes and biomarkers.40 Recent biomarker-based studies have demonstrated that children with a vitamin D deficiency had significantly higher odds (OR: 1.5; 95% CI: 1.1, 1.9) of having an ED visit or hospitalization within four years of baseline biomarker measurement.41 Our geomarker for housing code violation density demonstrated a similar association with child asthma morbidity.
Biomarkers may predict future asthma-related ED visits and hospitalizations.42,43 However, geomarkers may be able to guide care and discharge planning to a greater degree. They could quickly be brought into the electronic health record without the need to collect a biological specimen, directing care from the moment a patient registers his or her address with a provider.
Given the interrelated nature of substandard housing and asthma morbidity, we focused on geomarkers related to housing. The impact on asthma morbidity of residential exposures to pests, mold, and other objects associated with deteriorated housing is well established.44
We were guided in the construction of our locally derived predictor variable of housing code violation density by previous work. Lindsay Rosenfeld and coauthors calculated serious housing code violations per 1,000 rental units in New York City. Within a population of 261 Puerto Rican children, their measure was significantly associated with sensitization to asthma-related indoor allergens such as cockroaches.22,23
Our analogous measure was attached to smaller geographical regions (census tracts with populations of approximately 4,000, compared to New York community planning districts with populations of more than 100,000). Additionally, instead of allergen sensitization, we tracked utilization outcomes for clinically high-risk children—those who had already been hospitalized. However, we found similarly significant and independent relationships.
The use of public nonmedical data in a clinical context has great potential for facilitating tailored clinical care that improves the care experience and health outcomes while reducing cost.18 Indeed, such data could highlight who is likely to benefit from additional risk-targeted hospital- or community-based resources. It could also promote collaboration between those providers based in the clinical setting and those based in the community.
Our findings are especially noteworthy given the relative homogeneity of the population studied. Our previous work28 found strong associations between socioeconomic measures at the census-tract level (extreme poverty, home value, and adult educational attainment) and patient-level asthma-related reutilization of hospital services. However, that work analyzed an eight-county region that contained urban, suburban, and rural areas. In the study reported here, our sample was clustered almost entirely in an urban setting, with approximately 75 percent of the patients living in census-defined poverty areas.
Despite this socioeconomic homogeneity, housing code violation density had strong, independent associations with population-level rates of use of hospital services. Use of the density measure also illustrated strong gradients in patient-level risk of return to the ED or hospital. National data (for example, census-tract vacancy rates)19 were associated with our outcomes of interest and are potentially generalizable to other communities. However, local data on housing code violations performed better.
Locally collected and publicly available data could facilitate action to address the social determinants of health, especially for conditions such as asthma that are highly sensitive to contextual and geographical factors.18,45,46 In an era when home visits are rare, geomarker data could highlight the impact of the neighborhood context on health, identifying where efforts to reduce disparities could be targeted within both clinical and community settings.4,47,48 Such a reorientation toward risk mitigation is especially relevant as health systems shift their focus to preventive and accountable care.49,50
The physical environment, including substandard housing stock, is one area in which asthma-targeted preventive care could originate.13,51,52 At Cincinnati Children’s Hospital Medical Center, we have partnered with Cincinnati Health Department housing inspectors, who can order risk abatement if violations are noted.11 We have also worked through a medical-legal partnership14 to identify and address housing issues for both individual patients and entire building complexes.53
Other interventions that aim to reduce adverse environmental exposures have employed community health workers or involved partnerships with community housing agencies.54-56 Such programs would likely benefit from more efficient risk identification processes that used geomarkers to highlight both populations and patients at high risk.
The intersection of housing conditions and health disparities further supports a place-based and data-driven approach to policy, public health, and clinical care delivery.33,57 Housing is increasingly thought of as a platform for health promotion—a concept that was endorsed by the recent release of a new National Healthy Housing Standard.58 Similarly, the Department of Housing and Urban Development has adopted a "health in all policies" approach, which emphasizes the intersection between the physical environment and health.59
The use of housing-related geomarkers represents a highly complementary "health in all data" approach. Indeed, data collected and tracked by community agencies can serve a health-promoting purpose for policy makers, community developers, public health practitioners, and clinicians. This underscores the potential power of collaboration across agencies and disciplines to target risk-focused interventions.54,60
We plan to test additional geomarkers of the physical and the health service environments (for example, distance to a pharmacy and access to primary care). We will also test geomarkers against patient-level factors to more effectively validate our findings. Additionally, we believe that further delineation of geomarkers will translate into the implementation and evaluation of both population- and patient-level interventions aimed at reducing asthma morbidity.
