Abstract
Aim
Smoking is the one of the most preventable causes of death worldwide. Dental professionals may play an important role in anti-smoking campaigns. The aim of this study was to evaluate current knowledge of and attitudes toward smoking and its cessation among dental professionals.
Materials and methods
This questionnaire-based study was carried out among general dental practitioners (GDPs) and dental students in Saudi Arabia. The questionnaire was used to collect data on sociodemographic characteristics, knowledge, and attitudes toward tobacco use and cessation. Data were analyzed using SPSS software (version 18.0; IBM) and the Mann–Whitney U-test, with a significance level of p < 0.001.
Results
A total of 342 participants (130 GDPs, 212 dental students) with the mean age of 24 (standard deviation, 5) years participated in the study. One-third (33.8%, n = 44) of GDPs and 30.2% (n = 64) of dental students were smokers; small percentages (GDPs, 9.1% [n = 4]; dental students, 7.8% [n = 5]) were heavy smokers. The majority of participants rated both smoking cessation and prevention together as a very important preventive measure. Families were rated as the most important factor responsible for smoking cessation, whereas general practitioners were rated as the most important factor for providing assistance with cessation.
Conclusion
More meaningful participation of dental professionals in tobacco cessation is needed, with implications for related curriculum changes.
Keywords: Smoking, Tobacco cessation, Knowledge, Students, Questionnaire study
1. Introduction
Tobacco use is among the most preventable causes of disease and premature death worldwide (USDHHS, 2010). The detrimental effects of tobacco use on oral health have been well documented in studies focusing on changes in the oral mucosa (Warnakulasuriya, 2005; Warnakulasuriya et al., 2005) and periodontal tissues (Johnson and Slach, 2001; Palmer et al., 2005; Tonetti, 1998). Substantial evidence indicates that tobacco cessation not only reduces the prevalence of a range of diseases, but also limits their progression and improves treatment outcomes (Preshaw et al., 2005).
Dental professionals play a significant role in identifying smokers, as they may notice intraoral signs such as odor, tooth stains, and oral hygiene problems earlier than other healthcare professionals; they are thus in a better position to offer preventive care (Ramseier et al., 2006, 2010). In addition, they have access to protocols that encourage smoking cessation and pharmaceutical support if needed (Wiener and Wiener Pla, 2011). As a result, dentists’ knowledge about tobacco use and various methods available for its cessation is crucial, along with increased involvement of dental professionals in anti-smoking campaigns to minimize smoking-related harmful effects (Ehizele et al., 2011).
Patients who visit dental clinics routinely have little interaction with healthcare professionals about tobacco use and related hazardous effects. This factor has been attributed to the lack of practice, time, and resistance on the part of the patients, as well as insufficient knowledge and confidence among oral healthcare professionals in providing preventive measures (Rikard-Bell et al., 2003; Rosseel et al., 2011). To minimize this communication gap, a strategy involving employment of dental professionals in preventive anti-smoking programs and improvement of education and counseling in tobacco cessation should be considered. As a first step, data have been collected from various countries on the knowledge and attitudes of dental professionals, including dental students, regarding tobacco use and cessation (Alomari et al., 2006; Barrieshi-Nusair et al., 2006; Dumitrescu, 2007; Huang et al., 2011; Smith and Leggat, 2007).
In Saudi Arabia, few studies have addressed this problem (Abdulghani et al., 2013; Al-Haqwi et al., 2010; Azhar and Alsayed, 2012; Kujan et al., 2013) and research data related to the role of dental professionals in tobacco cessation interventions are sparse. The aim of the present study was to assess the knowledge and attitudes of Saudi dental professionals regarding tobacco use, specifically smoking, and smoking cessation.
2. Materials and methods
This cross-sectional study was conducted over a 6-month period from March to August 2013 in Riyadh, Kingdom of Saudi Arabia, using a self-administered, two-page structured questionnaire derived from the Global Tobacco Survey (http://www.cdc.gov/tobacco/global/gats/questionnaire/index.htm [updated 25 May 2009, accessed June 2009]). The study population comprised dental undergraduate students and general dental practitioners (GDPs). Questionnaires were distributed to students during routine lectures and to GDPs at their workplaces. Each questionnaire was accompanied by a cover letter explaining the purpose of the study and providing specific instructions for questionnaire completion. Standard procedures of informed consent were used, including the protection of participants’ anonymity and confidentiality.
