Abstract
Background
Hoarseness (dysphonia) is the reason for about 1% of all consultations in primary care. It has many causes, ranging from self-limited laryngitis to malignant tumors of the vocal cords.
Methods
This review is based on literature retrieved by a selective search in PubMed employing the terms “hoarseness,” “hoarse voice,” and “dysphonia,” on the relevant guideline of the American Academy of Otolaryngology —Head and Neck Surgery, and on Cochrane reviews.
Results
Hoarseness can be caused by acute (42.1%) and chronic laryngitis (9.7%), functional vocal disturbances (30%), and benign (10.7–31%) and malignant tumors (2.2–3%), as well as by neurogenic disturbances such as vocal cord paresis (2.8–8%), physiologic aging of the voice (2%), and psychogenic factors (2–2.2 %). Hoarseness is very rarely a manifestation of internal medical illness. The treatment of hoarseness has been studied in only a few randomized controlled trials, all of which were on a small scale. Voice therapy is often successful in the treatment of functional and organic vocal disturbances (level 1a evidence). Surgery on the vocal cords is indicated to treat tumors and inadequate vocal cord closure. The only entity causing hoarseness that can be treated pharmacologically is chronic laryngitis associated with gastro-esophageal reflux, which responds to treatment of the reflux disorder. The empirical treatment of hoarseness with antibiotics or corticosteroids is not recommended.
Conclusion
Voice therapy, vocal cord surgery, and drug therapy for appropriate groups of patients with hoarseness are well documented as effective by the available evidence. In patients with risk factors, especially smokers, hoarseness should be immediately evaluated by laryngoscopy.
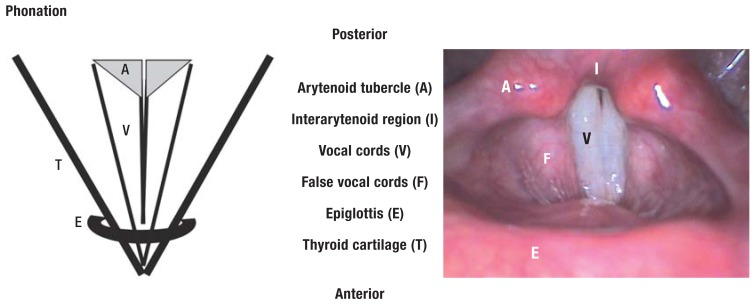
Dysphonia, with the cardinal symptom of hoarseness, has a prevalence of around 1% among patients in general (1) and a lifetime prevalence of approximately 30% (e1). The term dysphonia is used to describe any impairment of the voice—alteration in the sound of the voice with hoarseness, restriction of vocal performance, or strained vocalization. The pathophysiology of hoarseness is characterized by muscle tone– related irregularity in the oscillation of the vocal cords owing to hypertonic dysphonia, incomplete closure of the glottis on vocalization, or an increase in vocal cord bulk, perhaps due to a tumor (Figure 1a, b).
Figure 1a.
Indirect laryngoscopy during phonation
The aim of this review is to summarize the current knowledge of hoarseness: the potential causes, the means of diagnosis, the treatment options, and the evidence for their efficacy (eTable) (2, e2, e3).
eTable. Definition and classification of evidence levels and recommendation grades.
| Evidence level | Strength | Definition | Recommendation |
|---|---|---|---|
| 1a | A | Meta-analyses. systematic _reviews of randomized controlled trials. megatrials | "Should" |
| 1b | Randomized controlled trials | ||
| 2a | B | Non-randomized studies. cohort studies with control groups | "Probably should" |
| 2b | C | Observational studies _(case–control studies. cohort _studies) | "May" |
| 3 | D | Cross-sectional studies. _ecological studies. cohort studies without control group. case reports | GCP |
| 4 | X | Clinical experience | GCP |
To this end, we carried out a selective survey of the literature using the search terms “hoarseness,” “hoarse voice,” and “dysphonia,” with particular reference to evidence-based guidelines from America (2, e4). Moreover, we included treatment recommendations from Cochrane reviews. Because no evidence-based guidelines have been published in German, we also took account of expert opinion.
The causes of hoarseness are diverse:
Acute and chronic laryngitis (accounting for 42.1% and 9.7% of cases respectively)
Functional dysphonia (30%)
Benign and malignant tumors (10.7 to 31.0% and 2.2 to 3.0% respectively)
Neurogenic factors such as vocal cord paralysis (2.8 to 8%)
Physiological aging (2%)
Very occasionally hoarseness can be attributed to manifestations of laryngeal disease other than tumors (Table 1).
Table 1. Causes and characteristics of hoarseness.
| Pathology | Proportion of all cases | Typical symptoms | Treatment | Evidence | ||
|---|---|---|---|---|---|---|
| Functional dysphonia | Hyperfunctional dysphonia | 30% | Hoarseness with vocal strain | Voice therapy | 1a/A | |
| Secondary manifestation of functional dysphonia | Vocal cord nodules | Included in benign tumors (10.7–31%) | Hoarseness with vocal strain | Voice therapy (phonosurgery) | 1a/A | |
| Organic dysphonia | Laryngitis | Acute | 42.1% | Hoarseness. infection | No medicinal treatment. self-limiting | 1a/A |
| Chronic | 9.7% | Constant hoarseness. dysphonia. throat _sensations. compulsion to clear throat | Avoidance of noxae. laryngostroboscopic _monitoring | 4/X | ||
| Benign tumors | Polyps/cysts | 10.7–31% | Hoarseness. reduced volume of voice. _vocal fatigue | Phonosurgery. if applicable voice therapy | 2a/B | |
| Reinke edema | Hoarseness. vocal fatigue. deep voice | Avoidance of noxae. phonosurgery. _if applicable voice therapy | 2a/B | |||
| Recurring _papillomatosis | Hoarseness. dyspnea | Phonosurgery | 2a/B | |||
| Vocal cord malignancies | 2.2–3% | Hoarseness as early symptom | (Laser) surgery. radiotherapy | 2a/B | ||
| Vocal cord scarring | n.d. | Constant hoarseness. quiet voice | Voice therapy (phonosurgery) | 4/X | ||
| Presbyphonia | 2% | Hoarseness. high-pitched voice | Voice therapy. phonosurgery | 2a/B | ||
| Manifestation of internal_ disease | Laryngopharyngeal reflux | Included in chronic laryngitis (9.7%) | Only slight hoarseness. throat sensations _predominantly at night | With signs of reflux: PPIs | 2b/C | |
| Without signs of reflux: no PPIs | 2a/B | |||||
| Tuberculosis | n.d. | Dyspnea. cough | Tuberculostatic treatment | 3/D | ||
| Rheumatoid diseases | Rheumatoid arthritis | n.d. | Hoarseness. dyspnea. or dysphagia. _depending on site | Antirheumatic treatment | 3/D | |
| Collagenoses (systemic lupus erythematosus) | n.d. | |||||
| Vasculitides (Wegener disease) | n.d. | |||||
| Sarcoidosis | n.d. | |||||
| Amyloidosis | n.d. | Hoarseness. dyspnea. or dysphagia. _depending on site | Phonosurgery. internal / hematological _treatment | 3/D | ||
| Lymphoma | n.d. | Dysphonia. dyspnea | Internal / hematological treatment | 4/X | ||
| Neurological diseases | Vocal cord paresis | 2.8–8.0% | Hoarseness. impaired speech breathing | Voice therapy. phonosurgery | 1a/A. 2a/B | |
| Spasmodic dysphonia | n.d. | Variable hoarseness | Administration of botolinumtoxin A | 2a/B | ||
| Vocal cord dysfunction | n.d. | Hoarseness during an episode of respiratory distress (few seconds) | Discuss with patient. breathing therapy. _psychotherapy | 4/X | ||
| Psychogenic dysphonia | 2–2.2% | Sudden hoarseness (hours or days) | Psychological and psychosomatic treatment. psychotherapy | 4/X | ||
Etiological classification of dysphonias according to causes. typical symptoms and characteristics of hoarseness. showing each cause’s percentage contribution to the total. Phonosurgery is an operative intervention to improve the voice. usually using microinstruments inserted transorally via a laryngoscope. sometimes by means of laser. n.d.. no data or prevalence <1%; PPIs. proton pump inhibitors (1, 2. e2-e5)
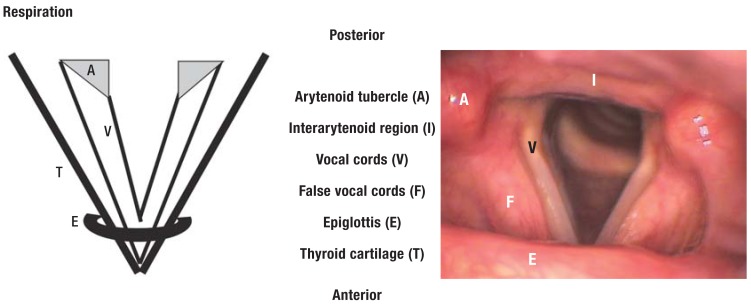
Suspicion of a serious underlying disease (Box, Figure 2) or persistence of hoarseness for more than 3 months (eTable) (2) should prompt immediate investigation by means of indirect laryngoscopy.
