Abstract
Background
The significance of scapular dyskinesis is being challenged due to a lack of the association with pain and ability to predict injury in athletic populations. However, it is unknown whether asymptomatic overhead athletes with dyskinesis cope by normalizing scapular position with higher demand activities.
Hypothesis/Purpose
The purpose of this study was to compare change in scapular kinematics from an active unweighted contraction to a maximal isometric contraction in asymptomatic overhead athletes with and without scapular dyskinesis. Secondarily, force generated with manual muscle tests were explored for differences and relationships with kinematics.
Study Design
Cross‐sectional laboratory study
Methods
Twenty‐five matched asymptomatic overhead athletes with (n=14) and without (n=11) scapular dyskinesis, defined with a reliable and validated clinical method, participated in this study. Three‐dimensional scapular kinematics were evaluated in an active unweighted condition, and during maximal isometric contractions at 90 ° of shoulder flexion. Isometric force produced with lower trapezius and serratus anterior manual muscle tests were assessed with a dynamometer. Changes in scapular kinematics were compared between groups. Differences in force generated with manual muscle tests between groups and relationships with kinematics were explored.
Results
Athletes with dyskinesis demonstrated greater deficits in scapular upward rotation with maximal contraction (p=<0.001), less external rotation (p=0.036) and weaker lower trapezius manual muscle test strength (p=0.031). Lower trapezius (p=0.003;r=0.57) and serratus anterior (p=0.042;r=0.41) manual muscle test strength deficits were fair to moderately associated with a lack of scapular upward rotation during maximal contraction.
Conclusion
Small to moderate changes in scapular kinematics are normal responses to a maximal contraction, but with scapular dyskinesis this response is accentuated. Athletes with dyskinesis generate less force with lower trapezius manual muscle testing compared to athletes without dyskinesis. Decreased strength with lower trapezius and serratus anterior manual muscle testing was also related to a lack of upward rotation in all athletes.
Level of Evidence
3
Keywords: Shoulder, biomechanics upper extremity, scapula, strength testing
INTRODUCTION
Abnormal movement of the scapula, termed scapular dyskinesis,1 is common among athletes who participate in overhead sports2,3 and has been theorized to predispose athletes to shoulder injury. In a prospective study of asymptomatic rugby players, players identified with scapular dyskinesis during preseason had a high incidence of in‐season shoulder injury.4 However, there is also evidence to support the contrary.2,5 Additionally, the presence of clinically observed scapular dyskinesis exists independent of shoulder pain in athletes participating in overhead sports. As such, the significance of clinically observed scapular dyskinesis and need for scapular stabilization programs are being scrutinized.
Underlying conflicting study results is the fact that scapular motion is complex, occurring three‐dimensionally (3D). This has challenged the clinician's ability to reliably detect, much less subcategorize abnormal movement into types such as inferior angle prominence versus excessive shoulder shrug6‐8 without sophisticated laboratory measures.9 Several clinical methods to evaluate scapular motion have been described with good reproducibility,10‐14 but few have been validated.11,15 Visual observation of scapular motion during shoulder flexion with a light resistive load, termed the scapular dyskinesis test16, has been shown to be both a reliable and validated method to clinically identify the presence of dyskinesis in overhead athletes in terms of either dysrhythmia or inferior/medial boarder prominence.3,7,16 Clinical measures should demonstrate both acceptable reliability and validity to be useful, and research that does not utilize such measures to identify dyskinesis should be taken in this context.
One possible reason for the conflicting evidence examining relationships between the presence of scapular dyskinesis and injury risk in overhead athletes may be due to the load used during testing. Studies investigating pain3 or injury risk2 in overhead athletes with dyskinesis have used visual observation methods which incorporate the use of light external load during repeated arm elevation. Clinically, scapular dyskinesis is often attributed to scapular muscle weakness, but evidence to support this relationship using the visual observation method to define dyskinesis is lacking. It is possible that asymptomatic overhead athletes with scapular dyskinesis with light external loads may respond differently with heavier external loads.
Previous investigations demonstrate that varying external resistance loads change 3D scapular motion during humeral elevation with inconsistent results.16‐22 Discrepancies have been attributed to the varying loads used.17 However, only one study evaluated participants for scapular dyskinesis.17 To the authors’ knowledge, whether changes in 3D scapular kinematics differ in overhead athletes with and without scapular dyskinesis in response to a higher demand activity, such as a maximal contraction, is unknown. If scapular dyskinesis is related to impaired scapular muscle strength contributing to the lack of scapular stability, then scapular alterations in individuals with scapular dyskinesis would persist or worsen with greater loads. However, it is possible that overhead athletes with scapular dyskinesis detected with light loads may uniquely possess adequate scapular muscle strength and scapular stability with higher demand activities due to their specific sport training.
