Abstract
BACKGROUND:
Fascia iliaca compartment nerve block (FICNB) has been an established technique for postoperative analgesia after surgery for femoral bone fracture. FICNB is technically easy, effective for postoperative pain control after operation for femoral bone fracture and decreases the complications induced by systemic analgesic drugs. The severity of postoperative pain is affected by genetics, cultural and social factors across the world. In this study we assessed the efficacy of fascia iliaca compartment nerve block when it is used as part of multimodal analgesia after surgery for femoral bone fracture.
METHODS:
An institution-based case control study was conducted from September, 2013 to May, 2014. All patients who had been operated on under spinal anesthesia for femoral bone fracture were included. The patients divided into a FICNB group (n=20) and a control group (n=20). The FICNB group was given 30 mL of 0.25% bupivacaine at the end of the operation. Postoperative pain was assessed within the first 24 hours, i.e. at 15 minutes, 2 hours, 6 hours, 12 hours and 24 hours using 100 mm visual analogue scale (VAS), total analgesic consumption, and the time for the first analgesic request.
RESULTS:
VAS pain scores were reduced within the first 24 hours after operation in the FICNB group compared wtih the control group. VAS scores at 2 hours were taken as median values (IQR) 0.00 (0.00) vs.18.00 (30.00), P=0.001; at 6 hours 0.00 (0.00) vs. 34.00 (20.75), P=0.000; at 24 hours 12.50 (10.00) vs. 31.50 (20.75), P=0.004; and at 12 hours (17.80±12.45) vs. (29.95±12.40), P=0.004, respectively. The total analgesic consumption of diclofenac at 12 and 24 hours was reduced in the FICNB group, and the time for the first analgesic request was significantly prolonged (417.50 vs. 139.25 minutes, P=0.000).
CONCLUSIONS:
A single injection for FICNB could lead to postoperative pain relief, reduction of total analgesic consumption and prolonged time for the first analgesic request in the FICNB group after surgery for femoral bone fracture. We recommend FICNB for analgesia after surgery for femoral bone fracture and for patients with femoral bone fracture at the emergency department.
KEY WORDS: Surgery, Femoral bone fracture, Fascia iliaca compartment nerve block, Postoperative pain
INTRODUCTION
The incidence of road traffic accidents was close to 50% in one of the largest hospitals in our country. Of these, the highest rate of limb fracture in the femur was 15.8% followed by the tibiofibula 14.4% and the humerus 12.9% in a 6-month period in 2007.[1] Femoral bone fractures which are too painful can have profound physiological and psychological changes.[2]
However, management of pain is associated with good clinical outcomes. Fascia iliaca compartment nerve block (FICNB) was more effective than opioids in the treatment of femoral bone fracture pain.[3] The block was first described by Dalens et al[4] in 1989, with the original understanding that it was used in pediatric patients.[4–6] This new technique of regional block was used to block the femoral lateral cutaneous nerve of the thigh and the obturator nerve. The landmark of this technique was a line drawn between the anterior superior iliac spine and the pubic tubercle along the deep inguinal ligament.[7] By negative aspiration, 30 mL of 0.25% local anesthetics is placed behind the fascia iliaca compartment when the weight of the patient is less than 80 kg, even 40 mL for the patient who is above 80 kg. The two pop techniques are appreciated blindly while passing the fascia lata and fascia iliaca.[7–9]
The FICNB has proved to be an easy and safe technique. It is free from complications because of the major nerves and vessels are far from the site of needle insertion.[10]
Systemic analgesics such as opioids and non-steroidal antinflamatory drugs are associated with different side effects.[6,11] Even though the usual definitive treatment is surgical, pain after femoral bone fracture surgery impairs the ability of ambulation of the patient and may delay the hospital discharge.[12]
A study[13] from the USA revealed that measurements of visual analogue scale (VAS) at 15 minutes between FICNB and systemic analgesics were 6.24±0.17 and 2.9 ±0.16 respectively and that VAS scores were reduced at 2 hours in the FICNB group. A case control study from the UK showed that VAS scores were significantly lowered at 2 and 8 hours respectively, and that patients needed less systemic analgesics in the FICNB group.[3]
A Korean study found decreased VAS scores and shorter time of the first analgesic request in the FICNB group (4.5±2.9 hours and 8.6±2.8 hours respectively, P<0.001).[14]
FICNB is safe, easy and effective for postoperative pain management after femoral bone fracture surgery, and it decreases the rate of complications associated with the use of systemic analgesics. The severity of postoperative pain is affected by genetics, cultural and social factors around the world.[15,16] Since similar study on FICNB as multimodal analgesia was not conducted in our country, we assessed the efficacy of FICNB using a blind anatomical technique (double pop technique) with local anesthetics to control post-operative pain after femoral bone fracture surgery.
