Abstract
BACKGROUND:
Noninvasive monitoring of intra-abdominal pressure (IAP) by measuring abdominal wall tension (AWT) was effective and feasible in previous postmortem and animal studies. This study aimed to investigate the feasibility of the AWT method for noninvasively monitoring IAP in the intensive care unit (ICU).
METHODS:
In this prospective study, we observed patients with detained urethral catheters in the ICU of Shanghai Tenth People’s Hospital between April 2011 and March 2013. The correlation between AWT and urinary bladder pressure (UBP) was analyzed by linear regression analysis. The effects of respiratory and body position on AWT were evaluated using the paired samples t test, whereas the effects of gender and body mass index (BMI) on baseline AWT (IAP<12 mmHg) were assessed using one-way analysis of variance.
RESULTS:
A total of 51 patients were studied. A significant linear correlation was observed between AWT and UBP (R=0.986, P<0.01); the regression equation was Y=–1.369+9.57X (P<0.01). There were significant differences among the different respiratory phases and body positions (P<0.01). However, gender and BMI had no significant effects on baseline AWT (P=0.457 and 0.313, respectively).
CONCLUSIONS:
There was a significant linear correlation between AWT and UBP and respiratory phase, whereas body position had significant effects on AWT but gender and BMI did not. Therefore, AWT could serve as a simple, rapid, accurate, and important method to monitor IAP in critically ill patients.
KEY WORDS: Abdominal wall tension, Intra-abdominal pressure, Noninvasive monitoring, Abdominal compartment syndrome
INTRODUCTION
The intra-abdominal pressure (IAP) of critically ill patients is usually kept at 5–7 mmHg. Intra-abdominal hypertension (IAH) is defined by the World Society of Abdominal Compartment Syndrome (WSACS) as that which continually increases to or repeatedly exceeds 12 mmHg; abdominal compartment syndrome (ACS) is diagnosed if IAP is >20 mmHg accompanied by new organ dysfunction or failure (with or without abdominal perfusion pressure<60 mmHg).[1] IAH occurs in approximately 50% of patients in the intensive care unit (ICU) of general adults.[2,3] The ACS fatality rate usually reaches 50%–75%[4] and is considered as a critical cause of higher morbidity and mortality rates of patients in the ICU.[5–7] A high IAP could increase intestinal injury, an important cause of dysfunction syndromes in multiple organs.[8] A rapidly increasing IAP could result in ACS and directly result in multi-organ dysfunction or failure. The IAP level can reflect multiple organ dysfunction severity and help to predict disease treatment, so IAP monitoring could enable early treatment and thereby reduce the incidence of IAH, ACS, and patient mortality. However, the currently available method for directly measuring IAP is invasive and difficult to use in most patients. The urinary bladder pressure (UBP) method is considered as the gold standard for indirect IAP measurement. UBP is also used to represent IAP, but it is not the gold standard for diseases such as bladder tumors and pelvic hematoma oppressing the bladder.[9–11] In addition, since the UBP method is complicated and time-consuming, we attempt to develop a simple, fast, accurate, and noninvasive IAP monitoring method for ICU patients.
AWT involves palpation of abdominal muscle tension in which the abdomen becomes tense or expands when IAP increases; consequently, AWT is enhanced, the physiological basis for its feasibility. A significant linear correlation was observed between AWT and UBP in postmortem and animal studies.[12,13] However, the correlation between AWT and UBP and the use of AWT in the clinical setting has not been reported. Therefore, we observed and analyzed the effects of respiratory phase, posture, gender, and body mass index (BMI) on AWT to evaluate its feasibility for monitoring IAP.
METHODS
Subjects
This prospective study included patients with detained urethral catheters in the ICU of Shanghai Tenth People’s Hospital between April 2011 and March 2013. Exclusion criteria were as follows: use of muscle relaxants, abdominal operation within the previous 3 months, acute peritonitis, abdominal mass, acute injury to the urinary bladder, acute cystitis, neurogenic bladder, pelvic hematoma, and pelvic fracture. All operations followed the ethical standards of the medical ethics committee of the Tenth People’s Hospital of Tongji University. The patients or their families were informed of this study and signed informed consent.
AWT method
The prototype AWT measurement instrument includes one thrust meter (Aidebao Instruments Co. Ltd., Zhejiang, China) and one self-made device (Figure 1). This instrument can measure the required thrust to produce displacement (mm). AWT was described as thrust/displacement (N/mm).
Figure 1.

The device used for the abdominal wall tension (AWT) measurements. This instrument can measure the required thrust to produce displacement (mm). A: thrust meter; B: self-made device; D: oval head. Vertical pressure during the measurement drives the device to the abdominal wall and stops when C is touched by the abdominal wall. X is the vertical displacement of the abdominal wall sag. The thrust is recorded by A. AWT is defined as thrust/displacement (N/mm).