Therefore, the primary aim of this study was to compare change in 3D scapular kinematics with a maximal contraction between asymptomatic overhead athletes with and without scapular dyskinesis. It was hypothesized that compared to asymptomatic overhead athletes without dyskinesis, athletes with scapular dyskinesis would demonstrate alterations in 3D scapular kinematics during unweighted arm elevation, but those alterations would be less pronounced with a maximal isometric elevation contraction. It was also hypothesized that overhead athletes without scapular dyskinesis would demonstrate smaller changes in scapular kinematics between the unweighted and maximum contraction arm elevation because these individuals are able to sufficiently stabilize the scapula during both contraction conditions. The secondary aims of the study were to explore scapular muscle strength as a potential explanatory factor for differences between groups.
METHODS
Subjects
The University institutional review board approved this study. Overhead athletes were recruited to participate in this cross‐sectional study from local college and university populations. Twenty‐eight asymptomatic overhead athletes agreed to participate and signed the university‐approved informed consent. Subjects were eligible if they were currently participating without restrictions in a club or varsity level overhead sport, defined as baseball, swimming, tennis, water polo, or volleyball. The dominant shoulder was tested in all eligible participants. Exclusion criteria are listed in Table 1. The scapular dyskinesis test3 was used to define scapular motion as normal, subtle, or obvious dyskinesis, by two independent examiners. The examiners were physical therapists and an athletic trainer professional with experience ranging from 2‐19 years. Examiners completed standardized training in the dyskinesis visual observation method.16 The test consists of five repetitions of bilateral, active, shoulder flexion and abduction holding 1.4kg (3lb) or 2.3kg (5lb) weights, 2.3kgs was used for athletes weighing over 68.1kgs.16 Obvious dyskinesis was defined as dysrhythmia or inferior angle/medial boarder prominence of at least 2.5cm during at least 3 repetitions. Athletes classified with normal scapular motion were included and matched by age (±5 years), laterality, and gender to participants with obvious dyskinesis (Figure 1). Three subjects with normal scapular motion were excluded due to a rating of subtle dyskinesis by at least one of the two independent examiners. Thus, twenty‐five subjects were included in the final analysis, fourteen subjects with scapular dyskinesis and eleven subjects with normal motion (Table 2). Prior to initiating the study, a sample size of 16 total subjects was deemed necessary to provide 90% power, with α=0.05, to detect a 5 ° difference in change in 3D scapular kinematics with a maximal contraction between groups using effect size estimates from prior work.3,23,24
TABLE 1.
Participant study exclusion criteria
| Athletes with any of the following were excluded: |
Figure 1.
An athlete classified with scapular dyskinesis (right shoulder) with the visual observation method.
TABLE 2.
Overhead athlete participant characteristics
| With Dyskinesis (n=14) | Without Dyskinesis (n=11) | |
|---|---|---|
| Gender (male/females) | 5 (35.7%) / 8 (64.3%) | 5 (38.5%) / 6 (54.5%) |
| Age (mean ± SD), years | 20.3 ± 1.4 | 20.5 ± 1.2 |
| Height (mean ± SD), cm | 175.5 ± 13.9 | 175.3 ± 9.0 |
| Mass (mean ± SD), kg | 67.0 ± 12.4 | 71.6 ± 10.3 |
| Arm Dominance | 1 left; 13 right | 1 left; 10 right |
| Participant Sport (n) | 3 Swimming | 2 Swimming |
| 9 Volleyball | 6 Volleyball | |
| 2 Water Polo | 3 Water polo |
Manual Muscle Testing
Shoulder strength during manual muscle testing (MMT) was defined as peak isometric force measured with a handheld dynamometer. Assessment of shoulder strength with a handheld dynamometer has demonstrated excellent inter‐rater and intra‐rater reliability.25 The order of the muscle testing was randomized by blinded drawing prior to testing. For the serratus anterior muscle, the subject was seated upright in a chair positioned with feet flat on the floor, shoulder‐width apart. Subjects were asked to look straight ahead and flex the dominant shoulder to 120 °, confirmed with a goniometer, with the thumb facing upward. For the lower trapezius muscle, the subject was prone on a plinth with the dominant arm in 120 ° of abduction and thumb facing upward. With both tests, the pad of a handheld force dynamometer was placed at the distal aspect of the wrist, just proximal to the radial styloid process, and held stationary by the examiner with two hands. Subjects were asked to push as hard as possible into the dynamometer pad for a verbal 5‐second count. Before maximal testing of each muscle, a sub‐maximal (50%) effort trial was performed to minimize learning effects. Maximum force output (kg) of two separate 5‐second maximal isometric contractions was recorded. A 30‐second rest period was provided between trials. The peak force of the two trials was averaged, normalized to the subject's bodyweight (kg) and expressed as a percentage. These muscle testing positions have been validated to produce the maximum surface EMG activity of the primary agonist and the least involvement of surrounding muscles with electromyography.26 Therefore, the authors’ took force production in these positions to represent strength of the respective muscle. Within session, test‐retest reliability was established for the examiners in this study. Intraclass correlation coefficients (ICC), standard error of measurement , and minimal detectable change , were calculated. The MMT measurements showed excellent reliability (ICC 0.95‐0.98). The lower trapezius MMT showed SEM=0.4% of body weight and MDC=0.5%, while the serratus anterior MMT showed SEM=0.6% and MDC=0.8%.
