This article has supplementary material on the Web site: www.jdbp.org.
Index terms: infant sleeping, infant crying, settling, parenting
ABSTRACT:
Objective:
Most infants become settled at night by 3 months of age, whereas infants not settled by 5 months are likely to have long-term sleep-waking problems. We assessed whether normal infant development in the first 3 months involves increasing sleep-period length or the ability to resettle autonomously after waking in the night.
Methods:
One hundred one infants were assessed at 5 weeks and 3 months of age using nighttime infrared video recordings and parental questionnaires.
Results:
The clearest development was in sleep length; 45% of infants slept continuously for ≥5 hours at night at 3 months compared with 10% at 5 weeks. In addition, around a quarter of infants woke and resettled themselves back to sleep in the night at each age. Autonomous resettling at 5 weeks predicted prolonged sleeping at 3 months suggesting it may be a developmental precursor. Infants reported by parents to sleep for a period of 5 hours or more included infants who resettled themselves and those with long sleeps. Three-month olds fed solely breast milk were as likely to self-resettle or have long sleep bouts as infants fed formula or mixed breast and formula milk.
Conclusions:
Infants are capable of resettling themselves back to sleep in the first 3 months of age; both autonomous resettling and prolonged sleeping are involved in “sleeping through the night” at an early age. Findings indicate the need for physiological studies of how arousal, waking, and resettling develop into sustained sleeping and of how environmental factors support these endogenous and behavioral processes.
Infant waking and crying out at night is the earliest and most common type of infant sleep problem, reported in around 20% to 30% of infants in many countries.1,2 Most such infants are healthy,2,3 but their unsettled nighttime behavior may exhaust or depress parents and incur substantial health service costs.4–6 A better understanding should help many families and improve service cost-effectiveness.
Recent research has suggested a “developmental-behavioral” explanation for how infant night waking and crying comes about. First, infrared video recordings have shown the popular belief that older infants “sleep through the night” to be wrong: most infants continue to wake up in the night.7–9 Mature sleep waking involves the ability to resettle to sleep after waking, as well as prolongation of nighttime sleep periods.8 Infants who continue to cry out and receive parental involvement to resettle have been called “signalers” to distinguish them from those who develop autonomous resettling.8 The difference between settled and unsettled infants may often lie not in a sleep disorder so much as in how they behave on waking at night.
Second, evidence has accumulated that the process of consolidating settled behavior into the night usually takes place in the first 3 to 4 months of age.10–12 For instance, English parents reported that just 20% of infants slept for a period of 5 hours or more during most nights measured at 3 weeks, whereas 70% of the same infants did so at 3 months of age.12 Infants who do not become settled at night early on are at increased risk of later sleep-waking problems. For instance, Bavarian infants who were not settled at 5 months were 2 to 3.5 times more likely than other infants to wake and signal in the night at 20 months of age.13,14
Building on these findings, this study is designed to clarify the infant developmental processes involved in becoming settled at night by 3 months of age. It has 2 aims:
To assess whether infant development in the first 3 months involves increasing the length of sleep periods or acquiring the ability to resettle back to sleep autonomously after waking in the night. Including its relevance to research, the answer to this question has clinical implications since the UK National Health Service Web site “NHS Choices” has queried whether infants are able to settle themselves at an early age.15
To measure changes in infant sucking behavior during this period, because sucking has been considered a self-regulatory behavior for initiating or maintaining sleep.16 “Self-regulatory behaviors” are those developed by an individual to manage his or her arousal as opposed to external regulation provided by caregivers and other parts of the environment.8
Most studies of infant crying and sleeping have used parental reports. Those are needed to assess the impact of infant signaling on parents, but parents are often unaware of infant waking that does not include signaling.17 Of more objective methods available, polygraphy can disturb infant sleeping and actigraphy, which measures limb movement, is insensitive to the open-eyed waking periods typical of infants.18 Instead, we used nighttime infrared video recording methods proven valid for this purpose.7,8,18 Anders et al have pioneered “videosomnography” methods but, to our knowledge, they have not been used before to distinguish prolonged sleeping from waking and resettling during this important early period for sleep-waking development.
