Abstract
Objectives
The aim of this study was to evaluate the strength of the bond between newly introduced self-adhesive resin cements and tooth structures (i.e., enamel and dentin).
Methods
Three self-adhesive cements (SmartCem2, RelyX Unicem, seT SDI) were tested. Cylindrical-shaped cement specimens (diameter, 3 mm; height, 3 mm) were bonded to enamel and dentin. Test specimens were incubated at 37 °C for 24 h. The shear bond strength (SBS) was tested in a Zwick Roll testing machine. Results were analyzed by one-way ANOVA and t-test. Statistically significant differences were defined at the α = 0.05 level. Bond failures were categorized as adhesive, cohesive, or mixed.
Results
The SBS values ranged from 3.76 to 6.81 MPa for cements bonded to enamel and from 4.48 to 5.94 MPa for cements bonded to dentin (p > 0.05 between surfaces). There were no statistically significant differences between the SBS values to enamel versus dentin for any given cement type. All cements exhibited adhesive failure at the resin/tooth interface.
Conclusions
Regardless of their clinical simplicity, the self-adhesive resin cements examined in this study exhibit limited bond performance to tooth structures; therefore, these cements must be used with caution.
Keywords: Self-adhesive, Shear bond strength, Enamel, Dentin, Cement
1. Introduction
Cementation is a critical step in ensuring the longevity of indirect restorations. Indeed, in certain clinical situations (e.g., when using ceramic or composite indirect restorations), adhesive cements must be used. Various dental luting agents are available to clinicians, each with its own particularities and indications; thus, choosing which cement to use may be difficult. Resin cements possess superior mechanical properties, as they are relatively insoluble, can withstand the stresses of the oral environment, provide excellent retention, and are capable of maintaining the integrity of the tooth and restoration (Rosenstiel et al., 1998). However, resin cements require multiple sensitive clinical steps. For this reason, self-adhesive cements were recently introduced, aimed at simplifying the luting procedure.
Manufacturers of self-adhesive resin cements advocate that these cements require neither conditioning of the tooth nor surface treatment of the restoration (Abo Hamar et al., 2005; Behr et al., 2004). These cements are moisture-tolerant and capable of fluoride release in a manner similar to glass ionomer cements (Gerth et al., 2006). However, one study reported that the dentin surface should ideally be treated before applying a self-adhesive system, to improve the dentin/alloy bond strength (El-Guindy et al., 2010). Moreover, etching the enamel with phosphoric acid, either alone (De Munck et al., 2004; Duarte et al., 2008; Hikita et al., 2007) or followed by a bonding agent (Lin et al., 2010), can significantly improve the bond strength of the self-adhesive cement to the tooth structure. RelyX Unicem (3M ESPE, Seefeld, Germany) was the first self-adhesive resin cement to be launched on the market and, therefore, is the most thoroughly studied of these cements (Behr et al., 2004; Duarte et al., 2008; Hikita et al., 2007). This product was intended to combine the ease of use of glass ionomer cements with the adhesive properties of resin cements, without the complexity of the procedure.
The bonding properties of resin cements are related to the chemical composition. The organic matrix of the cement, consisting of multifunctional phosphoric acid methacrylates, is proposed to be capable of simultaneously demineralizing and infiltrating the tooth surface (Yoshida et al., 2000). The phosphoric (Gerth et al., 2006; Radovic et al., 2008) and carboxylic groups of polyalkenoic acid form ionic bonds with hydroxyapatite, thereby ensuring a second means of retention (Fukuda et al., 2003; Gerth et al., 2006; Radovic et al., 2008). However, studies have shown that RelyX Unicem has a limited demineralization capacity and interacts only superficially with the tooth structure (Aguiar et al., 2013; Al-Assaf et al., 2007; Duarte et al., 2008; Monticelli et al., 2008). Compared to conventional luting systems, RelyX Unicem showed equivalent or lower bond strength values in bonding to dentin or enamel, respectively (Behr et al., 2004; Chai et al., 2008; Duarte et al., 2008; Flury et al., 2010; Hikita et al., 2007; Poitevin et al., 2013). Nevertheless, RelyX Unicem exhibited superior strength in bonding to restorative materials compared to glass ionomer cement (Capa et al., 2009; Piwowarczyk et al., 2004).