Box. Serious comorbidities of hoarseness.
Comorbidities and additional risk factors that require urgent laryngoscopic examination by an otorhinolaryngologist:
History of nicotine and/or alcohol consumption
Enlarged cervical lymph nodes
Hoarseness following trauma
Association with hemoptysis, dysphagia, odynophagia, otalgia, or dyspnea
Neurological symptoms
Unexplained weight loss
Progression of hoarseness
Immunosuppression
Possible bolus aspiration
Hoarseness after an operative intervention (intubation, neck surgery)
Figure 1b.
Indirect laryngoscopy during respiration
Functional dysphonia
In the absence of a specific anatomic correlate such as a tumor, patients with hyperfunctional dysphonia, i.e., a non-physiological increase in tone of the vocal cords on phonation, in speaking or breathing, develop marked difficulties in speaking, with accompanying hoarseness. Women are more frequently affected than men (e5). The stroboscopic oscillation of the vocal cords is impaired or irregular due to abnormal muscle tone. The measure of choice is conservative treatment to counteract the damaging strain on the voice. Various procedures are available to improve vocal and respiratory technique and vocal hygiene (evidence level 1a, recommendation grade A) (2, e4). The prognosis of speech therapy is favorable (e6– e17); in 46 to 93% of cases (e8, e9) vocal performance is clearly improved. Only a few randomized controlled trials have been published, all of them with small case numbers, and there are no long-term studies (Table 2) (3, e16, e17).
Table 2. Characteristics of randomized controlled trials on treatment of hoarseness.
| Reference | Disease | n | Form of _evaluation | Treatment procedure/group | Remarks |
|---|---|---|---|---|---|
| (e10) | Functional dysphonia (female teachers with voice problems) |
44 | 1. 3 | G1 = vocal hygiene (n = 15) G2 = voice amplifier (n = 15) G3 = no treatment (control) (n = 14) |
G1 and G2 benefited compared with G3 |
| (e9) | Functional dysphonia | 30 | 1. 2. 3. 4 | G1 = indirect treatment (n = 10) G2 = direct and indirect treatment (n = 10) G3 = no treatment (control) (n = 10) |
G1 (60%) and G2 (90%) benefited compared with G3 (10%) |
| (e8) | Functional dysphonia | 45 | 1. 2. 3. 4 | G1 = indirect treatment (n = 10) G2 = direct and indirect treatment (n = 10) G3 = no treatment (control) (n = 10) | G1 (46%) and G2 (93%) benefited most; G3 (14%) |
| (e11) | Functional dysphonia (female teachers with voice problems) |
40 | 2. 3 | G1 = treatment (n = 22) G2 = no treatment (control) (n = 18) |
Significant improvement in G1 compared with G2 |
| (e12) | Functional dysphonia | 50 | 1. 2. 5 _(electroglottography) | G1 = classic voice therapy (n = 26) G2 = voice therapy with visual biofeedback. flexible transnasal (n = 25) |
G1 und G2 benefited significantly; G2 was more effective |
| (e13) | Female teachers with voice problems | 20 | 1. 4 | G1 = voice therapy (n = 9) G2 = no treatment (control) (n = 11) |
Significant improvement in G1 compared with G2 |
| (e14) | Patients with functional dysphonia but without any other relevant organic pathology such as polyps or vocal cord paresis | 133 | 1. 2. 3. 4 | G1 = voice exercise treatment (n = 70) G2 = no treatment (control) (n = 63) |
Significant improvement in G1 compared with G2 |
| (e15) | Female student teachers with mild voice problems due to vocal cord edema or functional dysphonia | 40 | 1. 2. 4 | G1 = voice exercise treatment (group therapy) (n = 20) G2 = no treatment (control) (n = 20) |
Significant improvement in G1 compared with G2 |
| (e42) | Status post laser resection/irradiation of vocal cord cancer | 23 | 1. 2. 4 | G1 = voice therapy (n = 12) G2 = no treatment (control) (n = 11) |
G1 benefited compared with G2 |
| (e26) | Acute laryngitis | 106 | 2. 4 | G1 = erythromycin (n = 56) G2 = no treatment (control) (n = 50) |
No differences in voice quality or laryngoscopy findings |
| (e25) | Acute laryngitis | 100 | 2 | G1 = penicillin V (n = 50) G2 = no treatment (control) (n = 50) |
No differences in voice quality |
| (18) | Presbyphonia | 16 | 1 | G1 = VFE (n = 6) G2 = PhoRTE (n = 5) G3 = no treatment (control) (n = 5) |
Significant improvement in G1 und G2 compared with G3 |
| (36) | Spasmodic dysphonia of _adductor type | 13 | 3 | G1 = administration of botulinumtoxin A _(n = 7) G2 = no treatment (control) (n = 6) |
Distinct improvement of voice in G1 compared with control G2 |
Summary of randomized controlled trials on treatment of hoarseness with evidence level 1a or 1b
Form of evaluation: 1 = assessment of quality of life; 2 = auditory perception; 3 = acoustic/technical analyses; 4 = laryngo(strobo)scopy; 5 = other
G. group; n. number of patients; VFE. vocal function exercise; PhoRTE. phonation resistance training exercise
Organic secondary manifestation of functional dysphonia
Juvenile and adult forms of vocal cord nodules are distinguished (screamer’s nodules and singer’s nodules). The vocal cord changes are a secondary manifestation of untreated hyperfunctional dysphonia. Initially, there is reactive phonation hyperplasia of the medial margin of the vocal cord—at the junction of the anterior third and middle third, the site of greatest stress on phonation. The tissue swells reversibly and edema arises. With the passage of time, the soft swellings undergo fibrosis and turn into hard nodules (e18, e19), preventing complete closure of the vocal cords in the affected area. The treatment of choice is voice therapy (evidence level 1a, recommendation grade A) (2, e6, e20). Only infrequently is microsurgical excision necessary in adults (2, e6, e16, e18). In over 80% of patients the voice is restored to normal by voice therapy alone (e21). Recurrence rates of 30% after voice therapy and 13% after phonosurgery have been reported (e22). In children the change of voice is often followed by spontaneous remission (>90% of boys, ca. 50% of girls) (2, e4, e23, e24).
Organic dysphonia
Acute laryngitis
Acute laryngitis is the most common cause of hoarseness, accounting for 40% of cases (1), and is almost always viral in origin. It occurs in infections of the upper respiratory tract and is self-limiting, subsiding after 1 to 2 weeks (2, e25, e26). Patients are counseled to limit how much they talk, but absolute voice rest is not advised in order to avoid the risk of overcompensation to the point of aphonia (4). Routine antibiotic treatment is discouraged (evidence level 1a, recommendation grade A) (2, 5, e4); antibiotics are prescribed only in exceptional circumstances, e.g., in the presence of bacterial superinfection or laryngeal tuberculosis (Table 1). Indirect or direct laryngoscopy is indicated in such severe cases (evidence level 4, recommendation grade C) (Figure 2). Corticosteroids should not be administered in acute laryngitis (evidence level 3, recommendation grade B) (2).
Chronic laryngitis
Chronic laryngitis has an incidence of 3.5 /1000 in the general population (e27) and is a precursor of vocal cord cancer (6, 7). The following have been proposed as important etiological factors:
Nicotine abuse
Inhaled corticoid treatment
Inhaled environmental noxae
Gastroesophageal reflux with laryngopharyngeal involvement.
