Abstract
Background
Understanding the demographics of patellofemoral pain is important to determine the best practices in diagnosis and treatment of this difficult pathology. The occurrence of patellofemoral pain has been reported from isolated sports medicine clinics and from within the military, but its incidence has never been examined in the general population within the United States.
Purpose
The purpose of this study was to examine the reported occurrence of patellofemoral pain for those individuals seeking medical care and to compare that to all other pathologies that result in anterior knee pain, such as tendinopathies, patella subluxation, osteoarthritis, or meniscal and bursal conditions. Occurrence rates were examined across sex, age and region within a large healthcare provider database that contains over 30 million individuals.
Methods
Data were queried with the PearlDiver Patient Record Database, a national database containing orthopedic patient records. Two common International Classification of Disease, Ninth Revision (ICD‐9) codes for patellofemoral pain (717.7 – Patella Chondromalacia and 719.46 – Pain in joint, lower leg) were utilized and were searched from the years 2007‐2011. The top twenty additional ICD‐9 codes that were concurrently coded with 717.7 and 719.46 were removed from the data. Chi‐squared and Mantel‐Haenszel tests were utilized to identify statistically significant differences in the diagnosis of patellofemoral pain between sex, age, and year.
Results
During this five‐year period, there were 2,188,753 individuals diagnosed with patellofemoral pain. The diagnosis was more common in females compared to males with 1,211,665 and 977,088 cases respectfully (p<0.001). Statistically significant differences between ages was found, with 50‐59 year olds having the most cases with 578,854, p<0.001. And, during the five‐year examination period, there was a steady increase between 2007‐2011, p<0.01.
Conclusion
Patellofemoral pain was diagnosed between 1.5% and 7.3% of all patients seeking medical care within the United States. Females experienced patellofemoral pain more often than males and there was a steady increase of cases in the United States during the 2007‐2011 examination period. The diagnosis of patellofemoral pain increased with age and the 50‐59 year old age group had the most cases.
Level of Evidence
2b
Keywords: Anterior knee pain, chondromalacia, epidemiology
INTRODUCTION
Patellofemoral Pain (PFP) is an overuse condition that increases pain and compressive force on the patellofemoral joint with activity and is generally not linked to trauma or known intra‐articular damage to the knee.1‐6 PFP is also commonly referred to as anterior knee pain or chondromalacia patella, however while these conditions often present with similar symptoms and are exacerbated by similar activities, the subtitle differences in improper interchanging nomenclature creates difficultly in the description of this pathology.7,8 Anterior knee pain is a generic term that can incorporate PFP as well as anterior knee pathologies such as a plica, fat pad fibrosis or bursitis compared to chondromalacia patella which requires softening or damage to the cartilage under the patella.9‐11 PFP is specifically pain to the retro‐ or peri‐patellar area during an array of activities ranging from prolonged sitting, squatting, to jumping and running.12‐17 Those experiencing PFP often have major limitations of daily activities, work, and athletic participation. It has been reported that 74% of individuals experiencing PFP will limit or stop sport participation due to their painful symptoms.18‐20 Emerging evidence suggests that PFP may also contribute to the development of patellofemoral osteoarthritis, which not only creates long‐term implications for these individual's health but also increases healthcare costs.21,22
PFP is often described as one of the most common knee conditions seen by sports medicine providers. Incidence rates have been reported to vary between 8% and 33% of all knee related injuries in small‐scale epidemiological studies.23‐26 It has also been reported that PFP not only occurs within physically active individuals and military personnel, but is also seen throughout the general population.25,27 While PFP is commonly believed to be experienced by adolescent and younger individuals, results of some of the earliest epidemiological studies suggest that PFP is one ofthe most frequently reported pathologies in individuals into their 60's.24,28 Females have been reported to experience PFP two to ten times more often than their male counterparts.25,29
Previous studies provide some insight into the incidence rate of this chronic condition; however, the accuracy of these numbers has been called into question. Ireland et al,30 McConnell et al,31 and Witvrouw et al32 have all referenced incidence rates of PFP within the general population, yet there currently is insufficient data to support these claims.7 These studies only provide data collected within individual sports medicine clinics, military populations and running clinics, which decreases the generalizability of their findings.23‐26,33 Such practices or sites typically provide care to specific populations and therefore there is minimal data on the occurrence of PFP across the lifespan.7,23‐26 It is important to appreciate the incidence of PFP and who may be susceptible to developing the condition in order to provide early interventions. The true understanding of the epidemiology of the pathology and its long‐term consequences will influence appropriate care from healthcare professionals and help develop mechanisms to ultimately improve outcomes.
Since previous research has only provided incidence data from isolated sports medicine centers, single military academies and small epidemiological studies, such research offers limited information and may represent only a narrow population. Therefore, the purpose of this study was to examine current trends in the diagnosis of patellofemoral pain by physicians within the general population by utilizing two International Classification of Disease, Ninth Revision (ICD‐9) codes commonly used to diagnose PFP. The authors hypothesized that the incidence rate of patellofemoral pain would be lower than previously published incidence rates. The current data set included diagnoses from visits to orthopedic physicians while previous researchers examined smaller cohorts of potentially more physically active individuals. Based on previous literature, the authors also hypothesized that females would present with higher incidence rates of PFP compared to males, and that the majority of PFP cases would be seen in the younger active population, particularly in the 10‐19 year old age group.