Most of the currently available data for self-adhesive cements are based on in vitro investigations, with very few studies of clinical performance. One short-term clinical study revealed that the performance of self-adhesive cements is comparable to that of zinc phosphate cement (Behr et al., 2009). Therefore, the purpose of this study was to evaluate the shear bond strength (SBS) values of self-adhesive resin cements to enamel and dentin tooth structures. The null hypothesis was that there is no significant difference in SBS among the different types of self-adhesive resin cements.
2. Methods
The tested self-adhesive cements were RelyX Unicem, SmartCem2 (Caulk-Dentsply, Milford, DE), and seT SDI (SDI Limited, Victoria, Australia), as shown in Table 1.
Table 1.
Materials used in this study.
| Luting agent | Delivery system | Batch number | Composition |
|---|---|---|---|
| RelyX Unicem (3M ESPE, Seefeld, Germany) | Capsules | 384237 | Methacrylated phosphoric esters, dimethacrylates, acetate, glass fillers, silica, calcium hydroxide, stabilizers, co-initiators, pigments |
| Filled to approximately 72% by weight | |||
| SmartCem2 (Caulk-Dentsply, Milford, DE, USA) | Paste/paste dual syringe auto mixing | 0808013 | Urethane dimethacrylate (UDMA), di and tri methacrylate resin, 4-methacryloxyethyl trimellitate anhydride (4-META), phosphoric acid modified acrylate resin, barium boron fluoroaluminosilicate glass, initiators, accelerators, UV stabilizers |
| Filled to approximately 69% by weight | |||
| seT SDI (SDI Limited, Victoria, Australia) | Capsules | S0904282 | Methacrylate phosphoric esters, Urethane dimethacrylate (UDMA), Strontium fluoroaluminosilicate glass, silica camphorquinone stabilizer, co-initiators, pigments |
| Filled to approximately 67.5% |
2.1. Tooth preparation
Freshly extracted posterior teeth were collected and inspected for existing caries, lesions, and fillings. Only sound teeth were used in this study. Teeth were kept in saline water for later use. A diamond disk (Diamant GmbH, D&Z, Berlin, Germany) was used to cut the teeth (bucco-lingual section) and to expose the dentin and enamel. Surfaces were polished with 600-grit sandpaper for 5 s. Polished tooth sections were embedded in brass mold holders, which had been specifically designed for conducting shear testing.
Resin cements were mixed in accordance with the manufacturers’ recommendations. Custom-made Teflon disks (internal diameter, 3 mm; external diameter, 14.4 mm; thickness, 3 mm) were fixed over the tooth surface, and the cement was injected inside the Teflon mold. All cements were light-cured for 40 s with a QTH light-curing unit (Optilux501, SDS Kerr, Danbury, USA), which was operated in standard mode. The light-curing unit emitted 760 mW/cm2 irradiance, as measured by the incorporated radiometer that had been calibrated against a flat-response power meter. Once curing was completed, the molds were removed, and specimens were incubated in a wet environment at 37 ± 1 °C for 24 h before testing.
2.2. SBS testing
Tests of the SBS were performed with a custom-made device designed according to ISO TR 11405 (1994)(E). Test specimens were placed inside the testing device, which was fixed in a universal testing machine (Zwick/Roell; Z020, Germany). Shear loading was applied at the interface between the cement and tooth surface at a cross-speed of 0.8 mm/min. The maximum debonding force (F, in N) for each specimen was recorded and used in calculating the SBS value (in MPa), according to the equation: SBS = F/A, where A is the cross-sectional area (in mm). Tooth surfaces were inspected by an optical microscope at 40× magnification and analyzed for failure type. Bonding failure was categorized as adhesive (failure between the cement and tooth structure), cohesive (failure within the tooth structure or cement itself), or mixed.
2.3. Statistical analysis
Statistical analysis was performed with SPSS 17 for Windows (SPSS Inc., Chicago IL, USA). Descriptive statistics were generated. One-way ANOVA and Bonferroni post hoc tests were used to examine differences among cements. Independent t-tests were used to compare the SBS values of each cement to enamel and dentin (α = 0.05 significance level). The present study employed only restorative materials; therefore, no ethical consent was required.
