Abstract
We evaluated the performance of a point-of-contact circulating cathodic antigen assay (POC-CCA) to detect schistosome infections in primary school children (N = 1,801) living in areas with low, moderate, and high Schistosoma mansoni prevalence in western Kenya. The commercially available assay (CCA-1) and a second, experimental formulation (CCA-2) were compared against Kato-Katz stool examinations and an anti-schistosome enzyme-linked immunosorbent assay (ELISA). A latent class model based on the four tests was used to establish “true infection status” in three different zones based on their distance from Lake Victoria. As a screening tool for community treatment according to World Health Organization (WHO) guidelines, the Kato-Katz examination was in closest agreement with the latent class model, followed by the experimental CCA-2, soluble adult worm antigen preparation (SWAP) ELISA, and CCA-1, which had high sensitivity compared with the other tests but was consistently the least specific. Our experience suggests that POC-CCA tests offer a field-friendly alternative to Kato-Katz, but need further interpretation for appropriate field use.
Introduction
Recent initiatives to scale-up schistosomiasis control programs have highlighted the critical need for more effective diagnostic tools.1,2 Accurate detection of infection is essential not only for the quantification of disease burden, but also for effective design, evaluation, and coordination of control programs. The efficiencies gained from focused drug administration, drug efficacy measurements, pharmacovigilance, impact monitoring, and integration with other infection control programs are all contingent upon correct prevalence assessments.1–4 The Kato-Katz stool examination is the most widely used technique for detecting intestinal schistosome infections due to its relatively simple technology and low material cost.5 However, the cost of labor is high as the process is time consuming and must be performed by trained microscopists, who in addition may be exposed to infectious agents when handling fresh stools.6 Sensitive egg detection is largely dependent on the skill of the technician. Moreover, results are subject to intraspecimen variations in egg distribution and daily fluctuations in egg excretion.2,3,7–9
Antibody detection techniques such as enzyme-linked immunosorbent assay (ELISA) offer improved sensitivity over direct microscopic techniques but they require well-equipped laboratories and highly trained technicians.6 In addition, antibody levels vary across individuals, do not always correspond with worm burden, and typically persist in the bloodstream for years after an infection has cleared.6,10 As a result, current antibody detection methods are generally unable to distinguish between light and heavy infection or current and past infection, severely limiting their utility as operational tools.3,10 Cross-reactivity with other parasitic helminths is also a concern with regard to specificity of these techniques.4
Methods for detecting schistosome antigens in the blood or urine offer the advantage of reflecting active infection and infection intensity. Of particular note, a urine-based circulating cathodic antigen (CCA) rapid test has been developed by Rapid Medical Diagnostics (Pretoria, South Africa) for use at the point of contact (POC) with potentially infected individuals.11 It is the only rapid test for schistosomiasis that is commercially available. We had previously compared this test with egg (Kato-Katz) and antibody (ELISA) detection methods in high Schistosoma mansoni prevalence settings in western Kenya and found that it performed well.6 However, when we used this test in studies in Togo and Suriname, although no study participants were egg positive, up to 50% of the POC-CCA tests yielded a positive result (Mathieu and others and Foo and others, unpublished data). This caused us to question the specificity of the test and desire to perform further testing in endemic areas that also have lower S. mansoni intensity.
The study presented here was conducted as part of a multi-country initiative by the Schistosomiasis Consortium for Operational Research and Evaluation (SCORE) to evaluate the POC-CCA for operational use in areas of low and moderate S. mansoni infection at various sites across sub-Saharan Africa.12–17 Two versions of the POC-CCA—one commercially available (CCA-1) and one experimental formulation (CCA-2)—were compared against Kato-Katz stool examinations and an anti-schistosome IgG ELISA in communities with different prevalence strata. Latent class analysis (LCA) modeling was used to derive more empirically reliable prevalence, sensitivity, and specificity estimates than those obtained through the use of an imperfect gold standard, such as the Kato-Katz examination.18–20 The day-to-day reproducibility of CCA-1 as well as its ability to detect an effect of treatment with praziquantel (PZQ) were also evaluated. Finally, each test method was assessed against LCA for its ability to accurately predict the appropriate community level treatment approach according to World Health Organization (WHO) guidelines.21
Materials and Methods
Ethical considerations.
The study protocol was approved by the Kenya Medical Research Institute (KEMRI) Scientific Steering Committee, Kenyan Ethical Review Committee, and Centers for Disease Control and Prevention (CDC) Institutional Review Board. Written informed consent was given by each participating child's parent or guardian, and assent was obtained from each child in the local language. Because the high prevalence of schistosomiasis in this area warranted mass treatment according to WHO guidelines, all children were offered PZQ (40 mg/kg Prazitel®; Cosmos Pharmaceuticals Ltd., Nairobi, Kenya) by the study nurse.
Study setting and population.
