Abstract
Background:
Onychopathies constitute one of the major challenges faced by a dermatologist in terms of its early detection and diagnosis. Utility of dermoscope as a tool for detection is increasing by the day and its use in onychopathies needs to be explored.
Aims:
To study the dermoscopic features of nails in patients of chronic plaque psoriasis.
Materials and Methods:
In a cross-sectional study, a total of 68 patients with chronic plaque psoriasis were recruited. Dermoscopy of nail plate was conducted and were compared with equal number of age and sex matched healthy volunteers.
Results:
Forty-six patients showed dermoscopic findings. Twenty-two patients did not show any dermoscopic findings. Coarse pits (18/46, P < 0.0001), onycholysis (10/46, P < 0.001), oil drop sign (2/46, P = 0.12) and splinter hemorrhages (5/46, P = 0.05) were seen. In addition certain findings of interest were stout, globose, dilated, pink- to red-colored nail bed vessels arranged longitudinally at the onychodermal band surrounded by a prominent halo (9/46, P = 0.01). In contrast, splinter hemorrhages appeared as streaks and were purple in color.
Conclusion:
In a psoriasis patient, dermoscope can be a useful tool to detect early nail involvement in psoriasis and aid in differentiating it from other disorders of nails.
Keywords: Dermoscopy, psoriasis, nail
What was known?
Dermoscope is a handy non invasive instrument used in dermatology.
Use in onychopathies has been established for subungual melanoma.
Psoriasis of nails can be reliably diagnosed at present by histopathology.
Introduction
Psoriasis of nails may affect the nail bed or the nail matrix. The various nail signs in psoriasis are the presence of coarse irregular pits, splinter hemorrhages, subungual hyperkeratosis, oil drop sign, onycholysis etc. These changes are detected on gross examination. By then considerable damage to the nail unit has usually occurred and normal functions are hampered affecting the day to day life of the individual. In this study, we used dermoscope as a tool to detect signs of psoriasis in the nails and to find if any signs can help in early detection of nail affection.
Materials and Methods
The study was conducted in the department of Dermatology, venereology and leprology at K.E.M hospital, Mumbai from September 2013 to November 2014. This study was approved by the Institutional ethics committee of K.E.M Hospital in the month of August 2013. Sixty-eight patients were recruited in the study. All patients were of chronic plaque psoriasis. Other forms of psoriasis were excluded. Equal numbers of age- and sex-matched controls were taken. Patients who had gross visible nail changes were excluded. Patients who only had subtle nail findings, not easily discernible by naked eye, were taken. Detailed history including the age, sex, duration of the disease and details of any past topical or systemic treatment was noted. Cutaneous and systemic examination of the patient was done. Clinical photographs of the nails were taken. Examination of the nail was done using a contact dermoscope (Heine's delta 20) and a video dermoscope. Oily medium such as liquid paraffin or gel was used for interface in case of a contact dermoscope. Video dermoscope of the type ultracam TLS manufactured by dermaindia was used. Clinical photographs of the nails were taken using a canon powershot G12 camera. The nails were examined by the video dermoscope on a white light, polarized light. The parts of nail that were examined were the nail plate, proximal and lateral nail fold, cuticle and the subungual region. The findings were appreciated well through a hand held dermoscope with an oily medium at the interface or using a video dermoscope with a polarized light. The statistical analysis was done using the Fishers exact test with the mid-P method.
Results
Sixty-eight patients were analyzed in the present study. Out of which, dermoscopic findings were seen in 46 patients. Twenty-two patients did not show any findings [Table 1]. Out of the 46 patients who had findings, the mean age was 38.36 years with a range of 13 to 66 years. Mean average duration of the disease is 2.69 years with duration ranging from 2 months to 10 years. Thirty-four males and 12 females comprised the study population.
Table 1.