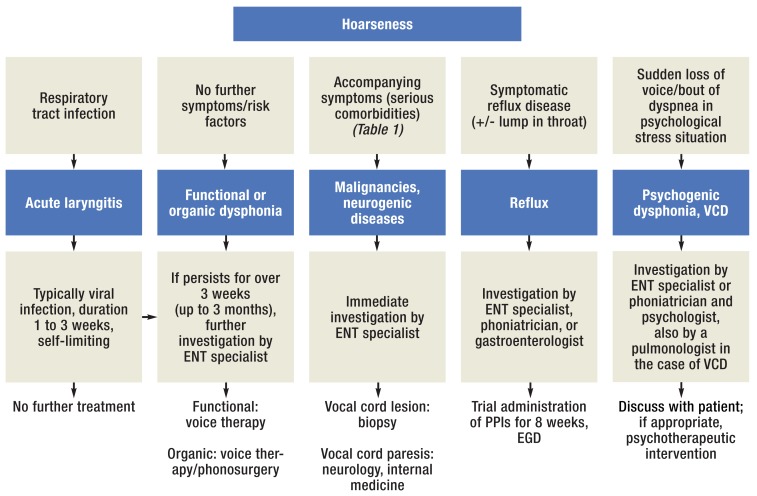
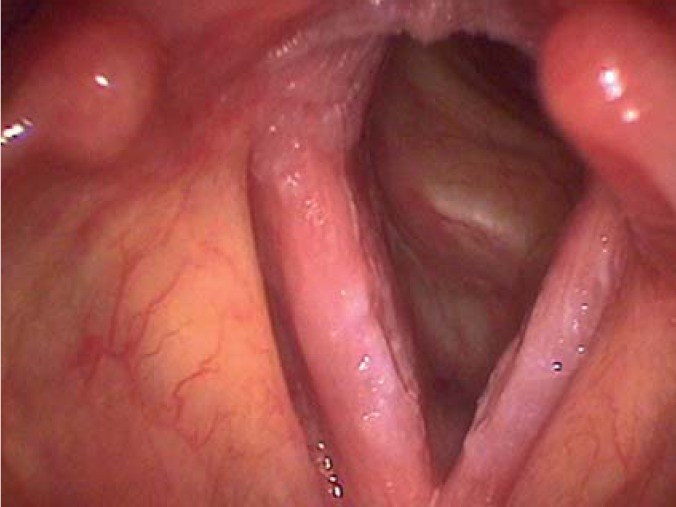
Not infrequently leukoplakia arises (Figure 3). Possible clinical signs of chronic laryngitis are dysphonia, sensations in the throat, and a constant urge to clear the throat (e27). The principal therapeutic measures are avoidance of noxae and regular laryngeal stroboscopy for early detection of malignancy (4, 6). Meta-analyses have shown that laryngeal dysplasia or leukoplakia progresses to cancer in 14 to 16% of patients after a mean interval of 43 months (range 4 to 192 months) (e28, e29).
Figure 2.
Algorithm for diagnosis of hoarseness. ENT, ear, nose, and throat; VCD, vocal cord dysfunction; PPI, proton pump inhibitor; EGD, esophagogastroduodenoscopy; VC, vocal cord
Benign and malignant tumors
Vocal cord polyps/vocal cord cysts – Vocal cord polyps are unilateral tissue proliferations on the free margin of the vocal cord and thus hamper phonation (8). Men are more frequently affected (55%) (e30). The factors promoting the formation of vocal cord polyps include smoking (51 to 90%) (8), chronic laryngitis, and phonation trauma, i.e., microvascular trauma with local edematous remodeling processes and accompanying inflammation as a result of misuse of the voice (9). Retention cysts arise when the excretory ducts of the mucous glands are obstructed. The symptoms are hoarseness together with reduced volume and fatigue of the voice. The treatment of choice for polyps is phonosurgical excision at the base. Cysts must be removed in toto with the capsule (evidence level 2a, recommendation grade B) (2) (9, e24, e31).
Reinke edema – Reinke edema is caused predominantly by tobacco smoke and mainly affects women (80%) between the ages of 40 and 60 years (ca. 47%) (e30). Phonosurgical removal of the edema results in improvement of the pitch, resonance, and also resilience of the voice. Dysplasia is rare (<1%) (e32). It is essential to stop smoking, although this does not always achieve marked amelioration of the edema (e33). As with polyps and cysts, additional voice therapy may be required to correct a reactive vocal dysfunction that has arisen preoperatively (evidence level 2a, recommendation grade B) (2).
Recurring papillomatosis – Juvenile (RJP) and adult (RAP) forms of recurring papillomatosis are distinguished. RJP usually arises between the ages of 2 and 4 years and is a major cause of hoarseness and also dyspnea in childhood (10– 12). There are over 100 different types of human papilloma virus (HPV), the most important of which are HPV 6, 11, 16, and 18 (10, 13). In children, infection with HPV 11 has a severe course and may even lead to obstruction of the respiratory tract (12). Hoarseness is the cardinal symptom of RAP, the occurrence of which peaks between the ages of 20 and 40 years. A retrospective cohort study found epithelial dysplasia in 28% of cases (e34). Association of HPV with laryngeal cancer is rare (1.6 to 1.7%) (e35, e36), and association with squamous epithelial carcinoma of the lung has been described only in isolated cases (12, 14, e37). The precise mode of transmission is unknown (10). The primarily benign, cauliflower-like neoplasms are found mostly in the area of the vocal cords or extralaryngeally in the trachea, bronchi, or lungs (11). Papillomas are excised microsurgically (evidence level 2a, recommendation grade B) (2). There is insufficient evidence (15) to support adjuvant antiviral treatment with intralesional administration of cidofovir, which is currently licensed only for the treatment of cytomegalovirus (CMV) retinitis in AIDS patients (e38). Individual cases of successful active immunization against HPV in laryngeal papillomatosis have been reported, albeit with limited follow-up (13). The disease course varies from spontaneous remission over a stable stage to aggressive progression necessitating repeated interventions (11).
Vocal cord malignancies – Around two thirds of laryngeal cancers are located in the area of the vocal cords. The incidence in the general population is 7/100 000 (e39). Squamous epithelial carcinoma accounts for more than 90% of cases (7). In contrast to the strong association of HPV with tonsillar carcinoma (OR 15.1, 95% confidence interval [CI] 6.8 to 33.7), only a weak association has been demonstrated for laryngeal cancer (odds ratio [OR] 2.0, 95% CI 1.0 to 4.2) (e40). Dysphonia is considered an early symptom (7). In microlaryngostroboscopy, the term phonatory standstill is used to describe the state in which the fine vibrations of the tumor-infiltrated vocal cords are abolished. The swift occurrence of hoarseness leads to diagnosis of (glottic) laryngeal cancer at an early stage (T1) in 24 to 30% of cases (e39). Correspondingly, the rates of lymph-node and distant metastases at the time of diagnosis are low. The 5-year survival rate is practically 100%. The treatment comprises transoral (laser) resection or primary low-volume radiotherapy (e41). An up-to-date S3 guideline is currently being compiled. Treatment may be followed by hoarseness owing to scarring or, in the case of tissue loss, incomplete glottic closure (16). In this event, voice therapy often has a successful result (evidence level 1b, recommendation grade A) (e42).
Vocal cord scarring – Scarring of the sulcus between the vocal cord epithelium and the vocal muscle may be congenital, but in most cases occurs following severe laryngitis (Figure 3) or (phono)surgical interventions. Laryngoscopy of the area around the sulcus shows abolition of the fine vibrations or, in the event of significant tissue loss, incomplete glottic closure (16). The voice is constantly hoarse and may be breathy and poorly audible. Voice therapy usually only corrects the dysfunction, failing to achieve any relevant improvement in resonance, and surgery to release the scars or deal with the incomplete closure of the glottis is also challenging. Reported results mostly describe the authors’ own experience; there are no prospective studies from which evidence-based treatment recommendations could be derived (17).
