Abstract
Background and purpose:
Sacroiliac joint pain and dysfunction affect 15–25% of patients reporting low back pain, including reports of spontaneous, idiopathic, traumatic, and non-traumatic onsets. The poor reliability and validity associated with diagnostic clinical and imaging techniques leads to challenges in diagnosing and managing sacroiliac joint dysfunction.
Case description:
A 35-year-old nulliparous female with a 14-year history of right sacroiliac joint dysfunction was managed using a multimodal and multidisciplinary approach when symptoms failed to resolve after 2 months of physical therapy. The plan of care included four prolotherapy injections, sacroiliac joint manipulation into nutation, pelvic girdle belting, and specific stabilization exercises.
Outcomes:
The patient completed 20 physical therapy sessions over a 12-month period. At 6 months, the patient’s Oswestry Disability Questionnaire score was reduced from 34% to 14%. At 1-year follow-up, her score was 0%. The patient’s rating of pain on a numeric rating scale decreased to an average of 4/10 at 6 months and 0/10 at 1-year follow-up.
Discussion:
A multidisciplinary and multimodal approach for the management of chronic sacroiliac joint dysfunction appeared successful in a single-case design at 1-year follow-up.
Keywords: Sacroiliac joint dysfunction, Pelvic ring instability, Prolotherapy, Rehabilitation, Manual therapy
Background
Sacroiliac joint pain and dysfunction affect 15–25% of patients reporting non-radicular low back pain.1–4 Episodes of sacroiliac joint pain can occur spontaneously with or without trauma.5,6 Sacroiliac joint dysfunction can be difficult to diagnose and manage secondary to a poor correlation of history with diagnosis, and poor reliability and validity of the clinical examination and diagnostic imaging.5
Current medical management is variable including oral non-steroidal anti-inflammatory drugs, sacral belting,7–10 activity modification, manipulation,3–15 physical therapy,16,17 sacroiliac joint block,5 acupuncture, prolotherapy, neuroaugmentation, viscosupplementation,18 radiofrequency ablation,19,20 and fusion.21,22 The current gold standard for diagnosing sacroiliac joint pain is the performance of a sacroiliac joint double anesthetic block. During this procedure, the patient receives a fluoroscopic guided short-acting anesthetic block. Immediately following this procedure, sacroiliac joint pain provocation tests are performed to assess the efficacy of the block. If the results are positive, a second confirmatory block is performed.5
The purpose of this case report is to describe the changes observed in a patient’s sacroiliac joint pain, mobility, and overall function using a multimodal, multi-disciplinary approach aimed at promoting sacroiliac joint force closure. To the best of the authors’ knowledge, no study to date has evaluated the value of prolotherapy combined with pelvic ring belting, sacroiliac joint manipulation, and stabilization exercises in order to achieve the aforementioned outcomes in a patient with chronic sacroiliac joint pain.
Patient Characteristics
A 35-year-old nulliparous female consultant with a 14-year history of right low back and sacral pain subsequent to a fall of 4 feet onto the sacrum and low back was self-referred for physical therapy. Lumbo-pelvic radiographs taken following the injury were unremarkable. A Physical Medicine and Rehabilitation Physician and Doctor of Osteopathic Medicine both diagnosed her with sacroiliac joint dysfunction. The Osteopathic Doctor performed osteopathic manipulations to the lower lumbar spine and pelvis; specific interventions are unknown. The patient received two courses of physical therapy, which included therapeutic exercise and manipulation of the lumbar spine and pelvis; specific interventions are unknown. The patient reported relief with these interventions; however, they did not completely resolve her complaints. During her evaluation with the primary author, she reported being unable to sit for extended periods of time, especially slouched sitting on a soft chair or couch, run, or perform yoga without reporting posterior pelvic pain.
Examination
After obtaining informed consent, the patient underwent a physical therapy examination. The Oswestry Low Back Pain Disability Questionnaire (OSW) and a Numeric Pain Rating Scale were administered followed by a subjective interview and clinical examination. The location of the patient’s symptoms was depicted on a self-administered pain drawing over the area of the right posterior iliac crest and sacrum. The clinical examination included an assessment of posture and structural alignment, lumbar, thoracic spine, and hip range of motion, a neurological screen, lumbar repeated movements, sacroiliac joint provocation testing,23 active straight leg raise (ASLR) test,10 sitting forward flexion test, standing forward flexion test,24,25 strength testing of muscles crossing the pelvic girdle, and palpation. Segmental thoracic and lumbar mobility was not assessed as gross movements were within normal range without provocation of pain. Upon palpation, there was tenderness over the area of the right long dorsal sacroiliac ligament, as well as increased tone of the hip adductors-left greater than right. Remarkable findings are reported in Table 1.