Conclusion
Marketers and political campaigns can target mailings and advertising campaigns because they know where their clientele or audience lives. In medicine, existing public data could be used similarly to understand a population’s or patient’s risks. Geomarker-based data could high-light at-risk areas and patients for targeted interventions, facilitating a cost-effective and efficient approach to improving health and health care delivery at the population and patient levels.
Supplementary Material
Acknowledgments
Support for this research was provided by the Cincinnati Children’s Hospital Medical Center Procter Scholar Award and the National Institutes of Health (Grant No. 1K23AI112916). The funders played no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. The authors thank Karen Jerardi, Lauren Solan, and Hadley Sauers for reviewing the manuscript. All four of the authors are responsible for the reported research and participated in the concept and design, analysis and interpretation of data, and drafting of the manuscript. Each author had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. An earlier version of this article was presented at the annual meeting of the Pediatric Academic Societies, Vancouver, British Columbia, May 5, 2014.
Contributor Information
Andrew F. Beck, Cincinnati Children’s Hospital Medical Center, in Ohio; andrew.beck1@cchmc.org.
Bin Huang, Cincinnati Children’s Hospital Medical Center.
Raj Chundur, Cincinnati Area Geographic Information System, in Hamilton County, Ohio.
Robert S. Kahn, Cincinnati Children’s Hospital Medical Center.
NOTES
- 1.Akinbami LJ, Moorman JE, Garbe PL, Sondik EJ. Status of childhood asthma in the United States, 1980-2007. Pediatrics. 2009;123(Suppl 3):S131–45. doi: 10.1542/peds.2008-2233C. [DOI] [PubMed] [Google Scholar]
- 2.Beck AF, Moncrief T, Huang B, Simmons JM, Sauers H, Chen C, et al. Inequalities in neighborhood child asthma admission rates and underlying community characteristics in one US county. J Pediatr. 2013;163(2):574–80. doi: 10.1016/j.jpeds.2013.01.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta RS, Zhang X, Sharp LK, Shannon JJ, Weiss KB. Geographic variability in childhood asthma prevalence in Chicago. J Allergy Clin Immunol. 2008;121(3):639–45. doi: 10.1016/j.jaci.2007.11.036. [DOI] [PubMed] [Google Scholar]
- 4.Williams DR, Sternthal M, Wright RJ. Social determinants: taking the social context of asthma seriously. Pediatrics. 2009;123(Suppl 3):S174–84. doi: 10.1542/peds.2008-2233H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu SY, Pearlman DN. Hospital readmissions for childhood asthma: the role of individual and neighborhood factors. Public Health Rep. 2009;124(1):65–78. doi: 10.1177/003335490912400110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wright RJ, Subramanian SV. Advancing a multilevel framework for epidemiologic research on asthma disparities. Chest. 2007;132(5 Suppl):757S–69S. doi: 10.1378/chest.07-1904. [DOI] [PubMed] [Google Scholar]
- 7.Sandel M, Wright RJ. When home is where the stress is: expanding the dimensions of housing that influence asthma morbidity. Arch Dis Child. 2006;91(11):942–8. doi: 10.1136/adc.2006.098376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krieger JW, Song L, Takaro TK, Stout J. Asthma and the home environment of low-income urban children: preliminary findings from the Seattle–King County Healthy Homes Project. J Urban Health. 2000;77(1):50–67. doi: 10.1007/BF02350962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cutts DB, Meyers AF, Black MM, Casey PH, Chilton M, Cook JT, et al. US housing insecurity and the health of very young children. Am J Public Health. 2011;101(8):1508–14. doi: 10.2105/AJPH.2011.300139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Olmedo O, Goldstein IF, Acosta L, Divjan A, Rundle AG, Chew GL, et al. Neighborhood differences in exposure and sensitization to cockroach, mouse, dust mite, cat, and dog allergens in New York City. J Allergy Clin Immunol. 2011;128(2):284–92. doi: 10.1016/j.jaci.2011.02.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beck AF, Simmons JM, Sauers HS, Sharkey K, Alam M, Jones C, et al. Connecting at-risk inpatient asthmatics to a community-based program to reduce home environmental risks: care system redesign using quality improvement methods. Hosp Pediatr. 2013;3(4):326–34. doi: 10.1542/hpeds.2013-0047. [DOI] [PubMed] [Google Scholar]
