Abstract
Background
Limited information exists regarding injury risk factors for high school athletes. The Functional Movement Screen (FMS™) has been used to identify functional movement impairments and asymmetries, making it a potential predictor of injury.
Hypothesis/Purpose
To determine if the FMS™ is a valid predictor of injury in high school athletes and to identify a potential new FMS™ cutoff score for this population.
Study Design
Prospective Cohort
Methods
167 high school athletes among several sports were scored using the FMS™ and were monitored for injury during a single season. Likelihood ratios were calculated to determine how much a subject's total FMS™ score influenced the post‐test probability of becoming injured.
Results
Of the 167 participants, 39 sustained a musculoskeletal injury. Of all component scores, the in‐line lunge scores were significantly higher for injured players. For shoulder mobility, scores were significantly lower for injured players. No statistically significant associations were found between total FMS™ scores and injury status.
Conclusion
The FMS™ may be useful for recognizing deficiency in certain movements, however this data suggests that the FMS™ should not be used for overall prediction of injury in high school athletes throughout the course of a season. Normative data from a large sample size is now available in the high school athlete demographic.
Level of Evidence
3
Keywords: Functional Movement Screen (FMS™), high school athlete, injury risk factors, sports injury
Introduction
High school athletics involve an estimated 7.7 million participants each year as reported by the National High School Sports‐Related Injury Surveillance Study, 2011‐2012.1 This participation results in an estimated 1.4 million injuries at a rate of 2.2 injuries per 1,000 athletic exposures (practices or competitions). Limited data exists regarding injury risk factors for high school athletes. Previous authors have suggested that more years of playing experience, previous history of being injured, and being involved in a greater number of coached sports are risk factors for injury in adolescent athletes, whereas physical characteristics such as height, weight, and strength are poor predictors.2,3,4 Although BMI is a poor predictor, authors of a previous study found that overweight high school football players were at an increased risk for ankle injuries, particularly in those who had previously sprained their ankle.5 Qualifications of the coach, in terms of level of experience and additional training and education, have been associated with a decreased risk of injury in adolescent athletes.6 Asymmetries, including mobility, range of motion and strength differences between sides, have also been identified as possible factors.7,8,9,10
The movement patterns examined in the Functional Movement Screen (FMS™) place the athlete in positions where functional movement limitations and asymmetries may be identified, making it a potential predictor of injury.2 The FMS™ consists of seven tests, each scored between zero and three points with three representing the best possible score. The composite score, or total screen score, ranges from 0 to 21 points. The seven tests include the deep squat, hurdle step, inline lunge, shoulder mobility, active straight‐leg raise, trunk stability pushup, and rotary stability tests. Descriptions of the tests and scoring criteria have been described previously.11,12,13,14
Previous research by Kiesel, et al15 suggested that the total FMS™ score could identify National Football League (NFL) players at risk for serious injury. Chorba et al16 found a significant correlation between low‐scoring female collegiate athletes and injury. Both studies identified a cutoff score of 14 or less as a positive predictor of injury. Similarly, a study conducted on collegiate NCAA Division I and club athletes involved in swimming/diving, rugby, and soccer found that subjects with composite scores of 14 or less and a self‐reported history of previous injury were 15 times more likely to incur an injury versus those scoring above 14.17 To the knowledge of the authors, the FMS™ has not been validated for use in high school athletes, although normative values in physically active adolescent school‐aged children have been reported.18 Using this tool could provide physical therapists, athletic trainers, coaches and other clinicians with the necessary information to have the injury risk in high school athletics reduced. Identifying at‐risk athletes in pre‐season screening with the use of a low cost, time efficient, and low physical risk screen can potentially decrease the number of injuries, decrease medical costs to parents and schools, and keep athletes from injury related school absences.
The purpose of this study was to determine if the FMS™ is a valid predictor of injury in high school athletes. It was hypothesized that those with lower FMS™ scores were at a higher risk of injury. Results of the study would also be used to examine if a score of 14 out of 21, as determined by Kiesel et al6 in NFL players, is an appropriate cutoff score in predicting injury in high school athletes.
