The patient is a 6-month-old infant who presented with annular erythematous plaques with mild scaling on the face, especially forehead and around the eyes, gradually spreading to the neck, trunk and extremities since 4 months ago [Figures 1-3]. Its general health has been good and he had no problems at birth. The patient has been the first child of the family, with a history of pain in the joints of hand in the mother from about 3 years ago without citing a specific diagnosis. Skin biopsy was taken from the infant, which showed vacuolar changes in the epithelial basement membrane in dermoepidermal junction and in the epithelial junction of the appendages with necrotic keratinocytes, perivascular and periadnexal infiltrates with lymphocyte predominance and precipitation of dermal mucin [Figures 4 and 5].
Figure 1.

Annular erythematous plaques on the face
Figure 3.

Annular erythematous plaques on the lower extremities
Figure 4.
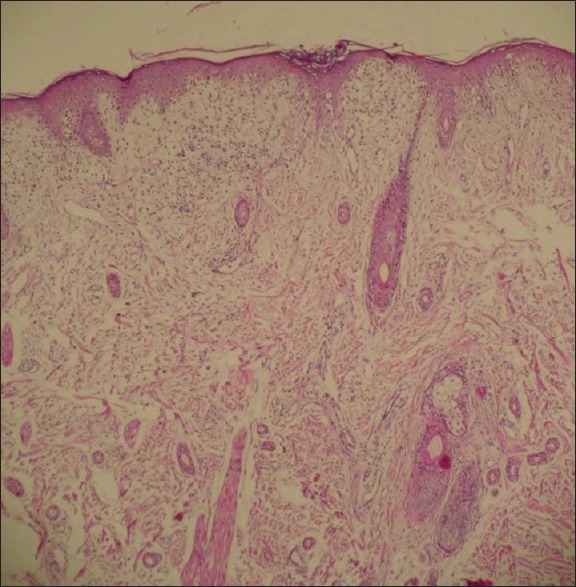
Hydropic degeneration of basal keratinocytes, dermal edema and a superficial lymphohistiocytic chronic inflammatory cell infiltrate (H and E, ×40)
Figure 5.

Basal vacuolar change with occasional civatte bodies (H and E, ×100 and ×400)
Figure 2.