Frequency of patients showing findings
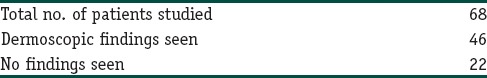
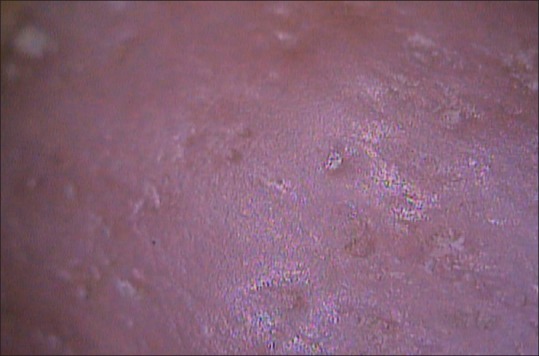
Of the various findings, irregular pits were the most common. It was seen in 18 out of 46 patients in the study population [Table 2] and in 2 persons in the control group (P < 0.0001) [Figure 1]. Onycholysis, most commonly presenting as distal lateral onycholysis, was present in 10 patients and in 1 in the control group (P < 0.001) [Figures 2 and 3]. An oil drop sign was seen in two patients and none in the control group.
Table 2.
Frequency of dermoscopy findings
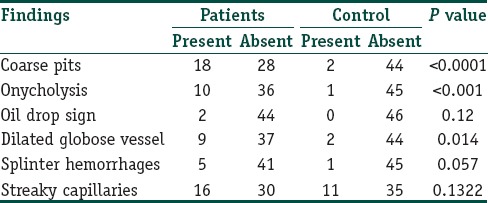
Figure 1.
Coarse irregular pits of various sizes and shapes (40x)
Figure 2.

Onycholysis occurring at the distal lateral border
Figure 3.
Onycholysis appearing as reddish orange discoloration through a video dermoscope (40x)
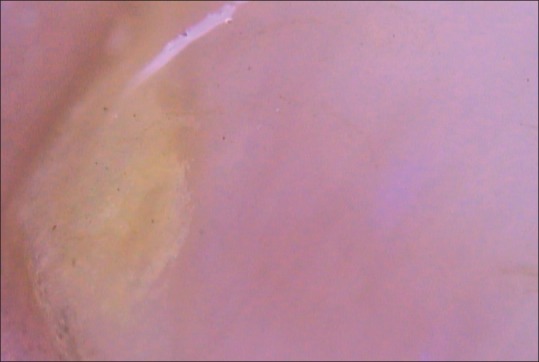
Subclinically, the following findings of interest were noted: Dilated globose vessels at the onychodermal band were a consistent finding seen in nine patients and were statistically significant. (P < 0.01). Stout, globose, dilated, red to maroon-appearing nail bed vessels arranged longitudinally at the onychodermal band were surrounded by a prominent halo [Figures 4 and 5]. Splinter hemorrhages, manifesting as purplish stain were seen in five patients (P = 0.057) [Figure 6]. In 16 patients, rather than fusiform dilatation, the vessels were visible as streaks through the nail plate.
Figure 4.
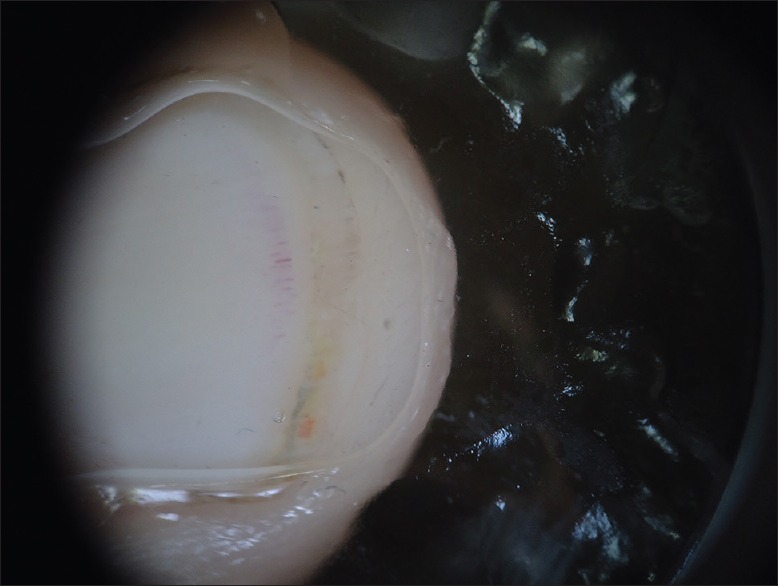
Dilated globose vessels at the onychodermal band (20x) through a contact dermoscope
Figure 5.