3. Results
The mean, standard deviation, and range of SBS values for the bonding of different cements to enamel and dentin are presented in Table 2. Fig. 1 demonstrates the SBS of each cement to enamel and dentin. No significant differences were observed among the SBS values of the three types of cement when bonded to enamel or dentin, as indicated by one-way ANOVA. All cements failed in the adhesive mode at the cement/tooth interface, regardless of whether the bond was to enamel or dentin.
Table 2.
Shear bond strength (MPa) of different cements to enamel and dentin.
| Cement type | Shear bond to enamel (MPa) |
Shear bond to dentin (MPa) |
||||||
|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | Range (min–max) | N | Mean | SD | Range (min–max) | |
| RelyX Unicem | 8 | 6.81a | 2.27 | 4.07–10.60 | 7 | 5.94a | 2.17 | 3.89–10.50 |
| SmartCem2 | 8 | 5.41a | 2.27 | 2.15–8.16 | 8 | 4.71a | 3.81 | 1.35–12.93 |
| seT SDI | 3 | 3.76a | 2.52 | 0.85–5.38 | 6 | 4.48a | 4.40 | 0.45–11.81 |
Within mean columns; similar superscript letters indicate homogeneous sets (P > .05) between the cements; and between tooth structures within each cement type.
Figure 1.
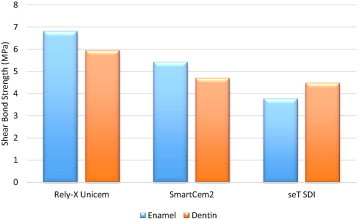
Shear bond strength values (MPa) for self-adhesive cements, bonded to enamel and dentin.
4. Discussion
This study investigated the bonding effectiveness of two novel self-adhesive cements (SmartCem2 and seT) and a universal self-adhesive resin luting agent (RelyX Unicem) to enamel and dentin. No statistically significant differences among the cements were found; thus, the null hypothesis of the study was confirmed.
Comparable bond strength values to those found in this study have been reported in previous studies. For example, Chai et al. (2008) recorded similar SBS values when RelyX Unicem was used to bond nickel–chromium to human dentin. Al-Saleh and El-Mowafy (2010) reported similar SBS values to our study for RelyX Unicem in bonding orthodontic brackets. However, in that study, the samples were subjected to thermocycling, and the cements were applied onto polished-unground enamel surfaces.
The relative low SBS values obtained here and elsewhere (Al-Saleh and El-Mowafy, 2010; Chai et al., 2008; Lin et al., 2010; Piwowarczyk et al., 2007; Viotti et al., 2009) confirm the notion that self-adhesive cements do not dissolve the smear layer (Goracci et al., 2006) and interact only superficially with the tooth structure. A few factors may contribute to this possibility. First, the light-cured cement exhibits a high viscosity and limited penetration/interaction time (Duarte et al., 2008; Monticelli et al., 2008). Second, self-adhesive cements need to be applied with some pressure (Chieffi et al., 2007; Duarte et al., 2008), to ensure that the relatively highly viscous cement intimately adapts to the surface (El-Guindy et al., 2010). Third, the design of shear testing necessitates that resin cylinders be bonded to the tooth. Light curing of these relatively thick specimens might result in a high polymerization stress, causing resin contraction away from the surface.
The self-etching potential is attributed to the presence of multifunctional monomers, which might differ according to cement type. RelyX Unicem and seT SDI contain methacrylated phosphoric esters, whereas SmartCem2 also contains a hydrophilic monomer (4-META), both supposedly having a low initial pH. Normally, the cements should be capable of demineralizing and infiltrating the tooth structure. Nevertheless, only inconsistent areas of etching (De Munck et al., 2004) and almost no distinct demineralization (Lin et al., 2010) or hybrid layer formation (Al-Assaf et al., 2007) have been observed after using these materials. Therefore, chemical rather than micromechanical bonding is responsible for the dental adhesion of the resin components, especially 4-META, which has been shown to chelate the calcium ions of hydroxyapatite crystals (Nagakane et al., 2006). On the other hand, Han et al. (2007) demonstrated that self-adhesive cements do not achieve a neutral pH, and that maintaining a low initial pH for a long period can adversely affect the dentin bonding of these cements.