Table 1. Remarkable clinical examination findings followed over the course of care.
| Test and measure | Initial evaluation | 6 months | 12 months |
| Transverse abdominus timed isometric hold | 20 seconds | 60 seconds | 60 seconds |
| Levator ani timed isometric hold | 12 seconds | 60 seconds | 60 seconds |
| The Oswestry Low Back Pain Disability Questionnaire Score | 34% (moderate disability)35 | 14% (minimal disability)35 | 0% |
| Numeric Pain Rating Scale Score | 6/10 | 4/10 | 0/10 |
| Forward flexion test right | Positive | Positive | Negative |
| Seated flexion test right | Positive | Positive | Negative |
| Active straight leg raise test right | Positive | Positive | Negative |
| Sacroiliac joint distraction test right | Positive | Negative | Negative |
| Sacroiliac joint compression test right | Positive | Positive | Negative |
| Sacroiliac joint thigh thrust test right | Positive | Positive | Negative |
| Manual muscle testing | |||
| Hip extension left | 4/5 | 4+/5 | 5/5 |
| Hip extension right | 3+/5 | 4/5 | 5/5 |
| Hip abduction left | 4−/5 | 4/5 | 5/5 |
| Hip abduction right | 3+/5 | 4/5 | 5/5 |
| Latissimus dorsi left | 4/5 | 4+/5 | 5/5 |
| Latissimus dorsi right | 4−/5 | 4+/5 | 5/5 |
Clinical Impression
The patient was classified into the following diagnostic classification: Impaired Joint Mobility, Motor Function, Muscle Performance, and Range of Motion Associated with Spinal Disorders.26 This was evidenced by a positive history of a fall onto the low back and sacrum, a negative screen of the lumbar spine and hip joints and a cluster of three positive sacroiliac joint provocation tests, positive ASLR test, and observed asymmetries during mobility testing using the forward flexion test in sitting and standing. Based on observed impairments and functional limitations, it was the opinion of the primary author that the patient presented with right sacroiliac joint dysfunction with pelvic ring instability. The patient’s goals were to eliminate pain and return to jogging, yoga, and sitting for long periods of time without restriction.
Intervention
The patient was treated weekly for 2 months. Interventions included: lumbo-pelvic strengthening and stabilization training (Table 2), right sacroiliac joint nutation manipulation27 (Fig. 1), muscle energy technique for pubic symphysis28 (Fig. 2a, 2b), and pelvic ring belting29 high on the pelvis just below the level of the anterior superior iliac spine (ASIS). The nutation direction of manipulation was selected based on the observations during the standing and sitting forward flexion test. During these tests, the symptomatic right posterior superior iliac spine was positioned in a more cranial orientation as compared to the contralateral side. The muscle energy technique selected is proposed as a technique to restore alignment of the pubic symphysis following mobilization or manipulation of the pelvis.28 If an asymmetry was observed prior to a subsequent session of physical therapy, these techniques were performed. Although the patient reported relief post manipulation and belting, resolution only lasted a few days. The patient’s symptoms failed to resolve within 2 months, so she was referred to a physiatrist. Upon further evaluation, it was proposed by the authors that secondary to the evidence of pelvic ring instability,10 14-year history of recurrent symptoms, and previous history of failed physical therapy, prolotherapy be utilized as a method to assist in stabilizing the sacroiliac joint. Administration of the agent to the ligament-bone interface stimulates collagen regeneration, thus stabilizing the joint.30
Table 2. Stabilization training program used in this case.