METHODS
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement recommendations to report the study methods and results was utilized.34 Data were collected with the PearlDiver Patient Record Database (PearlDiver Inc., Fort Wayne IN). The PearlDiver Database is an online database that is commercially available for retrospective reviews of all data submitted to private insurance companies. The largest provider within the database is the UnitedHeath Group (UnitedHealth Group, Minnetonka, MN). Patients who are insured via Medicare, Medicaid or uninsured are not included within the PearlDiver database. The database contains over 1.1 billion patient records on over 30 million individual patients records between 2007 and 2011. The database can be used to identify ICD‐9 codes and Current Procedural Terminology (CPT) codes.
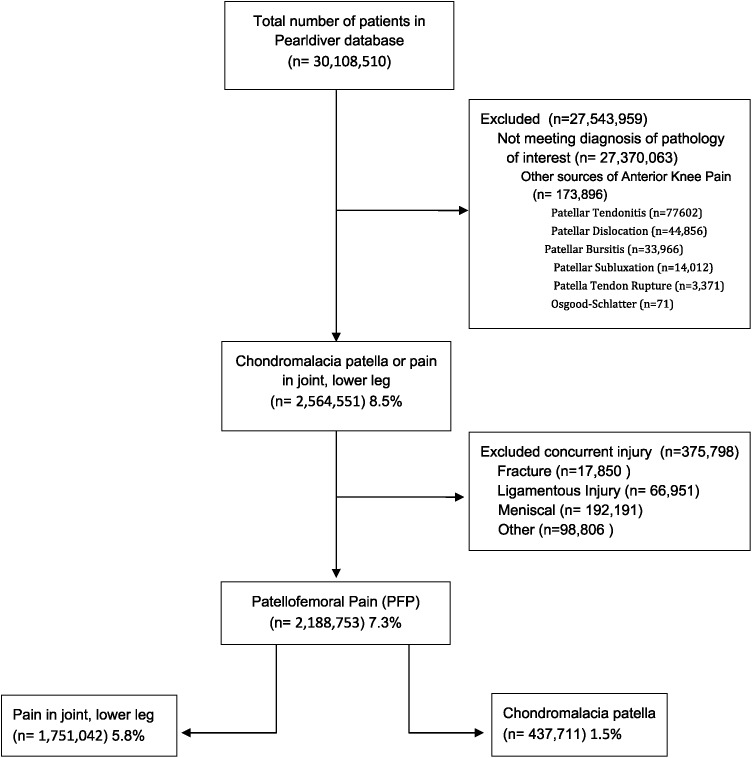
The methodology of the current study is represented as a flow chart and is reported in Figure 1. The database was queried for patients who had been diagnosed with ICD‐9 codes for patellofemoral pain (717.7 – Chondromalacia of patella and 719.46 – Pain in joint, lower leg). These two ICD‐9 codes were selected since previous research identified them as the two most common diagnostic codes for PFP that does not involve structural damage or patellar tendinitis.25 Additionally, other common pathologies that may have been coded in conjunction to the 719.46 were also removed. For example, if a patient also concurrently had diagnoses corresponding to osteoarthritis, knee meniscal tears, cruciate ligament sprains, collateral ligament sprains, tendonitis, bursitis, or fractures to the patella, proximal tibia or proximal fibula, they were removed from the analysis. The authors also searched seven other possible sources of anterior knee pain using nine common ICD‐9 codes and removed those diagnoses from the analysis as well. (Table 1, Figure 1) The decision to removed these pathologies and corresponding ICD‐9 codes were related to the exclusion criteria of these pathologies seen within current PFP literature. 15,35
Figure 1.
Flow Diagram.
Table 1.
ICD‐9 codes for the patellofemoral pain group and anterior knee pain pathologies
| Patellofemoral Pain | Anterior Knee Pain Pathologies |
|---|---|
| 717.7 – Chondromalacia of patella | 718.36 – Patellar Subluxation |
| 719.46‐ Pain in joint, lower leg | 718.96 – Patellar Maltracking |
| 726.64 – Patellar Tendonitis | |
| 726.65 – Patellar Bursitis | |
| 727.66 – Patellar Tendon Rupture | |
| 734.2 Osgood Schlatter | |
| 755.64, 836.3, 836.4 – Patellar Dislocation |
The remaining data were considered to be the PFP group, yet the authors chose to split the diagnoses of chondromalacia patella and pain in the lower leg in order to distinguish the prevalence of each ICD‐9 code. Within those two sub‐diagnoses, the number of total visits to physician's offices by sex (male and female) and age (in ten year increments) were examined. Those data were also evaluated by region within the United States (South, Midwest, West and Northeast) and by year (2007, 2008, 2009, 2010, 2011) within the dataset.
Chi‐square analyses were used to examine differences between stratifications by sex and age groups. A Mantel‐Haenszel test was utilized to evaluate differences in each year that was examined within the dataset. Incidence proportions were calculated by comparing the number of individuals with PFP by the total number of individuals reported in the database. Statistical analyses were conducted using SPSS (Version 20; SPSS Inc., Chicago, IL) with an alpha level set a priori at p≤0.05.