- 12.Klein MD, Beck AF, Henize AW, Parrish DS, Fink EE, Kahn RS. Doctors and lawyers collaborating to HeLP children—outcomes from a successful partnership between professions. J Health Care Poor Underserved. 2013;24(3):1063–73. doi: 10.1353/hpu.2013.0147. [DOI] [PubMed] [Google Scholar]
- 13.Crocker DD, Kinyota S, Dumitru GG, Ligon CB, Herman EJ, Ferdinands JM, et al. Effectiveness of home-based, multi-trigger, multicomponent interventions with an environmental focus for reducing asthma morbidity: a community guide systematic review. Am J Prev Med. 2011;41(2 Suppl 1):S5–32. doi: 10.1016/j.amepre.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 14.Sandel M, Hansen M, Kahn R, Lawton E, Paul E, Parker V, et al. Medical-legal partnerships: transforming primary care by addressing the legal needs of vulnerable populations. Health Aff (Millwood) 2010;29(9):1697–705. doi: 10.1377/hlthaff.2010.0038. [DOI] [PubMed] [Google Scholar]
- 15.Jacobs DE, Brown MJ, Baeder A, Sucosky MS, Margolis S, Hershovitz J, et al. A systematic review of housing interventions and health: introduction, methods, and summary findings. J Public Health Manag Pract. 2010;16(5 Suppl):S5–10. doi: 10.1097/PHH.0b013e3181e31d09. [DOI] [PubMed] [Google Scholar]
- 16.Krieger J, Jacobs DE, Ashley PJ, Baeder A, Chew GL, Dearborn D, et al. Housing interventions and control of asthma-related indoor biologic agents: a review of the evidence. J Public Health Manag Pract. 201016(5 Suppl):S11–20. doi: 10.1097/PHH.0b013e3181ddcbd9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berwick DM, Nolan TW, Whittington J. The Triple Aim: care, health, and cost. Health Aff (Millwood) 2008;27(3):759–69. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- 18.Miranda ML, Ferranti J, Strauss B, Neelon B, Califf RM. Geographic health information systems: a platform to support the “Triple Aim.”. Health Aff (Millwood) 2013;32(9):1608–15. doi: 10.1377/hlthaff.2012.1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Census Bureau . American FactFinder [Internet] Census Bureau; Washington (DC): [cited 2014 Sep 3] Available from: http://factfinder2.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t. [Google Scholar]
- 20.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Painting a truer picture of US socioeconomic and racial/ethnic health inequalities: the Public Health Disparities Geocoding Project. Am J Public Health. 2005;95(2):312–23. doi: 10.2105/AJPH.2003.032482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jacobs DE, Wilson J, Dixon SL, Smith J, Evens A. The relationship of housing and population health: a 30-year retrospective analysis. Environ Health Perspect. 2009;117(4):597–604. doi: 10.1289/ehp.0800086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rosenfeld L, Chew GL, Rudd R, Emmons K, Acosta L, Perzanowski M, et al. Are building-level characteristics associated with indoor allergens in the household? J Urban Health. 2011;88(1):14–29. doi: 10.1007/s11524-010-9527-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosenfeld L, Rudd R, Chew GL, Emmons K, Acevedo-García D. Are neighborhood-level characteristics associated with indoor allergens in the household? J Asthma. 2010;47(1):66–75. doi: 10.3109/02770900903362676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.City of Cincinnati Community Development . Property maintenance: property maintenance code enforcement [Internet] Cincinnati (OH): City of Cincinnati: c2014. [cited 2014 Sep 3] Available from: http://www.cincinnati-oh.gov/community-development/property-maintenance/ [Google Scholar]