| Exercise intervention | Parameters |
| Phase I: Protective phase 0–3 months | Phase I: Protective phase 0–3 months |
| 1. Isometric: Transverse abdominus and levator ani | 6–60 second hold |
| 10 repetitions, daily | |
| 2. Isometric: Transverse abdominus, levator ani, and multifidus | 6–60 second hold, 10 repetitions, daily |
| 3. Isometric: Hip abduction | 6–60 second hold, 5–10 repetitions, 3 times per week |
| 3a. Isometric: Bridge, hip abduction, and latissimus dorsi (progression) | 6–60 second hold, 5–10 repetitions, 3 times per week |
| 4. Isometric: Hip adduction | 6–60 second hold, 5–10 repetitions, 3 times per week |
| 4a. Isometric: Bridge, hip adduction, and latissimus dorsi (progression) | 6–60 second hold, 5–10 repetitions, 3 times per week |
| Phase II: Controlled motion phase 4–8 months | Phase II: Controlled motion phase 4–8 months |
| 5. Isometric: Wall bridge, hip abduction, and latissimus dorsi | 6–60 second hold, 5–10 repetitions, 3 times per week |
| 5a. Isometric: Single leg wall bridge, hip abduction, and latissimus dorsi (progression) | 6–60 second hold, 5 repetitions each side, 3 times per week |
| 6. Isometric: Wall bridge, hip abduction, and latissimus Dorsi | 6–60 second hold, 5–10 repetitions, 3 times per week |
| 6a. Isometric: Single leg wall bridge, hip adduction, and latissimus dorsi (progression) | 6–60 second hold, 5 repetitions each side, 3 times per week |
| 7. Firehydrant | 6–60 second hold, 5 repetitions each side, 3 times per week |
| 7a. Alternating arm-leg raise (progression) | 6–60 second hold, 5 repetitions each side, 3 times per week (no >2.5 minutes each leg) |
| 8. Front plank | 6–60 second hold, 5–10 repetitions, daily |
| 8a. Front plank (progression) | 6–60 second hold, 5–10 repetitions, daily |
| 9. Side plank | 6–60 second hold, 5–10 repetitions each side, 3 times per week (no > 2.5 minutes each side) |
| 10. Isometric: Wall sit, hip abduction, and latissimus dorsi | 6–60 second hold, 5–10 repetitions, 3 times per week |
| 10a. Isometric: Wall sit, hip abduction, and latissimus pull downs (progression) | 20 pull downs, 5 repetitions, 3 times per week |
| 11. Isometric: Wall sit, hip adduction, and latissimus dorsi | 6–60 second hold, 5–10 repetitions, 3 times per week |
| 11a. Isometric: Wall sit, hip abduction, and latissimus dorsi pull downs (progression) | 20 pull downs, 5 repetitions, 3 times per week |
| 12. Isometric: Standing hip abduction | 6–60 second hold, 5–10 repetitions each side, 3 times per week (no >2.5 minutes each side) |
| Phase III: Return to function phase 9–12 months | Phase III: Return to function phase 9–12 months |
| 13. Heel strike to foot flat with latissimus dorsi activation | 5×20 repetitions, each side, performed 3 times per week |
| 13a. Heel strike hop with latissimus dorsi activation (progression) | 3×20 repetitions, each side, performed 3 times per week |
| 14. Front plank progression | 6–60 second hold, 5–10 repetitions each side, daily (no >2.5 minutes per leg); add ankle weight as tolerated |
| 15. Side plank progression | 6–60 second hold, 5–10 repetitions each side, daily (no >2.5 minutes each side); add ankle weight as tolerated |
A stabilisation training video accompanying this paper can be found at http://www.maneyonline.com/doi/suppl/10.1179/2042618614Y.0000000086.S1.
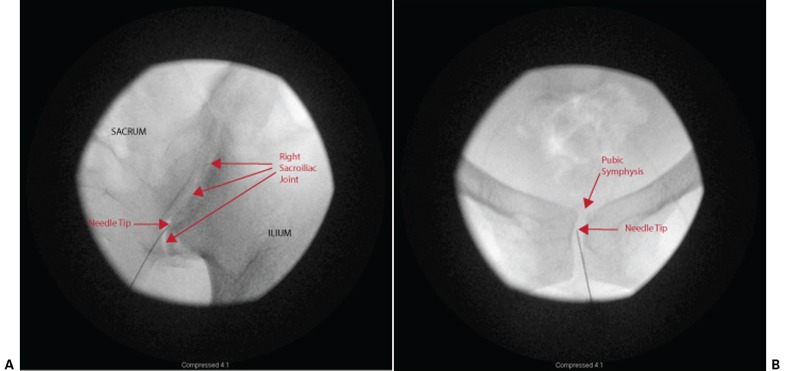
Figure 1.
Sacroiliac joint nutation manipulation positioning for the right sacroiliac joint. To promote locking of the lumbar spine, the patient was positioned in ipsilateral sidebending and contralateral trunk rotation. The ilium was brought into maximum nutation directly by the hands on the pelvis and indirectly through bringing the right hip into greater flexion. The contralateral leg was stabilized into extension. While maintaining the vertical position of the pelvis, the manipulation was performed by rotating the top ilium dorsally.
Figure 2.
Muscle energy technique for pubic symphysis. This technique utilizes reciprocal inhibition of the hip adductors by first performing an isometric contraction of the hip abductors. This is followed by an isotonic contraction of the hip adductors to correct dysfunction at the junction of the pubic symphysis. The patient lies supine in hooklying. The therapist places the palm of each hand over the lateral condyle of the femurs of the patients adducted and flexed knees. With the therapist forearms perpendicular to the distal end of the patients femurs, the patient is then instructs to press out against the resistance of the therapist (A). The therapist then abducts the patient’s legs and places the palm of one hand over the medial aspect of one knee and the bend of the elbow over the medial aspect of the other knee. The patient is then instructed to adduct their legs against the resistance of the therapist for 3–5 seconds (B). The procedure is repeated with further abduction of the patient’s thighs. An audible pop and/or shifting at the level of the pubic symphysis may be heard/felt by the patient.