This study was approved by the University of Virginia Institutional Review Board for Human Science Research. The review board granted access to utilize the aggregated data from the database without personal informed consent from the patients included within the study.
RESULTS
Patellofemoral Pain
The PearlDiver database contains a total of 30,108,510 patients with valid ICD‐9 diagnosis or procedure codes during the years of 2007‐2011. During this five‐year period, there were 2,188,753 individuals diagnosed with PFP as defined by using the two selected ICD‐9 codes, or 7.3% of all individuals within the database. There were 437,711 cases of Chondromalacia patella, (20% of the patients with PFP) and 1.5% of all diagnoses of individuals seeking care. There were 1,751,042 cases of joint pain of the lower limb (80% of the patients with PFP) and representing 5.8% of all diagnoses.
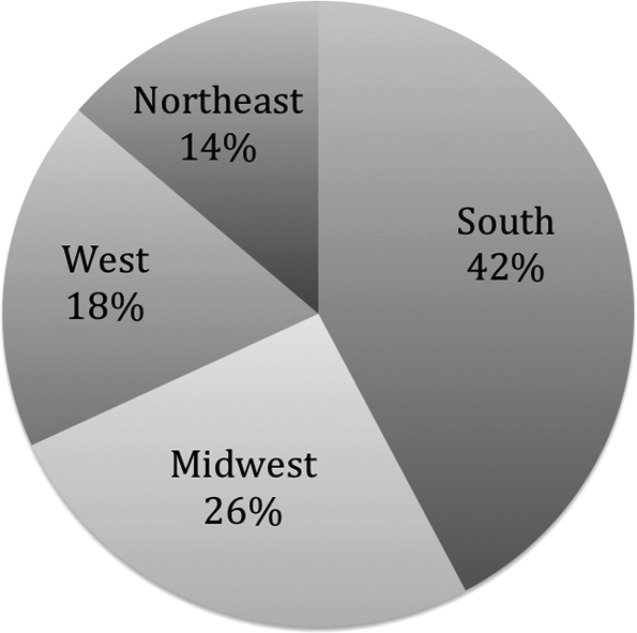
Within the dataset of PFP, those with the diagnosis of joint pain of the lower limb were seen a total of 16,498,162 times while there were 2,803,842 physician visits for chondromalacia. Therefore, individuals with joint pain of the lower limb were seen by medical providers on average of 10.6 times, while those with chondromalacia were seen 6.4 times. When examining the location where medical providers diagnosed these individuals, the top three were medical healthcare office, 64%, outpatient hospital, 23%, and ambulatory surgical center, 3%. When comparing the percentage of PFP cases by region, the South resulted in 925,395 cases, followed by the Midwest region at 565,085, West region at 397,695 and Northeast region at 300,578. (Figure 2)
Figure 2.
PFP breakdown by Region (In Percentages).
The total PFP incidence, and subcategories were compared by sex using Chi Square analyses and revealed that females accounted for 1,211, 665 cases (55%) compared to males who had 977,088 cases (45%) (p<.001). Females accounted for 262,754 cases or 60% of all chondromalacia patella compared to 174,957 cases in males or 40% (p<.001). Joint pain of the lower limb had a similar trend, with females tallying 55% with 948,911 cases compared to males who had 45% with 802,131 cases (p<.001).
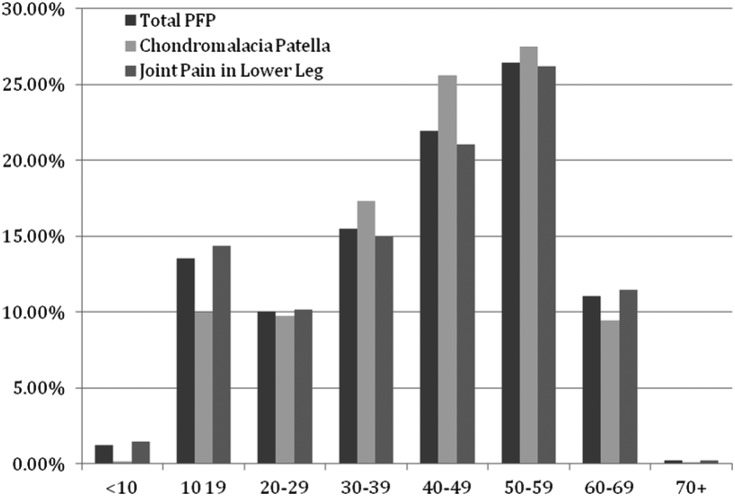
Comparison by age group demonstrated that the occurrence of PFP increased within the age groups and peaked within the 50‐59 year old group. The age groups of 50‐59, 40‐49, and 30‐39 had the greatest incidence, respectively, followed by the 10‐19 year old group. (Figure 3) Chi‐squared testing identified statistically significantly differences between ages for both total and subcategories of PFP cases, p<0.001. Differences between the sexes were examined within the age groups for the combined and subdivision as well. (Table 2) Within most age groups, females reported PFP more often than males.
Figure 3.