3D Scapular Kinematics
The Ascension Trakstar electromagnetic‐based motion capture system (Ascension Technology Corporation, Milton, VT, USA) with a sampling rate of 240 Hz was used with Motion Monitor software (Innovative Sports Training, Inc., Chicago, IL, USA) to collect 3D kinematic data of the scapula, humerus, and trunk. The system consists of a transmitter that emits a magnetic field detected by 4 receivers. The reported accuracy of the electromagnetic tracking device is 1.4 mm and 0.5 ° 27 and mean errors for skin mounted receivers are 3.56 ° for scapular rotation below 120 ° of humeral elevation.28
Electromagnetic receivers were placed on the thorax over the spinous process of T3, the posterior‐lateral acromion, and the posterior aspect of the distal humerus of the dominant arm using double‐sided tape (3M HealthCare, St Paul, MN). The humeral receiver was further secured with PreWrap (Mueller, Prairie du Sac, WI). The fourth receiver was used to digitize anatomical landmarks on each segment following International Society of Biomechanics (ISB) recommendations.29 Digitization allowed transformation of the sensor position and orientation into anatomically‐based position and orientation data of the humerus and scapula with respect to the thorax. Euler angle sequences for humeral (Y‐X’‐Y”) and scapular (Y‐X’‐Z”) rotations were used.29 Scapular upward/downward rotation occurs around a horizontal axis perpendicular to the plane of the scapula, anterior/posterior tilting occurs around a horizontal axis parallel to the scapular spine, and internal/external rotation occurs around a vertical axis through the plane of the scapula.30,31 Scapular movements into the directions of upward rotation, posterior tilt, and external rotation were defined as positive values for clinical interpretation. Three‐dimensional kinematic data were collected during two 5‐second trials of shoulder flexion (humeral elevation in the sagittal plane) at 90 ° under each contraction condition. Kinematic data collected during a one second interval identified by the midpoint in each of the two separate 5‐second trials were averaged and used for analysis. The three scapular rotations showed excellent reliability (ICC 0.98‐0.99). The measurement error for the scapular rotations were: upward rotation SEM=3.0°, MDC=4.2°; posterior tilt SEM=1.9°, MDC=2.7°; external rotation SEM=2.0°, MDC=2.8°.
Elevation Contraction Conditions
Two repetitions each of two contraction conditions (unweighted active contraction; maximal contraction) were performed, with the order assigned by random drawing. During both contraction conditions, subjects were positioned with a non‐elastic strap under both feet, standing shoulder‐width apart, and over the distal aspect of both arms, proximal the radial styloid process at the wrist, thumbs facing upward. Both elbows were fully extended and shoulders flexed to 90 °, confirmed with a goniometer. The length of the strap was adjusted so no slack was present maintaining the testing position (Figure 2). Once the strap was properly tensioned, the subject relaxed both arms at his/her side for 30‐seconds. The subject would then assume this testing position with the strap with each of the contraction conditions.
Figure 2.
Subject positioned with a non‐elastic strap during both the active and maximal isometric contraction testing conditions.
During the unweighted active condition, subjects actively raised both arms to 90 ° in the sagittal plane, verified with a goniometer, taking up the slack in the strap and avoiding additional force. Three‐dimensional kinematic data were recorded for a 5‐second verbal count. During the maximum contraction condition, subjects assumed the testing position then were asked to push both arms upward into the strap at 50% effort for verbal 5‐second count, maintaining a straight spine. This submaximal trial was used to gain familiarity with the procedure and make any necessary adjustments to the length of strap by verifying the 90 ° shoulder position with a goniometer. During this submaximal trial, additional verbal cues were provided to avoid substitutional movements such as trunk hyperextension. Two maximal contractions were then performed. During the maximal contraction condition, standardized verbal encouragement with a series of four sequential, loud cues of “push” was provided by the second examiner. During either contraction condition, if the subject's position was not properly maintained, the trial was discarded and another trial was performed.