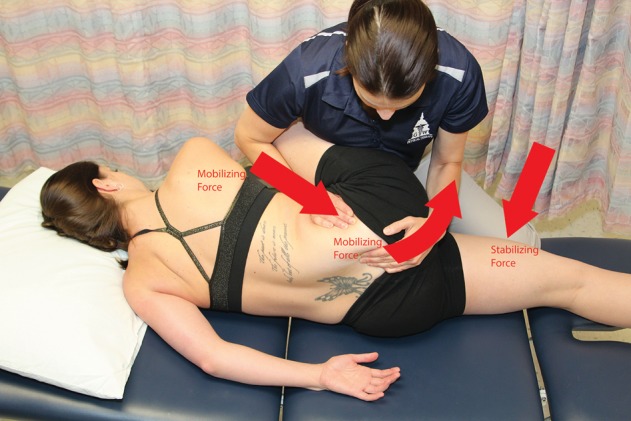
The frequency of prolotherapy injections and target tissue selected vary in the literature; however, this intervention appears to provide adequate pain relief with fewer interventions than steroid treatment.31,32 For this patient’s case, the authors chose a three-injection series protocol for the right sacroiliac joint under fluoroscopic guidance once every 3 weeks in conjunction with her physical therapy plan of care. This frequency was selected to maximize the body’s inflammatory and proliferative repair phases of healing in an effort to increase the amount of collagen regeneration. A fourth injection was performed at 5 months secondary to continued intermittent reports of sacroiliac joint dysfunction and pain monthly during the time of her menses. This procedure included an injection of both the right sacroiliac joint and pubic symphysis in an attempt to maximize the stability of the entire pelvic ring. Each procedure included the following technique: a 25-gauge, 3.5-inch spinal needle was advanced using a bull’s eye technique and bony contact was made. A total of 8 ml of a 10 ml mixture containing 5 ml of 50% dextrose, 3 ml of 0.25% bupivacaine, and 2 ml of 1% lidocaine was peppered along both sides of the joint, periarticularly and intraarticularly (Fig. 3).
Figure 3.
Fluoroscopic images of prolotherapy injection: (A) right sacroiliac joint; (B) pubic symphysis.
Before each procedure, the physical therapist performed the forward flexion test in standing and sitting to observe symmetry. If an asymmetry was present, a manipulation of the sacroiliac joint and a muscle energy technique for the pubic symphysis were performed and the patient was then stabilized with a pelvic ring belt. The belt remained on the patient, but was loosened during the procedure to allow the physician access to the area. The belt was secured immediately following the injection.
Pelvic ring belting was used, in this patient’s case, to provide external force closure, specifically during the protection and controlled motion phases of rehabilitation. It has been suggested that scar tissue is responsive to remodeling up to 14 weeks33 and, after that period, can take 12–18 months33,34 to skeletally mature. In support of collagen maturation, the patient was instructed to wear the pelvic ring belt for 23 hours per day, only to be removed while showering. The belt was worn daily for 9 months and then only at night for an additional 3 months. The patient did not report any episodes of chafing associated with wearing the belt.
Physical therapy focused on progression of stabilization exercises for the lumbo-pelvic girdle. Stabilization training centered around coactivation and endurance training of the transverse abdominus, pelvic floor, and multifidi. Once independent activation without tactile cueing of the foundational muscle groups was established, further training focused on strength and endurance of the gluteal, hip adductor, and abdominal muscle groups, as well as the latissimus dorsi. Activation of these muscle groups was emphasized to improve force closure and dynamic stability of the pelvic ring.35,36
The patient was seen at each phase of exercise progression and then 1 week after to focus on review of the program modifications. Exercises were progressed from non-weight bearing to weight bearing, and from double limb to single limb support (Table 2). All exercises were performed with instruction to maintain transverse abdominus, pelvic floor, and multifidus muscle coactivation. The patient wore the pelvic ring belt at all times. Manipulation of the right sacroiliac joint and pubic symphysis was performed as needed based on findings of the standing and seated forward flexion tests. All manipulations were ceased after the fourth prolotherapy injection series because, at 1-month follow-up and subsequent follow-up appointments, the forward flexion and seated forward flexion test were unremarkable.
During rehabilitation, the patient was instructed to cease yoga and running until stabilization training was completed. The patient was instructed to use a lumbar roll to assist in support of lumbar lordosis and to promote sacral nutation. She was also instructed to avoid long periods of sitting with a posterior pelvic tilt, sustained standing with weight unevenly supported, lying on the affected side, crossing her legs, and sexual intercourse where the hips were abducted and/or flexed to end range.