Presbyphonia
Presbyphonia, the physiological hoarseness of old age, is found in around 25% of those over 65 years of age. The frequency is about the same in men and women (e43). The vocal cord musculature atrophies in the course of the physiological aging process, giving rise to a more oval shape of the vocal cord fissure during phonation. Furthermore, the mucus-producing cells of the vocal cord also atrophy with age, so the surface film increases in viscosity, negatively influencing the sound of the voice. The leading symptom is a weak, less intense voice produced at the cost of pronounced strain. Presbyphonia must be distinguished from organic disorders of the vocal cords and from other illnesses, e.g., chronic obstructive pulmonary disease (e44). Treatments that can be considered are voice therapy, which may help to regulate the tone and improve the subglottic air pressure, and phonosurgical measures to reinforce glottis closure (evidence level 2a, recommendation grade B) (18, e43).
Manifestation of internal diseases
Laryngopharyngeal reflux
Nine to 26% of the population (e5, e45) suffer from reflux-related mucosal irritation of the larynx and pharynx with chronic laryngitis (e45). Moreover, reflux is an important trigger factor for laryngospasm or vocal cord dysfunction (VCD). Up to 92% of these patients mention hoarseness, chronic urge to cough, throat clearing, a lump in the throat, and unspecific swallowing difficulties (e45, e46). Laryngoscopy reveals vocal cord edema, mucosal erythema, or gastric laryngitis, i.e., mucosal hyperplasia with plication of the interarytenoid region in the posterior part of the larynx (Figure 1a, b) (e45, e46). Trial treatment with proton pump inhibitors is important in establishing the diagnosis (e47). Another treatment option is antireflux therapy, if hoarseness occurs in chronic laryngitis with signs of reflux disease (evidence level 2b, recommendation grade C). In the absence of reflux this treatment is inappropriate (evidence level 2a, recommendation grade B) (2, e4, e48). Overall, the diagnosis of laryngopharyngeal reflux (LPR) is assigned uncritically and too often among patients with dysphonia (e48). Accordingly, the symptomatic measures remain ineffective.
Internal diseases with occasional laryngeal manifestations
Tuberculosis (19, e49); rheumatoid diseases such as rheumatoid arthritis (20, e50), systemic lupus erythematosus (21, e51), Wegener disease (22, e52), and laryngeal sarcoidosis (23); amyloidosis (24, e53, e54); and manifestations of lymphoma (e55, e56) are among the internal diseases with occasional laryngeal involvement (Table 1). In all these diseases interdisciplinary management is mandatory. The treatment is usually based on experience from case series (evidence level 3, recommendation grade D) (25, 26).
Neurogenic causes
Vocal cord paralysis
Vocal cord paralysis may be partial (reduced mobility) or complete, caused by damage to the recurrent laryngeal nerve; a dysphonia arises from the incomplete glottic closure or irregular vibration of the vocal cords. The majority of vocal cord paralyses (24 to 79%) can be attributed to iatrogenic causes, such as surgery or trauma in the region of the vagus nerve or the recurrent laryngeal nerve (27, 28, e57, e58). A prominent role is played by thyroid gland interventions, 0.5 to 2.3% of which result in permanent vocal cord paresis (29, 30). Other operations that have been described as causing vocal cord paralysis (28, 29) include surgery on the heart or aorta (e59), cervical spine surgery, and thoracic surgery (e58). Vocal cord paresis may be the first symptom of malignancy; this is the case in 0.9 to 1.6% of thyroid cancers (e60) and 1.5 to 43% of bronchial carcinomas (28, e57, e61). In 2 to 41% of cases the paralysis is idiopathic—the cause is never ascertained (27, 28, e57, e58, e62– e65).
The treatment should begin with speech therapy (evidence level 1a, recommendation grade A). If voice quality has shown no decisive improvement after 2 months and incomplete vocal cord closure persists, temporary vocal cord filling (injection glottoplasty/augmentation) is recommended, e.g., with hyaluronic acid (evidence level 2a, recommendation grade B) (32, e66– e70). Once the paresis has persisted for 12 months, recovery is unlikely. In this case autologous fat (less resorbable) should be used for injection glottoplasty (e71), or external thyroplasty can be performed (32, e72).
Spasmodic dysphonia
Spasmodic dysphonia (SD) is one of the focal dystonias. It occurs almost exclusively in adulthood and predominantly in women (33). This severe dysphonia leads to involuntary spasms of the laryngeal musculature with increased adduction or abduction of the vocal cords, depending on subtype. Sensorimotor control of the larynx is affected, probably owing to a neurotransmitter disorder (34). The adductor type of SD, found in 90% of cases, is characterized by the vocal cords pressing harder against each other during phonation. This results in a creaky voice and intermittent voice breaks during speech (so-called vocal stuttering) (e73). The abductor type, in the remaining 10% of patients, leads to voiceless phases with breathy intonation. Treatment comprises injection of the neurotoxic protein botulinum toxin into the affected vocal cord muscles (evidence level 2a, recommendation grade B) (2, 34– 36, e74).
Vocal cord dysfunction
VCD, sometimes called “laryngeal asthma,” is an intermittent, functional laryngeal obstruction causing dyspnea. It occurs due to laryngeal hyperreactivity on inspiration. A multifactorial etiology is assumed. Proposed trigger mechanisms include repeated exposure of the larynx to irritative inhaled stimuli such as perfumes or allergens and microaspiration in the presence of laryngopharyngeal reflux (37, e75, e76). Patients with VCD subjectively experience the bouts of respiratory distress as life-threatening and often develop secondary anxiety and panic attacks. The episodic dyspnea with stridor is accompanied by further symptoms such as dysphonia or aphonia. Many years often elapse before VCD is diagnosed. Flexible transnasal laryngoscopy is considered the gold standard for diagnosis and shows the paradoxical vocal cord motion with adduction on inspiration. VCD may occur in isolation but is also found in 3 to 5% of asthmatics (37). In contrast to the classical bronchial asthma, medicinal therapy is ineffective (37, e77, e78). The episodes of respiratory distress can usually be controlled well by means of special breathing techniques (37). Psychotherapy is sometimes also recommended, particularly for patients with secondary anxiety and panic attacks, but the fact that predominantly case series have been published means there is no sufficient evidence of its effect (e79).
Psychogenic dysphonia
Psychogenic dysphonia preferentially affects women between the ages of 20 and 40 years (e80). The patients complain of sudden extreme hoarseness or even acute aphonia. By contrast, loud coughing or throat clearing is still possible, i.e. vocal function is impaired only in communicative contexts. Laryngoscopy shows no inflammation, but sometimes there is muscle tone-related limitation of adduction of the vocal cords during phonation (e81, e82). These findings are often incorrectly diagnosed and treated as acute laryngitis (38, e80). Our investigation of 40 patients showed that psychogenic dysphonia is often an acute manifestation preceded by severe psychological stress (38). Behavioral psychotherapy is helpful (38, e81), whereas voice therapy is completely ineffective (38– 40).
Figure 3.
Laryngoscopy in a heavy smoker with chronic leukoplakia and bilateral sulcus vocalis. His voice sounded husky and strained
Key Messages.
Hoarseness has many different causes and interdisciplinary management is often required.
In the presence of risk factors, investigation by laryngoscopy is mandatory.
Only a small number of randomized controlled trials of treatment for hoarseness have been published.
Options for treatment are voice therapy and phonosurgery, i.e., an operation to improve the voice.
Trial use of antibiotics to treat hoarseness is strongly discouraged.
Acknowledgments
Translated from the original German by David Roseveare.
Footnotes
Conflict of interest statement
Prof. Reiter has received study support (third-party funding) and reimbursement of travel costs from bess medizintechnik.
The remaining authors declare that no conflict of interest exists.