Percentage of PFP by Age Group.
Table 2.
Breakdown of Joint Pain in Lower Leg, Chondromalacia and total PFP by age.
| Joint Pain in Lower Leg | Chondromalacia Patella | PFP | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Combined | Male | Female | Combined | Male | Female | Combined | |
| <10 | 17,180 | 8,644 | 25,824 | 341 | 534 | 341 | 17,521 | 9,178 | 26,699 |
| 10‐19 | 127,348 | 124,682 | 252,030 | 14,639 | 29,257 | 14,639 | 141,987 | 153,939 | 295,926 |
| 20‐29 | 93,308 | 84,421 | 177,729 | 17,442 | 25,209 | 17,442 | 110,750 | 109,630 | 220,380 |
| 30‐39 | 133,361 | 129,870 | 263,231 | 33,003 | 42,857 | 33,003 | 166,364 | 172,727 | 339,091 |
| 40‐49 | 168,196 | 200,075 | 368,271 | 47,052 | 65,059 | 47,052 | 215,248 | 265,134 | 480,382 |
| 50‐59 | 181,508 | 276,928 | 458,436 | 45,986 | 74,432 | 45,986 | 227,494 | 351,360 | 578,854 |
| 60‐69 | 78,954 | 122,133 | 201,087 | 16,236 | 25,164 | 16,236 | 95,190 | 147,297 | 242,487 |
| 70+ | 2,276 | 2,158 | 4,434 | 258 | 242 | 258 | 2,534 | 2,400 | 4,934 |
| Total | 802,131 | 948,911 | 1,751,042 | 174,957 | 262,754 | 437,711 | 977,088 | 1,211,665 | 2,188,753 |
Of the total 2,188,753 cases reported between 2007 and 2011, there appeared to be an increase in the condition over this five‐year period. (Table 3) The smallest percentage of those experiencing PFP occurred in 2007 at 18.7% from 410,852 cases, while 2011 had the largest percentage at 22.7% including 496,816 cases. Mantel‐Haenszel test identified a statistically significant difference in the condition over the five‐year period, p<.001.
Table 3.
Number of PFP cases and percentage during 2007‐2011.
| Year | Number of Cases | Percentage of cases |
|---|---|---|
| 2007 | 410,852 | 18.77% |
| 2008 | 423,042 | 19.33% |
| 2009 | 419,073 | 19.15% |
| 2010 | 438,970 | 20.06% |
| 2011 | 496,816 | 22.70% |
| Total | 2,188,753 | 100% |
Additional Sources of Anterior Knee Pain
The incidence of other sources of anterior knee pain totaled 173,896 individuals during this 5‐year period. (Figure 1) Osgood‐Schlatters disease, patellar tendonitis, dislocation, bursitis and subluxations were most common diagnoses. There were 375,798 cases of other pathologies that were diagnosed on the same day the 719.46 ICD‐9 codes and were removed from the analysis.
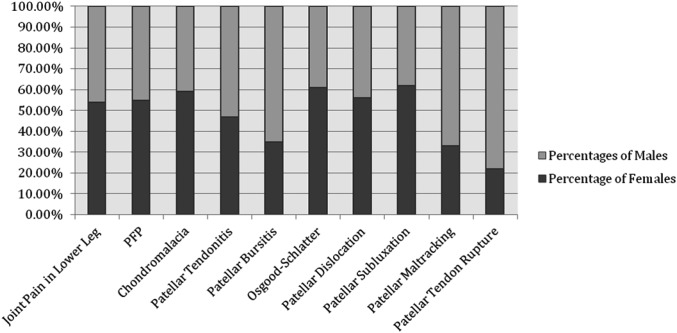
Females were more likely to present with Osgood‐Schlatter, patellar dislocation, and patellar subluxation, with statistically significant differences in both patellar dislocation and subluxation as compared to males (p<0.001) (Figure 4). Statistically significant differences between sexes were also found with males having greater incidence of patellar tendonitis, patellar bursitis, and patellar tendon rupture, (p<0.001). Statistical differences between the seven additional sources of anterior knee pain could not be computed within age groups in order to maintain patient confidentiality, as PearlDiver would not provide exact numbers if fewer than 10 patients existed in a subdivision. This occurred in multiple age group subdivisions in all of the lower incidence pathologies.
Figure 4.
Breakdown of all sources of AKP by Sex
DISCUSSION
The purpose of this study was to examine trends in diagnosis of PFP using two common ICD‐9 codes in the general population based on age, sex, and region for those individuals within the United States seeking orthopedic medical care. Over 30 million cases were used to determine the diagnosis rates. The incidence rate of PFP was approximately 7.3% of all orthopedic visits and that there were differences in age and sex and an increase in the rate of PFP over the five‐year period that was examined. The authors believed that these data are representative of the occurrence of PFP in the general population, compared to the previous studies that only examined sports medicine clinics, military settings or small epidemiological samples.23‐26,36
Whitman et al 37 conducted one of the first studies to provide incidence rates of individuals experiencing patellofemoral pain. They found that PFP accounted for 25% of all knee related injuries within a 4 1/2 year study performed in a single sports medicine clinic.37 This reported rate is similar to other data from other sports medicine clinics during a comparable time period.26 These values do differ slightly from previously collected data examining military personnel, which have been reported to range between 12‐ 15%.25,36 PFP was also identified by Baquie et al as the most common orthopedic conditions treated during a single year in Australia sports medicine clinic.38 While Baquie et al38 did not provide an exact incidence rate, these findings suggest PFP is a common pathology presenting in patients from multiple countries.