Outcomes
The patient completed 20 physical therapy sessions over a 12-month period. At 1-year follow-up, her OSW score was 0% indicating no disability associated with her history of sacroiliac joint dysfunction. The patient also reported returning to yoga and low mileage jogging without complaint. See Table 1 for results of all objective measures followed.
Discussion
This is the first report of multimodal and multidisciplinary management of a young woman with chronic unilateral sacroiliac joint pain and pelvic ring dysfunction of traumatic onset. The combination of prolotherapy, specific exercises, manipulative therapy, and pelvic ring belting successfully addressed the patient’s condition. The interventions were aimed at restoring alignment, increasing stability of the patient’s sacroiliac joint through force closure7,24 and at reducing her chronic sacroiliac joint pain.
The effect of sacroiliac joint manipulation on managing sacroiliac joint dysfunction has been examined with positive outcomes, including reduced muscle inhibition,13 improved muscle performance,12 gait symmetry, and improved range of motion and posture.11,37 The literature, however, fails to suggest a specific manipulation technique for treating the sacroiliac joint. A few authors suggest that a nutation manipulation technique, but fail to justify their reasoning for selection,12–14 whereas others select a nutation or counter nutation technique based on clinical examination findings.15 It has been suggested that patients with symptomatic sacroiliac joint dysfunction exhibit more often an anterior rotation of the innominate during single leg support, whereas asymptomatic control patients present with a posterior rotation of the innominate.38 These observed findings may, therefore, support a clinician’s reasoning for manipulation of the sacroiliac joint first in the direction of nutation instead of depending on mobility tests, such as the standing and seated forward flexion test, which exhibit poor sensitivity and reliability.24,25
Pelvic ring belting has been suggested by researchers8,39 to assist with pelvic ring force closure. Electromyography recordings of the psoas, iliacus, transversus abdominus, external and internal obliques, rectus abdominus, rectus femoris, adductor longus, erector spinae, biceps femoris, and gluteus maximus muscles were performed in healthy participants during an ASLR and while treadmill walking. Recordings with and without a belt placed just below the level of the ASIS (high position) were performed. Belting reduced electromyography muscle activity significantly in the transverse abdominus, external and internal obliques during both treadmill walking and the ASLR, and in the iliacus, erector spinae, and biceps femoris during treadmill walking only. In contrast, an increase in muscle activity was observed in the contralateral biceps femoris during the ASLR and in the gluteus maximus during treadmill walking. Therefore, it is postulated that belting may provide increased pelvic ring support and, therefore, the patient will rely less on the stabilizing muscles for maintaining force closure.8,39
The effect of pelvic belt position on sacroiliac joint stability has been examined in asymptomatic and post-partum women with pelvic girdle pain.40,41 The effect of vibration on sacroiliac joint stability was examined using Doppler imaging. Patients wore pelvic support belts positioned high (just below the ASIS) and low (in line with the pubic symphysis). Asymptomatic patients were examined, while prone and post-partum women with pelvic girdle pain were examined while performing an ASLR. In the prone position, belting inferior to the ASIS produced a significantly larger amount of sacroiliac joint stability than belting over the pubic symphysis. Additionally, both belting positions resulted in a significant increase in stability during the ASLR. Pelvic ring belting in either the low or high positions may, therefore, be considered as a temporary solution for supporting the pelvic girdle.
Various authors42,43 have examined the change in sacroiliac joint stability during muscle activation using vertical vibration to the ilium and the adjacent sacrum. In these studies, the amplitude of the vibration through the sacroiliac joint was measured using Doppler imaging during a relaxed state and during activation of the following muscles individually: transverse abdominus, biceps femoris, gluteus maximus, erector spinae, and contralateral latissimus dorsi. Individual activation of each muscle group exhibited a decrease in amplitude, suggesting increased sacroiliac joint stiffness.
Electromyographic studies have recorded differences in muscular recruitment in individuals experiencing sacroiliac joint pain, as compared to healthy controls.44,45 Shadmehr et al.44 reported that participants with sacroiliac joint pain demonstrated decreased tone in their external oblique, biceps femoris, gluteus maximus, and erector spinae during the ASLR.44 Likewise, Hungerford et al.45 found that while performing standing hip flexion, participants with sacroiliac joint pain experienced a delay in the activation of their internal oblique, multifidus, and gluteus maximus on the affected side. Therefore, the introduction of a stabilization program, addressing these muscle groups, may assist in restoring muscle strength and timing resulting in improving pelvic girdle stability.
This case report has several limitations. Although we used validated clinical tests for the diagnosis of sacroiliac joint dysfunction,10,23 we did not perform a sacroiliac joint double anesthetic block.5,46 Additionally, vibration and Doppler have been validated for the assessment of asymmetric sacroiliac joint stiffness,47,48 but were not used in this study. Combining diagnostic blocks with vibration and Doppler imaging may be of assistance when designing future studies to examine management of the dysfunctional sacroiliac joint and determining the best candidate for a multimodal approach to management of sacroiliac joint pain with pelvic ring instability.