Methods
One hundred eighty‐five student athletes (97 female, 88 male) from one public high school were recruited for the study during the 2012 fall season. All fall sport athletes were educated on the study design and participation was voluntary. Parental consent was obtained if the athletes were under the age of 18. The athletes or their guardians had the opportunity to opt out of participation at any point in the screening process and throughout data collection during the season. Represented sports included boys and girls cross‐country, boys football, boys and girls soccer, girls swimming, girls tennis, and girls volleyball. Inclusion criteria included those ages 13‐18 in good academic standing. Exclusion criteria included those not cleared by the school or their physician in a pre‐participation physical exam and those who had reported any health contraindications to exercise and athletic activity including current musculoskeletal injury. The study was approved by the SUNY Upstate Medical University Institutional Review Board. Volunteers and their parents/legal guardians were required to provide written informed consent prior to participation in the study.
Testing occurred within the first week of the fall sports season. Four examiners, including one licensed physical therapist with 20 + years experience and three third year doctor of physical therapy candidates, conducted the testing. All examiners held Functional Movement Screen certification through Functional Movement Systems, Inc. (Chatham, VA). Prior to data collection, each examiner participated in pilot study screening of at least 10 participants each, in addition to online training and formal classroom education of the FMS™. The FMS™ has been reported to have high interrater composite score reliability (ICC = .98) between an experienced and novice tester,19 and moderate to good interrater and intrarater composite score reliability (ICC = .74 and ICC = .76, respectively) among novice testers.4 Prior to testing, subjects were familiarized to the FMS™ and study protocol, and examiners utilized the same verbal instructions provided by Cook, et al5 during testing. Scores were recorded at this pre‐season screening session and the athletes were then monitored by the school's certified athletic trainer (ATC) in order to obtain injury information throughout the fall season. All participating coaches were briefed on the study and were required to uphold policy that all injuries be reported to the ATC. The ATC was blinded from each subject's FMS™ score. Based on previous research,16 injury was defined as a musculoskeletal injury that occurred as a result of participation in an organized high school practice or competition setting that required medical attention in which the athlete sought care from an ATC, physical therapist, physician, or other health care provider, and was restricted from complete participation for one or more exposures (practice or game). A single incidence of injury in accordance with this definition was considered an adequate inclusion in the injured group. Multiple injuries to the same athlete were not counted. Exclusion criteria included any neurological or non‐musculoskeletal injury, such as a concussion, eye injury, or skin disorder. The identity of the subjects was protected and only the injury information was recorded and disclosed to the examiners. All injury data was collected for analysis at the conclusion of each team's season.
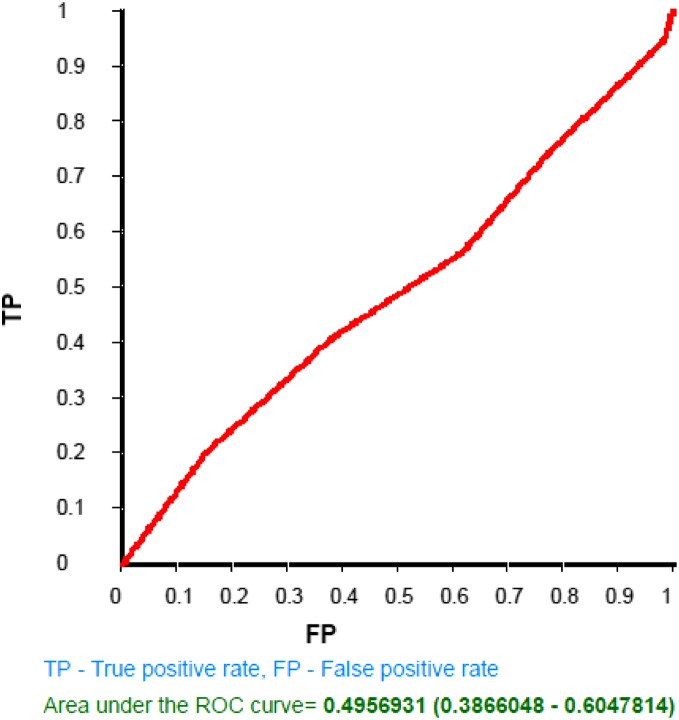
The distributions of FMS™ scores and participant age were evaluated and found to be non‐Gaussian. Accordingly, Wilcoxon signed‐rank tests were performed to determine associations between total and component FMS™ scores and injury status (any injury versus no injury), and between age and injury status. Statistical significance was set at p (alpha) < 0.05. To assess the predictive validity of the FMS™, sensitivity and specificity were calculated at different cut‐off points. A receiver operator characteristics (ROC) curve was created to determine a cut‐off score that maximized both sensitivity and specificity of total FMS™ scores. Likelihood ratios were calculated to determine how much a subject's total FMS™ score influenced the post‐test probability of becoming injured.