Statistical Analysis
Descriptive statistics were computed for all demographic variables. Independent t‐tests were used to compare age, height and mass between groups. Separate 2x2 factorial mixed‐model analysis of variance (ANOVAs) were used to compare mean 3D scapular kinematics between groups with factors of group (dyskinesis; normal), contraction condition (active; maximum), and interactions. With a statistical significance, post hoc comparisons were made using linear contrasts with a Bonferroni adjusted alpha for a priori comparisons of interest to include main effects contraction condition, group, or interactions. To explore potential explanatory factors for MMT differences between the groups, independent t‐tests were used. Bivariate correlation analyses were used to determine the relationships between lower trapezius and serratus anterior MMT and change in scapular kinematics with maximal contraction. For all statistical analyses, significance was set at α=.05. All analyses were performed using SAS Software (JMP 9.0.3;SAS Institute Inc., Cary, NC, USA).
RESULTS
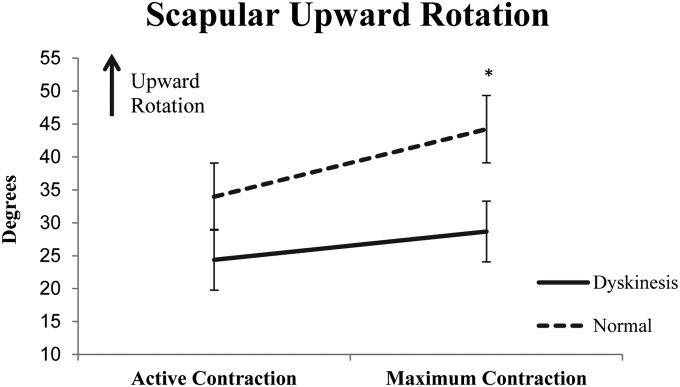
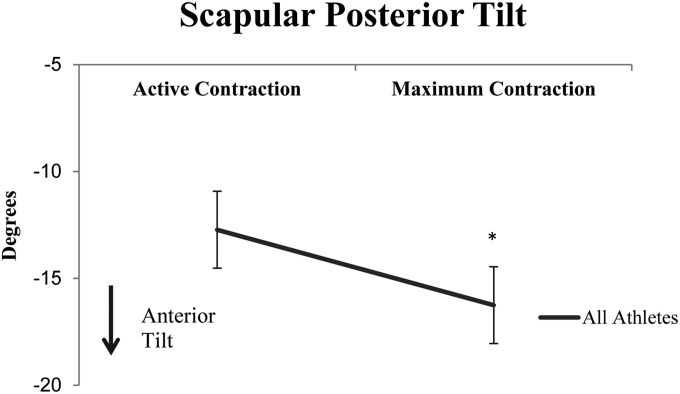
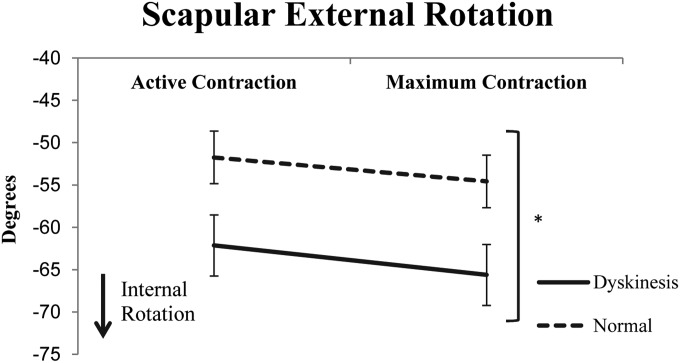
There were no significant differences (p > 0.05) in age, height and mass characteristics between groups. Scapular upward rotation showed both within group (contraction main effect) and between group (group‐by‐contraction interaction) differences during the two contraction conditions (Table 3 and Figure 3). The change in upward rotation between the unweighted and maximal contraction conditions was 6.3 ° (p<0.001; 95%CI=5.0 °,7.6 °) greater in athletes without dyskinesis. Athletes with dyskinesis demonstrated a smaller but significant 4.3 ° (p = 0.018; 95%CI=0.4 °, 8.2 °) increase in scapular upward rotation from unweighted to maximal contraction conditions compared to a 10.3 ° (p < 0.001; 95%CI=6.3 °,14.2 °) significant increase in athletes without dyskinesis. With scapular posterior tilt, there were no significant interactions or group main effect, but a significant main effect of contraction condition (Table 3). This showed that athletes, regardless of group, had a 3.5 ° (p < 0.001; 95%CI=1.7 °,5.3 °) increase in scapular anterior tilt with maximal compared to active contraction conditions (Figure 4). With regard to scapular external rotation, there were no significant interactions, but significant main effects of group and contraction condition (Table 3 and Figure 5). These findings showed that athletes with dyskinesis demonstrated 10.7 ° greater internal rotation (p=0.036; 95%CI=0.8 °,20.6 °) across both contraction conditions than athletes with normal scapular motion, and both groups demonstrated a 3.2 ° (p<0.001;95%CI=1.8 °,4.4 °) increase in scapular internal rotation with maximal contraction compared to active contraction condition.