Dilated vessels with a prominent halo as seen through a non-contact dermoscope in a polarized light (40x)
Figure 6.
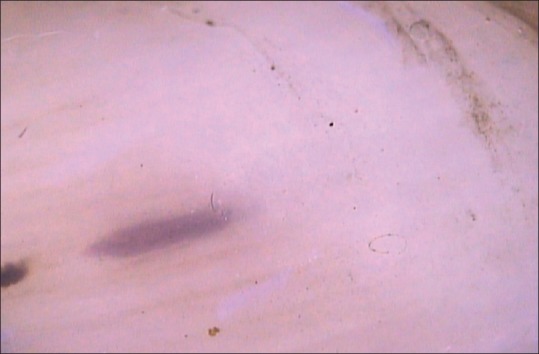
Splinter hemorrhages appearing as purple-colored streaks (40x)
Discussion
The dermoscopic features described in literature for nail psoriasis are pitting, onycholysis, salmon spot, oil spot, splinter hemorrhages and subungual hyperkeratosis.[1]
In our patients, the most common findings seen in nails were small irregular pits over the nail plate. They were seen as indentations over the nail plate and are irregular, both in size and shape. Fine pits could be appreciated well with a dermoscope.[2] Pits results from defective nail formation in the proximal portion of the nail matrix.[3] The keratinization of the stratum corneum of the proximal nail matrix is disrupted leading to formation of parakeratotic cells.[4] These columns of loose parakeratotic cells fall off leading to deep and coarse pits later.[2,5,6]
Next common finding observed in our study was onycholysis. Onycholysis is due to involvement of the nail bed or hyponychium. It can also occur due to extension of an oil spot distally.[7] The separation of nail plate from the nail bed allows air to enter inside giving a white appearance.[8] Serum can exude and accumulate below the nail plate giving it a yellowish appearance.[9] It was seen in 10 patients occurring at the distal lateral margin. The nail appears whitish in color as compared to the pale pink appearance of the normal nail. There is a reddish orange- to brownish-colored band separating the area of onycholysis with the normal nail.[7,10,11,12] This feature can be helpful in differentiating it from traumatic onycholysis. In traumatic onycholysis, the line of detachment of the plate from the bed is regular and smooth, and is surrounded by a normally pale pink bed. There is no reddish orange band seen in traumatic onycholysis.[11]
Nine patients showed bright red to dusky colored dilated vessels arranged parallel over the onychodermal band of the nail plate. They were seen close to the free distal end of the nail plate. They appear as fusiform dilatation surrounded by a prominent halo. They can be appreciated well with either a video dermoscopeor a hand held dermoscope.[7,12] In our study it was seen to be more common in psoriatic patients as compared to general population. In 2012, Piraccini et al., described dilatation and tortuosity of the nail bed vessels in psoriatic patients which were appreciated by examining the hyponychium. However, it was not appreciated in our study due to the pigmentation of the skin in the Indian population.[10] In 2008, Iorizzo et al., showed regular red dots in the hyponychium corresponding to the dilated tortuous vessels in the nail beds of patients with psoriasis. They compared this finding with hyponychium of normal persons and with patients of lichen planus. It was seen that the vessels were less tortuous and reduced in number in patients of lichen planus. Moreover, they showed that capillary density is positively correlated with the severity of the condition. This study also showed that quantitative analysis of the capillaries correlates with response to treatment. In this study, following 3 months of topical treatment with calcipotriol, a reduction in the number of capillaries was found in the patients.[11]
Oil drop sign was seen in two patients in the present study. It occurs due to focal nail bed parakeratosis leading to focal onycholysis. Similar to onycholysis, this area shows a red brown- colored margin separating it from the normal pink nail.[3,7,13]
In our study, splinter hemorrhages were seen in five patients. They were visible as longitudinal purple to black streaks. Recent splinter hemorrhages were purple in color, whereas long-standing splinter hemorrhages were darker and appeared blackish in color. Splinter hemorrhages are the result of bleeding in the capillaries of the nail bed. They were seen as marks that run longitudinally in the direction of nail growth, and are caused by the successive incorporation of blood in the ventral nail plate.[2,7,10]
In 16 patients, nail bed capillaries were visible through the nail plate as bright red streaks. This feature was seen in 11 controls and was not statistically significant. Such lines have also been described in people engaged in intense manual activity.[11]
Conclusion
Dermoscopy is a noninvasive, quickly applied and inexpensive test that may aid diagnosis of nail psoriasis in inconclusive cases. Subclinical lesions of nail psoriasis can be appreciated well with the help of a dermoscope and appropriate treatment can be instituted.