METHODS
Recruitment of Participants
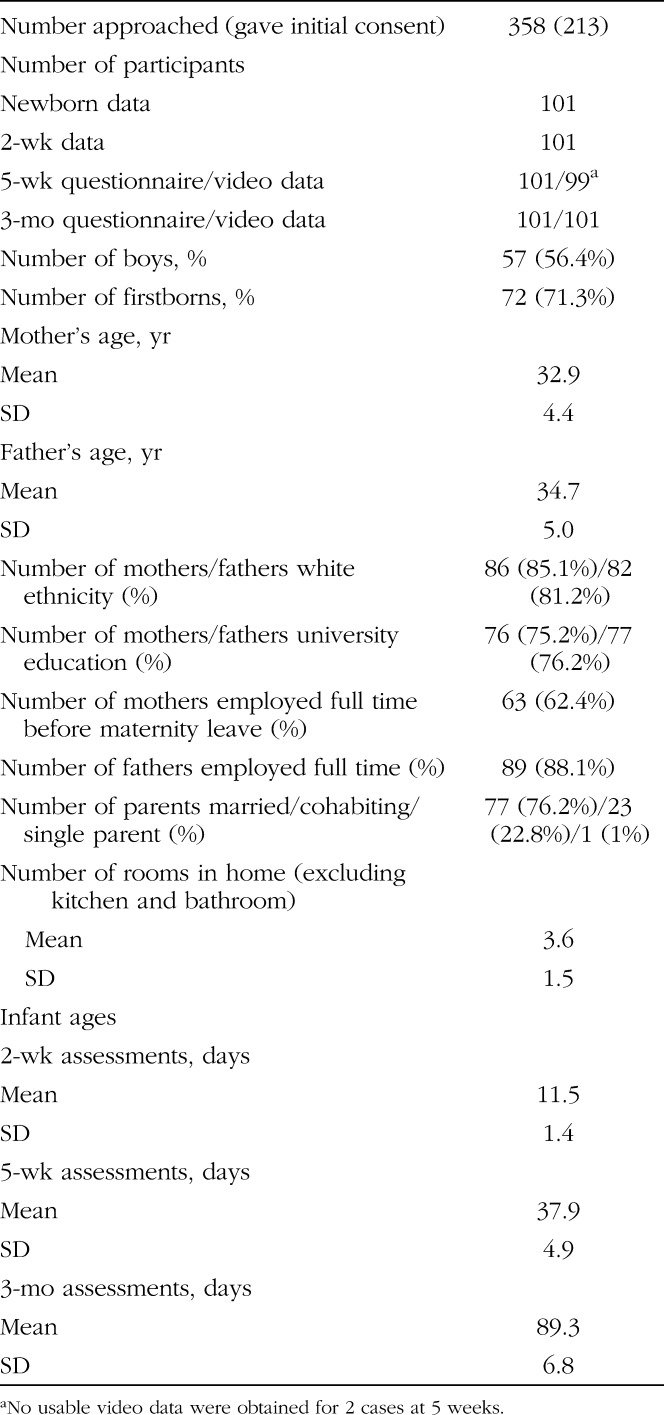
Participants were mothers and breast-fed singleton newborn infants living within the M25 motorway around London, approached in postnatal wards of a community maternity hospital (N = 101). We excluded multiple births, infants with birth weight <2500 g, admitted to special care or who medical staff considered unwell, and mothers with limited English. Otherwise, mothers were approached consecutively, introduced to the study, and asked to allow a telephone call to explain the research fully after they returned home. Mothers who agreed gave written informed consent. Table 1 lists recruitment, participant, and missing data.
Table 1.