TABLE 3.
Results of mixed‐model analysis of variance (ANOVA) for scapular kinematics under active and maximal contraction conditions
| Source | df | Scapular Kinematics | |||||
|---|---|---|---|---|---|---|---|
| Upward Rotation | Posterior Tilt | External Rotation | |||||
| F Ratio | p‐value | F Ratio | p‐value | F Ratio | p‐value | ||
| Group | 1, 23 | 3.4 | 0.077 | 0.4 | 0.521 | 5.0 | 0.036* |
| Contraction Condition | 1, 23 | 32.6 | <0.001* | 17.7 | <0.001* | 24.7 | <0.001* |
| Group x Contraction Condition | 1, 23 | 5.5 | 0.029* | 1.6 | 0.218 | 0.3 | 0.620 |
p < 0.05
Figure 3.
Scapular upward rotation in athletes with (dyskinesis) and without (normal) scapular dyskinesis. *Significant difference between groups and contraction conditions (p = 0.029).
Figure 4.
Scapular posterior tilt in all athletes with the active and maximal contraction conditions. *Significant difference between contraction conditions regardless of group (p<0.001).
Figure 5.
Scapular external rotation in athletes with (dyskinesis) and without (normal) scapular dyskinesis *Significant difference between groups (p=0.036) and contraction conditions (p<0.001).
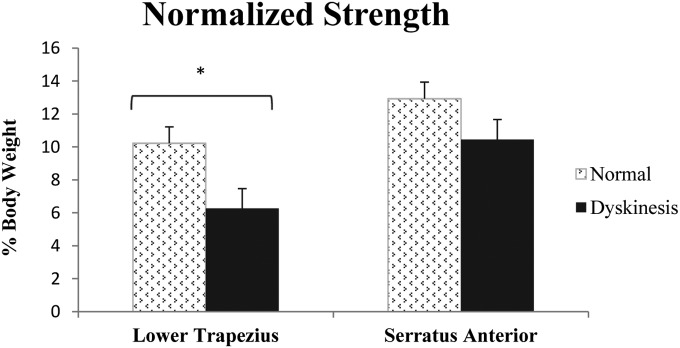
Results of MMT testing are shown in Figure 6. There were significant differences in the lower trapezius MMT strength between groups (t = 2.3;p = 0.031). Athletes with dyskinesis had weaker lower trapezius MMT mean normalized peak isometric force by 4.0% bodyweight (95%CI=0.4%, 7.5%) compared to athletes without dyskinesis. There was also a significant moderate positive linear correlation (r = 0.57, p = 0.003) between lower trapezius MMT and the change in scapular upward rotation between contraction conditions (Table 4). Less scapular upward rotation was associated with a weaker lower trapezius MMT, defined by normalized isometric force. The trend of a weaker serratus anterior MMT in athletes with dyskinesis did not reach statistical significance (t = 1.5; p = 0.15); however, there was a significant moderate positive linear correlation (r = 0.41, p = 0.042) between serratus anterior MMT and change in scapular upward rotation between contraction conditions. This means that less change in scapular upward rotation from active unweighted elevation to maximal contraction was related to less serratus anterior MMT strength. There were no other significant relationships (Table 4) between change in scapular muscle MMT strength and change in scapular kinematics.
Figure 6.
Lower trapezius and serratus anterior normalized peak isometric muscle force (strength).
Table 4.
Results of bivariate linear correlation analyses between lower trapezius and serratus anterior manual muscle test (MMT) strength (normalized isometric force) and change in scapular motion with maximal contraction
| Scapular Motion | Normalized MMT Isometric Strength | |
|---|---|---|
| Lower Trapezius | Serratus Anterior | |
| Upward Rotation | r = 0.57* | r = 0.41† |
| Posterior Tilt | r = −0.025 | r = −0.11 |
| External Rotation | r = −0.06 | r = −0.17 |
p = 0.003;
p = 0.042
DISCUSSION
The authors hypothesized that asymptomatic overhead athletes with dyskinesis have the ability to correctively stabilize their scapula during higher demand activities, explaining why athletes are able to participate in overhead sports without higher risk of injury. Contrary to the stated hypotheses, results suggest asymptomatic overhead athletes with visually observed scapular dyskinesis do not correctively stabilize the scapula with a maximal contraction. Specifically, athletes with dyskinesis demonstrated a lack of scapular upward rotation from active to maximal contraction (Figure 3) and less external rotation with both contractions (Figure 5) compared to athletes with normal scapular motion.