The newly developed self-adhesive cements display disparate properties. After testing the push-out bond strength of ceramic inlays luted to dentin with self-adhesive resin cements, Flury et al. (2010) concluded that these cements showed marked variations in bond strength. Moreover, based on the significant differences in pH values (Han et al., 2007; Saskalauskaite et al., 2008), degree of cure (Vrochari et al., 2009), flexural strength, film thickness, particle content, and surface morphology of these cements (Han et al., 2007), they cannot be considered as one homogeneous group. Nevertheless, Nakamura et al. (2010) found that certain self-adhesive cements, particularly SAC (Kuraray Medical), have excellent mechanical properties in terms of flexural strength, elastic modulus, and water absorption, which they attributed to the presence of 10-methacryloyloydecyldihydrogen phosphate (MDP) in SAC. MDP is the same acidic monomer as is found in Panavia (Kurary Dental, Japan), and its presence may have enhanced bonding to the tooth structure.
In the present work, the lowest SDS values and fewest successful specimens were reported when the seT SDI cement was used. A recent study reported comparable microtensile bond strength values for the same cements as this study and found that seT SDI demonstrated the lowest bond strength (Viotti et al., 2009). During sample preparation, the seT SDI cement showed multiple premature failures. Not accounting for these failures probably results in an overestimation of the bonding potential (Scherrer et al., 2010). Many previous reports have also found large numbers of pretesting failures (Goracci et al., 2006), and others showed little to no bonding of certain types of self-adhesive cements, particularly SAC and BisCem (Bisco, IL, USA) (Cantoro et al., 2009). These observations may give some insight into the in vivo performances of these cements.
In previous studies, the most common failure modes for self-adhesive cements have been adhesive and mixed failures, with only a small percentage comprising true cohesive failures (Braga et al., 2010). The failure mode is largely influenced by the test mechanics and material properties. In this study, failures were adhesive in nature and occurred at the resin/tooth interface in both enamel and dentin specimens, consistent with the findings of other studies (Duarte et al., 2008; Flury et al., 2010; Lin et al., 2010; Viotti et al., 2009). These observations support the conclusion that self-adhesive cements interact only superficially, with little infiltration in the tooth.
Shear and tensile tests of bond strength can provide insight into the adhesion of a specific material to the tooth structure, but they cannot be used to predict clinical performance. Bond strength is influenced by numerous parameters related to the specimen design or test mechanics (Braga et al., 2010), which cannot be standardized. Comparison among studies is difficult, if not impossible (Scherrer et al., 2010). The high variability among bond strength values reported in the literature has been attributed to the lack of a standard testing protocol (Van Meerbeek et al., 2010) and to the heterogeneity in tooth structure and composition. For example, many studies have reported equivalent bond strength values of self-adhesive cements to dentin compared to conventional cements (Behr et al., 2004; Duarte et al., 2008; Hikita et al., 2007), whereas other studies have reported inferior bond strength values (Escribano and de la Macorra, 2006; Holderegger et al., 2008; Lührs et al., 2010; Viotti et al., 2009). Furthermore, most of these studies investigated early-generation cements, especially RelyX Unicem; therefore, their results do not represent the entire category of self-adhesive cements. Overall, as promising as self-adhesive cements might seem due to their simplicity, adequate data on their true clinical performance are not available.
5. Conclusion
The tested self-adhesive resin cements exhibited similar SBS values to enamel and dentin. Their simplicity renders their use favorable; however, their performance is far from being comparable to that of multistep conventional resin cements. These cements must be used with caution, in light of their limited bond performance.
Conflict of interest
The authors have no conflict of interest to declare.
Footnotes
Peer review under responsibility of King Saud University.
Contributor Information
Susan Hattar, Email: s.hattar@ju.edu.jo, susanhattar@yahoo.fr.
Muhanad M. Hatamleh, Email: muhanad.hatamleh@nhs.net.