Questionnaire items solicited data on participants’ sociodemographic characteristics (age, gender, residence type, academic year of study) and knowledge and attitudes regarding smoking and its cessation. Eight questions were used to assess participants’ knowledge about the hazardous effects of tobacco use and attitudes toward the role of dental professionals in smoking cessation campaigns. Nine questions focused on participants’ attitudes toward smoking, and five questions were designed to collect data about personal and family smoking habits. The questionnaire was pretested to ensure that all questions were clear and understandable to participants. The institutional research and ethics committee approved this study.
Data were analyzed using SPSS (version 18.0; IBM Corporation, Armonk, NY, USA). Responses were coded numerically to facilitate data entry. Comparison of smoking characteristics among the GDPs and dental students was performed and the data was analyzed using the Mann–Whitney U-test, with the level of significance set to p < 0.001.
3. Results
A total of 342 subjects with the mean age of 24 (standard deviation [SD], 5) years completed the questionnaire. The response rate was 86.5%. Of the participants, 130 (mean age, 30 [SD, 5] years) were GDPs and 212 (mean age, 21 [SD, 3] years) were dental students. Among the GDPs and dental students, 63.8% and 75.5% of participants, respectively, were male.
3.1. Smoking behavior
One-third (33.8%, n = 44) of GDPs and 30.2% (n = 64) of dental students reported that they smoked when asked about their personal smoking habits (Table 1). Tobacco users were classified as; Occasional smokers: those who smoked 1–3 days per week; Regular smokers: those who smoked every day; Heavy smokers: those who smoked one pack of cigarette or more a day. Most (n = 30) smokers among the GDPs were regular smokers, reporting that they usually smoked on a daily basis; in contrast, most (n = 50) dental students who smoked did so less frequently, on average 1–3 days a week. Small percentages (GDPs, 9.1% [n = 4]; dental students, 7.8% [n = 5]) of these respondents were heavy smokers, smoking one pack of cigarettes or more per day. The majority of participants in both groups were non-smokers, and no significant difference was noted between groups.
Table 1.
Comparison of smoking characteristics among GDPs and dental students.
| Variables | GDPs (n = 44) | Dental students (n = 64) |
|---|---|---|
| Smoking prevalence (in last month) | ||
| 1–7 days | 8 | 10 |
| 8–20 days | 6 | 50 |
| Every day | 30 | 4 |
| Frequency of smoking (per day) | ||
| 1–10 cigarettes | 35 | 54 |
| 11–20 cigarettes | 5 | 5 |
| >20 cigarettes | 4 | 5 |
| Age of initiation of smoking | ||
| <16 years | 4 | 20 |
| 16–18 years | 28 | 40 |
| >18 years | 12 | 4 |
| Giving up smoking | ||
| Tried at least once | 3 | 5 |
| Never tried | 41 | 59 |
GDPs and dental students who smoked reported that they were 15–19 years old when they acquired a smoking habit. However, dental students started smoking earlier than GDPs. Only 6.8% of GDPs and 7.8% of dental students who smoked reported that they had tried to quit smoking at least once.
3.2. Attitudes toward tobacco use and cessation
Sixty-two percent of GDPs and 67% of dental students rated both smoking cessation and prevention together as a very important preventive measure; others perceived either smoking cessation or prevention as important. Smoking prevention was rated by 32% of GDPs and 23% of dental students.
When asked about the hazardous effects of smoking on general health, the majority of participants identified oral cancer and lung cancer as the most common consequences of smoking (Table 2). Overall, responses were similar in the two groups; dental students, however, rated oral cancer, lung cancer, hypertension, heart attack, and impotence significantly higher than their counterparts. The majority of participants rated stress and social influence as the most important factors influencing smoking initiation, and more than 40% of participants identified peer pressure and substitute activity as such factors (Table 3).
Table 2.