While no prior study has examined the effect of a maximal load in individuals with dyskinesis for comparison, the current study results are in agreement with Tate et al3 who found athletes with scapular dyskinesis had a statistically significant 9 ° deficit in scapular upward rotation during concentric humeral elevation below 90 ° in the sagittal plane while holding light weights (1.4/2.3kgs) compared to athletes with normal scapular motion. In the current study, the authors utilized a higher demand activity, maximal isometric contraction, and found athletes with dyskinesis to have significantly greater (15 °) scapular upward rotation deficits. Athletes with dyskinesis also had significantly greater (10.7 °) scapular internal rotation under both contraction conditions, while only trends of this were found in the prior study.3 Greater differences between groups found in the current study are attributed to using a higher demand activity. Also, the prior study included athletes with shoulder pain, which may have influenced their results.
The second hypothesis was that overhead athletes with normal scapular motion would demonstrate small changes in scapular kinematics with a maximum contraction because these individuals are able to sufficiently stabilize the scapula. This was partially confirmed. Athletes without dyskinesis had small changes in scapular anterior tilt (3.5 °) and internal rotation (3.2 °) with maximal isometric contraction, but larger increases in scapular upward rotation (10.3 °). Camci et al17 found similar changes in scapular upward rotation (1.4 ° increase) and in scapular anterior tilt (4.3 ° increase) at 90 ° flexion during concentric sagittal plane elevation with an external load of elastic resistance compared to an unloaded condition. The authors of the current study attribute the larger changes in upward rotation to the use of a higher demand maximal contraction. It is difficult to compare our results to the other previous research examining the effects of load on scapular kinematics16‐22 since previous studies may have included a heterogeneous mix of participants with and without dyskinesis.
Athletes with scapular dyskinesis had impaired force generation with manual muscle tests used to test lower trapezius activity (Figure 6). Athletes with dyskinesis were able to generate force with the manual muscle test of the lower trapezius equal to 6.3% bodyweight, a 40% deficit compared to athletes without dyskinesis. Scapular muscle MMT was also related to change in scapular upward rotation with maximal resistance. Weaker lower trapezius (r = 0.57) and serratus anterior (r = 0.41) MMT values were related to a lack of scapular upward rotation from the active to maximal contraction. Thus, strength during manual muscle tests of the lower trapezius and serratus anterior accounted for 32.5% and 16.8% of the variance (r2) in scapular upward rotation, respectively. These findings are consistent with those of Laudner et al,32 who reported a moderate positive relationship between lower trapezius strength and scapular upward rotation (r2=0.56) at 90 ° of humeral elevation in the scapular plane (scaption). In contrast to Laudner et al.,32 the current authors found a moderate relationship between serratus anterior strength and scapular upward rotation at 90 ° of shoulder flexion, whereas they reported a poor relationship (r2=0.16) at 90 ° of scaption. The current study strength results should be tempered since multiple shoulder muscles are activated during manual muscle testing intended to target one specific muscle. Specific to this study, the MMT used for the serratus anterior was modeled after the study by Ekstrom et al26 and did not involve stabilization of the lateral border of the scapula, as proposed by Kendall.33 This could have led to greater involvement of the anterior deltoid during the MMT used in this study. The results of these MMT tests show a moderate relationship between a lack of scapular upward rotation and normalized MMT strength deficits of the lower trapezius in overhead athletes and identify deficits of lower trapezius MMT strength in asymptomatic athletes with dyskinesis.
While this study provides new insight, the results are limited to asymptomatic overhead athletes. Further study in athletes with shoulder pain is necessary in order to determine if a distinct subgroup of athletes with pain have similar deficits in scapular muscle strength and a lack of scapular upward rotation. Additionally, no inferences can be made with regard to these athletes’ injury risk given the cross‐sectional study design. Results of this study were in conflict with the authors’ hypothesis that overhead athletes may normalize scapular stabilization or position with a higher demand activity. A limitation of studying clinically identified scapular dyskinesis is that examiners may identify cases of dyskinesis with a heterogeneous mix of underlying factors, so future biomechanical studies may benefit from subgrouping scapular dyskinesis based on specific identifiable biomechanical factors such as specific muscle strength imbalance or aberrant muscle co‐contraction patterns. A limitation specific to this study is that the authors measured scapular kinematics isometrically at 90 ° of shoulder flexion, which provides only a snapshot of overall scapular kinematics across the range of shoulder motions and muscular contractions. Further study is warranted to determine whether a cluster of impairments, beyond the presence of dyskinesis, may increase injury risk in overhead athletes. Lastly, while athletes who experienced shoulder pain in the last 6 months were excluded, participants’ history of pain before the research timeframe was unknown.