References
- 1.Cohen SM, Kim J, Roy N, Asche C, Courey M. Prevalence and causes of dysphonia in a large treatment—seeking population. Laryngoscope. 2012;122:343–348. doi: 10.1002/lary.22426. [DOI] [PubMed] [Google Scholar]
- 2.Schwartz SR, Cohen SM, Dailey SH, et al. Clinical practice guideline: hoarseness (dysphonia) Otolaryngol Head Neck Surg. 2009;141:1–31. doi: 10.1016/j.otohns.2009.06.744. [DOI] [PubMed] [Google Scholar]
- 3.Bos-Clark M, Carding P. Effectiveness of voice therapy in functional dysphonia: where are we now? Curr Opin Otolaryngol Head Neck Surg. 2011;19:160–164. doi: 10.1097/MOO.0b013e3283448f85. [DOI] [PubMed] [Google Scholar]
- 4.Dworkin JP. Laryngitis: Types, causes and treatments. Otolaryngol Clin North Am. 2008;41:419–436. doi: 10.1016/j.otc.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 5.Reveiz L, Cardona AF. Antibiotics for acute laryngitis in adults. Cochrane Database Syst Rev. 2013;3 doi: 10.1002/14651858.CD004783.pub4. CD004783. [DOI] [PubMed] [Google Scholar]
- 6.Reiter R, Brosch S. Chronic laryngitis-associated factors and voice assessment. Laryngorhinootologie. 2009;88:181–185. doi: 10.1055/s-0028-1100390. [DOI] [PubMed] [Google Scholar]
- 7.Schultz P. Vocal fold cancer. Eur Ann Otorhinolaryngol Head Neck Dis. 2011;128:301–308. doi: 10.1016/j.anorl.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 8.Martins RH, Defaveri J, Domingues MA, de Albuquerque e Silva R. Vocal polyps: clinical, morphological, and immunohistochemical aspects. J Voice. 2011;25:98–106. doi: 10.1016/j.jvoice.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 9.Bohlender J. Diagnostic and therapeutic pitfalls in benign vocal fold diseases. Laryngorhinootologie. 2013;92:239–257. doi: 10.1055/s-0032-1333304. [DOI] [PubMed] [Google Scholar]
- 10.Venkatesan NN, Pine HS, Underbrink MP. Recurrent respiratory papillomatosis. Otolaryngol Clin North Am. 2012;45:671–694. doi: 10.1016/j.otc.2012.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Derkay CS, Wiatrak B. Recurrent respiratory papillomatosis: a review. Laryngoscope. 2008;118:1236–1247. doi: 10.1097/MLG.0b013e31816a7135. [DOI] [PubMed] [Google Scholar]
- 12.Mauz PS, Zago M, Kurth R, et al. A case of recurrent respiratory papillomatosis with malignant transformation, HPV11 DNAemia, high L1 antibody titre and a fatal papillary endocardial lesion. Virol J. 2014;11:114–120. doi: 10.1186/1743-422X-11-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Malagón T, Drolet M, Boily MC, et al. Cross protective afficacy of two human papillomavirus vaccines: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12:781–789. doi: 10.1016/S1473-3099(12)70187-1. [DOI] [PubMed] [Google Scholar]
- 14.Mammas IN, Sourvinos G, Zaravinos A, Spandidos DA. Vaccination against human papilloma virus (HPV): epidemiological evidence of HPV in non-genital cancers. Pathol Oncol Res. 2011;17:103–119. doi: 10.1007/s12253-010-9288-0. [DOI] [PubMed] [Google Scholar]
- 15.Chadha NK, James A. Adjuvant antiviral therapy for recurrent respiratory papillomatosis. Cochrane Database Syst Rev. 2012;12 doi: 10.1002/14651858.CD005053.pub4. CD005053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Allen J. Cause of vocal fold scar. Curr Opin Otolaryngol Head Neck Surg. 2010;18:475–480. doi: 10.1097/MOO.0b013e32833fecd1. [DOI] [PubMed] [Google Scholar]
- 17.Friedrich G, Dikkers FG, Arens C, et al. Vocal fold scars: current concepts and future directions. Consensus report of the Phonosurgery Committee of the European Laryngological Society. Eur Arch Otorhinolaryngol. 2013;270:2491–2507. doi: 10.1007/s00405-013-2498-9. [DOI] [PubMed] [Google Scholar]
- 18.Ziegler A, Verdolini Abbott K, Johns M, Klein A, Hapner ER. Preliminary data on two voice therapy interventions in the treatment of presbyphonia. Laryngoscope. 2014;124:1869–1876. doi: 10.1002/lary.24548. [DOI] [PubMed] [Google Scholar]
- 19.Lim JY, Kim KM, Choi EC, Kim YH, Kim HS, Choi HS. Current clinical propensity of laryngeal tuberculosis: review of 60 cases. Eur Arch Otorhinolaryngol. 2006;263:838–842. doi: 10.1007/s00405-006-0063-5. [DOI] [PubMed] [Google Scholar]
- 20.Bayar N, Kara SA, Keles I, Koç C, Altinok D, Orkun S. Cricoarytenoiditis in rheumatoid arthritis: radiologic and clinical study. J Otolaryngol. 2003;32:373–378. doi: 10.2310/7070.2003.13910. [DOI] [PubMed] [Google Scholar]
- 21.Reiter R, Stier KH, Brosch S. Hoarseness in patient with systemic lupus erythematosus. Laryngorhinootologie. 2011;90:226–227. doi: 10.1055/s-0030-1262795. [DOI] [PubMed] [Google Scholar]
- 22.Gottschlich S, Ambrosch P, Kramkowski D, et al. Head and neck manifestations of Wegener’s granulomatosis. Rhinology. 2006;44:227–233. [PubMed] [Google Scholar]
- 23.Mrówka-Kata K, Kata D, Lange D, Namysłowski G, Czecior E, Banert K. Sarcoidosis and its otolaryngological implications. Eur Arch Otorhinolaryngol. 2010;267:1507–1514. doi: 10.1007/s00405-010-1331-y. [DOI] [PubMed] [Google Scholar]
- 24.Penner CR, Muller S. Head and neck amyloidosis: a clinico pathologic study of 15 cases. Oral Oncol. 2006;42:421–429. doi: 10.1016/j.oraloncology.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 25.Pickhard A, Smith E, Rottscholl R, Brosch S, Reiter R. Disorders of the larynx and chronic inflammatory diseases. Laryngorhinootologie. 2012;91:758–766. doi: 10.1055/s-0032-1323769. [DOI] [PubMed] [Google Scholar]
- 26.Reiter R, Brosch S, Froboese N, Barth TF, Rottscholl R, Pickhard A. Manifestation of rheuma in the larynx. Laryngorhinootologie. 2015;94:189–198. doi: 10.1055/s-0034-1398672. [DOI] [PubMed] [Google Scholar]
- 27.Reiter R, Pickhard A, Smith E, et al. Vocal cord paralysis—analysis of a cohort of 400 patients. Laryngorhinootologie. 2015;94:91–96. doi: 10.1055/s-0034-1370927. [DOI] [PubMed] [Google Scholar]
- 28.Takano S, Nito T, Tamaruya N, Kimura M, Tayama N. Single institutional analysis of trends over 45 years in etiology of vocal fold paralysis. Auris Nasus Larynx. 2012;39:597–600. doi: 10.1016/j.anl.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 29.Rayes N, Seehofere D, Neuhaus P. The surgical treatment of bilateral benign nodular goiter: balancing invasiveness with complications. Dtsch Arztebl Int. 2014;111:171–178. doi: 10.3238/arztebl.2014.0171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jeannon JP, Orabi AA, Bruch GA, Abdalsalam HA, Simo R. Diagnosis of recurrent laryngeal nerve palsy after thyroidectomy: a systematic review. Int J Clin Pract. 2009;63:624–629. doi: 10.1111/j.1742-1241.2008.01875.x. [DOI] [PubMed] [Google Scholar]
- 31.Reiter R, Brosch S. Laryngoplasty with hyaluronic acid in patients with unilateral vocal fold paralysis. J Voice. 2012;26:785–789. doi: 10.1016/j.jvoice.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 32.Reiter R, Hoffmann TK, Rotter N, Pickhard A, Scheithauer MO, Brosch S. Etiology, diagnosis, differential diagnosis and therapy of vocal fold paralysis. Laryngorhinootologie. 2014;93:161–173. doi: 10.1055/s-0033-1355373. [DOI] [PubMed] [Google Scholar]