- 25.Clark N, Lachance L, Milanovich AF, Stoll S, Awad DF. Characteristics of successful asthma programs. Public Health Rep. 2009;124(6):797–805. doi: 10.1177/003335490912400606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hardt NS, Muhamed S, Das R, Estrella R, Roth J. Neighborhood-level hot spot maps to inform delivery of primary care and allocation of social resources. Perm J. 2013;17(1):4–9. doi: 10.7812/TPP/12-090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Freudenberg N, Pastor M, Israel B. Strengthening community capacity to participate in making decisions to reduce disproportionate environmental exposures. Am J Public Health. 2011;101(Suppl 1):S123–30. doi: 10.2105/AJPH.2011.300265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Beck AF, Simmons JM, Huang B, Kahn RS. Geomedicine: area-based socioeconomic measures for assessing risk of hospital reutilization among children admitted for asthma. Am J Public Health. 2012;102(12):2308–14. doi: 10.2105/AJPH.2012.300806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Castro M, Schechtman KB, Halstead J, Bloomberg G. Risk factors for asthma morbidity and mortality in a large metropolitan city. J Asthma. 2001;38(8):625–35. doi: 10.1081/jas-100107540. [DOI] [PubMed] [Google Scholar]
- 30.Corburn J, Osleeb J, Porter M. Urban asthma and the neighbourhood environment in New York City. Health Place. 2006;12(2):167–79. doi: 10.1016/j.healthplace.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 31.Rauh VA, Landrigan PJ, Claudio L. Housing and health: intersection of poverty and environmental exposures. Ann N Y Acad Sci. 2008;1136:276–88. doi: 10.1196/annals.1425.032. [DOI] [PubMed] [Google Scholar]
- 32.Pearlman DN, Zierler S, Meersman S, Kim HK, Viner-Brown SI, Caron C. Race disparities in childhood asthma: does where you live matter? J Natl Med Assoc. 2006;98(2):239–47. [PMC free article] [PubMed] [Google Scholar]
- 33.Morello-Frosch R, Zuk M, Jerrett M, Shamasunder B, Kyle AD. Understanding the cumulative impacts of inequalities in environmental health: implications for policy. Health Aff (Millwood) 2011;30(5):879–87. doi: 10.1377/hlthaff.2011.0153. [DOI] [PubMed] [Google Scholar]
- 34.Bosnjakovic E. INSIGHT database. Ohio Hospital Association; Columbus (OH): 2009. [Google Scholar]
- 35.Gruchalla RS, Pongracic J, Plaut M, Evans R, 3rd, Visness CM, Walter M, et al. Inner City Asthma Study: relationships among sensitivity, allergen exposure, and asthma morbidity. J Allergy Clin Immunol. 2005;115(3):478–85. doi: 10.1016/j.jaci.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 36.Wang J, Visness CM, Calatroni A, Gergen PJ, Mitchell HE, Sampson HA. Effect of environmental allergen sensitization on asthma morbidity in inner-city asthmatic children. Clin Exp Allergy. 2009;39(9):1381–9. doi: 10.1111/j.1365-2222.2009.03225.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 38.Bishaw A. Areas with concentrated poverty: 2006–2010 [Internet] Census Bureau; Washington (DC): Dec, 2011. [cited 2014 Sep 3] (American Community Survey Brief). Available from: http://www.census.gov/prod/2011pubs/acsbr10-17.pdf. [Google Scholar]
- 39.Biomarkers In risk assessment: validity and validation [Internet] World Health Organization; Geneva: 2001. [cited 2014 Sep 3] Available from: http://www.inchem.org/documents/ehc/ehc/ehc222.htm#3.0. [Google Scholar]
- 40.Hamburg MA, Collins FS. The path to personalized medicine. N Engl J Med. 2010;363(4):301–4. doi: 10.1056/NEJMp1006304. [DOI] [PubMed] [Google Scholar]
- 41.Brehm JM, Schuemann B, Fuhlbrigge AL, Hollis BW, Strunk RC, Zeiger RS, et al. Serum vitamin D levels and severe asthma exacerbations in the Childhood Asthma Management Program study. J Allergy Clin Immunol. 2010;126(1):52–8. doi: 10.1016/j.jaci.2010.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Forno E, Celedón JC. Predicting asthma exacerbations in children. Curr Opin Pulm Med. 2012;18(1):63–9. doi: 10.1097/MCP.0b013e32834db288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Robroeks CM, van Vliet D, Jöbsis Q, Braekers R, Rijkers GT, Wodzig WK, et al. Prediction of asthma exacerbations in children: results of a one-year prospective study. Clin Exp Allergy. 2012;42(5):792–8. doi: 10.1111/j.1365-2222.2012.03992.x. [DOI] [PubMed] [Google Scholar]