CONCLUSIONS
In overhead athletes with normal scapular motion, a maximal isometric elevation contraction at 90 ° results in small increases (<3.5 °) in scapular internal rotation and anterior tilt, but moderate increases in scapular upward rotation (10 °) compared to an unloaded active elevation condition. Athletes with scapular dyskinesis showed less upward rotation and greater internal rotation of the scapula at rest than those without dyskinesis. These scapular kinematic alterations are accentuated with a maximal isometric contraction in individuals with dyskinesis. Therefore, clinicians could consider using a maximal isometric contraction at 90 ° flexion to clarify the presence of dyskinesis or assess scapular stabilization in overhead athletes. Lastly, this study provides evidence that links lower trapezius MMT strength deficits with alterations in scapular motion in overhead athletes, and specifically identifies deficits in scapular muscle MMT strength in overhead athletes with clinically identified scapular dyskinesis.
REFERENCES
- 1.Kibler WB McMullen J. Scapular dyskinesis and its relation to shoulder pain. J Am Acad Orthop Surg. 2003;11(2):142‐151. [DOI] [PubMed] [Google Scholar]
- 2.Myers JB Oyama S Hibberd EE. Scapular dysfunction in high school baseball players sustaining throwing‐related upper extremity injury: a prospective study. J Shoulder Elbow Surg. 2013;22(9):1154‐1159. [DOI] [PubMed] [Google Scholar]
- 3.Tate AR McClure P Kareha S Irwin D Barbe MF. A clinical method for identifying scapular dyskinesis, part 2: validity. J Athl Train. 2009;44(2):165‐173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kawasaki T Yamakawa J Kaketa T Kobayashi H Kaneko K. Does scapular dyskinesis affect top rugby players during a game season? J Shoulder Elbow Surg. 2012;21(6):709‐714. [DOI] [PubMed] [Google Scholar]
- 5.Struyf F Nijs J Meeus M, et al. Does Scapular Positioning Predict Shoulder Pain in Recreational Overhead Athletes? Int J Sports Med. 2014;35(1):75‐82. [DOI] [PubMed] [Google Scholar]
- 6.Ellenbecker TS Kibler WB Bailie DS Caplinger R Davies GJ Riemann BL. Reliability of scapular classification in examination of professional baseball players. Clin Orthop Relat Res. Jun 2012;470(6):1540‐1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Uhl TL Kibler WB Gecewich B Tripp BL. Evaluation of clinical assessment methods for scapular dyskinesis. Arthroscopy. 2009;25(11):1240‐1248. [DOI] [PubMed] [Google Scholar]
- 8.Kibler WB Uhl TL Maddux JW Brooks PV Zeller B McMullen J. Qualitative clinical evaluation of scapular dysfunction: a reliability study. J Shoulder Elbow Surg. 2002;11(6):550‐556. [DOI] [PubMed] [Google Scholar]
- 9.Warner MB Whatling G Worsley PR, et al. Objective classification of scapular kinematics in participants with movement faults of the scapula on clinical assessment. Comput Methods Biomech Biomed Engin. 2015;18(7):782‐9. [DOI] [PubMed] [Google Scholar]
- 10.DiVeta J Walker ML Skibinski B. Relationship between performance of selected scapular muscles and scapular abduction in standing subjects. Phys Ther. 1990;70(8):470‐476. [DOI] [PubMed] [Google Scholar]
- 11.Johnson MP McClure PW Karduna AR. New method to assess scapular upward rotation in subjects with shoulder pathology. J Orthop Sports Phys Ther. 2001;31(2):81‐89. [DOI] [PubMed] [Google Scholar]
- 12.Odom CJ Taylor AB Hurd CE Denegar CR. Measurement of scapular asymetry and assessment of shoulder dysfunction using the Lateral Scapular Slide Test: a reliability and validity study. Phys Ther. 2001;81(2):799‐809. [DOI] [PubMed] [Google Scholar]
- 13.Peterson DE Blankenship KR Robb JB, et al. Investigation of the validity and reliability of four objective techniques for measuring forward shoulder posture. J Orthop Sports Phys Ther. 1997;25(1):34‐42. [DOI] [PubMed] [Google Scholar]
- 14.Watson L Balster SM Finch C Dalziel R. Measurement of scapula upward rotation: a reliable clinical procedure. Br J Sports Med. 2005;39(9):599‐603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26(2):325‐337. [DOI] [PubMed] [Google Scholar]