- 33.Murry T. Spasmodic dysphonia: let’s look at that again. J Voice. 2014;28:694–699. doi: 10.1016/j.jvoice.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 34.Blitzer A, Brin MF, Stewart CF. Botulinum toxin management of spasmodic dysphonia (laryngeal dystonia): a 12-year experience in more than 900 patients. Laryngoscope. 1998;108:1435–1441. doi: 10.1097/00005537-199810000-00003. [DOI] [PubMed] [Google Scholar]
- 35.Persaud R, Garas G, Silva S, Stamatoglou C, Chatrath P, Patel K. An evidence-based review of botulinum toxin (Botox) applications in non-cosmetic head and neck conditions. JRSM Short Rep. 2013;4 doi: 10.1177/2042533312472115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Troung DD, Rontal M, Rolnick M, Aronson AE, Mistura K. Double-blind controlled study of botulinum toxin in adductor spasmodic dysphonia. Laryngoscope. 1991;101:630–634. doi: 10.1288/00005537-199106000-00010. [DOI] [PubMed] [Google Scholar]
- 37.Kenn K, Hess MM. Vocal cord dysfunction: an important differential diagnosis of bronchial asthma. Dtsch Arztebl Int. 2008;105:699–704. doi: 10.3238/arztebl.2008.0699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Reiter R, Rommel D, Brosch S. Long term outcome of psychogenic voice disorders. Auris Nasus Larynx. 2013;40:470–475. doi: 10.1016/j.anl.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 39.Butcher P. Psychological processes in psychogenic voice disorder. Eur J Disord Commun. 1995;30:467–474. doi: 10.3109/13682829509087245. [DOI] [PubMed] [Google Scholar]
- 40.Baker J. Psychogenic voice disorders—heroes or hysterics? A brief overview with questions and discussion. Logoped Phoniatr Vocol. 2002;27:84–89. doi: 10.1080/140154302760409310. [DOI] [PubMed] [Google Scholar]
- e1.Roy N, Merrill RM, Gray SD, Smith EM. Voice disorders in the general population: prevalence, risk factors, and occupational impact. Laryngoscope. 2005;115:1988–1995. doi: 10.1097/01.mlg.0000179174.32345.41. [DOI] [PubMed] [Google Scholar]
- e2.American Academy of Pediatrics Steering Committee on Quality Improvement and Management Classifying recommendations for clinical practice guidelines. Pediatrics. 2004;114:874–877. doi: 10.1542/peds.2004-1260. [DOI] [PubMed] [Google Scholar]
- e3.Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin. DEGAM-Leitlinie Nr. 15 Brustschmerz. www.degam.de/files/Inhalte/Leitlinien-Inhalte/Dokumente/DEGAM-S3-Leitlinien/LL-15_Brustschmerz_Evidenzbericht.final.pdf. (last accessed on 23 February 2015)
- e4.Chang JI, Bevans SE, Schwartz SR. Otolaryngology clinic of North America: evidence-based practice: management of hoarseness/dysphonia. Otolaryngol Clin North Am. 2012;45:1109–1126. doi: 10.1016/j.otc.2012.06.012. [DOI] [PubMed] [Google Scholar]
- e5.Van Houtte E, Van Lierde K, D’Haeseleer E, Claeys S. The prevalence of laryngeal pathology in a treatment-seeking population with dysphonia. Laryngoscope. 2010;120:306–312. doi: 10.1002/lary.20696. [DOI] [PubMed] [Google Scholar]
- e6.Syed I, Daniels E, Bleach NR. Hoarse voice in adults: an evidence-based approach to the 12 minute consultation. Clin Otolaryngol. 2009;34:54–58. doi: 10.1111/j.1749-4486.2008.01872.x. [DOI] [PubMed] [Google Scholar]
- e7.Speyer R. Effects of voice therapy: a systematic review. J Voice. 2008;22:565–580. doi: 10.1016/j.jvoice.2006.10.005. [DOI] [PubMed] [Google Scholar]
- e8.Carding PN, Horsley IA, Docherty GJ. A study of the effectiveness of voice therapy in the treatment of 45 patients with nonorganic dysphonia. J Voice. 1999;13:72–104. doi: 10.1016/s0892-1997(99)80063-0. [DOI] [PubMed] [Google Scholar]
- e9.Carding PN, Horsley IA. An evaluation study of voice therapy in non-organic dysphonia. Eur J Disord Commun. 1992;27:137–158. doi: 10.3109/13682829209012036. [DOI] [PubMed] [Google Scholar]
- e10.Roy N, Weinrich B, Gray SD, et al. Voice amplification versus vocal hygiene instruction for teachers with voice disorders: a treatment outcomes study. J Speech Lang Hear Res. 2002;45:625–638. doi: 10.1044/1092-4388(2002/050). [DOI] [PubMed] [Google Scholar]
- e11.Nguyen DD, Kenny DT. Randomized controlled trial of vocal function exercises on muscle tension dysphonia in Vietnamese female teachers. J Otolaryngol Head Neck Surg. 2009;38:261–278. [PubMed] [Google Scholar]
- e12.Rattenbury HJ, Carding PN, Finn P. Evaluating the effectiveness and efficiency of voice therapy using transnasal flexible laryngoscopy: a randomized controlled trial. J Voice. 2004;18:522–533. doi: 10.1016/j.jvoice.2004.01.003. [DOI] [PubMed] [Google Scholar]
- e13.Gillivan-Murphy P, Drinnan MJ, O’Dwyer TP, Ridha H, Carding P. The effectiveness of a voice treatment approach for teachers with self-reported voice problems. J Voice. 2006;20:423–431. doi: 10.1016/j.jvoice.2005.08.002. [DOI] [PubMed] [Google Scholar]
- e14.MacKenzie K, Millar A, Wilson JA, Sellars C, Deary IJ. Is voice therapy an effective treatment for dysphonia? A randomised controlled trial. BMJ. 2001;323:658–661. doi: 10.1136/bmj.323.7314.658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e15.Simberg S, Sala E, Tuomainen J, Sellman J, Rönnemaa AM. The effectiveness of group therapy for students with mild voice disorders: a controlled clinical trial. J Voice. 2006;20:97–109. doi: 10.1016/j.jvoice.2005.01.002. [DOI] [PubMed] [Google Scholar]
- e16.Ruotsalainen JH, Sellman J, Lehto L, Jauhiainen M, Verbeek JH. Interventions for treating functional dysphonia in adults. Cochrane Database Syst Rev. 2007;3 doi: 10.1002/14651858.CD006373.pub2. CD006373. [DOI] [PubMed] [Google Scholar]
- e17.Ruotsalainen J, Sellman J, Lehto L, Verbeek J. Systematic review of the treatment of functional dysphonia and prevention of voice disorders. Otolaryngol Head Neck Surg. 2008;138:557–565. doi: 10.1016/j.otohns.2008.01.014. [DOI] [PubMed] [Google Scholar]
- e18.Johns MM. Update on the etiology, diagnosis, and treatment of vocal fold nodules, polyps, and cysts. Curr Opin Otolaryngol Head Neck Surg. 2003;11:456–461. doi: 10.1097/00020840-200312000-00009. [DOI] [PubMed] [Google Scholar]
- e19.Kunduk M, McWhorter AJ. True vocal fold nodules: the role of differential diagnosis. Curr Opin Otolaryngol Head Neck Surg. 2009;17:449–452. doi: 10.1097/MOO.0b013e3283328b6d. [DOI] [PubMed] [Google Scholar]
- e20.Sulica L, Behrman A. Management of benign vocal fold lesions: a survey of current opinion and practice. Ann Otol Rhinol Laryngol. 2003;112:827–833. doi: 10.1177/000348940311201001. [DOI] [PubMed] [Google Scholar]
- e21.McCrory E. Voice therapy outcomes in vocal fold nodules: a retrospective audit. Int J Lang Commun Disord. 2001;36:19–24. doi: 10.3109/13682820109177852. [DOI] [PubMed] [Google Scholar]