PFP has also been studied in multiple sports, with a focus on female participants due to their higher suggested prevalence and incidence rates.25,39 Nejati et al found prevalence rates of between 13 – 26% in females participating in soccer, volleyball, running, fencing and rock climbing.39 This incidence is higher than the current results, which ranged from 1.5 – 7.3% of those seeking orthopedic care. The difference is likely attributed to the wider age group, varied activity levels, the much larger sample size, and where/how the data was collected in the current study. (Table 4)
Table 4.
Previous PFP incidence and prevalence studies.
| Author | Setting | Percentage of PFP Injuries | Number of Participants |
|---|---|---|---|
| Wiltman et al. (1981) | Sports Medicine Clinic | Incidence rate of 25.2% | 1,280 |
| Devereaux and Lachmann (1984) | Sports Medicine Clinic | 25% of knee injuries were patellofemoral arthralgia | 2,519 |
| DeHaven and Linter (1986) | Sports Medicine Clinic | 18.1% of knee injuries to males 33.2% of knee injuries to females | 3,431 |
| Kannus et al. (1987) | Sports Medicine Clinic | 33% of knee injuries | 814 |
| Milgrom et al. (1991) | Military Recruits | 15% of recruits | 390 |
| Baquie and Brunker (1997) | Sports Medicine Clinic | Most common pathology | 2,429 |
| Taunton (2002) | Sports Medicine Clinic | 17% of knee injuries | 2,002 |
| Boling (2010) | Naval Academy | Prevalence of 15% in females and 12% in males | 1,525 |
| Wood (2011) | Database of 8 General Practitioner's | 17% knee injuries | 57,555 |
| Nejati (2011) | Sports Medicine Clinis | Prevalence of 16.74% | 418 |
Females presented with PFP more often than males in the combined PFP data and the isolated ICD‐9 code analysis in the majority of age groups. The largest differences between sex within age groups was the chondromalacia subdivision in the 10‐19 age group, with 66.6% of all cases being females compared to 33.4% in males. Females had significantly higher prevalence of chondromalacia in all age groups except the 70 + group. For joint pain in the lower leg, females presented with significantly more diagnoses in the 40‐69 age groups. When the ICD‐9 codes were combined, there were more females diagnosed within 10‐19 and 30‐69 age groups. These findings support other claims that females present with PFP more than males.25,40 Boling et al reported that females in the United States Naval Academy were 2.23 times more likely to develop PFP than males.25 PFP has also been studied in running clinics and of the 331 cases reported, 62% were by female runners.33 The higher PFP rates in females have also been a reason they are often solely enrolled in studies examining screening methods, muscle function, electromyography, and kinematic alteration during functional tasks.40‐43
Perhaps the most surprising finding of the current research was that the highest percentage of a PFP diagnosis occurred in the 50‐59 year age group and that the 10‐19 year age group was the fourth highest percentage. The frequency of PFP was 13.5% and 10% in the 10‐19 and 20‐29 age groups respectively, while previous research has reported that 70% of all PFP is found in individuals between the ages of 16 and 25.26 Age has also been previously identified as a risk for developing PFP, as those under the age of 34 years were considered at a greater risk than older individuals.33 The current conflicting findings may be due to the previous study only examining athletes in a sports medicine clinic over a 5‐year period. The current methodology of retrospective chart review used data from insurance company reported ICD‐9 codes, so high school and college aged athletes being treated or evaluated in athletic training settings or direct access physical therapy clinics would not be included unless they sought medical attention at a physicians office. Other researchers have reported that females seek medical care more often with traumatic knee pain compared to when they experience insidious knee pain28 The current data indicates that PFP is experienced by a wide age range, which is supported by DeHaven et al who reported that the condition was one of the most commonly treated conditions seen in their sports medicine clinic in patients between the ages of 10 and 60.24
The increased number of older individuals being diagnosed with PFP may actually represent those experiencing patellofemoral osteoarthritis (PFOA) or osteoarthrosis. The recognition of PFOA has increased over past years, and has been recently labeled a subgroup of knee osteoarthritis.22 Isolated PFOA has been studied over the last 20 years, with linear trends in occurrence rates identified between the ages of 50‐70, which is similar to the findings of this study.44 It has been estimated that 25% of all individuals over the age of 50 who experience knee pain have isolated PFOA.45 Wood et al collected PFP disorder rates from a database of 57,555 patients representing eight general practitioner clinics over a single year and found high rates of PFP between 15‐44 year olds and an increased rate in 75 + individuals.46 They also found a gradual increase in PFOA between the ages of 30 and 75+, which is similar to this study's findings and may explain the increase in reported cases in the 50‐59 year old group.46 While there were increased cases reported within the 50‐59 year old age group, it is not possible to truly ascertain which individuals presented with PFP or PFOA. While individuals with concurrent osteoarthritic ICD‐9 codes were removed, the challenge in calculating the occurrence of PFP within this dataset is dependent on proper ICD‐9 coding from the medical healthcare provider. It is also difficult to use the findings gleaned from this dataset without the benefit of a movement based assessment or physical evaluation which are commonly needed to diagnose this condition and to differentiate between PFP and additional pathologies that present with pain to the anterior knee.