Although the passage of time may account for some changes in this patient’s case, a multidisciplinary and multimodal approach to management of a woman with a 14-year history of recurrent sacroiliac joint dysfunction was associated with complete resolution of symptoms at 1-year follow-up. Future research with a larger sample and comparison group should be performed to assess the effect of this multidisciplinary and multimodal management of chronic sacroiliac dysfunction with pelvic ring instability as the findings of this case report cannot be generalized to the population with sacroiliac joint dysfunction.
Disclaimer Statements
Contributors All authors listed were authors on the paper.
Funding None.
Conflicts of interest None.
Ethics approval Not required.
References
- 1.Schwarzer AC, Aprill CN, Bogduk N. The sacroiliac joint in chronic low back pain. Spine (Phila Pa 1976). 1995;20:31–7. doi: 10.1097/00007632-199501000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Maigne JY, Aivaliklis A, Pfefer F. Results of sacroiliac joint double block and value of sacroiliac pain provocation tests in 54 patients with low back pain. Spine (Phila Pa 1976). 1996;21:1889–92. doi: 10.1097/00007632-199608150-00012. [DOI] [PubMed] [Google Scholar]
- 3.Bernard TN, Jr, Kirkaldy-Willis WH. Recognizing specific characteristics of nonspecific low back pain. Clin Orthop Relat Res. 1987;217:266–80. [PubMed] [Google Scholar]
- 4.Cohen SP, Chen Y, Neufeld NJ. Sacroiliac joint pain: a comprehensive review of epidemiology, diagnosis and treatment. Expert Rev Neurother. 2013;13:99–116. doi: 10.1586/ern.12.148. [DOI] [PubMed] [Google Scholar]
- 5.Chou LH, Slipman CW, Bhagia SM, Tsaur L, Bhat AL, Isaac Z, et al. Inciting events initiating injection-proven sacroiliac joint syndrome. Pain Med. 2004;5:26–32. doi: 10.1111/j.1526-4637.2004.04009.x. [DOI] [PubMed] [Google Scholar]
- 6.Cohen SP. Sacroiliac joint pain: a comprehensive review of anatomy, diagnosis, and treatment. Anesth Analg. 2005;101:1440–53. doi: 10.1213/01.ANE.0000180831.60169.EA. [DOI] [PubMed] [Google Scholar]
- 7.Hu H, Meijer OG, van Dieën JH, Hodges PW, Bruijn SM, Strijers RL, et al. Muscle activity during the active straight leg raise (ASLR), and the effects of a pelvic belt on the ASLR and on treadmill walking. J Biomech. 2011;43:532–9. doi: 10.1016/j.jbiomech.2009.09.035. [DOI] [PubMed] [Google Scholar]
- 8.Beales DJ, O’Sullivan PB, Briffa NK. The effects of manual pelvic compression on trunk motor control during an active straight leg raise in chronic pelvic girdle pain subjects. Man Ther. 2010;15:190–9. doi: 10.1016/j.math.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 9.Vleeming A, Buyruk HM, Stoeckart R, Karamursel S, Snijders CJ. An integrated therapy for peripartum pelvic instability: a study of the biomechanical effects of pelvic belts. Am J Obstet Gynecol. 1992;166:1243–7. doi: 10.1016/s0002-9378(11)90615-2. [DOI] [PubMed] [Google Scholar]
- 10.Mens J, Vleeming A, Snijders CJ, Koes BW, Stam HJ. Validity of the active straight leg raise test for measuring disease severity in patients with posterior pelvic pain after pregnancy. Spine. 2002;27:196–200. doi: 10.1097/00007632-200201150-00015. [DOI] [PubMed] [Google Scholar]
- 11.Stolinski L, Kotwicki T. Change of the child’s posture after sacroiliac joint manipulation: Improved symmetry assessed with the POTSI index. Scoliosis. 2012;7(Suppl 1):O65. [Google Scholar]
- 12.Marshall P, Murphy B. The effect of sacroiliac joint manipulation feed-forward activation times of the deep abdominal musculature. J Manipulative Physiol Ther. 2006;29:196–202. doi: 10.1016/j.jmpt.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 13.Orakifar N, Kamali F, Pirouzi S, Jamshidi F. Original article: sacroiliac joint manipulation attenuates alpha-motoneuron activity in healthy women: a quasi-experimental study. Arch Phys Med Rehabil. 2012;93:56–61. doi: 10.1016/j.apmr.2011.05.027. [DOI] [PubMed] [Google Scholar]