UBP method
UBP was measured using the AbViserAutoValve device (Wolfe Tory Medical, Inc., Salt Lake City, UT, USA; Figure 2) connected to a Fleischl catheter and an ICU general pressure sensor. Normal saline (25 mL) was injected into the bladder and the bladder pressure (mmHg) was directly read on the monitor. When patients were in the supine position during late expiration and the abdominal muscles were relaxed, the IAP was measured with the midaxillary at the level of the superior iliac crest as the zero reference point.[1]
Figure 2.

The AbViserAutoValve device connected to the catheter.
Procedure
In a similar study, Cheatham et al[14] found that the location of 5 cm subxiphoid was the best point for measuring AWT, so we chose it. The measurement was performed once the patients were in a stable and quiet condition in the ICU. The AWT measuring device and AbViserAutoValve apparatus were used to measure the AWT and UBP in supine and 30° supine positions during late inspiration and expiration respectively. The measurements were performed three times, and all of the values were converted to average values.
The correlation between AWT and UBP was statistically analyzed. The two different postures and respiration phases of the AWT values were compared. The gender, height and weight of each patient were recorded. The BMI values of the patients with IAP<12 mmHg were calculated and the patients were divided into three groups from low to high using BMI values of 18 and 25 mmHg as the cutoff points. The patients’ IAP values in the three groups were compared by gender and BMI. Those patients who could not be weighed or for whom a value could not be provided by family members were excluded from the study. Since the standard UBP method adopted the supine position during late expiration, we examined the AWT values of the supine position during late expiration to assess the correlation between AWT and UBP as well as the effect of gender and BMI on AWT.
Statistical analysis
Statistical analysis was performed using SPSS 13.0 statistical software (SPSS, Chicago, IL, USA). All data were presented as mean±standard deviation. The correlation between AWT and UBP was examined using linear regression analysis. The effects of respiratory phase and body position on AWT were assessed using a paired samples t test, while the effects of gender and BMI on baseline AWT (IAP<12 mmHg) were evaluated using one-way analysis of variance. P<0.05 was considered statistically significant.
RESULTS
Patient data
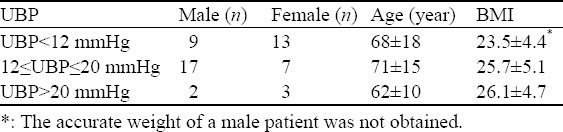
A total of 51 ICU patients, 28 men and 23 women, were included in the study. The age ranged from 5 to 89 years, with a mean age of 69±15 years. UBP was 4–26 mmHg (average 13±5 mmHg), and BMI was 15.6–38.6 (average 24.8±4.5) (Table 1).
Table 1.
Distribution of urinary bladder pressure, gender, age, and body mass index
The patients were admitted to the ICU because of cardiopulmonary resuscitation (n=12), severe pneumonia (n=10), acute respiratory distress syndrome (n=6), sepsis (n=5), cerebral hemorrhage (n=4), cerebral infarction (n=4), organophosphorus poisoning (n=4), diazepam poisoning (n=3), multiple trauma (n=2), and severe tetanus (n=1).
Correlation between AWT and UBP
A significant linear correlation was observed between AWT and UBP, with a correlation coefficient of R=0.986 (t=41.08, P<0.01). The linear regression equation was Y=–1.369+9.57X using AWT as the independent variable and UBP as the dependent variable on linear regression analysis (Figure 3).
Figure 3.
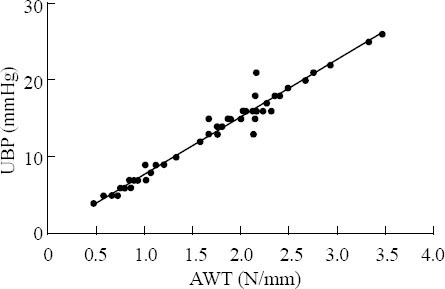
Scatterplots of abdominal wall tension (AWT) and urinary bladder pressure (UBP).
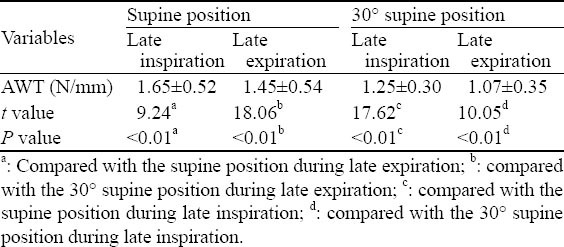
Effects of respiration and body position on AWT
The AWT of patients in the two postures during late inspiration was higher than that during late expiration (P<0.01). The AWT of patients with two respiratory phases in the supine position was higher than that in the 30° supine position (P<0.01) (Table 2).
Table 2.