Descriptive Figures for Recruitment, Attrition, and Participants' Characteristics
Assessments
Home visits to collect data were made when infants were 2 weeks (2W), 5 weeks (5W), and 3 months (3M) old. Full written informed consent and demographic information were collected at the 2W visit. Parents also completed questionnaire measures of parenting and infant behavior at each visit, which will be examined in full elsewhere (St James-Roberts I, Roberts M, Hovish K, et al, unpublished data, 2015).
Video data were collected at the 5W and 3M visits. Following previous studies,8,18,19 researchers installed a self-focusing digital infrared video camera (Sony HDR-XR200VE) on a tripod directed at the infant's usual nighttime sleep location allowing up to 13 hours of continuous recording. Parents were instructed in using the camera and asked to switch it on when they began settling their infant to sleep at night and off the next morning. They were asked to follow their usual nighttime habits and could switch the equipment off at any time they judged necessary. The video was checked by researchers the next day and, if technical problems had arisen, 1 further attempt was made to obtain a recording. Because of their extensive assistance with data collection, parents received high street shopping vouchers of value £100 on returning the 3M data. The study received ethical approval from Riverside Medical Research Ethics Committee (REC 09/H0706/11).
Video Data Coding and Analysis
The data were computer coded in Excel spreadsheets by researchers using written manuals who were trained to >90% reliability and blinded to participants' other data. The Excel data were exported to SPSS 2220 for analysis. Video coding rules were based on Anders' methods and conventional definitions of infant behavior states.7,8 Two stages occurred. First, the iMovie application in an Apple Mac computer was set to display successive 10-second behavior “clips”. The infant's predominant behavior state (lasting >5 seconds) in each clip was then coded as 1 of 8 predefined mutually exclusive categories: sleep, drowsy, awake content, awake crying or fussing, awake feeding, indeterminate, out of view, and video switched off. Table 2 gives definitions for the behaviors. Codes stored on the video gave the time the video started, of each clip, and when the recorder was switched off.
Table 2.
Definitions for Infant Behavior States and Other Video Categories
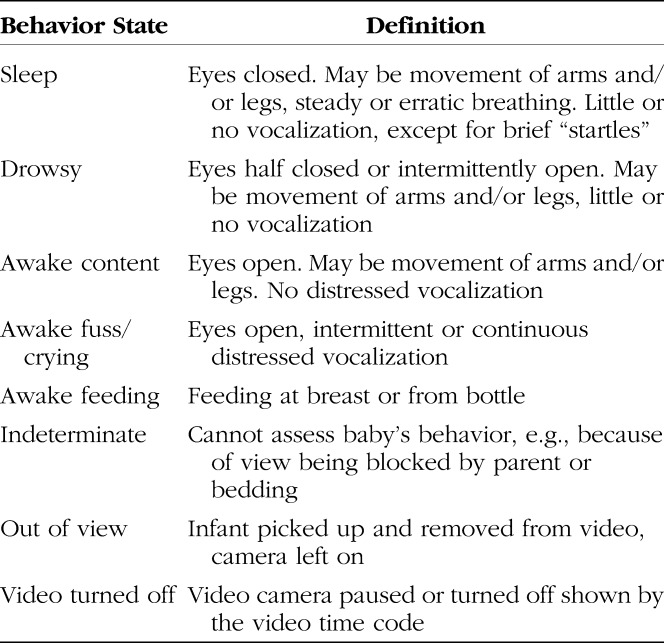
Stage 2 identified the main behavior periods, isolated 10-second codes, and period transitions again using trained blinded researchers and manualized procedures. Five period types were distinguished: awake, sleep, indeterminate, out of view, and video turned off. Awake periods required a continuous sequence of awake codes (awake content, fuss/crying, or feeding) lasting at least 30 seconds; sleep and other periods required a continuous sequence of codes lasting at least 5 minutes. The infant's behavior after the video started defined the first period. Each period continued until a different period type met criteria. These rules do not discard any coded behaviors. They assign the behaviors to one or the other period type, so that measures can be made of the periods and amounts of time spent in each behavior state in each period and overall. Infant sucking behaviors (sucking fingers or hands, sucking a dummy/pacifier) were coded separately in the same way, as were the time and duration of each “direct parental contact” (touching, holding, or speaking to an infant) and “checking” (approach to an infant without direct contact). Measures were computed of the time and length of waking and sleeping periods, whether the infant signaled (fuss/cried) during these periods, how long any signaling lasted, whether a parent checked or made direct contact with the infant during the period, and the amount of infant sucking behavior during sleep and waking periods.