Seven additional pathologies were included within the database search in order to provide a picture of all potential anterior knee pain sources. Since there is no true ICD‐9 code for PFP, there are multiple possible diagnoses that medical providers can classify the condition. Due to this limitation, inspecting other possible diagnoses of anterior knee pain can provide insight into what pathologies healthcare providers are commonly evaluating and treating within the population who seek medical care. This information can help clinicians become aware of the frequency of multiple pathologies they commonly treat. If there are high numbers of individuals developing PFP pain severe enough to receive treatment, a specific ICD‐9 code would be vital to provide the accurate diagnosis. As medicine advances to a more evidence based approach, proper evaluation and coding of diagnoses will be vital in providing optimal treatment plans.
It is of interest that diagnoses of patellar maltracking and Osgood‐Schlatter each had fewer than 100 cases over a five‐year period, which is extremely low. The frequency of patella maltracking may actually be underreported as physicians may view it as a mechanism that leads to the pathological process for PFP, but not an actual diagnosis. However, when the incidence of patella maltracking with a concurrent diagnosis of chondromalacia or lower extremity joint pain, there was an increase to 13% of all reported cases, indicating a prevalence of medical care providers that use multiple ICD‐9 codes. While there is empirical evidence PFP and patella maltracking are related, current research does not support the association. 47 The treatments of each may be different as well, supporting the notion that clinicians need accurate diagnoses to provide optimal care. The frequency of patellar tendonitis, the next most common anterior knee pathology, is also very low at .25% of all individuals over the 5‐year period. Rutland et al found that overuse tendon injuries accounted for 7% of all orthopedic physician visits, but they did not provide a specific categorical analysis.48
There are limitations to this retrospective chart review that should be considered; specifically, a lack of a true, stand‐alone ICD‐9 code for PFP. The ICD‐9 codes of 719.46 (general joint pain in the lower leg) and 717.7 (chondromalacia patella) are the two most frequent codes used to classify PFP. 25 Boling et al used these two ICD‐9 codes in previous published PFP epidemiological research in addition to a screening process for concurrent ligamentous and meniscal injuries.22 While this study was modeled for data extraction to also remove these pathologies; there may be the concern for improper or mistaken coding. While advancement and evolution of ICD‐9 codes has occurred culminating in the recent release of ICD‐10 codes, there is still no true PFP code for clinicians to use for the diagnosis of this condition. Differentiating between PFP and patellofemoral osteoarthritis in the older population is also difficult, as it is not possible to identify true PFP versus PFOA. Removal of concurrent osteoarthritis codes was performed, however there is still a chance that improper diagnostic codes were utilized. Another limitation is the distribution of insurance providers who provide data for PearlDiver. UnitedHealthcare is the largest contributor to the PearlDiver system and is primarily utilized within the southern states, which may explain the higher occurrence in that region. These values also only include individuals who have received care through their insurance provider. High school and college aged athletes may receive care from their athletic trainers, patients treated by physical therapists via direct access and military personnel who utilized TriCare insurance were not included in this database which may account for the lower values in the younger population. However, with over 30 million data points, this database represents the largest general population sample that has been evaluated.
CONCLUSION
This study provides evidence that PFP accounts for 1.5 ‐ 7.3% of the diagnoses of those who seek orthopedic care by physicians in the United States. Females experienced PFP more often than males and that PFP is experienced within the general population at high rates in all age groups, with an increase in the ages of 50‐59. Due to the large percentage of individuals who require medical treatment for this condition, risk factors to prospectively identify those susceptible to develop PFP should be examined. Effective interventions should also be studied to decrease the long‐term care needed to minimize the possible progression of PFP into PFOA and decrease health costs associated with this condition.