Correlation of respiration, body position, and abdominal wall tension
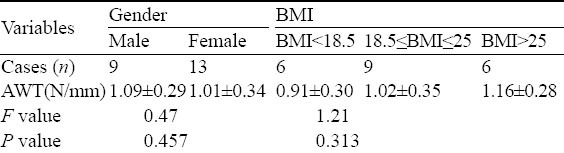
Effects of gender and BMI on AWT
No significant differences were observed between the AWT of men and women with an IAP<12 mmHg. The AWT of all patients divided by BMI was not significantly different (Table 3).
Table 3.
Correlation of gender, body mass index, and abdominal wall tension in patients with an intra-abdominal pressure<12 mmHg
DISCUSSION
Our study is the first to confirm the linear correlation between AWT and UBP in ICU patients by using a self-made AWT measurement device that has laid a theoretical foundation for its clinical application. The deficiencies of the UBP method for clinical application cannot be ignored for several reasons. First, patients treated with the UBP method must have an indwelling urinary catheter, which may increase the incidence of urinary tract and systemic infections, and some patients may refuse the procedure or be difficult to be catheterized. Second, in patients with serious colon edema or exudation, the IAP of high abdominal tension was high and that of low abdominal tension was normal. In patients with limited pancreatitis or retroperitoneal edema, the increase of IAP was not obvious and the bladder pressure may be normal, which cannot confirm the absence of IAH and ACS. Third, in patients with decreased bladder compliance,[15, 16] bladder tumors, or a pelvic hematoma oppression bladder, the accuracy of the UBP method may disappear. Fourth, the use of the UBP method is complicated. The WSACS suggested that if severe patients have the risk factors of IAH/ACS, IAP should be monitored continuously or at least every 4–6 hours.[1] Because of the frequent requests for IAP monitoring, a simple, rapid, accurate, and noninvasive method for monitoring IAP is needed for ICU patients; for this reason, we developed the AWT method, which not only fits the requirement of strict IAP monitoring, but is convenient and easy to use in the ICU. Therefore, we believe that this device and method may benefit ICU patients.
We also studied the respiratory phase and the effect of two ICU common positions (supine and 30° supine) on AWT. We found that AWT during late inspiration was higher than that during late expiration in both positions, which is consistent with the observation of Cheatham et al.[14] Vasquez and colleagues[15] reported that IAP gradually increased as body position was elevated. This finding was similar to that of Wilson et al.[17] However, we found that the AWT of the 30° supine position was lower than that of the supine position. We believe that when the head was raised, the abdominal wall muscles relaxed and the AWT decreased. To maintain the unity and stability of the AWT method, we recommend supine position during late expiration when using AWT to monitor IAP.
Although the IAP of critically ill patients was usually 5–7 mmHg according to the WSACS criteria, we found that the organ function in ICU patients was minimally affected at IAP<12 mmHg. Based on this finding and the WSACS criteria, we considered that IAP<12 mmHg was normal in this study. Cheatham et al[14] found that AWT values were higher in men than in women in healthy volunteers. However, we found no effects of gender on the baseline AWT values in our study. The reason may be that patients in the study of Van et al[12] were healthy and young, whereas patients we observed were older and critically ill and had much weaker abdominal wall muscles. Sugerman et al[16] compared the IAP values of non-obese and obese people and found that they were higher in the latter than in the former. Wilson et al[17] also reported similar findings that were incompatible with our observation in this study. We speculated that this was associated with the BMI range of the study objects: BMI in the study of Wilson et al[17] were all >25 and some were even >40, but BMI in our study was relatively lower. In future studies, the numbers of observed patients should be increased and BMI should be included to investigate the effects of BMI on IAP and AWT. When IAP values are evaluated in clinical practice via AWT, especially when normal, gender and BMI should not be ignored.
In conclusion, a significant linear correlation was observed between AWT and UBP in ICU patients. It was feasible to use AWT to monitor IAP. The AWT method is very simple, fast, and accurate. It is an important method to monitor IAP in the clinical setting. However, as a new method, the AWT measurement device used in this study should be standardized. A commercially available AWT measurement device may become a powerful tool for monitoring IAP. The effects of common factors such as muscle relaxants and mechanical ventilation on AWT in the ICU should be evaluated in future studies. Conclusions can be reached once a large-scale and multicenter clinical trial is performed with a large number of patients.
Footnotes
Funding: The study was supported by a grant from Shanghai Municipal Health Bureau Program (2009143).
Ethical approval: The study was approved by the Ethical Committee of Shanghai Tenth People’s Hospital, Tongji University, Shanghai, China.
Conflicts of interest: There was no conflict of interest related to this study.
Contributors: Chen YZ proposed and wrote the study. All authors contributed to the design and interpretation of the study, and approved the final manuscript.