Results
A total of 185 students underwent screening using the FMS™ prior to beginning the season. Over the course of the season, 39 participants sustained a musculoskeletal injury. Eleven students were lost to academic ineligibility, radiographic evidence of injury prior to testing, or not qualifying for participation on a varsity or junior varsity level team. In addition, seven subjects incurred a concussion, and one sustained an eye injury. These 18 participants were excluded from analyses, leaving a sample of 167 participants, 90 females and 77 males, with complete data. Table 1 shows the distribution of participants by sport and gender.
Table 1.
Distribution of Participants by Sport and Gender
| Sport | Female | Male | Total |
|---|---|---|---|
| Cross Country | 10 | 16 | 26 |
| Football | 0 | 40 | 40 |
| Soccer | 37 | 21 | 58 |
| Swimming | 18 | 0 | 18 |
| Tennis | 9 | 0 | 9 |
| Volleyball | 16 | 0 | 16 |
Mean (SD) age of the sample was 15.2 years, while the median age was 15 years. Median ages of injured participants was 16 years, and of non‐injured participants was 15 years (p = .024, Wilcoxon rank‐sum test). Mean (SD) total and component FMS™ scores are displayed in Table 2. Among the component FMS™ scores, in‐line lunge and shoulder mobility were significantly different according to injury status. For in‐line lunge, scores were higher for injured players, for shoulder mobility, scores were lower for injured players. The average score for males was 13.0 and 13.1 for females, while those injured scored a 13.0 compared to the non‐injured group score of 13.1. Total FMS™ scores were not associated with injury status. Sensitivity, specificity, positive likelihood ratio and negative likelihood ratio are displayed in Table 3. Figure 1 displays a ROC curve based on this analysis.
Table 2.
Component and Total FMS Scores by Injury Status
| FMS Component | Not Injured (n = 128) | Injured (n = 39) | p | ||||
|---|---|---|---|---|---|---|---|
| Deep Squat | 1.86 ± 0.67 | 1.79 ± 0.66 | .522 | ||||
| Hurdle Step | 1.91 ± 0.38 | 1.82 ± 0.39 | .188 | ||||
| In‐line Lunge | 1.97 ± 0.55 | 2.21 ± 0.61 | .022 | ||||
| Shoulder Mobility | 2.67 ± 0.55 | 2.23 ± 0.84 | .001 | ||||
| Active SLR | 1.98 ± 0.68 | 1.97 ± 0.58 | .850 | ||||
| Pushup | 1.20 ± 0.49 | 1.41 ± 0.72 | .100 | ||||
| Rotary Stability | 1.51 ± 0.53 | 1.56 ± 0.55 | .701 | ||||
| Total | 13.11 ± 1.69 | 13.00 ± 2.32 | .954 | ||||
Values are mean (SD)
p‐values are derived from Wilcoxon signed‐rank tests
Table 3.