Smoking-related health risks as reported by the participants.
| All |
GDPs |
Dental students |
Mann–Whitney U test | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | Significance | |
| Oral cancer | 303 | 88.59 | 107 | 82.30 | 196 | 92.45 | 0.005 |
| Lung cancer | 320 | 93.56 | 111 | 85.38 | 208 | 98.11 | <0.001 |
| Heart attack | 277 | 80.99 | 105 | 80.76 | 172 | 81.13 | 0.933 |
| Preterm birth | 232 | 67.83 | 78 | 60.00 | 154 | 72.64 | 0.015 |
| Gastric cancer | 129 | 37.71 | 40 | 30.76 | 89 | 41.98 | 0.038 |
| Periodontal diseases | 238 | 69.59 | 90 | 69.23 | 148 | 69.81 | 0.909 |
| Hypertension | 216 | 63.15 | 71 | 54.61 | 145 | 68.39 | 0.010 |
| Arteriosclerosis | 284 | 83.04 | 108 | 83.07 | 176 | 83.01 | 0.988 |
Table 3.
Main factors influencing smoking initiation.
| Altogether |
GDPs |
Dental students |
||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Stress | 207 | 60.52 | 71 | 54.61 | 136 | 64.15 |
| Risk taking behavior | 184 | 53.80 | 62 | 47.69 | 122 | 57.54 |
| Social impact | 177 | 51.75 | 50 | 38.46 | 127 | 59.90 |
| Fashionable to smoke | 114 | 33.33 | 27 | 20.76 | 87 | 41.03 |
| Leisure activity | 208 | 60.81 | 76 | 58.46 | 134 | 63.20 |
| Unknown | 1 | 0.29 | 0 | 0.0 | 1 | 0.47 |
When asked about the role of education in relation to smoking cessation and prevention, 64% of GDPs and 78% of dental students denied receiving any relevant information regarding smoking cessation during their years of study. However, more than 50% of GDPs and dental students stated that they expected to have received smoking-related information.
Responsibility regarding smoking cessation assistance was enquired in two questions. The first question focused on identifying those responsible for providing it and grading them by importance. The majority of participants rated family as the most important factor. General practitioners, peer groups, and schools were also reported to play a role in smoking cessation (Fig. 1). The second question explored participants’ attitudes towards factors that may assist in smoking cessation; respondents in both groups identified general practitioners, followed by family members and specialists, as the primary providers of counseling (Fig. 2).
Figure 1.
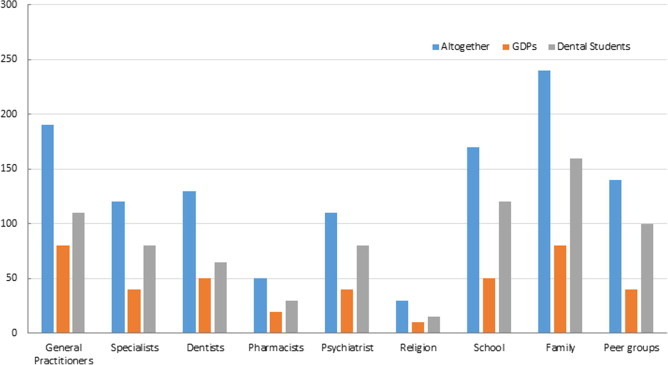
Factors rated by the participants to be responsible for smoking cessation.
Figure 2.
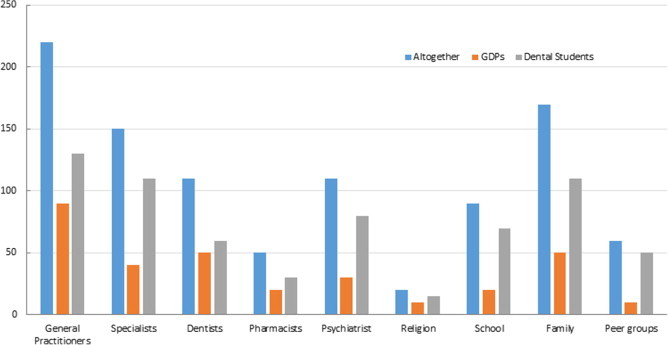
Factors reported by the participants to currently assist in smoking cessation.
Lastly, the participants were asked about their readiness to provide assistance to patients who want to quit smoking. Forty-three percent of GDPs and 52% of dental students responded positively in providing the smoking cessation assistance.