The study was conducted in Asembo, a region belonging to the Rarieda Division of Nyanza province in western Kenya. With an estimated population of 57,000, Asembo covers an area of ∼200 km2 along the northern shore of Lake Victoria's Winam Gulf. Samples were collected from 8 to 12-year-old students at 49 different primary schools. A study performed 10 years earlier in this area demonstrated a mean school prevalence of S. mansoni infection of 16.3% (range 0–80%), with a strong correlation between proximity to Lake Victoria and school prevalence.22 By choosing all public primary schools within a 10-km wide transect that extended ∼12 km from the lake, we anticipated inclusion of schools with varying S. mansoni prevalence depending on their distance from the lake.
Sample collection and testing.
Each participant was asked to provide one stool and one midstream urine sample on each of 3 consecutive days. In addition, one finger-stick sample of blood was collected in a 300-μL serum capillary tube (Microvette® CB300; Sarstedt Inc., Nümbrecht, Germany). To evaluate whether the POC-CCA could be a useful tool for monitoring treatment effects, a second urine sample was collected 7 days after PZQ treatment.
The Kato-Katz technique was used to prepare two slides from each stool sample. Slides were examined by two trained microscopists, and results were recorded in eggs per gram feces (EPG). If at least one slide (out of two) from the first day's stool sample was egg positive, the individual was considered positive by first day Kato-Katz, and if at least one slide from any of three stool samples collected (six slides) was egg positive, the individual was considered positive by multiple Kato-Katz.
POC-CCA assays were performed at each school site according to the manufacturer's instructions (Rapid Medical Diagnostics). Tests were scored as “0” if the result was negative (i.e., the control line developed, but no test line appeared); “1+” if a test line appeared, but its color was less intense than that of the control line; “2+” if the test and control lines were equally intense in color; and “3+” if the test line's color was more intense than the control line's color. The CCA-1 was conducted for all the three urine samples, whereas the CCA-2 assay was conducted only on the first day's sample. Urine collected 7 days after treatment was also evaluated using the CCA-1 test.
Blood samples were centrifuged to collect sera, which were then stored at −20°C until the time of analysis. Microtiter plates (Immulon 2HB, Dynex Technologies, Chantilly, VA) were coated with 100 μL of 0.01 mg/mL soluble adult worm antigen preparation (SWAP) in 0.05 M sodium carbonate buffer, pH 9.6, for at least 4 hours at room temperature or overnight at 4°C. Plates were blocked with 100 μL phosphate buffered saline (PBS) containing 0.3% Tween 20 and 5% nonfat dry milk (blocking buffer) and then incubated for at least 1 hour at room temperature or overnight at 4°C. Next, 100 μL of sera diluted to 1:100 in blocking buffer was loaded into each well. After incubation at room temperature for 1 hour, plates were washed with PBS containing 0.05% Tween 20. Wells were next incubated with horseradish peroxidase–conjugated mouse antihuman IgG1, IgG2, IgG3, and IgG4 (1:2,000 each; Southern Biotechnology Associates, Birmingham, AL) in PBS/0.3% Tween 20 and incubated for another hour at room temperature. After a final washing step, plates were developed with 3,3′,5,5′-Tetramethylbenzidine substrate (Kirkegaard and Perry Laboratories, Gaithersburg, MD) and stopped with 18% sulfuric acid. The developed plates were read at 450 nm on a Molecular Diagnostics VMax microplate reader (Molecular Devices, Sunnyvale, CA) and analyzed using Softmax Pro v5.4 (Molecular Devices).
All serum samples were run in duplicate wells, and each plate included three non-endemic negative controls, a serum-free control, and a standard curve to ensure consistency between plates. The standard curve was prepared by 1:3 serial dilution of a plasma pool of high antibody titer plasma of adult male car washers from the local area. A five-parameter curve fitting model was used to assign anti-SWAP IgG concentration units (CU) to each participant's serum sample. The 1:100 dilution of the positive pool was given a value of 1,000 CU, and 25 CU was established as the positive cutoff value.
Defining prevalence regions.
Handzel and others22 demonstrated an inverse relationship between prevalence and distance from the lake. A piecewise constant model was assumed, and the algorithm of Bai and Perron was used to identify optimal breakpoints in the data (Strucchange R package, R Foundation for Statistical Computing, Vienna, Austria).23 Bayesian information criterion model diagnostics indicated that two breakpoints near 1,200 and 3,800 m best fit the data. Therefore, we defined schools 1,200 m away from the lake and closer as being in Zone A (highest prevalence), schools farther than 1,200 m but no more than 3,800 m away as being in Zone B (moderate prevalence), and schools farther than 3,800 m away as being in Zone C (lowest prevalence).
Statistical analysis.
For each of the zones, the sensitivity and specificity of each test, as well as the prevalence, were estimated using LCA. This method considers results from the four different tests (CCA-1, CCA-2, Kato-Katz, and SWAP-ELISA) as imperfect indicators of an underlying latent class, representing the true infection status of the individuals.24 The multiple stool sample result (requiring at least four Kato-Katz slides) was used over the first day stool sample result for increased sensitivity of Kato-Katz data. Because the POC-CCA assays are designed to measure the same antigen, the LCA model used a random effect to account for conditional dependence between the two CCA tests.