Annular erythematous plaques on the trunk
Question
What is your diagnosis?
Answer
Neonatal lupus erythematosus.
Neonatal lupus erythematosus (NLE) is an autoimmune disease caused by in utero transfer of maternal antibodies to the fetus through the placenta, with an incidence between 1 in 12,500 and 1 in 20, 000 live births. NLE has a higher incidence in female and premature newborns.[1] This disease occurs in children of women with systemic lupus erythematosus, Sjögren's syndrome and other collagen vascular diseases, but about half of the mothers are asymptomatic at the time of diagnosis of their son's disease, and are only characterized by positive Anti Ro test.[2] The characteristic serologic finding of this disease is the maternal autoantibody of Anti Ro/SSA or Anti La/SSB, or both,[1] with Ro almost seen in all patients and La in a fewer cases.[1] U1RNP is involved in very few cases of NLE, usually associated with atypical cutaneous lesions without cardiac or systemic abnormality.[1] The main clinical manifestations of this disease include skin, heart, blood, liver and neurological manifestations, of which skin and heart problems are more common.[1,3]
Cutaneous lesions are common in NLE. These lesions may be present at birth, but are usually found several weeks after birth.[1] Morphology of the lesions presents as annular erythematous plaques with central erasure with or without delicate flakes similar to subactue cutaneous lupus erythematosus lesions.[1,4,5] The face and scalp are almost always affected, but the lesions can be seen anywhere in the body.[6] Extensive confluent erythema, especially around the eyes, causes the raccoon sign.[1] Cutaneous lesions of NLE can be caused or aggravatedby ultraviolet (UV) or phototherapy, but because the skin lesions of NLE can exist at birth or occur in covered areas, UV does not seem to be necessary for incidence of the lesions.[1] The rashes are completely eliminated within 1 year without leaving scars. With respect to spontaneous recovery of cutaneous lesions, there is no need for treatment, but the use of topical steroids and protection from sun are useful. Cutaneous lesions are not expected after the first year of life; in such cases, the diagnosis must be reviewed.[4]
Biopsy of the skin lesions tends to be similar to SCLE rash, and is seen in two forms: Desquamative erythmatous and wheal-like lesions. The main findings include vacuolar changes in the epithelial basement membrane in the dermoepidermal junction and in the epithelial junction of appendages with necrotic keratinocytes, perivascular and periadnexal infiltrates with lymphocyte predominance and precipitation of dermal mucin.[7]
The most common cardiac finding is third-degree congenital heart block typically beginning in the second or third trimester of pregnancy,[5] caused by fibrosis and calcification of atrioventricular node[4,5] that is irreversible.[4] The infant is often identified by bradycardia or arrhythmia during pregnancy in routine screening by a gynecologist.[1] Most patients require pacemaker.[3] The risk of cardiac involvement in the first child of Anti Ro positivemother is 1-2%, and is 18% in the second child.[2] Fetal echocardiography has been recommended from 16 weeks of pregnancy in all Anti Ro positivewomen.[2]
Thrombocytopenia occurs in 10% of NLE patients, which is transient and not usually clinically significant.[5] Neutropenia, hemolytic anemia, pancytopenia and aplastic anemia have also occasionally been reported.[8]
About 10% of infants have liver involvement with clinical symptoms of conjugated hyperbilirubinemia, elevated transaminase, cholestatic hepatitis, hepatic failure, hemochromatosis, hepatomegaly and splenomegaly.[2,8] Increased transaminases are usually transient.[8]
NLE is suspected in every infant born with congenital heart block or afflicted within the first year of life with cutaneous erythematous rashor telangiectasia.In these cases, if the mother has already given birth to a child suffering from NLE, has autoimmune disease or symptoms suggestive of an autoimmune disease, the diagnostic will be suspected.The diagnosis is usually based on clinical findings and serology for detection of auto antibodies in mother and infant.[7] Complete physical examination of the infant may reveal additional findings indicating heart, liver and blood involvement. Laboratory tests including electrocardiogram, complete blood count, platelets, Anti Ro, La and U1RNP antibody serology, should be done. Biopsy of skin lesions can show characteristic findings of lupus erythematosus, but often biopsy is not necessary for diagnosis.[7] Because of the absence of permanent symptoms in mother and variability in cutaneous lesions in infants, in some cases, histopathological examination may be necessary to confirm diagnosis and rule out other similar lesions.[7]
Points
NLE is an uncommon rash in neonates and infants, which can give rise to cardiac and hepatic problems in children. As it is uncommon in neonates of asymptomatic mothers, it may be misdiagnosed as other causes of rash and, therefore, we lose the gold time for assessment of these children for systemic involvement
NLE is suspected in every infant born with congenital heart block or afflicted within the first year of life with cutaneous erythematous rashor telangiectasia.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Wisuthsarewong W, Soongswang J, Chantorn R. Neonatal lupus erythematosus: Clinical character, investigation, and outcome. PediatrDermatol. 2011;28:115–21. doi: 10.1111/j.1525-1470.2011.01300.x. [DOI] [PubMed] [Google Scholar]
- 2.Perez MF, Torres ME, Buján MM, Lanoël A, Cervini AB, Pierini AM. Neonatal lupus erythematosus: A report of four cases. An Bras Dermatol. 2011;86:347–51. doi: 10.1590/s0365-05962011000200021. [DOI] [PubMed] [Google Scholar]
- 3.Lee LA. Neonatal lupus erythematosus: Clinical findings and pathogenesis. J Investig Dermatol Symp Proc. 2004;9:52–6. doi: 10.1111/j.1087-0024.2004.00827.x. [DOI] [PubMed] [Google Scholar]
- 4.Lee LA. Cutaneous lupus in infancy and childhood. Lupus. 2010;19:1112–7. doi: 10.1177/0961203310370347. [DOI] [PubMed] [Google Scholar]
- 5.Lee LA. Neonatal lupus: Clinical features and management. Paediatr Drugs. 2004;6:71–8. doi: 10.2165/00148581-200406020-00001. [DOI] [PubMed] [Google Scholar]
- 6.Neiman AR, Lee LA, Weston WL, Buyon JP. Cutaneous manifestations of neonatal lupus without heart block: Characteristics of mothers and children enrolled in a national registry. J Pediatr. 2000;137:674–80. doi: 10.1067/mpd.2000.109108. [DOI] [PubMed] [Google Scholar]
- 7.Peñate Y, Guillermo N, Rodríguez J, Hernández-Machín B, Montenegro T, Afonso JL, Borrego L. Histopathologic characteristics of neonatal cutaneous lupus erythematosus: Description of five cases and literature review. JCutanPathol. 2009;36:660–7. doi: 10.1111/j.1600-0560.2008.01136.x. [DOI] [PubMed] [Google Scholar]
- 8.Silverman E, Jaeggi E. Non-cardiac manifestations of neonatal lupus erythematosus. Scand J Immunol. 2010;72:223–5. doi: 10.1111/j.1365-3083.2010.02443.x. [DOI] [PubMed] [Google Scholar]