- 44.Rauh VA, Chew GR, Garfinkel RS. Deteriorated housing contributes to high cockroach allergen levels in inner-city households. Environ Health Perspect. 2002;110(Suppl 2):323–7. doi: 10.1289/ehp.02110s2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Comer KF, Grannis S, Dixon BE, Bodenhamer DJ, Wiehe SE. In corporating geospatial capacity within clinical data systems to address social determinants of health. Public Health Rep. 2011;126(Suppl 3):54–61. doi: 10.1177/00333549111260S310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Berke EM. Geographic information systems (GIS): recognizing the importance of place in primary care research and practice. J Am Board Fam Med. 2010;23(1):9–12. doi: 10.3122/jabfm.2010.01.090119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gottlieb L, Sandel M, Adler NE. Collecting and applying data on social determinants of health in health care settings. JAMA Intern Med. 2013;173(11):1017–20. doi: 10.1001/jamainternmed.2013.560. [DOI] [PubMed] [Google Scholar]
- 48.Erickson D, Andrews N. Partnerships among community development, public health, and health care could improve the well-being of low-income people. Health Aff (Millwood) 2011;30(11):2056–63. doi: 10.1377/hlthaff.2011.0896. [DOI] [PubMed] [Google Scholar]
- 49.Baum FE, Bégin M, Houweling TA, Taylor S. Changes not for the faint-hearted: reorienting health care systems toward health equity through action on the social determinants of health. Am J Public Health. 2009;99(11):1967–74. doi: 10.2105/AJPH.2008.154856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hacker K, Walker DK. Achieving population health in accountable care organizations. Am J Public Health. 2013;103(7):1163–7. doi: 10.2105/AJPH.2013.301254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Labre MP, Herman EJ, Dumitru GG, Valenzuela KA, Cechman CL. Public health interventions for asthma: an umbrella review, 1990–2010. Am J Prev Med. 2012;42(4):403–10. doi: 10.1016/j.amepre.2011.11.016. [DOI] [PubMed] [Google Scholar]
- 52.Saegert SC, Klitzman S, Freudenberg N, Cooperman-Mroczek J, Nassar S. Healthy housing: a structured review of published evaluations of US interventions to improve health by modifying housing in the United States, 1990–2001. Am J Public Health. 2003;93(9):1471–7. doi: 10.2105/ajph.93.9.1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Beck AF, Klein MD, Schaffzin JK, Tallent V, Gillam M, Kahn RS. Identifying and treating a substandard housing cluster using a medical-legal partnership. Pediatrics. 2012;130(5):831–8. doi: 10.1542/peds.2012-0769. [DOI] [PubMed] [Google Scholar]
- 54.Braunstein S, Lavizzo-Mourey R. How the health and community development sectors are combining forces to improve health and well-being. Health Aff (Millwood) 2011;30(11):2042–51. doi: 10.1377/hlthaff.2011.0838. [DOI] [PubMed] [Google Scholar]
- 55.Krieger JW, Takaro TK, Song L, Weaver M. The Seattle–King County Healthy Homes Project: a randomized, controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. Am J Public Health. 2005;95(4):652–9. doi: 10.2105/AJPH.2004.042994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Breysse J, Dixon S, Gregory J, Philby M, Jacobs DE, Krieger J. Effect of weatherization combined with community health worker in-home education on asthma control. Am J Public Health. 2014;104(1):e57–64. doi: 10.2105/AJPH.2013.301402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jacobs DE. Environmental health disparities in housing. Am J Public Health. 2011;101(Suppl 1):S115–22. doi: 10.2105/AJPH.2010.300058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.National Center for Healthy Housing . Policy: National Healthy Housing Standard [Internet] NCHH; Columbia (MD): [cited 2014 Sep 3] Available from: http://www.nchh.org/Policy/NationalHealthyHousingStandard.aspx. [Google Scholar]
- 59.Bostic RW, Thornton RL, Rudd EC, Sternthal MJ. Health in all policies: the role of the US Department of Housing and Urban Development and present and future challenges. Health Aff (Millwood) 2012;31(9):2130–7. doi: 10.1377/hlthaff.2011.1014. [DOI] [PubMed] [Google Scholar]
- 60.Berke EM, Vernez-Moudon A. Built environment change: a framework to support health-enhancing behaviour through environmental policy and health research. J Epidemiol Community Health. 2014;68(6):586–90. doi: 10.1136/jech-2012-201417. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.