Faleh Sawair, Email: sawair@ju.edu.jo.
Mohammad Al-Rabab’ah, Email: malrababah@ju.edu.jo.
References
- Abo Hamar S.E., Hiler K.A., Jung H., Federlin M., Friedl K.H., Schmalz G. Bond strength of a new universal self adhesive resin luting cement to dentin and enamel. Clin. Oral. Investig. 2005;9:161–167. doi: 10.1007/s00784-005-0308-5. [DOI] [PubMed] [Google Scholar]
- Aguiar T.R., Vermelho P.M., Andre C.B., Giannini M. Interfacial ultramorphology evaluation of resin luting cements to dentin: a correlative scanning electron microscopy and transmission electron microscopy analysis. Microsc. Res. Tech. 2013;76:1234–1239. doi: 10.1002/jemt.22290. [DOI] [PubMed] [Google Scholar]
- Al-Assaf K., Chakmakchi M., Palaghias G., Karanika-Kouma A., Eliades G. Interfacial characteristics of adhesive luting resins and composites with dentine. Dent. Mater. 2007;23:829–839. doi: 10.1016/j.dental.2006.06.023. [DOI] [PubMed] [Google Scholar]
- Al-Saleh M., El-Mowafy O. Bond strength of orthodontic brackets with new self-adhesive resin cements. Am. J. Orthod. Dentofacial Orthop. 2010;137:528–533. doi: 10.1016/j.ajodo.2008.04.027. [DOI] [PubMed] [Google Scholar]
- Behr M., Rosentritt M., Regnet T., Lang R., Handel G. Marginal adaptation in dentin of a self-adhesive universal resin cement compared with well tried systems. Dent. Mater. 2004;20:191–197. doi: 10.1016/s0109-5641(03)00091-5. [DOI] [PubMed] [Google Scholar]
- Behr M., Rosentritt M., Wimmer J., Lang R., Kolbeck C., Burgers R., Handel G. Self adhesive resin cement versus zinc phosphate luting material: a prospective clinical trial begun 2003. Dent. Mater. 2009;25:601–604. doi: 10.1016/j.dental.2008.11.003. [DOI] [PubMed] [Google Scholar]
- Braga R.R., Meira J.B., Boaro L.C., Xavier T.A. Adhesion to tooth structure: a critical review of “macro” test methods. Dent. Mater. 2010;26:e38–e49. doi: 10.1016/j.dental.2009.11.150. [DOI] [PubMed] [Google Scholar]
- Cantoro A., Goracci C., Carvalho C.A., Coniglio I., Ferrari M. Bonding potential of self-adhesive luting agents used at different temperatures to lute composite onlays. J. Dent. 2009;37:454–461. doi: 10.1016/j.jdent.2009.02.006. [DOI] [PubMed] [Google Scholar]
- Capa N., Ozkurt Z., Canpolat C., Kazazoglu E. Shear bond strength of luting agents to fixed prosthodontic restorative core materials. Aust. Dent. J. 2009;54:334–340. doi: 10.1111/j.1834-7819.2009.01159.x. [DOI] [PubMed] [Google Scholar]
- Chai J., Chu F.C., Chow T.W., Liang B.M. Shear bond strength between nickel–chromium and human dentine using a dual-cure, self-adhesive universal resin luting agent. Eur. J. Prosthodont. Restor. Dent. 2008;16:85–88. [PubMed] [Google Scholar]
- Chieffi N., Chersoni S., Papacchini F., Vano M., Goracci C., Davidson C.L., Tay F.R., Ferrari M. The effect of application sustained seating pressure on adhesive luting procedure. Dent. Mater. 2007;23:159–164. doi: 10.1016/j.dental.2006.01.006. [DOI] [PubMed] [Google Scholar]
- De Munck J., Vargas M., Van Landuyt K., Hikita K., Lambrechts P., Van Meerbeek B. Bonding of an auto adhesive luting material to enamel and dentin. Dent. Mater. 2004;20:963–971. doi: 10.1016/j.dental.2004.03.002. [DOI] [PubMed] [Google Scholar]