METHODS
Study design and patients
An institution-based case control study was conducted from September, 2013 to May, 2014 in our hospital. Patients with femoral bone fracture underwent operation under spinal anesthesia in our hospital.
Inclusion criteria: Patients aged≥18 years old, who had ASA physical status I–III, femoral bone fracture surgery under subarachnoid block anesthesia, 30 mL of 0.25% bupivacaine prescribed at the end of surgery, and body weight 40–80 kg.
Exclusion criteria: Patients with bleeding disorders, GCS<15, communication failure, allergy to local anesthetics, multiple trauma, sedation, and femoral graft in the affected limb.
Study variables
Dependent variable is post-operative pain which was assessed using visual analogue scale (VAS), total post-operative analgesic consumption, and time for the first analgesic request.
Independent variables included age, sex, body mass index (BMI), American Society of Anesthesiologists (ASA) status, preoperative analgesia, intraoperative analgesia, and time of intraoperative anesthesia.
VAS is a method of pain assessment determined by patients making a mark of their pain intensity on a line which is 100 mm long.
No pain ——————— worst imaginable pain
Time for the first analgesic request is the initial time in which patients need pain treatment.
VAS scores of cases and controls were determined 24 hours postoperation (FICNB versus controls, mean±SD)=(2.5±0.6) vs. (3.0±1.2)[14] using a mean comparison formula:
n=(s12 + s22) f (α, β)[17] (m1–m2)2
Where β=20% and α=alpha error=5%. m1, s1 and m2, s2 are the mean and standard deviation of the cases and controls respectively. The total sample size was calculated using the above formula. The number of cases and controls was 20 respectively.
Since RCT was not yet allowed in our university, the patients were not randomized. Rather, the patients were classified as cases and controls based on the responsible anesthetists’ independent decision to use FICNB at the end of the operation.
Data collection
The patients who had FICNB were enrolled in a FICNB group and those who were managed without FICNB served as a control group. The patients had FICNB after the completion of the procedure. One of the data collectors recorded intraoperative information. The immediate postoperative time, the presence and scale of pain, the time for the first analgesic request, and the need of analgesics were assessed by another collector who was blinded to group allocation. These assessments were carried out at 15 minutes, 2 hours, 6 hours, 12 hours and 24 hours postoperation. The VAS score was determined by the patients marking their pain intensity on a line which was 100 mm long.
Data analysis
Data were analyzed using SPSS software version 20. Demographic data were analyzed using Student’s t test (for normal distribution variables) and Fisher’s exact test (for categorical variables). The data were tested for normality using the Shapiro-Wilk normality test. There was normal distribution of data for the time of the first analgesic request as checked using Shapiro-Wilk test and homogeneity of variance assessed using the Levene’s test for equality of variances. Therefore, an independent t-test was performed on the data with a 95% confident interval to analyze the measurement at the time of the first analgesic request.
However, no normal distribution was observed for repeated VAS measurements, and total post-operative analgesic consumption was checked using the Shapiro-Wilk test. Therefore, the non-parametric Mann-Whitney U test was performed on the data, and a 95% confident interval (CI) was used to analyze for paired comparison at each time interval. Categorical parameters were analyzed using the Chi-square test or Fisher’s exact test. Normally distributed data were presented as mean±SD, whereas not normally distributed data were presented as median (IQR) and categorical data as frequencies (percentages). A P value<0.05 was considered statistically significant.
Ethical approval
Ethical clearance was obtained from the School of Medicine Ethical Review committee, Gondar College of Medicine and Health Sciences. Written informed consent was obtained from the patients after clear explanation what they had to do in the study and the possible results of the study. Anyone who was not willing to participate in the study could resign at any time. Confidentiality was guaranteed using anonymous questionnaires and keeping them locked.
RESULTS
Socio-demographic characteristics of the patients
The 40 patients who had been operated upon under spinal anesthesia were enrolled in this study. Of these patients, 20 were given FICNB with 30 mL of 0.25% bupivacaine and 20 without FICNB but with post-operative systemic analgesia. Two patients were excluded from the study because spinal anesthesia failed and converted to general anesthesia.
Demographic characteristics such as age, sex, height, weight and BMI were comparable between the two groups (Table 1). In this study, 90% of the FICNB group and 80% of the control group were males, but 10% of the FICNB group and 20% of the control group were females.
Table 1.