4. Discussion
To our knowledge, this study is the first to document the knowledge, attitudes, behavior, and perceived effectiveness and barriers regarding tobacco use and cessation simultaneously among dental professionals in Saudi Arabia. Tobacco use and related health impacts pose a significant problem globally, and tobacco use is among the leading causes of morbidity and mortality. Studies have highlighted the need for involvement of various healthcare professionals in the fight against tobacco use (Murthy and Saddichha, 2010). Dentists can play a pivotal role in providing assistance to patients in terms of smoking cessation and prevention.
The number of smokers in our study was expectedly small, in line with other reports of smoking prevalence among healthcare professionals (Secker-Walker et al., 1994). Given this small number of smokers, any observed significant relationship based on smoking status should be viewed with caution. The majority of participants among the smoker group were male (81.5%, n = 88), perhaps reflecting the greater freedom of males in terms of individual behavior in Arab culture, which may make men more likely than women to indulge in smoking (Ertas, 2007).
We found that the majority of dental students who smoked were occasional smokers, smoking on only a few days per week. These results are in line with international trends; for example, an increase in the number of occasional smokers and decrease in the number of regular smokers in the USA have been reported (Centers for Disease & Prevention, 2011).
In our study, the common age of smoking initiation was 15–19 years among both GDPs and dental students. The 2011 General Lifestyle Survey of adult smokers revealed that almost two-fifths (40%) had started smoking regularly before the age of 16 (Office for National Statistics, 2013). The main reason for the initiation of a smoking habit at this early age could be the common practice among adolescents of imitating the behavior of their friends (Conrad et al., 1992; Tyas and Pederson, 1998; Zahid and Qidwai, 2005). Aggressive marketing of tobacco products, smoking by parents, peer pressure, availability and price of tobacco products, and lack of behavioral skills to resist tobacco offers are other factors that may contribute to smoking initiation at an early age.
Encouragingly, both dental students and GDPs reported favorable knowledge and attitudes regarding the hazardous effects of smoking on general health. Stress was rated as the most important factor contributing to smoking. Other studies have also reported a strong association between stress and smoking, especially during academic examination periods (Dudas et al., 2005; Piko et al., 1996). Although both GDPs and dental students rated family as the main factor responsible for support and assistance in smoking cessation, many believed that significant support and assistance could also come from general practitioners. Unfortunately, only about 50% of GDPs and dental students reported readiness to provide support and assistance in smoking cessation to patients, which emphasizes the need for education and motivation of dental professionals. This is an agreement with results of other studies (Logan et al., 1992; Clover et al., 1999; Wyne et al., 2006) where the Dentists generally believed that it was part of their responsibility to help patients in smoking cessation.
5. Conclusion
Family and general practitioners play major roles in providing support and assistance to individuals in smoking cessation, but dental professionals are also an important source of support. They frequently provide dental services to adult and adolescent smokers, and are thus positioned uniquely to provide specific and authoritative information to patients about the hazardous effects of tobacco use. Thus, we strongly recommend that dental professionals receive proper training and acquire knowledge and clinical skills for the prevention and cessation of tobacco use, and that education on this issue is included in the undergraduate dental curriculum.
Conflict of interest
The authors declare that they have no conflict of interest.
Acknowledgements
The author would like to thank the College of Dentistry Research Centre and Deanship of Scientific Research at King Saud University, Saudi Arabia for funding this research project (Project # FR 0107).
Footnotes
Peer review under responsibility of King Saud University.