REFERENCES
- 1.Aminaka N Gribble PA. Patellar taping, patellofemoral pain syndrome, lower extremity kinematics, and dynamic postural control. J Athl Train. 2008;43(1):21‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bolgla LA Boling MC. An update for the conservative management of patellofemoral pain syndrome: A systematic review of the literature from 2000 to 2010. Int J Sports Phys Ther. 2011;6(2):112‐125. [PMC free article] [PubMed] [Google Scholar]
- 3.Crossley K Bennell K Green S McConnell J. A systematic review of physical interventions for patellofemoral pain syndrome. Clin J Sport Med. 2001;11(2):103‐110. [DOI] [PubMed] [Google Scholar]
- 4.Davis IS Powers CM. Patellofemoral pain syndrome: Proximal, distal, and local factors, an international retreat, April 30‐May 2, 2009, Fells Point, Baltimore, MD. J Orthop Sports Phys Ther. 2010;40(3):A1‐16. [DOI] [PubMed] [Google Scholar]
- 5.Duffey MJ Martin DF Cannon DW Craven T Messier SP. Etiologic factors associated with anterior knee pain in distance runners. Med Sci Sports Exerc. 2000;32(11):1825‐1832. [DOI] [PubMed] [Google Scholar]
- 6.Fulkerson JP. Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med. 2002;30(3):447‐456. [DOI] [PubMed] [Google Scholar]
- 7.Callaghan MJ Selfe J. Has the incidence or prevalance of patellofemoral pain in the general population in the united kingdom been properly evaluated? Phys.Ther.Sport. 2007;8:37‐43. [Google Scholar]
- 8.Crossley K Bennell K Green S Cowan S McConnell J. Physical therapy for patellofemoral pain: A randomized, double‐blinded, placebo‐controlled trial. Am J Sports Med. 2002;30(6):857‐865. [DOI] [PubMed] [Google Scholar]
- 9.Thomee R Augustsson J Karlsson J. Patellofemoral pain syndrome. A review of current issues. Sports medicine (Auckland, N.Z.). 1999;28(4):245‐262. [DOI] [PubMed] [Google Scholar]
- 10.Tuna B Semiz‐Oysu A Pekar B Bukte Y Hayirlioglu A. The association of patellofemoral joint morphology with chondromalacia patella: A quantitative MRI analysis. Clinical Imaging. 2014;38(4):495‐498. [DOI] [PubMed] [Google Scholar]
- 11.Rothermich MA Glaviano NR Li J Hart JM. Patellofemoral pain: Epidemiology, pathophysiology, and treatment options. Clin Sports Med. 2015;34(2):313‐327. [DOI] [PubMed] [Google Scholar]
- 12.Willson JD Binder‐Macleod S Davis IS. Lower extremity jumping mechanics of female athletes with and without patellofemoral pain before and after exertion. Am J Sports Med. 2008;36(8):1587‐1596. [DOI] [PubMed] [Google Scholar]
- 13.Willson JD Davis IS. Lower extremity mechanics of females with and without patellofemoral pain across activities with progressively greater task demands. Clin Biomech (Bristol, Avon). 2008;23(2):203‐211. [DOI] [PubMed] [Google Scholar]
- 14.Hewett TE Myer GD Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. Am J Sports Med. 2005;33(4):492‐501. [DOI] [PubMed] [Google Scholar]
- 15.Nakagawa TH Moriya ET Maciel CD Serrao FV. Trunk pelvis, hip, and knee kinematics #hip |strength, and gluteal muscle activation during a single‐leg squat in males and females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2012;42(6):491‐501. [DOI] [PubMed] [Google Scholar]
- 16.Brindle TJ Mattacola C McCrory J. Electromyographic changes in the gluteus medius during stair ascent and descent in subjects with anterior knee pain. Knee Surg Sports Traumatol Arthrosc. 2003;11(4):244‐251. [DOI] [PubMed] [Google Scholar]
- 17.Kernozek TW Torry MR Van Hoof H Cowley H Tanner S. Gender differences in frontal and sagittal plane biomechanics during drop landings. Med Sci Sports Exerc. 2005;37(6):1003‐12; discussion 1013. [PubMed] [Google Scholar]
- 18.Heintjes E Berger M Bierma‐Zeinstra SM. Exercise therapy for patellofemoral pain syndrome. Cochrane Database Syst Rev. 2003;4(CD003472). [DOI] [PubMed] [Google Scholar]
- 19.Fairbank JC Pynsent PB van Poortvliet JA Phillips H. Mechanical factors in the incidence of knee pain in adolescents and young adults. J Bone Joint Surg Br. 1984;66(5):685‐693. [DOI] [PubMed] [Google Scholar]
- 20.Blond L Hansen L. Patellofemoral pain syndrome in athletes: A 5.7‐year retrospective follow‐up study of 250 athletes. Acta Orthop Belg. 1998;64(4):393‐400. [PubMed] [Google Scholar]
- 21.Utting MR Davies G Newman JH. Is anterior knee pain a predisposing factor to patellofemoral osteoarthritis? Knee. 2005;12(5):362‐365. [DOI] [PubMed] [Google Scholar]
- 22.Thomas MJ Wood L Selfe J Peat G. Anterior knee pain in younger adults as a precursor to subsequent patellofemoral osteoarthritis: A systematic review. BMC Musculoskelet Disord. 2010;11:201‐2474‐11‐201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kannus P Aho H Jarvinen M Niittymaki S. Computerized recording of visits to an outpatient sports clinic. Am J Sports Med. 1987;15(1):79‐85. [DOI] [PubMed] [Google Scholar]
- 24.DeHaven KE Lintner DM. Athletic injuries: Comparison by age, sport, and gender. Am J Sports Med. 1986;14(3):218‐224. [DOI] [PubMed] [Google Scholar]