To confirm coding reliability, 20 videos were duplicate coded by independent coders. Between-coder Pearson correlations were 1.00 (video turned off, out of view); 0.862 (indeterminate); 0.985 (sleep); 0.861 (awake content); 0.883 (fuss/crying).
RESULTS
Most participants were of white ethnicity, highly educated, and married or cohabiting (Table 1). All infants were fed breast milk in the newborn period; 64.4% (65) were still fed breast milk at 3M. Most (93.1%) infants initially slept in cots next to their parents' bed or elsewhere in the parents' bedroom.
Video Measures of Infant Sleep-Waking Development
On an average, video recording at 5W began at 10:20 pm and lasted for 9 hours 03 minutes, starting at 9:44 pm and lasting 10 hours 09 minutes at 3M, providing approximately 1000 hours of recording per age. Table 3 provides detailed figures.
Table 3.
Descriptive Figures for the Video Measures
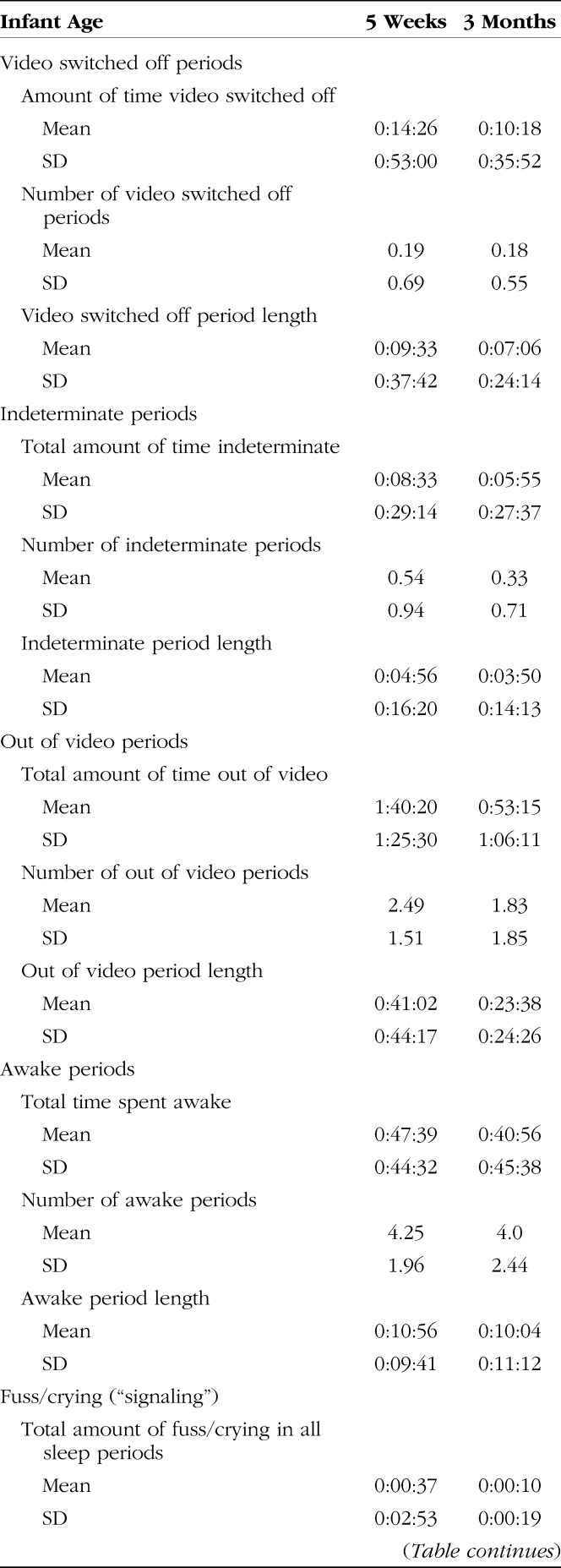
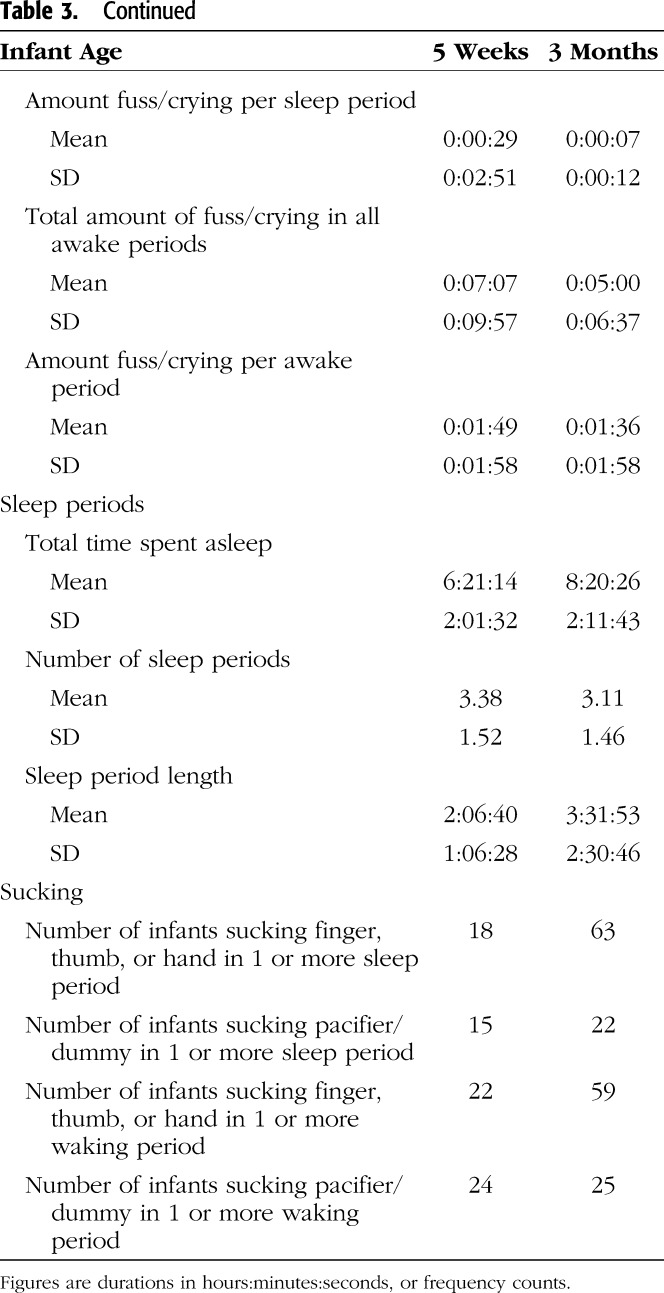
Infant waking totaled approximately 40–50 minutes per night at both 5W and 3M with no clear change with age. The clearest developmental progression was in sleep periods, which lengthened significantly from a mean of 2 hours 07 minutes at 5W to 3 hours 32 minutes at 3M resulting in a significant increase in total sleep of almost 2 hours per night at 3M.