The reliability, or ordinal agreement, of test results across three administrations of the CCA-1 was measured by the intra-class correlation coefficient (ICC).25,26 We also calculated a kappa statistic to evaluate the reliability of the binomial (positive or negative) result for CCA-1. For these tests, scores were interpreted as follows: < 0, poor intra-test agreement; 0–0.20, slight agreement; 0.21–0.40, fair agreement; 0.41–0.60, moderate agreement; 0.61–0.80, substantial agreement; and 0.81–1.0, almost perfect agreement.27 The Wilcoxon signed-rank test was used to assess reduction in band intensity within 1 week of treatment. To assess each method's performance as a screening tool for mass treatment programs, schools were classified in accordance with WHO recommendations, which define communities with ≥ 50% prevalence of infection among school-aged children as high risk, those with ≥ 10% but < 50% prevalence as moderate risk, and those with < 10% as low risk. An LCA agreement score for each test was calculated by taking the number of schools for which the prevalence class identified by the given test matched the LCA classification of the school, divided by the total number of schools.
Results
Prevalence estimates.
A total of 1,801 students (831 male and 970 female with a mean age of 10 years) provided a full set of data, defined as at least one test result for each of the four test types. Three stool samples were obtained for 1,515 (84%) of the 1,801 students. Table 1 shows the estimated prevalence in each zone for the various tests and the LCA model. For CCA-1, data from the first day's sampling were used and predicted the highest prevalence in each of the zones. By contrast, the experimental CCA-2, which was designed to have increased specificity, was more closely aligned with prevalence estimates by stool examination, SWAP ELISA, and the LCA models than with CCA-1. According to the LCA model, among the 49 schools surveyed, 5 schools fell into the WHO high-risk category (> 50% of children infected), 23 into the moderate-risk category (10–50% of children infected), and 21 into the low-risk category (< 10% of children infected). The number of participants from each school ranged from 10 to 76, with a mean of 37.7 participants per school.
Table 1.
Prevalence as measured by each test method at different distances from Lake Victoria
| Diagnostic method | Zone A* (9 schools, N = 327) | Zone B (12 schools, N = 457) | Zone C (28 schools, N = 1,060) |
|---|---|---|---|
| LCA | 44.0 (34.3, 54.5)† (N = 304) | 21.5 (15.5, 28.5) (N = 409) | 9.2 (7.0, 12.1) (N = 989) |
| First day CCA-1 | 70.2 (64.9, 75.1) (N = 322) | 63.3 (58.6, 67.7) (N = 449) | 39.9 (36.9, 43.0) (N = 1,029) |
| CCA-2 | 39.8 (34.5, 45.4) (N = 324) | 26.7 (22.7, 31.1) (N = 449) | 13.5 (11.5, 15.8) (N = 1,029) |
| First day Kato-Katz | 36.8 (31.5, 42.3) (N = 321) | 17.4 (14.0, 21.2) (N = 454) | 7.0 (5.5, 8.8) (N = 988) |
| Multiple Kato-Katz | 52.3 (46.5, 57.9) (N = 310) | 26.0 (21.8, 30.5) (N = 416) | 11.6 (9.7, 13.8) (N = 1,005) |
| SWAP ELISA | 43.9 (38.4, 49.4) (N = 326) | 23.2 (19.4, 27.3) (N = 457) | 16.5 (14.3, 18.9) (N = 1,060) |
CCA = circulating cathodic antigen; LCA = latent class analysis; SWAP ELISA = soluble adult worm antigen preparation enzyme-linked immunosorbent assay.
Zone A includes schools within 1,200 m of the lake; Zone B includes schools located between 1,200 and 3,800 m of the lake; and Zone C includes schools further than 3,800 m from the lake.
Exact 95% confidence interval for all except for LCA, for which a 95% credible interval is reported.
Sensitivity and specificity.
The sensitivities and specificities of each method were estimated using the LCA model (Table 2). The commercially available CCA-1 demonstrated the highest sensitivities for Zones A and B, followed by the multiple stool Kato-Katz method. In Zone C, the Kato-Katz method had the highest sensitivity, followed by the experimental CCA-2 and then the commercial CCA-1. CCA-1 was consistently the least specific test in comparison to the LCA. By contrast, the CCA-2 and the Kato-Katz methods exhibited the highest specificities (> 80%) across all zones. The SWAP ELISA was consistently less sensitive and less specific than the Kato-Katz method, regardless of zone, but showed better specificity than CCA-1 at all prevalence levels.
Table 2.