- Duarte S., Jr., Botta A.C., Meire M., Sadan A. Microtensile bond strengths and scanning electron microscopic evaluation of self-adhesive and self-etch resin cements to intact and etched enamel. J. Prosthet. Dent. 2008;100:203–210. doi: 10.1016/S0022-3913(08)60179-1. [DOI] [PubMed] [Google Scholar]
- El-Guindy J., Selim M., El-Agroudi M. Alternative pretreatment modalities with a self-adhesive system to promote dentin/alloy shear bond strength. J. Prosthodont. 2010;19:205–211. doi: 10.1111/j.1532-849X.2009.00541.x. [DOI] [PubMed] [Google Scholar]
- Escribano N., de la Macorra J.C. Microtensile bond strength of self-adhesive luting cements to ceramic. J. Adhes. Dent. 2006;8:337–341. [PubMed] [Google Scholar]
- Flury S., Lussi A., Peutzfeldt A., Zimmerli B. Push out bond strength of CAD/CAM ceramic luted to dentin with self adhesive resin cements. Dent. Mater. 2010;26:855–863. doi: 10.1016/j.dental.2010.05.001. [DOI] [PubMed] [Google Scholar]
- Fukuda R., Yoshida Y., Nakayama Y., Okazaki M., Inoue S., Sano H., Suzuki K., Shintani H., Van Meerbeek B. Bonding efficacy of polyalkenoic acids to hydroxyapatite, enamel and dentin. Biomaterials. 2003;24:1861–1867. doi: 10.1016/s0142-9612(02)00575-6. [DOI] [PubMed] [Google Scholar]
- Gerth H.U., Dammaschke T., Züchner H., Schäfer E. Chemical analysis and bonding reaction of RelyX Unicem and Bifix composites – a comparative study. Dent. Mater. 2006;22:934–941. doi: 10.1016/j.dental.2005.10.004. [DOI] [PubMed] [Google Scholar]
- Goracci C., Cury A.H., Cantoro A., Papacchini F., Tay F.R., Ferrari M. Microtensile bond strength and interfacial properties of self-etching and self-adhesive resin cements used to lute composite onlays under different seating forces. J. Adhes. Dent. 2006;8:327–335. [PubMed] [Google Scholar]
- Han L., Okamoto A., Fukushima M., Okiji T. Evaluation of physical properties and surface degradation of self-adhesive resin cements. Dent. Mater. J. 2007;26:906–914. doi: 10.4012/dmj.26.906. [DOI] [PubMed] [Google Scholar]
- Hikita K., Van Meerbeek B., De Munck J., Ikeda T., Van Landuyt K., Maida T., Lambrechts P., Peumans M. Bonding effectiveness of adhesive luting agents to enamel and dentin. Dent. Mater. 2007;23:218–225. doi: 10.1016/j.dental.2005.12.002. [DOI] [PubMed] [Google Scholar]
- Holderegger C., Sailer I., Schuhmacher C., Schläpfer R., Hämmerle C., Fischer J. Shear bond strength of resin cements to human dentin. Dent. Mater. 2008;24:944–950. doi: 10.1016/j.dental.2007.11.021. [DOI] [PubMed] [Google Scholar]
- International Organization for Standardization ISO TR 11405 . ISO; Geneva: 1994. Dental Materials-Guidance on Testing Adhesion to Tooth Structure. [Google Scholar]
- Lin J., Shinya A., Gomi H., Shinya A. Effect of self-adhesive resin cement and tribochemical treatment on bond strength to zirconia. Int. J. Oral. Sci. 2010;2:28–34. doi: 10.4248/IJOS10002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lührs A.K., Guhr S., Günay H., Geurtsen W. Shear bond strength of self-adhesive resins compared to resin cements with etch and rinse adhesives to enamel and dentin in vitro. Clin. Oral. Investig. 2010;14:193–199. doi: 10.1007/s00784-009-0279-z. [DOI] [PubMed] [Google Scholar]
- Monticelli F., Osorio R., Mazzitelli C., Ferrari M., Toledano M. Limited decalcification/diffusion of self-adhesive cements into dentin. J. Dent. Res. 2008;87:974–979. doi: 10.1177/154405910808701012. [DOI] [PubMed] [Google Scholar]