Demographic and anesthetic baseline characteristics of the patients who underwent femoral bone fracture surgery in the period of September 2013– May 2014
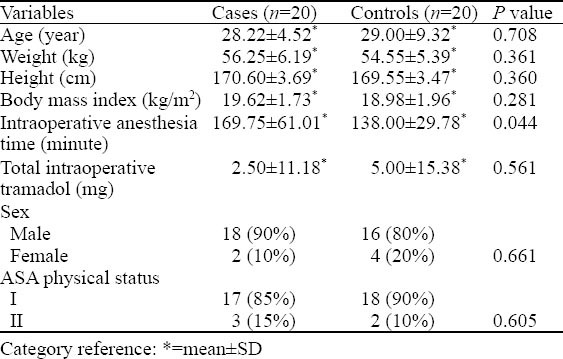
Assessment of ASA physical status showed that 85% of the FICNB patients and 90% of the controls had ASA I but 15% of the FICNB patients and 10% of the controls had ASA II. There were no complications related to FICNB.
Postoperative pain VAS scores
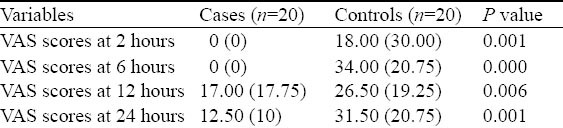
There was no difference in VAS scores at 15 minutes after operation, which were equal to zero between the FICNB and control groups (Table 2).
Table 2.
VAS scores of the patients who underwent femoral bone fracture surgery in the first 24 postoperative hours in the period of September 2013–May 2014
Postoperative total analgesic consumption
Diclofenace and tramadol consumption was checked by the Shapiro-Wilk test at the postoperative 12 and 24 hours. The Mann-Whitney U test was used to assess their associations. The patients undergoing FICNB showed a reduced total diclofenace consumption at 12 and 24 hours after operation (FICNB vs. controls) i.e. at 12 hours [75.00 (18.75) vs. 100.00 (75), P=0.000] and at 24 hours [75.00 (25) vs. 100.00 (75), P=0.001]. On the contrary, the total tramadol consumption at 12 and 24 hours (FICNB vs control) was described as median (IQR) mg, i.e. at 12 hours [50.00 (50.00) vs. 50.00 (0.00), P=0.146] and at 24 hours [50.00 (50.00) vs. 100.00 (50.00), P=0.083] (Figure 1).
Figure 1.
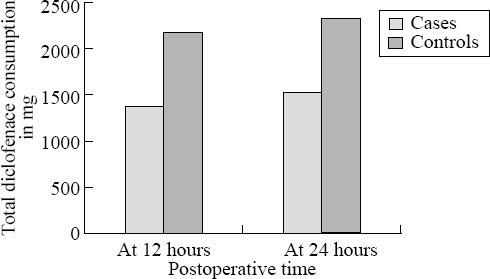
Postoperative total diclofenace consumption of the patients who underwent femoral bone fracture surgery at 12 and 24 hours in the period of September 2013–May 2014.
Postoperative time for the first analgesic request
Postoperatively, an independent t-test showed that the time from the end of anesthesia to the first analgesic request was significantly different between the two groups (P=0.000). The FICNB group had a longer time for the first analgesic request than the control group (mean±SD) (417±112.10) vs. (139.25±37.67) minutes.
DISCUSSION
This study shows that FICNB provides effective postoperative analgesia when it is used as a multimodal analgesia in the first 24 hours as measured by pain on VAS, total analgesic consumption, and the time for the first analgesic request.
In this study, there was no difference in VAS scores at 15 minutes between the FICNB and control groups. This finding was not consistent with a study from the USA where there was a different pain score on the VAS at 15 minutes.[13] This difference may be due to the analgesic effect of spinal anesthesia that might be continued in the FICNB and control groups by the end of 15 minutes.
The postoperative VAS score was reduced more significantly in the FICNB group than in the control group at 2, 6, 12, and 24 hours. The result at 2 hours was incomparable with that of a study from the USA.[13] This difference might be due to the high prevalence of comorbidities found in the studied groups in the USA. However, our finding was consistent with that of a study from the UK.[3] The similarity might be due to the same dose of a local anesthetic, 30 mL of 0.25% bupivacaine given for patients of 40 to 80 kg body weight both in our study and the UK study.
The median VAS score at 6 hours was more significantly reduced in the FICNB group than in the control group (P=0.000). Our finding was comparable with that of a Korean study.[14] This similarity might be related to the wear off analgesic effects of spinal anesthesia in the control group, and the efficacy of nerve block in the FICNB group continued since the duration of FICNB was expected for 8–10 hours.[6]
The VAS score at 12 hours was lower in the FICNB group than in the control group (P=0.006); this finding was consistent with that of a Japanese study.[12] This might be due to pain management using the same class of drug, i.e. diclofenac was given repeatedly at this time interval for both groups.
