Case
A 39-year-old female presented with foul smelling, variously sized, painless, large, asymptomatic tumor-like lesions on neck, chest, back, vulva, thighs, buttocks and lower legs since last 6-7 months. The lesions started as pea sized papules, gradually enlarged in size with subsequent foul smelling discharge [Figures 1a and b].
Figure 1.

(a) Variously sized, large, flesh colored, coalescing tumor-like giant lesions on lower back and posterior thigh region. (b) Large nodular skin colored lesions in the vulval region of the patient
She had pallor but no icterus, clubbing, cyanosis or wasting were seen. There was no hepato-splenomegaly. Local examination revealed multiple, discreet, sessile, verrucous, skin-colored, discharging papulo-nodular coalescing lesions on the above sites. On pressing the lesions, extremely foul smelling whitish cheesy material was seen oozing from them [Figure 2a and b]. The microscopic examination of caseous cheesy material showed homogeneous inclusion bodies within the keratinocytes.
Figure 2.

(a) Giant lesions on gluteal area. (b) Milky white fluid oozing from lesions by slightly pressing the lesions
The biopsy was done and histopathology picture is as below [Figure 3] showing hyperplastic epidermis with cells showing intracytoplasmic inclusions.
Figure 3.
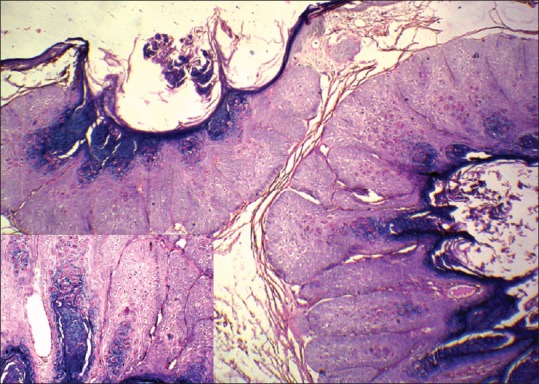
Histopathology picture showing lobules of keratinocytes with epidermal hyperplasia and large eosinophilic intracytoplasmic inclusion bodies (H and E, original magnification ×20). Inset shows close up of inclusion bodies (H and E, original magnification ×100)
She was diagnosed to be HIV positive by ELISA method with CD4+ count to be 67 cells/mm3.
Question
What is your diagnosis?
Answer
The diagnosis in this case was; Giant molluscum contagiosum in a setting of immune suppression with positive ’Bateman's sign’.
Discussion
Molluscum contagiosum has been reclassified as a type member in a separate genus Molluscipox virus by International committee on Taxonomy of Viruses (ICTV) in 1991. It targets epidermal keratinocytes and replication occurs within the cytoplasm of infected cells, generating the characteristic Henderson Patterson (HP) cytoplasmic inclusion bodies.
The association between HIV/AIDS and molluscum infection was first reported in 1983 when it was noted by Reichart CM et al.,[1] that 2 out of 10 patients with AIDS had MCV infection on autopsy. In contrast, in HIV-seronegative adults, MC lesions are usually genital; lesions in HIV individuals most often involve the face, eyelid, neck and trunk. Because this distribution is similar to that seen in children, in whom the spread is thought to occur through fomites or casual contact, transmission in HIV-infected patients does not appear to be solely by sexual contact. Other states associated with widespread MCV are sarcoidosis, use of immunosuppressants, topical steroids and also topical cacineurin inhibitors suggesting a role of cell mediated immunity in control of infection.
In HIV-infected patients, the lesions are more widespread, larger (giant > 10mm in diameter) and resistant to conventional therapy. Often they do not manifest classic pathognomonic morphology and may lack the central umbilication or delling. The differential diagnoses to be considered are cryptococcosis, histoplasmosis, coccidioidomycosis, Penicillium marneffei infection, epitheliomas, basal cell carcinoma and sebaceous hyperplasia. Diagnosis is mainly clinical but in atypical cases as in this case, squash preparation, fine-needle aspiration cytology and histopathology may be done. Molecular diagnostics by in situ hybridization and PCR and MCV Elisa are additional tools used for unclear cases. Topical imiquimod, topical and systemic cidofovir, intralesional interferon-α, photodynamic therapy and electron beam therapy have been found to be variously effective. The introduction of HAART can elicit resolution, but an increased incidence has also been reported. Depsipeptides, a new class of naturally occurring bioactive molecules have immunomodulatory, antiviral and antitumor activities. Pulsed dye laser is a quick, bloodless and effective modality of treatment with minimal side effects.
This case is very unique in terms of size; the largest lesion being on posterior thigh region measuring about 4.5 × 3.5 cm in diameter [Figure 1] with other lesions varying in size between 0.5 and 3.0 cm in diameter. The typical observation of Bateman that the milky fluid is emanated from the lesion on slightly pressing the lesions was also characteristically present. The same has not been previously documented in literature although a mention of white curdy discharge is done by Brown et al.[2] Therefore, we also propose ’Bateman's Sign’ to be elicited in giant molluscum contagiosum with or without immunosuppression, in future, in honor of Dr Bateman[3] who first gave a mention of this finding.
The presence of lesions in young adults on face, eyelids, trunk and genital should alert the clinician for possibility of HIV infection. Also, HIV-1-positive patients with verrucous MC and giant MC are in late stages of the disease with low CD4+ counts and high viral load.
Take home learning points:
Molluscum contagiosum lesions are a cutaneous marker for advanced HIV infection (CD4+ T-cell count less than 100/μL)
Large, confluent, giant lesions suggest advanced HIV infection and may lack the characteristic umbilication
Large lesions may occasionally show foul smelling discharge, initially described by Bateman
Presence of lesions in young adults on face, eyelids, trunk and genital should alert the clinician for possibility of HIV infection
Diagnosis can be rapid and simple by either crush preparation or staining of this curdy white discharge by Giemsa method
After initiation of ART, these lesions show signs of resolution.
References
- 1.Reichert CM, O’Leary TJ, Levens DL, Simrell CR, Macher AM. Autopsy pathology in the acquired immune deficiency syndrome. Am J Pathol. 1983;112:357–82. [PMC free article] [PubMed] [Google Scholar]
- 2.Brown J, Janniger CK, Schwartz RA, Silverberg NB. Childhood molluscum contagiosum. Int J Dermatol. 2006;45:93–9. doi: 10.1111/j.1365-4632.2006.02737.x. [DOI] [PubMed] [Google Scholar]
- 3.Bateman F. Molluscum contagiosum. In: Shelley WB, Crissey JT, editors. Classics in dermatology. Springfield (IL): Charles C Thomas Publisher; 1953. p. 20. [Google Scholar]