- 25.Boling M Padua D Marshall S Guskiewicz K Pyne S Beutler A. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand J Med Sci Sports. 2010;20(5):725‐730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Devereaux MD LS. Patellofemoral arthralgia in athletes attending a sports injury clinic. Br J Sports Med. 1984;18:18‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Witvrouw E Callaghan MJ Stefanik JJ, et al. Patellofemoral pain: Consensus statement from the 3rd international patellofemoral pain research retreat held in vancouver, september 2013. Br J Sports Med. 2014;48(6):411‐414. [DOI] [PubMed] [Google Scholar]
- 28.Rathleff MS Skuldbol SK Rasch MN Roos EM Rasmussen S Olesen JL. Care‐seeking behaviour of adolescents with knee pain: A population‐based study among 504 adolescents. BMC Musculoskelet Disord. 2013;14:225‐2474‐14‐225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Myer GD Ford KR Barber Foss KD, et al. The incidence and potential pathomechanics of patellofemoral pain in female athletes. Clin Biomech (Bristol, Avon). 2010;25(7):700‐707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ireland ML Willson JD Ballantyne BT Davis IM. Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther. 2003;33(11):671‐676. [DOI] [PubMed] [Google Scholar]
- 31.McConnell J. Management of patellofemoral problems. Man Ther. 1996;1(2):60‐66. [DOI] [PubMed] [Google Scholar]
- 32.Witvrouw E Cambier D Danneels L, et al. The effect of exercise regimens on reflex response time of the vasti muscles in patients with anterior knee pain: A prospective randomized intervention study. Scand J Med Sci Sports. 2003;13(4):251‐258. [DOI] [PubMed] [Google Scholar]
- 33.Taunton JE Ryan MB Clement DB McKenzie DC Lloyd‐Smith DR Zumbo BD. A retrospective case‐control analysis of 2002 running injuries. Br J Sports Med. 2002;36(2):95‐101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.von Elm E Altman DG Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495‐1499. [DOI] [PubMed] [Google Scholar]
- 35.Souza RB Powers CM. Differences in hip kinematics #muscle |strength, and muscle activation between subjects with and without patellofemoral pain. J Orthop Sports Phys Ther. 2009;39(1):12‐19. [DOI] [PubMed] [Google Scholar]
- 36.Milgrom C Finestone A Eldad A Shlamkovitch N. Patellofemoral pain caused by overactivity. A prospective study of risk factors in infantry recruits. J Bone Joint Surg Am. 1991;73(7):1041‐1043. [PubMed] [Google Scholar]
- 37.Whitman P Melvin M Nicholas J. Common problems seen in a metropolitan sports injury clinic. Phys.Sportsmed. 1981;9:105‐108. [DOI] [PubMed] [Google Scholar]
- 38.Baquie P Brukner P. Injuries presenting to an australian sports medicine centre: A 12‐month study. Clin J Sport Med. 1997;7(1):28‐31. [DOI] [PubMed] [Google Scholar]
- 39.Nejati P Forogh B Moeineddin R Baradaran H Nejati M. Patellofemoral pain syndrome in iranian female athletes. Acta Medica Iranica. 2011;49(3):169‐172. [PubMed] [Google Scholar]
- 40.Grenholm A Stensdotter AK Hager‐Ross C. Kinematic analyses during stair descent in young women with patellofemoral pain. Clin Biomech (Bristol, Avon). 2009;24(1):88‐94. [DOI] [PubMed] [Google Scholar]
- 41.Kaya D Citaker S Kerimoglu U, et al. Women with patellofemoral pain syndrome have quadriceps femoris volume and strength deficiency. Knee Surg Sports Traumatol Arthrosc. 2011;19(2):242‐247. [DOI] [PubMed] [Google Scholar]
- 42.Powers CM Landel R Perry J. Timing and intensity of vastus muscle activity during functional activities in subjects with and without patellofemoral pain. Phys Ther. 1996;76(9):946‐55. [DOI] [PubMed] [Google Scholar]
- 43.Dolak KL Silkman C Medina McKeon J Hosey RG Lattermann C Uhl TL. Hip strengthening prior to functional exercises reduces pain sooner than quadriceps strengthening in females with patellofemoral pain syndrome: A randomized clinical trial. J Orthop Sports Phys Ther. 2011;41(8):560‐570. [DOI] [PubMed] [Google Scholar]
- 44.McAlindon TE Snow S Cooper C Dieppe PA. Radiographic patterns of osteoarthritis of the knee joint in the community: The importance of the patellofemoral joint. Ann Rheum Dis. 1992;51(7):844‐849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Duncan RC Hay EM Saklatvala J Croft PR. Prevalence of radiographic osteoarthritis‐‐it all depends on your point of view. Rheumatology (Oxford). 2006;45(6):757‐760. [DOI] [PubMed] [Google Scholar]
- 46.Wood L Muller S Peat G. The epidemiology of patellofemoral disorders in adulthood: A review of routine general practice morbidity recording. Prim Health Care Res Dev. 2011;12(2):157‐164. [DOI] [PubMed] [Google Scholar]
- 47.Narkbunnam R Chareancholvanich K Hanroongroj T. Sagittal plane evaluation of patellofemoral movement in patellofemoral pain patients with no evidence of maltracking. Knee Surg Sports Traumatol Arthrosc. 2013. [DOI] [PubMed] [Google Scholar]
- 48.Rutland M O'Connell D Brismee JM Sizer P Apte G O'Connell J. Evidence‐supported rehabilitation of patellar tendinopathy. N Am J Sports Phys Ther. 2010;5(3):166‐178. [PMC free article] [PubMed] [Google Scholar]