References
- Abdulghani H.M., Alrowais N.A., Alhaqwi A.I., Alrasheedi A., Al-Zahir M., Al-Madani A., Ahmad F. Cigarette smoking among female students in five medical and nonmedical colleges. Int. J. Gen. Med. 2013;6:719–727. doi: 10.2147/IJGM.S48630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Haqwi A.I., Tamim H., Asery A. Knowledge, attitude and practice of tobacco smoking by medical students in Riyadh, Saudi Arabia. Ann. Thorac. Med. 2010;5(3):145–148. doi: 10.4103/1817-1737.65044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alomari Q., Barrieshi-Nusair K., Said K. Smoking prevalence and its effect on dental health attitudes and behavior among dental students. Med. Princ. Pract. 2006;15(3):195–199. doi: 10.1159/000092181. [DOI] [PubMed] [Google Scholar]
- Azhar A., Alsayed N. Prevalence of smoking among female medical students in Saudi Arabia. Asian Pac. J. Cancer Prev. 2012;13(9):4245–4248. doi: 10.7314/apjcp.2012.13.9.4245. [DOI] [PubMed] [Google Scholar]
- Barrieshi-Nusair K., Alomari Q., Said K. Dental health attitudes and behaviour among dental students in Jordan. Community Dent. Health. 2006;23(3):147–151. [PubMed] [Google Scholar]
- Centers for Disease & Prevention Vital signs: current cigarette smoking among adults aged ⩾18 years – United States, 2005–2010. MMWR Morb. Mortal. Wkly Rep. 2011;60(35):1207–1212. [PubMed] [Google Scholar]
- Clover K., Hazell T., Stanbridge V., Sanson-Fisher R. Dentists’ attitudes and practice regarding smoking. Aust Dent J. 1999;44(1):46–50. doi: 10.1111/j.1834-7819.1999.tb00535.x. [DOI] [PubMed] [Google Scholar]
- Conrad K.M., Flay B.R., Hill D. Why children start smoking cigarettes: predictors of onset. Br. J. Addict. 1992;87(12):1711–1724. doi: 10.1111/j.1360-0443.1992.tb02684.x. [DOI] [PubMed] [Google Scholar]
- Dudas R.B., Hans K., Barabas K. Anxiety, depression and smoking in schoolchildren–implications for smoking prevention. J. R. Soc. Promot. Health. 2005;125(2):87–92. doi: 10.1177/146642400512500213. [DOI] [PubMed] [Google Scholar]
- Dumitrescu A.L. Tobacco and alcohol use among Romanian dental and medical students: a cross-sectional questionnaire survey. Oral Health Prev. Dent. 2007;5(4):279–284. [PubMed] [Google Scholar]
- Ehizele A.O., Azodo C.C., Ezeja E.B., Ehigiator O. Nigerian dental students’ compliance with the 4As approach to tobacco cessation. J. Prev. Med. Hyg. 2011;52(1):12–16. [PubMed] [Google Scholar]
- Ertas N. Factors associated with stages of cigarette smoking among Turkish youth. Eur. J. Public Health. 2007;17(2):155–161. doi: 10.1093/eurpub/ckl095. [DOI] [PubMed] [Google Scholar]
- Huang B., Inagaki K., Yoshii C., Kano M., Abbott P.V., Noguchi T., Bessho K. Social nicotine dependence in Australian dental undergraduate students. Int. Dent. J. 2011;61(3):152–156. doi: 10.1111/j.1875-595X.2011.00032.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson G.K., Slach N.A. Impact of tobacco use on periodontal status. J. Dent. Educ. 2001;65(4):313–321. [PubMed] [Google Scholar]
- Kujan O., Abuderman A., Azzegahiby S., Alenzi F.Q., Idrees M. Assessing oral cancer knowledge among Saudi medical undergraduates. J. Cancer Educ. 2013;28(4):717–721. doi: 10.1007/s13187-013-0527-4. [DOI] [PubMed] [Google Scholar]
- Logan H., Levy S., Ferguson K., Pomrehn P., Muldoon J. Tobacco related attitude and counseling practices of Iowa dentists. Clin Prev Dent. 1992;14(1):19–22. [PubMed] [Google Scholar]
- Murthy P., Saddichha S. Tobacco cessation services in India: recent developments and the need for expansion. Indian J. Cancer. 2010;47(Suppl. 1):69–74. doi: 10.4103/0019-509X.63873. [DOI] [PubMed] [Google Scholar]
- Office for National Statistics, 2013. General Lifestyle Survey Overview: A report on the 2011 General Lifestyle Survey.