Validity Indices for Total FMS Scores at Various Cut‐off Points
| FMS Cut‐off Score* | Sensitivity | Specificity | Positive Likelihood Ratio | Negative Likelihood Ratio |
|---|---|---|---|---|
| 11 | .15 | .94 | 2.46 | 0.90 |
| 12 | .21 | .84 | 1.31 | 0.94 |
| 13 | .41 | .62 | 1.07 | 0.96 |
| 14 | .56 | .38 | 0.91 | 1.14 |
| 15 | .74 | .23 | 0.96 | 1.13 |
| 16 | .87 | .09 | 0.96 | 1.37 |
| 17 | .95 | .02 | 0.96 | 3.28 |
At risk status is below the indicated cut‐off score
Figure 1.
Receiver Operator Characteristic Curve for Total FMS Scores at Different Cut‐off Points.
Discussion
The results of the current investigation demonstrated that the FMS™ screening tool was not a valid predictor of injury in male and female high school athletes participating in various sports over one season of competition. Participants who sustained musculoskeletal injuries were more likely to be older than participants who were not injured. This is consistent with previous research regarding high school football players.2 It has been shown that the greatest risk factor for injury is sustaining a previous injury,20 thus older athletes have likely been playing for longer amounts of time than younger athletes and have had more opportunities for injury. In addition, the nature of higher “varsity” level athletics and the increased exposure time in older athletes over more years of participation could result in more injuries and therefore greater risk for future injury.
Significant findings included lower scores on the shoulder‐mobility movement in injured athletes (p = .001). This finding may support the regional interdependence model, in which “seemingly unrelated impairments in a remote anatomical region may contribute to, or be associated with, the patient's primary complaint.”21 Though the type of injuries sustained by these athletes varied in terms of body region, published research supports the notion of regional interdependence and how it could be used to potentially explain the lower scores that were found in shoulder mobility correlating to missed exposures. In the baseball literature, Scher et al determined that decreases in hip internal rotation in the non‐dominant hip highly correlated with predisposition to shoulder injuries in the non‐pitching baseball players.22 This is an example of how impairments in a remote anatomical region such as the hip could have profound effects on a distant structure and correlate to injury. This is one of few significant findings in the data set and it is understood that a limitation of the current study may deem these results a spurious finding.
The other statistically significant finding was that higher scores for the in‐line lunge were exhibited in athletes who were injured (2.21 + 0.61), as compared to lower scores in uninjured athletes (1.97 + 0.55) (p = .022). The authors cannot explain this counterintuitive finding. Ultimately, the conclusion from this data is that in this particular population total FMS™ scores were a poor predictor of injury status in high school athletes. It is possible that younger athletes present with varying levels of maturity, development and motor control, and the FMS™ is not an appropriate test battery to detect those at risk for injury in this population. Future research is needed to further validate an association between age and FMS™ scores in younger populations.
The authors feel that this research has provided a basis for normative data for high school aged athletes performing the FMS™. The deep squat, hurdle step and active straight leg raise trended towards lower scores in injured athletes compared to higher scores in uninjured athletes, without reaching statistically significant differences. The authors are unable to propose a cutoff score for high school athletes as the ROC curve indicates that there is no cutoff point that might be considered predictive of injury. Further research is necessary to identify if an alternate cutoff score other than 14 (as determined by Kiesel et al6 in NFL players) is appropriate for high school athletes. The trend does indicate, however, that in this population a cutoff score of 13 may warrant closer examination, as those injured had a slightly lower score of 13 while those uninjured scored just above 13. Other additional research in the future may compare FMS™ in fatigued to non‐fatigued athletes, as multiple sources indicate a loss of motor control in a fatigued state.23,24,25,26
Study Limitations
There are inconsistencies across the literature in terms of definition of injury. The definition for this study was limited to a single incidence of a musculoskeletal injury and was not specified to contact or non‐contact. Further research may be more specific in defining this. The authors were not able to capture exposures in this study. Those with a higher score may have better movement quality and patterns, and consequently be better athletes. Better athletes are more likely to be starters in competitions and have more exposures, which may in turn lead to an increased risk of injury. It was difficult to keep track of exposures, and although the ATC did try to identify who started versus who did not, however, this was not an accurate enough means of measurement and was therefore not included in the data analysis. Athlete side‐to‐side asymmetries were not collected during testing due to time constraints. The authors’ acknowledge that this was a potential limitation for the study, and further studies could examine if there is a correlation of asymmetrical scoring on FMS™ tests to injury risk. It was thought that the FMS™ could potentially identify athletes who sustained noncontact injuries, but this detail was not recorded in the injury reporting. Further studies may try to focus on tracking exposure and nature of injury.