Approximately, one quarter of infants woke and resettled back to sleep without direct parental contact at least once during the night at each age (27 at 5W and 23 at 3M) without a clear age difference. Of these “self-resettlers,” most (14 at 5W, 12 at 3M) woke and settled back to sleep without signaling. Others (10 at 5W, 4 at 3M) woke and fuss/cried briefly, then resettled themselves without a parental intervention. The mean (SD) length of signaling in these cases was 1 minute 8 seconds (1 minute 5 seconds) at 5W and 1 minute 19 seconds (1 minute 19 seconds) at 3M. A few infants (3 at 5W, 7 at 3M) showed both types of self-resettling in the same night. With parental permission, a 3-minute video extract of a study baby waking and self-resettling at 3 months of age can be seen in Supplemental Digital Content 1, http://links.lww.com/JDBP/A76.
One community infant was awake or out of view throughout the 5W recording. The number of infants with video-recorded sleep periods lasting 5 hours or more increased from 10 of 98 at 5W to 45 of 98 at 3M (Fisher's exact test, 2 sided, p = .040). Of these 98 infants, 66.7% (18 of 27) self-resettlers at 5W had sleep of 5 hours or more at 3M compared with 38.0% (27 of 71) infants without self-resettling or long sleeps at 5W (Fisher's exact test, 2 sided, p = .013). Self-resettling at 5W predicted prolonged sleeping at 3M.
At 3M, 67 parents reported that their baby slept continuously for a period of 5 hours or more during most (≥4) nights in the last week compared with 45 infants who slept for a period of 5 hours or more in the video records. In cross-tabulations, all 45 infants who had video recorded ≥5 hour sleep periods along with 16 of 23 videoed self-resettlers were included in the parents' 67 cases: 23.9% of 3M infants reported by parents to sleep for periods of 5 hours or more actually woke and resettled autonomously.
The numbers of infants sucking their fingers or hands during sleep and waking periods more than trebled between 5W and 3M, the increase from 18 to 63 infants doing so during sleep periods being significant (Fisher's exact test, 2 sided, p = .036). Numbers sucking a pacifier/dummy increased little (Table 3). On average, 3M community infants with sleep period of 5 or more hours spent 8 minutes 25 seconds per sleep period sucking fingers or hands compared with 1 minute 13 seconds among other infants (analysis of variance, 1 df, F = 10.01, p = .002).
Feed Constituents
The constituents of breast milk have been assumed to lead infants to need to feed frequently causing night waking.21 However, 2 randomized control trials found settled nighttime behavior in breast milk–fed infants.12,22 To explore this, we cross tabulated whether infants did, versus did not, resettle themselves or sleep continuously for periods of 5 hours or more at 3M against whether they were fed solely breast milk versus formula or mixed breast and formula. Among infants who resettled themselves or slept for a period of 5 hours or more at 3M, 65.6% (40 of 61) were fed solely breast milk, whereas 62.5% (25 of 40) infants who did not resettle or sleep for 5 hours or more were fed solely breast milk, which is not significantly different (Fisher's exact test, 2 sided, p = .833).
DISCUSSION
Although many studies have attempted to treat infant sleep problems, fewer have tried to prevent them and with mixed results.5,23 Arguably, prevention needs to be based on an understanding of how sleep waking normally develops. To that end, this study used video recording and parental questionnaire methods to observe 101 London infants' normal nighttime sleep-waking behaviors at home during the first 3 months of age, the period when most western infants become settled at night. There are 2 main findings.
First, the clearest infant developmental change was in the length of sleep periods, such that the average length of sleeps increased by 80 minutes and total nighttime sleep by almost 2 hours between 5 weeks and 3 months of age, a remarkable achievement in 8 weeks. However, another infant ability, whereby infants woke and resettled themselves back to sleep without parental intervention was also observed in around a quarter of infants. This did not become more common with age but did predict longer nighttime sleep periods at 3 months suggesting that it may be a developmental precursor of sustained sleeping. Parents were often unaware of this waking, so that most of these infants were included among those reported by parents to sleep continuously for periods of 5 hours or more at 3 months. The implication is that around one quarter of the approximately 70% of 3-month-old infants reported to “sleep through the night” by parents10,24 in fact wake up and resettle themselves.