The VAS score at 24 hours was lower in the FICNB group than in the control group (P=0.001); the result was incomparable with a UK study.[3] This discrepancy might be due to the involvement of different junior doctors without training of anesthesia in dealing with FICNB patients and controls in the UK. However, our finding was comparable with a Korean study showing that FICNB could have a better control of pain than intravenous alfentanil during the first 24 hours.[14] This might be related to the equivalent duration of surgery in the FICNB and control groups.
Regarding the postoperative total analgesic consumption of diclofenace at 12 hours, 38.7% was given to the FICNB group and the remaining 61.3% to the control group (P=0.000). This finding was highly comparable with a Japanese study[12] where the 12-hour diclofenac consumption was 21% in the FICNB group. This difference might be due to a 100% success rate of FICNB in Japan where the success rate was not checked. However, the total tramadol consumption at 12 and 24 hours was not statistically significant respectively (P=0.146 and P=0.083). Another study showed that FICNB reduces the requirement of morphine by 41% compared to those patients who received systemic analgesia (P=0.018).[9] The difference might be due to only few patients who were given opioid analgesia at the postoperative period in our hospital.
In our study, the time for the first analgesic request was prolonged in the FICNB group. The FICNB group had the first analgesic request after 417.50 minutes, and the control group after 139.25 minutes. A Korean study found that the first analgesic request happened after 8.6 hours (516 minutes) in the FICNB group, whereas after 4.5 hours (270 minutes) in the control group.[14] This marked difference compared to that of our study might be related to the cases delt with by the experienced anesthetists, who also rejected patients with failure of nerve block.
There was no complication induced by FICNB technique because the site of needle injection for FICNB is far from the femoral nerves and blood vessels. Thus accidental intraneural and intravascular injury can be avoided.[18–20] The results of this study will promote the practice of FICNB in our institute, which is part of the MSc course.
There are limitations in this study. The FICNB failure rate at the postoperative period was not checked, and the patients were not randomized even though they were comparable between the FICNB and control groups. The involvement of four MSc anaesthesia students in the management of patients both in FICNB and controls group might affect the result of the study due to interpersonal variation of skill and knowledge. The data collectors were not truly blinded because they might get the nerve block information from the chart of anesthesia.
In conclusion, a single injection of FICNB could relieve pain during the first 24-hour postoperative period, decrease the total postoperative analgesic consumption at 12 and 24 hours, and significantly prolong the time for the first analgesic request after femoral bone fracture surgery. We recommend FICNB for analgesia after surgery for femoral bone fracture and for patients with femoral bone fracture at the emergency department. We also recommend further study to determine the optimal effects of this regional block on such patients by checking the success rate of FICNB.
Footnotes
Funding: This study was granted by the Amhara Regional State.
Ethical approval: Ethical clearance was obtained from the School of Medicine Ethical Review committee, Gondar College of Medicine and Health Sciences, the University of Gondar.
Conflicts of interest: We do not have any conflicts of interest.
Contributors: All authors conceived the study, developed the proposal, involved in data collection, data analysis, and manuscript preparation. All authors approved the final version of the article and agreed to publish in WJEM.