Conclusion
Previous studies using the FMS™ as a screening tool investigated performance in college age or professional athletes, and in these studies, the FMS™ had some predictive validity for injury.6,7 According to the results of this study, the FMS™ is not a predictor of injury in high school age athletes. Normative data now exists on each of the seven movements of the FMS™ for clinicians to access when evaluating athletes of a similar demographic. The authors conclude that the FMS™ does have benefits in recognizing deficiency in certain movements, and with further training the performance of these particular movements could improve, but it should not be used for overall prediction of injury in high school athletes throughout the course of a season.
References
- 1.Comstock RD Collins CL Corlette JD Fletcher EN. National High School Sports‐Related Injury Surveillance Study ‐ 2011‐12 school year. Columbus, OH: Nationwide Children's Hospital; 2012. Available at http://www.nationwidechildrens.org/cirp-rio-study-reports/2011-12HighSchoolRIOSummaryReport.pdf. Accessed February 27, 2013. [Google Scholar]
- 2.Turbeville SD Cowan LD Owen WL Asal NR Anderson MA. Risk factors for injury in high school football players. Am J Sports Med. 2003; 31(6):974‐980. [DOI] [PubMed] [Google Scholar]
- 3.Emery CA Tyreman H. Sports participation, sport injury, risk factors and sport safety practices in Calgary and area junior high schools. Paediatr Child Health. 2009; 14(7): 439‐444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knowles SB Marshall SW Bowling MJ, et al. Risk factors for injury among high school football players. Epidemiology. 2009; 20(2):302‐310. [DOI] [PubMed] [Google Scholar]
- 5.Tyler TF McHugh MP Mirabella MR Mullaney MJ Nicholas SJ. Risk factors for noncontact ankle sprains in high school football players: The role of previous ankle sprains and body mass index. Am J Sports Med. 2006; 34(3);471‐475. [DOI] [PubMed] [Google Scholar]
- 6.Schulz MR Marshal SW Yang J Mueller FO Weaver NL Bowling JM. A prospective cohort study of injury incidence and risk factors in North Carolina high school competitive cheerleaders. Am J Sports Med. 2004; 32(2):396‐405. [DOI] [PubMed] [Google Scholar]
- 7.Knapik JJ Bauman CL Jones BH Harris JM Vaughan L. Preseason strength and flexibility imbalances associated with athletic injuries in female collegiate athletes. Am J Sports Med. 1991; Jan‐Feb;19(1):76‐81. [DOI] [PubMed] [Google Scholar]
- 8.Nadler SF Malanga GA Feinberg JH Prybicien M Stitik TP DePrince M. Relationship between hip muscle imbalance and occurrence of low back pain in collegiate athletes: a prospective study. Am J Phys Med Rehabil. 2001; 80(8):572‐577. [DOI] [PubMed] [Google Scholar]
- 9.Plisky PJ Rauh MJ Kaminski TW Underwood FB. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006; 36(12):911‐919. [DOI] [PubMed] [Google Scholar]
- 10.Shanley E Rauh MJ Michener LA Ellenbecker TS Garrison JC Thigpen. Shoulder range of motion measures as risk factors for shoulder and elbow injuries in high school softball and baseball players. Am J Sports Med. 2011; 39(9):1997‐2006. [DOI] [PubMed] [Google Scholar]