Sensitivities and specificities of each test by zone
| Zone* | Number of schools | Test method | Sensitivity (95% CI) | Specificity (95% CI) |
|---|---|---|---|---|
| A | 9 (N = 304) | CCA-1 | 90.4 (83.2, 95.9) | 49.1 (41.1, 57.2) |
| CCA-2 | 74.2 (61.5, 86.1) | 86.2 (79.9, 91.6) | ||
| Multiple Kato-Katz | 96.9 (88.9, 99.9) | 83.2 (71.3, 96.1) | ||
| SWAP ELISA | 67.5 (57.1, 78.1) | 73.7 (66.0, 80.7) | ||
| B | 12 (N = 409) | CCA-1 | 95.1 (88.8, 98.6) | 46.6 (40.6, 52.9) |
| CCA-2 | 77.1 (64.1, 88.8) | 85.3 (80.4, 89.9) | ||
| Multiple Kato-Katz | 91.1 (76.1, 99.5) | 91.1 (85.7, 96.1) | ||
| SWAP ELISA | 61.3 (47.7, 76.0) | 87.0 (82.6, 91.0) | ||
| C | 28 (N = 989) | CCA-1 | 78.0 (63.6, 88.2) | 65.1 (61.9, 68.3) |
| CCA-2 | 88.1 (77.6, 94.6) | 92.3 (90.3, 94.1) | ||
| Multiple Kato-Katz | 94.0 (80.8, 99.8) | 96.7 (94.7, 98.9) | ||
| SWAP ELISA | 61.7 (49.2, 74.0) | 87.7 (85.3, 89.9) |
CCA = circulating cathodic antigen; CI = confidence interval; SWAP ELISA = soluble adult worm antigen preparation enzyme-linked immunosorbent assay.
Zone A includes schools within 1,200 m of the lake; Zone B includes schools located between 1,200 and 3,800 m of the lake; and Zone C includes schools further than 3,800 m from the lake.
Consistency of the commercial CCA assay.
Complete test results for the CCA-1 (i.e., from all three urine samples collected on consecutive days) were available for 1,442 individuals. The ICC and kappa statistics of agreement were calculated to estimate the reproducibility among the three samples obtained on consecutive days for each zone (Table 3). The ICC statistics take the level of the responses into account (0, 1+, 2+, or 3+), and the kappa statistics treat the responses as binary (negative or positive). For ICC analysis, CCA-1 showed substantial agreement across multiday testing in zones with higher prevalence (A and B) but only moderate agreement in the lower prevalence zone (C). Binary analysis showed moderate agreement between testing on different days for all three zones.
Table 3.
Consistency of results for CCA-1 over 3 days
CCA = circulating cathodic antigen; ICC = intra class correlation coefficient.
Zone A includes schools within 1,200 m of the lake; Zone B includes schools located between 1,200 and 3,800 m of the lake; and Zone C includes schools further than 3,800 m from the lake.
ICC measures ordinal agreement.
Kappa statistic compares binary agreement.
POC-CCA band intensity and EPG infection intensity.
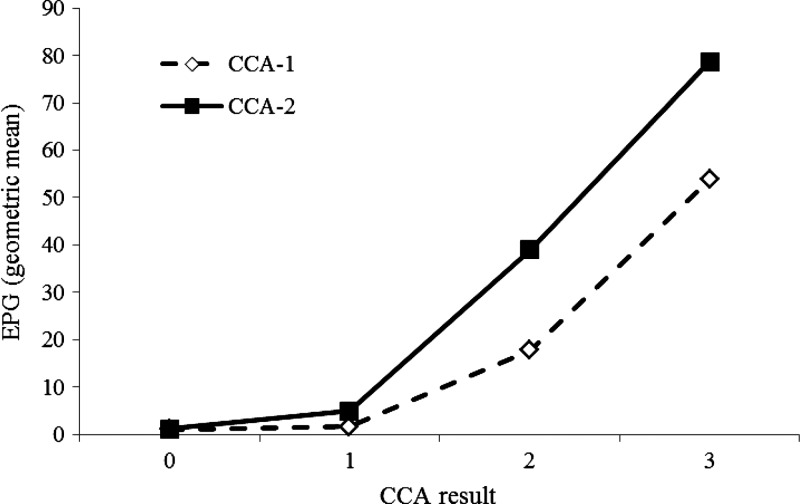
The geometric mean egg count of three stool samples was used as a measure of infection intensity and was calculated for each band intensity level of the POC-CCA test (Figure 1). Data for all three stools (at least one Kato-Katz slide per stool) and the commercial CCA-1 test were available for 1,510 participants, whereas data for three stools and the CCA-2 test were available for 1,501 participants. For both POC-CCA tests, the geometric mean egg count increased with increased band intensity, consistent with results demonstrated by ourselves and others.6,22,28–31
Figure 1.
Intensity of infection as measured by circulating cathodic antigen (CCA) assay and Kato-Katz eggs per gram feces (EPG) from three stool samples. For CCA-1, N = 1,510 and for CCA-2, N = 1,501.
Measuring treatment outcome with the commercial POC-CCA.
To determine whether CCA-1 could be a useful tool for monitoring treatment efficacy, repeat urine samples were requested from participants 7 days after they had received PZQ. A total of 936 participants who were tested at baseline provided a 1-week follow-up urine sample (Table 4). Of the 697 individuals who had a positive CCA-1 response at baseline, 424 (60.8%) demonstrated a reduction in band intensity 1 week after treatment, with 351 (50.4%) of these tests becoming negative. Persons with a 1+ result at baseline were more likely to become negative by 1 week (333/592, 56.3%) than those who had a 2+ CCA-1 result at baseline (18/87, 20.7%). None of the 18 individuals with a 3+ score at baseline became negative, although 14 (77.8%) demonstrated reduced band intensity at 1 week after treatment. Of the 239 individuals who had a negative CCA-1 result at baseline, 59 (24.7%) demonstrated a positive CCA-1 result 1 week after treatment.