- e22.Wendler J, Seidner W, Nawka T. Phonochirurgische Erfahrungen aus der Phoniatrie. Sprache Stimme Gehör. 1974;18 [Google Scholar]
- e23.De Bodt MS, Ketelslagers K, Peeters T, et al. Evolution of vocal fold nodules from childhood to adolescence. J Voice. 2007;21:151–156. doi: 10.1016/j.jvoice.2005.11.006. [DOI] [PubMed] [Google Scholar]
- e24.Altman KW. Vocal fold masses. Otolaryngol Clin North Am. 2007;40:1091–1108. doi: 10.1016/j.otc.2007.05.011. [DOI] [PubMed] [Google Scholar]
- e25.Schalén L, Christensen P, Eliasson I, Fex S, Kamme C, Schalén C. Inefficacy of penicillin V in acute laryngitis in adults. Evaluation from results of double-blind study. Ann Otol Rhinol Laryngol. 1985;94:14–17. doi: 10.1177/000348948509400103. [DOI] [PubMed] [Google Scholar]
- e26.Schalén L, Eliasson I, Kamme C, Schalén C. Erythromycin in acute laryngitis in adults. Ann Otol Rhinol Laryngol. 1993;102:209–214. doi: 10.1177/000348949310200308. [DOI] [PubMed] [Google Scholar]
- e27.Stein DJ, Noordzij JP. Incidence of chronic laryngitis. Ann Otol Rhinol Laryngol. 2013;122:771–774. doi: 10.1177/000348941312201207. [DOI] [PubMed] [Google Scholar]
- e28.Weller MD, Nankivell PC, McConkey C, Paleri V, Mehanna HM. The risk and interval to malignancy of patients with laryngeal dysplasia; a systematic review of case series and meta-analysis. Clin Otolaryngol. 2010;35:364–372. doi: 10.1111/j.1749-4486.2010.02181.x. [DOI] [PubMed] [Google Scholar]
- e29.Montgomery J, White A. A decade of laryngeal dysplasia in Paisley, Scotland. Eur Arch Otorhinolaryngol. 2012;269:947–951. doi: 10.1007/s00405-011-1684-x. [DOI] [PubMed] [Google Scholar]
- e30.Zhukhovitskaya A, Battaglia D, Khosla SM, Murry T, Sulica L. Gender and age in benign vocal fold lesions. Laryngoscope. 2015;125:191–196. doi: 10.1002/lary.24911. [DOI] [PubMed] [Google Scholar]
- e31.Remacle M, Friedrich G, Dikkers FG, de Jong F. Phonosurgery of the vocal folds: a classification proposal. Eur Arch Otorhinolaryngol. 2003;260:1–6. doi: 10.1007/s00405-002-0507-5. [DOI] [PubMed] [Google Scholar]
- e32.Lim S, Sau P, Cooper L, McPhaden A, Mackenzie K. The incidence of premalignant and malignant disease in Reinke’s edema. Otolaryngol Head Neck Surg. 2014;150:434–436. doi: 10.1177/0194599813520123. [DOI] [PubMed] [Google Scholar]
- e33.Mau T. Diagnostic evaluation and management of hoarseness. Med Clin North Am. 2010;94:945–960. doi: 10.1016/j.mcna.2010.05.010. [DOI] [PubMed] [Google Scholar]
- e34.Davids T, Muller S, Wise JC, Johns MM, 3rd, Klein A. Laryngeal papillomatosis associated dysplasia in the adult population: An update on prevalence and HPV subtyping. Ann Otol Rhinol Laryngol. 2014;123:402–408. doi: 10.1177/0003489414526848. [DOI] [PubMed] [Google Scholar]
- e35.Dedo HH, Yu KC. CO(2) laser treatment in 244 patients with respiratory papillomas. Laryngoscope. 2001;111:1639–1644. doi: 10.1097/00005537-200109000-00028. [DOI] [PubMed] [Google Scholar]
- e36.Klozar J, Taudy M, Betka J, Kana R. Laryngeal papilloma-precancerous condition? Acta Otolaryngol Suppl. 1997;527:100–102. [PubMed] [Google Scholar]
- e37.Morshed K, Polz-Dacewicz M, Szymanski M, Polz D. Short-fragment PCR assay for highly sensitive broad-spectrum detection of human papillomaviruses in laryngeal squamous cell carcinoma and normal mucosa: clinico-pathological evaluation. Eur Arch Otorhinolaryngol. 2008;265:89–96. doi: 10.1007/s00405-007-0569-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e38.GILEAD>Sciences GmbH. Rote-Hand-Brief vom 27.2.2013 zu Vistide® (Cidofovir) www.akdae.de/Arzneimittelsicherheit/RHB/Archiv/2013/20130227.pdf. (last accessed on 16 March 2015)
- e39.Robert Koch-Institut, Zentrum für Krebsregisterdaten. Krebs in Deutschland. www.rki.de/DE/Content/Gesundheitsmonitoring/Gesundheitsberichterstattung/GBEDownloadsB/KID2012.pdf;jsessionid=1709CED381A128835BB9288911737070.2_cid372?__blob=publicationFile. (last accessed on March 2015)
- e40.Hobbs CG, Sterne JA, Bailey M, Heyderman RS, Birchall MA, Thomas SJ. Human papillomavirus and head and neck cancer: a systematic review and meta-analysis. Clin Otolaryngol. 2006;31:259–266. doi: 10.1111/j.1749-4486.2006.01246.x. [DOI] [PubMed] [Google Scholar]
- e41.Feng Y, Wang B, Wen S. Laser surgery versus radiotherapy for T1-T2N0 glottic cancer: a meta-analysis. ORL J Otorhinolaryngol Relat Spec. 2011;73:336–342. doi: 10.1159/000327097. [DOI] [PubMed] [Google Scholar]
- e42.van Gogh CD, Verdonck-de Leeuw IM, Boon-Kamma BA, Rinkel RN, de Bruin MD, Langendijk JA, et al. The efficacy of voice therapy in patients after treatment for early glottic carcinoma. Cancer. 2006;106:95–105. doi: 10.1002/cncr.21578. [DOI] [PubMed] [Google Scholar]
- e43.Bradley JP, Hapner E, Johns MM., 3rd What is the optimal treatment for presbyphonia? Laryngoscope. 2014;124:2439–2440. doi: 10.1002/lary.24642. [DOI] [PubMed] [Google Scholar]
- e44.Gregory ND, Chandran S, Lurie D, Sataloff RT. Voice disorders in the elderly. J Voice. 2012;26:254–258. doi: 10.1016/j.jvoice.2010.10.024. [DOI] [PubMed] [Google Scholar]
- e45.Schreiber S, Garten D, Sudhoff H. Pathophysiological mechanisms of extraesophageal reflux in otolaryngeal disorders. Eur Arch Otorhinolaryngol. 2009;266:17–24. doi: 10.1007/s00405-008-0770-1. [DOI] [PubMed] [Google Scholar]
- e46.Hom C, Vaezi MF. Extraesophageal manifestations of gastroesophageal reflux disease. Gastroenterol Clin North Am. 2013;42:71–91. doi: 10.1016/j.gtc.2012.11.004. [DOI] [PubMed] [Google Scholar]
- e47.Koop H, Fuchs KH, Labenz J, Lynen Jansen P, Messmann H, Miehlke S, et al. S2k-Leitlinie 021/013 Gastroösophageale Refluxkrankheit. www.awmf.org/uploads/tx_szleitlinien/021-013l_S2k_Refluxkrankheit_2014-05.pdf. doi: 10.1055/s-0034-1385202. (last accessed on 21 February 2015) [DOI] [PubMed] [Google Scholar]
- e48.Rafii B, Taliercio S, Achlatis S, Ruiz R, Amin MR, Branski RC. Incidence of underlying laryngeal pathology in patients initially diagnosed with laryngopharyngeal reflux. Laryngoscope. 2014;124:1420–1424. doi: 10.1002/lary.24483. [DOI] [PubMed] [Google Scholar]
- e49.Schröck A, Göke F, Jakob M, et al. Initial diagnosis of head and neck tuberculosis. Laryngo Rhino Otol. 2011;90:604–608. doi: 10.1055/s-0031-1283140. [DOI] [PubMed] [Google Scholar]
- e50.Abdel-Aziz M, Azab NA, Bassyouni IH, Hamdy G. Laryngeal involvement in juvenile idiopathic arthritis patients. Clin Rheumato. 2011;30:1251–1256. doi: 10.1007/s10067-011-1781-7. [DOI] [PubMed] [Google Scholar]
- e51.Hilgert E, Toleti B, Kruger K, Nejedlo I. Hoarseness due to bamboo nodes in patients with autoimmune diseases: a review of literature. J Voice. 2008;22:343–350. doi: 10.1016/j.jvoice.2006.10.009. [DOI] [PubMed] [Google Scholar]