- Palmer R.M., Wilson R.F., Hasan A.S., Scott D.A. Mechanisms of action of environmental factors–tobacco smoking. J. Clin. Periodontol. 2005;32(Suppl. 6):180–195. doi: 10.1111/j.1600-051X.2005.00786.x. [DOI] [PubMed] [Google Scholar]
- Piko B., Barabas K., Markos J. Health risk behaviour of a medical student population: report on a pilot study. J. R. Soc. Health. 1996;116(2):97–100. doi: 10.1177/146642409611600207. [DOI] [PubMed] [Google Scholar]
- Preshaw P.M., Heasman L., Stacey F., Steen N., McCracken G.I., Heasman P.A. The effect of quitting smoking on chronic periodontitis. J. Clin. Periodontol. 2005;32(8):869–879. doi: 10.1111/j.1600-051X.2005.00779.x. [DOI] [PubMed] [Google Scholar]
- Ramseier C.A., Mattheos N., Needleman I., Watt R., Wickholm S. Consensus report: first European workshop on tobacco use prevention and cessation for oral health professionals. Oral Health Prev. Dent. 2006;4(1):7–18. [PubMed] [Google Scholar]
- Ramseier C.A., Warnakulasuriya S., Needleman I.G., Gallagher J.E., Lahtinen A., Ainamo A., Zoitopoulos L. Consensus report: 2nd European workshop on tobacco use prevention and cessation for oral health professionals. Int. Dent. J. 2010;60(1):3–6. [PubMed] [Google Scholar]
- Rikard-Bell G., Groenlund C., Ward J. Australian dental students’ views about smoking cessation counseling and their skills as counselors. J. Public Health Dent. 2003;63(3):200–206. doi: 10.1111/j.1752-7325.2003.tb03500.x. [DOI] [PubMed] [Google Scholar]
- Rosseel J.P., Jacobs J.E., Hilberink S.R., Maassen I.M., Segaar D., Plasschaert A.J., Grol R.P. Experienced barriers and facilitators for integrating smoking cessation advice and support into daily dental practice. A short report. Br. Dent. J. 2011;210(7):E10. doi: 10.1038/sj.bdj.2011.241. [DOI] [PubMed] [Google Scholar]
- Secker-Walker R.H., Solomon L.J., Flynn B.S., Dana G.S. Comparisons of the smoking cessation counseling activities of six types of health professionals. Prev. Med. 1994;23(6):800–808. doi: 10.1006/pmed.1994.1137. [DOI] [PubMed] [Google Scholar]
- Smith D.R., Leggat P.A. An international review of tobacco smoking among dental students in 19 countries. Int. Dent. J. 2007;57(6):452–458. doi: 10.1111/j.1875-595x.2007.tb00149.x. [DOI] [PubMed] [Google Scholar]
- Tonetti M.S. Cigarette smoking and periodontal diseases: etiology and management of disease. Ann. Periodontol. 1998;3(1):88–101. doi: 10.1902/annals.1998.3.1.88. [DOI] [PubMed] [Google Scholar]
- Tyas S.L., Pederson L.L. Psychosocial factors related to adolescent smoking: a critical review of the literature. Tob. Control. 1998;7(4):409–420. doi: 10.1136/tc.7.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- USDHHS. Healthy People 2010, ed. US Department of Health & Human Services, National Centre for Chronic Diseases Prevention & Health Promotion. Office of Smoking and Health. Atlanta, GA: USDHHS 2004.
- Warnakulasuriya S. Bidi smokers at increased risk of oral cancer. Evid. Based Dent. 2005;6(1):19. doi: 10.1038/sj.ebd.6400297. [DOI] [PubMed] [Google Scholar]
- Warnakulasuriya S., Sutherland G., Scully C. Tobacco, oral cancer, and treatment of dependence. Oral Oncol. 2005;41(3):244–260. doi: 10.1016/j.oraloncology.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Wiener R.C., Wiener Pla R.M. Evaluation of educational material for tobacco prevention and cessation used in west virginia university dental programs. J. Dent. Hyg. 2011;85(3):204–210. [PubMed] [Google Scholar]
- Wyne A.H., Chohan A.N., Al-Moneef M.M., Al-Saad A.S. Attitudes of general dentists about smoking cessation and prevention in child and adolescent patients in Riyadh. Saudi Arabia. J Contemp Dent Pract. 2006;7(1):35–43. [PubMed] [Google Scholar]
- Zahid N., Qidwai W. Characteristics of smokers and their knowledge about smoking at a teaching hospital in Karachi. Pak. J. Med. Sci. 2005;21:109–111. [Google Scholar]