Table 4.
Change in CCA-1 band intensity 1 week after treatment
| CCA-1 result | Total N | % Increased (N) | % Stayed same (N) | % Decreased (N) | % Became negative (N) |
|---|---|---|---|---|---|
| 0 | 239 | 24.7 (59) | 75.3 (180) | − | − |
| 1+ | 592 | 1.0 (6) | 42.7 (253) | 56.3 (333) | 56.3 (333) |
| 2+ | 87 | 1.2 (1) | 10.3 (9) | 88.5 (77) | 20.7 (18) |
| 3+ | 18 | − | 22.2 (4) | 77.8 (14) | 0.0 (0) |
CCA = circulating cathodic antigen.
Accuracy of treatment classification.
The real measure of utility for an S. mansoni test is how accurately it indicates the correct prevalence in communities. To evaluate how well the various tests performed in this regard, we used the LCA results to classify each school according to the WHO treatment recommendation categories (i.e., prevalence < 10%, ≥ 10% but < 50%, and ≥ 50%) and determined the percentage of schools in agreement with the LCA for each test (Table 5). Of the five methods considered (CCA-1, CCA-2, first day Kato-Katz, multiple Kato-Katz, and ELISA), the multiple Kato-Katz examination exhibited the greatest agreement, assigning 79.6% of schools to the same treatment group as LCA. The first day Kato-Katz and the CCA-2 assay performed comparably, with agreement scores of 73.5% and 67.3%, respectively, though the first day Kato-Katz method placed relatively more schools in the low-prevalence category and fewer in the high-prevalence category, whereas the experimental CCA assay tended to place more schools in the moderate-prevalence group. The first day CCA-1 assay showed the least agreement (24.5%), identifying more schools as high risk and fewer as low risk than either the LCA or the other methods.
Table 5.
School classification as high, moderate, or low risk for schistosomiasis at different distances from Lake Victoria using WHO cutoffs
| Zone A* (N = 9) | Zone B (N = 12) | Zone C (N = 28) | Agreement† | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| High | Moderate | Low | High | Moderate | Low | High | Moderate | Low | Score (under, same, over) | |
| LCA | 4 | 4 | 1 | 1 | 8 | 3 | 0 | 11 | 17 | 100 (0, 49, 0) |
| CCA-1 | 7 | 2 | 0 | 9 | 3 | 0 | 8 | 19 | 1 | 24.5 (0, 12, 37) |
| CCA-2 | 3 | 6 | 0 | 1 | 11 | 0 | 0 | 18 | 10 | 67.3 (3, 33, 13) |
| First Kato-Katz | 1 | 6 | 2 | 1 | 8 | 3 | 0 | 8 | 20 | 73.5 (10, 36, 3) |
| Multi Kato-Katz | 6 | 3 | 0 | 3 | 8 | 2 | 0 | 14 | 14 | 79.6 (1, 39, 9) |
| ELISA | 2 | 7 | 0 | 0 | 9 | 3 | 0 | 27 | 1 | 55.1 (4, 27, 18) |
CCA = circulating cathodic antigen; ELISA = enzyme-linked immunosorbent assay; LCA = latent class analysis; WHO = World Health Organization.
Zone A includes schools within 1,200 m of the lake, Zone B includes schools located between 1,200 and 3,800 m of the lake, and Zone C includes schools further than 3,800 m from the lake.
In comparison to LCA result.
Discussion
We compared the commercially available POC-CCA antigen detection assay with an experimental version of the test, first day or multiple day stool collection with two Kato-Katz slides per stool, and an adult worm antigen ELISA to detect anti-schistosome antibodies. We chose to use a latent class model as the diagnostic “gold standard” as an alternative to the imperfect Kato-Katz method. In the context of preventive chemotherapy, the multiple stool Kato-Katz showed the most overall agreement with the LCA (Table 5). This is not surprising as the WHO mass treatment recommendations for S. mansoni were developed based on Kato-Katz results. By contrast, the commercially available CCA-1 demonstrated relatively low agreement with LCA as a tool for community treatment decisions under the current guidelines. It placed a higher number of schools into the high-risk category, which could result in overtreatment and wasting of resources. Compared with the first day Kato-Katz stool examination, the CCA-2 was similar in determining the correct treatment categorization for a given school's community. Although the first day Kato-Katz placed too many schools in the low-risk group, which would result in undertreatment of communities, the CCA-2 corrected for this without tending toward overtreatment. These findings suggest that either the performance of the commercial POC-CCA could be improved or new thresholds for its use in drug distribution should be defined, as has been suggested by others.15,28
The prevalence as determined by SWAP ELISA demonstrated good overall agreement with the LCA (Table 1) but was not as sensitive as anticipated (Table 2) and had relatively low agreement with the LCA for treatment decisions (Table 5). These results argue that using a crude antigen may not be a good diagnostic tool and support efforts to identify recombinant, or at least less complex antigen preparations for serodiagnostic tools for schistosomiasis.