- 11.Cook G Burton L Hoogenboom B. Pre‐Participation screening: The use of fundamental movements as an assessment of function—part 1. North Am J Sports Phys Ther. 2006; 1(2):62‐72. [PMC free article] [PubMed] [Google Scholar]
- 12.Cook G Burton L Hoogenboom B. Pre‐Participation screening: The use of fundamental movements as an assessment of function—part 2. North Am J Sports Phys Ther. 2006; 1(3):132‐139. [PMC free article] [PubMed] [Google Scholar]
- 13.Teyhen DS Shaffer SW Lornson CL, et al. The Functional Movement Screen: a reliability study. J Orthop Sports Phys Ther. 2012; 42(6): 530‐540. [DOI] [PubMed] [Google Scholar]
- 14.Cook G Burton L Kiesel K Rose G Bryant MF. Movement: Functional Movement Systems: Screening‐Assessment‐Corrective Strategies. Aptos, CA: On Target Publications; 2010. [Google Scholar]
- 15.Kiesel K Plisky JP Voight ML. Can serious injury in professional football be predicted by a preseason functional movement screen? North Am J Sports Phys Ther. 2007; 2(3):147‐158. [PMC free article] [PubMed] [Google Scholar]
- 16.Chorba RS Chorba DJ Bouillon LE Overmyer CA Landis JA. Use of a functional movement screening tool to determine injury risk in female collegiate athletes. North Am J Sports Phys Ther. 2010; 5(2):47‐54. [PMC free article] [PubMed] [Google Scholar]
- 17.Garrison M Westrick R Johnson MR Benenson J. Association between the Functional Movement Screen and injury development in college athletes. Int J Sports Phys Ther. 2015; 10(1):21‐28. [PMC free article] [PubMed] [Google Scholar]
- 18.Abraham A Sannasi R Nair R. Norative values for the Functional Movement Screen™ in adolescent school aged children. Int J Sports Phys Ther. 2015; 10(1):29‐36. [PMC free article] [PubMed] [Google Scholar]
- 19.Onate JA Dewey T Kollock RO Thomas KS Van Lunen BL DeMaio M, and Ringleb SI. Real‐time intersession and interrater reliability of the functional movement screen. J Strength Cond Res. 2012; 26(2):408–415. [DOI] [PubMed] [Google Scholar]
- 20.Emery CA Meeuwisse WH Hartmann SE. Evaluation of risk factors for injury in adolescent soccer: Implementation and validation of an injury surveillance system. Am J Sports Med. 2005; 33(12):1882‐1891. [DOI] [PubMed] [Google Scholar]
- 21.Wainner RS Whitman JM Cleland JA Flynn TW. Regional interdependence: a musculoskeletal examination model whose time has come. J Orthop Sports Phys Ther. 2007; 37(11):658‐60. [DOI] [PubMed] [Google Scholar]
- 22.Scher S Anderson K Weber N Bajorek J Rand K Bey MJ. Associations among hip and shoulder range of motion and shoulder injury in professional baseball players. J Athl Train. 2010; 45:191‐197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McLean SG Samorezov JE. Fatigue‐induced ACL injury risk stems from degradation in central control. Med Sci Sports Exerc. 2009; 41(8):1661‐1672. [DOI] [PubMed] [Google Scholar]
- 24.Mathers JF Grealy MA. Motor control strategies and the effects of fatigue on golf putting performance. Front Psychol. 2013; 4:1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lees A. Science and the major racket sports: a review. J. Sports Sci. 2003; 21:707‐732. [DOI] [PubMed] [Google Scholar]
- 26.Forestier N Nougier V. The effects of muscular fatigue on the coordination of a multijoint movement in human. Neurosci Lett. 1998; 252(3):187‐190. [DOI] [PubMed] [Google Scholar]