- Nagakane K., Yoshida Y., Hirata I., Fukuda R., Nakayama Y., Shirai K., Ogawa T., Suzuki K., Van Meerbeek B., Okazaki M. Analysis of chemical interaction of 4-MET with hydroxyapatite using XPS. Dent. Mater. J. 2006;25:645–649. doi: 10.4012/dmj.25.645. [DOI] [PubMed] [Google Scholar]
- Nakamura T., Wakabayashi K., Kinuta S., Nishida H., Miyamae M., Yatani H. Mechanical properties of new self-adhesive resin-based cement. J. Prosthodont. Res. 2010;54:59–64. doi: 10.1016/j.jpor.2009.09.004. [DOI] [PubMed] [Google Scholar]
- Piwowarczyk A., Lauer H.C., Sorensen J.A. In vitro shear bond strength of cementing agents to fixed prosthodontics restorative materials. J. Prosthet. Dent. 2004;92:265–273. doi: 10.1016/j.prosdent.2004.06.027. [DOI] [PubMed] [Google Scholar]
- Piwowarczyk A., Bender R., Ottl P., Lauer H.C. Long-term bond between dual-polymerizing cementing agents and human hard dental tissue. Dent. Mater. 2007;23:211–217. doi: 10.1016/j.dental.2006.01.012. [DOI] [PubMed] [Google Scholar]
- Poitevin A., De Munck J., Van Ende A., Suyama Y., Mine A., Peumans M., Van Meerbeek B. Bonding effectiveness of self-adhesive composites to dentin and enamel. Dent. Mater. 2013;29:221–230. doi: 10.1016/j.dental.2012.10.001. [DOI] [PubMed] [Google Scholar]
- Radovic I., Monticelli F., Goracci C., Vulicevic Z., Ferrari M. Self adhesive resin cements: a literature review. J. Adhes. Dent. 2008;10:251–258. [PubMed] [Google Scholar]
- Rosenstiel S.F., Land M.F., Crispin B.J. Dental luting agents: a review of the current literature. J. Prosthet. Dent. 1998;8:280–301. doi: 10.1016/s0022-3913(98)70128-3. [DOI] [PubMed] [Google Scholar]
- Saskalauskaite E., Tam L.E., McComb D. Flexural strength, elastic modulus and pH profile of self-etch resin luting cements. J. Prosthodont. 2008;17:262–268. doi: 10.1111/j.1532-849X.2007.00278.x. [DOI] [PubMed] [Google Scholar]
- Scherrer S.S., Cesar P.F., Swain M.V. Direct comparison of the bond strength results of the different test methods: a critical literature review. Dent. Mater. 2010;26:e78–e93. doi: 10.1016/j.dental.2009.12.002. [DOI] [PubMed] [Google Scholar]
- Van Meerbeek B., Peumans M., Poitevin A., Mine A., Van Ende A., Neves A., De Munck J. Relationship between bond-strength tests and clinical outcomes. Dent. Mater. 2010;26:100–121. doi: 10.1016/j.dental.2009.11.148. [DOI] [PubMed] [Google Scholar]
- Viotti R.G., Kasaz A., Pena C.E., Alexandre R.S., Arrais C.A., Reis A.F. Microtensile bond strength of new self-adhesive luting agents and conventional multistep systems. J. Prosthet. Dent. 2009;102:306–312. doi: 10.1016/S0022-3913(09)60180-3. [DOI] [PubMed] [Google Scholar]
- Vrochari A., Eliades G., Hellwig E., Wrbas K.T. Curing efficiency of four self-etching, self-adhesive resin cements. Dent. Mater. 2009;25:1104–1108. doi: 10.1016/j.dental.2009.02.015. [DOI] [PubMed] [Google Scholar]
- Yoshida Y., Van Meerbeek B., Nakayama Y., Snauwaert J., Hellemans L., Lambrechts P., Vanherle G., Wakasa K. Evidence of chemical bonding at biomaterial-hard tissues interfaces. J. Dent. Res. 2000;79:709–714. doi: 10.1177/00220345000790020301. [DOI] [PubMed] [Google Scholar]