REFERENCES
- 1.Kirkpatrick AW, Roberts DJ, De Waele J, Jaeschke R, Malbrain ML, De Keulenaer B, et al. Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the World Society of the Abdominal Compartment Syndrome. Intensive Care Med. 2013;39:1190–1206. doi: 10.1007/s00134-013-2906-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen H, Li F, Sun JB, Jia JG. Abdominal compartment syndrome in patients with severe acute pancreatitis in early stage. World J Gastroenterol. 2008;14:3541–3548. doi: 10.3748/wjg.14.3541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Malbrain MLNG, Chiumello D, Pelosi P, Wilmer A, Brienza N, Malcangi V, et al. Prevalence of intra-abdominal hypertension in critically ill patients: a multicentre epidemiological study. Intensive Care Med. 2004;30:822–829. doi: 10.1007/s00134-004-2169-9. [DOI] [PubMed] [Google Scholar]
- 4.De Waele JJ, Leppäniemi AK. Intra-abdominal hypertension in acute pancreatitis. World J Surg. 2009;33:1128–1133. doi: 10.1007/s00268-009-9994-5. [DOI] [PubMed] [Google Scholar]
- 5.Chen H, Li F, Sun JB, Jia JG. Abdominal compartment syndrome in patients with severe acute pancreatitis in early stage. World J Gastroenterol. 2008;14:3541–3548. doi: 10.3748/wjg.14.3541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hang Y, Chen Y, Lu LX, Zhu CQ. Acute hyperlipidemic pancreatitis in a pregnant woman. World J Emerg Med. 2013;4:311–313. doi: 10.5847/wjem.j.issn.1920-8642.2013.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang YJ, Sun JB, Li F. Relationship between intra-abdominal pressure and severity in patients with severe acute pancreatitis. Chin J Emerg Med. 2009;18:632–635. [Google Scholar]
- 8.Guo YY, Liu ML, He XD, Jiang CQ, Liu RL. Functional changes of intestinal mucosal barrier in surgically critical patients. World J Emerg Med. 2010;1:205–208. [PMC free article] [PubMed] [Google Scholar]
- 9.De Laet IE, Hoste EA, De Waele JJ. Survey on the perception and management of the abdominal compartment syndrome among Belgian surgeons. Acta Chir Belg. 2007;107:648–652. doi: 10.1080/00015458.2007.11680140. [DOI] [PubMed] [Google Scholar]
- 10.Otto J, Kaemmer D, Höer J, Jansen M, Schumpelick V, Strik M, et al. Importance of abdominal compartment syndrome in Germany: A questionnaire. Anaesthesist. 2009;58:607–610. doi: 10.1007/s00101-009-1541-0. [DOI] [PubMed] [Google Scholar]
- 11.Ravishankar N, Hunter J. Measurement of intra-abdominal pressure in intensive care units in the United Kingdom: Anational postal questionnaire study. Br J Anaesth. 2005;94:763–766. doi: 10.1093/bja/aei117. [DOI] [PubMed] [Google Scholar]
- 12.Van Ramshorst GH, Lange JF, Goossens RH, Agudelo NL, Kleinrensink GJ, Verwaal M, et al. Non-invasive measurement of intra-abdominal pressure: a preliminary study. Physiol Meas. 2008;29:N41–N47. doi: 10.1088/0967-3334/29/8/N01. [DOI] [PubMed] [Google Scholar]
- 13.van Ramshorst GH, Salih M, Hop WC, van Waes OJ, Kleinrensink GJ, Goossens RH, et al. Noninvasive assessment of intra-abdominal pressure by measurement of abdominal wall tension. J Surg Res. 2011;171:240–244. doi: 10.1016/j.jss.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 14.Cheatham ML, De Waele JJ, De Laet I, De Keulenaer B, Widder S, Kirkpatrick AW, et al. The impact of body position on intra-abdominal pressure measurement: a multicenter analysis. Crit Care Med. 2009;37:2187–2190. doi: 10.1097/CCM.0b013e3181a021fa. [DOI] [PubMed] [Google Scholar]
- 15.Vasquez DG, Berg-Copas GM, Wetta-Hall R. Influence of semirecumbent position on intra-abdominal pressure as measured by bladder pressure. J Surg Res. 2007;139:280–285. doi: 10.1016/j.jss.2006.10.023. [DOI] [PubMed] [Google Scholar]
- 16.Sugerman H, Windsor A, Bessos M, Wolfe L. Intra-abdominal pressure, sagittal abdominal diameter and obesity comorbidity. J Intern Med. 1997;241:71–79. doi: 10.1046/j.1365-2796.1997.89104000.x. [DOI] [PubMed] [Google Scholar]
- 17.Wilson A, Longhi J, Goldman C, McNatt S. Intra-abdominal pressure and the morbidly obese patients: the effect of body mass index. J Trauma. 2010;69:78–83. doi: 10.1097/TA.0b013e3181e05a79. [DOI] [PubMed] [Google Scholar]