Our results mirror closely those of Adriko and others,17 which was also part of the multi-country study in Uganda. They also observed a high proportion of CCA-1 1+ individuals that were egg negative for six Kato-Katz slides. Our studies differ, however, in that they performed two sets of analyses, one considering a barely visible line (trace) as a positive result and one where a trace result was considered as a negative. In our study, we did not distinguish trace from 1+ as we used the manufacturer's guidelines that stated any visible line should be considered positive. Similarly, Adriko and others17 concluded from their results that trace scores should be considered as a positive result.
It is possible that the CCA-1 results in low-prevalence areas that appear to be false positives are actually detecting infections in people that the other methods are missing. In the studies by Coulibaly and others,12 and Tchuem Tchuente and others,13 where up to nine Kato-Katz slides were examined, the specificity of the CCA-1 was much better. Other discrepancies could be related to children sharing stool samples; we did not have any controls in place to guard against this possibility. However, the modest day-to-day agreement between tests in low-prevalence areas in our study and the relatively high proportion of CCA-1-negative individuals who became CCA-1 positive 1 week after treatment suggests to us that some results are false positives. In addition, most individuals who are positive by CCA-1 but negative by Kato-Katz are also negative by stool polymerase chain reaction (PCR), with CCA-1 1+ individuals more like to be PCR negative than those with a 2+ or 3+ CCA-1 result (Ochola and others in preparation). Although it is possible that these results could be explained by variation of CCA levels in the urine of infected individuals, stool sampling limitations in the PCR assays, or the presence of non-fecund or juvenile worms, the very high proportion of CCA-1-positive, egg-negative individuals that were PCR negative (72%)15 suggests that the CCA-1 scored at least some S. mansoni-infection-negative individuals as positives.
We used one POC-CCA reader in our study, whereas other studies in the multi-country evaluation had two readers score each cassette.12,13 Thus, our protocol may have been improved by using more than one interpreter of CCA results. As mentioned above, we also did not make a distinction between 1+ and trace results as was done in some of the other studies.13,14,28,29 Instead, we adhered to the manufacturer's instructions to better simulate how the test may be interpreted in programmatic use. In light of these considerations, the importance of developing training procedures and validation of reader competence for programmatic use is highlighted.
Taken as a whole, the results of this study add to the growing body of literature evaluating the POC-CCA for field use to map S. mansoni infections.13–17,22,29–31 The assay's rapid turnaround and ease of use eliminate the need for multiple sample collections and specialized technicians, although as discussed above, adjustments to the assay's formulation or interpretation in light of WHO guidelines are still needed. For example, our data suggest that although individuals with 2+ and 3+ results would be clearly positive, perhaps only a proportion of the 1+ results should be counted toward the prevalence of infected persons in a given school or village. Despite concerns about the cost of the POC-CAA cassettes in comparison to Kato-Katz supplies, similar to Adriko and others,17 we found that when equipment, labor, and transportation expenses are included, the costs of performing prevalence mapping using POC-CCA are comparable to those for Kato-Katz (Worrell and others32). In addition, bulk production and purchasing of the cassettes, particularly in the context of drug administration programs, have real potential for cost savings.
ACKNOWLEDGMENTS
We thank the field, laboratory, and data teams from the schistosomiasis laboratory at the Centre for Global Health Research/KEMRI, whose hard work and dedication powered this study. We are grateful to the teachers and headmasters of the Asembo primary schools for their assistance and cooperation and to the parents and children for graciously participating in the study. We also acknowledge John Williamson and Björn Södergård for their advice and support.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. This work is published with permission of the Director, Kenya Medical Research Institute.
Footnotes
Financial support: This project was funded by the University of Georgia Research Foundation, Inc, which is funded by the Bill and Melinda Gates Foundation for this SCORE project, the Division of Parasitic Diseases and Malaria/CDC and the United States Agency for International Development (USAID).
Authors' addresses: Karen T. Foo, Anna J. Blackstock, Susan P. Montgomery, and W. Evan Secor, Division of Parasitic Diseases and Malaria, Centers for Disease Control and Prevention, Atlanta, GA, E-mails: karen.t.foo@gmail.com, hyp9@cdc.gov, zqu6@cdc.gov, and was4@cdc.gov. Elizabeth A. Ochola, Daniel O. Matete, Pauline N. M. Mwinzi, and Diana M. S. Karanja, Neglected Tropical Diseases Unit, Center for Global Health Research, Kenya Medical Research Institute (KEMRI), Kisumu, Kenya, E-mails: eakinyi@kemricdc.org, dmatete@kemricdc.org, pmwinzi@kemricdc.org, and dkaranja@kemricdc.org.