- e52.Wittekindt C, Lüers JC, Drebber U, Guntinas-Lichius O, Hüttenbrink KB. ANCA-negative subglottic laryngeal stenosis in childhood. HNO. 2007;55:807–811. doi: 10.1007/s00106-006-1457-9. [DOI] [PubMed] [Google Scholar]
- e53.Reiter R, Brosch S, Rottscholl R, Smith E. Dysphonia as a symptom of an amyloidosis. Laryngorhinootologie. 2013;92:541–542. doi: 10.1055/s-0033-1343484. [DOI] [PubMed] [Google Scholar]
- e54.Gallivan GJ, Gallivan HK. Laryngeal amyloidosis causing hoarseness and airway obstruction. J Voice. 2010;24:235–239. doi: 10.1016/j.jvoice.2008.07.006. [DOI] [PubMed] [Google Scholar]
- e55.Markou K, Goudakos J, Constantinidis J, Kostopoulos I, Vital V, Nikolaou A. Primary laryngeal lymphoma: report of 3 cases and review of the literature. Head Neck. 2010;32:541–549. doi: 10.1002/hed.21104. [DOI] [PubMed] [Google Scholar]
- e56.Smith E, Rottscholl R, Brosch S, Reiter R. Malignant lymphoma in the larynx. Laryngorhinootologie. 2013;92:381–388. doi: 10.1055/s-0033-1341465. [DOI] [PubMed] [Google Scholar]
- e57.Loughran S, Alves C, MacGregor FB. Current aetiology of unilateral vocal fold paralysis in a teaching hospital in the West of Scotland. J Laryngol Otol. 2002;116:907–910. doi: 10.1258/00222150260369426. [DOI] [PubMed] [Google Scholar]
- e58.Sielska-Badurek E, Domeracka-Kołodziej A, Zawadzka R, Debowska-Jarzebska E. Vocal fold paralysis in the Medical University of Warsaw’s Ambulatory of Phoniatry in years 2000-2011. Otolaryngol Pol. 2012;66:313–317. doi: 10.1016/j.otpol.2012.06.025. [DOI] [PubMed] [Google Scholar]
- e59.Dilisio RP, Mazzeffi MA, Bodian CA, Fischer GW. Vocal cord paralysis after aortic surgery. J Cardiothorac Vasc Anesth. 2013;27:522–527. doi: 10.1053/j.jvca.2012.09.011. [DOI] [PubMed] [Google Scholar]
- e60.Heman-Ackah YD, Joglekar SS, Caroline M, Becker C, Kim EJ, Gupta R, et al. The prevalence of undiagnosed thyroid disease in patients with symptomatic vocal fold paresis. J Voice. 2011;25:496–500. doi: 10.1016/j.jvoice.2010.03.008. [DOI] [PubMed] [Google Scholar]
- e61.Kang BC, Roh JL, Lee JH, et al. Usefulness of computed tomography in the etiologic evaluation of adult unilateral vocal fold paralysis. World J Surg. 2013;37:1236–1240. doi: 10.1007/s00268-013-1991-z. [DOI] [PubMed] [Google Scholar]
- e62.Dworkin JP, Treadway C. Idiopathic vocal fold paralysis: clinical course and outcomes. J Neurol Sci. 2009;284:56–62. doi: 10.1016/j.jns.2009.04.004. [DOI] [PubMed] [Google Scholar]
- e63.Urquhart AC, St Louis EK. Idiopathic vocal cord palsies and associated neurological conditions. Arch Otolaryngol Head Neck Surg. 2005;131:1086–1089. doi: 10.1001/archotol.131.12.1086. [DOI] [PubMed] [Google Scholar]
- e64.Yamada M, Hirano M, Ohkubo H. Recurrent laryngeal nerve paraysis A 10-year review of 564 patients. Auris Nasus Larynx. 1983;10:1–15. doi: 10.1016/s0385-8146(83)80001-7. [DOI] [PubMed] [Google Scholar]
- e65.Tsikoudas A, Paleri V, El-Badawey MR, Zammit-Maempel I. Recommendations on follow-up strategies for idiopathic vocal fold paralysis: evidence-based review. J Laryngol Otol. 2012;126:570–573. doi: 10.1017/S0022215112000576. [DOI] [PubMed] [Google Scholar]
- e66.Hertegård S, Hallén L, Laurent C, Lindström E, Olofsson K, Testad P, et al. Cross-linked hyaluronan used as augmentation substance for treatment of glottal insufficiency: safety aspects and vocal fold function. Laryngoscope. 2002;112:2211–2219. doi: 10.1097/00005537-200212000-00016. [DOI] [PubMed] [Google Scholar]
- e67.Song PC, Sung CK, Franco, RA Voice outcomes after endoscopic injection laryngoplasty with hyaluronic acid stabilized gel. Laryngoscope. 2010;120 doi: 10.1002/lary.21666. [DOI] [PubMed] [Google Scholar]
- e68.Carroll TL, Rosen CA. Long-term results of calcium hydroxylapatite for vocal fold augmentation. Laryngoscope. 2011;121:313–319. doi: 10.1002/lary.21258. [DOI] [PubMed] [Google Scholar]
- e69.Shen T, Damrose EJ, Morzaria S. A meta-analysis of voice outcome comparingcalcium hydroxylapatite injection laryngoplasty to silicone thyroplasty. Otolaryngol Head Neck Surg. 2013;148:197–208. doi: 10.1177/0194599812464193. [DOI] [PubMed] [Google Scholar]
- e70.Rosen CA, Gartner-Schmidt J, Casiano R, Anderson TD, Johnson F, Remacle M, et al. Vocal fold augmentation with calcium hydroxylapatite: twelve-month report. Laryngoscope. 2009;119:1033–1041. doi: 10.1002/lary.20126. [DOI] [PubMed] [Google Scholar]
- e71.Hartl DM, Hans S, Crevier-Buchman L, Vaissière J, Brasnu DF. Long-term acoustic comparison of thyroplasty versus autologous fat injection. Ann Otol Rhinol Laryngol. 2009;118:827–832. doi: 10.1177/000348940911801201. [DOI] [PubMed] [Google Scholar]
- e72.Isshiki N, Morita H, Okamura H, Hiramoto M. Thyroplasty as a new phonosurgical technique. Acta Otolaryngol. 1974;78:451–457. doi: 10.3109/00016487409126379. [DOI] [PubMed] [Google Scholar]
- e73.Ludlow CL. Treatment for spasmodic dysphonia: limitations of current approaches. Curr Opin Otolaryngol Head Neck Surg. 2009;17:160–165. doi: 10.1097/MOO.0b013e32832aef6f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e74.Watts CR, Truong DD, Nye C. Evidence for the effectiveness of botulinum toxin for spasmodic dysphonia from high-quality research designs. J Neural Transm. 2008;115:625–630. doi: 10.1007/s00702-007-0757-x. [DOI] [PubMed] [Google Scholar]
- e75.Morris MJ, Christopher KL. Diagnostic criteria for the classification of vocal cord dysfunction. Chest. 2010;138:1213–1223. doi: 10.1378/chest.09-2944. [DOI] [PubMed] [Google Scholar]
- e76.Kenn K. [Vocal Cord Dysfunction-what do we really know? A review.] Pneumologie. 2007;61:431–439. doi: 10.1055/s-2007-959199. [DOI] [PubMed] [Google Scholar]
- e77.Newman KB, Mason UG, 3rd, Schmaling KB. Clinical features of vocal cord dysfunction. Am J Respir Crit Care Med. 1995;152:1382–1386. doi: 10.1164/ajrccm.152.4.7551399. [DOI] [PubMed] [Google Scholar]
- e78.Kenn K, Balkissoon R. Vocal cord dysfunction: what do we know? Eur Respir J. 2011;371:94–200. doi: 10.1183/09031936.00192809. [DOI] [PubMed] [Google Scholar]
- e79.Guglani L, Atkinson S, Hosanagar A, Guglani L. A systematic review of psychological interventions for adult and pediatric patients with vocal cord dysfunction. Front Pediatr. 2014;2 doi: 10.3389/fped.2014.00082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e80.Bader CA, Schick B. Psychogenic aphonia. A challenging diagnosis? HNO. 2013;61:678–682. doi: 10.1007/s00106-013-2726-z. [DOI] [PubMed] [Google Scholar]
- e81.Kollbrunner J, Menet AD, Seifert E. Psychogenic aphonia: no fixation even after a lengthy period of aphonia. Swiss Med Wkly. 2010;9:12–17. doi: 10.4414/smw.2010.12776. [DOI] [PubMed] [Google Scholar]
- e82.Leonard R, Kendall K. Differentiation of spasmodic and psychogenic dysphonias with phonoscopic evaluation. Laryngoscope. 1999;109:295–300. doi: 10.1097/00005537-199902000-00022. [DOI] [PubMed] [Google Scholar]