REFERENCES
- 1.Admassie D, Yirga T, Wamisho LB. Adult limb fractures in Tikur Anbessa Hospital caused by road traffic injuries: Half year plain radiographic pattern. Ethiop J Health Dev. 2010;24:61–63. [Google Scholar]
- 2.Newman B, McCarthy L, Thomas PW, May P, Layzell M, Horn K. A comparison of pre-operative nerve stimulator-guided femoral nerve block and fascia iliaca compartment block in patients with a femoral neck fracture. Anaesthesia. 2013;68:899–903. doi: 10.1111/anae.12321. [DOI] [PubMed] [Google Scholar]
- 3.Hanna L, Gulati L, Graham A. Hindawi Publishing Corporation; 2014. The role of fascia iliaca blocks in hip fractures: A prospective case-control study and feasibility assessment of a junior-doctor-delivered service. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dalens B, Vanneuville G, Alain Tanguy A. Comparison of the fascia iliaca compartment block with the 3-in-1 block in children. Anesth Analg. 1989;69:705–713. [PubMed] [Google Scholar]
- 5.Lopez S, Gros T, Bernard N, Plasse C, Capdevila X. Fascia iliaca compartment block for femoral bone fractures in prehospital care. Reg Anesth Pain Med. 2003;28:203–207. doi: 10.1053/rapm.2003.50134. [DOI] [PubMed] [Google Scholar]
- 6.Høgh A, Dremstrup L, Jense SS, Lindholt J. Fascia iliaca compartment block performed by junior registrars as a supplement to pre-operative analgesia for patients with hip fracture. Strat Traum Limb Recon. 2008;3:65–70. doi: 10.1007/s11751-008-0037-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dolan J, Williams A, Murney E, Kenny NCG. Ultrasound guided fascia iliaca block: A comparison with the loss of resistance technique. Reg Anesth Pain Med. 2008;33:526–531. doi: 10.1016/j.rapm.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 8.Capdevila X, Biboulet P, Bouregba M, Barthelet Y, Rubenovitch J, d'Athis F. Comparison of the three-in-one and fascia iliaca compartment blocks in adults: clinical and radiographic analysis. Anesth Analg. 1998;86:1039–1044. doi: 10.1097/00000539-199805000-00025. [DOI] [PubMed] [Google Scholar]
- 9.Leeper DA, Brandon PT, Morgan AVM, Cutts S, Cohen AMM. Fascia iliaca compartment block reduces morphine requirement pre-operatively for patients with fractured neck of femur. Eur J Trauma Emerg Surg. 2012;38:673–677. doi: 10.1007/s00068-012-0230-x. [DOI] [PubMed] [Google Scholar]
- 10.Kaldirim U, Yolcu U. Fascia iliaca compartment block for hip dislocation. Eur J Emerg Med. 2015;22:145–146. doi: 10.1097/MEJ.0000000000000190. [DOI] [PubMed] [Google Scholar]
- 11.Chu RS, Browne GJ, Cheng NG, Lam LT. Femoral nerve block for femoral shaft fractures in a paediatric Emergency Department: can it be done better? Eur J Emerg Med. 2003;10:258–263. doi: 10.1097/00063110-200312000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Fujihara Y, Fukunishi S, Nishio S, Miura J, Koyanagi S, Yoshiya S. Fascia iliaca compartment block: its efficacy in pain control for patients with proximal femoral fracture. J Orthop Sci. 2013;18:793–797. doi: 10.1007/s00776-013-0417-y. [DOI] [PubMed] [Google Scholar]
- 13.Monzón GD, Vazquez J, Jauregui RJ, Iserson VK. Pain treatment in post traumatic hip fracture in the elderly: regional block vs. systemic nonsteroidal analgesics. Int J Emerg Med. 2010;3:321–325. doi: 10.1007/s12245-010-0234-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yun JM, Kim HY, Han KM, Kim HJ, Hwang WJ, DO HS. Analgesia before a spinal block for femoral neck fracture: fascia iliaca compartment block. Acta Anaesthesiol Scand. 2009;53:1282–1287. doi: 10.1111/j.1399-6576.2009.02052.x. [DOI] [PubMed] [Google Scholar]
- 15.Martinez KA, Snyder CF, Malin JL, Dy SM. Is race/ethnicity related to the presence or severity of pain in colorectal and lung cancer? J Pain Symptom Manage. 2014;48:1050–1059. doi: 10.1016/j.jpainsymman.2014.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matutina ER, Mueller M, Kelechi JT. Racial differences in pain reports between black and white participants with chronic venous disorders treated with cryotherapy compared to usual care. Ethn Dis. 2011;21:451–457. [PubMed] [Google Scholar]
- 17.Degu G, Tessema F. Lecture notes for health science students biostatistics. University of Gondar. 2005;184 [Google Scholar]
- 18.Foss BN, Kristensen BB, Bundgaard M, Bak M, Heiring C, Virkelyst C, et al. Fascia iliaca compartment blockade for acute pain control in hip fracture patients. Anesthesiology. 2007;106:773–778. doi: 10.1097/01.anes.0000264764.56544.d2. [DOI] [PubMed] [Google Scholar]
- 19.Mouzopoulos G, Vasiliadis G, Lasanianos N, Nikolaras G, Morakis E, Kaminaris M. Fascia iliaca block prophylaxis for hip fracture patients at risk for delirium: a randomized placebo-controlled study. J Orthopaed Traumatol. 2009;10:127–133. doi: 10.1007/s10195-009-0062-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wathen EJ, Gao D, Merritt G, Georgopoulos G, Battan KF. A Randomized Controlled Trial comparing a fascia iliaca compartment nerve block to a traditional systemic analgesic for femur fractures in a pediatric emergency department. Ann Emerg Med. 2007;50:162–171. doi: 10.1016/j.annemergmed.2006.09.006. [DOI] [PubMed] [Google Scholar]