References
- 1.Fenwick A, Webster JP, Bosque-Oliva E, Blair L, Fleming FM, Zhang Y, Stothard JR, Gabrielli AF, Clements ACA, Kabatereine NB, Toure S, Dembele R, Nyandindi U, Mwansa J, Koukounari A. The Schistosomiasis Control Initiative (SCI): rationale, development and implementation from 2002–2008. Parasitology. 2009;136:1719–1730. doi: 10.1017/S0031182009990400. [DOI] [PubMed] [Google Scholar]
- 2.Barreto ML, Silva JT, Mott KE, Lehman JS., Jr Stability of faecal egg excretion in Schistosoma mansoni infection. Trans R Soc Trop Med Hyg. 1978;103:347–354. doi: 10.1016/0035-9203(78)90056-1. [DOI] [PubMed] [Google Scholar]
- 3.Utzinger J, N'Goran EK, Caffrey CR, Keiser J. From innovation to application: social-ecological context, diagnostics, drugs and integrated control of schistosomiasis. Acta Trop. 2010;2558:S121–S137. doi: 10.1016/j.actatropica.2010.08.020. [DOI] [PubMed] [Google Scholar]
- 4.Stothard JR. Improving control of African schistosomiasis: towards effective use of rapid diagnostic tests within an appropriate disease surveillance model. Trans R Soc Trop Med Hyg. 2009;103:325–332. doi: 10.1016/j.trstmh.2008.12.012. [DOI] [PubMed] [Google Scholar]
- 5.Katz N, Chaves A, Pellegrino J. A simple device for quantitative stool thick-smear technique in schistosomiasis mansoni. Rev Inst Med Trop Sao Paulo. 1972;14:397–400. [PubMed] [Google Scholar]
- 6.Shane HL, Verani JR, Abudho B, Montgomery SP, Blackstock AJ, Mwinzi PNM, Butler SE, Karanja DMS, Secor WE. Evaluation of urine CCA assays for detection of Schistosoma mansoni infection in western Kenya. PLoS Negl Trop Dis. 2011;5:e951. doi: 10.1371/journal.pntd.0000951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Teesdale CH, Fahringer K, Chitsulo L. Egg count variability and sensitivity of a thin smear technique for the diagnosis of Schistosoma mansoni. Trans R Soc Trop Med Hyg. 1985;79:369–373. doi: 10.1016/0035-9203(85)90384-0. [DOI] [PubMed] [Google Scholar]
- 8.Kongs A, Marks G, Verle P, van der Stuyft P. The unreliability of the Kato-Katz technique limits its usefulness for evaluating S. mansoni infections. Trop Med Int Health. 2001;6:163–169. doi: 10.1046/j.1365-3156.2001.00687.x. [DOI] [PubMed] [Google Scholar]
- 9.Engels D, Sinzinkayo E, Gryseels B. Day-to-day egg count fluctuation in Schistosoma mansoni infection and its operational implications. Am J Trop Med Hyg. 1996;57:571–577. doi: 10.4269/ajtmh.1996.54.319. [DOI] [PubMed] [Google Scholar]
- 10.Doenhoff MJ, Chiodini PL, Hamilton JV. Specific and sensitive diagnosis of schistosome infection: can it be done? Trends Parasitol. 2004;20:35–39. doi: 10.1016/j.pt.2003.10.019. [DOI] [PubMed] [Google Scholar]
- 11.van Dam GJ, Wichers JH, FalcaoFeirreira TM, Ghati D, van Amerongen A, Deelder AM. Diagnosis of schistosomiasis by reagent strip test for detection of circulating cathodic antigen. J Clin Microbiol. 2004;42:5458–5461. doi: 10.1128/JCM.42.12.5458-5461.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coulibaly JT, Knopp S, N'Guessan NA, Silué KD, Fürst T, Lohourignon LK, Brou JK, N'Gbesso YK, Vounatsou P, N'Goran EK, Utzinger J. Accuracy of urine circulating cathodic antigen (CCA) test for Schistosoma mansoni diagnosis in different settings of Côte d'Ivoire. PLoS Negl Trop Dis. 2011;5:e1384. doi: 10.1371/journal.pntd.0001384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tchuem Tchuenté LA, Kueté Fouodo CJ, Kamwa Ngassam RI, Sumo L, DongmoNoumedem C, Kenfack CM, Gipwe NF, Nana ED, Stothard JR, Rollinson D. Evaluation of circulating cathodic antigen (CCA) urine-tests for diagnosis of Schistosoma mansoni infection in Cameroon. PLoS Negl Trop Dis. 2012;6:e1758. doi: 10.1371/journal.pntd.0001758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Navaratnam AM, Mutumba-Nakalembe MJ, Stothard JR, Kabatereine NB, Fenwick A, Sousa-Figueiredo JC. Notes on the use of urine-CCA dipsticks for detection of intestinal schistosomiasis in preschool children. Trans R Soc Trop Med Hyg. 2012;106:619–622. doi: 10.1016/j.trstmh.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 15.Colley DG, Binder S, Campbell C, King CH, Tchuem Tchuenté LA, N'Goran EK, Erko B, Karanja DM, Kabatereine NB, van Lieshout L, Rathbun S. A five-country evaluation of a point-of-care circulating cathodic antigen urine assay for the prevalence of Schistosoma mansoni. Am J Trop Med Hyg. 2013;88:426–432. doi: 10.4269/ajtmh.12-0639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Erko B, Medhin G, Teklehaymanot T, Begarege A, Legesse M. Evaluation of urine-circulating cathodic antigen (Urine-CCA) cassette test for the detection of Schistosoma mansoni infection in areas of moderate prevalence in Ethiopia. Trop Med Int Health. 2013;18:1029–1035. doi: 10.1111/tmi.12117. [DOI] [PubMed] [Google Scholar]