- 14.Kamali F, Shokri E. The effect of two manipulative therapy techniques and their outcome in patients with sacroiliac joint syndrome. J Bodywork Movement Ther. 2012;16:29–35. doi: 10.1016/j.jbmt.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 15.Grassi Dde O, de Souza MZ, Ferrareto SB, Montebelo MI, Guirro EC. Immediate and lasting improvements in weight distribution seen in baropodometry following a high-velocity, low-amplitude thrust manipulation of the sacroiliac joint. Man Ther. 2011;16:495–500. doi: 10.1016/j.math.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 16.Mooney V, Pozos R, Vleeming A, Gulick J, Swenski D. Exercise treatment for sacroiliac pain. Orthopedics. 2001;24:29–32. doi: 10.3928/0147-7447-20010101-14. [DOI] [PubMed] [Google Scholar]
- 17.Stuge B, Veierod MB, Laerum E, Vollestad N. The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy: a two-year follow-up of a randomized clinical trial. Spine (Phila Pa 1976). 2004;29:E197–203. doi: 10.1097/00007632-200405150-00021. [DOI] [PubMed] [Google Scholar]
- 18.Srejic U, Calvillo O, Kabakibou K. Viscosupplementation: a new concept in the treatment of sacroiliac joint syndrome: a preliminary report of four cases. Reg Anesth Pain Med. 1999;24:84–8. doi: 10.1016/s1098-7339(99)90170-0. [DOI] [PubMed] [Google Scholar]
- 19.Yin W, Willard F, Carreiro J, Dreyfuss P. Sensory stimulation-guided sacroiliac joint radiofrequency neurotomy: technique based on neuroanatomy of the dorsal sacral plexus. Spine (Phila Pa 1976). 2003;28:2419–25. doi: 10.1097/01.BRS.0000085360.03758.C3. [DOI] [PubMed] [Google Scholar]
- 20.Cohen SP, Abdi S. Lateral branch blocks as a treatment for sacroiliac joint pain: a pilot study. Reg Anesth Pain Med. 2003;28:113–9. doi: 10.1053/rapm.2003.50029. [DOI] [PubMed] [Google Scholar]
- 21.Dabezies EJ, Millet CW, Murphy CP, Acker JH, Robicheaux RE, D’Ambrosia RD. Stabilization of sacroiliac joint disruption with threaded compression rods. Clin Orthop Relat Res. 1989;246:165–71. [PubMed] [Google Scholar]
- 22.Waisbrod H, Krainick JU, Gerbershagen HU. Sacroiliac joint arthrodesis for chronic lower back pain. Arch Orthop Trauma Surg. 1987;106:238. doi: 10.1007/BF00450461. [DOI] [PubMed] [Google Scholar]
- 23.Laslett M, Aprill CN, McDonald B, Young SB. Original article: diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of tests. Man Ther. 2005;10:207–18. doi: 10.1016/j.math.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 24.Dreyfuss P, Dryer S, Griffin J, Hoffman J, Walsh N. Positive sacroiliac screening tests in asymptomatic adults. Spine (Phila Pa 1976). 1994;19:1138–43. doi: 10.1097/00007632-199405001-00007. [DOI] [PubMed] [Google Scholar]
- 25.Riddle DL, Freburger JK. Evaluation of the presence of sacroiliac joint region dysfunction using a combination of tests: a multicenter intertester reliability study. Phys Ther. 2002;82:772–81. [PubMed] [Google Scholar]
- 26.American Physical Therapy Association. Guide to Physical Therapist Practice. Second Edition. American Physical Therapy Association. Phys Ther. 2001;81:9. [PubMed] [Google Scholar]
- 27.Winkle D, Aufdemkampe G, Matthijs O, Meijer O, Phelps V. Diagnosis and treatment of the spine. Gaithersburg: Aspen; 1996. p. 968. [Google Scholar]
- 28.Chaitow L. Muscle energy techniques. 4th ed. London: Churchill Livingston Elsevier; 2013. [Google Scholar]
- 29.Nelson P, Apte G, Justiz R, 3rd, Brismee JM, Dedrick G, Sizer PS., Jr Chronic female pelvic pain — Part 2: Differential diagnosis and management. Pain Pract. 2012;12:111–41. doi: 10.1111/j.1533-2500.2011.00492.x. [DOI] [PubMed] [Google Scholar]
- 30.Banks A. A rational for prolotherapy. J Orthop Med. 1991;13:54. [Google Scholar]
- 31.Kim WM, Lee HG, Won Jeong C, Kim CM, Yoon MH. A randomized controlled trial of intra-articular prolotherapy versus steroid injection for sacroiliac joint pain. J Altern Complement Med. 2010;16:1285–90. doi: 10.1089/acm.2010.0031. [DOI] [PubMed] [Google Scholar]