- 16.McClure P Tate AR Kareha S Irwin D Zlupko E. A clinical method for identifying scapular dyskinesis, part 1: reliability. J Athl Train. 2009;44(2):160‐164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Camci E Duzgun I Hayran M Baltaci G Karaduman A. Scapular kinematics during shoulder elevation performed with and without elastic resistance in men without shoulder pathologies. J Orthop Sports Phys Ther. 2013;43(10):735‐743. [DOI] [PubMed] [Google Scholar]
- 18.de Groot JH van Woensel W van der Helm FC. Effect of different arm loads on the position of the scapula in abduction postures. Clin Biomech.(Bristol., Avon.). 1999;14(5):309‐314. [DOI] [PubMed] [Google Scholar]
- 19.Forte FC de Castro MP de Toledo JM Ribeiro DC Loss JF. Scapular kinematics and scapulohumeral rhythm during resisted shoulder abduction‐‐implications for clinical practice. Phys Ther Sport. 2009;10(3):105‐111. [DOI] [PubMed] [Google Scholar]
- 20.McQuade KJ Smidt GL. Dynamic scapulohumeral rhythm: the effects of external resistance during elevation of the arm in the scapular plane. J Orthop Sports Phys Ther. 1998;27(2):125‐133. [DOI] [PubMed] [Google Scholar]
- 21.Michiels I Grevenstein J. Kinematics of shoulder abduction in the scapular plane. On the influence of abduction velocity and external load. Clin Biomech (Bristol, Avon). 1995;10(3):137‐143. [DOI] [PubMed] [Google Scholar]
- 22.Pascoal AG van der Helm FF Pezarat CP Carita I. Effects of different arm external loads on the scapulo‐humeral rhythm. Clin Biomech.(Bristol., Avon.). 2000;15 Suppl 1:S21‐S24. [DOI] [PubMed] [Google Scholar]
- 23.Seitz AL McClure PW Finucane S, et al. The scapular assistance test results in changes in scapular position and subacromial space but not rotator cuff strength in subacromial impingement. J Orthop Sports Phys Ther. 2012;42(5):400‐412. [DOI] [PubMed] [Google Scholar]
- 24.Seitz AL McClure PW Lynch SS Ketchum JM Michener LA. Effects of scapular dyskinesis and scapular assistance test on subacromial space during static arm elevation. J Shoulder Elbow Surg. 2012;21(5):631‐640. [DOI] [PubMed] [Google Scholar]
- 25.Agre JC Magness JL Hull SZ, et al. Strength testing with a portable dynamometer: reliability for upper and lower extremities. Arch Phys Med Rehabil. 1987;68(7):454‐458. [PubMed] [Google Scholar]
- 26.Ekstrom RA Soderberg GL Donatelli RA. Normalization procedures using maximum voluntary isometric contractions for the serratus anterior and trapezius muscles during surface EMG analysis. J Electromyogr Kinesiol. 2005;15(4):418‐428. [DOI] [PubMed] [Google Scholar]
- 27.An KN Browne AO Korinek S Tanaka S Morrey BF. Three‐dimensional kinematics of glenohumeral elevation. J Orthop Res. 1991;9(1):143‐149. [DOI] [PubMed] [Google Scholar]
- 28.Karduna AR McClure PW Michener LA Sennett B. Dynamic measurements of three‐dimensional scapular kinematics: a validation study. J Biomech Eng. 2001;123(2):184‐190. [DOI] [PubMed] [Google Scholar]
- 29.Wu G van der Helm FC Veeger HE, et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion‐‐Part II: shoulder, elbow, wrist and hand. J Biomech. 2005;38(5):981‐992. [DOI] [PubMed] [Google Scholar]
- 30.McClure PW Bialker J Neff N Williams G Karduna A. Shoulder function and 3‐dimensional kinematics in people with shoulder impingement syndrome before and after a 6‐week exercise program. Phys Ther. 2004;84(9):832‐848. [PubMed] [Google Scholar]
- 31.McClure PW Michener LA Karduna AR. Shoulder function and 3‐dimensional scapular kinematics in people with and without shoulder impingement syndrome. Phys Ther. 2006;86(8):1075‐1090. [PubMed] [Google Scholar]
- 32.Laudner KG Stanek JM Meister K. The relationship of periscapular strength on scapular upward rotation in professional baseball pitchers. J Sport Rehabil. 2008;17(2):95‐105. [DOI] [PubMed] [Google Scholar]
- 33.Kendall FP McCreary EK Provance PG. Muscles, testing and function: with Posture and pain. 4th ed. Baltimore, Md: Williams & Wilkins; 1993. [Google Scholar]
- 34.Guanche CA Jones DC. Clinical testing for tears of the glenoid labrum. Arthroscopy. 2003;19(5):517‐523. [DOI] [PubMed] [Google Scholar]
- 35.Kim SH Ha KI Han KY. Biceps load test: a clinical test for superior labrum anterior and posterior lesions in shoulders with recurrent anterior dislocations. Am J Sports Med. 1999;27(3):300‐303. [DOI] [PubMed] [Google Scholar]
- 36.Jobe FW Moynes DR. Delineation of diagnostic criteria and a rehabilitation program for rotator cuff injuries. Am J Sports Med. 1982;10(6):336‐339. [DOI] [PubMed] [Google Scholar]