- 17.Adriko M, Standley CJ, Tinkitina B, Tukahebwa EM, Fenwick A, Fleming FM, Sousa-Figueiredo JC, Stothard JR, Kabatereine NB. Evaluation of circulating cathodic antigen (CCA) urine-cassette assay as a survey tool for Schistosoma mansoni in different transmission settings within Bugiri District, Uganda. Acta Trop. 2014;136:50–57. doi: 10.1016/j.actatropica.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 18.Carabin H, Balolong E, Joseph L, McGarvey ST, Johansen MV, Fernandez T, Willingham AL, Olveda R. Estimating sensitivity and specificity of a faecal examination method for Schistosoma japonicum infection in cats, dogs, water buffaloes, pigs, and rats in western Samar and Sorsogon Provinces, the Philippines. Int J Parasitol. 2005;35:1517–1524. doi: 10.1016/j.ijpara.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 19.Koukounari A, Webster JP, Donnelly CA, Bray BC, Naples J, Bosompem K, Shiff C. Sensitivities and specificities of diagnostic tests and infection prevalence of Schistosoma haematobium estimated from data on adults in villages northwest of Accra, Ghana. Am J Trop Med Hyg. 2009;80:435–441. [PMC free article] [PubMed] [Google Scholar]
- 20.Tarafder MR, Carabin H, Joseph L, Balolong E, Jr, Olveda R, McGarvey ST. Estimating the sensitivity and specificity of Kato-Katz stool examination technique for detection of hookworms, Ascaris lumbricoides and Trichuris trichiura infections in humans in the absence of a ‘gold standard.’. Int J Parasitol. 2010;40:399–404. doi: 10.1016/j.ijpara.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization . Preventive Chemotherapy in Human Helminthiasis: Coordinated Use of Anthelminthic Drugs in Control Interventions: A Manual for Health Professionals and Program Managers. Geneva, Switzerland: World Health Organization; 2006. [Google Scholar]
- 22.Handzel T, Karanja DMS, Addiss DG, Hightower AW, Rosen DH, Colley DG, Andove J, Slutsker L, Secor WE. Geographic distribution of schistosomiasis and soil-transmitted helminths in western Kenya: implications for anthelminthic mass treatment. Am J Trop Med Hyg. 2003;69:318–323. [PubMed] [Google Scholar]
- 23.Bai J, Perron P. Computation and analysis of multiple structural change models. J Appl Econ. 2003;18:1–22. [Google Scholar]
- 24.Dendukuri N, Hadgu A, Wang L. Modeling conditional dependence between diagnostic tests: a multiple latent variable model. Stat Med. 2009;28:442–461. doi: 10.1002/sim.3470. [DOI] [PubMed] [Google Scholar]
- 25.Bartko JJ. The intraclass correlation coefficient as a measure of reliability. Psychol Rep. 1966;19:3–11. doi: 10.2466/pr0.1966.19.1.3. [DOI] [PubMed] [Google Scholar]
- 26.Fleiss JL, Levin B, Paik MC. Statistical Methods for Rates and Proportions. 3rd Ed. New York, NY: John Wiley and Sons; 2003. [Google Scholar]
- 27.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 28.Standley CJ, Lwambo NJS, Lange CN, Kariuki HC, Adriko M, Stothard J. Performance of circulating cathodic antigen (CCA) urine-dipsticks for rapid detection of intestinal schistosomiasis in schoolchildren from shoreline communities of Lake Victoria. Parasit Vectors. 2010;3:7. doi: 10.1186/1756-3305-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Standley CJ, Adriko M, Arinaitwe M, Atuhaire A, Kazibwe F, Fenwick A, Kabatereine NB, Stothard JR. Epidemiology and control of intestinal schistosomiasis on the Sesse Islands, Uganda: integrating malacology and parasitology to tailor local treatment recommendations. Parasit Vectors. 2010;3:64. doi: 10.1186/1756-3305-3-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sousa-Figueiredo JC, Betson M, Kabatereine NB, Stothard JR. The urine circulating cathodic antigen (CCA) dipstick: a valid substitute for microscopy for mapping and point-of-care diagnosis of intestinal schistosomiasis. PLoS Negl Trop Dis. 2013;7:e2008. doi: 10.1371/journal.pntd.0002008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Coulibaly JT, N'Gbesso YK, Knopp S, N'Guessan NA, Silué KD, van Dam GJ, N'Goran EK, Utzinger J. Accuracy of urine circulating cathodic antigen test for the diagnosis of Schistosoma mansoni in preschool-aged children before and after treatment. PLoS Negl Trop Dis. 2013;7:e2109. doi: 10.1371/journal.pntd.0002109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Worrell CM, Bartoces M, Karanja DMS, Ochola EA, Matete DO, Mwinzi PNM, Montgomery SP, Secor WE. Cost analysis of tests for the detection of Schistosoma mansoni infection in children in western Kenya. Am J Trop Med Hyg. 2015;92:1233–1239. doi: 10.4269/ajtmh.14-0644. [DOI] [PMC free article] [PubMed] [Google Scholar]