This finding confirms young infants' ability to settle themselves back to sleep with little or no distress15 and indicates the need for physiological studies of how arousal, waking, and resettling develop into sustained sleeping. If mature sleeping involves arousal and resettling, as Anders et al and others25 have found, there is a need for theory-guided research into how the ultradian, circadian, and homeostatic systems that regulate sleep waking26 develop during this early period. Including electroencephalographic and other physiological measures in future studies should help to clarify these endogenous developments. Since it is easy to understand that rapid parental response may influence infant autonomous resettling, environmental support for these endogenous and behavioral processes is a promising avenue for research. The constituents of breast milk have been assumed to underlie the need for night waking.21 The analyses of this issue performed here were exploratory, but feeding solely breast milk did not account for the night waking of 3-month-old infants here or in 2 controlled studies.12,22
Our second finding was that this developmental progression in sleep length was accompanied by an increased use of sucking hands or fingers by infants with long sleep periods, a strategy, which may help them to initiate or maintain their sleep.16 The implication is that many 3-month-old infants use self-regulatory strategies to prolong sleeping. If so, we need to understand how these strategies develop and which factors support this development.
These findings need to be interpreted in light of the methodological limitations of this study including that participants were highly educated, largely white parents in stable relationships in London, and reliance on only 1 night of video recording at 2 ages. As Table 3 shows, not much observation time was lost because of the video being switched off or infant behavior being unclear, but parents removed infants from the video recording for substantial periods (1 hour 40 minutes at 5W; 53 minutes at 3M) largely for feeding and care (only 9 of 99 infants were recorded feeding at 5 weeks). This is unlikely to distort the findings reported but is a limitation of the video methods used here. Since our aim was to measure infant sleep-waking development in normal home settings, we did not attempt to standardize the infants' sleep environments. However, future studies that do so and control for infant sleep-waking in the period before measurement should increase our understanding. Assessment of infant temperament influences on sleep-waking will also be worthwhile.
In conclusion, this study has found that infants are capable of resettling themselves back to sleep in the night in the first 3 months of age and that both autonomos resettling and prolonged sleeping are involved in becoming settled at night during this period. Findings indicate the need for studies of how arousal, waking, and resettling develop into sustained sleeping and of how environmental factors support these endogenous and behavioral processes. If they fulfill their promise, the findings may eventually help to resolve the puzzle of why so many healthy infants should be diagnosed with sleep problems, as well as helping the families involved.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank the families who participated and the staff of Queen Charlotte's and Chelsea Hospital for their support.
Footnotes
Supported by project grant 085752 from the Wellcome Trust, United Kingdom.
Disclosure: The authors declare no conflict of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jdbp.org).
This study was approved by Riverside Research Ethics Committee (REC 09/H0706/11) and full written informed consent was given by all participating parents.
REFERENCES
- 1.Mindell JA, Sadeh A, Wiegand B, et al. Cross-cultural differences in infant and toddler sleep. Sleep Med. 2010;11:274–280. [DOI] [PubMed] [Google Scholar]
- 2.Sadeh A, Sivan Y. Clinical practice: sleep problems during infancy. Eur J Pediatr. 2009;168:1159–1164. [DOI] [PubMed] [Google Scholar]
- 3.Mindell JA. Children and sleep. In: Pressman MR, Orr WC. eds. Understanding Sleep: The Evaluation and Treatment of Sleep Disorders. Washington, DC: American Psychological Association; 2008:427–440. [Google Scholar]