What is new?
Dermoscope is a handy non invasive instrument used in dermatology.
Use in onychopathies has been established for subungual melanoma.
Psoriasis of nails can be reliably diagnosed at present by histopathology.
Footnotes
Source of support: Nil
Conflict of Interest: Nil.
References
- 1.Nakamura RC, Costa MC. Dermatoscopic findings in the most frequent onychopathies: Descriptive analysis of 500 cases. Int J Dermatol. 2012;51:483–5. doi: 10.1111/j.1365-4632.2010.04720.x. [DOI] [PubMed] [Google Scholar]
- 2.Farias DC, Tosti A, Chiacchio ND, Hirata SH. Dermoscopy in nail psoriasis. An Bras Dermatol. 2010;85:101–3. doi: 10.1590/s0365-05962010000100017. [DOI] [PubMed] [Google Scholar]
- 3.Langley RG, Krueger GG, Griffiths CE. Psoriasis: Epidemiology, clinical features, and quality of life. Ann Rheum Dis. 2005;64:18–23. doi: 10.1136/ard.2004.033217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jiaravuthisan MM, Sasseville D, Vender RB, Murphy F, Muhn CY. Psoriasis of the nail: Anatomy, pathology, clinical presentation, and a review of the literature on therapy. J Am Acad Dermatol. 2007;57:1–27. doi: 10.1016/j.jaad.2005.07.073. [DOI] [PubMed] [Google Scholar]
- 5.Zaias N. Psoriasis of the nail unit. Dermatol Clin. 1984;2:493–505. [Google Scholar]
- 6.Zaias N, editor. 2nd ed. London: Appleton and Lange; 1990. Nail in Health and Disease. [Google Scholar]
- 7.Dogra A, Arora AK. Nail psoriasis: The journey so far. Indian J Dermatol. 2014;59:319–33. doi: 10.4103/0019-5154.135470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McGonagle D, Palmou Fontana N, Tan AL, Benjamin M. Nailing down the genetic and immunological basis for psoriatic disease. Dermatology. 2010;221:15–22. doi: 10.1159/000316171. [DOI] [PubMed] [Google Scholar]
- 9.Fleckman P. Structure and function of the nail unit. In: Scher RK, Daniel CR 3rd, editors. Nails: Diagnosis, therapy, surgery. 3rd ed. Philadelphia: Elsevier Saunders; 2005. pp. 13–26. [Google Scholar]
- 10.Piraccini BM, Bruni F, Starace M. Dermoscopy of non-skin cancer nail disorders. Dermatol Ther. 2012;25:594–602. doi: 10.1111/j.1529-8019.2012.01521.x. [DOI] [PubMed] [Google Scholar]
- 11.Iorizzo M, Dahdah M, Vicenzi C, Tosti A. Videodermoscopy of the hyponychium in nail bed psoriasis. J Am Acad Dermatol. 2008;58:714–5. doi: 10.1016/j.jaad.2007.11.026. [DOI] [PubMed] [Google Scholar]
- 12.Micali G, Lacarrubba F. Possible applications of videodermatoscopy beyond pigmented lesions. Int J Dermatol. 2003;42:430–3. doi: 10.1046/j.1365-4362.2003.01802.x. [DOI] [PubMed] [Google Scholar]
- 13.Kouskoukis CE, Scher RK, Ackerman AB. The ‘oil drop’ sign of psoriatic nails. A clinical finding specific for psoriasis. Am J Dermatopathol. 1983;5:259–62. doi: 10.1097/00000372-198306000-00012. [DOI] [PubMed] [Google Scholar]