- 32.Cusi M, Saunders J, Hungerford B, Wisbey-Roth T, Lucas P, Wilson S. The use of prolotherapy in the sacroiliac joint. Br J Sports Med. 2010;44:100–4. doi: 10.1136/bjsm.2007.042044. [DOI] [PubMed] [Google Scholar]
- 33.Cummings GS, Tillman LJ. Remodeling of dense connective tissue in normal adult tissue. In: Currier DP, Nelson RM, editors. Dynamics of human biologic tissues. Philadelphia, PA: F.A. Davis; 1992. p. 45. [Google Scholar]
- 34.Enwemeka CS. Connective tissue plasticity: ultrastructural, biomechanical, and morphometric effects of physical factors on intact and regenerating tendons. J Orthop Sports Phys Ther. 1991;14:198–212. doi: 10.2519/jospt.1991.14.5.198. [DOI] [PubMed] [Google Scholar]
- 35.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000;25:2940–52. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 36.Cusi M, Saunders J, van der Wall H, Fogelman I. Metabolic disturbances identified by SPECT–CT in patients with a clinical diagnosis of sacroiliac joint incompetence. Eur Spine J. 2013;22:1674–82. doi: 10.1007/s00586-013-2725-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pollard H, Ward G. The effect of upper cervical or sacroiliac manipulation on hip flexion range of motion. J Manipulative Physiol Ther. 1998;21:611–6. [PubMed] [Google Scholar]
- 38.Hungerford B, Gilleard W, Lee D. Altered patterns of pelvic bone motion determined in subjects with posterior pelvic pain using skin markers. Clin Biomech. 2004;19:456–64. doi: 10.1016/j.clinbiomech.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 39.Kim YR, Kim JW, An DH, Yoo WG, Oh JS. Effects of a pelvic belt on the EMG activity of the abdominal muscles during a single-leg hold in the hook-lying position on a round foam roll. J Phys Ther Sci. 2013;25:793–5. doi: 10.1589/jpts.25.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Damen L, Spoor CW, Snijders CJ, Stam HJ. Does a pelvic belt influence sacroiliac joint laxity? Clin Biomech (Bristol, Avon). 2002;17:495–8. doi: 10.1016/s0268-0033(02)00045-1. [DOI] [PubMed] [Google Scholar]
- 41.Mens JM, Damen L, Snijders CJ, Stam HJ. The mechanical effect of a pelvic belt in patients with pregnancy-related pelvic pain. Clin Biomech (Bristol, Avon). 2006;21:122–7. doi: 10.1016/j.clinbiomech.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 42.van Wingerden JP, Vleeming A, Buyruk HM, Raissadat K. Stabilization of the sacroiliac joint in vivo: verification of muscular contribution to force closure of the pelvis. Eur Spine J. 2004;13:199–205. doi: 10.1007/s00586-003-0575-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Richardson CA, Snijders CJ, Hides JA, Damen L, Pas MS, Storm J. The relation between the transversus abdominis muscles, sacroiliac joint mechanics, and low back pain. Spine. 2002;27:399–405. doi: 10.1097/00007632-200202150-00015. [DOI] [PubMed] [Google Scholar]
- 44.Shadmehr A, Jafarian Z, Talebian S. Changes in recruitment of pelvic stabilizer muscles in people with and without sacroiliac joint pain during the active straight-leg-raise test. J Back Musculoskelet Rehabil. 2012;25:27–32. doi: 10.3233/BMR-2012-0307. [DOI] [PubMed] [Google Scholar]
- 45.Hungerford B, Gilleard W, Hodges P. Evidence of altered lumbopelvic muscle recruitment in the presence of sacroiliac joint pain. Spine. 2003;28:1593–600. [PubMed] [Google Scholar]
- 46.Rupert MP, Lee M, Manchikanti L, Datta S, Cohen SP. Evaluation of sacroiliac joint interventions: a systematic appraisal of the literature. Pain Physician. 2009;12:399–418. [PubMed] [Google Scholar]
- 47.Damen L, Stijnen T, Roebroeck ME, Snijders CJ, Stam HJ. Reliability of sacroiliac joint laxity measurement with Doppler imaging of vibrations. Ultrasound Med Biol. 2002;28:407–14. doi: 10.1016/s0301-5629(02)00491-x. [DOI] [PubMed] [Google Scholar]
- 48.Damen L, Buyruk HM, Guler-Uysal F, Lotgering FK, Snijeders CJ, Stam HJ. The prognostic value of asymmetric laxity of the sacroiliac joints in pregnancy-related pelvic pain. Spine. 2002;27:2820–4. doi: 10.1097/00007632-200212150-00018. [DOI] [PubMed] [Google Scholar]