- 4.Dennis C, Ross L. Relationships among infant sleep patterns, maternal fatigue and development of depressive sympomatology. Birth. 2005;32:187–193. [DOI] [PubMed] [Google Scholar]
- 5.Stremler R, Hodnett E, Kenton L, et al. Effect of behavioural-educational intervention on sleep for primiparous women and their infants in early postpartum: multisite randomised controlled trial. BMJ. 2013;346:f1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morris S, St James-Roberts I, Sleep J, et al. Economic evaluation of strategies for managing infant crying and sleeping problems in the first 12 weeks of age: the COSI study. Arch Dis Child. 2001;84:15–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anders TF, Keener M. Developmental course of nighttime sleep-wake patterns in full-term and premature infants during the first year of life. Sleep. 1985:8;173–192. [DOI] [PubMed] [Google Scholar]
- 8.Goodlin-Jones BL, Burnham M, Gaylor E, et al. Night waking, sleep-wake organisation, and self-soothing in the first year of life. J Dev Behav Pediatr. 2001;22:226–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Minde K, Popiel K, Leos N, et al. The evaluation and treatment of sleep disturbances in young children. J Child Psychol Psychiatry. 1993;34:521–533. [DOI] [PubMed] [Google Scholar]
- 10.Moore T, Ucko L. Night waking in early infancy: part 1. Arch Dis Child. 1957;32:333–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Henderson JM, France KG, Owens JL, et al. Sleeping through the night: the consolidation of self-regulated sleep across the first year of life. Pediatrics. 2010;126:e1081–e1087. [DOI] [PubMed] [Google Scholar]
- 12.St James-Roberts I, Sleep J, Morris S, et al. Use of a behavioural programme in the first 3 months to prevent infant crying and sleep problems. J Paediatr Child Health. 2001;37:289–297. [DOI] [PubMed] [Google Scholar]
- 13.Wolke D, Meyer R, Ohrt B, et al. The incidence of sleeping problems in pre-term and full-term infants discharged from neonatal special care units: an epidemiological longitudinal study. J Child Psychol Psychiatry. 1995;36:203–225. [DOI] [PubMed] [Google Scholar]
- 14.Wolke D, Meyer R, Ohrt B, et al. Co-morbidity of crying and sleeping problems with feeding problems in infancy: concurrent and predictive associations. Early Dev Parent. 1995;4:191–208. [Google Scholar]
- 15.NHS Choices 2013. Dubious claims that crying babies self-soothe. Available at: http://www.nhs.uk/news/2013/01january/pages/dubious-claims-that-crying-babies-self-soothe.aspx. Accessed December 1, 2014.
- 16.Burnham MM, Goodlin-Jones BL, Gaylor EE, et al. Use of sleep aids during the first year of life. Pediatrics. 2002;109:594–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sadeh A. Evaluating night waking in sleep disturbed infants: a methodological study of parental reports and actigraphy. Sleep. 1996;19:757–762. [DOI] [PubMed] [Google Scholar]
- 18.Sitnick SL, Goodlin-Jones BL, Anders TF. The use of actigraphy to study sleep disorders in preschoolers: some concerns about detection of nighttime awakenings. Sleep. 2008;31:395–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ball HL. Bed-sharing practices of initially breastfed infants in the first 6 months of life. Infant Child Dev. 2007;16:387–401. [Google Scholar]
- 20.IBM. SPSS Version 22. New York, NY: New York IBM; 2013.
- 21.Blurton-Jones N. Ethological Studies of Child Behaviour. Cambridge, United Kingdom: Cambridge University Press; 1972. [Google Scholar]
- 22.Pinilla T, Birch L. Help me make it through the night: behavioural entrainment of breast-fed infants' sleep patterns. Pediatrics. 1993;91:436–444. [PubMed] [Google Scholar]
- 23.Hiscock H, Cook F, Bayer J, et al. Preventing early infant sleep and crying problems and postnatal depression: a randomized trial. Pediatrics. 2014;133:e346–e354. [DOI] [PubMed] [Google Scholar]
- 24.Sadeh AA. Brief screening questionnaire for infant sleep problems: validation and findings for an internet sample. Pediatrics. 2004;113: e570–e577. [DOI] [PubMed] [Google Scholar]
- 25.Halász P, Terzano M, Parriono L, et al. The nature of arousal in sleep. J Sleep Res. 2004;13:1–23. [DOI] [PubMed] [Google Scholar]
- 26.Borbély AA, Acherman P. Sleep homeostasis and models of sleep regulation. J Biol Rhythms. 1999;14:559–568. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


